Abstract
Reproductive aging impacts women’s health through fertility decline, disease susceptibility, and systemic aging. This study explores the retinal age gap—the difference between predicted retinal age and chronological age—as a novel biomarker for reproductive aging. By developing a Swin-Transformer-based dual-channel transfer learning model with data from 1294 healthy women, we examined associations between the retinal age gap and Anti-Müllerian Hormone (AMH), a key marker of ovarian reserve. Findings revealed a negative association between the retinal age gap and AMH levels, particularly among women aged 40–50. Lower AMH levels correlated with earlier reproductive aging milestones, emphasizing the predictive value of retinal aging. Genetic data from genome-wide association studies further supported these associations and enhanced AMH prediction through multimodal modeling. These findings highlight the retinal age gap as a promising, non-invasive biomarker for reproductive aging and its potential role in disease prediction and personalized health interventions in women.
Similar content being viewed by others
Introduction
Reproductive aging is a complex biological process influenced by various hormonal, genetic, and environmental factors. As women age, the decline in ovarian reserve significantly impacts fertility, highlighting the need for reliable biomarkers to assess reproductive aging1. Anti-Müllerian Hormone (AMH) is widely recognized as a robust biomarker for ovarian reserve2,3, offering valuable insights into reproductive potential4,5. However, current method for measuring AMH levels involves invasive procedures, and its accuracy is subject to variability due to hormonal fluctuations. This underscores the need for complementary indicators using noninvasive measurement methods to enhance predictive accuracy.
Notably, AMH levels have also been linked to vascular aging, with studies showing correlations between AMH and markers of vascular health6,7, including intima-media thickness, coronary artery calcification6, and chronic kidney disease8. These findings suggest a bidirectional relationship, where vascular aging could serve as a proxy for ovarian aging.
Noninvasive retinal imaging has emerged as a novel tool to leverage this connection. Retinal fundus imaging captures microvascular features in the eye that reflect systemic aging9,10,11. Advances in artificial intelligence have further enabled the calculation of the retinal age gap, defined as the difference between predicted retinal age and chronological age. This measure has shown potential as a biomarker for both biological and reproductive aging12,13,14,15,16,17, including stroke12, kidney diseases14, Parkinson’s disease15, central obesity16, as well as mortality risk and age-related diseases13,17. Given the vascular underpinnings of both retinal and ovarian aging, retinal imaging may represent a groundbreaking, non-invasive approach to predicting AMH levels and, by extension, reproductive health.
In this study, we introduce the Frozen and Learning Ensemble Crossover (FLEX), a deep learning framework designed to predict retinal age from fundus images with high precision. By leveraging fundus images and incorporating healthy model weights derived from healthy cohorts (Fig. 1a), we developed the FLEX model using data from the Healthy Female Cohort and examined the association between the retinal age gap and AMH levels. Furthermore, our study explores the link between retinal aging and reproductive health, integrating genetic data to uncover the interplay between vascular aging and ovarian reserve, while also enhancing reproductive health assessment through the fusion of genetic and imaging data (Fig. 1b). By combining advanced AI techniques with retinal imaging, this research represents a novel, multimodal approach to understanding reproductive aging. Our findings provide valuable insights into the genetic and physiological mechanisms underlying ovarian reserve, paving the way for improved diagnostic tools and targeted interventions in reproductive medicine.
Workflow of the proposed FLEX framework, outlining the development and application of retinal age models in healthy women to explore the relationship between retinal aging and reproductive aging. a The Healthy Cohort Retinal Age Model Weights were trained using transfer learning based on the Healthy Cohort, and these weights were subsequently utilized for fundus feature extraction. b The study involved ophthalmic examinations, questionnaires, and Anti-Müllerian hormone (AMH) testing for the Healthy Female Cohort (middle panel). The cohort was stratified by AMH levels into quartiles, with the middle two quartiles (medium AMH group) being used to train a Female Retinal Age Model using the Healthy Cohort Retinal Age Model Weights (upper left panel). The trained model was then applied to predict retinal age for the highest quartile (high AMH group) and the lowest quartile (low AMH group). The retinal age gap served as a measure of an individual’s reproductive aging level. Further analyses were conducted to explore the relationship between the retinal age gap and AMH levels, as well as between reproductive characteristics and AMH levels (lower left panel). Whole-genome sequencing identified Single Nucleotide Polymorphisms (SNPs), which were analyzed in relation to the predicted retinal age gap (top right panel). Additionally, retinal images were integrated with genetic data to predict AMH levels (bottom right panel).
Results
Cohorts and subjects characteristics
We utilized two cohorts to develop and validate retinal age prediction models and investigate the relationship between retinal age gap and reproductive aging. The Healthy Cohort comprised 20,139 fundus images from 10,013 subjects (55.8% female), with ages ranging from 19.11 to 85.30 years (mean ± SD, 38.00 ± 4.76 years; see Fig. 2a). This cohort was used to construct a generalized retinal age prediction model, capturing the normal aging process across a broad population.
A comprehensive overview of participant demographics and the performance assessment of retinal age prediction in the Healthy Cohort and Healthy Female Cohort. a Distribution of male and female participants across different age groups in the Healthy Cohort, with females represented in red and males in teal. b A scatter plot illustrating the relationship between age and anti-Müllerian hormone (AMH) levels within the Healthy Female Cohort, stratified into three groups based on AMH levels: high (cyan), medium (purple), and low (yellow). c Scatterplots showing the correlation between retinal age and chronological age in the Healthy Cohort, where data points are color-coded based on the retinal age gap, with larger gaps shown in red and smaller gaps in blue. d Bland–Altman plots illustrating the agreement between retinal age and chronological age in the Healthy Cohort, with similar color-coding based on retinal age gap. e Scatterplots displaying the correlation between retinal age and chronological age in the Healthy Female Cohort, with data points color-coded according to the retinal age gap (red for larger gaps and blue for smaller gaps). f Bland–Altman plots depicting the agreement between retinal age and chronological age in the Healthy Female Cohort, with the same color scheme based on retinal age gap.
The Healthy Female Cohort, consisting of 2560 fundus images from 1294 females aged between 25.01 and 47.14 years, was specifically designed to explore the link between retinal aging and reproductive aging. Patients were categorized into 3 groups based on AMH levels: high (n = 320, median = 4.66 ng/mL, IQR: 3.38–6.06), medium (n = 654, median = 1.96 ng/mL, IQR: 1.22–2.88), and low (n = 320, median = 0.58 ng/mL, IQR: 0.20–1.02), with no significant age differences between groups (P = 0.912) (Table 1 and Fig. 2b). The retinal age model was then trained on the medium AMH group to capture typical female aging patterns, avoiding the extremes represented by high or low AMH levels. The low AMH group exhibited significantly lower mean age at first childbirth (26.79 ± 2.87) and first pregnancy (26.36 ± 2.71) compared to the high and medium AMH groups (P = 0.003) (Table 1).
Retinal image-based age prediction using the FLEX model
To achieve precise retinal age prediction, fundus image features from the Healthy Cohort were used by the model to learn optimal weights that minimize the difference between predicted retinal age and true chronological age. The model demonstrated strong predictive performance, with a Pearson’s Correlation Coefficient (PCC) of 0.96, a Mean Absolute Error (MAE) of 2.69 years, a Coefficient of Determination (R²) of 0.91, and an Intraclass Correlation Coefficient (ICC) of 0.96 (Fig. 2c, d).
The final FLEX model was established by fine-tuning the initial weights using the medium AMH group data from the Healthy Female Cohort, allowing it to capture the unique characteristics of female aging (Supplementary Fig. 1). The FLEX model achieved robust predictive performance, with a PCC of 0.83, an MAE of 2.21 years, an R² of 0.68, and an ICC of 0.83, and revealed that the predicted retinal age often deviates from the true chronological age, highlighting individual variations (Fig. 2e, f).
To further validate the robustness and generalizability of the FLEX model, we evaluated its predictive performance in cross-eye and retrospective predictions. In the spatial consistency validation experiment, we paired each image from one eye with the retinal age predicted by our FLEX model from the contralateral eye of the same individual, using retinal images from 1243 women. The model achieved a PCC of 0.90 and an MAE of 1.60 years when predicting the right eye based on the left, and a PCC of 0.88 and an MAE of 1.63 years when predicting the left eye based on the right (Supplementary Fig. 2a and b). Additionally, the model’s ability to forecast retinal age based on fundus images taken two years prior (623 fundus images from 317 women taken in 2019) was confirmed, achieving a PCC of 0.86 and an MAE of 1.83 years (Supplementary Fig. 2c). These results demonstrate FLEX model’s ability to produce consistent retinal age predictions across both temporally and spatially different sources.
The retinal age gap is associated with AMH levels
The FLEX model was used to predict retinal age in women from high and low AMH groups to explore the relationship between retinal age gap and AMH levels. While mean retinal age was similar across groups, the low AMH group showed a significantly higher retinal age gap (mean = 0.71 ± 2.50 years) compared to the high AMH group (mean = 0.36 ± 2.77 years, P = 0.021) (Fig. 3a).
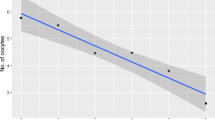
The association between retinal age gap and AMH levels is analyzed through group comparisons and correlation analyses across different age groups. a Comparison of retinal age gap between the high AMH group (red) and the low AMH group (blue) overall and across different age groups. *p-value < 0.05. b–f Correlation between retinal age gap and log AMH levels across different age groups. b 25–29 years old. c 30–34 years old. d 35–39 years old. e 40–44 years old. f 45–50 years old.
Age subgroup analysis revealed significant differences in the 40–50 years range, with the high AMH group showing a significantly smaller retinal age gap compared to the low AMH group of the same age group. A significant negative correlation emerged in women aged 40–50, particularly in the 40–44 years (R = −0.098, P = 0.019) and 45–50 years (R = −0.250, P = 0.002) age brackets (Fig. 3b–f), suggesting an inverse relationship between retinal age gap and AMH levels in women aged 40–50. However, no significant correlation between retinal age gap and AMH levels was found in the 25–39 age group. (P = 0.599 to P = 0.969) (Fig. 3a–d).
Retinal age gap and reproductive events predict AMH levels
Age-specific associations between retinal age gap and AMH levels were observed in women aged 40–44, where each additional year in the retinal age gap was linked to a 12% increase in the odds of low AMH levels (OR = 1.12, 95% CI: 1.02–1.22, P = 0.018) (Fig. 4a). This association was even more pronounced in women aged 45–50, with a 20% higher likelihood of low AMH levels for each additional year in the retinal age gap (OR = 1.20, 95% CI: 1.02–1.44, P = 0.038). No significant associations were found in women aged 25–39 (P > 0.05).
Univariate and multivariate logistic regression analyses evaluating the association between AMH levels, retinal age gap, and reproductive factors. a Univariate logistic regression analysis of AMH Levels based on retinal age gap across different age groups. b Univariate logistic regression analysis of AMH levels based on retinal age gap, childbirth number, pregnancy number, First childbirth age, and First pregnancy age. c Multivariate logistic regression analysis of AMH levels based on retinal age gap, childbirth number, pregnancy number, first childbirth age, and first pregnancy age, adjusted for chronological age, eye laterality, smoking status, drinking status, and marriage status. Error bars represent 95% confidence intervals (CI) for odds ratios (OR). OR Odds ratio, CI Confidence interval. The high AMH group serves as the reference group for logistic regression analysis against the low AMH group, and p-values < 0.05 are considered statistically significant.
Retinal age gap and reproductive events were examined independently. The analysis showed that accelerated retinal aging, as indicated by a more positive retinal age gap, was associated with a 5% increased risk of having low AMH levels (OR = 1.05, 95% CI: 1.01–1.10, P = 0.022; Fig. 4b). This association remained significant after adjusting for potential confounders (Fig. 4c). Additionally, having a greater number of childbirths and being at younger ages during the first pregnancy and childbirth is also positively associated with having lower AMH level than average (Fig. 4b), and these trends were still observed while adjusting for other confounding factors (Fig. 4c). Notably, the number of pregnancies did not show any significant correlation with AMH levels whether alone or considering other variables.
Reproductive factors significantly influence AMH levels, particularly in women aged 30–39. For women aged 35–39, each additional childbirth increases the risk of having a low AMH level by 51% (Supplementary Fig. 3a). Delaying first childbirth and first pregnancy by one year was associated with a 17% and 16% reduction, respectively, in the risk of low AMH levels among women aged 30–34. Among women aged 35–39, the corresponding reductions were 10% and 9%, respectively (Supplementary Fig. 3b, c). The number of pregnancies did not show a significant association with AMH levels among any age groups (P > 0.05) (Supplementary Fig. 3d). Notably, the impact of reproductive factors on AMH level is most significant at the 30–39 range, indicating a critical period where reproductive choices may significantly affect ovarian reserve.
Sexual hormones and time of menopause are associated with retinal age gap
We assessed sex hormone levels in 71 females (140 eyes), focusing on Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), progesterone (P), estradiol (E2), testosterone (T), and prolactin (PRL). For each hormone, we stratified the data into quartiles, with the top and bottom 25% classified as high and low hormone levels, respectively. Higher levels of FSH and PRL were significantly associated with higher retinal age gaps, particularly in women aged 40–50 (Supplementary Fig. 4a and b). However, we did not find significant correlations between retinal age gap and E2, LH, P, and T levels (Supplementary Fig. 4c–f).
Additionally, among 403 postmenopausal women (773 eyes), with a mean menopause age of 49.99 years (SD = 3.00), we found age of menopause to be negatively correlated with retinal age gap (R = −0.17, P < 0.001) (Supplementary Fig. 5a), where women who experienced menopause later had smaller retinal age gaps (P < 0.001) (Supplementary Fig. 5b). Each additional year in the retinal age gap increases the risk of experiencing menopause before age 45 by 36% (P < 0.001) and increases the risk of experiencing menopause between 45 and 49 by 12% (P = 0.004), relative to those experiencing menopause at age 55 or older (Supplementary Fig. 5c). When considering other variables with retinal age gap, we found that each additional year of the retinal age gap increased the risk of experiencing menopause before the age of 45 by 22% (OR = 1.22, P = 0.025) (Supplementary Fig. 5d).
Model explainability
By applying a Visualizer to identify salient features influencing our model’s output, we found vascular regions in the fundus images to be most prominent in age estimation. As predicted age increased, our model’s attention shifted from the nasal vasculature around the optic disc to the temporal vasculature, with a more refined focus concentrated on vascular regions, a pattern most noticeable in the 40–50 age group (Fig. 5).
Genome-wide association study for reproductive aging-related retinal age gap
Knowing that genetic factors contribute to reproductive aging18,19, we speculate whether there are shared genetic factors between retinal and reproductive aging. The genome-wide association study (GWAS) on retinal age gap has provided several important insights into the genetic and biological factors that influence retinal aging. A total of 4000 single-nucleotide polymorphisms (SNPs) were identified as significantly associated with retinal age variation, highlighting the genetic basis of individual differences in retinal aging. Gene Ontology (GO) analysis pinpointed 38 key GOs, mostly of the cellular components (CC) domain, with enriched GO terms such as synaptic membrane, postsynaptic membrane, ion channel complex, cation channel complex, and extrinsic component of the plasma membrane, among others (Adjusted P < 0.05) (Fig. 6). These findings, particularly enrichment of functions in neuronal signaling, suggest a crucial role of neuronal signaling in regulating retinal aging (Fig. 6b).
Overview of the gene analysis workflow and corresponding enrichment analysis results, detailing the key steps and methodologies involved. a Flowchart illustrating the gene analysis process. Starting with 16,987,370 Single Nucleotide Polymorphisms (SNPs), quality control (QC) filtering resulted in 8,089,940 SNPs for subsequent gene feature selection. Gene features selection involved a genome-wide association study (GWAS) for retinal age gap, identifying 7780 SNPs with P < 0.001, followed by LassoNet to select the top 4000 ranked SNPs based on importance. The selected genes then underwent gene annotation, as well as Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses. b Results of the GO enrichment analysis. c Results of the KEGG enrichment analysis. SNPs Single Nucleotide Polymorphisms, QC quality control, GWAS Genome-wide association study, GO Gene Ontology, KEGG Kyoto Encyclopedia of Genes and Genomes.
Among genes of interest in retinal aging, 14 pathways were significantly enriched. Notably, pathways related to reproductive and hormonal functions, such as progesterone-mediated oocyte maturation and oxytocin signaling pathway, were identified, suggesting shared genetic factors among reproductive and retinal aging. Additionally, several cardiovascular pathways were found, including Arrhythmogenic right ventricular cardiomyopathy, Adrenergic signaling in cardiomyocytes, Renin secretion, and Platelet activation. Neuronal signaling pathways such as circadian entrainment, glutamatergic synapse, and dopaminergic synapse were also identified. These results collectively emphasize the intricate relationships between retinal aging, reproductive aging, cardiovascular health, and neuronal signaling, suggesting that genetic factors influencing retinal aging may have broader implications for overall health and aging processes (Fig. 6c).
Enhanced prediction of AMH levels through integration of retinal and genomic data
Given that multimodal approaches can improve predictive accuracy20,21, we leveraged both fundus images and genetic data to predict AMH levels as a proxy for ovarian reserve. We focused on predictions in women aged 40–50 due to this period being a critical transition phase in reproductive health, often leading up to menopause, making it an ideal group to explore the relationship between retinal aging, AMH levels, and reproductive health. Using data from a cohort of 176 women (352 fundus images), we developed two regression models, one based solely on fundus images and the other integrating fundus images with SNP data (fusion model). (For details on fusion model construction, see Supplementary Fig. 6). While both achieved satisfactory performance in predicting AMH level, the fusion model did show a modest improvement (PCC = 0.78, MAE = 0.27 ng/mL, R² = 0.52) (Supplementary Fig. 7). These results highlight the potential of retinal images, especially when combined with genetic data, in providing reliable predictions of AMH levels and offering clinically meaningful fertility guidance for women in this age group.
Discussion
In this study, we investigated the potential of retinal age, as quantified by the retinal age gap, as a non-invasive marker of reproductive aging. By analyzing fundus images of healthy Chinese women, the research demonstrates that the retinal age gap is closely associated with key indicators of reproductive health, including AMH levels and hormonal factors.
We found a significant association between lower AMH levels and an increased retinal age gap, indicating accelerated retinal aging, particularly in women aged 40–50. This age range is crucial for reproductive health, as AMH levels typically begin to decline in the years leading up to menopause22,23,24. With the progress of reproductive aging, AMH levels decline, leading to a reduction in sex hormones like estrogen and progesterone4,5,25, which are known to exert protection over the retina26,27. This decline in protective hormones may accelerate retinal aging, creating the link between reproductive aging and retinal health. Additionally, women with lower AMH levels also showed a higher frequency of earlier reproductive events, such as childbirth. These results suggest that the retinal age gap may serve as a valuable non-invasive marker for reproductive aging, offering insight into the physiological processes that underpin ovarian reserve and fertility.
Further analysis revealed that the retinal age gap is not only linked to AMH but also to other hormonal markers, including FSH and PRL. Elevated FSH and PRL levels, which have been previously described to be linked to ovarian aging28,29,30,31, were also found to accelerate retinal aging, increasing the retinal age gap, particularly in women aged 40–50 years. While we did not observe links between retinal aging and other hormones related to ovarian aging, such as E2 and LH29, we attribute this absence to the influences of the menstrual cycle on these hormones’ levels, which could be an important variable to consider in future research. In contrast, AMH proves to be a more stable marker for assessing reproductive aging, as its levels remain almost consistent throughout the menstrual cycle32.
Notably, the smaller retinal age gap correlated with later menopause, indicative of prolonged reproductive function28, further supporting its potential role as an indicator of reproductive aging. These findings align with previous studies that have shown that retinal aging could be an external reflection of internal, reproductive processes. The connection between retinal age and hormonal factors underscores the broader potential of retinal imaging in assessing age-related physiological changes.
Reproductive timing and the number of childbirths were also associated with AMH levels, with younger reproductive ages and higher childbirth frequency linked to lower AMH. However, prior studies on this relationship have been controversial33,34,35. In younger women, follicle loss occurs through atresia, but the depletion becomes nonlinear around ages 37.5–3836,37,38, making reproductive events more impactful in this age range due to accelerated follicle loss. Additionally, earlier and more frequent childbearing could have a cumulative effect on ovarian reserve, potentially leading to lower AMH levels, though the underlying mechanisms require further clarification.
We also explored the genetic underpinnings of retinal aging, identifying significant associations between retinal age variation and genetic factors involved in reproductive senescence. Genetic pathways related to progesterone-mediated oocyte maturation and oxytocin signaling were enriched in the analysis. Both pathways are critical components of reproductive function39,40, highlighting the potential genetic link between retinal and reproductive aging. Furthermore, pathways associated with cardiovascular health, such as adrenergic signaling and renin secretion, were also implicated. Given that cardiovascular, retinal, and ovarian health are all interconnected through vascular structures, the decline in cardiovascular health can have a systemic impact, impairing blood supply to the retina and ovary and subsequently accelerating their aging41,42,43,44.
Salient mapping further confirmed our speculations, showing that the model focuses on blood vessels around the optic disc, which are areas sensitive to systemic and female aging45,46. Our genetic investigations also identified genes related to reproductive conditions, such as premature ovarian insufficiency (POI) and polycystic ovary syndrome (PCOS), to be associated with retinal age gap. While out of the current study’s scope, these findings may offer insights for future therapeutic interventions aimed at delaying reproductive decline.
The potential clinical applications of this study are significant. The retinal age gap could serve as a useful, non-invasive biomarker for reproductive aging, offering insights into a woman’s ovarian reserve and overall reproductive health without the need for invasive procedures. Such a tool could be valuable for fertility counseling, decision-making regarding reproductive treatments, and monitoring during the menopausal transition. However, several limitations remain and should be addressed in future research. The cross-sectional study design restricts causal inferences, and longitudinal studies are needed to establish temporal relationships. Expanding the sample to include multi-ethnic cohorts and women with diverse reproductive conditions, such as POI or PCOS, would enhance the study’s generalizability. Moreover, future studies should account for confounding factors such as lifestyle choices and menstrual cycle variations. Technical improvements, such as higher-quality retinal imaging, could also refine model accuracy, while balancing dataset age distribution would help minimize bias. These considerations underline the study’s significant impact while highlighting areas for improvement in future investigations.
In summary, we developed a model to predict retinal age gap, as measured through non-invasive fundus imaging, as a proxy for AMH levels and ovarian reserve. The findings highlight the potential of retinal imaging as a tool for assessing reproductive aging, offering a promising direction for early intervention and personalized care in clinical and community settings. Ultimately, the integration of AI, retinal imaging, and genetic data holds great promise for advancing our understanding of reproductive aging and improving women’s health care outcomes.
Methods
Study design and participants
We conducted a cross-sectional study using data from two cohorts within the China Bioage Investigation Consortium20, the Healthy Cohort and the Healthy Female Cohort (Fig. 1). Our study adheres to the tenets of the Declaration of Helsinki, and the protocols were approved by the Clinical Research Ethics Committee of the Eye Hospital, Wenzhou Medical University (No 2023-200-K-162).
The Healthy Cohort, derived from the China Optimal Health Cohort Study (COACS)47, included participants from northern and southern China for retinal age model development (Fig. 1a). The Healthy Female Cohort comprised premenopausal women aged 25–50 years for reproductive health assessments (Fig. 1b). Participants provided written informed consent.
Inclusion criteria for the Healthy Cohort were general good health and absence of serious systemic diseases, nor gynecological diseases, surgical menopause, or hormone therapy. The Healthy Female Cohort excluded participants with gynecological diseases, surgical menopause, hormone therapy, or major systemic conditions like diabetes. More specifically, we excluded individuals with fasting blood glucose levels (FPG) ≥ 7.0 mmol/L, systolic blood pressure (SBP) ≥ 140 mmHg, or diastolic blood pressure (DBP) ≥ 90 mmHg. These thresholds were applied to minimize the confounding effects of systemic vascular conditions on retinal aging. We randomly assigned participants to training (70%), internal validation (20%), and testing (10%) sets.
Ophthalmic assessments
At least two ophthalmologists performed comprehensive eye examinations, including best-corrected visual acuity testing and refractive status assessment using an autorefractometer (KR800; Topcon; Tokyo, Japan) for all participants, excluding patients with ocular disease or vision loss. We then captured and manually reviewed 45° nonmydriatic fundus images (CR2AF; Canon; Tokyo, Japan), excluding low-quality images from analysis. Chronological age was calculated as the difference between birth date and image capture date.
Retinal age gap definition
We developed a deep learning model to predict retinal age from fundus images. The retinal age gap was defined as the difference between chronological age and predicted retinal age, calculated on a per-image basis. A higher gap indicates greater physiological aging.
Reproductive health assessments and AMH stratification
In the Healthy Female Cohort, we measured AMH levels and conducted gynecological evaluations, including uterine ultrasound and cervical cytology. A subset of participants underwent sex hormone tests (FSH, LH, P, E2, T, PRL) and whole-genome sequencing for SNP analysis. We also included a group of healthy postmenopausal women, defined as those reporting cessation of menstruation for over one year, excluding those with menopause onset before age 35 or after age 60.
We stratified participants into age-specific AMH quartiles: the lowest quartile as the low AMH group (high reproductive aging), the middle two quartiles as the medium AMH group, and the highest quartile as the high AMH group (low reproductive aging). This quartile-based stratification strategy aligns with previous studies on reproductive aging, in which AMH levels were commonly divided into quartiles to capture population-level variations in ovarian reserve and facilitate comparisons between groups with distinct reproductive profiles48,49. To capture typical aging patterns and reduce bias from extreme values, the FLEX model was fine-tuned using data from the medium AMH group. We then compared the low and high AMH groups to examine the relationship between retinal age gap and reproductive aging.
Deep learning model for age prediction in healthy cohort
To extract age-related features from retinal images, we developed the Healthy Cohort Retinal Age Model Weights by training a deep learning model on data from the Healthy Cohort. These model weights were then applied to analyze fundus images from the Healthy Female Cohort. The model was built using a Swin Transformer architecture for age regression50, specifically with the Swin-Base configuration, which includes a patch size of 4, a window size of 12, and an input resolution of 384 \(\times\) 384 (swin_base_patch4_window12_384). Pretrained weights from the Japan Ocular Imaging Registry’s JOI model (http://www.joir.jp/data/en_index.html) were used to initialize the network.
Training occurred over 100 epochs, starting with a learning rate of 0.75e−4, which was dynamically adjusted using StepLR. The AdamW optimizer was used with a weight decay of 1.5e−3, and a batch size of 8. To avoid overfitting, early stopping was implemented if the validation loss did not improve after 10 epochs. Stratified sampling was employed to ensure the dataset reflected the overall age distribution, dividing participants into 10-year age intervals.
Modified model FLEX for age prediction in healthy female cohort
We trained the FLEX model on retinal images from the medium AMH level group, indicating nonextreme reproductive aging, to estimate retinal age and analyze its trends in different AMH levels. The FLEX network features a Dual-Channel Transfer Learning architecture, using two parallel Swin Transformer encoders (Supplementary Fig. 1). One encoder’s parameters were kept frozen, while the other was allowed to learn from the new data, preserving the original model’s feature extraction while updating it to suit the Healthy Female Cohort’s images. The outputs of the two encoders were fused and processed through normalization and adaptive pooling to predict retinal age.
To mitigate overfitting, training was limited to 5 epochs, with data augmentation techniques, such as flipping and random rotation. The training process also included age-stratified sampling at 5-year intervals. The final model weights, based on the lowest validation loss, were used to predict retinal age for participants in the low and high AMH groups.
Two validation experiments were conducted to assess the consistency of retinal age predictions: (1) Spatial consistency was evaluated by training the model on paired data, where each retinal image from one eye was matched with the predicted retinal age of the contralateral eye (i.e., using the left eye image paired with the right eye’s predicted age, and vice versa); (2) Temporal consistency was assessed by pairing retinal images acquired in 2019 with the retinal ages predicted by the FLEX model from the corresponding images collected in 2021 for the same individuals. This design allowed us to evaluate the stability of retinal age predictions over time. For both experiments, the datasets were partitioned into training, validation, and test sets (7:2:1), following the same procedure as the main analysis, with no subject-level overlap.
Explainability of model predictions
To enhance the explainability of the retinal age predictions, we utilized the Visualizer tool (https://github.com/luo3300612/Visualizer), which visualizes the attention modules of deep learning models. The tool provided local variable insights from the model without altering its internal code. Specifically, attention feature maps from the Swin Transformer were intercepted at each layer using forward hooks, and visualization was performed on the final attention block of both encoder networks in the FLEX model.
Preprocessing SNP data in the healthy female cohort
Genetic analysis was conducted on 928 female participants from the Healthy Female Cohort who completed whole-genome sequencing. This reduced the sample size from an initial 1294 participants due to exclusions for incomplete genetic data or poor sample quality. PLINK 1.90b6.24 (June 6, 2021)51 was used for SNP quality control, removing variants with missing genotype rates over 2%, minor allele frequencies under 1%, or those that did not pass the Hardy-Weinberg equilibrium test (p-value < 1e−5). After filtering, 8,089,940 variants were retained for further analysis.
Extraction of gene features in the healthy female cohort
Given the large number of SNPs called, traditional false discovery rate and Bonferroni correction methods were considered too conservative, potentially leading to a low true positive rate. Therefore, we used a combination of GWAS and deep learning for better identification of genes related to the retinal age gap.
For extraction of gene features, GWAS was conducted for preliminary SNP screening. Considering that genetic influences affect the body systemically and are shared across both eyes, we performed the association analysis using the average retinal age gap derived from both eyes. Linear regression models were applied using PLINK to analyze the retinal age gap. Our study focused on Han Chinese women from the same geographic region with similar environmental backgrounds, assuming minimal population structure differences among samples, thus not performing principal component analysis (PCA) to adjust for population structure. SNPs with p-values less than 1e−3 were selected for further feature extraction. We employed the LassoNet52,53 model for further screening of these SNPs, which integrates deep learning with Lasso regression (L1 regularization) to facilitate automatic feature selection within a neural network. In this model, let \({{FFN}}_{W}\,:\,{{\mathbb{R}}}^{d}{\mathbb{\longrightarrow }}{\mathbb{R}}\) represent a dense feed-forward neural network parameterized by weights \(W\). For any input \(x\in \,{{\mathbb{R}}}^{d}\) and parameter \(\theta \in \,{{\mathbb{R}}}^{d}\), the LassoNet model can be expressed as Eq. (1):
This formulation can be seen as a residual neural network with an additional skip connection. To optimize the model, we solve the following problem using projected proximal gradient descent, as shown in Eq. (2):
Here, \({{||}\theta {||}}_{1}\) denotes the L1 norm of \(\theta\), enforcing sparsity. The optimization process involves incrementally increasing \(\lambda\) by a factor of \(1+{\rm{\epsilon }}\) until the first-layer weights \({W}^{\left(1\right)}\) reduce to zero. This creates a path of solutions, enabling the selection of an optimal feature set based on the desired sparsity level. The significance of each feature is determined by the point at which its corresponding weight \({W}_{{\rm{j}}}^{\left(1\right)}\) becomes zero as \(\lambda\) increases. Features are chosen by identifying those that are the last to be zeroed out. To enhance model performance, we configured hidden layers with sizes 1200, 800, and 200, increasing the complexity of the neural network. And using default parameters \(M=10\) and \({\rm{\epsilon }}=0.02\). Missing data was filled with the SNPs median, and data standardization was applied to ensure consistent scaling of features. The dataset was divided into 742 samples for training and 186 samples for testing. By default, 10% of the training data is automatically allocated for validation to monitor performance and prevent overfitting. We selected the top 4000 SNPs based on their importance and better model fit (lower and faster-changing MAE) for further analysis.
Gene annotation and enrichment analyses
The selected SNPs underwent gene annotation, which was performed using the online Variant Effect Predictor (VEP). To explore the biological significance of the gene modules, we conducted GO54 and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analyses55 using the clusterProfiler package56 in R. P-values were adjusted using the Benjamini–Hochberg algorithm, with a threshold of P < 0.05 considered statistically significant. The results were visualized using bar plots and dot plots.
AMH concentration prediction using integrated retinal and genetic data
Based on the observed relationship between retinal images and AMH levels in women aged 40–50, we further developed the SNPs-Attention Swin Transformer (SNPs-AST) model to predict AMH concentrations by integrating retinal images and genetic data from this population. This model was compared to a Swin Transformer-based model that used only image data for AMH prediction (Supplementary Fig. 6).
The model for image-based prediction relied on the Swin Transformer architecture, initialized with pre-trained weights from the Healthy Cohort Retinal Age Model weights. These weights had already learned image features related to eye aging, which could potentially enhance the prediction of AMH concentrations. The final layer is configured as a fully connected (FC) layer without additional weights. All model parameters were randomly initialized and standardized to ensure uniform training conditions. Other training parameters remain consistent with previous configurations.
For the gene-image fusion model, we developed an improved version model (SNPs-AST) based on the co-attention technique. The framework consists of three primary components: an image feature embedding encoder, an SNP-specific encoder, and a cross-modal fusion mechanism utilizing a multi-head attention mechanism for integrating images and SNPs.
The image feature embedding encoder employs the Swin Transformer encoder, initialized with the pre-trained weights from the Healthy Cohort Retinal Age Model. For the SNP-specific encoder, we designed a dedicated network consisting of a simple multi-layer perceptron (two FC layers with ReLU activation functions) to embed the input SNPs into the same dimensional space as the image features. The input SNP features include SNP variation (0, 1, 2), chromosome location (1, 2, 3, etc.), and mutation type, with mutation types recoded according to their frequency (e.g., C/T is 1, G/A is 2). These three gene features are combined as the gene information input for the model.
Finally, we custom-designed a multi-head attention mechanism that leverages image features as query vectors and SNP-embedded features as keys and values. This mechanism allows the model to focus on relevant parts of the input sequence (SNP features) when processing the image features. The attention function can be described by the following Eq. (3):
In this context, \(Q\) represents the image feature vectors, \(K\) and \(V\) represent the SNPs embedded feature vectors, with \({d}_{k}\) denoting the dimensionality of the key vectors. The dot product \({{QK}}^{T}\) computes the similarity between image and SNPs features, producing the attention scores, which are then scaled by \(\sqrt{{d}_{k}}\) to mitigate the effects of large dot product values. The softmax function is applied to obtain the attention weights, which are subsequently used to compute a weighted sum of the SNPs feature vectors, yielding the final attention output.
The attention scores calculated from this mechanism dynamically filter SNPs potential features relevant to AMH. We then employ a residual connection mechanism to add the image features to the SNP potential features, followed by a FC layer acting as a regressor to predict AMH concentrations.
Statistical analysis
Descriptive statistical analysis was conducted using χ2 tests or Fisher’s exact tests for categorical variables, and Student’s t tests or Mann–Whitney U-tests for continuous variables, depending on data distribution. Age then was segmented into 5-year intervals, with t-tests performed to compare retinal age gap differences across AMH groups within each interval. Additionally, Pearson’s correlation was used to assess the relationship between log-transformed AMH (to account for its non-normal distribution) and the retinal age gap. Univariate and multivariate logistic regression analyses were conducted using a generalized linear model (GLM) to examine the influence of the retinal age gap and other fertility-related factors on outcomes within different AMH categories. The high AMH group was used as a reference to evaluate the odds ratios (OR), 95% confidence intervals, and p-values for the low AMH group. In all multivariate logistic regression analyses, the covariates adjusted in the model included age, eye laterality, BMI, smoking status, alcohol consumption, and marital status. To maximize statistical power, both eyes were included in the analysis. Given the potential for inter-eye differences, eye laterality was explicitly adjusted for in the regression models to account for intra-individual correlation. The inclusion of BMI, smoking, alcohol consumption, and marital status was justified, as these clinical factors may influence either AMH levels or retinal health57, making them relevant to the study hypothesis. Additionally, the parameters were also analyzed through the univariate GLM segmented by different age groups, without adjustments due to the small amount of data for each age group.
We also assessed participants from the Healthy Female Cohort who underwent additional sex hormone testing. These participants were divided into quartiles for each hormone based on 10-year age intervals. T-tests were then used to compare the retinal age gap between the highest and lowest quartile groups, offering further insights into the relationship between the retinal age gap and reproductive aging.
Furthermore, we analyzed the menopausal timing of postmenopausal participants. Initially, we examined the association between menopausal timing and the retinal age gap. We then divided the menopausal age into groups above and below the average and compared the retinal age gap of each group using t-tests. Additionally, the menopausal age was categorized into intervals of <45, 45–49, 50–54, and ≥55 years. Using the ≥55 years group as a reference, we examined the association between the retinal age gap and menopausal timing using univariate and multivariate logistic regression analyses. Since all individuals in the study have been married, age, eye laterality, BMI, smoking status, and alcohol consumption were adjusted for as covariates.
Model performance was assessed using PCC, MAE, R², Bland–Altman plots, and ICC to evaluate agreement between predicted and actual values. All analyses were performed using R Studio (version 4.1.2), with model training and validation in Python (version 3.7.15). A p-value < 0.05 was considered statistically significant.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Code availability
The underlying code for this study and training/validation datasets is not publicly available but may be made available to qualified researchers on reasonable request from the corresponding author.
References
Li, J. et al. Determining a multimodal aging clock in a cohort of Chinese women. Medicine 4, 825–848 e813 (2023).
Sermondade, N. et al. Serum antimullerian hormone is associated with the number of oocytes matured in vitro and with primordial follicle density in candidates for fertility preservation. Fertil. Steril. 111, 357–362 (2019).
de Kat, A. C., Broekmans, F. J. M. & Lambalk, C. B. Role of AMH in prediction of menopause. Front. Endocrinol. 12, 733731 (2021).
Dewailly, D. & Laven, J. AMH as the primary marker for fertility. Eur. J. Endocrinol. 181, D45–D51 (2019).
Moolhuijsen, L. M. E. & Visser, J. A. Anti-Mullerian hormone and ovarian reserve: update on assessing ovarian function. J. Clin. Endocrinol. Metab. 105, 3361–3373 (2020).
Fallahzadeh, A., Ramezeni Tehrani, F., Rezaee, M., Mahboobifard, F. & Amiri, M. Anti-Mullerian hormone and cardiometabolic status: a systematic review. Biomarkers 28, 486–501 (2023).
de Kat, A. C., Verschuren, W. M., Eijkemans, M. J., Broekmans, F. J. & van der Schouw, Y. T. Anti-Mullerian hormone trajectories are associated with cardiovascular disease in women: results from the Doetinchem cohort study. Circulation 135, 556–565 (2017).
Dumanski, S. M. et al. Anti-Mullerian hormone and vascular dysfunction in women with chronic kidney disease. Physiol. Rep. 10, e15154 (2022).
London, A., Benhar, I. & Schwartz, M. The retina as a window to the brain-from eye research to CNS disorders. Nat. Rev. Neurol. 9, 44–53 (2013).
Miao, H., Zou, Z., Xu, J. & Gao, Y. Advancing systemic disease diagnosis through ophthalmic image-based artificial intelligence. MedComm Future Med. 3, e75 (2024).
Marchesi, N., Fahmideh, F., Boschi, F., Pascale, A. & Barbieri, A. Ocular neurodegenerative diseases: interconnection between retina and cortical areas. Cells 10, https://doi.org/10.3390/cells10092394 (2021).
Zhu, Z. et al. Retinal age gap as a predictive biomarker of stroke risk. BMC Med. 20, 466 (2022).
Zhu, Z. et al. Retinal age gap as a predictive biomarker for mortality risk. Br. J. Ophthalmol. 107, 547–554 (2023).
Zhang, S. et al. Association of retinal age gap and risk of kidney failure: a UK Biobank study. Am. J. Kidney Dis. 81, 537–544 e531 (2023).
Hu, W. et al. Retinal age gap as a predictive biomarker of future risk of Parkinson’s disease. Age Ageing 51, https://doi.org/10.1093/ageing/afac062 (2022).
Chen, R. et al. Central obesity and its association with retinal age gap: insights from the UK Biobank study. Int. J. Obes. 47, 979–985 (2023).
Ahadi, S. et al. Longitudinal fundus imaging and its genome-wide association analysis provide evidence for a human retinal aging clock. Elife 12, https://doi.org/10.7554/eLife.82364 (2023).
Miller, E. C. et al. Pregnancy, preeclampsia and maternal aging: From epidemiology to functional genomics. Ageing Res. Rev. 73, 101535 (2022).
Dong, L., Teh, D. B. L., Kennedy, B. K. & Huang, Z. Unraveling female reproductive senescence to enhance healthy longevity. Cell Res. 33, 11–29 (2023).
Wang, J. et al. Accurate estimation of biological age and its application in disease prediction using a multimodal image Transformer system. Proc. Natl Acad. Sci. USA 121, e2308812120 (2024).
Acosta, J. N., Falcone, G. J., Rajpurkar, P. & Topol, E. J. Multimodal biomedical AI. Nat. Med. 28, 1773–1784 (2022).
Levine, M. E. et al. Menopause accelerates biological aging. Proc. Natl Acad. Sci. USA 113, 9327–9332 (2016).
Henderson, V. W. Action of estrogens in the aging brain: dementia and cognitive aging. Biochim. Biophys. Acta 1800, 1077–1083 (2010).
Uddenberg, E. R. et al. Menopause transition and cardiovascular disease risk. Maturitas 185, 107974 (2024).
de Vet, A., Laven, J. S., de Jong, F. H., Themmen, A. P. & Fauser, B. C. Antimullerian hormone serum levels: a putative marker for ovarian aging. Fertil. Steril. 77, 357–362 (2002).
Nuzzi, R., Scalabrin, S., Becco, A. & Panzica, G. Gonadal Hormones and Retinal Disorders: A Review. Front Endocrinol. 9, 66 (2018).
Nuzzi, R. & Caselgrandi, P. Sex hormones and their effects on ocular disorders and pathophysiology: current aspects and our experience. Int. J. Mol. Sci. 23, https://doi.org/10.3390/ijms23063269 (2022).
Broekmans, F. J., Soules, M. R. & Fauser, B. C. Ovarian aging: mechanisms and clinical consequences. Endocr. Rev. 30, 465–493 (2009).
Bosch, E. et al. Reduced FSH and LH action: implications for medically assisted reproduction. Hum. Reprod. 36, 1469–1480 (2021).
Bernard, V., Young, J. & Binart, N. Prolactin - a pleiotropic factor in health and disease. Nat. Rev. Endocrinol. 15, 356–365 (2019).
Auriemma, R. S. et al. The Interplay Between Prolactin and Reproductive System: Focus on Uterine Pathophysiology. Front. Endocrinol. 11, 594370 (2020).
Dewailly, D. et al. The physiology and clinical utility of anti-Mullerian hormone in women. Hum. Reprod. Update 20, 370–385 (2014).
Dolleman, M. et al. Reproductive and lifestyle determinants of anti-Mullerian hormone in a large population-based study. J. Clin. Endocrinol. Metab. 98, 2106–2115 (2013).
Bragg, J. M., Kuzawa, C. W., Agustin, S. S., Banerjee, M. N. & McDade, T. W. Age at menarche and parity are independently associated with Anti-Mullerian hormone, a marker of ovarian reserve, in Filipino young adult women. Am. J. Hum. Biol. 24, 739–745 (2012).
Grimes, N. P. et al. The association of parity and breastfeeding with anti-Mullerian hormone levels at two time points. Maturitas 155, 1–7 (2022).
Gougeon, A., Ecochard, R. & Thalabard, J. C. Age-related changes of the population of human ovarian follicles: increase in the disappearance rate of non-growing and early-growing follicles in aging women. Biol. Reprod. 50, 653–663 (1994).
Faddy, M. J. & Gosden, R. G. A model conforming the decline in follicle numbers to the age of menopause in women. Hum. Reprod. 11, 1484–1486 (1996).
Faddy, M. J. Follicle dynamics during ovarian ageing. Mol. Cell Endocrinol. 163, 43–48 (2000).
Salehnia, M. & Zavareh, S. The effects of progesterone on oocyte maturation and embryo development. Int. J. Fertil. Steril. 7, 74–81 (2013).
Gimpl, G. & Fahrenholz, F. The oxytocin receptor system: structure, function, and regulation. Physiol. Rev. 81, 629–683 (2001).
Hanssen, H., Streese, L. & Vilser, W. Retinal vessel diameters and function in cardiovascular risk and disease. Prog. Retin. Eye Res. 91, 101095 (2022).
Quinn, M. M. & Cedars, M. I. Cardiovascular health and ovarian aging. Fertil. Steril. 110, 790–793 (2018).
Brown, H. M. & Russell, D. L. Blood and lymphatic vasculature in the ovary: development, function and disease. Hum. Reprod. Update 20, 29–39 (2014).
Mu, L. et al. Physiological premature aging of ovarian blood vessels leads to decline in fertility in middle-aged mice. Nat. Commun. 16, 72 (2025).
Vajaranant, T. S., Nayak, S., Wilensky, J. T. & Joslin, C. E. Gender and glaucoma: what we know and what we need to know. Curr. Opin. Ophthalmol. 21, 91–99 (2010).
Dastiridou, A. et al. Age and signal strength-related changes in vessel density in the choroid and the retina: an OCT angiography study of the macula and optic disc. Acta Ophthalmol. 100, e1095–e1102 (2022).
Wang, Y. et al. China suboptimal health cohort study: rationale, design and baseline characteristics. J. Transl. Med. 14, 291 (2016).
Freeman, E. W., Sammel, M. D., Lin, H. & Gracia, C. R. Anti-mullerian hormone as a predictor of time to menopause in late reproductive age women. J. Clin. Endocrinol. Metab. 97, 1673–1680 (2012).
Liu, S. et al. Association of antimüllerian hormone with polycystic ovarian syndrome phenotypes and pregnancy outcomes of in vitro fertilization cycles with fresh embryo transfer. BMC Pregnancy Childbirth 22, 171 (2022).
Liu, Z. et al. Swin transformer: hierarchical vision transformer using shifted windows. In: IEEE/CVF International Conference on Computer Vision (ICCV), 9992–10002, https://doi.org/10.1109/iccv48922.2021.00986 (2021).
Purcell, S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet 81, 559–575 (2007).
Lemhadri, I., Ruan, F. & Tibshirani, R. LassoNet: neural networks with feature sparsity. Proc. Mach. Learn Res. 130, 10–18 (2021).
Sajwani, H. & Feng, S. Identifying SNP associations and predicting disease risk from Genome-wide association studies using LassoNet, https://doi.org/10.1101/2021.08.29.458051 (2021).
Ashburner, M. et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat. Genet. 25, 25–29 (2000).
Kanehisa, M. & Goto, S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30 (2000).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Oldfield, A. L., Kazemi, M. & Lujan, M. E. Impact of obesity on anti-Mullerian hormone (AMH) levels in women of reproductive age. J. Clin. Med. 10, https://doi.org/10.3390/jcm10143192 (2021).
Acknowledgements
This research was supported by National Natural Science Foundation of China (W2431057); Wenzhou Eye Hospital, State Key Laboratory of Eye Health, Institute for Advanced Study on Eye Health and Diseases, Wenzhou Medical University; Southern Medical University; the Macau Science and Technology Development Fund, Macao (0003/2021/AKP); Macao Young Scholars Program (AM2023018); Guangzhou National Laboratory (YW-SLJC0201); Jiangsu Provincial Health Commission Medical Research (Guiding) Project (Z2022063); Nanjing Medical University Changzhou Medical Center (Basic Research) Project (CMCB202333). We thank Prof Yong Zhou, physicians and patients for providing clinical data.
Author information
Authors and Affiliations
Contributions
K.Z. conceptualized the work. K.Z., Y.G., Z.S., H.M., Z.W., S.L., Y.K., L.C., W.Y. and D.Y. designed the study, collected data and performed analyses. K.Z., H.M., S.L., Z.W., Y.G. and Z.S. wrote the first draft and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Miao, H., Liu, S., Wang, Z. et al. Artificial intelligence-derived retinal age gap as a marker for reproductive aging in women. npj Digit. Med. 8, 367 (2025). https://doi.org/10.1038/s41746-025-01699-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41746-025-01699-8