Abstract
Nocturia can be caused by urological disorders and systemic diseases, including heart diseases. We aimed to investigate the relationship between nocturia and structural abnormalities on echocardiography. Adult patients who underwent echocardiography for cardiac symptoms or heart murmur or had a history of structural heart disease were included. The voiding times during sleep hours were collected prospectively. Univariate and multivariate analyses were performed to evaluate the predictive value of bothersome nocturia (nocturia ≥ 2) on echocardiographic abnormalities. Of 299 patients, 182 (60.9%) reported bothersome nocturia. In patients aged ≥ 65 years, hypertension and left atrial enlargement (LAE) were associated with higher occurrences of bothersome nocturia. On multivariate analysis, bothersome nocturia was a predictive factor of LAE (odds ratio [OR] 2.453, 95% confidence interval [CI] 1.363–4.416, p = 0.003). Moreover, bothersome nocturia could predict both LAE and left ventricular hypertrophy (LVH) (OR 2.285, 95% CI 1.151–4.536, p = 0.018; OR 2.056, 95% CI 1.025–4.124, p = 0.043) in the elderly. Older age, hypertension, and LAE were risk factors for bothersome nocturia. Moreover, bothersome nocturia was predictive of LAE and LVH in the elderly. Patients with bothersome nocturia without other significant lower urinary tract symptoms should be referred to cardiologists.
Similar content being viewed by others
Introduction
Nocturia is the most common and troublesome lower urinary tract symptom (LUTS)1. Nocturia prevalence ranges from 11 to 35.2% in young men and 20.4% to 43.9% in young women. Moreover, the prevalence is between 68.9 and 93% in the elderly population2. Nocturia is associated with poor quality of life and increased morbidity3. Furthermore, nocturia is strongly associated with depression4 and leads to a higher risk of incident falls in the elderly5. In addition to urological disorders, nocturia is also caused by systemic diseases6. Previous studies have reported that heart failure and uncontrolled hypertension were responsible for clinically significant nocturia7,8. Other cardiac diseases may also contribute to nocturia. One study revealed that electrocardiographic evidence of left ventricular hypertrophy (LVH) and left atrial enlargement (LAE) were significantly associated with nocturia9. However, to the best of our knowledge, no studies have so far thoroughly evaluated the association between structural cardiac abnormalities and nocturia. We, thus, investigated the relationship between nocturia and structural abnormalities on cardiac sonography.
Materials and methods
The study was approved by the Institutional Review Board of Taipei City Hospital (approval number: TCHIRB-11002002) and performed in accordance with the guidelines of the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from all patients.
We prospectively included adult patients from the cardiology outpatient department who underwent cardiac sonography between June 1, 2021, and July 31, 2021. Cardiac sonography was undertaken for clinical symptoms like chest pain or tightness, physical examination with heart murmur, or follow-up of structural heart disease. Patients with urinary tract infection, neurogenic bladder, or a prior history of lower urinary tract or pelvic surgery were excluded. Before the echocardiographic examination, nocturia was assessed using Question 7 of the International Prostate Symptom Score (IPSS) questionnaire “How many times did you typically get up at night to urinate?”. The patients’ basic data included age, body mass index (BMI), and presence of comorbidities, such as diabetes mellitus, hypertension, heart failure and cardiomyopathy. Elderly patients were defined as those aged ≥ 65 years. BMI ≥ 25 kg/m2 was defined as obesity in the Asian population10.
The 2018 International Continence Society (ICS) defines nocturia as waking for passing urine during the main sleep hours11. Previous literature showed that the majority of people report being troubled when the number of nocturia episodes is ≥ 2 and that over two voids per night is associated with impaired health-related quality of life12. Therefore, we classified the participants into two groups based on the number of nocturia episodes: bothersome nocturia (nocturia ≥ 2) vs non-bothersome nocturia (nocturia ≤ 1).
Cardiac sonography was performed by a single technician and interpreted by a cardiologist. A cardiologist has validated this cardiac sonography report. All three cardiac staff were blinded to the patients’ nocturia conditions. The performance and measurements of echocardiographic parameters were based on the 2015 recommendations of chamber quantification of the American Society of Echocardiography (ASE) and the European Association of Cardiovascular Imaging (EACVI)13. Echocardiological parameters, including the size of the left atrium (LA), left ventricle (LV), aorta, aortic valve (AV), mitral valve (MV), tricuspid valve (TV), and pulmonary valve (PV), were measured. The aortic valve sinus diameter, interventricular septal thickness at end-diastole (IVSd), left ventricular posterior wall thickness at end-diastole (LVPWd), left ventricular internal diameter in diastole (LVIDd), and left ventricular internal diameter in systole (LVIDs) were recorded. Left ventricular systolic and diastolic function and valve regurgitation were also measured using Doppler echocardiography.
Left ventricular ejaction fraction (LVEF) was calculated using the Simpson’s biplane method. In males, the normal LVEF range was 52–72%, mildly abnormal was 41–51%, moderately abnormal was 30–40%, and severely abnormal was less than 30%. In females, the normal range was 54–74%, mildly abnormal was 41–53%, moderately abnormal was 30–40%, and severely abnormal was less than 30%13. LV diastolic dysfunction (LVDD) was measured by mitral valve E velocity divided by A-wave velocity (E/A ratio) and mitral valve E velocity divided by mitral annular e′velocity (average E/e’ ratio), and the normal range was E/A ≥ 0.8 and E/e’ ratio < 10, grade I was E/A ≤ 0.8 and E/e’ ratio < 10, grade II was E/A > 0.8 to < 2 and E/e’ ratio 10–14, and grade III was E/A > 2 and E/e’ ratio > 1414. Left atrial enlargement (LAE) was defined as a left atrial dimension of > 40 mm15. Aortic root dilation was defined as an aortic valve sinus diameter > 38 mm in men and > 36 mm in women16. Left ventricular mass (LVM) was calculated using the following formula: LVM = 0.8 × [1.04 × {(LVIDd + LVPWd + IVSd)3- (LVIDd)3}] + 0.6 g17. The left ventricular mass index (LVMI) was calculated by normalizing the LVM by the body surface area based on Devereux’s formula18. Left ventricular hypertrophy (LVH) was defined as an increased left ventricular mass index (LVMI) (≥ 125 g/m2 in men and ≥ 110 g/m2 in women)19. Concentric LV remodeling was defined as LVMI ≤ 115 g/m2 in men or ≤ 95 g/m2 in women and LV relative wall thickness (RWT) > 0.4220. Moderate-to-severe AV regurgitation (AR) was considered to have intermediate-to-large color flow in AR jet width, increment vena contracta width (> 3 mm), and a decrease in pressure half-time (< 500 ms). Moderate-to-severe TV regurgitation (TR), MV regurgitation (MR), and PV regurgitation (PR) were defined as intermediate-to-large color flows in the TR, MR, and PR jet widths and dense continuous wave signals of the TR, MR, and PR jets, respectively21.
Statistical analyses were performed using IBM SPSS Statistics for Macintosh, ver. 24 (IBM Corp., Armonk, NY, USA). Pearson’s chi-square test was used to analyze factors associated with bothersome nocturia. Univariate and multivariate analyses were performed with logistic regression to evaluate the predictive value of bothersome nocturia on echocardiographic abnormalities after adjusting for sex, age, obesity, hypertension, diabetes mellitus, diuretic use and heart disease. Statistical significance was set at p < 0.05.
Results
A total of 299 patients aged between 20 and 95 years were included in the study, of whom 134 (44.8%) were men and 165 (55.2%) were women. Elderly patients accounted for 70.6%, while patients with obesity accounted for 50.8%. Hypertension was found in 226 (75.6%) patients, and 4 (1.3%) patients had a history of heart diseases, including three with heart failure and one with cardiomyopathy. Bothersome nocturia was reported in 182 patients (60.9%). Regarding echocardiographic abnormalities, 27 (9%) had abnormal LVEF, 10 (3.3%) had grade II-III LV diastolic dysfunction, 109 (36.5%) had LAE, and 85 (28.4%) patients had LVH (Table 1).
Among all patients, those older than 65 years of age were found to have higher occurrences of bothersome nocturia (69.2% vs. 40.9%, p < 0.001). Patients with hypertension (64.2% vs. 50.7%, p = 0.040) and LAE (73.4% vs. 53.7%, p = 0.001) also had higher occurrences of bothersome nocturia. Additionally, there was a tendency for patients with LVH to have higher occurrences of bothersome nocturia with a borderline significance (69.4% vs. 57.5%, p = 0.056) (Table 2).
In elderly patients, the prevalence of bothersome nocturia was not associated with increasing age and the presence of hypertension. Similarly, patients with LAE had higher occurrences of bothersome nocturia (77.9% vs. 63.2%, p = 0.024), and those with LVH tended to have higher occurrences of bothersome nocturia with a borderline significance (77.5% vs. 65.0%, p = 0.064). Furthermore, the prevalence of bothersome nocturia was lower in obese patients compared with that in non-obese patients (58.1% vs. 75.7%, p = 0.038) (Table 2).
On multivariate analysis, in addition to age, sex, obesity, hypertension, diabetes mellitus, use of diuretics and heart disease, we also adjusted for LVH in the evaluation of the predictive value of bothersome nocturia on LAE because LVH and LAE are related to each other with respect to diastolic dysfunction. Bothersome nocturia was a predictive factor of LAE (odds ratio [OR], 2.453; 95% confidence interval [CI], 1.363–4.416; p = 0.003). Moreover, in the subgroup of patients older than 65 years, bothersome nocturia was predictive of LAE (OR, 2.285; 95% CI, 1.151–4.536; p = 0.018) and LVH (OR, 2.056; 95% CI, 1.025–4.124, p = 0.043) (Table 3).
Discussion
In the present study, we found that old age, hypertension, and echocardiographic evidence of LAE were significantly associated with a higher prevalence of bothersome nocturia. Moreover, bothersome nocturia was predictive of LAE and LVH, especially in the elderly. To the best of our knowledge, this is the first study to correlate nocturia with echocardiographic evidence of structural heart diseases. Urologists should consider referring patients with bothersome nocturia to cardiologists to evaluate the presence of LAE or LVH.
Nocturia is closely associated with cardiac complications. Nocturia may be a risk factor for coronary heart disease in young men and increases the possibility of death in older men22. Left atrial enlargement is the most significant cardiac abnormality associated with nocturia. This connection has been documented previously and is believed to result from the elevation of atrial natriuretic peptide (ANP) levels in patients with LAE23. A previous study showed that increased ANP due to subclinical heart failure can cause nocturnal urinary symptoms24. ANP increases the glomerular filtration rate (GFR), renal plasma flow, and sodium excretion, which causes diuresis and natriuresis25. Another possible mechanism is that LAE leads to cardiac structural changes and causes sodium and water retention in the extracellular space26. When sleeping in a supine position, the redistribution of fluid from edematous legs may cause nocturnal polyuria27.
Bothersome nocturia was also predictive of LVH in patients older than 65 years. Left ventricular hypertrophy increases the risk of both systolic and diastolic heart failure27. Congestive heart failure may decrease renal plasma flow, increase the filtration fraction during ambulation, and cause sodium retention. Nighttime sleep in the supine position improves renal hemodynamics and sodium excretion, leading to nocturia28.
We found that bothersome nocturia was more prevalent among older adults. This is consistent with the results of previous studies29,30. The incidence and severity of nocturia increase with age in both men and women31. Urological problems and systemic diseases affect nocturia in older patients equally, including bladder storage problems, polyuria, nocturnal polyuria, and sleep-related issues32. Nocturia in the elderly leads to impaired quality of life, for both the patients and their cohabitants, and increases the incidence of falls, resulting in higher morbidity30. Interventions such as behavioral, pharmacological, or surgical management should be considered to improve nocturia severity in the elderly33.
Our study reported that the prevalence of bothersome nocturia was lower in obese patients compared with that in non-obese patients in the elderly patient group, implying a protective role of obesity in the development of bothersome nocturia. In contrast, previous studies demonstrated a positive association between obesity and nocturia. A study that included approximately 3,600 patients in Finland concluded that obesity is strongly associated with increased nocturia34. Another study that analyzed 14135 patients from the National Health and Nutrition Examination Survey in the United States showed that obesity is significantly associated with nocturia35. Our results, which differ from previous studies, may be due to the differences in race, age, and study population. We focused on elderly patients with cardiac symptoms and potential structural heart disease, which may have a stronger negative effect than obesity on nocturia and modify the effect of obesity on nocturia. Moreover, the definitions of obesity based on BMI also differ between Asians and Caucasians36. These disparities could have contributed to the different results.
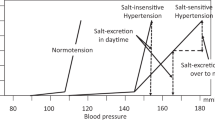
Our study showed a significant relationship between hypertension and bothersome nocturia. Uncontrolled hypertension and elevation of blood pressure are reportedly related to nocturia9,37. Hypertension affects renal glomerular filtration and tubular transport. In addition, hypertension can increase renal plasma flow and decrease sodium reabsorption, leading to nocturia38,39. A previous study indicated a significant relationship between diabetes mellitus and nocturia40. Hyperglycemia and osmotic diuresis occur in patients with diabetes mellitus, predisposing them to nocturia41. Proper control of serum glucose levels in diabetic patients helps improve nocturia41. However, in this study, a history of diabetes mellitus was not significantly associated with bothersome nocturia. One possible explanation is that all patients included in our study received appropriate treatment for blood sugar.
Our study had several limitations. First, we included patients from the cardiology department rather than the general population. The association between bothersome nocturia and echocardiographic abnormalities, especially in those without obvious cardiac symptoms, may be underestimated. Second, although this was a prospective study, we did not analyze the effects of antihypertensive drugs other than diuretics on nocturia. Third, we did not perform prostate ultrasonography to evaluate the size of the prostate gland in male participants, which may also have an impact on the severity of nocturia. Fourth, we did not follow-up with the patients in a cross-sectional study to evaluate the association between nocturia and echocardiographic abnormalities. Fifth, we evaluated LA size using conventional M-mode LA dimension rather than LA volume. Measurement of LA size using conventional M-mode LA dimension is simple and convenient but not reliably accurate, given that the LA is not a symmetrically shaped three-dimensional structure. It is unknown whether treatment of structural heart diseases, such as LAE or LVH, could also improve the severity of nocturia. Nevertheless, the results of this study have important implications. Our results suggest that urologists should refer patients with bothersome nocturia without other significant LUTS to cardiologists to evaluate the presence of structural heart disease, which may be potentially critical to patients.
Conclusion
Older age, hypertension, and echocardiographic evidence of LAE are associated with a higher incidence of bothersome nocturia. Furthermore, bothersome nocturia could predict structural heart diseases, including LAE and LVH, in the elderly. Referral to cardiologists should be considered for patients with bothersome nocturia.
Data availability
Data utilized in our study are available from the Taipei City Hospital. Based on the “Personal Information Protection Act” in Taiwan, data cannot be made publicly available due to legal restrictions imposed by the government of Taiwan. Requests for data can be sent as a formal proposal to the Institutional Review Board of Taipei City Hospital.
References
Welliver, C. et al. Analyzing why men seek treatment for lower urinary tract symptoms and factors associated with nonimprovement. Urology 86, 862–867 (2015).
Bosch, J. L. & Weiss, J. P. The prevalence and causes of nocturia. J. Urol. 184, 440–446 (2010).
Wyndaele, J. J. Nocturia and quality of life. Eur. Urol. 61, 85–87 (2012).
Breyer, B. N. et al. The association of depression, anxiety and nocturia: A systematic review. J. Urol. 190, 953–957 (2013).
Vaughan, C. P. et al. The association of nocturia with incident falls in an elderly community-dwelling cohort. Int. J. Clin. Pract. 64, 577–583 (2010).
Gulur, D. M., Mevcha, A. M. & Drake, M. J. Nocturia as a manifestation of systemic disease. BJU Int. 107, 702–713 (2011).
Redeker, N. S. et al. Nocturia, sleep and daytime function in stable heart failure. J. Card. Fail. 18, 569–575 (2012).
Victor, R. G. et al. Nocturia as an unrecognized symptom of uncontrolled hypertension in black men aged 35 to 49 years. J. Am. Heart. Assoc. 8, e010794 (2019).
Mekki, P. et al. Nocturia and electrocardiographic abnormalities among patients at an inner-city cardiology clinic. Neurourol. Urodyn. 40, 509–514 (2021).
Weir, C. B. & Jan, A. BMI classification percentile and cut off points. In StatPearls [Internet]. (Treasure Island [FL]: StatPearls Publishing 2022).
Hashim, H. & Blanker, M. H. International continence society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol. Urodyn. 38, 499–508 (2019).
Tikkinen, K. A. et al. Nocturia frequency, bother, and quality of life: How often is too often? A population-based study in Finland. Eur. Urol. 57, 488–496 (2010).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 28, 1-39.e14 (2015).
Nagueh, S. F. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the american society of echocardiography and the european association of cardiovascular imaging. J. Am. Soc. Echocardiogr. 29, 277–314 (2016).
Batra, M. K., Khan, A., Farooq, F., Masood, T. & Karim, M. Assessment of electrocardiographic criteria of left atrial enlargement. Asian Cardiovasc. Thorac. Ann. 26, 273–276 (2018).
Roman, M. J., Devereux, R. B., Kramer-Fox, R. & O’Loughlin, J. Two-dimensional echocardiographic aortic root dimensions in normal children and adults. Am. J. Cardiol. 64, 507–512 (1989).
Lang, R. M. et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J. Am. Soc. Echocardiogr. 18, 1440–1463 (2005).
Devereux, R. B. et al. Echocardiographic assessment of left ventricular hypertrophy: Comparison to necropsy findings. Am. J. Cardiol. 57, 450–458 (1986).
Mancia, G. et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 25, 1105–1187 (2007).
Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of, Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging. 17, 412. (2016)
Lancellotti, P. et al. Recommendations for the echocardiographic assessment of native valvular regurgitation: An executive summary from the European Association of Cardiovascular Imaging. Eur. Heart. J. Cardiovasc. Imaging. 14, 611–644 (2013).
Lightner, D. J. et al. Nocturia is associated with an increased risk of coronary heart disease and death. BJU Int. 110, 848–853 (2012).
Roman, M. J. et al. Relationship of atrial natriuretic factor to left ventricular volume and mass. Am. Heart. J. 118, 1236–1242 (1989).
Carter, P. G., Cannon, A., McConnell, A. A. & Abrams, P. Role of atrial natriuretic peptide in nocturnal polyuria in elderly males. Eur. Urol. 36, 213–220 (1999).
Needleman, P. & Greenwald, J. E. Atriopeptin: a cardiac hormone intimately involved in fluid, electrolyte, and blood-pressure homeostasis. N. Engl. J. Med. 314, 828–834 (1986).
Torimoto, K. et al. The relationship between nocturnal polyuria and the distribution of body fluid: Assessment by bioelectric impedance analysis. J. Urol. 181, 219–224 (2009).
Katholi, R. E. & Couri, D. M. Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications. Int. J. Hypertens. https://doi.org/10.4061/2011/495349 (2011).
Vertuno L. L. & Kozeny, G. A. Nocturia in Clinical Methods: The History, Physical, and Laboratory Examinations 3rd edn. (eds. Walker, H.K., Hall, W.D., Hurst, J.W.) (Butterworths, London, 1990).
Kujubu, D. A. & Aboseif, S. R. An overview of nocturia and the syndrome of nocturnal polyuria in the elderly. Nat. Clin. Pract. Nephrol. 4, 426–435 (2008).
Mobley, D. F. & Baum, N. Etiology, evaluation, and management of nocturia in elderly men and women. Postgrad. Med. 126, 147–153 (2014).
Schatzl, G. et al. Cross-sectional study of nocturia in both sexes: analysis of a voluntary health screening project. Urology 56, 71–75 (2000).
Wein, A., Lose, G. R. & Fonda, D. Nocturia in men, women and the elderly: A practical approach. BJU Int. 90, 28–31 (2002).
Kallas, H. E., Chintanadilok, J., Maruenda, J., Donahue, J. L. & Lowenthal, D. T. Treatment of nocturia in the elderly. Drugs Aging. 15, 429–437 (1999).
Tikkinen, K. A., Auvinen, A., Huhtala, H. & Tammela, T. L. Nocturia and obesity: A population-based study in Finland. Am. J. Epidemiol. 163, 1003–1011 (2006).
Moon, S. et al. The association between obesity and the nocturia in the U.S. Popul. Int. Neurourol. J. 23, 169–176 (2019).
Deurenberg, P., Deurenberg-Yap, M. & Guricci, S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes. Rev. 3, 141–146 (2002).
Sugaya, K. et al. Relationship between blood pressure and nocturia in hypertensive patients. LUTS Low Urin. Tract Symptoms 1, 16–19 (2009).
Feldstein, C. A. Nocturia in arterial hypertension: A prevalent, underreported, and sometimes underestimated association. J. Am. Soc. Hypertens. 7, 75–84 (2013).
Koch, K. M., Aynedjian, H. S. & Bank, N. Effect of acute hypertension on sodium reabsorption by the proximal tubule. J. Clin. Investig. 47, 1696–1709 (1968).
Asplund, R. Nocturia in relation to sleep, somatic diseases and medical treatment in the elderly. BJU Int. 90, 533–536 (2002).
Weiss, J. P., Weinberg, A. C. & Blaivas, J. G. New aspects of the classification of nocturia. Curr. Urol. Rep. 9, 362–367 (2008).
Author information
Authors and Affiliations
Contributions
K.W.K. and Y.H.F. conceived and designed the study; C.J.W. and Y.H.F. directed the study including data analysis and interpretation; W.M.C. performed statistical analysis; K.W.K. and W.M.C. wrote the manuscript; Y.H.F. revised it critically for important intellectual content. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kao, KW., Cheng, W., Wu, CJ. et al. Nocturia independently predicts left ventricular hypertrophy and left atrial enlargement among patients with cardiac symptoms. Sci Rep 12, 14897 (2022). https://doi.org/10.1038/s41598-022-19190-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-19190-9
This article is cited by
-
Nocturia: when the heart wakes you up at night
World Journal of Urology (2026)
-
Nocturia and Blood Pressure Elevation in Adolescents
Journal of Community Health (2024)