Abstract
Purpose
Non-White patients are poorly represented in prostate cancer trials. MRI PI-RADS scoring was developed in primarily White populations, but prostate cancer differs in non-White men. We aimed to explore differences in PI-RADS calibration for Asian and Black men.
Materials and methods
This is a secondary analysis of PREVENT, a multi-institutional study of infection rates for transrectal vs. transperineal biopsy. We compared cancer detection for self-identifying Asian and Black men. We compared detection rates on a per-person basis, stratified by index PI-RADS lesion, to White men, using Fisher’s exact and logistic regression.
Results
Of 665/752 trial patients with PI-RADS 3-5 lesions, 88 (13%) were Black and 36 (6%) were Asian. Black men were younger at diagnosis with increased rates of overall (70% vs. 43%%, P = 0.004) and clinically significant prostate cancer (60% vs. 27%, P = 0.003) and Asian men had decreased rates of overall (0% vs. 47%, P = 0.004) and clinically significant prostate cancer (0% vs. 27%, P = 0.003) in PI-RADS 3 lesions compared to White men. On multivariable regression, Black men with PI-RADS 3/4 lesions had higher odds of overall (OR 1.17, P = 0.009) and clinically significant prostate cancer (OR 1.20, P = 0.004) and Asian men had lower odds of overall (OR 0.79, P = 0.01) but not clinically significant prostate cancer (OR 0.94, P = 0.5).
Conclusions
Black men with PI-RADS 3/4 lesions had 20% higher odds of clinically significant prostate cancer than White men while all PI-RADS 3 lesions in Asian men were negative. These findings suggest PI-RADS may require differential interpretation when assessing prostate cancer risk in non-White men.
Trial Registration
Registered at ClinicalTrials.gov (NCT04843566, https://clinicaltrials.gov/study/NCT04843566).
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the most common solid malignancy in men, affecting 1 in 8 men in their lifetime [1]. There is a significant differential in PCa disease burden by race in the United States with Black men experiencing younger age at PCa diagnosis, higher grade PCa at diagnosis, and higher PCa-specific mortality [2]. Multiple theories exist in the literature as to why this health disparity exists, including access to care, genetic variations (such as CDKN1B deletions), and Vitamin D related molecular mechanisms [3,4,5,6]. While many of these may contribute to the differences in PCa outcomes for Black men, none of these have been able to fully explain the disparity.
Another reason that has been well-documented across multiple fields of medicine is that randomized controlled trials (RCT) tend to have poor accrual of non-White patients, which can prevent findings from being validated across racial groups and possibly lead to unintentional mismanagement of non-White patients [7, 8]. Over the past several decades, there has been significant attention directed to refine the evaluation of PSA testing to better balance detection of clinically significant cancer with harms associated with over-diagnosis. Although algorithms differ from institution to institution, many algorithms use serum PSA level and PI-RADS lesions on MRI as the main factors that determine when to biopsy a patient. Given that PSAD and PI-RADS were validated in a predominantly White population [9], it is possible that mis-calibration of these clinical factors could be contributing to PCa outcome disparities for Black men.
Similarly, Asian men remain under-represented in pivotal PCa trials [10]. While the known disparities for Black men have generated a significant arm of research into the cause, there is a much smaller body of literature surrounding PCa in Asian men, a demographic that is growing rapidly in the United States. What data does exist, however, demonstrates lower rates of grade group (GG) 1 PCa detection and fewer positive biopsies for PI-RADS 3 lesions compared to non-Asian peers, suggesting a possible mis-calibration of current risk stratification tools for Asian men as well [11].
The PREVENT trial was a multi-institutional randomized controlled trial which compared infectious outcomes between transperineal (TP) and transrectal (TR) prostate needle biopsy (PNB). The study captured self-identified race and MRI lesion data with self-identifying Asian men representing 4.9% and self-identifying Black men representing 13.4% of the overall trial cohort, respectively [12]. Here, we analyze biopsy outcomes for both self-identifying Black and Asian patients in the PREVENT trial with the hypothesis that MRI may not be appropriately calibrated for these populations.
Materials and methods
Study participants
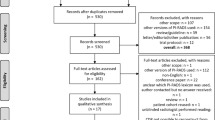
Patients randomly allocated to the PREVENT trial’s TP vs. TR PNB comparison were eligible for study. Informed consent was obtained from all subjects. The first efficacy results from this comparison have been published previously [12]. Briefly, from March 2021 through May 2023, patients were recruited at ten centers and were eligible for enrollment if they had not undergone prior PNB, had an elevated PSA level and/or abnormal digital rectal examination (DRE), and had suspicious prostate magnetic resonance imaging (MRI) characteristics (Prostate Imaging Reporting and Data System, version 2.1 [13] scores 3–5). They were then randomized 1:1 to TP PNB without antibiotic prophylaxis or TR PNB with targeted antibiotic prophylaxis. All patients underwent multiparametric MRI (mpMRI) per study protocol prior to enrollment and randomization. mpMRI protocols had slight variation by study site but all included T1 and T2 weighted sequences with diffusion-weighted imaging and dynamic contrast enhancement series. Reviewers were blinded to treatment allocation and outcomes as previously reported [12]. A small number of participants had biopsy without MRI (claustrophobia and metal prosthesis) and were included in the original trial but were excluded from this secondary analysis as the primary outcome of this analysis is predicated on presence or absence of mpMRI PI-RADS lesions. The exclusion criteria were acute prostatitis in the last 6 months or any current bacterial infection requiring antibiotic treatment. All patients provided written informed consent. The trial is registered at ClinicalTrials.gov (NCT04843566), funded by the NCI (5R01CA241758-05) and had full regulatory, national ethics committee, and local site approval. Full details of the PREVENT trial protocol is provided in Supplementary Methods 1. As part of the trial, race data was collected via self-reporting and used for this secondary analysis.
Outcomes
The PREVENT trial comparison’s primary outcome measure was infection rate by PNB approach but here we focus on overall and clinically significant PCa (csPCa) rates by race. Rates of overall and csPCa defined as Gleason Grade Group \(\ge\)2 detection on a per-person basis were compared based on self-identified race, stratified by PI-RADS score of the person’s index lesion. As such, only those patients with PI-RADS \(\ge\)3 lesions on MRI were included.
Statistical analysis
For continuous variables, Shapiro-Wilk test was used to assess normality. We then used Kruskal-Wallis and one-way ANOVA tests as appropriate to compare continuous variables across racial groups; for comparisons that were found to be significantly different across racial groups, we performed subsequent pairwise Wilcoxon or t-tests, respectively, with Bonferroni correction applied to adjust for multiple comparisons. Fisher’s exact test was used to compare categorical variables. For the subset of patients who had a PI-RADS 3 or 4 lesions (considered to be intermediate to high risk under PI-RADS), we created separate multivariable logistic regression models with the outcome of interest as either any PCa detection or csPCa. We used these models to assess for possible associations between patient reported race and these outcomes of interests. Variables were included in our model by consensus from our study team based on likelihood of association with cancer detection.
Cutoff for significance for all analyses was p < 0.05. All statistical analysis was conducted in R version 4.4.2.
Results
At the completion of enrollment, the PREVENT trial included 665 patients from March 2021 through May 2023 who had a PI-RADS lesion visible on MRI. The CONSORT diagram from the original trial is included as Supplementary Fig. 1. Of this cohort, 414 (62%) patients self-identified as White, 88 (13%) as Black, 36 (6%) as Asian, and 125 (19%) declined to report their race or identified as “Other.” Black men were significantly younger at PCa diagnosis (P = 0.001) with higher PSA (P = 0.02) and higher PSA density (PSAD) (P = 0.01). Baseline patient characteristics, including prostate cancer risk factors are summarized in Table 1.
When assessing for cancer detection, there was a statistically significant increase in rates of overall PCa (70% vs. 43%%, P = 0.004) (Fig. 1) and csPCa (60% vs. 27%, P = 0.003) for Black patients with PI-RADS 3 lesions compared to White patients (Fig. 2) (Table 2). On logistic regression controlling for age, biopsy approach, and PSAD, Black men with PI-RADS 3 or 4 lesions had higher odds of overall PCa (OR 1.17, P = 0.009) and csPCa (OR 1.20, P = 0.004) detection than White men with PI-RADS 3 or 4 lesions (Table 3).
For Asian men, there was a statistically significant decrease in rates of overall PCa (0% vs. 47%, P = 0.004) (Fig. 1) and csPCA (0% vs. 27%, P = 0.003) (Fig. 2) (Table 2). On logistic regression controlling for age, biopsy approach, and PSAD, Asian men with PI-RADS 3 or 4 lesions had lower odds of overall PCa (OR 0.79, P = 0.01) but not csPCa (OR 0.94, P = 0.5) than White men with PI-RADS 3 or 4 lesions (Table 3).
Discussion
In this secondary analysis of the first multicenter, randomized trial comparing novel, office-based transperineal prostate biopsy with the traditional transrectal approach, we found increased detection of overall PCa and clinically significant PCa in Black men with a PI-RADS 3 lesion compared to non-Black men. We also found decreased detection of overall PCa and clinically significant PCa in Asian men with a PI-RADS 3 lesion compared to non-Asian men.
These findings in Black men suggest that the PI-RADS system in its current form is not appropriately calibrated for PCa risk assessment in Black men. Our data shows that Black men with a PI-RADS 3 or 4 lesions are 20% more likely to harbor csPCa than their non-Black counterparts, suggesting that a PI-RADS 3 or 4 lesion should be treated as a more concerning finding in this patient population. Furthermore, when looking at the data globally, the csPCa detection rate for a PI-RADS 3 lesion in a Black man exceeded the csPCa rate for PI-RADS 4 lesion in White patients, which in our study was 70%. This suggests that PI-RADS 3 lesions in Black men should be treated like PI-RADS 4 lesions in White men from a risk stratification perspective. While this simple “upgrading” of intermediate risk PI-RADS lesions for Black men is a certainly a compelling and facile clinical heuristic, it should not be a substitute for a more systematic and nuanced recalibration of the PI-RADS system.
Given that most current biopsy algorithms weigh a PI-RADS 4 differently than a PI-RADS 3 lesions for determining pre-test probability, it may explain why there is often a delay in diagnosis for Black men which in turn creates a racial disparity in PCa outcomes. Previous studies have suggested that differences in dynamic contrast enhanced MRI parameters exist between Black and White men [14, 15], which may explain the different behavior of PI-RADS lesions found in our study. Zabihollahy et al. (2024) performed a quantitative mpMRI study of PCa in Black and White patients and similarly found that there was an increased risk of csPCa in PI-RADS 3 and 4 lesions in Black men, along with higher rates of csPCa in the peripheral zone and posterior aspect of the prostate [16]. Multiple other studies agree with this finding of increased rate of csPCa despite equivalent PI-RADS lesion in Black men [17, 18], although there are some studies that found that the PI-RADS 2.0 system underperforms in Hispanic men relative to White men but no difference between Black and White men [9]. Although not entirely novel, our findings provide the highest level of evidence of this relationship, as this is the first data from a randomized controlled trial compared to non-randomized data in prior studies.
Further, in this study Black patients had significantly higher PSAD at time of enrollment compared to non-Black patients. It has previously been well documented in the literature that Black men have higher PSAD compared to non-Black men. There is also evidence that using the Prostate Health Index (PHI) may function better in Black men, who typically present with larger prostates and higher PSAD [19, 20]. Other studies have shown that biparametric MRI (bpMRI) performs as well as mpMRI in Black men [21], a subject which was not explored in this study but provides a promising framework for further study.
Given that this is a randomized trial, this also represents the highest quality data to date in the literature evaluating PI-RADS performance in Asian men. None of the Asian men with PI-RADS 3 lesions in this study were diagnosed with PCa. While these results suggest that the risk of PCa may be overestimated using the PI-RADS system, it is important that they are interpreted in the context of a small sample size with only 7 patients. It is hard to know if these findings would be validated in a larger sample size. However, it is consistent with previous literature that Asian men have lower risk of csPCa per equivalent PI-RADS lesion compared to non-Asian men [11, 22]. While the two Gross et al. studies performed their analysis on Asian American men specifically, other cohort studies in Asia have demonstrated similar findings with rates of csPCa detection around 10% in PI-RADS 3 lesions, which is well below our findings of 28% in this study for White patients [23, 24].
Historically, Asian men have a lower prostate cancer incidence relative to other men in Western countries [25, 26]. While there are multiple explanations hypothesized for this, ranging from the protective effect of a soy-based diet to differences in nationalized screening protocols, there is no agreed upon explanation for this consistent finding [25, 27]. One major component to this difference may be that Asian/Pacific Islander men only account for 1.5% of all patients in PCa clinical trials per a 2023 meta-analysis [28]. Given this disparity in representation, it is unsurprising that the risk assessment calculators derived from European trials, such as the European Randomized Trial for Screening of Prostate Cancer (ERSPC), underperform in Korean men relative to the Seoul National University Prostate Cancer Risk Calculator or that a universal PSA screening program in Japan yielded a ten-fold lower rate of PCa diagnosis than similar universal screening programs in other countries [29, 30]. With 5% of our trial population self-identifying as Asian, our data contains a more representative population of Asian men relative to the US population and provides the highest representation in a PCa randomized trial to date.
This study does have a couple of limitations. By including only patients from the original PREVENT trial with PI-RADS 3 or greater lesions on mpMRI, the sample size of Asian and Black men was relatively small. Despite this, the distribution of race in our cohort closely reflects national demographic data and the rate of non-White patients is well above the representation in most previous clinical trials. This study was completed with mpMRI as the imaging modality, which is not feasible in every clinical setting secondary to availability and/or cost. We believe that our findings would remain true even with bpMRI as the imaging modality of choice and hope to validate these findings in a similar patient population with bpMRI. Given that MRI was completed prior to study enrollment, the well-established limitations of inter-reader reliability of PI-RADS scoring or variable mpMRI protocols also apply to this study. Finally, the PREVENT trial was based on prostate biopsy specimens and not prostatectomy specimens and was powered to detect differences in infection rate, not cancer detection. As such, it may be underpowered to detect differences in cancer detection by race and the rates of csPCa detected may differ with prostatectomy specimens. Yet, despite this limitation we were able to identify clinically meaningful differences in cancer detection by race.
Conclusions
Black men with PI-RADS 3 or 4 lesions had 20% higher odds of csPCa detection than their White counterparts, even after adjusting for other risk factors. By contrast, all PI-RADS 3 lesions in Asian men were negative. These findings suggest that PI-RADS, which was validated in a population of men of predominantly European descent, may have poor calibration when assessing csPCa risk in Black and Asian men. This could be related to greater prostate cancer prevalence or more aggressive prostate cancer among Black men and contribute to unnecessary biopsies in Asian men. The PI-RADS classification system should be systematically re-evaluated considering these findings to ensure adequate validation amongst different racial groups.
Data availability
Study protocol and statistical analysis plan are fully available in the text and supplement. After de-identification, individual participant data that underlie the study results and analytic code will be available immediately upon publication with no end date to researchers who provide a methodologically sound proposal. Proposals should be directed to e-schaeffer@northwestern.edu. To gain access, data requestors must sign a data access agreement.
Code availability
Study protocol and statistical analysis plan are fully available in the text and supplement. After de-identification, individual participant data that underlie the study results and analytic code will be available immediately upon publication with no end date to researchers who provide a methodologically sound proposal. Proposals should be directed to e-schaeffer@northwestern.edu. To gain access, data requestors must sign a data access agreement.
References
Culp MB, Soerjomataram I, Efstathiou JA, Bray F, Jemal A. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur Urol. 2020;77:38–52.
Lillard JW Jr, Moses KA, Mahal BA, George DJ. Racial disparities in Black men with prostate cancer: A literature review. Cancer. 2022;128:3787–95.
Lent AB, Garrido CO, Baird EH, Viela R, Harris RB. Racial/ethnic disparities in health and life insurance denial due to cancer among cancer survivors. Int J Environ Res Public Health. 2022;19:2166.
Taylor JA, Hirvonen A, Watson M, Pittman G, Mohler JL, Bell DA. Association of prostate cancer with vitamin D receptor gene polymorphism. Cancer Res. 1996;56:4108–10.
Ufuah S, Tallman JE, Moses KA. The Pursuit of Health Equity and Equality in Urologic Oncology: Where We Have Been and Where We Are Going. Eur Urol Focus. 2021;7:929–36.
Faisal FA, Murali S, Kaur H, Vidotto T, Guedes LB, Salles DC, et al. CDKN1B Deletions are Associated with Metastasis in African American Men with Clinically Localized, Surgically Treated Prostate Cancer. Clin Cancer Res. 2020;26:2595–602.
Kaplan CP, Napoles AM, Narine S, Gregorich S, Livaudais-Toman J, Nguyen T, et al. Knowledge and attitudes regarding clinical trials and willingness to participate among prostate cancer patients. Contemp Clin Trials. 2015;45:443–8.
Rogers CR, Rovito MJ, Hussein M, Obidike OJ, Pratt R, Alexander M, et al. Attitudes Toward Genomic Testing and Prostate Cancer Research Among Black Men. Am J Prev Med. 2018;55:S103–S11.
Meza J, Babajide R, Saoud R, Sweis J, Abelleira J, Helenowski I, et al. Assessing the accuracy of multiparametric MRI to predict clinically significant prostate cancer in biopsy naive men across racial/ethnic groups. BMC Urol. 2022;22:107.
Halabi S, Dutta S, Tangen CM, Rosenthal M, Petrylak DP, Thompson IM Jr, et al. Comparative Survival of Asian and White Metastatic Castration-Resistant Prostate Cancer Men Treated With Docetaxel. JNCI Cancer Spectr. 2020;4:pkaa003.
Gross MD, Al Hussein Al Awamlh B, Shoag JE, Mauer E, Banerjee S, Margolis DJ, et al. Race and prostate imaging: implications for targeted biopsy and image-based prostate cancer interventions. BMJ Surg Inter Health Technol. 2019;1:e000010.
Hu JC, Assel M, Allaf ME, Ehdaie B, Vickers AJ, Cohen AJ, et al. Transperineal Versus Transrectal Magnetic Resonance Imaging-targeted and Systematic Prostate Biopsy to Prevent Infectious Complications: The PREVENT Randomized Trial. Eur Urol. 2024;86:61–8.
Turkbey B, Rosenkrantz AB, Haider MA, Padhani AR, Villeirs G, Macura KJ, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019;76:340–51.
Futterer JJ, Engelbrecht MR, Huisman HJ, Jager GJ, Hulsbergen-van De Kaa CA, Witjes JA, et al. Staging prostate cancer with dynamic contrast-enhanced endorectal MR imaging prior to radical prostatectomy: experienced versus less experienced readers. Radiology. 2005;237:541–9.
Yuan Q, Costa DN, Senegas J, Xi Y, Wiethoff AJ, Rofsky NM, et al. Quantitative diffusion-weighted imaging and dynamic contrast-enhanced characterization of the index lesion with multiparametric MRI in prostate cancer patients. J Magn Reson Imaging. 2017;45:908–16.
Zabihollahy F, Miao Q, Naim S, Sonni I, Vangala S, Kim H, et al. Investigating MRI-Associated Biological Aspects of Racial Disparities in Prostate Cancer for African American and White Men. J Magn Reson Imaging. 2025;61:121–31.
Hines L, Zhu D, DeMasi M, Babar M, Chernyak V, Kovac EZ, et al. A Comparison of Image-Guided Targeted Prostate Biopsy Outcomes by PI-RADS(R) Score and Ethnicity in a Diverse, Multiethnic Population. J Urol. 2021;206:586–94.
Patel HD, Doshi CP, Koehne EL, Hart S, Van Kuiken M, Quek ML, et al. African American Men have Increased Risk of Prostate Cancer Detection Despite Similar Rates of Anterior Prostatic Lesions and PI-RADS Grade on Multiparametric Magnetic Resonance Imaging. Urology. 2022;163:132–7.
Garraway IP, Carlsson SV, Nyame YA, Vassy JL, Chilov M, Fleming M, et al. Prostate Cancer Foundation Screening Guidelines for Black Men in the United States. NEJM Evid. 2024;3:EVIDoa2300289.
Smith ZL, Eggener SE, Murphy AB. African-American Prostate Cancer Disparities. Curr Urol Rep. 2017;18:81.
Abramson M, DeMasi M, Zhu D, Hines L, Lin W, Kanmaniraja D, et al. Biparametric versus multiparametric MRI for the detection of clinically significant prostate cancer in a diverse, multiethnic population. Abdom Radio. 2024;49:2491–8.
Gross MD, Marks LS, Sonn GA, Green DA, Wang GJ, Shoag JE, et al. Variation in Magnetic Resonance Imaging-Ultrasound Fusion Targeted Biopsy Outcomes in Asian American Men: A Multicenter Study. J Urol. 2020;203:530–6.
Tan TW, Png KS, Lee CH, Yuwono A, Yeow Y, Chong KT, et al. MRI Fusion-Targeted Transrectal Prostate Biopsy and the Role of Prostate-Specific Antigen Density and Prostate Health Index for the Detection of Clinically Significant Prostate Cancer in Southeast Asian Men. J Endourol. 2017;31:1111–6.
Zhang K, Chen R, Alberts AR, Zhu G, Sun Y, Roobol MJ. Distribution of Prostate Imaging Reporting and Data System score and diagnostic accuracy of magnetic resonance imaging-targeted biopsy: comparison of an Asian and European cohort. Prostate Int. 2019;7:96–101.
Kimura T. East meets West: ethnic differences in prostate cancer epidemiology between East Asians and Caucasians. Chin J Cancer. 2012;31:421–9.
Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12–49.
Yan L, Spitznagel EL. Soy consumption and prostate cancer risk in men: a revisit of a meta-analysis. Am J Clin Nutr. 2009;89:1155–63.
Riaz IB, Islam M, Ikram W, Naqvi SAA, Maqsood H, Saleem Y, et al. Disparities in the Inclusion of Racial and Ethnic Minority Groups and Older Adults in Prostate Cancer Clinical Trials: A Meta-analysis. JAMA Oncol. 2023;9:180–7.
Jeong CW, Lee S, Jung JW, Lee BK, Jeong SJ, Hong SK, et al. Mobile application-based Seoul National University Prostate Cancer Risk Calculator: development, validation, and comparative analysis with two Western risk calculators in Korean men. PLoS ONE. 2014;9:e94441.
Kitagawa Y, Mizokami A, Nakashima K, Koshida K, Shimamura M, Miyazaki K, et al. Clinical outcomes of prostate cancer patients detected by prostate-specific antigen-based population screening in Kanazawa City, Japan. Int J Urol. 2011;18:592–6.
Funding
Supported by the NCI (5R01CA241758-05).
Author information
Authors and Affiliations
Contributions
CBD - Conceptualization, Methodology, Validation, Investigation, Writing – Original Draft, Writing – Review & Editing; NH- Validation, Writing – Review & Editing; MMH- Data Curation, Formal analysis, Writing – Review & Editing; ABM- : Investigation, Data Curation, Writing – Review & Editing; JCH- Conceptualization, Project Administration, Funding Acquisition: EMS- Conceptualization, Supervision, Project Administration, Funding Acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with the principles put forth in the Declaration of Helsinki and the CONSORT checklist. Approval was obtained from the institutional review board at study sites and Biomedical Research of New York (BRANY) 18-02-365. Informed consent was obtained from all patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
IRB: The institutional review board at study sites and Biomedical Research of New York (BRANY) 18-02-365. The study was performed in accordance with the Declaration of Helsinki.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Driscoll, C.B., Handa, N., Huang, M.M. et al. Evaluating PI-RADS lesions and clinically significant prostate cancer in Black and Asian men: a PREVENT randomized clinical trial secondary analysis. Prostate Cancer Prostatic Dis (2025). https://doi.org/10.1038/s41391-025-01057-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41391-025-01057-5
This article is cited by
-
Best of 2025 in prostate cancer and prostatic diseases
Prostate Cancer and Prostatic Diseases (2026)