Abstract
Drug-resistant bacteria, bacterial biofilms and toxins impede skin wound healing. Traditional medical dressings, such as gauzes, serve merely as physical barriers and are insufficient to prevent bacterial adhesion and invasion. Herein, we present a composite nonwoven fabric dressing (PVA@HD5-myr) by covalently conjugating multi-bioactive human α defensin 5 derivative (HD5-myr) to polyvinyl alcohol (PVA). PVA@HD5-myr fibers are produced in one step by incorporating Tyzor®LA, a titanate coupling agent, into the spinning dope during the spinning process. The resulting PVA@HD5-myr demonstrates satisfactory antibacterial activity against multiple drug-resistant bacteria through adhesion and cell membrane disruption. Additionally, PVA@HD5-myr effectively inhibits biofilm formation on its surface, blocks bacterial invasion, and significantly promotes wound healing in vivo. This dressing also disrupts endotoxin release in skin wound environments, with favorable safety profiles both in vitro and in vivo assessments. Our findings suggest that PVA@HD5-myr is a promising candidate for next-generation clinical dressings, offering effective antimicrobial properties alongside wound protection.
Similar content being viewed by others
Introduction
As the largest organ by surface area in the human body, the skin plays a pivotal role in maintaining homeostasis and shielding internal organs from microbial invasion, physical harm and mechanical damage1. Acute and chronic wounds pose significant challenges to individual health and the healthcare economy2,3. The wound healing process undergoes three distinct but overlapping phases, including inflammation, cell proliferation, and remodeling. Infections occur easily in invasive wounds that disrupt the early tissue pro-regenerative microenvironment, thereby delaying the healing process and potentially leading to systemic infection and multiple organ dysfunction, namely sepsis4,5,6. In particular, multidrug-resistant bacterial infections complicate the management of skin wounds7. Moreover, pathogens such as methicillin-resistant S. aureus (MRSA) and multidrug-resistant P. aeruginosa in chronic wounds are challenging to treat due to their propensity to form biofilms, the structured communities encased in a self-produced polymeric matrix, which enhances bacteria adhesion, immune evasion, and antibiotic resistance8,9. Besides their direct damage to the host, bacteria in wound beds can exacerbate the local microenvironment by releasing toxins, such as endotoxin (also known as lipopolysaccharide (LPS)), the principal component of the Gram-negative bacteria outer membrane2,6. Endotoxin from the wound area can be absorbed into the blood and induce systemic inflammatory responses and immunosuppression10,11. Hence, bacteria, biofilms and toxins are the most important external factors affecting wound healing.
Besides aseptic technology and systemic antibiotic therapy, the application of antibacterial dressings to create a barrier for the skin is an important step in preventing bacterial invasion12,13. Recent efforts have been directed toward the development of advanced functionalized medical dressings by incorporating various antibacterial ingredients, including antibiotics14, metal ions (e.g., Zn2+, Ag+, and Cu2+)15,16,17, cationic molecules (e.g., quaternary ammonium salt)18, antimicrobial peptides (AMPs)19 and other biologically active molecules originating from human body or nature20. Among them, antibiotics are not the ideal choice due to their propensity to increase bacterial resistance, while some metal ions have certain toxicity in vivo21. It is well documented that AMPs usually do not easily induce bacterial resistance, making them more suitable for application in skin wounds22.
Previously, we successfully converted human α-defensin 5 (HD5), an endogenous AMP secreted by Paneth cells located in the small intestine, into efficacious antibiotics (termed HD5-myr) via a C-terminal myristoylation design strategy23. Compared with HD5, HD5-myr exhibited more potent broad-spectrum bactericidal activity in vitro and in vivo23. This study also validated this design strategy using human β-defensin 1 (hBD-1), a cationic, amphiphilic peptide containing 36 amino acids with a β-sheet structure24. As shown in Supplementary Table 1 and Supplementary Fig. 1, we designed N- or C- terminally myristoylated hBD-1 (termed myr-hBD-1 and hBD-1-myr). A virtual colony-count assay revealed that hBD-1-myr exhibited stronger bactericidal activity against E. coli, A. baumannii and P. aeruginosa than hBD-1 and myr-hBD-1 (Supplementary Fig. 2). Our previous study had proved that HD5-myr most likely killed bacteria by disrupting bacterial membranes and cell wall23,25. This distinct mechanism from traditional antibiotics is expected to be useful in treating resistant bacteria. Because bacterial resistance development is a major concern in skin wound infection, we assessed the ability of Gram-negative (G-) and Gram-positive (G+) bacteria to develop resistance to HD5-myr. Serial passage (more than 20 passages) of A. baumannii or S. aureus in the presence of sub-minimum inhibitory concentration (MIC) levels of HD5-myr failed to produce resistant mutants. In contrast, exposure to the antibiotic imipenem/cilastatin sodium or vancomycin, respectively, resulted in a rapid increase in MIC after a few passages (Supplementary Fig. 3). Furthermore, our findings indicate that HD5-myr exhibits anti-biofilm and endotoxin-neutralizing properties, making it an optimal candidate for wound infection management.
Polyvinyl alcohol (PVA) is a biodegradable synthetic polymer widely used in the field of biotechnology26,27. PVA-based micro/nanofiber dressing, featured with mimicry of extracellular matrix, flexibility in material selection, and diversity in assembly structure, holds huge potential for replacement of their classic counterparts12,28. However, PVA itself is unable to inhibit or kill bacteria. Recently, proteins/peptides-enriched bioactive surfaces have emerged as a versatile and promising strategy for enhancing the biocompatibility and performance of various biomedical materials29. Hence, based on the favorable biological characteristics of HD5-myr, we hypothesized that adding HD5-myr to PVA to construct a bioactive fiber dressing will have significant clinical translational potential. Currently, the most frequently employed methods for material surface modification can be classified as either physical or chemical30. Compared with physical methods, chemically prepared grafted layers can bind more firmly to the surface because chemical bonds are much stronger than intermolecular interactions.
Coupling agents are commonly used materials for chemical modification and possess numerous types, among which silane coupling agents (SCAs) and titanate coupling agents (TCAs) are more widely used in dentistry, dressings and other medical fields owing to their excellent performance and relatively high cost-effectiveness31,32. Existing research has indicated that TCAs are superior to SCAs in terms of the surface modification effect. This is mainly due to the titanium atoms’ high reactivity and chemical bond strength in the titanate part of the TCAs. By contrast, the chemical bonds in SCAs are relatively weaker. Moreover, silane tends to hydrolytically degrade in the aqueous environment at high temperatures or alkaline pH33. Hence, we choose chemical methods to get a firmer crosslink between HD5-myr and PVA, specifically by adding TCAs in this study. TCAs are organometallic interfacial chemicals containing titanium (molecular formula: (RO)m-Ti-(OX-R’-Y)n) that can provide good chemical bonding and homogenous dispersion32,34. More importantly, TCAs can form a single molecular layer on the filler surface without forming a multi-molecular layer. Here, we choose Tyzor®LA, a type of TCA, to bind HD5-myr to PVA by reacting with the hydroxyl groups of HD5-myr and PVA. Tyzor®LA, a lactic acid titanium chelate ammonium salt, is very stable and less susceptible to hydrolysis in aqueous solutions, and its structure is shown in Supplementary Fig. 435.
To simplify industrial processes, we developed a one-step route to synthesize composite polyvinyl alcohol nonwoven fabric dressing (PVA@HD5-myr). In the production process, we have not only ensured the stable conjugation of HD5-myr with PVA but also maintained the bioactivity of the HD5-myr by controlling temperature and other conditions. After the synthesis of PVA@HD5-myr, the elemental composition and chemical bonds of PVA@HD5-myr surface were characterized. We verified the satisfactory antibacterial and anti-biofilm effect of PVA@HD5-myr in vitro. We also found that PVA@HD5-myr could effectively prevent bacterial invasion and endotoxin release in skin wounds in vivo. PVA@HD5-myr exhibited favorable safety profiles in vitro and in vivo. Overall, the present study provides a biomaterial, PVA@HD5-myr, featuring bactericidal, anti-biofilm and endotoxin adsorption roles that represent a promising candidate for translation into clinical dressings for wound protection.
Results and Discussion
Preparation and characterization of PVA@HD5-myr nonwoven fabrics
HD5-myr and its parent HD5 were successfully synthesized via solid-phase peptide synthesis. The amino acid sequence is shown in Supplementary Fig. 4. All peptides were purified to >95% purity by high-performance liquid chromatography (HPLC) and verified by matrix-assisted laser desorption/ionization time of flight (MALDI-TOF) mass spectrometry (MS) (Supplementary Fig. 5). Circular dichroism (CD) analysis was performed to estimate the secondary structure of peptides. The CD spectra of both peptides are consistent with previous reports23,36, confirming their correct folding into β-sheets and the formation of disulfide bonds (Supplementary Fig. 6).
To enhance the clinical applicability of HD5-myr in wound healing, we synthesized PVA@HD5-myr via a one-step route designed for industrial production (Fig. 1). In the production process of PVA@HD5-myr, factors such as temperature and 60Co irradiation may damage the structure of the HD5-myr and affect its biological activity. Therefore, HD5-myr was first exposed to 50 °C for 72 h or to 60Co irradiation (15 kGy) and then analyzed for changes in its structure and bactericidal activity. As shown in Supplementary Fig. 7, after treatment at 50 °C for 72 h or to 60Co irradiation (15 kGy), the bactericidal activity of HD5-myr against MRSA was not affected (Supplementary Fig. 7a, c). MALDI-TOF MS and CD spectra confirmed the constant molecular weight (Supplementary Fig. 7b, d) and secondary structure (Supplementary Fig. 7e–g) of HD5-myr. These results confirm the feasibility of the synthetic route.
Macroscopic morphology and high-magnification scanning electron microscopy (SEM) showed no significant difference in the microstructures between PVA@HD5-myr and PVA nonwoven fabrics with basis weight of 68 g m-2 produced by the same process (Fig. 2a). Atomic force microscopy (AFM) showed that the surface of PVA@HD5-myr nonwoven fabrics is rougher than that of PVA (Supplementary Fig. 8). Further, the elemental composition of PVA and PVA@HD5-myr surface were analyzed via SEM-energy dispersive X-ray spectroscopy (EDS) and X-ray photoelectron spectroscopy (XPS). To remove the HD5-myr that was not covalently bound on the surface, PVA@HD5-myr was washed thoroughly with distilled water. As shown in Fig. 2b, the surface of PVA@HD5-myr exhibited evenly distributed C, O and N elements, while the surface of PVA only exhibited C and O elements but no N element. The N element was uniformly distributed on the surface of PVA@HD5-myr. Since the N element originates solely from HD5-myr, this indicates that HD5-myr is uniformly distributed on the surface of PVA@HD5-myr. Subsequently, HD5-myr, PVA and PVA@HD5-myr were characterized by XPS spectra to confirm their elemental compositions and chemical state. The elements composition of PVA, HD5-myr and PVA@HD5-myr were shown (Fig. 2c–e and Supplementary Table 2). In Fig. 2f, the N 1 s spectrum of HD5-myr (at 399.38 eV) and PVA@HD5-myr (at 399.18 eV) showed only one signal and their maximum centers aligned, which corresponded to amide bond (–CONH–) according to the previous studies37,38. The XPS spectra of S 2p of HD5-myr (at 163.08 eV) correspond to sulfur atoms participating in disulfide chemical bonds (-S-S-) (Fig. 2g)39,40,41. By contrast, the S 2p spectra of PVA@HD5-myr exhibited two peaks, at 162.98 eV and 167.88 eV, corresponding to the -S-S- and sulfate radical (SO₄²-), respectively42,43. This could be attributed to the impurity of sodium sulfate in the calcium carbide raw material used to produce PVA. The Ti core-level XPS spectrum of PVA@HD5-myr showed two peaks centered at 463.98 and 458.38 eV (Fig. 2h), which were assigned, respectively, to the Ti 2p1/2 and Ti 2p3/2 spin-orbital splitting photoelectrons in the Ti4+ state44,45. In agreement with previous reports, this peak was assigned to the binding energy of Ti in Ti−O bond46. Furthermore, to verify whether HD5-myr is easy to detach from PVA@HD5-myr, PVA@HD5-myr (2 g) was soaked in 30 mL of ultrapure water at 50 °C for 24 or 48 h. After leaching, the components of the extract were analyzed by MS. The results showed that HD5-myr was not found in the extract at 24 h (Fig. 2i, j). The extract contained a substance with a molecular weight of 3972.094 at 48 h, which was speculated to be the major part of HD5-myr (MW: 3976.7) with some atoms retained on the PVA matrix during soaking. These findings confirm the stable chemical bonding of HD5-myr to the PVA matrix, ensuring sustained functionality. To further detect the HD5-myr content on PVA@HD5-myr, PVA@HD5-myr (200 cm2) was soaked in 50 mL of ultrapure water at 50 °C. At 48, 72, 96 and 120 h, respectively, 500 µL of the above liquid was collected and detected by liquid chromatography-mass spectrometry (LC-MS). As shown in Supplementary Fig. 9, the concentration of HD5-myr in the extract increased with time and reached 371.71 ng mL-1 at 120 h, which is close to its theoretical value of 382 ng mL-1. This corresponds to an HD5-myr content of 93 ng cm-2, which is close to its theoretical value of 95.5 ng cm-2, indicating that almost all HD5-myr on PVA@HD5-myr is shed after soaking for 120 h at 50 C. Taken together, HD5-myr was uniformly and firmly distributed on the surface of PVA material by the Ti−O bond.
a Photographs and SEM images of surface morphologies of PVA and PVA@HD5-myr dressings. Scales bars, 100 μm. b EDS elemental mapping images of the following elements: C, O of PVA and C, O, N of PVA@HD5-myr. Scales bars, 100 μm. c-e XPS spectra of (c) PVA, (d) HD5-myr and (e) PVA@HD5-myr. f N 1 s core-level spectra for amide groups of HD5-myr and PVA@HD5-myr. g S 2p core-level spectra of HD5-myr and PVA@HD5-myr. h Ti 2p core-level spectra of PVA@HD5-myr. i, j The composition of the PVA@HD5-myr extract was analyzed by MALDI-TOF MS. PVA@HD5-myr (2 g) was placed in 30 mL of ultrapure water and treated at 50 °C for (i) 24 h or (j) 48 h. Then, the extract was analyzed by MALDI-TOF MS.
Antibacterial effect and mechanism of PVA@HD5-myr and its stability
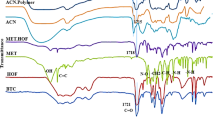
To evaluate the antibacterial property of PVA@HD5-myr, three pieces of PVA@HD5-myr nonwoven fabrics (6 × 6 cm) were incubated with bacteria (1 × 106 CFU mL-1; in 50 mL phosphate buffer saline, PBS) for 1 h at 37 °C, 200 rpm in an incubator, using PVA sample as control (Supplementary Fig. 10). To investigate whether any HD5-myr on the PVA@HD5-myr shed into the solution, MALDI-TOF MS was employed to analyze the extract composition. No detectable HD5-myr was observed (Supplementary Fig. 11). Our previous study demonstrated that HD5-myr possesses excellent bactericidal effects on both G- and G+ bacteria23. However, it is unknown whether HD5-myr retains its strong bactericidal activity when immobilized onto PVA. Here, several common and drug-resistant bacteria that infect skin wounds were selected to test the antibacterial effect of PVA@HD5-myr, including E. coli, K. pneumoniae, vancomycin-resistant S. aureus, A. baumannii, P. aeruginosa, MRSA, imipenem/cilastatin sodium-resistant A. baumannii and carbapenems-resistant P. aeruginosa (The results of 16S rRNA sequencing and antimicrobial susceptibility test of drug-resistance bacteria were shown in Supplementary Table 3, 4 and Supplementary Fig. 12). We found that PVA@HD5-myr demonstrated potent and broad-spectrum antibacterial effects, even for drug-resistant bacteria (Fig. 3a–h and Supplementary Fig. 13). Furthermore, to verify the fabrics’ stability in a moist and warm environment, PVA@HD5-myr nonwoven fabrics were incubated at 60% relative humidity (RH) and 37 °C for 33 days, after which their bactericidal activity was analyzed. As shown in Supplementary Fig. 14, PVA@HD5-myr still showed strong antibacterial ability, although the antibacterial effect on certain bacteria was slightly diminished.
a–h Viable count assay detected the live E. coli, K. pneumoniae, vancomycin-resistant S. aureus, A. baumannii, P. aeruginosa, MRSA, imipenem/cilastatin sodium-resistant A. baumannii and carbapenems-resistant P. aeruginosa before and after treatment with PVA or PVA@HD5-myr. Bacteria (1 × 106 CFU mL-1) were incubated with three pieces of PVA or PVA@HD5-myr (6 × 6 cm) at 200 rpm, 37 °C for 1 h, then the number of viable bacteria (on a logarithmic scale) was counted. The lower limit of detection was 100 CFU. Data are shown as mean ± SD and statistical significance was calculated by one-way ANOVA analysis of variance with Bonferroni corrections for multiple comparisons (n = 3). *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant. i–k SEM images of (i) imipenem/cilastatin sodium-resistant A. baumannii, (j) carbapenems-resistant P. aeruginosa and (k) MRSA 1 h after treatment with PVA or PVA@HD5-myr (n = 3). Scales bars in left (10,000 ×) and right (30,000 ×) pictures are 1 and 0.5 μm in length, respectively.
The proposed antimicrobial mechanisms of AMPs include membrane translocation of the peptides, followed by binding to intracellular targets, affects the life activity of bacteria, or membrane perturbation that directly interacts with the negatively charged components on the bacterial membrane47,48. Our previous study preliminarily confirmed through SEM that HD5-myr can disrupt the bacterial membrane and cell wall structure23. In this study, fluorescent probe N-phenyl-1-naphthylamine (NPN) assay indicated that treatment of HD5-myr increased the permeability of the outer membrane of G- bacteria such as E. coli and P. aeruginosa in a dose-dependent manner (Supplementary Fig. 15a, d). For G+ bacteria, we measured bacterial membrane permeabilization by assaying for bacterial uptake of propidium iodide (PI), a membrane-impermeant dye. The results confirmed that HD5-myr promoted the dose-dependent uptake of PI by MRSA and S. aureus (Supplementary Fig. 15b, e). Surface plasmon resonance (SPR) assays demonstrated that HD5-myr could effectively bind to outer membrane protein A (OmpA, Ka = 1.76 × 102 Ms-1, Kd = 2.20 × 10-5 s-1, KD = 1.25 × 10-7 M) of G- bacteria as well as lipoteichoic acid (Ka = 6.38 Ms-1, Kd = 1.15 × 10-5 s-1, KD = 1.8 × 10-6 M) of G+ bacteria with a high affinity (Supplementary Fig. 15c, f). These data revealed that HD5-myr killed G- and G+ bacteria by disrupting their membranes through high-affinity binding with surface components. To gain visual insight into how PVA@HD5-myr kills bacteria, imipenem/cilastatin sodium-resistant A. baumannii, carbapenems-resistant P. aeruginosa and MRSA were incubated with PVA or PVA@HD5-myr nonwoven fabrics at room temperature for 1 h before being observed by SEM. The images showed evidence of bacterial cell wall damage and cytoplasmic leakage (Fig. 3i–k), suggesting that similar to HD5-myr, PVA@HD5-myr also killed bacteria by permeabilizing their membranes. In addition, the live/dead staining results also reflected the increased permeability of the bacterial membrane after treatment with PVA@HD5-myr. As shown in Fig. 4, no red fluorescence was detected in the PVA group, implying that the membrane with full integrity blocked the entering of PI. In contrast, red fluorescence was observed inside bacterial cells in the PVA@HD5-myr group, indicating severe damage to the bacterial membrane. Together, the above results proved that PVA@HD5-myr has excellent antibacterial activity against both G- and G+ antimicrobial resistant bacteria through contact-killing rather than release-killing effect.
a–c Confocal fluorescence images of (a) carbapenems-resistant P. aeruginosa, (b) imipenem/cilastatin sodium-resistant A. baumannii and (c) MRSA 1 h after treatment with PVA or PVA@HD5-myr (n = 6). Live (SYTO 9, green) and dead (PI, red) bacterial staining are shown. PI, propidium iodide; Scale bars, 20 μm.
Anti-biofilm effect of PVA@HD5-myr
Biofilm formation is a common occurrence in wounds and significantly impedes healing. In addition, biofilms readily attach to medical dressings and become a persistent source of chronic skin infections. AMPs possess significant advantages in inhibiting the formation of bacterial biofilms22,49. However, it remains unclear whether HD5-myr inhibits bacterial biofilm formation. We compared the ability of common A. baumannii, P. aeruginosa and S. aureus to form biofilms with their drug-resistant counterparts. As shown in Supplementary Fig. 16, drug-resistant bacteria are more inclined to form biofilms than non-resistant bacteria, which may be related to mutations in biofilm formation-related genes50. Therefore, we selected imipenem/cilastatin sodium-resistant A. baumannii, carbapenems-resistant P. aeruginosa and MRSA to study the antibiofilm effects of HD5-myr. As shown in Fig. 5a–c, HD5-myr effectively inhibited the formation of biofilms of the aforementioned three types of bacteria in a concentration-dependent manner. HD5-myr demonstrated a more profound bactericidal effect than its parent HD5 peptide.
a–c Biofilm formation by (a) imipenem/cilastatin sodium-resistant A. baumannii, (b) carbapenems-resistant P. aeruginosa and (c) MRSA after 48 h incubation in bacteria medium containing 3.125–50 μg mL-1 of HD5-myr and HD5. Results are expressed as the percentage of biofilm growth for each sample relative to the positive control. Data are shown as mean ± SD and statistical significance was calculated by unpaired two-tailed Student’s t-test (n = 3). *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant. d–f SEM images of bacterial biofilms formation on PVA and PVA@HD5-myr dressings through incubation with (d) imipenem/cilastatin sodium-resistant A. baumannii, (e) carbapenems-resistant P. aeruginosa and (f) MRSA for 48 h (n = 3). Scales bars in left (350 ×), middle (2500 ×) and right (5000 ×) pictures are 50, 10, and 5 μm in length, respectively.
Based on the above results, we speculated that PVA@HD5-myr exhibits similar antibiofilm effects. As anticipated, substantial biofilms were observed on PVA following incubation with imipenem/cilastatin sodium-resistant A. baumannii, carbapenems-resistant P. aeruginosa and MRSA for 48 h. Conversely, minimal biofilm was evident on PVA@HD5-myr (Fig. 5d–f). Taken together, these data demonstrate the promising anti-biofilm activity of PVA@HD5-myr.
The efficacy of PVA@HD5-myr in preventing bacteria invasion and endotoxin release of skin wounds
To evaluate the clinical potential, we applied PVA or PVA@HD5-myr to full-thickness excisional murine wounds infected with MRSA, P. aeruginosa or endotoxin. Our results demonstrated that the wound healing of the mice treated with PVA@HD5-myr was markedly superior to that of the PVA group in the MRSA infection model (Fig. 6a). Hematoxylin and eosin (H&E) staining and Masson’s trichrome staining of skin tissue sections obtained from murine wound models were shown in Fig. 6b–d. The wounded skin of the mice treated with PVA@HD5-myr was significantly more intact than that of the PVA group. The growth of granulation tissue and collagen deposition were more abundant, consistent with the total skin score and collagen positive area results. Of further note, the skin wounds of mice covered with PVA@HD5-myr had a lower bacterial load than those of the PVA group (Fig. 6e). In terms of body weight variations, another indicator of recovery, the mice treated with PVA@HD5-myr maintained similar weight to those of the sham group and were significantly heavier than those of the PVA group (Fig. 6f). At three days after wound dressing, the formation of bacterial biofilms on the PVA dressing was more extensive than on the PVA@HD5-myr dressings (Fig. 6g). Furthermore, a large number of bacterial biofilms formed on the skin surface of the mice in the PVA group, while in the PVA@HD5-myr group, almost no biofilms were formed on the skin surface (Fig. 6h). Next, we evaluated the difference between free HD5-myr and PVA@HD5-myr in the prevention of bacterial invasion of skin wounds. As shown in Supplementary Fig. 17, compared with free HD5-myr, PVA@HD5-myr was more effective in preventing MRSA from invading skin wounds in mice, reducing local bacterial load, and thereby improving skin tissue healing.
a-h Mice skin wound model complicated with MRSA infection. Before bacterial infection, the skin wounds of mice in the PVA group and the PVA@HD5-myr group were respectively covered with two pieces of PVA or PVA@HD5-myr nonwoven fabrics (2 × 2 cm). a Macroscopic imaging of wounds immediately following surgery (day 0) and after 5, 10, or 15 days of treatment in PVA treatment and PVA@HD5-myr treatment group. b Representative images of H&E staining and Masson’s trichrome staining of skin tissue sections from murine wound models. c Total murine skin histopathological scores according to results of H&E staining and Masson’s trichrome staining (n = 8). d Quantification of the positive area of collagen deposition according to Masson’s trichrome staining images (n = 8). e Bacterial burden analysis of murine regenerated skin tissues in PVA and PVA@HD5-myr group after modeling for 15 days (n = 8). f Analysis of body weight change in mice after modeling for 15 days (n = 8). g Formation of bacterial biofilms on PVA or PVA@HD5-myr dressings after modeling for 3 days (n = 5). Scales bars in left (1200 ×) and right (3000 ×) pictures are 10 and 4 μm in length, respectively. h Formation of bacterial biofilms on the skin surface of mice in PVA or PVA@HD5-myr group after modeling for 3 days (n = 5). Scales bars in left (2500 ×) and right (10000 ×) pictures are 5 and 1 μm in length, respectively. Data are shown as mean ± SD and statistical significance was calculated by unpaired two-tailed Student’s t-test for comparison between two experimental groups and one-way ANOVA analysis of variance with Bonferroni corrections for multiple comparisons. *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant.
MRSA is the main G+ bacteria that causes skin wound infections, while P. aeruginosa is the major G- bacteria that infects multiple types of wounds including burn wounds, chronic surgical wounds and diabetic wounds51. Therefore, we further evaluated the therapeutic potential of PVA@HD5-myr using a lethal skin wound model where mice (in three groups of 10 mice each) were infected with lethal doses of P. aeruginosa (1 × 108 CFU per mouse). As shown in Fig. 7a, all the mice died within 40 h after bacterial infection without treatment. Although the physical barrier effect of PVA improved the survival of mice to 40% at 72 h, PVA@HD5-myr achieved more desirable outcomes, raising the survival rate to 80%. The above experiments have confirmed that compared with PVA or free HD5-myr, PVA@HD5-myr has a stronger protective effect against skin wound infections in mice. This could be because PVA@HD5-myr dressings combine both the physical barrier effect of PVA and the bactericidal activity of HD5-myr. The conjugation of HD5-myr to the surface of PVA endows it with the self-cleaning ability, enabling it to adhere to bacteria, disrupt their structure, and inhibit biofilm formation. Moreover, PVA fibers, at the micrometer level, provide the spatial structure that allows HD5-myr to come into full contact with bacteria.
a Kaplan−Meier survival analysis of mice. A full-thickness back skin wound (1 × 1 cm) of BALB/c mice (n = 10) was constructed. Two pieces of PVA or PVA@HD5-myr nonwoven fabrics (2 × 2 cm) covered the wound bed and were fixed with thin transparent dressings. Then P. aeruginosa (ATCC 27853, 1 × 108 CFU in 50 µL PBS) was added. The survival of mice was continuously monitored for 72 h. The data were analyzed by the Mantel-Cox test. b,c Measurement of the binding affinities between HD5 or HD5-myr and LPS by SPR assay using Biacore. (b) HD5 or (c) HD5-myr were covalently immobilized on the CM5 sensor chip through their amine groups and LPS flowed over HD5 or HD5-myr. LPS was diluted to different concentrations (from 0.63 to 10 μM). The interactive parameters, including association constant (Ka), dissociation constant (Kd) and equilibrium dissociation constant (KD) were calculated by BIA evaluation software. The resulting data were fit to a 1:1 binding model. d–g Mice skin wound model complicated with endotoxin infection. Analysis of (d) endotoxin and cytokines including (e) TNF-α, (f) IL-1β and (g) IL-6 in skin wound of mice after modeling for 6 h (n = 13). Data are shown as mean ± SD and statistical significance was calculated by one-way ANOVA analysis of variance with Bonferroni corrections for multiple comparisons. *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant.
A previous study demonstrated that HD5, which contains three disulfide bonds, has little anti-endotoxin effect52. Here, we found that unlike HD5 (KD = 9.44×10-6 M), HD5-myr can strongly bind to endotoxin (KD = 5.14×10-10 M) (Fig. 7b, c). This binding capacity is crucial for neutralizing the pathogenic effects of LPS52. Moreover, targeting LPS and its transporters is also an emerging research direction for antibacterial drugs53,54. As shown in Supplementary Fig. 18 and Supplementary Table 5, HD5-myr inhibited the release of tumor necrosis factor (TNF)-α at the cellular level in vitro, whereas HD5, which exhibits weaker binding capacity to LPS, lacked this effect. This enhanced endotoxin-binding ability may be related to increased hydrophobicity when modified with myristic acid55. To evaluate the ability of PVA@HD5-myr to adsorb endotoxins and protect skin wounds in vivo, we further established an endotoxin infection model (Supplementary Fig. 19). As shown in Fig. 7d–g, after endotoxin inoculation on wounds of mice in the control and PVA group, the levels of endotoxin and inflammatory factors (TNF-α, IL-1β and IL-6) in the skin were significantly increased compared to the PVA@HD5-myr group. These results demonstrate that the application of PVA@HD5-myr can effectively prevent endotoxin diffusion into skin wounds and then mediate the local inflammatory response.
Biocompatibility of PVA@HD5-myr
This PVA@HD5-myr will be in direct contact with the open wound as a dressing. Accordingly, we evaluated the hemolysis and cytotoxicity of PVA@HD5-myr in vitro. Our previous study has demonstrated that the antimicrobial peptide HD5-myr exhibited no meaningful hemolytic activity and cytotoxicity even at relatively high concentrations (100 μg mL-1)23. In order to determine its biocompatibility, PVA@HD5-myr was immersed in Roswell Park Memorial Institute (RPMI) 1640 medium for 24 h, and then the extract was analyzed by MTT (3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide) assay and hemolysis assay. A mouse fibroblast, namely L929, was selected to evaluate the cytotoxicity using the MTT assay. Supplementary Fig. 20a, b showed that both PVA and PVA@HD5-myr extract exhibited acceptable cytotoxicity at 100% concentrations. In the hemolysis assay, no visible hemolytic effect was observed after 1 h of incubation with red blood cells (RBCs) (Supplementary Fig. 20c, d). To further evaluate the biocompatibility of PVA@HD5-myr in vivo, we induced a full-thickness back skin wound in mice. We covered the wound with the PVA@HD5-myr or PVA (as a control) dressing, which was changed every 2 days for 15 days before organs and blood were harvested. Histopathological examination showed no significant pathological changes between the groups in the liver, spleen or kidney (Supplementary Fig. 20e). Biochemical analysis of the blood, including blood urea nitrogen (BUN), creatinine (CREA), aspartate aminotransferase (AST) and alanine aminotransferase (ALT) also confirmed no liver and kidney damage (Supplementary Fig. 20f–i). In addition, H&E staining, Masson’s trichrome staining and immunohistochemical staining of skin tissue sections were obtained from murine wound models. Granulation tissue formation was enhanced, and abundant collagen accumulated within the wound beds after PVA@HD5-myr treatment (Supplementary Fig. 20e). Immunohistochemical staining was performed on the vascular endothelial cell marker CD31 (also known as platelet endothelial cell adhesion molecule-1, PECAM-1)56, macrophage marker F4/80 and neutrophil marker Ly6G to verify the effect of PVA@HD5-myr on angiogenesis and local inflammation during wound healing. Vascular endothelial cells (CD31-positive cells) were abundant in both PVA and PVA@HD5-myr groups (Supplementary Fig. 20e), indicating good angiogenesis. All groups had minimal neutrophil infiltration (Ly6G-positive cells) in all groups, demonstrating that PVA@HD5-myr did not lead to persistent inflammatory response. Macrophages play a critical role in routine wound healing and tissue regeneration, and increasing the number of macrophages in the wound can significantly accelerate wound healing1,57. Infiltration of macrophages (F4/80-positive cells) in PVA and PVA@HD5-myr groups was more abundant than that in the sham operation group during the wound remodeling stage, indicating good wound healing (Supplementary Fig. 20e). Moreover, there was no difference in body weight variations between PVA and PVA@HD5-myr groups after 15 days of treatment (Supplementary Fig. 20j). Based on the above experimental results, we revealed that PVA@HD5-myr did not cause significant cytotoxicity or systemic damage, and fully complied with the clinical application needs.
Conclusions
In summary, we developed and produced a medical dressing capable of effectively protecting skin wounds through a designed industrial production route. Based on the biological activity of HD5-myr, the designed PVA@HD5-myr nonwoven fabrics exhibited excellent bactericidal, anti-biofilm and endotoxin adsorption capabilities, including clinical multidrug-resistant bacteria. Furthermore, the HD5-myr was grafted to the surface of PVA in the spinning process of PVA fibers by incorporating the titanate coupling agent Tyzor®LA. This straightforward and efficient method diminishes the production process and the cost. More importantly, this production process preserved the biological activity of HD5-myr, which is highly susceptible to temperature and other factors. Collectively, PVA@HD5-myr dressings provide a safe, effective, and economical strategy to protect wounds from infection, with substantial potential for clinical application.
Methods
Materials
HD5 and HD5-myr in this study were chemically synthesized via solid-phase peptide synthesis by CHINESE PEPTIDE (Hangzhou, China). The obtained peptides were purified by HPLC, and molecular weights were verified by MALDI-TOF MS (BRUKER ultrafleXtreme, Germany). PVA (26–99), with degree of alcoholysis 98–100%, was purchased from Anhui Wanwei Group Co., Ltd (Chao Hu, China). The Luria-Bertani (LB) medium was composed of 5 g yeast extract (Thermo Scientific Oxoid, USA), 10 g tryptone (Thermo Scientific Oxoid, USA) and 10 g NaCl (Sinopharm Chemical Reagent Co., Ltd.; China) per 1000 mL double distilled water (ddH2O). To generate solid LB agar plates, and additional 15 g agar powder (Sinopharm Chemical Reagent Co., Ltd.; China) was added to the above formula. All bacterial culture media were sterilized by autoclaving to remove possible biological contamination before use. The bacterial strains used in this project, including E. coli (25922), K. pneumoniae (13883), S. aureus (25923), A. baumannii (17978), P. aeruginosa (27853), MRSA (43300), were obtained from American Type Culture Collection (ATCC). The clinical isolates, carbapenems-resistant P. aeruginosa, were obtained from the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China. The bacterial strains including imipenem/cilastatin sodium-resistant A. baumannii and vancomycin-resistant S. aureus used in this study were induced from A. baumannii (17978) and S. aureus (25923).
Animals
BALB/c and C57BL/6 mice used in this study were purchased from the Shanghai SLAC Laboratory Animal Center. Animal protocols were approved by the Institutional Animal Care and Use Committee (IACUC) of Zhejiang University.
Synthesis of PVA@HD5-myr nonwoven fabrics
PVA was repeatedly cleaned with ultrapure water and soaked for 2 h at room temperature. Then PVA aqueous solution (16 %, wt/wt) was prepared by dissolving PVA granule in ultrapure water with vigorous stirring at 90 °C–100 °C and the pH of the solution was adjusted to 5.5–6.5 with aqueous solution of citric acid. After the solution was cooled down to 25 °C ± 2 °C, HD5-myr (14 ppm) was added to form the mixtures. The mixtures were stirred thoroughly to obtain homogeneous spinning dope. Before ejecting the fiber from the spinneret, the crosslinking agent Tyzor®LA (60 ppm) was added continuously through the metering pump. Then the spinning dope containing Tyzor®LA was made into PVA@HD5-myr fibers, which were dried and stretched in the spinning shaft containing hot air (45 °C–50°C). Next, the PVA@HD5-myr fibers were prepared into spunlaced nonwoven fabrics with a basis weight of 68 g m-2. Finally, PVA@HD5-myr nonwoven fabrics were sterilized by 60Co (15 kGy) irradiation.
SEM and EDS analysis of PVA and PVA@HD5-myr nonwoven fabrics
The physical morphologies and element composition of PVA and PVA@HD5-myr nonwoven fabrics were analyzed via the combined SEM and SEM-EDS. Firstly, PVA@HD5-myr was washed thoroughly with distilled water to remove the HD5-myr that was not covalently bound on the surface. Dried samples were sputter-coated with platinum using a sputter coater (Hitachi, Japan). The morphology of samples was examined using an SEM (ZEISS GeminiSEM 300, Germany), while elemental analysis (C, O, N for PVA and PVA@HD5-myr) was performed using BRUKER EDS (Germany) at 12 keV.
XPS analysis
The surface elemental composition of PVA and PVA@HD5-myr nonwoven fabrics were analyzed using an X-ray photoelectron spectrometer (Thermo Scientific ESCALAB 250Xi, USA). Monochromatic Al Kα X-ray (hv = 1486.6 eV) was employed for analysis. The analysis diameter of the samples was approximately 500 µm. The analysis depth of the samples was approximately 50–100 nm. The elemental atomic percentages of PVA (C, O), HD5-myr (C, O, N, S) and PVA@HD5-myr (C, O, N, S, Ti) were determined.
In vitro antimicrobial activity assay of PVA@HD5-myr nonwoven fabrics
The antimicrobial activity assay of PVA and PVA@HD5-myr nonwoven fabrics referred to the National Standards of P.R.C (GB 15979-2002) and was modified appropriately. Briefly, single colonies from LB agar plates were cultured in 5 mL LB medium. After growing for 6–8 h at 37 °C, 200 rpm in an incubator, the bacteria were washed thrice with PBS. To determine the bactericidal activity, 5 mL bacterial suspension was added into a conical flask containing 50 mL PBS, and the bacterial concentration was adjusted to 1 × 106 CFU mL-1. Three pieces of PVA or PVA@HD5-myr nonwoven fabrics (6 × 6 cm) were added into the conical flask and then incubated at 37 °C, 200 rpm for 1 h. Following incubation, the bacteria in the conical flask were counted. In some experimental groups, PVA@HD5-myr nonwoven fabrics were treated at 37 °C, 60% RH for 33 days before antimicrobial activity assay to test their stability. The experiments were repeated three times. The lower limit of detection was 100 CFU. To visualize the data on a logarithmic scale, a value of 100 CFU was assigned when no bacterial growth occurred.
Bacterial morphology under SEM
The morphologies of carbapenems-resistant P. aeruginosa, imipenem/cilastatin sodium-resistant A. baumannii and MRSA after treatment with PVA or PVA@HD5-myr nonwoven fabrics were observed under a Nova Nano 450 field-emission electron microscope (Thermo FEI, USA). Bacteria (OD600 = 1.0) were added to PVA or PVA@HD5-myr nonwoven fabrics and incubated at room temperature for 1 h. A 2.5% glutaraldehyde solution was added for fixation overnight at 4 °C. Then, the samples were washed with PBS three times and then incubated with 1% OSO4 solution for 1.5 h. After washing another three times with PBS, dehydration was performed using a gradient concentration of ethanol solution (one time in 30, 50, 70, 80, 90, and 95% for 15 min and two times in 100% for 20 min each). After drying in a LEICA EM CPD300 critical point dryer (LEICA, Germany), the samples were coated with platinum before SEM analysis.
LIVE/DEAD assay to examine bacterial viability
Bacteria suspension (final concentration of 5 × 107 CFU mL-1) was added into a conical flask containing 50 mL PBS. PVA or PVA@HD5-myr nonwoven fabrics were added into the conical flask and then incubated at 37 °C, 200 rpm. After 1 h, the bacteria were pelleted and resuspended with 0.9% NaCl. Then bacteria were stained with LIVE/DEAD BacLight Bacterial Viability Kits (including PI and SYTO 9 dye; Invitrogen L13152, USA) for 15 min and observed with a laser scanning confocal microscopy (Olympus FV3000, Japan)58. The excitation/emission maxima for these dyes are about 480/500 nm for SYTO 9 stain and 490/635 nm for PI.
In vitro inhibition of biofilm formation by HD5 and HD5-myr
As described previously59, single colonies of bacteria (carbapenems-resistant P. aeruginosa, imipenem/cilastatin sodium-resistant A. baumannii, or MRSA) from LB agar plates were selected and cultured to mid-logarithmic growth phase in 5 mL of LB medium at 37 °C, 200 rpm. In the 96-well polypropylene plates (Corning, USA), bacteria (a final OD600 of 0.01) were exposed to HD5 and HD5-myr in Tryptic Soy Broth (TSB) medium (Solarbio, China) supplemented with 1% (wt/vol) glucose (Sinopharm Chemical Reagent Co., Ltd.; China). The final concentrations of HD5 and HD5-myr ranged from 3.125 to 50 μg mL-1. As an untreated control, bacteria were exposed to a TSB medium supplemented with 1% (wt/vol) glucose without HD5 or HD5-myr. After 48 h incubation at 37 °C, spent growth medium and non-adhered planktonic cells were removed by three washes with PBS. Biofilms were stained with 0.1% (wt/vol) crystal violet (Aladdin, China) for 30 min at room temperature with gentle shaking on an orbital shaker, washed again, and solubilized with 75% ethanol for 30 min. The absorbance at 595 nm was determined on a microplate spectrophotometer to measure biofilm mass.
In vitro antibiofilm effect of PVA@HD5-myr nonwoven fabrics
The antibiofilm effect of PVA@HD5-myr nonwoven fabrics was evaluated against bacteria of imipenem/cilastatin sodium-resistant A. baumannii, carbapenems-resistant P. aeruginosa and MRSA. Briefly, microbial suspension (1 mL, 3 × 106 CFU mL-1) was cultured with PVA or PVA@HD5-myr (1 × 1 cm) in a 24-well plate (Corning, USA) and incubated for 48 h at 37 °C. After that, all samples were taken out and washed thoroughly with PBS to remove the plankton bacteria. Then PVA and PVA@HD5-myr were added into 2.5% glutaraldehyde solution for fixation overnight 4 °C. Samples were prepared using the above method and observed with SEM.
Murine wound bacterial infection model
Seven to eight weeks of male BALB/c mice, weighing 22–24 g, were used in this experiment. The mice were individually raised in cages at a standardized environment and night cycle and given an autoclaved rodent diet and sterile water and then randomly divided into three groups, including the sham-operated group, the PVA treatment group, and the PVA@HD5-myr treatment group. Mice were weighed and anesthetized with an intraperitoneal injection of ketamine/xylazine (100 and 10 mg kg-1). Then, the hair was shaved from the backside of the mice using a depilatory cream. The mice of the sham-operated group did not undergo cutaneous wound surgery, while the other groups underwent cutaneous wound surgery after anesthesia. A full-thickness back skin wound (1 × 1 cm) of mice was cut using a surgical scalpel. Two pieces of PVA or PVA@HD5-myr nonwoven fabrics (2 × 2 cm) covered the wound bed and were fixed with thin transparent dressings (SIMP, Shanghai, China). To verify the effect of nonwoven fabrics against bacterial infection, 1 × 106 CFU of MRSA was added. After 15 days, the mice were weighed again. We photographed the wound areas to analyze wound healing and all mice in the three groups. Skin tissue samples were excised and used for bacterial burden measurement, H&E staining and Masson’s trichrome staining. Skin histopathological scores were based on the five aspects described previously60, including epidermal regeneration (0, none; 1, mild; 2, moderate; 3, complete), neovascularization (0, absence; 1, occasional presence; 2, light scattering; 3, abundance), collagen deposition (0, 0–10% positive area; 1, 10–20% positive area; 2, 20%-30% positive area; 3, 30%-40% positive area; 4, å 40% positive area), granulation tissue thickness (0, none; 1, mild; 2, moderate; 3, complete) and inflammatory infiltration (0, severe; 1, moderate; 2, mild; 3, almost absent). The positive area of skin collagen deposition was analyzed using ImageJ software. On the third day after the injury, bacterial biofilm formation on the PVA or PVA@HD5-myr dressings and on the skin surface of mice were examined under SEM.
Bacterial burden measurement
Skin tissue samples collected 15 days post-wounding were homogenized using a homogenizer (TissuePrep, Tianjin, China) and diluted in sterile PBS. The homogenate was diluted and then inoculated on LB plates. The number of bacteria was counted after overnight incubation at 37 °C, and the results were expressed as CFU per gram of tissue. To visualize the data on a logarithmic scale, a value of 1 CFU was assigned when no growth occurred61.
SPR
SPR binding experiments were carried out on a BIAcore 3000 system. The assay buffer adopted in this assay was HBS-EP, containing 0.15 M NaCl, 3 mM EDTA, 0.05% (vol/vol) surfactant P20, and 0.01 M HEPES (pH 7.4). HD5 and HD5-myr dissolved in 10 mM NaAc (pH 4.5) were immobilized on a CM5 sensor chip using the amine-coupling chemistry recommended by the manufacturer’s instructions. A series of concentrations of LPS (Escherichia coli O111:B4; Sigma-Aldrich L2630, USA) was introduced into the flow channels at 30 mL min-1 in the assay buffer. The molecular mass for E. coli O111:B4 LPS was considered to be 10 KDa62. Association and dissociation were assessed for 3 min. Resonance signals were corrected for non-specific binding by subtracting the background of the control flow channel. After each analysis, the CM5 sensor chip surfaces were regenerated with 10 mM citric acid/1 M NaCl (pH 2.95) and 10 mM Gly/HCl solution (pH 2.5) for 400 s at a flow rate of 30 μL min-1, and equilibrated with the buffer before next injection. The manufacturer-supplied software for BIAcore 3000 was applied to analyze the signal curves and calculate the association constant (Ka), dissociation constant (Kd), and affinity constant (KD). Data was analyzed using GraphPad 7.0 software.
Mouse wound acute inflammation model
Seven to eight weeks of male BALB/c mice were randomly divided into four groups, the sham-operated group, the control group, the PVA treatment group, and the PVA@HD5-myr treatment group. Each group of mice except the sham-operated group were treated with the same trauma described above. The PVA and PVA@HD5-myr treatment group were covered with two pieces of PVA and PVA@HD5-myr nonwoven fabrics (2 × 2 cm), respectively, and then thin transparent dressings (SIMP, Shanghai, China) were fixed. To verify the effect of nonwoven fabrics against bacterial endotoxin, LPS (20 μg in 50 μL PBS) was added to the wound site. After 6 h, the wound areas were washed six times with 50 μL of endotoxin-free water (Sigma-Aldrich, USA) each time. Endotoxin was removed from all instruments used in this experiment.
Survival analysis of mice
A full-thickness back skin wound (1 × 1 cm) of BALB/c mice was constructed. Then two pieces of PVA or PVA@HD5-myr dressings (2 × 2 cm) covered the wound bed and were fixed with thin transparent dressings. The skin wound of mice in control group was not covered with dressing. Then P. aeruginosa (ATCC 27853, 1 × 108 CFU in 50 µL PBS) was added. The survival of mice was continuously monitored for 72 h.
Limulus amebocyte lysate (LAL) assay
According to the manufacturer’s instructions, the endotoxin content in skin washing fluids was measured by a PierceTM Chromogenic Endotoxin Quant kit (Thermo Scientific, USA).
Cytokine Measurement
The skin washing fluids were used to analyze TNF-α, IL-6 and IL-1β protein levels using enzyme-linked immunosorbent assay (Novus Biologicals, Bio-Techne China) according to the manufacturer’s recommendations.
Data availability
All data generated or analyzed during this study are included in this paper and its supplementary information files.
References
Peña, O. A. & Martin, P. Cellular and molecular mechanisms of skin wound healing. Nat. Rev. Mol. Cell Biol. 25, 599–616 (2024).
Kim, H. S. et al. Advanced drug delivery systems and artificial skin grafts for skin wound healing. Adv. Drug Deliv. Rev. 146, 209–239 (2019).
Sen, C. K. et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 17, 763–771 (2009).
Rudd, K. E. et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet 395, 200–211 (2020).
Eming, S. A., Martin, P. & Tomic-Canic, M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci. Transl. Med. 6, 265sr6 (2014).
Ding, X. et al. Challenges and innovations in treating chronic and acute wound infections: from basic science to clinical practice. Burns Trauma 10, tkac014 (2022).
Lachiewicz, A. M., Hauck, C. G., Weber, D. J., Cairns, B. A. & van Duin, D. Bacterial Infections After Burn Injuries: Impact of Multidrug Resistance. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 65, 2130–2136 (2017).
Flemming, H.-C. et al. Biofilms: an emergent form of bacterial life. Nat. Rev. Microbiol. 14, 563–575 (2016).
Rumbaugh, K. P. & Sauer, K. Biofilm dispersion. Nat. Rev. Microbiol. 18, 571–586 (2020).
Biswas, S. K. & Lopez-Collazo, E. Endotoxin tolerance: new mechanisms, molecules and clinical significance. Trends Immunol. 30, 475–487 (2009).
Rathinam, V. A. K., Zhao, Y. & Shao, F. Innate immunity to intracellular LPS. Nat. Immunol. 20, 527–533 (2019).
Dong, Y., Fu, S., Yu, J., Li, X. & Ding, B. Emerging smart micro/nanofiber-based materials for next-generation wound dressings. Adv. Funct. Mater. 34, 2311199 (2023).
Farahani, M. & Shafiee, A. Wound healing: from passive to smart dressings. Adv. Healthc. Mater. 10, e2100477 (2021).
López-Iglesias, C. et al. Vancomycin-loaded chitosan aerogel particles for chronic wound applications. Carbohydr. Polym. 204, 223–231 (2019).
Xiang, J. et al. Mussel-inspired immobilization of zwitterionic silver nanoparticles toward antibacterial cotton gauze for promoting wound healing. Chem. Eng. J. 409, 128291 (2021).
Wang, M. et al. Antibacterial fluorescent nano-sized lanthanum-doped carbon quantum dot embedded polyvinyl alcohol for accelerated wound healing. J. Colloid Interface Sci. 608, 973–983 (2022).
Liu, N. et al. Construction of multifunctional hydrogel with metal-polyphenol capsules for infected full-thickness skin wound healing. Bioact. Mater. 24, 69–80 (2023).
Xu, H. et al. Green fabrication of amphiphilic quaternized β-chitin derivatives with excellent biocompatibility and antibacterial activities for wound healing. Adv. Mater. 19, e1801100 (2018).
Zou, P. et al. Wound dressing from polyvinyl alcohol/chitosan electrospun fiber membrane loaded with OH-CATH30 nanoparticles. Carbohydr. Polym. 232, 115786 (2020).
Sarhan, W. A., Azzazy, H. M. E. & El-Sherbiny, I. M. Honey/chitosan nanofiber wound dressing enriched with allium sativum and cleome droserifolia: enhanced antimicrobial and wound healing activity. ACS Appl. Mater. Interfaces 8, 6379–6390 (2016).
Li, W., Thian, E. S., Wang, M., Wang, Z. & Ren, L. Surface Design for Antibacterial Materials: From Fundamentals to Advanced Strategies. Adv. Sci. 8, e2100368 (2021).
de Breij, A. et al. The antimicrobial peptide SAAP-148 combats drug-resistant bacteria and biofilms. Sci. Transl. Med. 10, eaan4044 (2018).
Lei, R. et al. Self-assembling myristoylated human alpha-defensin 5 as a next-generation nanobiotics potentiates therapeutic efficacy in bacterial infection. ACS Nano 12, 5284–5296 (2018).
Gao, X. et al. Defensins: the natural peptide antibiotic. Adv. Drug Deliv. Rev. 179, 114008 (2021).
Fu, J. et al. Mechanisms and regulation of defensins in host defense. Signal Transduct. Target. Ther. 8, 300 (2023).
Teodorescu, M., Bercea, M. & Morariu, S. Biomaterials of PVA and PVP in medical and pharmaceutical applications: perspectives and challenges. Biotechnol. Adv. 37, 109–131 (2019).
Zhao, H. et al. ROS-scavenging hydrogel to promote healing of bacteria infected diabetic wounds. Biomaterials 258, 120286 (2020).
Homaeigohar, S. & Boccaccini, A. R. Antibacterial biohybrid nanofibers for wound dressings. Acta Biomaterialia 107, 25–49 (2020).
Fu, C. et al. Protein-based bioactive coatings: from nanoarchitectonics to applications. Chem. Soc. Rev. 53, 1514–1551 (2024).
Sun, W., Liu, W., Wu, Z. & Chen, H. Chemical surface modification of polymeric biomaterials for biomedical applications. Macromol. Rapid Commun. 41, e1900430 (2020).
Zhang, J. et al. Modified magnesium oxide/silver nanoparticles reinforced poly (butylene succinate-co-terephthalate) composite biofilms for food packaging application. Food Chem. 435, 137492 (2024).
Elshereksi, N. W., Ghazali, M., Muchtar, A. & Azhari, C. H. Review of titanate coupling agents and their application for dental composite fabrication. Dent. Mater. J. 36, 539–552 (2017).
Goddard, J. M. & Hotchkiss, J. H. Polymer surface modification for the attachment of bioactive compounds. Prog. Polym. Sci. 32, 698–725 (2007).
Elshereksi, N. W., Ghazali, M. J., Muchtar, A. & Azhari, C. H. Studies on the effects of titanate and silane coupling agents on the performance of poly (methyl methacrylate)/barium titanate denture base nanocomposites. J. Dent. 56, 121–132 (2017).
Prosini, P. P., Cento, C. & Pozio, A. Tyzor®-LA used as a precursor for the preparation of carbon coated TiO2. J. Power Sources 248, 1021–1027 (2014).
Mathew, B. & Nagaraj, R. Antimicrobial activity of human alpha-defensin 5 and its linear analogs: N-terminal fatty acylation results in enhanced antimicrobial activity of the linear analogs. Peptides 71, 128–140 (2015).
Lin, W. et al. Multi-biofunctionalization of a titanium surface with a mixture of peptides to achieve excellent antimicrobial activity and biocompatibility. J. Mater. Chem. B 3, 30–33 (2015).
Guo, Y., Nuermaimaiti, A., Kjeldsen, N. D., Gothelf, K. V. & Linderoth, T. R. Two-dimensional coordination networks from cyclic dipeptides. J. Am. Chem. Soc. 142, 19814–19818 (2020).
Salles, R. C. M., Coutinho, L. H., da Veiga, A. G., Sant’Anna, M. M. & de Souza, G. G. B. Surface damage in cystine, an amino acid dimer, induced by keV ions. J. Chem. Phys. 148, 045107 (2018).
Wang, X. et al. A soft multifunctional film from chitosan modified with disulfide bond cross-links and prepared by a simple method. Int. J. Biol. Macromol. 253, 126774 (2023).
Zhang, P. et al. Disulfide bond reconstruction: a novel approach for grafting of thiolated chitosan onto wool. Carbohydr. Polym. 203, 369–377 (2019).
Sun, H. et al. High-safety and high-energy-density lithium metal batteries in a novel ionic-liquid electrolyte. Adv. Mater. 32, e2001741 (2020).
Zhang, Z., Wang, M., Zhou, H. & Wang, F. Surface sulfate ion on CdS catalyst enhances syngas generation from biopolyols. J. Am. Chem. Soc. 143, 6533–6541 (2021).
Ren, Y. et al. Effects of different TiO2 particle sizes on the microstructure and optical limiting properties of TiO2/reduced graphene oxide nanocomposites. Nanomaterials 9, 730 (2019).
Sher Shah, M. S. A., Park, A. R., Zhang, K., Park, J. H. & Yoo, P. J. Green synthesis of biphasic TiO₂-reduced graphene oxide nanocomposites with highly enhanced photocatalytic activity. ACS Appl. Mater. Interfaces 4, 3893–3901 (2012).
Zhou, T. et al. Super-tough MXene-functionalized graphene sheets. Nat. Commun. 11, 2077 (2020).
Mookherjee, N., Anderson, M. A., Haagsman, H. P. & Davidson, D. J. Antimicrobial host defence peptides: functions and clinical potential. Nat. Rev. Drug Discov. 19, 311–332 (2020).
Lazzaro, B. P., Zasloff, M. & Rolff, J. Antimicrobial peptides: application informed by evolution. Science 368, eaau5480 (2020).
Hancock, R. E. W., Alford, M. A. & Haney, E. F. Antibiofilm activity of host defence peptides: complexity provides opportunities. Nat. Rev. Microbiol. 19, 786–797 (2021).
Haidar, A. et al. Biofilm formation and antibiotic resistance in Pseudomonas aeruginosa. Microbe 3, 100078 (2024).
Uberoi, A., McCready-Vangi, A. & Grice, E. A. The wound microbiota: microbial mechanisms of impaired wound healing and infection. Nat. Rev. Microbiol. 22, 507–521 (2024).
Wang, C. et al. Reduction impairs the antibacterial activity but benefits the LPS neutralization ability of human enteric defensin 5. Sci. Rep. 6, 22875 (2016).
Zampaloni, C. et al. A novel antibiotic class targeting the lipopolysaccharide transporter. Nature 625, 566–571 (2024).
Pahil, K. S. et al. A new antibiotic traps lipopolysaccharide in its intermembrane transporter. Nature 625, 572–577 (2024).
Lei, R. et al. Turning cationic antimicrobial peptide KR-12 into self-assembled nanobiotics with potent bacterial killing and LPS neutralizing activities. Nanoscale 16, 887–902 (2024).
Piera-Velazquez, S. & Jimenez, S. A. Endothelial to mesenchymal transition: role in physiology and in the pathogenesis of human diseases. Physiol. Rev. 99, 1281–1324 (2019).
Rodrigues, M., Kosaric, N., Bonham, C. A. & Gurtner, G. C. Wound healing: a cellular perspective. Physiol. Rev. 99, 665–706 (2019).
Yan, D. et al. Adding flying wings: butterfly-shaped NIR-II aiegens with multiple molecular rotors for photothermal combating of bacterial biofilms. J. Am. Chem. Soc. 145, 25705–25715 (2023).
Etayash, H., Haney, E. F. & Hancock, R. E. W. Assessing biofilm inhibition and immunomodulatory activity of small amounts of synthetic host defense peptides synthesized using SPOT-array technology. Nat. Protoc. 16, 1850–1870 (2021).
Luo, G. et al. Nanodefensin-encased hydrogel with dual bactericidal and pro-regenerative functions for advanced wound therapy. Theranostics 11, 3642–3660 (2021).
Riool, M. et al. Staphylococcus epidermidis originating from titanium implants infects surrounding tissue and immune cells. Acta Biomaterialia 10, 5202–5212 (2014).
Domadia, P. N., Bhunia, A., Ramamoorthy, A. & Bhattacharjya, S. Structure, interactions, and antibacterial activities of MSI-594 derived mutant peptide MSI-594F5A in lipopolysaccharide micelles: role of the helical hairpin conformation in outer-membrane permeabilization. J. Am. Chem. Soc. 132, 18417–18428 (2010).
Acknowledgements
This work was supported by the Key Research and Development Program of Zhejiang (NO. 2022C03163), the National Natural Science Foundation of China (NO. 82072148 and 81902008) and Natural Science Foundation of Zhejiang Province (LQ21H150003). We give special thanks to Mr. Sidong Zhang and Ms. Longxue Fan from Zhejiang Longterm Medical Technology Co., Ltd. (Huzhou, China) for their excellent guidance in the design and production of the PVA@HD5-myr dressings. We thank Mr. Qikang Gao and Ms. Chao Sun in the Analysis Center of Agrobiology and Environmental Sciences, Zhejiang University, for their technical assistance in SPR and MALDI-TOF MS. We are grateful to Ms. Dandan Song and Ms. Guizhen Zhu in the Center of Cryo-Electron Microscopy (CCEM), Zhejiang University, for performing SEM and EDS. We thank Ms. Xinning Zhang from Testing and Analysis Center of Department of Ploymer Science and Engineering, Zhejiang University for the assistance in performing AFM measurements. We thank Ms. Yangfan Lu in the School of Materials Science and Engineering, Zhejiang University, for her help on XPS measurement and analysis. We thank Ms. Zhaoxiaonan Lin from the Core Facilities, Zhejiang University School of Medicine for her technical support in laser scanning confocal microscopy. Authors also thank Dr. Dingxiang Xu, Meng Liu and Jingdu Li from Shanghai Personal Biotechnology Co., Ltd. (Shanghai, China) for their technical assistance in 16S rRNA gene sequencing.
Author information
Authors and Affiliations
Contributions
X.F., R.L., Q.S., Y.S. and J.H. conceived the project and designed the experiments. Y.S., L.H. and Y.L. carried out the experiments and obtained the data. H.Y. and J.H. contributed to interpretation of the results. H.Y., Z.X., Y.Z., Q.C., G.X. and H.L. guided conduct of the experiment and analyzed the data. X.F., Y.S., R.L. and Y.W. wrote the manuscript. X.F. and R.L. supervised the study. All authors discussed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Materials thanks the anonymous reviewers for their contribution to the peer review of this work. [A peer review file is available].
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
43246_2025_944_MOESM2_ESM.pdf
Supplementary Information for Defensin-Conjugated Polymer Fabrics Combat Drug-Resistant Biofilms and Toxins in Skin Wounds
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, Y., Ye, H., Hao, L. et al. Defensin-conjugated polymer fabrics combat drug-resistant biofilms and toxins in skin wounds. Commun Mater 6, 224 (2025). https://doi.org/10.1038/s43246-025-00944-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43246-025-00944-7