Abstract
Adolescent and young adults (AYAs) with chronic myeloid leukemia in chronic phase (CML-CP) reportedly respond worse to tyrosine kinase inhibitors (TKIs) than adults, potentially due to additional genetic abnormalities, including mutations in cancer-related genes (CRGs). This real-life study compared mutation profiles and their impact on outcomes in 80 AYA, 97 adult, and 16 pediatric CML-CP patients, alongside 81 BCR::ABL1-positive acute lymphoblastic leukemia (Ph+ ALL) patients. CRG mutations were more frequent in AYAs (25.0%) than in adults (19.6%) or children (12.5%). AYAs with Ph+ ALL exhibited higher mutational frequencies (53.3%) compared to children (26.7%) and adults (38.9%). At diagnosis, mutations in ASXL1, DNMT3A, and TET2 dominated in CML-CP and RUNX1, IKZF1, and BCR::ABL1 in Ph+ ALL. ASXL1 mutations correlated with reduced progression-free survival (PFS) in AYAs and adults. Unlike adults, AYAs showed no increase in BCR::ABL1 kinase domain mutations during TKI therapy. Nilotinib improved PFS in AYAs with ASXL1 mutations, highlighting the efficacy of higher-generation TKIs. ASXL1 mutations also impaired erythropoiesis, warranting further validation. Despite a higher mutational burden, AYAs did not exhibit worse prognoses than adults. Lower mutation rates at follow-up suggest potential impact of nilotinib. Mutation profiling and optimized TKI use are crucial to mitigate progression risks in CRG-mutated patients.

Similar content being viewed by others
Introduction
Chronic myeloid leukemia (CML) is characterized by a translocation t(9;22)(q34;q11.2), which results in BCR::ABL1 rearrangement. Targeting the BCR::ABL1 protein with tyrosine kinase inhibitors (TKIs) dramatically changed outcome of CML patients. The landscape of TKI therapy has evolved with the introduction of second and third-generation TKIs that have demonstrated enhanced efficacy and a broader spectrum of BCR::ABL1 inhibition compared to their predecessors [1, 2]. Currently, most patients with chronic phase CML (CML-CP) achieve a normal life expectancy. Factors affecting the efficiency of TKI treatment include the availability of drugs, their tolerability, the emergence of resistance to TKIs, as well as patient compliance, comorbidities, and age-related considerations [3, 4].
The incidence of CML rises with age, with the median age at diagnosis exceeding 60 years [5, 6] and the highest occurrence observed in individuals aged 75 and over. Prior to the integration of TKIs into clinical practice, advanced age was regarded as an adverse prognostic factor [7] and was involved in calculation of SOKAL and Euro scores [8, 9]. Despite adolescents and young adults (AYAs), defined by the National Comprehensive Cancer Network (NCCN) Guidelines (Version 2.2024) as patients aged 15–39, accounting for 7–10% of newly diagnosed CML cases, they remain understudied.
Several clinical trials have indicated that AYA CML patients present with elevated white blood cell counts, larger spleen sizes, and lower hemoglobin levels at diagnosis compared to their older counterparts [10, 11]. Additionally, a higher proportion of AYA patients exhibit BCR::ABL1 transcript levels exceeding 10% on the international scale (IS) at 3 months post-TKI initiation [10]. These indicators are reflective of the potentially aggressive nature of CML in this specific age group and underscore the unique challenges faced by AYA patients in disease management. However, studies have not consistently demonstrated lower probabilities of achieving major molecular response (MMR) and complete cytogenetic response (CCgR) in AYA patients. Importantly, none of these studies have confirmed the impact of age on overall survival and progression-free survival (PFS). The lack of consistent evidence emphasizes the need for further research and comprehensive investigations of AYA CML patients.
Despite the continual improvement in CML patient outcomes, ongoing research has shown that additional genetic abnormalities, including somatic mutations in cancer-related genes (CRGs), were responsible for worse response to TKIs [12,13,14,15]. Mutations in genes encoding epigenetic modifiers such as ASXL1, DNMT3A, and TET2 have been shown to elevate the risk of molecular relapse upon treatment discontinuation [16]. Moreover, these mutations are not isolated events but are frequently associated with clonal hematopoiesis, especially in CML patients of advanced age, typically those above 65 years [17,18,19]. On the other hand, patients carrying ASXL1 mutations at the time of diagnosis are often characterized as younger individuals facing a higher risk classification [13], indicating a role of clonal evolution associated with ASXL1 mutations in CML pathogenesis. This suggests a potential role for these mutations as prognostic markers in guiding treatment decisions and long-term management strategies for CML patients.
In this study, our objective was to explore the spectrum of somatic mutations in adolescent and young adult patients with CML in chronic phase (CML-CP) treated with adult protocol and to compare them with pediatric and adult CML patients, as well as with patients diagnosed with BCR::ABL1-positive acute lymphoblastic leukemia (Ph+ ALL).
Materials and methods
Patient cohorts
The total cohort of 193 patients diagnosed with chronic myeloid leukemia in chronic phase, classified according to European Leukemia Net (ELN) criteria [3]. Patients were treated at the Institute of Hematology and Blood Transfusion and University Hospital in Motol in Prague, Czech Republic. Detailed clinical information is given in Table 1. Despite the NCCN-recommended age definition for AYA cancer patients, we categorized patients based on treatment practices for CML and Ph+ ALL in the Czech Republic. Patients aged 0–17 years are treated in pediatric clinics following pediatric protocols, while those aged 18 and older are treated in hematology centers according to adult protocols. It is common practice that children treated under pediatric protocols transition to adult hematology centers upon reaching 18 years of age, where they continue therapy according to adult guidelines. Therefore, reflecting standard treatment practices in the Czech Republic, patients were divided into three groups based on their age at diagnosis: children (0–17 years), adolescent and young adults (AYAs) (18–39 years), and adults (>40 years). In alignment with the revised adolescent age definition proposed by Sawyer et al. [20], which considers individuals aged 10–24 years as adolescents, the AYA cohort in our study includes adolescence patients aged 18–24 years who were treated with adult protocols. The CML cohort consisted of 16 children (median 12 years; range 2–17 years), 80 AYAs (median 33 years; range 19–39 years), and 97 adults (median 58 years; range 40–79 years). Ph+ ALL cohort comprised 30 children, 15 AYAs, and 36 adult patients with median age 10 (range 2–17 years), 33 years (range 18–39 years), 56 years (range 40–77 years), respectively. All patients or their guardians provided written informed consent. The study was approved by the institutional ethical committee and performed in accordance with the Declaration of Helsinki.
Primary cell isolation
Total leukocytes were isolated from peripheral blood (PB) or bone marrow (BM). Peripheral blood mononuclear cells (PMNCs) were isolated using Lymphoprep density gradient centrifugation (STEMCELL Technologies, Vancouver, Canada) according to the manufacturer´s recommendations.
Mutation detection in BCR::ABL1 kinase domain
BCR::ABL1 kinase domain (BCR::ABL1 KD) amplicon libraries were prepared using the Nextera XT DNA Library Prep Kit (Cat. No. FC-131-1096, Illumina, San Diego, CA, USA) as previously reported [21]. Data processing, error filtering, and mutation calling at significant levels were performed using the NextGENe software (Softgenetics, State College, PA, USA) and the in-house bioinformatic tool NextDom [21].
NGS panel sequencing
DNA for NGS panel sequencing was isolated from PB/BM using MagCore (RBC Bioscience, New Taipei City, Taiwan) or from TRIzol/ITG lysates by phenol-chloroform extraction. The custom panel sequencing of 22 whole genes and the selected exons of additional 40 genes (Roche, Basel, Switzerland) frequently mutated in myeloid and lymphoid malignancies (Supplementary Table S1) was used for the detection of somatic mutations. The library was prepared using KAPA HyperPlus (Roche) according to the protocol of manufacturer and sequenced 2×150-bp on the MiSeq instrument (Illumina, San Diego, CA, USA). Data were evaluated using the NextGENe software (Softgenetics). The clinical relevance of the detected variants with minimal coverage 500× and variant allele frequencies (VAF) > 5% was evaluated using VarSome [22]. The somatic origin of mutations, where the VAF did not correspond to the level of BCR::ABL1, was confirmed using genomic DNA from buccal swabs.
Response and clinical outcomes
Total RNA was isolated from PB/BM total leukocytes using standard procedures. BCR::ABL1 transcript levels were quantified using RT-qPCR and expressed on the International Scale (IS) [23]. Response definitions and CML phases classifications followed ELN criteria [3]. The probability of progression-free survival (PFS) was estimated from the start of TKI treatment to the date of progression defined as TKI treatment failure, the presence of high-risk additional chromosomal abnormalities, BCR::ABL1 KD mutations, or CML-related death.
Colony forming assays
Clonogenic assays were conducted using CML progenitor CD34+ or peripheral blood mononuclear cells (PBMCs) from patients with ASXL1 mutation detected at diagnosis (N = 4). Mononuclear cells were isolated using Lymphoprep separation and CD34+ cells were purified by immunomagnetic beads (CD34 MicroBead Kit Human, 130-097-047; Miltenyi Biotec, Bergish Gladbach, Germany). PBMCs were from healthy donor served as a control. CD34+ (1 × 103) or PBMCs (2 × 105) were seeded into methylcellulose MethoCultTM H4435 medium (STEMCELL Technologies, Vancouver, Canada). Samples were analyzed in duplicate, and colonies were enumerated and characterized after 14 days. Colony counts were compared to reference progenitor cell colony frequencies in MethoCultTM of healthy donors, as reported by the manufacturer.
Statistical analysis
Baseline characteristics and hematological parameters were compared using Fisher´s exact test, Pearson´s Chi-squared or the Kruskal–Wallis tests. PFS was estimated by the Kaplan–Meier method and compared by log-rank test. Hazard ratio (HR) with a 95% confidence interval (CI) was calculated for risk factors using Cox proportional hazard regression models. The cumulative incidences of BCR::ABL1 KD mutations were estimated using the cumulative incidence method. Univariate and multivariate analyses were performed to evaluate associations between patient characteristics and survival outcomes. Colony forming assays were evaluated using Student´s t-test. A statistical significance level of p = 0.05 was applied throughout all the experiments. All statistical analyses were performed using R 4.3.1.
Results
Frequency and spectrum of mutations in each age group of CML-CP and Ph+ ALL patients
To characterize the spectrum of somatic mutations in detail and to clarify the mutation landscape in AYA (N = 80) patients with CML-CP, we compared them with adults (N = 97), and pediatric patients (N = 16). All 193 CML patients (Table 1; Supplementary Table S2) in this study were diagnosed with chronic phase and did not progress to the blast phase during TKI treatment.
We observed that AYAs had a significantly higher white blood count (p = 0.019) and number of platelets (p = 0.007) compared to adults (Table 1), and even when we included children (both p < 0.025) (Supplementary Table S2). Furthermore, AYAs had a significantly larger spleen size compared to adult CML patients (p = 0.016), however, no significant difference in the percentage of blasts was observed between the two age groups (p = 0.078).
Among the AYAs, 76.3% (61/80) patients were treated with imatinib as the first-line therapy, while 23.8% (19/80) patients received nilotinib. In the adult group, 96.9% (94/97) patients were treated with imatinib, and 3.1% (3/97) patients were treated with nilotinib. In the pediatric cohort, all patients received imatinib as first-line treatment and 56.3% (9/16) of pediatric patients underwent hematopoietic cell transplantation. None of the patients were pretreated with interferon alpha.
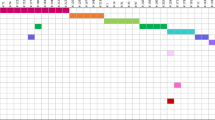
In total, 42 somatic mutations were identified in CML at diagnosis with a median VAF 32.2% (range 5.0–96.9) across 13 CRGs. These included 16 frameshift, 13 nonsense, 11 missense, and 2 start loss mutations (Supplementary Table S3). Somatic mutations were identified in 25% (20/80) of AYA CML patients, 19.6% (19/97) of adult patients, and 12.5% (2/16) of pediatric patients (Fig. 1A). The highest frequency of mutations was found also in Ph+ ALL AYAs (53.3%; 8/15) followed by adults (38.9%; 14/36) and children (26.7%; 8/30) (Fig. 1B).
The frequency of patients with mutations according to age and disease (A) CML and (B) Ph+ ALL. Patients were divided into subgroups based on age at diagnosis: children (0–17 years), AYA (18–39 years), and adults (>40 years). Spectrum of somatic mutations in (C) CML and (D) Ph+ ALL patients according to age subgroups. The total number of mutations identified is shown in tables.
Among the 13 CRGs mutated in CML, ASXL1 emerged as the most frequently mutated gene in CML, with mutations observed in 2 pediatric CML patients, 13 AYA patients, and 8 adult patients (Fig. 1C). Three recurrent mutations in ASXL1 were identified: c.1934dup G646Wfs*12, c.2077C>T R693*, and c.1773C>G Y591* affecting N = 8, 3, and 2 patients, respectively. All frameshift mutations led to premature stop codons with subsequent loss of the c-terminal plant-homeo-domain. Notably, only one AYA patient harbored two somatic CRG mutations. Epigenetic modifiers ASXL1, DNMT3A, and TET2 were mutated in 18.8% (15/80) AYAs and 14.4% (14/97) of adult patients with median VAFs 31.5% (range 5.4–46.5) and 32.2% (range 5.0–48.0), respectively. No mutation in BCR::ABL1 KD was detected in CML patients across all age groups at the time of diagnosis.
Overall, 35 somatic mutations were identified in Ph+ ALL patients with a median VAF of 44.5% (range 11.2–82.5) across 16 CRGs (Supplementary Table S3). Mutations in RUNX1 were the most common events in both Ph+ ALL children (N = 3) and AYAs (N = 4), while mutated IKZF1 in the adults (N = 4) (Fig. 1D). Mutation RUNX1 c.602G>A R201Q was recurrently identified in two patients. Five patients were found to have two distinct somatic mutations at diagnosis. In contrast to CML patients with no BCR::ABL1 KD mutation at diagnosis, two Ph+ ALL patients harbored BCR::ABL1 KD mutations at the time of diagnosis.
Frequency of CML patients with mutations in relation to TKI response
We next analyzed 177 paired samples from 80 AYA and 97 adult CML patients collected during TKI treatment, based on sample availability. At the time of follow-up sample analysis, patients were divided into TKI responders and non-responders according to ELN criteria [3] and analyzed for CRG mutations; AYA optimal responders median time 14 months since TKI start (6–87 months), warning signs median 36 months (10–164 months), therapy failure median 36 months (5–177 months); adult optimal responders median time 15 months since TKI start (6–31 months), warning median 13 months (12–52 months), failure median 24 months (5–167 months). Additionally, all the paired samples from the time of non-optimal TKI response (warning and failure) were analyzed for BCR::ABL1 KD mutations.
Overall, the frequency of CML patients with CRG mutations, regardless of TKI response and age, was 22% (39/177) at diagnosis and 25.4% (45/177) at TKI follow-up (Supplementary Table S4). Contrary to samples at the time of diagnosis, a significantly higher prevalence of CRG mutations was found in adults 32.0% (31/97) compared to AYA patients 17.5% (14/80) in TKI follow-up (p = 0.04). All the detected mutations are listed in Supplementary Table S3. Adult patients developed significantly more de novo mutations (both in BCR::ABL1 KD and other CRG) during treatment (27.8%) compared to AYA patients (12.5%) (p = 0.02).
At diagnosis, CRG mutations in optimal responders were slightly more frequently observed in AYAs (17.1%; 7/41) than in adult patients (12.5%; 6/48; p = 0.56). All 13 mutations identified in responders from both age groups except those in EZH2 c.2T>C M1T and DNMT3A c.1609T>C C537R, disappeared during the TKI treatment or were observed at low VAF corresponding to the residual level of BCR::ABL1 transcript. De novo mutations, namely ASXL1 c.1934dup G646Wfs*12, TET2 c.2429del Q810Rfs*3, and DNMT3A c.1591G>A D531N, were found only in adult responders (Supplementary Table S3).
In diagnostic samples of TKI non-responders, somatic mutations were detected in 9 different CRGs (Fig. 2A). All 7 ASXL1 mutations detected in adults at diagnosis and 3/4 in AYAs persisted during TKI treatment and were detectable at TKI failure (Fig. 2B, C). While mutations in ASXL1 most often appeared at diagnosis, mutations in BCR::ABL1 KD were the most common genetic alterations acquired during the therapy (Fig. 2D). The frequency of de novo BCR::ABL1 KD mutations was higher in adult patients (35.6%) compared to AYAs (24.0%). The treatment failure was also associated with the occurrence of de novo mutations in ASXL1, TET2, and RUNX1 in both age groups. Most failures in AYA and adult patients were at the time of follow-up sample analysis treated with imatinib 1st-line (Supplementary Table S5).
Impact of somatic mutations on outcomes of CML-CP patients
We evaluated the impact of somatic mutations detected in CRGs at diagnosis (20/80 AYA and 19/97 adult patients) and TKI follow-up (14/80 AYA and 31/97 adult patients) on progression-free survival (PFS) of CML patients. The presence of any mutation at diagnosis significantly reduced the probability of PFS compared to patients with no mutation both in AYA (p = 0.031; HR = 2.7; CI 1.09–6.66) and adult (p = 0.003; HR = 2.97; CI 1.46–6.04) CML patients (Fig. 3A, B). ASXL1 mutations identified at diagnosis were associated with inferior PFS compared to patients with no mutation in both age groups, AYA (p = 0.094; HR = 2.5; CI 0.86–7.33) and adult (p = 0.009; HR = 3.21; CI 1.34–7.67) patients (Fig. 3C, D). The most common reason of therapy failure in AYAs was BCR::ABL1 transcript level >1% at any time after 12 months of TKI treatment (8/80; 10%) and in adult patients the BCR::ABL1 KD mutation acquisition (12/97; 12%).
PFS of (A) AYA and (B) adult CML patients with any mutation identified at diagnosis compared to patients with no mutation. Effect of ASXL1 mutations observed at diagnosis on PFS in (C) AYA and (D) adult patients. Hazard R (95% CI) derived from Cox proportional hazard regression models and the p-value calculated by the Log-rank test are shown. The number of patients at risk is shown in tables below. Allmut—patients with any mutation at diagnosis; wt - patients with no mutation during the whole TKI follow-up.
Univariate analysis further revealed that high prognostic scores (SOKAL, EUTOS, ELTS) were predictive of poor outcomes in adult patients but not in AYA patients (Table 2). ELTS and EUTOS scores were highly significant in the adults p < 0.001; HR = 7; CI 3.29–14.89 and p = 0.001; HR = 3.4, CI 1.66–6.98, respectively. In AYAs, the treatment with nilotinib significantly reduced the risk of progression (p = 0.05; HR = 0.23; CI 0.05–0.98). De novo CRG mutations significantly worsened the PFS in AYA (p = 0.002; HR = 6.1, CI 1.98–18.75), while they showed a trend toward increased risk in adult patients, though not statistically significant (p = 0.07; HR = 2.04, CI 0.95–4.36).
Impact of ASXL1 mutations on cumulative incidence of BCR::ABL1 kinase domain mutations during follow-up on TKI treatment
Cumulative incidence of mutations in BCR::ABL1 KD acquired during TKI treatment was significantly higher in adult patients with ASXL1 mutation at the time of diagnosis compared to adult patients with no mutation at diagnosis (p < 0.001) (Fig. 4). Five of six adult patients with ASXL1 mutation at diagnosis that acquired BCR::ABL1 KD mutation were treated with imatinib. Contrary to adults, only one AYA patient (Patient #13) with nonsense mutation ASXL1 E773* at diagnosis developed de novo mutations in BCR::ABL1 KD (F317L and M351T) (Supplementary Table S3).
Impact of ASXL1 mutations on clonogenicity
Next, we assessed the clonogenic potential of CD34+ cells and PBMCs from three patients with ASXL1 mutations, from whom the cells were available and vital (Supplementary Table S6). Blood count results showed reduced or minimal erythropoiesis at the time of diagnosis and anemia or mild anemia in Pt 2 and Pt 3 (Supplementary Table S7). Impaired erythropoiesis was observed in CD34+ cells, evidenced by a decrease in CFU-GM (Pt 1) of erythroid progenitor colonies (Supplementary Fig. S1, Panel A). In patients 2 and 3, PBMCs were available only for the clonogenicity analysis, which is not ideal sample as isolated CD34 + . However, impaired erythropoiesis was noted in PBMCs from a patient with the ASXL1 E877 frameshift mutation (Pt 3), as indicated by a decrease in BFU-E (p < 0.001), CFU-E (p < 0.001), and CFU-GEMM numbers (p < 0.01) (Supplementary Fig. S1, Panel B).
Additionally, we analyzed the blood counts of all AYA patients (N = 11) and all adults (N = 10) with the ASXL1 mutation (Supplementary Table S8). For comparison, we randomly selected 28 AYAs and 28 adults from the studied cohorts without ASXL1 mutations and evaluated their blood counts. Patients with the ASXL1 mutation (n = 20) exhibited a significantly higher platelet count compared to those without the mutation (N = 56) (p < 0.001). This difference remained statistically significant when analyzed within age groups (AYA patients with ASXL1 mutation vs. non-mutated ASXL1: p = 0.02; adults with ASXL1 mutation vs. non-mutated ASXL1: p = 0.016). As mentioned above, a higher platelet count was observed in AYA patients compared to adults. Moreover, an even higher platelet level was noted in AYA patients with ASXL1 mutations.
Discussion
This work focused on AYA CML-CP patients, whose outcome on TKI therapy has been previously reported as worse compared to adult patients [24]. The CML-CP cohort consisted of 80 AYAs, 97 adults and 16 pediatric patients. At diagnosis, AYAs exhibited significantly larger spleen sizes and higher levels of white blood cells and platelets compared to adult patients. This is consistent with studies reporting that younger CML patients often present more risk factors compared to older patients [10, 11]. There were also differences in baseline characteristics and treatment regimens; a greater proportion of AYA patients received the second-generation TKI nilotinib as a first-line treatment compared to adult patients, aligning with the observations of Castagnetti et al. [11], who noted age-based variations in TKI usage.
Altogether, 42 somatic mutations in 13 CRGs were identified, with a higher mutation frequency in AYA CML patients (25.0%) compared to adults (19.6%) and pediatric (12.5%) patients treated in real-clinical practice. Additionally, among Ph+ ALL patients, AYA individuals were diagnosed with CRG mutations more frequently (53.3%) than children (26.7%) and adult patients (38.9%). The elevated mutational burden in AYAs in both diseases is notable. The landscape of mutated genes at diagnosis differed between CML-CP and Ph+ ALL patients. Among 193 CML-CP patients, the most frequently mutated genes were ASXL1, DNMT3A, and TET2, which is consistent with recent studies [14, 15, 25]. In contrast, the most frequently mutated genes in 81 Ph+ ALL patients were RUNX1, IKZF1, and BCR::ABL1 KD. However, Feng et al. [26]. reported these mutations in Ph+ ALL patients but with lower frequency compared to mutations in genes involved in transcriptional regulation and epigenetic modulation, namely FAT1, CRLF2, SF1, EP300, and CREBBP (all these genes are included in our panel except for FAT1).
ASXL1 was the most frequently mutated gene at diagnosis across pediatric (2/16; 13%), AYA (12/80; 15%), and adult (10/97; 10%) CML patients. Our findings align with those of Ernst et al. [19], who reported a higher prevalence of ASXL1 mutations in young patients (29%) compared to adult CML-CP patients (7–13%). Similarly, ASXL1 was the most frequently mutated gene in pediatric CML patients (6/90; 6.7%) [27]. Notably, ASXL1 mutations were significantly associated with an increased cumulative incidence of BCR::ABL1 KD mutations during TKI therapy in adult CML patients, whereas this association was not observed in AYAs. Likewise, Guerineau et al. [28] demonstrated on a cohort of CML patients that was not divided into age groups that the presence of mutations in epigenetic genes at diagnosis was linked to a higher cumulative incidence of BCR::ABL1 KD mutations (p = 0.015). These findings suggest that mutations in epigenetic modulators may promote additional genetic events, such as BCR::ABL1 KD mutations, contributing to therapeutic failure. CML patients with significantly lower probability of PFS were those who carried mutated ASXL1 in both AYAs and adult patients in comparison with patients without mutations supporting the assumption that ASXL1 is the CML-related oncogene [13]. Furthermore, ASXL1 mutations may contribute to impaired erythropoiesis, as suggested by blood count abnormalities and reduced colony formation from erythroid progenitors, which is in line with findings from previous studies [29, 30]. Although several studies [10, 11, 31] have reported the elevated platelet counts in younger CML patients, very little is known about the association of increased platelet counts and mutations in ASXL1. Behrens et al. [27] has reported that pediatric CML patients harboring pathogenic ASXL1 mutations at diagnosis exhibited higher counts of leukocytes and platelets compared to patients without any mutation or other mutation than ASXL1, which may be a potential consequence of the relative increase in proliferative capacity in the study cohort. The elevated level of platelets in patients with ASXL1 mutation compared to patients without mutation has also been reported in adult CML patients, but not statistically significant [32].
Although CRG mutations were detected at diagnosis of CML at a lower frequency, their presence correlated with reduced PFS and enhanced the level of significance. Together, these findings support emerging evidence that mutations in CRGs detected at the time of diagnosis in CML-CP patients represent risk factors for disease progression. Based on BCR::ABL1 transcript kinetics and variant allele frequency (VAF) of mutations in CRGs, it is presumed that these mutations are present in CML cells, which is in line with previous works [19, 25].
BCR::ABL1 was the most frequent gene with mutation acquisition during TKI therapy with a markedly higher prevalence in adult patients, suggesting age-related susceptibility to additional mutations under TKI treatment pressure. This pattern aligns with Kim et al. [25], who reported higher rates of new mutations in older CML patients during TKI therapy. ASXL1 was the second most frequently mutated gene on TKI therapy, albeit at a much lower frequency than BCR::ABL1.
Univariate analysis revealed that high SOKAL, EUTOS and ELTS scores along with ASXL1 mutations were significantly associated with reduced PFS in adult patients. This pattern was not observed in AYAs, where nilotinib therapy showed significant association with PFS. Specifically, nilotinib was administered to 50% (6/12) of AYA patients with ASXL1 mutations, highlighting that more potent TKIs than imatinib, when used as first-line therapy in patients with ASXL1 mutations, may improve PFS.
As this study is based on real-world data, this hypothesis requires validation in larger cohorts of patients treated with higher-generation TKIs as a first-line approach. Conversely, previous work based on clinical trial data indicated that patients with ASXL1 mutations had inferior probability to achieve MMR on nilotinib as first-line therapy [13]. However, this study did not compare outcomes in patients treated with imatinib to evaluate the MMR rates in patients with ASXL1 mutations.
We acknowledge certain limitations of our study. First, the cohort of pediatric CML patients is relatively small, as CML is rare in this population. Consequently, statistical conclusions cannot be drawn from this subgroup alone. However, the inclusion of pediatric patients was primarily intended to provide a comprehensive overview of mutation spectra across all age groups for comparative purposes. Our analyses focused predominantly on AYA and adult patients, particularly those who were not initially referred for alloHSCT. Despite the low prevalence of CML in children and the rarity of somatic mutations in CRGs at diagnosis, we successfully characterized the spectrum of somatic mutations across all age categories.
Second, while our findings suggest that first-line treatment with second- or third-generation TKIs may lead to better outcomes in patients carrying ASXL1 mutations compared to those treated with imatinib as a first-line therapy, further validation through clinical studies is required. Additionally, the observed impact of ASXL1 mutations on impaired erythropoiesis should be investigated in a larger cohort, specifically comparing patients with ASXL1 mutations to those without CRG mutations.
In conclusion, this comparative study on mutation frequency and mutational landscapes in AYA, pediatric, and adult patients with CML-CP and Ph+ ALL revealed that CRG mutations were more frequently detected in AYA patients at the time of diagnosis. However, our findings did not support the initial hypothesis that AYA CML-CP patients might carry oncogenic mutations commonly observed in Ph+ ALL. This study demonstrated that mutations in CRGs in CML-CP patients (both AYA and adults) represent a risk factor for disease progression during TKI therapy. In general, CML-CP patients who responded optimally to TKI therapy exhibited lower mutation rates at both diagnosis and follow-up, particularly among AYA patients treated with nilotinib. Patients who did not respond to TKI therapy (treatment failures) exhibited higher mutation rates both at diagnosis and during follow-up. Nevertheless, adult patients generally showed higher mutation rates at follow-up, irrespective of response, suggesting a potential age-related factor. ASXL1 mutations and other CRG mutations serve as risk factors for progression during TKI therapy in both AYA and adult CML-CP patients. Although overall, AYA do not seem to have a worse prognosis than others, despite having more mutations. Using higher generations of TKIs at diagnosis that effectively target CML cells with ASXL1 mutations and possibly other CRGs could potentially reduce disease progression risk.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cortes JE, Jones D, O’Brien S, Jabbour E, Ravandi F, Koller C, et al. Results of dasatinib therapy in patients with early chronic-phase chronic myeloid leukemia. J Clin Oncol. 2010;28:389–404.
Saglio G, Kim D-W, Issaragrisil S, le Coutre P, Etienne G, Lobo C, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362:2251–9.
Hochhaus A, Baccarani M, Silver RT, Schiffer C, Apperley JF, Cervantes F, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34:966–84.
Jabbour E, Kantarjian HM, O’Brien S, Shan J, Quintás-Cardama A, Garcia-Manero G, et al. Front-line therapy with second-generation tyrosine kinase inhibitors in patients with early chronic phase chronic myeloid leukemia: what is the optimal response?. J Clin Oncol. 2011;29:4260–5.
National Cancer Institute SEER USA. SEER USA. https://seer.cancer.gov/statfacts/html/cmyl.html. Accessed 18 Dec 2024.
Cancer Research UK. Cancer Research UK. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/leukaemia-cml/incidence#heading-One. Accessed 18 Dec 2024.
Cortes J, Talpaz M, O’Brien S, Giles F, Rios MB, Shan J, et al. Effects of age on prognosis with imatinib mesylate therapy for patients with Philadelphia chromosome-positive chronic myelogenous leukemia. Cancer. 2003;98:1105–13.
Hasford J, Pfirrmann M, Hehlmann R, Allan NC, Baccarani M, Kluin-Nelemans JC, et al. A new prognostic score for survival of patients with chronic myeloid leukemia treated with interferon Alfa Writing Committee for the Collaborative CML Prognostic Factors Project Group. JNCI. 1998;90:850–9.
Sokal JE, Cox EB, Baccarani M, Tura S, Gomez GA, Robertson JE, et al. Prognostic discrimination in ‘good-risk’ chronic granulocytic leukemia. Blood. 1984;63:789–99.
Kalmanti L, Saussele S, Lauseker M, Proetel U, Müller MC, Hanfstein B, et al. Younger patients with chronic myeloid leukemia do well in spite of poor prognostic indicators: results from the randomized CML study IV. Ann Hematol. 2014;93:71–80.
Castagnetti F, Gugliotta G, Baccarani M, Breccia M, Specchia G, Levato L, et al. Differences among young adults, adults and elderly chronic myeloid leukemia patients. Ann Oncol. 2015;26:185–92.
Schmidt M, Rinke J, Schäfer V, Schnittger S, Kohlmann A, Obstfelder E, et al. Molecular-defined clonal evolution in patients with chronic myeloid leukemia independent of the BCR-ABL status. Leukemia. 2014;28:2292–9.
Schönfeld L, Rinke J, Hinze A, Nagel SN, Schäfer V, Schenk T, et al. ASXL1 mutations predict inferior molecular response to nilotinib treatment in chronic myeloid leukemia. Leukemia. 2022;36:2242–9.
Branford S, Kim DDH, Apperley JF, Eide CA, Mustjoki S, Ong ST, et al. Laying the foundation for genomically-based risk assessment in chronic myeloid leukemia. Leukemia. 2019;33:1835–50.
Shanmuganathan N, Wadham C, Shahrin N, Feng J, Thomson D, Wang P, et al. Impact of additional genetic abnormalities at diagnosis of chronic myeloid leukemia for first-line imatinib-treated patients receiving proactive treatment intervention. Haematologica. 2023. https://doi.org/10.3324/haematol.2022.282184.
Adnan Awad S, Kankainen M, Ojala T, Koskenvesa P, Eldfors S, Ghimire B, et al. Mutation accumulation in cancer genes relates to nonoptimal outcome in chronic myeloid leukemia. Blood Adv. 2020;4:546–59.
Midic D, Rinke J, Perner F, Müller V, Hinze A, Pester F, et al. Prevalence and dynamics of clonal hematopoiesis caused by leukemia-associated mutations in elderly individuals without hematologic disorders. Leukemia. 2020;34:2198–205.
Branford S, Wadham C, Shanmuganathan N, Fernandes A, Shahrin NH, Feng J, et al. Age-related clonal hematopoiesis mutations detected at the time of stopping tyrosine kinase inhibitor therapy predict the achievement of treatment-free remission for patients with CML. Blood. 2023;142:447–447.
Ernst T, Busch M, Rinke J, Ernst J, Haferlach C, Beck JF, et al. Frequent ASXL1 mutations in children and young adults with chronic myeloid leukemia. Leukemia. 2018;32:2046–9.
Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2:223–8.
Benesova A, De Santis S, Polivkova V, Pecherkova P, Krizkova J, Suchankova P, et al. Unstable major molecular response as a trigger for next generation sequencing-based BCR::ABL1 mutation testing in chronic myeloid leukemia. Am J Hematol. 2024;99:759–62.
Kopanos C, Tsiolkas V, Kouris A, Chapple CE, Albarca Aguilera M, Meyer R, et al. VarSome: the human genomic variant search engine. Bioinformatics. 2019;35:1978–80.
Cross NCP, White HE, Müller MC, Saglio G, Hochhaus A. Standardized definitions of molecular response in chronic myeloid leukemia. Leukemia. 2012;26:2172–5.
Pemmaraju N, Kantarjian H, Shan J, Jabbour E, Quintas-Cardama A, Verstovsek S, et al. Analysis of outcomes in adolescents and young adults with chronic myelogenous leukemia treated with upfront tyrosine kinase inhibitor therapy. Haematologica. 2012;97:1029–35.
Kim T, Tyndel MS, Kim HJ, Ahn J-S, Choi SH, Park HJ, et al. Spectrum of somatic mutation dynamics in chronic myeloid leukemia following tyrosine kinase inhibitor therapy. Blood. 2017;129:38–47.
Feng J, Li Y, Jia Y, Fang Q, Gong X, Dong X, et al. Spectrum of somatic mutations detected by targeted next-generation sequencing and their prognostic significance in adult patients with acute lymphoblastic leukemia. J Hematol Oncol. 2017;10:61.
Behrens YL, Gaschler L, Nienhold R, Reinkens T, Schirmer E, Knöß S, et al. Somatic variant profiling in chronic phase pediatric chronic myeloid leukemia. Haematologica. 2023. https://doi.org/10.3324/haematol.2023.283800.
Guerineau H, Cayuela J, Dulucq S, Tran Quang V, Tarfi S, Gricourt G, et al. Mutation of epigenetic regulators at diagnosis is an independent predictor of tyrosine kinase inhibitor treatment failure in chronic myeloid leukemia: a report from the RESIDIAG study. Am J Hematol. 2024. https://doi.org/10.1002/ajh.27553.
Shi H, Yamamoto S, Sheng M, Bai J, Zhang P, Chen R, et al. ASXL1 plays an important role in erythropoiesis. Sci Rep. 2016;6:28789.
Yamamoto S, Shi H, Chen S, Zhang P, Zhou Y, Xu M, et al. ASXL1 Is a key regulator for erythroid development and Asxl1 loss impairs erythropoiesis in vivo. Blood. 2015;126:3644–3644.
Gurrea Salas D, Glauche I, Tauer JT, Thiede C, Suttorp M. Can prognostic scoring systems for chronic myeloid leukemia as established in adults be applied to pediatric patients?. Ann Hematol. 2015;94:1363–71.
Bidikian A, Kantarjian H, Jabbour E, Short NJ, Patel K, Ravandi F, et al. Prognostic impact of ASXL1 mutations in chronic phase chronic myeloid leukemia. Blood Cancer J. 2022;12:144.
Acknowledgements
This work was supported by MHCZ NU21-07-00225, DRO (IHBT, 00023736) and European Treatment and Outcome Study for CML (EUTOS for CML). Samples collection was supported by grant no. LM2023033 (BBMRI.cz). Computational resources were provided by the e-INFRA CZ project (ID:90254), supported by the Ministry of Education, Youth and Sports of the Czech Republic.
Funding
Open access publishing supported by the institutions participating in the CzechELib Transformative Agreement.
Author information
Authors and Affiliations
Contributions
JK performed experiments and data analyses and wrote the manuscript; VP, AL, AB, NC, TS performed experiments and data analyses; PS performed bioinformatic and statistical analyses; VV, DM, HK, MMS, DS, CS provided samples and clinical data from the adult patients; MZ, JZ, JT provided samples and patients characteristics; KMP designed the study, supervised the study, interpreted the data, and wrote the manuscript. All authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
KMP—Novartis - advisory board and research support. The remaining authors declare no competing financial interests.
Ethics approval
The project was approved by the local Ethics Review Committee (EK 1/AZV ČR/06/2020).
Informed consent
All patients, as well as the parents of paediatric patients, provided written informed consent for the use of their samples and clinical data in the research project, in accordance with the Declaration of Helsinki and institutional guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Krizkova, J., Polivkova, V., Laznicka, A. et al. Somatic mutations and outcomes in chronic myeloid leukemia adolescent and young adults compared to children, adults, and BCR::ABL1-positive acute lymphoblastic leukemia. Leukemia 39, 1670–1677 (2025). https://doi.org/10.1038/s41375-025-02609-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02609-3