Abstract
Colorectal carcinoma (CRC) with deficient mismatch repair (dMMR) is an etiologically heterogeneous molecular entity. We investigated the genetic profile, focusing on key signaling pathways and molecular diversity of dMMR CRCs. In this study, next-generation sequencing was applied to 156 consecutive dMMR CRCs and 225 randomly selected proficient MMR (pMMR) CRCs diagnosed between July 2015 and December 2019 at Peking Union Medical College Hospital. Genetic alterations and MLH1 promoter hypermethylation (MLH1me+) were analyzed. Among the most frequently mutated genes, RNF43, ARID1A, PIK3CA, ATM, and BRCA2 mutants were enriched in dMMR CRCs, whereas APC and TP53 mutations were enriched in pMMR CRCs. In dMMR group, RNF43, APC, ARID1A, and BRCA2 mutations were largely microsatellite instability events. WNT pathway was commonly altered regardless of MMR status. Compared to pMMR CRCs, dMMR CRCs had remarkably more prevalent PI3K, RTK-RAS, TGFβ, and DNA damage repair pathway alterations and more multiple mutations in WNT and PI3K pathways. Within dMMR tumors, mutual exclusivity occurred between CTNNB1 mutation and APC or RNF43 mutation, while coexistence existed between BRAF and RNF43 mutation, as well as RAS and APC mutation. MLH1me+ dMMR CRCs had significantly more frequent RNF43 mutations but less frequent KRAS, APC, and CTNNB1 mutations comparing to MLH1-unmethylated dMMR CRCs. RNF43/BRAF comutations were detected in MLH1me+ dMMR CRCs, whereas RAS/APC comutations were largely detected in Lynch syndrome-associated cases. RNF43 mutation was independently associated with MLH1me+ rather than BRAF mutations. dMMR CRCs bearing receptor tyrosine kinase fusion demonstrated no additional RTK-RAS mutations, significantly fewer PI3K alterations and more TGFBR2 mutations than other dMMR tumors. Our study revealed that dMMR CRCs had distinctive gene mutation spectra and signaling pathway interaction patterns compared to proficient mismatch repair (pMMR) CRCs, and molecular heterogeneity was evident for these divergent oncogenic pathways. These findings justify the use of individualized therapy targeted to dMMR CRC subgroups.
Similar content being viewed by others
Introduction
Colorectal carcinoma (CRC) is one of the most prevalent malignancies worldwide, ranking as the third and fifth leading cause of cancer-related death in the USA and China [1, 2], respectively. Currently, although AJCC-TNM staging remains the main basis of treatment decision making, it has increasingly been shown to be insufficient for accurate prognosis or reliable personalized therapy.
Recent advancements in high-throughput genomic studies have revealed divergent intrinsic molecular features of CRC, which are of critical prognostic and predictive significance. One of these is deficient DNA mismatch repair (dMMR), leading to a phenotype of high-level microsatellite instability (MSI-H) in ~15% of CRCs [3]. Clinical studies have indicated a more favorable prognosis for patients with stage II/III dMMR CRCs. Most notably, dMMR status is associated with increased tumor mutational and neoantigen burdens, higher density of tumor-infiltrating lymphocytes and immune checkpoint protein compensatory upregulation and has been highlighted as an indication for the application of checkpoint blockade therapy in multiple solid tumors, including CRC [4,5,6]. However, a comprehensive characterization of the cancer-driving genes and signaling pathways that distinguish dMMR has not been thoroughly illustrated. In particular, MMR has been established as a crucial part of the DNA damage response (DDR) system, and the process is composed of a series of distinct yet functionally interwoven pathways that maintain genomic integrity [7]. The complexity and clinical relevance of the interaction between DDR pathways has been elucidated in lung adenocarcinoma [8] and is worthy of further exploration in dMMR CRCs.
Traditionally, three main etiologically distinct subgroups have been identified in dMMR CRCs [9]. The most common one is “sporadic dMMR CRCs,” of which the dMMR status is primarily attributed to epigenetic hypermethylation of the MLH1 promoter region and subsequent transcriptional silencing. Another subgroup consists of “Lynch syndrome-associated dMMR CRCs,” carrying deleterious germline alterations in MMR genes MLH1, MSH2, MSH6, PMS2, or EPCAM. Tumors bearing neither MLH1 hypermethylation nor germline MMR-mutated genes comprise a group of “unexplained dMMR CRCs” and are associated with a variety of possible causes. This molecular categorization has been emphasized for its significance in genetic risk evaluation and management. Nevertheless, the underlying molecular heterogeneity and implications for targeted therapy remain to be clarified. Furthermore, we and others [10,11,12,13] have recently recognized a distinguishable molecular subgroup composed of CRC tumors harboring therapeutically targetable receptor tyrosine kinase (RTK) fusion proteins, which are extremely uncommon but enriched in dMMR CRCs with MLH1 hypermethylation. Although certain molecular features of this subgroup have been previously described, an in-depth understanding awaits thorough study and comparison with other dMMR subgroups.
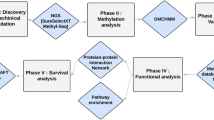
In the present study, we investigated the detailed molecular and genetic features of a consecutive dMMR CRC cohort, including subgroups, by comprehensive genomic profiling (CGP), and the findings are then compared with features of proficient MMR (pMMR) CRCs. We focused on mutations in key genes affecting the WNT, RTK-RAS, PI3K, TGF-β, TP53, and DDR pathways. The mutual relationships of alterations within the same and among different pathways were also explored. Herein, we demonstrate that dMMR CRCs display a characteristic yet remarkably heterozygous gene mutation profile and pathway interaction pattern, which might have important implications for individualized targeted therapy.
Materials and methods
Patient selection
The materials used in this retrospective study were collected from pathology archives of Peking Union Medical College Hospital (PUMCH) and included data of patients diagnosed with CRC between July 2015 and December 2019. All patients with data included in the study underwent partial colectomy for primary CRC. No patients were known to have received neoadjuvant therapy or tyrosine kinase inhibitor therapy. Tumors with intact immunohistochemical (IHC) staining of all four MMR proteins of interest [14] were identified as dMMR tumors. The dMMR group (n = 156) comprised consecutive cases, whereas the pMMR group (n = 225) comprised randomly selected cases. This study was approved upon ceding review by the PUMCH Institutional Review Board for review.
Comprehensive genomic profiling (CGP)
CGP was preformed using hybrid capture-based targeted next-generation sequencing as previously described [15, 16]. In brief, DNA from formalin-fixed paraffin-embedded colorectal tumors and patient-matched normal tissues was extracted and sheared. Barcoded libraries were hybridized to our customized panel of 1021 genes containing whole exons, selected introns of 288 genes, and selected regions of 733 genes (Supplementary Table 1). The libraries were prepared and sequenced to a uniform median depth (>500×). Genomic alterations, including single nucleotide variants, small insertions and deletions, copy number alterations, and gene fusions/rearrangements, were compared against each patient’s corresponding normal sample. MSI status was determined using MSIsensor (v0.2), which reported the percentage of unstable somatic microsatellites through a Chi-square test on predefined microsatellite regions covered by our panel. The loss of heterozygosity (LOH) in MMR genes was determined by an analysis of the variant allele fraction (VAF) using a local algorithm modified based on a previously reported method [14]. LOH was established when (1) the VAF for a mutation was >80% higher than the average VAF for somatic mutations in the tumor and when (2) LOH was verified by shifts in the expected VAFs, which indicate germline polymorphisms within the same gene region. A possible LOH was identified when the VAF of a mutation was between 40 and 80% higher than the average VAF for somatic mutations in the tumor. The average sequencing depth for the target regions of the tumor samples was 1026×, and 99.0% of the average coverage of the targeted regions was more than 200×, which were qualified for variant calling and the MSI analysis.
Key genes and determination of mutational significance
Within our 1021-gene panel, 26 genes involved in the WNT, RTK-RAS, PI3K, TGFβ, and TP53 pathways were recognized as genes with recurring mutations in key CRC signaling pathways, as determined by TCGA analysis [17]. Fifty-six genes has been identified as DDR-related genes in previous studies [18,19,20] and were assigned to eight DDR pathways: MMR, homologous recombination repair (HRR), Fanconi anemia (FA), base excision repair, checkpoint factor, nucleotide excision repair, nonhomologous end joining, and translesion DNA synthesis (Supplementary Table 2).
Mutations of oncogenes were filtered according to the related documentation in the Catalog of Somatic Mutations in Cancer (COSMIC) [21] and OncoKB annotation [22]. For tumor suppressor genes, only “predicted deleterious” mutations were included in our analysis. All loss-of-function mutations, including nonsense mutations, frameshift mutations, and mutations affecting canonical splice sites were defined as “predicted deleterious” mutations. Missense mutations were considered deleterious when identified in two or more of the following in silico functional analysis algorithms: predication score 0.0–0.05 in SIFT (sorting intolerant from tolerant) [23], “possibly damaging” or “probably damaging” in polymorphism phenotyping-2 (Polyphen2) [24], or “medium” or “high” in MutationAssessor [25]. For missense mutations in the DDR pathway, the functional effects were manually reviewed in the COSMIC, recurrent hotspot mutations [26] and PubMed searches, as previously described by Iyer et al. [27] and Teo et al. [28].
MLH1 promoter hypermethylation analysis
All tumors that presented with the loss of MLH1 expression and the lack of MMR germline mutations were analyzed for MLH1 promoter hypermethylation using methylation-specific PCR, with the protocol detailed in our previous report [10].
Statistical methods
Categorical variables were expressed as percentages. Chi-square test or Fisher’s exact test was used when appropriate to compare the frequencies of genetic alterations and to identify the coexistence or mutually exclusive associations. Correlation analysis was conducted using binary logistic regression. Statistical processing was performed using SPSS version 23 (SPSS Inc., Chicago, IL, USA), and P < 0.05 (two-sided) was considered significant.
Results
Gene mutations in the dMMR and pMMR CRCs
Of the key genes involved in WNT, RTK-RAS, PI3K, TGF-β, TP53, and DDR pathways, we found that RNF43 (56.4%), APC (54.5%), ARID1A (48.7%), PIK3CA (48.1%), KRAS (42.3%), TP53 (35.9%), ATM (31.4%), SOX9 (28.2%), TCF7L2 (23.1%), PTEN (23.1%), FAM123B (21.8%), CTNNB1 (20.5%), BRCA2 (20.5%), MLH1 (19.9%), and AXIN2 (17.9%) were the most frequently somatic genes mutated in the dMMR CRCs analyzed (Fig. 1a, Supplementary Table 3), whereas TP53 (83.1%), APC (71.6%), KRAS (45.3%), PIK3CA (15.1%), SOX9 (12.0%), SMAD4 (11.6%), ATM (10.7%), ARID1A (7.6%), FBXW7 (6.2%), NRAS (6.2%), RNF43 (5.8%), PTEN (5.3%), TCF7L2 (4.0%), and BRAF (4.0%) were the genes most frequently mutated in the pMMR CRCs analyzed (Fig. 1b, Supplementary Table 3). In comparison with those in the pMMR CRCs, the mutation rates of the majority of recurrently mutated genes in our analysis were significantly higher in the dMMR group (P < 0.05), while the APC and TP53 mutations were the only genomic alterations significantly enriched in the pMMR CRCs (54.5% vs. 71.6%, P = 0.001; 33.9% vs. 83.1%, P < 0.001). The prevalence of mutations in KRAS, NRAS, SMAD2, SMAD4, and RAD51 did not differ significantly between the dMMR and pMMR groups.
a Prevalence of most frequently mutated genes in the dMMR CRCs compared with that in the pMMR CRCs. b Prevalence of the most frequently mutated genes in the pMMR CRCs compared with that in the dMMR CRCs. c Fraction of MSI-related somatic mutations of the 20 most recurrently mutated tumor suppressor genes in the dMMR CRCs. d Bar chart showing the most commonly detected MSI-related genes in the dMMR CRCs. dMMR deficient mismatch repair, pMMR proficient mismatch repair, CRC colorectal carcinoma, MSI microsatellite instability. Asterisk (*) significant difference in mutation prevalence (Chi-square test or Fisher’s exact test, P < 0.05).
Of the recurrently mutated tumor suppressor genes in the dMMR CRCs, the majority of alterations in RNF43 (87/95, 91.6%), MSH3 (22/28, 78.6%), ARID1A (55/75, 73.3%), SOX9 (30/44, 68.2%), BRCA2 (33/49, 67.3%), APC (54/85, 63.5%), PTEN (34/58, 58.6%), and AXIN2 (17/30, 56.7%) were found to be insertions or deletions affecting homopolymer sequences and were recognized as MSI events (Fig. 1c). Specifically, the most commonly detected MSI-related alterations in the dMMR CRCs were the well-known RNF43 variants: p. G659fs and p. R117fs (Fig. 1d). Somatic mutations affecting PMS2, FBXW7, BRIP1, TP53, PIK3R1, and MLH1 were largely nonsense mutations or missense mutations predicted to be deleterious.
Signaling pathway alterations in the dMMR and pMMR CRCs
DDR-related pathway deficiencies were found to be exceedingly common among the dMMR CRCs, in contrast to the low frequencies in the pMMR CRCs. In addition to the MMR pathway, which was damaged in all the dMMR cases, the HRR and FA pathways were the most commonly mutated DDR pathways, affecting 55.8% (87/156) and 43.6% (68/156) of the dMMR tumors, respectively (Fig. 2a).
(a) Distribution of DNA damage repair pathways (apart frommismatch repair pathway); (b) Distribution of WNT, RTK0RAS, PI3K, TGFβ and TP53 pathways. dMMR deficient mismatch repair, pMMR proficient mismatch repair, CRC colorectal carcinoma, HRR homologous recombination repair, FA Fanconi anemia, BER base excision repair, CPFs checkpoint factors, NER nucleotide excision repair, NHEJ nonhomologous end joining, and TLS translesion synthesis.
Among defects in other key pathways driving CRC carcinogenesis, defects in the WNT signaling pathway were common to both groups, detected in 89.1% of the dMMR cases and 83.1% of the pMMR cases. However, defects in the PI3K (68.6% vs. 19.6%, P < 0.001), RTK-RAS (69.2% vs. 54.2%, P = 0.004), and TGFβ (32.7% vs. 14.2%, P = 0.001) pathways were significantly enriched in the dMMR CRCs compared with their frequencies in the pMMR CRCs, and aberrations in the TP53 pathway (55.8% vs. 85.3%, P < 0.001) were significantly more frequent in the latter cases (Fig. 2b).
Mutual relationships among key genes in the dMMR and pMMR CRCs
Compared to those in the pMMR CRCs, genes in the WNT (83.3% vs. 40.4%, P < 0.001) and PI3K (23.7% vs. 4.4%, P < 0.001) pathways in the dMMR CRCs were more likely to harbor two or more mutations. Specifically, of the mutations in the key genes in the WNT pathway, CTNNB1 mutations were always mutually exclusive of APC and RNF43 mutations (Fig. 3a), while AXIN2 mutations were often incompatible with APC mutations but coexisted with RNF43 mutations. PIK3CA and PIK3R1, two key components of the PI3K pathway, displayed neither a significant coexistent nor incompatible relationship. The majority of mutations of genes within the RTK-RAS and TGFβ pathways exhibited mutually exclusive patterns. Notably, all eight dMMR tumors bearing two or more RTK-RAS pathway alterations had a BRAF V600E or KRAS/NRAS-activating mutation and an additional oncogenic ERBB3 mutation (G284R or V104M).
(a) Mutation profile of key WNT and RTK-RAS pathway genes in the dMMR CRCs with MLH1 hypermethylation. Columns present individual cases of dMMR CRCs with MLH1 hypermethylation. APC, CTNNB1, RNF43, KRAS/NRAS and BRAF mutations are listed in rows. (b) Mutual relationships of key WNT and RTK-RAS pathway genes in the dMMR CRCs with MLH1 hypermethylation.
We further analyzed the coordination among key genes involved in WNT and RTK-RAS signaling, the two pathways with the most frequently mutated genes in CRCs. Among the dMMR CRCs, 19 of 22 (86.4%) BRAF mutations were carried concurrently with an RNF43 mutation, while 46 of 68 (67.6%) KRAS/NRAS mutations were carried concurrently with an APC mutation (Fig. 3a). A statistically significant coexistence relationship between BRAF and RNF43 mutations (P = 0.016) and between KRAS/NRAS and APC mutations (P = 0.006) was observed. However, neither the BRAF and APC mutations (P = 0.002) nor the KRAS/NRAS and RNF43 mutations (P = 0.001) exhibited mutually exclusive patterns. The mutual relationship between CTNNB1, APC, RNF43, KRAS/NRAS, and BRAF mutations in the dMMR group is illustrated in Fig. 3b. The RNF43 mutation was very uncommon in the pMMR group (13/225, 5.8%) and detected in two of nine (22.2%) BRAF mutant pMMR cases. There was a tendency for RNF43 and BRAF mutations to coexist in the pMMR CRCs, but a level of significance was not reached (P = 0.088, Fisher’s exact test).
Mutual relationships between signaling pathways in the dMMR and pMMR CRCs
The mutual relationships of the WNT, RTK-RAS, PI3K, TGF-β, and TP53 pathways are shown in Fig. 4, displaying remarkable differences between the dMMR and pMMR CRCs. Among the dMMR tumors, all the WNT pathway gene aberrations co-occurred with defects in other cancer-driving signaling pathways, including RTK-RAS (P = 0.008), TGFβ (P = 0.013), and PI3K (P = 0.043). In addition, the TGFβ pathway was generally altered concurrently with TP53 pathway alterations (P = 0.024). However, pMMR tumors showed co-alterations in the PI3K and RTK-RAS pathways (P = 0.038) and the PI3K and TGFβ pathways (P = 0.006). No mutually exclusive pattern was observed for the dMMR group genes, whereas TP53 pathway deficiency genes were not compatible with RTK-RAS (P = 0.002) or TGFβ (P = 0.012) pathway alterations in the pMMR group.
Mutation profile of the dMMR CRCs with MLH1 hypermethylation
The 156 dMMR CRC tumors were categorized into four groups: the Lynch syndrome-associated group consisted of 57 tumors harboring pathogenic/likely pathogenic germline mutations in one of the four MMR genes or combined EPCAM-MSH2 deletions (57/156, 36%); the MLH1-hypermethylated group (MLH1me+ group) consisted of 67 dMMR cases with lost MLH1/PMS2 expression and MLH1 promoter hypermethylation but no MLH1 germline mutation (67/156, 43%), and this group was further divided into the “MLH1me+ with fusion” (n = 15) subgroup and the “MLH1me+ without fusion” (n = 52) subgroup according to the presence or absence of oncogenic RTK gene rearrangements; and the Lynch-like group consisted of the remaining patients with neither MMR gene germline mutations nor MLH1 promoter hypermethylation (32/156, 21%) (Supplementary Fig. 1). As detailed in Fig. 5 and summarized in Fig. 6, apart from the enrichment of the BRAF V600E mutation (38.8%), the MLH1me+ group was found to harbor a significantly higher frequency of RNF43 mutations (73.1% vs. 43.8%, P < 0.001) but much lower frequencies of KRAS (28.1% vs. 61.7%, P < 0.001), APC (43.3% vs. 63.6%, P = 0.011), CTNNB1 (9.0% vs. 29.2%, P = 0.001), FAM123B (13.4% vs. 28.1%, P = 0.025), and SOX9 (17.9% vs. 40.0%, P = 0.012) mutations compared to those in the MLH1-unmethylated dMMR CRCs (MLH1me− group). Regarding co-alteration patterns, 19 cases of BRAF/RNF43 comutated tumors were exclusively detected in the MLH1me+ group, whereas 46 cases of RAS/APC comutated tumors were found mainly in the MLH1me− group (35/46, 76.1%), especially among tumors associated with Lynch syndrome (27/46, 58.7%). After controlling for BRAF mutation status, the MLH1me+ phenotype was independently associated with an increased incidence of RNF43 mutations (95% CI 1.76–6.91; P < 0.001) and a decreased incidence of CTNNB1 mutations (95% CI 0.09–0.62; P = 0.003). At the signaling pathway level, no significant differences in the WNT, RTK-RAS, PI3K, TGF-β, TP53, or DDR pathways were observed between the MLH1me+ and MLH1me− groups.
Columns represent individual cases sorted by MMR status and dMMR subgroups. Tracks indicate dMMR status, MLH1 promoter hypermethylation status, MMR gene germline mutation status and RTK-RAS, PI3K, WNT, TGFβ, and TP53 pathway gene mutations. Individual genes are listed in rows. Mutations affecting tumor suppressor genes are classified according to whether they bear the MSI signature (insertions or deletions affecting homopolymer sequences). dMMR deficient mismatch repair, pMMR proficient mismatch repair, MSI microsatellite stability.
Mutation profile of the dMMR CRCs harboring MLH1 hypermethylation with RTK fusion genes
Fifteen of sixty-seven (22.4%) MLH1me+ dMMR CRCs were identified with oncogenic RTK gene rearrangements, including NTRK1 (n = 7), NTRK3 (n = 3), ALK (n = 3), and RET (n = 2), and were classified as the “MLH1me+ with fusion” subgroup. As shown in Fig. 5, none of these “MLH1me+ with fusion” tumors harbored alterations in other key driver genes in the RTK-RAS pathway, including BRAF, KRAS, NRAS, ERBB2, or ERBB3. Mutations affecting WNT pathway components were found in 12 cases (80.0%), mainly including inactivating mutations in tumor suppressor genes, RNF43 (n = 12), ARID1A (n = 8), APC (n = 4), AXIN2 (n = 4), FBXW7 (n = 3), FAM123B (n = 2), SOX9 (n = 2), and TCF7L2 (n = 1), except for one activating mutation in CTNNB1. Mutations in the PI3K signaling pathway (PIK3CA, PIK3R1, and PTEN) were identified in three tumors. The incidence of PI3K pathway aberrations was significantly lower in the “MLH1me+ with fusion” subgroup tumors than it was in the other dMMR tumors (20% vs. 73.8%, P < 0.001) or MLH1me+ tumors without RTK fusions (20% vs. 73.1%, P = 0.001). In addition, all TGFβ pathway aberrations in the “MLH1me+ with fusion” subgroup were found to be TGFBR2 frameshift mutations bearing MSI signature, which were significantly more prevalent than those in other dMMR tumors (46.7% vs. 7.8%, P = 0.002).
Mutation profile of the Lynch-like group of dMMR CRCs
Among the 32 tumor cases in the Lynch-like subgroup, 5 cases had 2 different heterozygous deleterious mutations in the same MMR gene (3 in MLH1, 1 in MSH2, and 1 in MSH6), and 5 cases had a single deleterious mutation in genes accompanied with associated LOH (3 in MLH1, 1 in MSH2, and 1 in PMS2), findings consistent with “double somatic mutations” (10/32, 31.3%). Fourteen cases were found to have only one deleterious mutation with a possible LOH explaining their IHC staining and were considered to harbor “possible double somatic mutations” (14/32, 43.8%). The other eight cases (five with PMS2 loss and three with MSH2/MSH6 loss) remained unresolved. Tumors in the Lynch-like group displayed no BRAF mutations and exhibited a remarkably lower frequency of RNF43 (40.6% vs. 73.1%, P = 0.002) mutations but a much higher frequency of CTNNB1 mutations (37.5% vs. 9.0%, P = 0.001) compared with the MLH1me+ dMMR group. No significant differences in the mutation profiles of key genes were detected in the Lynch-like group and the Lynch group of dMMR CRCs.
Discussion
In this study, we conducted a detailed molecular genetic analysis of a retrospective cohort comprised of 156 dMMR CRC and 225 pMMR CRC cases. Through the use of CGP, the gene mutation prevalence and co-alteration relationship of genes in key CRC oncogenic pathways were profiled, including the WNT, RTK-RAS, PI3K, TGF-β, TP53, and DDR pathways. Based on MMR germline mutations, MLH1 hypermethylation status and the presence of RTK fusion, the “MLH1me+” and “MLH1me+ with fusion” subgroups of the dMMR CRCs were identified and their molecular features further analyzed. We documented the characteristic mutation spectrum, as well as the pattern of gene co-occurrence and mutual exclusivity in the dMMR CRCs, with an emphasis on the molecular heterogeneity among dMMR subgroups.
Our data showed noticeable differences in the composition of most recurrently altered genes and their mutation frequencies in the dMMR and pMMR CRCs. In agreement with previous reports [17, 29], mutations in RNF43 and TCF7L2, both of which acting as key negative regulators in the WNT signaling pathway, were highly prevalent in our dMMR cohort but uncommon in the pMMR cohort. Of the well-known CRC-driver genes, KRAS and NRAS were frequently mutated regardless of MMR status, indicating their universally important role in CRC carcinogenesis. PIK3CA mutations, which were reported to be moderately enriched in dMMR CRCs in early studies [30, 31], were also found at a higher frequency in our dMMR group. However, TP53 and APC mutations, although frequently detected in both groups, were far more common in the pMMR group, a finding similar to that for the TCGA cohort [17]. In particular, the remarkable preponderance of TP53 mutations in pMMR tumors, along with the lack of an MSI signature, suggested that TP53 is unlikely to be a main mutational target for deficient MMR.
Notably, our study revealed a considerably high mutational incidence in multiple components of the DDR system, including ARID1A, ATM, and BRCA2, which has not been highlighted in previous studies of dMMR CRCs. As previously demonstrated [32, 33], ARID1A, ATM, and BRCA2 are all essential tumor suppressor genes that directly participate in the HRR of DNA double-strand breaks. Accordingly, we also showed that the HRR pathway was the most frequently defected one in DDR system apart from MMR pathway. These findings indicated that coordinated alterations of the HRR and MMR pathways might play an important role in CRC carcinogenesis, highlighting the synergistic effect of the DDR system. Both germline and somatic deleterious BRCA mutations have been established as indicators for the application of poly (ADP-ribose) polymerase (PARP) inhibitors in ovarian cancer. The increased frequency of BRCA2 mutations documented in our dMMR cohort, which largely contributed to MSI-related aberrations, implied the potential application of PARPi therapy in a portion of dMMR CRC cases and hinted that MMR deficiency might precede and lead to BRCA2 alterations. Moreover, there is growing appreciation that, in multiple solid malignancies, such as prostate cancer, bladder cancer, and triple-negative breast cancer, the dysfunction of other essential HRR proteins might reflect a response to PARPis [34, 35]. In a preclinical study, CRC cell lines carrying inactivating ATM mutations were found to exhibit increased sensitivity to olaparib [36]. Therefore, our finding that HRR-related genes were recurrently affected targets in dMMR CRC cases justifies further exploration of HRR inhibition therapy as a promising anticancer strategy in these tumors.
We showed that the WNT pathway was commonly altered in CRCs regardless of MMR status, supporting the supposition that it has an indispensable role in CRC oncogenesis. In particular, dMMR CRCs were more likely to harbor multiple WNT pathway alterations with complicated mutual relationships. Considering that CTNNB1 (β-catenin) acts as the main effector of the canonical WNT pathway and is negatively regulated by APC and RNF43 at different levels, the mutual exclusivity of the CTNNB1 mutation and the APC or RNF43 mutation found in the dMMR cohort was predictable. The RTK-RAS pathway is also frequently hyperactivated in CRCs, endowing it with key prognostic and predictive relevance. Despite the general mutually exclusive pattern within this pathway, we noticed that ERBB3 mutations often co-occurred with other RTK-RAS oncogenic mutations in the dMMR CRCs. This observation was also evidenced by a preclinical study suggesting the inadequacy of isolated ERBB3 mutations for oncogenic transformation [37]. Therapeutically targeting the PI3K pathway has become an area of intensive studies of multiple solid tumors [38], and an oral PI3K inhibitor has recently been approved by the US Food and Drug Administration for advanced breast cancers with PIK3CA mutations. Our finding of remarkably increased PI3K pathway aberrations in the dMMR CRCs thus leads to the consideration of including PI3K-targeted therapy in anticancer regimens for these tumors. The preferential coexistence of the PI3K and WNT pathways in our dMMR cohort further indicated the promising application of a PI3K inhibition strategy, as shown in a functional study whereby PI3KCA and APC comutated CRCs were more likely to respond to dual PI3K/mTOR inhibitors [39].
We further explored the intricate interaction between key genes involved in the WNT and RTK-RAS pathways. In addition to the preferential co-occurrence of RNF43 and BRAF mutations reported in a previous study [40, 41], we presented a novel finding showing a high prevalence of concurrent APC and RAS mutations in dMMR CRCs. We additionally showed the mutually exclusive relationship between RNF43 and RAS mutations and between APC and BRAF mutations. More specifically, RNF43/BRAF comutations and APC/RAS comutations were found to be enriched in sporadic and hereditary dMMR CRC cases, respectively. Both clinical and functional findings have suggested that concurrent RNF43 and BRAF mutations generally indicate the serrated neoplasia pathway leading to the majority of sporadic dMMR CRCs [41, 42]. On the other hand, APC and RAS mutations collaborate in the conventional adenoma pathway, which accounts for carcinogenesis in the majority of Lynch syndrome-associated CRCs [43]. Taken together, our data provide molecular evidence that dMMR CRC oncogenesis follows separate pathways with divergent mechanisms of RTK-RAS and WNT activation. The predisposition for a specific set of driver mutations caused by intrinsic mutational processes has been suggested in various types of cancers [44]. Therefore, it is rational to assume that the comprehensive interplay between oncogenic events across pathways, which was found to be more remarkable among dMMR CRCs in our cohort, might reflect a distinctive driver mutation profile conferred by MMR defects.
The differential involvement of key WNT pathway genes in the MLH1me+ and MLH1me− dMMR CRCs was investigated by previous studies [41]. However, among MLH1me+ tumors, whether the increased RNF43 mutation frequency was directly linked to the MLH1me+ phenotype or BRAF mutational status was not previously elucidated. Through logistic regression analysis, we demonstrated that MLH1me+ was an independent factor associated with prevalent RNF43 mutations in dMMR CRCs, but not BRAF mutations. This association was further supported by the fact that RNF43 mutations were also relatively frequent in the MLH1me+ tumors with wild-type BRAF, including those harboring RTK fusion genes. It should be noted that RNF43 mutations were also detected in a considerable proportion of the MLH1me− dMMR tumors, although they were significantly less frequent than in the MLH1me+ tumors, hinting at a possible correlation between RNF43 defects and MMR deficiency not caused by MLH1 hypermethylation. Moreover, the majority of RNF43 mutations in both the MLH1me+ and MLH1me− dMMR tumors were found to be associated with MSI. All these results suggested that MMR deficiency, especially that caused by MLH1 hypermethylation, might be the direct cause of RNF43 mutations. In addition, RNF43 mutations in our pMMR group, which were uncommon and did not affect the MSI signature, exhibited a tendency to coexistence with BRAF mutations. This finding suggests a weak association between RNF43 and BRAF mutations in pMMR CRCs, albeit to a much lesser extent than their association in the dMMR CRCs. Referring to a previous study [41], these rare RNF43/BRAF comutated pMMR cases probably indicate germline RNF43 mutation carriers with a serrated polyposis phenotype. To summarize, our findings revealed that the mutation of RNF43, which might represent a dysfunctional negative feedback mechanism of the WNT pathway, was an indispensable yet relatively late event in MLH1me+ dMMR CRC oncogenesis and was independently correlated with MLH1 hypermethylation but not BRAF mutation. It should be noted that RNF43 p. G659Vfs*41, which was the most common RNF43 mutant and accounted for 60% of the RNF mutations in our dMMR cohort, was suggested to be fully functional in inhibiting WNT signaling in an in vitro study [45]. The significant role of mutated RNF43 in the pathogenesis of MLH1me+ tumors might not be entirely substantiated by the present data and awaits further exploration. In addition, we also observed decreased incidence of KRAS mutation and that of other WNT signaling components (CTNNB1, APC, FAM123B, and SOX9) in MLH1me+ tumors, reflecting the characteristic mutational spectrum of this subgroup.
A recent functional study suggested that RTK fusion genes might be alternative drivers of the sessile serrated pathway in CRC carcinogenesis [46]. Within our cohort, the “MLH1me+ with fusion” subgroup shared some genetic features typically presented by MLH1me+ dMMR CRCs but also displayed intricate differences (Supplementary Fig. 2). Given the established fact that oncogenic mutations within the RTK-RAS pathway are generally mutually exclusive, it was not surprising to find that other RTK-RAS oncogenic alterations were excluded from the “MLH1me+ with fusion” subgroup. Intriguingly, although PI3K pathway aberration was found to be highly prevalent in the dMMR CRCs, its incidence was significantly decreased in the “MLH1me+ with fusion” subgroup. This paradox might be partially explained by the fact that the constitutive activation of tyrosine kinase by gene rearrangements was able to simultaneously induce downstream RAS and PI3K pathways through the recruitment of various adapter proteins [47]. In those particular cases carrying concurrent RTK fusion and PI3K pathway aberration, we speculated the altered PI3K pathway might represent a nonoverlapping mechanism besides RTK hyperactivation, giving rise to downstream malignant transformation events. We also noticed that TGFβ pathway inactivation in the “MLH1me+ with fusion” subgroup was solely caused by TGFBR2 truncation mutations.
“Lynch-like” dMMR CRCs have long been recognized as an ill-defined subgroup. Our results revealed that the oncogenic pathway alteration profile of “Lynch-like” tumors was more similar to that of Lynch syndrome-associated tumors than to that of MLH1me+ tumors. In addition, we confirmed that the majority of cases in the “Lynch-like” subgroup can be explained by inactivation of somatic MMR genes that might be indicators of low cancer risk that do not necessarily need intensive screening or surveillance.
In the present study, the KRAS mutation frequency of dMMR CRCs was higher than it was in previous reports on Western populations [17, 48] but similar to that in studies based on the Chinese population [49, 50], which might be partially explained by the genetic differences among ethnic groups. However, our results need further validation in a larger multicenter cohort.
In summary, our comprehensive molecular study revealed a significant difference in the gene mutational spectrum and signaling pathway interaction pattern between dMMR and pMMR CRCs. Through detailed profiling of the molecular features among dMMR subgroups, we presented a differential mechanism and complex mutual relationship of the oncogenic events in the MSI and serrated pathways of CRC tumorigenesis (Supplementary Fig. 2) [40, 41]. This molecular heterogeneity probably underlies the different response to adjuvant therapy of dMMR CRCs and justifies individualized therapy targeting dMMR subgroups.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32.
Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, et al. Screening for the Lynch syndrome (hereditary nonpolyposis colorectal cancer). N Engl J Med. 2005;352:1851–60.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–13.
Fuchs TL, Sioson L, Sheen A, Jafari-Nejad K, Renaud CJ, Andrici J, et al. Assessment of Tumor-infiltrating lymphocytes using International TILs Working Group (ITWG) system is a strong predictor of overall survival in colorectal carcinoma: a study of 1034 patients. Am J Surg Pathol. 2020;44:536–44.
Chalmers ZR, Connelly CF, Fabrizio D, Gay L, Ali SM, Ennis R, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017;9:34.
Li Z, Pearlman AH, Hsieh P. DNA mismatch repair and the DNA damage response. DNA Repair. 2016;38:94–101.
Wang Z, Zhao J, Wang G, Zhang F, Zhang Z, Zhang F, et al. Comutations in DNA damage response pathways serve as potential biomarkers for immune checkpoint blockade. Cancer Res. 2018;78:6486–96.
Chen W, Swanson BJ, Frankel WL. Molecular genetics of microsatellite-unstable colorectal cancer for pathologists. Diagn Pathol. 2017;12:24.
Wang J, Yi Y, Xiao Y, Dong L, Liang L, Teng L, et al. Prevalence of recurrent oncogenic fusion in mismatch repair-deficient colorectal carcinoma with hypermethylated MLH1 and wild-type BRAF and KRAS. Mod Pathol. 2019;32:1053–64.
Sato K, Kawazu M, Yamamoto Y, Ueno T, Kojima S, Nagae G, et al. Fusion kinases identified by genomic analyses of sporadic microsatellite instability-high colorectal cancers. Clin Cancer Res. 2019;25:378–89.
Cocco E, Benhamida J, Middha S, Zehir A, Mullaney K, Shia J, et al. Colorectal carcinomas containing hypermethylated MLH1 promoter and wild-type BRAF/KRAS are enriched for targetable kinase fusions. Cancer Res. 2019;79:1047–53.
Lasota J, Chłopek M, Lamoureux J, Christiansen J, Kowalik A, Wasąg B, et al. Colonic adenocarcinomas harboring NTRK fusion genes: a clinicopathologic and molecular genetic study of 16 cases and review of the literature. Am J Surg Pathol. 2020;44:162–73. https://doi.org/10.1097/pas.0000000000001377
Schrader KA, Cheng DT, Joseph V, Prasad M, Walsh M, Zehir A, et al. Germline variants in targeted tumor sequencing using matched normal DNA. JAMA Oncol. 2016;2:104–11.
Lv X, Zhao M, Yi Y, Zhang L, Guan Y, Liu T, et al. Detection of rare mutations in CtDNA using next generation sequencing. J Vis Exp. 2017;126:56342.
Yang X, Chu Y, Zhang R, Han Y, Zhang L, Fu Y, et al. Technical validation of a next-generation sequencing assay for detecting clinically relevant levels of breast cancer-related single-nucleotide variants and copy number variants using simulated cell-free DNA. J Mol Diagn. 2017;19:525–36.
Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Knijnenburg TA, Wang L, Zimmermann MT, Chambwe N, Gao GF, Cherniack AD, et al. Genomic and molecular landscape of DNA damage repair deficiency across the Cancer Genome Atlas. Cell Rep. 2018;23:239–54.e6.
Pearl LH, Schierz AC, Ward SE, Al-Lazikani B, Pearl FM. Therapeutic opportunities within the DNA damage response. Nat Rev Cancer. 2015;15:166–80.
Scarbrough PM, Weber RP, Iversen ES, Brhane Y, Amos CI, Kraft P, et al. A cross-cancer genetic association analysis of the DNA repair and DNA damage signaling pathways for lung, ovary, prostate, breast, and colorectal cancer. Cancer Epidemiol Biomark Prev. 2016;25:193–200.
Forbes SA, Beare D, Boutselakis H, Bamford S, Bindal N, Tate J, et al. COSMIC: somatic cancer genetics at high-resolution. Nucleic Acids Res. 2017;45:D777–83.
Chakravarty D, Gao J, Phillips SM, Kundra R, Zhang H, Wang J, et al. OncoKB: a precision oncology knowledge base. JCO Precis Oncol. 2017;2017. https://doi.org/10.1200/PO.17.00011.
Sim NL, Kumar P, Hu J, Henikoff S, Schneider G, Ng PC. SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic Acids Res. 2012;40:W452–7.
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7:248–9.
Reva B, Antipin Y, Sander C. Predicting the functional impact of protein mutations: application to cancer genomics. Nucleic Acids Res. 2011;39:e118.
Chang MT, Asthana S, Gao SP, Lee BH, Chapman JS, Kandoth C, et al. Identifying recurrent mutations in cancer reveals widespread lineage diversity and mutational specificity. Nat Biotechnol. 2016;34:155–63.
Iyer G, Balar AV, Milowsky MI, Huang WC, Woods M, Donat SM, et al. Correlation of DNA damage response (DDR) gene alterations with response to neoadjuvant (neo) dose-dense gemcitabine and cisplatin (ddGC) in urothelial carcinoma (UC). J Clin Oncol. 2016;34:5011 https://doi.org/10.1200/JCO.2016.34.15_suppl.5011
Teo MY, Bambury RM, Zabor EC, Jordan E, Al-Ahmadie H, Boyd ME, et al. DNA damage response and repair gene alterations are associated with improved survival in patients with platinum-treated advanced urothelial carcinoma. Clin Cancer Res. 2017;23:3610–8.
Giannakis M, Hodis E, Jasmine Mu X, Yamauchi M, Rosenbluh J, Cibulskis K, et al. RNF43 is frequently mutated in colorectal and endometrial cancers. Nat Genet. 2014;46:1264–6.
Day FL, Jorissen RN, Lipton L, Mouradov D, Sakthianandeswaren A, Christie M, et al. PIK3CA and PTEN gene and exon mutation-specific clinicopathologic and molecular associations in colorectal cancer. Clin Cancer Res. 2013;19:3285–96.
Cohen SA, Turner EH, Beightol MB, Jacobson A, Gooley TA, Salipante SJ, et al. Frequent PIK3CA mutations in colorectal and endometrial tumors with 2 or more somatic mutations in mismatch repair genes. Gastroenterology. 2016;151:440–7.e1.
Shen J, Peng Y, Wei L, Zhang W, Yang L, Lan L, et al. ARID1A deficiency impairs the DNA damage checkpoint and sensitizes cells to PARP inhibitors. Cancer Discov. 2015;5:752–67.
Bakr A, Oing C, Köcher S, Borgmann K, Dornreiter I, Petersen C, et al. Involvement of ATM in homologous recombination after end resection and RAD51 nucleofilament formation. Nucleic Acids Res. 2015;43:3154–66.
Rimar KJ, Tran PT, Matulewicz RS, Hussain M, Meeks JJ. The emerging role of homologous recombination repair and PARP inhibitors in genitourinary malignancies. Cancer. 2017;123:1912–24.
Geenen JJJ, Linn SC, Beijnen JH, Schellens JHM. PARP Inhibitors in the treatment of triple-negative breast cancer. Clin Pharmacokinet. 2018;57:427–37.
Wang C, Jette N, Moussienko D, Bebb DG, Lees-Miller SP. ATM-deficient colorectal cancer cells are sensitive to the PARP inhibitor olaparib. Transl Oncol. 2017;10:190–6.
Jaiswal BS, Kljavin NM, Stawiski EW, Chan E, Parikh C, Durinck S, et al. Oncogenic ERBB3 mutations in human cancers. Cancer Cell. 2013;23:603–17.
Janku F, Yap TA, Meric-Bernstam F. Targeting the PI3K pathway in cancer: are we making headway?. Nat Rev Clin Oncol. 2018;15:273–91.
Foley TM, Payne SN, Pasch CA, Yueh AE, Van De Hey DR, Korkos DP, et al. Dual PI3K/mTOR inhibition in colorectal cancers with APC and PIK3CA mutations. Mol Cancer Res. 2017;15:317–27.
Sekine S, Mori T, Ogawa R, Tanaka M, Yoshida H, Taniguchi H, et al. Mismatch repair deficiency commonly precedes adenoma formation in Lynch Syndrome-Associated colorectal tumorigenesis. Mod Pathol. 2017;30:1144–51.
Yan HHN, Lai JCW, Ho SL, Leung WK, Law WL, Lee JFY, et al. RNF43 germline and somatic mutation in serrated neoplasia pathway and its association with BRAF mutation. Gut. 2017;66:1645–56.
Tsai JH, Liau JY, Yuan CT, Lin YL, Tseng LH, Cheng ML, et al. RNF43 is an early and specific mutated gene in the serrated pathway, with increased frequency in traditional serrated adenoma and its associated malignancy. Am J Surg Pathol. 2016;40:1352–9.
Ahadova A, Gallon R, Gebert J, Ballhausen A, Endris V, Kirchner M, et al. Three molecular pathways model colorectal carcinogenesis in Lynch syndrome. Int J Cancer. 2018;143:139–50.
Temko D, Tomlinson IPM, Severini S, Schuster-Böckler B, Graham TA. The effects of mutational processes and selection on driver mutations across cancer types. Nat Commun. 2018;9:1857.
Tu J, Park S, Yu W, Zhang S, Wu L, Carmon K, et al. The most common RNF43 mutant G659Vfs*41 is fully functional in inhibiting Wnt signaling and unlikely to play a role in tumorigenesis. Sci Rep. 2019;9:18557.
Chan AW, Pan Y, Tong JH, Lung RW, Kwan JS, Chow C, et al. Receptor tyrosine kinase fusions act as a significant alternative driver of the serrated pathway in colorectal cancer development. J Pathol. 2020;251:74–86.
Lange AM, Lo HW. Inhibiting TRK proteins in clinical cancer therapy. Cancers. 2018;10:105.
Schell MJ, Yang M, Teer JK, Lo FY, Madan A, Coppola D, et al. A multigene mutation classification of 468 colorectal cancers reveals a prognostic role for APC. Nat Commun. 2016;7:11743.
Zhang X, Ran W, Wu J, Li H, Liu H, Wang L, et al. Deficient mismatch repair and RAS mutation in colorectal carcinoma patients: a retrospective study in Eastern China. PeerJ. 2018;6:e4341.
Li W, Zhi W, Zou S, Qiu T, Ling Y, Shan L, et al. Distinct clinicopathological patterns of mismatch repair status in colorectal cancer stratified by KRAS mutations. PLoS ONE. 2015;10:e0128202.
Funding
This work was supported by Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (No. 2019-I2M-2-002) and CAMS Central Public Welfare Scientific Research Institute Basal Research Funds Clinical and Translational Medicine Research Program (2019XK320045).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, J., Li, R., He, Y. et al. Next-generation sequencing reveals heterogeneous genetic alterations in key signaling pathways of mismatch repair deficient colorectal carcinomas. Mod Pathol 33, 2591–2601 (2020). https://doi.org/10.1038/s41379-020-0612-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41379-020-0612-2
This article is cited by
-
Bacillus Calmette-Guerin induces CD8+ T cell infiltration and suppresses tumor progression in microsatellite stable colorectal cancer by downregulating ARID1A
Cancer Gene Therapy (2025)
-
Neoadjuvant immunotherapy for dMMR and pMMR colorectal cancers: therapeutic strategies and putative biomarkers of response
Nature Reviews Clinical Oncology (2024)
-
Targeting MEK/COX-2 axis improve immunotherapy efficacy in dMMR colorectal cancer with PIK3CA overexpression
Cellular Oncology (2024)
-
Roles of ARID1A variations in colorectal cancer: a collaborative review
Molecular Medicine (2022)
-
Comprehensive analysis of oncogenic fusions in mismatch repair deficient colorectal carcinomas by sequential DNA and RNA next generation sequencing
Journal of Translational Medicine (2021)