Abstract
The combination of mobile technologies and social media with Artificial Intelligence (AI) opens new opportunities for multi-modal data generation, analysis, and inference for various health applications. To investigate how these tools are being used for health applications in Africa, we conduct a scoping review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach. We screen 469 articles and synthesize 116. We include 29 studies documenting the use of a broad range of advanced and straightforward machine-learning techniques to study infectious and chronic diseases such as COVID-19 (4 studies, 13.8%), malaria (5, 17.2%), and cervical cancer (2, 6.9%). Countries with high internet and mobile phone penetration have higher representation. Based on identified gaps, we make research and policy recommendations to enhance the contribution of these tools in advancing health in Africa. These include investing in studies on chronic diseases and implementing frameworks to address geographic inequity.
Similar content being viewed by others
Introduction
Mobile phones and social media have been widely adopted in Africa. According to a survey by Further Africa, there were 495 million subscribers to mobile services in sub-Saharan Africa by the end of 2020, with Nigeria, South Africa, and Egypt being the three countries with the highest mobile phone usage1. A 2022 International Telecommunication Union Report noted that 61% of individuals aged ten and above own mobile phones in Africa2. It is projected that by 2025, 50% of sub-Saharan Africans will have access to a mobile phone1. Similarly, internet use increased by 23% between 2019 and 20213, and there were an estimated 384 million users in 20224.
Over the past three decades, mobile phones and social media platforms have been assessed and validated for global health applications5,6. Lee et al. 7 reported the implementation of 487 mHealth programmes in sub-Saharan Africa from 2006 to 2016, with many focused on clinical support, including disease diagnosis, treatment, and management8,9,10,11. Information shared on social media platforms also serves as essential data for understanding public health trends and population behaviours12. Studies have shown that monitoring discussions on the Internet can be helpful for early outbreak detection and gauging public sentiment towards health interventions, such as vaccine hesitancy13,14,15. As observed during the COVID-19 pandemic, platforms like Facebook, Twitter, and WhatsApp proved crucial for public health organizations like the World Health Organization (WHO) to disseminate health information and promote health behaviours16.
While studies using mobile phones and social media for health research in Africa have focused on improving surveillance and forecasting of infectious diseases (such as polio and Ebola), the COVID-19 pandemic spurred the exploration of new applications of these technologies17,18,19. The wealth of digital data originating from Africa—text, images, audio, and video—can be used to study and improve health at individual and population levels. Efficiently processing and gleaning health insights from these large digital datasets requires machine learning (ML) and artificial intelligence (AI). AI involves computer systems performing tasks requiring human intelligence, while ML, a subset of AI, involves computer models and algorithms that learn and improve from data. In Africa, AI and ML adoption offers unique opportunities and challenges due to varied technology infrastructure, data availability, and socio-economic conditions. The integration of AI/ML tools with social media and mobile technologies has the potential to overcome constraints, such as limited healthcare access points and professionals and to bridge gaps in healthcare delivery20. However, effective implementation demands a nuanced understanding of the continent’s distinct cultural, economic, and political landscapes.
Mobile phone applications and social media platforms can be made accessible and affordable. For example, it is straightforward and feasible to set up cost-effective crowdsourcing applications for health data collection using mobile phone applications21. These applications can be designed to function without requiring a continuous internet connection, allowing for offline data accumulation and subsequent upload when connectivity is available in both urban and rural areas. Social media platforms can foster community participation in health initiatives, disease monitoring, and robust public health campaigns. AI tools can ease implementation and create targeted solutions using mobile phones and social media platforms. These applications align with the Sustainable Development Goals 322; they offer a viable, scalable solution to pressing health challenges confronting many African countries. The utility of these digital tools extends to diverse applications, including disease management, diagnosis, and tracking infectious disease trends, which have supported organizations like the U.S. Centers for Disease Control and Prevention and WHO in early outbreak detection and epidemic intelligence, as recognized by the 2005 International Health Regulations23,24,25.
Despite this global progress, we do not know to what extent these tools, specifically mobile phones and social media, have been used in combination with AI for health applications in Africa. Several reviews have focused on mobile phone use and social media applications for health in Africa, including applications for disease surveillance26, diagnosis and treatment27, health literacy28, adolescents’ use of sexual and reproductive health services29, point of care diagnosis30, and challenges with scaling up31, among others. However, none has explicitly focused on how AI has been combined with these technologies.
In this scoping review, we aim to assess how AI/ML methods have been combined with social media and mobile phones to study health and disease dynamics in Africa. This involves assessing the various AI models used; diseases, conditions, and populations studied; types of social media platforms considered; and geographic representation of African countries to help guide future applications. Additionally, we identify shortcomings of current applications and future opportunities for health applications, research priorities, and policy innovations in Africa. Here, we define social media platforms as search engines, Internet forums, microblogging sites, and social networking sites. We also focus on mobile phone use, mobile applications, phone cameras and data, including location and call. Our findings would help decision-makers and researchers recognize the opportunities and possibilities for using these digital tools for equitable access to quality health care and address challenges that impede their use.
Results
We summarize significant findings focusing on study characteristics, health conditions and populations studied, types of AI and ML methods, uses of mobile phones and diversity in social media platforms.
Included studies
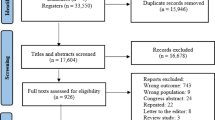
See Fig. 1 and Table SI 1. The search for articles published in the last ten years (January 2014 to January 2023) that met our study criteria yielded 469 articles: EMBASE (105 articles), PubMed Central (248 articles), Web of Science (87 articles), and Google Scholar search (29 articles). After applying our exclusion criteria and abstract screening, 116 articles remained. An additional 87 articles were removed during the full-text synthesis. Most of the excluded articles failed to explicitly mention using data from or being implemented in an African country or region. Some studies used AI or ML but did not use social media or mobile phones. Others mentioned ML and AI, but used other data science methods. One article, “Automatic cervical cancer diagnosis on a smartphone using deep learning method”, was excluded due to inaccessibility. The summary presented in this section covers the remaining 29 articles (SI1 Supplementary References).
Author and location characteristics of studies
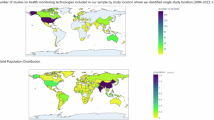
No consistent pattern emerged in the number of relevant papers published within the study period, though publications appear to have increased over time. Studies used data from or were implemented in 21 African countries (Fig. 2a). Ten papers were published in 2021, the highest number in any year and there were yearly variations in the number of studies that used social media or mobile phones (Fig. 2b). At least one country from every African region (i.e., North, South, West, Central, and East) was represented. However, there was a notable concentration of countries with high internet and mobile phone usage, such as South Africa, Nigeria, and Kenya. Approximately 215 authors contributed to the selected 29 papers, and 51 (24%) were affiliated with African institutions (Fig. 2c).
a The number of times each country was included in a study in the review. b The number of studies each year that used social media or mobile phones that were included in the review. All listed studies used AI or ML as mentioned in the study inclusion criteria. c Percentage of authors from African institutions and institutions outside Africa. The half pies are used to emphasize the difference in proportions. The small pie represents 23% of the larger pie.
Characteristics of health conditions and populations studied
The studies addressed various health challenges, including vaccination for pregnant women, infectious disease forecasting, cancer screening, malaria diagnosis, health information seeking and sharing (Table 1). A total of 15 unique diseases or conditions were mentioned, and some studies addressed multiple diseases or conditions. Infectious diseases, including COVID-19 (4 studies, 13.7% of mentions), malaria (5, 17.2%), HIV/AIDS (2, 6.9%), Ebola (3, 10.3%), tuberculosis (2, 6.9%), and influenza-like illnesses (2, 6.9%), were most frequently studied. Two (6.9%) studies focused on detection of cervical cancer. The remaining diseases and conditions were mentioned once: pneumonic plague, diabetes, influenza, maternal health, obesity, polio, schistosomiasis, soil-transmitted helminthiases, Trichuris trichiura, and yellow fever. Studies also focused on health behaviour and healthcare accessibility. Most studies focused on males and females, except three focused on females, one on mosquitoes, and one on drug design.
Characteristics of AI and ML algorithms
The ML and AI methods can be classified across seven broad categories, as detailed in Table 2, which also lists the specific algorithms and platforms used. Deep learning algorithms were used in 9 studies (31%), while supervised learning techniques, including ML regression, were the most common, appearing in 16 studies (55.2%), with regression methods used in 11 studies (38%). Unsupervised learning methods, such as topic modeling, were applied in 4 studies (14%). Spatial modelling and other natural language processing techniques were each used in one study (3.44%).
Within these broader AI and ML categories were 47 algorithms or techniques. The most widely used algorithms included Support Vector Machines (6 studies, 9.8%), Convolutional Neural Networks (5, 8.2%), Latent Dirichlet Allocation (4, 6.5%), K-Nearest Neighbour (2, 3.3%), and Random Forest (2, 3.3%). The remaining algorithms were used once and included other tree-based algorithms (e.g., Boosted Regression Trees), Author-Developed Algorithms, Neural Network Autoregression, Language Models (e.g., RoBerta), and other regression approaches. One study mentioned deep learning without specifying the specific algorithm used.
Characteristics of social media platforms and mobile phone usage
Of the 29 studies, 12 (41.4%), 16 (55.2%), and 1 (3.4 %) used mobile phones, social media, and other tools, respectively. Mobile phones were used as cameras for microscopy, telemedicine, and data collection. Several studies used multiple social media platforms besides news, blogs, and forums. Twitter and Facebook were most frequently used. Nairaland was the only African social media platform that was used. One study mentioned social media, but needed to specify the platform. In addition, 16 (55.2%) of the studies had publicly accessible datasets. Data could be available for 5 (17.2%) studies upon request. Eight (27.6%) studies did not make the data publicly available.
Effectiveness of ML and AI methods
Most studies reported that AI and ML algorithms accomplished the study aims (Table SI 1). However, these conclusions were subjective as studies reported varying values for the same measure, e.g., the reported F1-score could be 0.89 in one study and 0.65 for another. We could not compare across studies due to differences in study aims, data and measures used to assess effectiveness. Measures of performance included accuracy (11, 37.9%), precision (8, 27.6%), area under the curve (7, 24.1%), recall (7, 24.1%), F-score (9, 31.0%), sensitivity (9, 31.0%), and specificity (7, 24.1%). Studies have yet to acknowledge the limitations associated with using individual measures.
Discussion
Study findings and limitations
There is evident interest in using AI/ML, mobile technology, and social media to address various health challenges in Africa. The COVID-19 pandemic contributed to this growing interest by presenting real-time opportunities for developing and testing clinical and public health interventions. Several reviews on the technologies used in the COVID-19 pandemic response in Africa reported the broad application of diverse data (e.g., thermal imaging, GIS, radio data, virus sequencing) and technology (e.g., AI, 3D printing, telehealth, robotics)32,33,34. Similar applications are noted in our review; various simple and complex ML and AI methods are combined with well-known social media platforms and mobile phones for data collection, analysis and inference for disease screening, diagnosis, health behaviour and healthcare accessibility.
However, we observed several issues that could be improved for the effective use of these tools. First is the unequal distribution of research projects across countries, which mirrors more significant disparities in infrastructure and access to technology across the continent. Second, African institutions are underrepresented in the studies we reviewed, highlighting the critical need to invest in African scientists and equitable collaborations and to encourage research applying data science methods to address health problems. Scientists from other regions should only use data from African institutions and countries that provide appropriate credit. Papers calling for the “decolonization of global health”35 have emphasized the need to stop treating African researchers as glorified data collectors and to bridge the representation gap. Third is the notable problem of context incorporation, with some studies indicating limitations due to a lack of engagement with local context and institutions. Studies focused on using data science methods to study African health problems will have little impact without engagement with relevant communities, scientists, clinicians, and institutions36. Fourth, there was an overall lack of discussion on ethical challenges and considerations, which is critical given the known issues associated with using AI/ML to address health and social problems37,38.
Limitations related to disparities in the demographics of individuals represented on social media, data labelling, creation of machine-readable datasets, and ecological fallacies are widely known in AI and ML and are not limited to Africa39. However, a context-specific limitation is the challenge of developing tools that address Africa’s linguistic diversity. While the African machine-learning community is working to develop tools for machine-readable datasets in African languages40, the need for more data collection and analysis tools in most African languages limits the breadth of social media studies. Furthermore, social media and mobile phone use in Africa is uneven, with urban areas having better access and engagement than rural communities, where connectivity, literacy, and cost barriers limit digital inclusion and development41,42.
Gaps and policy recommendations
Based on our findings and the noted gaps, we make specific policy and research recommendations in the sections below regarding the combined use of AI/ML, mobile phones, and social media for health in Africa. These shortcomings may contribute to the underutilization of technological advancements across the continent. To address these issues, we present six critical areas of focus, accompanied by targeted recommendations. Policy changes by different actors across sectors and regions are pivotal in driving the effective use of these technologies to improve health in Africa. These six areas of focus reflect key challenges and opportunities identified through our review of AI/ML use via mobile technology and social media in African health contexts. While these areas may vary in importance depending on specific settings or challenges, they collectively represent foundational elements essential for enabling equitable, effective, and sustainable adoption of these tools. We acknowledge that other areas may emerge as critical in different contexts, and therefore encourage ongoing evaluation and adaptation of priorities as technologies and health systems evolve.
Geographic equity needed in science investments
Studies indicate a disparity in the use of AI/ML and mobile and social media technologies to advance health across Africa. Other reviews on the use of mobile phones and mHealth across Africa have made similar observations43,44. Direct research efforts are needed to build the necessary infrastructure, including computing resources, to support these technologies, especially in regions that are currently underserved. Only an estimated five percent of Africans working on AI have access to needed compute resources45. Some African AI experts have argued that local ownership of these resources is important for several reasons, including data sovereignty, control over sensitive health information, ease of innovation, and the ability to customize infrastructure to meet specific regional needs. The potential public health improvements from such advancements include better disease monitoring, screening, and broader healthcare access, particularly in rural areas. Comprehensive policies supporting equitable resource allocation are also needed to ensure fair distribution of these advancements across the continent46. These policies should foster collaborative engagement between policymakers and the research community, ensuring all countries within Africa benefit equally from scientific and technological progress.
Disparities in diseases and health conditions
While infectious diseases like malaria and COVID-19 have been the focus of published studies that use AI with mobile phones and social media, there is a growing need to apply these methods to better capture the complex adaptive nature of health systems and the increasing burden of non-communicable diseases (NCDs). The application of AI and ML for health in Africa requires a systems approach; one that moves beyond simple linear applications to consider the present realities of the healthcare infrastructure and system level challenges within a specific context. The incidence of and mortality from NCDs like cancer, cardiovascular disease, and type-2 diabetes are increasing in Africa47,48,49. There are opportunities for using AI to screen for and support the treatment of some NCDs, including self-management of specific disorders by enhancing early disease identification and management50. The development of mobile health solutions that can be adapted to areas with restricted internet connection should be prioritized. Researchers can use social media and mobile phones to capture individual and population behaviours, such as eating and exercise patterns, to study and predict risks for disease51. These tools can also nudge at-risk individuals to seek screening and treatment. Policymakers can facilitate the use of these technologies by creating data policies, allocating funding, and other incentives that encourage usage. Furthermore, policymakers, researchers, and clinicians can define how research can be translated into practical clinical and public health applications.
Lack of diversity in social media platforms
The scope of the current studies is mainly restricted to social media sites like Facebook and Twitter. Other platforms, such as WhatsApp and TikTok, are widely used throughout Africa and present substantial opportunities for health promotion. These platforms could be used to generate data and public health-relevant data posted on these platforms can be analyzed. While protecting user privacy and ensuring ethical use, expanding research to include AI data analysis from a broader range of social media platforms could be helpful for many applications. For example, platforms such as WhatsApp, which have been used for public health research in Africa52, could improve the use of social media for targeted public health communication and policy interventions in multiple African languages53. Homegrown platforms like Nairaland are designed to accommodate African languages54,55 and have also been used for public health research56. These platforms could support the development of patient communities actively exchanging culturally aware health practices.
Using a variety of platforms could fill gaps in individual platforms and enable the capture of a diversity of opinions and sentiments for policy decision-making. These studies can include other widely used tools. For example, ML has been combined with radio data for public health surveillance in Uganda57. Mobile money is used to fund healthcare, and analysis of usage patterns can provide insights on behavioural indicators to inform population health interventions. Funders, tech companies, and governments can set up legal frameworks that support the ethical use of social media data in health research, incorporate local perspectives about data sharing, protect user privacy, and maximize the potential of these digital platforms for public health in Africa.
Demystifying science knowledge and communication
The application of AI and social media to improve public understanding and accessibility of scientific and health communications did not receive enough attention in the reviewed studies. For example, although information about vaccine research is publicly available, mistrust of science and misinformation persists online and offline. AI-assisted tools can analyze misinformation prevalent in specific communities and address it with simple, understandable messages, which can remove obstacles to knowledge about disease and health. For example, the WHO collaborated with WhatsApp during the pandemic to address misinformation58,59. This approach can be extended to focus on specific communities, African languages, and diseases. Collaborations between public health authorities and tech companies are not only essential during public health emergencies. They can be used to cultivate a culture in which scientific and health information is shared broadly to increase awareness and trust in science. While AI tools are capable of promoting beneficial public health messages, the same tools can also promote misinformation, which poses complex ethical challenges that require transparent regulation, ethical oversight, and strategies to harness AI’s benefits while mitigating harm.
Digital access to healthcare resources
Telemedicine and drug design were separately mentioned in two studies. Telemedicine was hailed as necessary in increasing access to care during the pandemic60. AI-driven telemedicine can enhance healthcare access and improve preventive care, where Internet services are available. In Kenya, Goodlife Pharmacy has enabled online medication ordering61. Data on medication purchases can be analyzed using AI/ML to gain insights into medication usage, misuse, and allergy patterns. These data can also provide information on adoption and where access gaps remain. Governments can develop policies to regulate the creation and use of these technologies to ensure that these digital healthcare platforms and telemedicine services are robust and secure.
Data sharing for research
As previously noted, some of the studies did not include any authors with affiliations to African institutions. There is a need for more equitable partnerships between African researchers and researchers outside of the continent. Groups that have research data have the power to influence research priorities and policies. Abebe et al. outline several factors that impede data sharing in Africa, including power symmetries, trust, contexts, and local knowledge62. These factors, especially power symmetries and trust, mean public health researchers outside of Africa are more likely to afford the collection and analysis of data to describe health outcomes in Africa. Abebe et al. note that individuals outside the continent increasingly present narratives about the experiences of Africans. Mbaye et al. also noted an under-representation of Africans as first and last authors in papers using data from Africa63. Practices that do not give adequate credit to data collectors and local researchers could hamper research efforts and deprive African researchers from the opportunity to advance their own solutions to local problems.
In this scoping review, we aimed to evaluate the confluence of AI and two important tools shaping health globally—social media and mobile phones—to study health and disease dynamics in Africa. Our findings demonstrate an interest in developing effective solutions that address various health challenges in Africa; however, a systems-level focus and policies to address identified gaps are needed to take advantage of these tools to improve health on the continent. Specifically, we discuss six focal areas, including a need for geographic diversity, limited focus on infectious diseases, lack of diversity in social media platforms, digital literacy and access, and data sharing. Future studies can focus on developing innovative and contextualized approaches that account for current and emerging healthcare system challenges in Africa. Additionally, we have suggested areas where policy can be used to enable the equitable use of these tools across the continent. These insights can guide the adoption of these technologies in African countries and in similar low-resource settings globally. To leverage the full capabilities of these tools, funders and global and national organizations should work together to advance research opportunities and policies.
Methods
Design
We used a scoping review methodology because of the broad research question, the diversity of the study population (i.e., all of Africa), and the need for previous reviews on the topic. The scoping review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) approach extended to scoping reviews as described in Tricco et al.64 The methodological steps included a literature search, removing duplicates and articles not fitting inclusion criteria, screening abstracts, and article synthesis.
Literature search strategy
Our strategy aimed to identify a comprehensive collection of relevant articles from various databases. Relevant search databases were identified, and search strings were defined after consultation with a librarian at Boston University (Boston, MA). The search strings were refined after team discussion (see Box 1). We searched PubMed, Web of Science, and Embase for articles published from January 01, 2014, to January 31, 2023. Google Scholar was used to supplement our search strategy and identify missing articles from the databases, including peer-reviewed papers published in computer science conference proceedings. All articles published in English or other languages with English translations were considered. The articles were uploaded to Rayyan.ai—a systematic review management platform. We screened for and excluded duplicate articles.
Eligibility screening
Inclusion criteria
We applied the following screening criteria: (i) articles were published between January 2014 to January 2023; (ii) mentioned the use of social media and mobile phones for health applications (including the study of infectious diseases, noncommunicable diseases, and health management); (iii) the study involved the use of AI or ML methods; (iv) the article was focused on an African country, region or the entire continent; and (v) the article addressed the research question.
Exclusion criteria
Articles were excluded if they met the following criteria: (i) abstracts, commentaries, editorials, and opinion pieces; (ii) articles that could not be digitally accessed; and (iii) articles that needed to be peer-reviewed, including preprints.
Screening process
Four authors (SB, EON, OO, LV) screened each paper title and abstract to determine if the article met the inclusion criteria. The articles that met the inclusion criteria were included for full-text synthesis. The four authors discussed abstracts tagged as “maybe” or had conflicting labels to reach a consensus. Six reviewers (EON, SB, OO, LV, AO, HD) completed the full-text review and information charting. Each paper was reviewed at least twice; a first reviewer read and extracted details for charting, and a second reviewer verified the accuracy of the extracted information.
Data extraction
To gather evidence to answer the research questions, we extracted data on (i) article information, including number and percentage of authors from African institutions; (ii) study population; (iii) African countries from which data was obtained or where the study was implemented; (iv) whether social media or mobile phones were used in the study; (v) ML or AI methods used in the study; (vi) disease or health condition addressed; (vii) study aims, methods, limitations and significant findings. After discussing the data relevant to answering our research question, we agreed on the evidence to extract. All reviewers (EON, SB, OO, LV, AO, HD) extracted data from fifteen papers except one, who extracted data from fourteen papers. After discussion with project leads (EON, SB), additional articles were excluded during this step. Specifically, some papers mentioned that the research applied to Africa, but did not use data from any African countries. Some were conference abstracts with no accompanying full-text manuscripts. Others were included in the abstract screening because they mentioned social media and mobile phones, but upon full-text review, they did not use ML or AI.
In addition, three reviewers (OO, LV, EON) assessed inconsistencies in terminology and created a table of standard terms. They also evaluated significant characteristics, including the type of ML or AI method used, social media type (e.g., Twitter, Facebook, Google Trends, etc.), how mobile phones were used (e.g., tracking, diagnosis, tool, etc.), disease studied, and African countries listed.
Synthesis of results
To answer the research question, we used descriptive analysis and visualizations to summarize critical observations from our charting tables. We did not perform a meta-analysis because of heterogeneity in the type of studies and populations.
Data availability
This study is based entirely on previously published literature; no new datasets were generated. All data used are cited in the main text and Supplementary Information.
Code availability
Custom R script used for creating Fig. 2a, b are archived at https://github.com/ensoesie/Scoping-Review-of-AI-Mobile-Technology-and-Social-Media-for-Health-in-Africa.
References
FurtherAfrica. African countries with the highest number of mobile phones. Further Africa https://furtherafrica.com/2022/07/19/african-countries-with-the-highest-number-of-mobile-phones/ (2022).
International Telecommunication Union. Facts and Figures 2022 - Mobile phone ownership. https://www.itu.int/itu-d/reports/statistics/2022/11/24/ff22-mobile-phone-ownership (2022).
International Telecommunication Union (ITU) Measuring Digital Development. Facts and Figures. 24. https://www.itu.int/en/ITU-D/Statistics/Documents/facts/FactsFigures2021.pdf (2021).
Saifaddin, G. Social media in Africa - statistics & facts. Statista https://www.statista.com/topics/9922/social-media-in-africa/#topicOverview (2024).
Brownstein, J. S., Freifeld, C. C. & Madoff, L. C. Digital disease detection-harnessing the Web for public health surveillance. N. Engl. J. Med. 360, 2153–5, 2157 (2009).
Yu, V. L. & Madoff, L. C. ProMED-mail: an early warning system for emerging diseases. Clin. Infect. Dis. 39, 227–232 (2004).
Lee, S., Cho, Y. & Kim, S.-Y. Mapping mHealth (mobile health) and mobile penetrations in sub-Saharan Africa for strategic regional collaboration in mHealth scale-up: an application of exploratory spatial data analysis. Global. Health 13, 63 (2017).
Adepoju, I.-O. O., Albersen, B. J. A., De Brouwere, V., van Roosmalen, J. & Zweekhorst, M. mHealth for clinical decision-making in sub-Saharan Africa: a scoping review. JMIR Mhealth Uhealth 5, e38 (2017).
Osei, E., Kuupiel, D., Vezi, P. N. & Mashamba-Thompson, T. P. Mapping evidence of mobile health technologies for disease diagnosis and treatment support by health workers in sub-Saharan Africa: a scoping review. BMC Med. Inform. Decis. Mak. 21, 1–18 (2021).
Aboye, G. T., Vande Walle, M., Simegn, G. L. & Aerts, J.-M. Current evidence on the use of mHealth approaches in sub-Saharan Africa: a scoping review. Health Policy Technol. 12, 100806 (2023).
Hampshire, K. et al. Informal mhealth at scale in Africa: opportunities and challenges. World Dev. 140, 105257 (2021).
Kituyi, G., Engotoit, B. & Abima, B. A study on how social media users in sub-Saharan Africa are learning new health behaviors. https://doi.org/10.37532/jhmm.2020.4(2).116 (2021).
Wiyeh, A. B. et al. Social media and HPV vaccination: unsolicited public comments on a Facebook post by the Western Cape Department of Health provide insights into determinants of vaccine hesitancy in South Africa. Vaccine 37, 6317–6323 (2019).
Ogbuokiri, B. et al. Vaccine hesitancy hotspots in Africa: an insight from geotagged twitter posts. IEEE Trans. Comput. Soc. Syst. 11, 1325–1338 (2024).
Puri, N., Coomes, E. A., Haghbayan, H. & Gunaratne, K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccin. Immunother. 16, 2586–2593 (2020).
Asubiaro, T., Badmus, O., Ikenyei, U., Popoola, B. & Igwe, E. Exploring sub-Saharan Africa’s communication of COVID-19-related health information on social media. Libri 71, 123–139 (2021).
Schaible Braydon, J. et al. Twitter conversations and English news media reports on poliomyelitis in five different countries, January 2014 to April 2015. Perm. J. 23, 18–181 (2019).
Odlum, M. & Yoon, S. Health information needs and health seeking behavior during the 2014-2016 Ebola outbreak: a Twitter content analysis. PLoS Curr. 10, https://doi.org/10.1371/currents.outbreaks.fa814fb2bec36e29b718ab6af66124fa (2018).
Zhang, C. et al. The evolution and disparities of online attitudes toward COVID-19 vaccines: year-long longitudinal and cross-sectional study. J. Med. Internet. Res. 24, e32394 (2022).
Wahl, B., Cossy-Gantner, A., Germann, S. & Schwalbe, N. R. Artificial intelligence (AI) and global health: how can AI contribute to health in resource-poor settings? BMJ Glob. Health 3, e000798 (2018).
Capponi, A., Fiandrino, C., Kliazovich, D., Bouvry, P. & Giordano, S. A cost-effective distributed framework for data collection in cloud-based mobile crowd sensing architectures. IEEE Trans. Sustain. Comput. 2, 3–16 (2017).
World Health Organization (WHO). Sustainable Development Goal 3 “Good Health and Well-Being”. https://www.who.int/tools/your-life-your-health/a-healthy-world/people-s-needs/SDG-3-well-being (2022).
Salathé, M., Freifeld, C. C., Mekaru, S. R., Tomasulo, A. F. & Brownstein, J. S. Influenza A (H7N9) and the importance of digital epidemiology. N. Engl. J. Med. 369, 401–404 (2013).
Shakeri Hossein Abad, Z. et al. Digital public health surveillance: a systematic scoping review. npj Digital Med. 4, 41 (2021).
World Health Organization. International Health Regulations (2005) (World Health Organization, 2008).
Brinkel, J., Krämer, A., Krumkamp, R., May, J. & Fobil, J. Mobile phone-based mHealth approaches for public health surveillance in sub-Saharan Africa: a systematic review. Int. J. Environ. Res. Public Health 11, 11559–11582 (2014).
Osei, E. & Mashamba-Thompson, T. P. Mobile health applications for disease screening and treatment support in low-and middle-income countries: a narrative review. Heliyon 7, e06639 (2021).
Ismaila, O., Some, B. M. J., Benedikter, R. & Diallo, A. G. Improving health literacy in rural Africa through mobile phones: a systematic literature review. J. Health Inform. Afr. 8, 26–31 (2022).
Onukwugha, F. I. et al. The effectiveness and characteristics of mHealth interventions to increase adolescent’s use of sexual and reproductive health services in sub-Saharan Africa: a systematic review. PLoS ONE 17, e0261973 (2022).
Osei, E., Nkambule, S. J., Vezi, P. N. & Mashamba-Thompson, T. P. Systematic review and meta-analysis of the diagnostic accuracy of mobile-linked point-of-care diagnostics in sub-Saharan Africa. Diagnostics 11, 1081 (2021).
Manyati, T. K. & Mutsau, M. A systematic review of the factors that hinder the scale up of mobile health technologies in antenatal care programmes in sub-Saharan Africa. Afr. J. Sci. Technol. Innov. Dev. 13, 125–131 (2021).
Maharana, A., Amutorine, M., Sengeh, M. D. & Nsoesie, E. O. COVID-19 and beyond: use of digital technology for pandemic response in Africa. Sci. Afr. 14, e01041 (2021).
Mbunge, E., Batani, J., Gaobotse, G. & Muchemwa, B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: a systematic review. Glob. Health J. 6, 102–113 (2022).
Bakibinga-Gaswaga, E., Bakibinga, S., Bakibinga, D. B. M. & Bakibinga, P. Digital technologies in the COVID-19 responses in sub-Saharan Africa: policies, problems and promises. Pan Afr. Med. J. 35, 38 (2020).
Abebe, R. et al. Narratives and counternarratives on data sharing in Africa. In Proc. 2021 ACM Conference on Fairness, Accountability, and Transparency 329–341 (Association for Computing Machinery, 2021).
Igumbor, J. O. et al. Considerations for an integrated population health databank in Africa: lessons from global best practices. Wellcome Open Res. 6, 214 (2021).
Naik, N. et al. Legal and ethical consideration in artificial intelligence in healthcare: who takes responsibility? Front. Surg. 9, 862322 (2022).
Gerke, S., Minssen, T. & Cohen, G. Ethical and legal challenges of artificial intelligence-driven healthcare. In Artificial Intelligence in Healthcare 295–336. https://doi.org/10.1016/B978-0-12-818438-7.00012-5 (Elsevier, 2020).
Micheli, M., Hupont, I., Delipetrev, B. & Soler-Garrido, J. The landscape of data and AI documentation approaches in the European policy context. Ethics Inf. Technol. 25, 56 (2023).
Siminyu, K. et al. Consultative engagement of stakeholders toward a roadmap for African language technologies. Patterns 4, 100820 (2023).
Digital Inclusion Playbook 2.0. United Nations Development Programme (UNDP). https://www.undp.org/sites/g/files/zskgke326/files/2024-09/digital_inclusion_playbook_2.0.pdf.
Bakibinga, P., Matanda, D. & Bakibinga, E. Case study of prospects of digital health for Africa in Nairobi, Kenya. Urban Health Africa 302, 302–322 (John Hopkins University Press, 2025).
Doyle, A. M. et al. Mobile phone access and implications for digital health interventions among adolescents and young adults in Zimbabwe: cross-sectional survey. JMIR mHealth uHealth 9, e21244 (2021).
Okano, J. T., Ponce, J., Krönke, M. & Blower, S. Lack of ownership of mobile phones could hinder the rollout of mHealth interventions in Africa. Elife 11, e79615 (2022).
Tsado, A. & Lee, C. Only five percent of Africa’s AI talent has the compute power it needs. UNDP Digital. https://www.undp.org/digital/blog/only-five-percent-africas-ai-talent-has-compute-power-it-needs#:~:text=The%20gap%20in%20compute%20access,capacity%20than%20the%20first%20group (2024).
Erondu, N. A. et al. Open letter to international funders of science and development in Africa. Nat. Med. 27, 742–744 (2021).
Twagirumukiza, M. et al. Current and projected prevalence of arterial hypertension in sub-Saharan Africa by sex, age and habitat: an estimate from population studies. J. Hypertension 29, 1243–1252 (2011).
Motala, A. A., Mbanya, J. C., Ramaiya, K., Pirie, F. J. & Ekoru, K. Type 2 diabetes mellitus in sub-Saharan Africa: challenges and opportunities. Nat. Rev. Endocrinol. 18, 219–229 (2022).
Rebbeck, T. R. Cancer in sub-Saharan Africa. Science 367, 27–28 (2020).
Tighe, S. A. et al. Toward a digital platform for the self-management of noncommunicable disease: systematic review of platform-like interventions. J. Med. Internet Res. 22, e16774 (2020).
Mogo, E. R. I. et al. The other pandemic: social media engagement around non-communicable disease preventive behaviours during Nigeria’s COVID-19 lockdowns. Cities Health 7, 563–572 (2023).
Winters, M. et al. Debunking highly prevalent health misinformation using audio dramas delivered by WhatsApp: evidence from a randomised controlled trial in Sierra Leone. BMJ Glob. Health 6, e006954 (2021).
Olaoye, A. & Onyenankeya, K. A systematic review of health communication strategies in sub-Saharan Africa-2015-2022. Health Promot Perspect. 13, 10–20 (2023).
Nelson, O., Loto, G. & Omojola, O. Blogging, civic engagement, and coverage of political conflict in Nigeria: a study of nairaland.com. Kasetsart J. Soc. Sci. 39, 291–298 (2018).
Uwalaka, T. Nairaland and the Reconstruction of the Public Sphere in Nigeria. Australian and New Zealand Communication Association Conference, Rethinking Communication, Space and Identity, University of Canterbury, Queenstown, Aotearoa New Zealand, 1–13 (2016).
Aduragba, O. T., Yu, J., Cristea, A. & Long, Y. Improving health mention classification through emphasising literal meanings: a study towards diversity and generalisation for public health surveillance. Proc. ACM Web Conf. 2023, 3928–3936 (2023).
UN Global Pulse. When Old Technology Meets New: How UN Global Pulse is Using Radio and AI to Leave No Voice Behind. https://medium.com/un-global-pulse/when-old-technology-meets-new-how-un-global-pulse-is-using-radio-and-ai-to-leave-no-voice-behind-da58ab6466b1 (2023).
WhatsApp. The World Health Organization launches WHO Health Alert on WhatsApp. https://www.whatsapp.com/coronavirus/who.
WHO partners with WhatsApp, Facebook and Viber to bring most up to date and accurate information to billions of people. https://www.who.int/news-room/feature-stories/detail/who-partners-with-whatsapp-facebook-and-viber-to-bring-most-up-to-date-and-accurate-information-to-billions-of-people.
Omboni, S. et al. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connected Health https://doi.org/10.20517/ch.2021.03 (2022).
Goodlife Pharmacy Kenya. https://www.goodlife.co.ke/.
Abebe, R., Hill, S., Vaughan, J. W., Small, P. M. & Schwartz, H. A. Using search queries to understand health information needs in Africa. Proc. Int. AAAI Conf. Web Soc. Media 13, 3–14 (2019).
Mbaye, R. et al. Who is telling the story? A systematic review of authorship for infectious disease research conducted in Africa, 1980–2016. BMJ Glob. Health 4, e001855 (2019).
Tricco, A. C. et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473 (2018).
Parham, G. P. et al. Validation in Zambia of a cervical screening strategy including HPV genotyping and artificial intelligence (AI)-based automated visual evaluation. Infect. Agents Cancer 18, 61 (2023).
Movahedi Nia, Z. et al. Off-label drug use during the COVID-19 pandemic in Africa: topic modelling and sentiment analysis of ivermectin in South Africa and Nigeria as a case study. J. R. Soc. Interface 20, 20230200 (2023).
Maturana, C. R. et al. iMAGING: a novel automated system for malaria diagnosis by using artificial intelligence tools and a universal low-cost robotized microscope. Front. Microbiol. 14, 1240936 (2023).
Kabukye, J. K. et al. Implementing smartphone-based telemedicine for cervical cancer screening in Uganda: qualitative study of stakeholders’ perceptions. J. Med. Internet Res. 25, e45132 (2023).
Turon, G. et al. First fully-automated AI/ML virtual screening cascade implemented at a drug discovery centre in Africa. Nat. Commun. 14, 5736 (2023).
Fredriksson, A. et al. Machine learning for maternal health: Predicting delivery location in a community health worker program in Zanzibar. Front. Digit. Health 4, 855236 (2022).
Ogbuokiri, B. et al. Public sentiments toward COVID-19 vaccines in South African cities: an analysis of Twitter posts. Front. Public Health 10, 987376 (2022).
Dacal, E. et al. Mobile microscopy and telemedicine platform assisted by deep learning for the quantification of Trichuris trichiura infection. PLoS. Negl. Trop. Dis. 15, e0009677 (2021).
Gbashi, S. et al. Systematic delineation of media polarity on COVID-19 vaccines in Africa: computational linguistic modeling study. JMIR Med Inform. 9, e22916 (2021).
Bruzelius, E. et al. Satellite images and machine learning can identify remote communities to facilitate access to health services. J. Am. Med. Inform. Assoc. 26, 806–812 (2019).
Kraemer, M. U. et al. Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus. Nat. Microbiol. 4, 854–863 (2019).
Rosado, L., Da Costa, J. M. C., Elias, D. & Cardoso, J. S. Mobile-based analysis of malaria-infected thin blood smears: automated species and life cycle stage determination. Sensors 17, 2167 (2017).
Fast, S. et al. Predicting social response to infectious disease outbreaks from internet-based news streams. Ann. Oper. Res. 263, 551–564 (2017).
Oyebode, O. & Orji, R. Detecting factors responsible for diabetes prevalence in nigeria using social media and machine learning. In 2019 15TH International Conference on Network and Service Management (CNSM) 1–4 (Halifax, NS, Canada, IEEE, 2019).
Zhao, O. et al. Convolutional neural networks to automate the screening of malaria in low-resource countries. PEERJ 8, e9674 (2020).
Oladeji, O. et al. Monitoring information-seeking patterns and obesity prevalence in Africa with internet search data: observational study. JMIR Public Health Surveill. 7, e24348 (2021).
Yang, A. et al. Kankanet: an artificial neural network-based object detection smartphone application and mobile microscope as a point-of-care diagnostic aid for soil-transmitted helminthiases. PLoS Negl. Trop. Dis. 13, e0007577 (2019).
Mejía, K., Viboud, C. & Santillana, M. Leveraging Google search data to track influenza outbreaks in Africa [version 1; peer review: 1 approved, 1 not approved]. Gates Open Res. 3, 1653 (2019).
Aiken, E. L. et al. Real-time estimation of disease activity in emerging outbreaks using internet search information. PLoS Comput. Biol. 16, e1008117 (2020).
Nsoesie, E. O., Oladeji, O., Abah, A. S. A. & Ndeffo-Mbah, M. L. Forecasting influenza-like illness trends in Cameroon using Google Search Data. Sci. Rep. 11, 1–11 (2021).
Olukanmi, S. O., Nelwamondo, F. V. & Nwulu, N. I. Utilizing Google search data with deep learning, machine learning and time series modeling to forecast influenza-like illnesses in South Africa. IEEE Access 9, 126822–126836 (2021).
Tudor, C. & Sova, R. Infodemiological study on the impact of the COVID-19 pandemic on increased headache incidences at the world level. Sci. Rep. 12, 10253 (2022).
Adamu, H. et al. Framing Twitter public sentiment on Nigerian government COVID-19 palliatives distribution using machine learning. Sustainability 13, 3497 (2021).
Majam, M. et al. Utility of a machine-guided tool for assessing risk behaviour associated with contracting HIV in three sites in South Africa. Inform. Med. Unlocked 37, 101192 (2023).
Maffioli, E. M. & Gonzalez, R. Are socio-demographic and economic characteristics good predictors of misinformation during an epidemic?. PLoS Glob. Public Health 2, e0000279 (2022).
Potgieter, A. et al. Modelling representative population mobility for COVID-19 Spatial transmission in South Africa. Front. Big Data 4, 718351 (2021).
Acknowledgements
This manuscript is a part of a broader writing project on the State of Data Science for Health in Africa (https://bit.ly/StateDataSciAfrica). The project is led by three Scientific Co-Chairs, Catherine Kyobutungi of the African Population and Health Research Center (APHRC, Kenya), Emile R. Chimusa of the Northumbria University Newcastle (United Kingdom), and A. Kofi Amegah of the University of Cape Coast (Ghana). The project is coordinated and supported by the Center for Global Health Studies at the Fogarty International Center, U.S. National Institutes of Health (NIH), the African Population and Health Research Center (APHRC), Wellcome through Grant No. 228261/Z/23/Z, and the Bill & Melinda Gates Foundation through Grant No. INV-058418, in collaboration with other partner organizations. We would like to thank Hesborn Wao (APHRC), Marta Vicente-Crespo, and Fannie Kachale for their insightful feedback during the APHRC retreats. We are also grateful to Nicholas Ekow Thomford, Ruthbetha Kateule, Kristen Sheridan, and Richard Kimera for their valuable input at the start of the project.
Author information
Authors and Affiliations
Contributions
Conceptualization (S.B., E.O.N., V.M., H.D., A.P.O., F.K.). Data Extraction & Curation (S.B., E.O.N., H.D., A.P.O., L.V., O.O.). Visualization (S.B., E.O.N., L.V., O.O.). Writing Original Draft (S.B., E.O.N., L.V., O.O., H.D.). Writing–Review & Editing (S.B., E.O.N., V.M., H.D., A.P.O., F.K., L.V., O.O.). Supervision & Project Administration (S.B., E.O.N.).
Corresponding authors
Ethics declarations
Competing interests
All authors declare that they have no non-financial competing interests as defined by Nature Portfolio, or other interests that might be perceived to influence the interpretation of the article.
Peer review
Peer review information
Nature Communications thanks Humphrey Karamagi, who co-reviewed with Anabay Mamo, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Baichoo, S., Oladeji, O., Villareal, L. et al. Scoping review of artificial intelligence via mobile technology and social media for health in Africa. Nat Commun 16, 11288 (2025). https://doi.org/10.1038/s41467-025-64766-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-64766-4