Abstract
This study aimed to investigate the association between galectin-3 concentration and estimated glomerular filtration rate (eGFR) in patients with type 2 diabetes mellitus (T2DM) with and without albuminuria. In this cross-sectional study, we examined 334 patients with T2DM. The eGFR was calculated using a creatinine-based formula (eGFRcrea) and a combined creatinine-cystatin C equation (eGFRcrea-cyst). The participants were categorized into two groups based on the urinary albumin-to-creatinine ratio (UACR): patients without albuminuria (UACR < 30 mg/g) and those with albuminuria (UACR ≥ 30 mg/g). Greater concentrations of plasma galectin-3 were associated with lower eGFRcrea-cyst and eGFRcrea levels in patients with and without albuminuria. Plasma galectin-3 concentrations were negatively correlated with eGFRcrea-cyst in patients with normoalbuminuria and albuminuria (γ = − 0.405, P < 0.001; γ = − 0.525, P < 0.001, respectively). Galectin-3 concentrations were significantly associated with eGFRcrea-cyst after adjusting for sex, age, and other confounding factors, including UACR as a categorical or continuous variable in multiple regression analyses (β = − 0.294, 95% CI − 70.804 to − 41.768, P < 0.001; β = − 0.265, 95% CI − 65.192 to − 36.550, P < 0.001, respectively). Likewise, when eGFRcrea-cyst was treated in place of eGFRcrea, this result was replicated in the correlation and regression analyses. Galectin-3 concentration was negatively associated with eGFR in patients with T2DM, independent of albuminuria status.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disease that is characterized by chronic hyperglycemia1,2. The prevalence of T2DM is increasing, with a substantial burden on clinical and public health owing to its complications1. Chronic hyperglycemia plays a pivotal role in progressive end-organ damage in patients with T2DM2. Diabetic nephropathy is a common microvascular complication and an important cause of end-stage kidney disease, which may require dialysis or kidney transplantation2. A large body of evidence demonstrates that albuminuria is an important risk factor for progressive kidney failure and cardiovascular disease in patients with T2DM3,4,5,6. In addition, reduced glomerular filtration rate (GFR) has been suggested to be independently linked to the risk of detrimental cardiovascular and kidney outcomes in patients with T2DM3,7.
According to the traditional view, the natural history of diabetic nephropathy is characterized by a progressive increase in urinary albumin excretion from normoalbuminuria to microalbuminuria and, subsequently, to macroalbuminuria8,9. Furthermore, progression from microalbuminuria to macroalbuminuria is assumed to initiate renal function loss9. However, recent evidence suggests that an initial decline in GFR can occur in the setting of normal urinary albumin excretion10, indicating that albuminuria may not be a sensitive marker for early diabetic nephropathy11. Autopsy studies of patients with diabetes suggest that diabetes-related histopathological lesions in the kidney occur before the onset of albuminuria11,12,13. Therefore, in a clinical setting, it is crucial to identify the factors with implications for early kidney damage in patients with diabetes.
Galectin‐3, which belongs to the galectin family, is a β-galactoside‐binding protein mainly composed of a C-terminal carbohydrate-recognition domain and an N-terminal domain14. Galectin-3 is ubiquitously expressed in various cells and tissues and secreted into the bloodstream14. Its structural property allows galectin-3 to bind several proteins, thus exerting multiple context-dependent biological functions14,15. Recently, galectin-3 has been implicated in inflammation and fibrosis14,15. In addition, galectin-3 is linked to tissue injury at an early stage16. In a preclinical study, galectin-3 was found to be associated with renal injury17. Galectin-3 expression was rapidly up-regulated in models of renal damage18. In community-based studies, elevated concentrations of plasma galectin-3 were associated with an increased risk of chronic kidney disease19. In a renal biopsy-based study, plasma galectin-3 concentrations were positively correlated with renal fibrosis and inversely correlated with eGFR20. In addition, a longitudinal study of patients with T2DM showed that high concentrations of galectin-3 were associated with a doubling of serum creatinine levels and incident macroalbuminuria. However, little is known about the contribution of galectin-3 to early renal function decline in patients with T2DM and normoalbuminuria.
Therefore, this study aimed to evaluate the relationship between galectin-3 concentration and eGFR in patients with T2DM with and without albuminuria.
Results
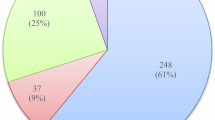
Table 1 summarizes the characteristics of the patients with T2DM in this study. Patients with albuminuria had higher systolic blood pressure, a longer duration of diabetes, higher A1C levels, higher triglyceride levels, and a higher prevalence of use of insulin and angiotensin converting enzyme inhibitors (ACEi)/angiotensin II receptor blockers (ARB). The eGFRcrea-cyst and eGFRcrea were significantly lower in patients with albuminuria than in those with normoalbuminuria. In addition, plasma galectin-3 concentrations were significantly higher in patients with albuminuria than those in patients with normoalbuminuria.
We subdivided patients with T2DM into with and without albuminuria at an overall median galectin-3 level of 8.73 ng/mL (Tables 2, 3). In both groups, higher concentrations of galectin-3 were associated with older age, longer duration of diabetes, and higher UACR (Tables 2, 3). In addition, higher concentrations of galectin-3 were associated with lower eGFRcrea-cyst and eGFRcrea.
Pearson’s correlation coefficients between plasma galectin-3 concentrations and eGFR are shown in Fig. 1. Negative correlations were observed between plasma galectin-3 and eGFRcrea-cyst in patients with normoalbuminuria (γ = − 0.405, P < 0.001) and albuminuria (γ = − 0.525, P < 0.001). Likewise, plasma galectin-3 concentrations were negatively correlated with eGFRcrea in patients with normoalbuminuria (γ = − 0.341, P < 0.001) and albuminuria (γ = − 0.466, P < 0.001).
Correlation between galectin-3 concentrations and estimated glomerular filtration rate in patients with T2DM with normoalbuminuria and albuminuria. A Correlation between galectin-3 concentrations and eGFRcrea-cyst. B Correlation between galectin-3 concentrations and eGFRcrea. eGFR estimated glomerular filtration rate, T2DM type 2 diabetes mellitus.
We evaluated the relationship between plasma galectin-3 concentration and eGFR in all patients with T2DM using linear regression models (Table 4). In multiple regression analyses, galectin-3 concentrations were significantly associated with eGFRcrea-cyst after adjusting for sex, age, body mass index, smoking, hemoglobin, duration of diabetes, A1C, hyperlipidemia, hypertension, and use of oral hypoglycemic agents (OHAs) and insulin (β = − 0.311, 95% confidence interval [CI] − 74.501 to − 44.854, P < 0.001). Furthermore, the significant relationship persisted after adjusting for UACR as a categorical variable (β = − 0.294, 95% CI − 70.804 to − 41.768, P < 0.001; Model 3a) and continuous measure (β = − 0.265, 95% CI − 65.192 to − 36.550, P < 0.001; Model 3b). Likewise, the results were replicated for eGFRcrea in the multiple regression analyses (Table 4). Alternatively, when systolic blood pressure, total cholesterol, and use of ACEi/ARB, statin and sodium-glucose cotransporter 2 inhibitors were included as independent variables in the models and hypertension, hyperlipidemia, and use of OHAs were excluded, plasma galectin-3 concentrations were still associated with eGFR (Supplementary Table 1). Additionally, when patients with use of glucagon-like peptide-1 receptor agonists (n = 2) were excluded in the analyses, almost identical results were found in multiple regression analyses (data not shown).
Discussion
In this study, we found that galectin-3 concentration was negatively associated with eGFR in patients with T2DM. Moreover, this association was independent of albuminuria status. Because galectin-3 is related to tissue injury14,16, our findings suggest a possible role of galectin-3 as an indicator of early diabetic nephropathy in patients with T2DM.
Galectin-3 has recently emerged as a modulator of several biological processes, including adhesion, proliferation, differentiation, and apoptosis14. In addition, galectin-3 levels have been suggested to increase following tissue damage and inflammatory stimuli15. Previous investigations on the association between galectin-3 and cardiovascular disease indicated that galectin-3 concentrations in circulation might be a potential biomarker for cardiovascular disease21. This speculation has been verified by a number of clinical studies showing that higher circulating concentrations of galectin-3 are associated with an increased risk of heart failure, coronary artery disease, ischemic stroke, and cardiovascular mortality21,22,23.
Recent data have suggested a close relationship between galectin-3 concentration and an increased risk of diabetes24,25,26. Increased circulating concentrations of galectin-3 are found in patients with T2DM compared with those without T2DM24. Vora et al.27 reported that galectin-3 concentration is positively associated with incident T2DM. In addition, mounting evidence suggests that galectin-3 is involved in the development of kidney disease19. In experimental studies, renal galectin-3 expression was found to increase after kidney injury17. An increase in circulating galectin-3 concentration has been linked to renal injury in humans19. In community-based population studies, elevated galectin-3 concentrations were found to be associated with the development of chronic kidney disease19,28,29. In addition, Tan et al.30 showed that galectin-3 concentration was associated with a twofold increase in serum creatinine levels and incident macroalbuminuria in a longitudinal study of patients with T2DM. In addition, high concentrations of galectin-3 are associated with worsening albuminuria in patients with T2DM31. Our data indicated that galectin-3 concentrations were inversely associated with eGFR in patients with T2DM and albuminuria, in agreement with previous findings30. Furthermore, we noticed a close association between galectin-3 concentration and eGFR in patients with T2DM with normoalbuminuria. To date, the relationship between galectin-3 and eGFR in patients with T2DM with normoalbuminuria has not been fully understood. Classically, an initial increase in urinary albumin excretion is presumed to precede a decrease in GFR9,32. However, recent studies have suggested that a decrease in GFR may begin earlier32,33. Consequently, the findings of this study suggest that increased concentrations of galectin-3 might be implicated in kidney injury in patients with T2DM, independently of albuminuria status.
Galectin-3 concentrations have been suggested to be associated with age30. In addition, several studies have reported that galectin-3 concentration is associated with glycemic status in patients with T2DM30,31. Similarly, plasma galectin-3 concentrations in the present study were associated with diabetes duration, reflecting the total glycemic control over time34. Because these elements are also involved in renal dysfunction35, the relationship between galectin-3 concentration and eGFR in the present study might be affected by these factors. However, in multivariable analysis, the association between galectin-3 concentrations and eGFR remained significant after adjusting for these confounders, thus implying that these factors did not significantly influence the relationship between galectin-3 concentrations and eGFR.
Despite a strong association between galectin-3 concentration and renal function loss in diabetes, the exact mechanism underlying the association is controversial. Galectin-3 is a potent activator of fibroblasts and may contribute to renal fibrosis19. Renal fibrosis is associated with loss of renal function in diabetes2. Pharmacological inhibition of galectin-3 attenuates hypertensive nephropathy in rodent models36. A phase II study using a galectin-3 inhibitor suggested an improvement in eGFR in patients with chronic kidney disease37. However, a contrasting role for galectin-3 in the kidneys has also been reported19. Advanced glycation end products (AGEs) are important contributors to the development of diabetic nephropathy38. Galectin-3 has a high binding affinity for AGEs39 and has been suggested to participate in the degradation of AGEs19. Studies using knockout mouse models have shown that targeted disruption of the galectin-3 gene results in accelerated diabetic glomerulopathy40. Therefore, further investigations are needed to establish the exact mechanism by which galectin-3 is involved in the pathogenesis of renal function loss in diabetes.
There are several limitations in our study. First, because of the cross-sectional design, the causal and temporal relationship could not be established in this study. Second, although several potential confounding factors were considered in the regression models, the association between galectin-3 and eGFR could still be affected by unmeasured confounders. Another limitation is that the sample size is relatively small. In spite of these limitations, we believe that our data provide valuable information on the relationship between galectin-3 concentration and eGFR in patients with T2DM with and without albuminuria.
In conclusion, galectin-3 concentrations were negatively associated with eGFR in patients with T2DM, independent of albuminuria status. Further large longitudinal investigations are warranted to confirm that galectin-3 predicts an early progressive decline in renal function in patients with T2DM with and without albuminuria.
Materials and methods
Participants
In this cross-sectional study, we consecutively recruited 334 patients with T2DM who visited the diabetes clinic of our hospital. T2DM was diagnosed according to the expert committee’s report on the diagnosis and classification of diabetes mellitus41. Patients taking glucocorticoids; those with an inflammatory disorder, infection, coronary artery disease, heart failure, peripheral artery disease, stroke, kidney disease unrelated to diabetes (e.g., intrinsic renal disease [nephritis or nephrotic syndrome], acute renal failure due to use of drugs, contrast agents, septic shock, or postrenal disease), chronic liver disease, malignancy, or end-stage kidney disease; those who had undergone kidney transplantation; and those who were on dialysis were excluded. If the patient had a blood pressure ≥ 140/90 mmHg or was taking antihypertensive agents, the patient was considered to have hypertension. If the patient had total cholesterol levels ≥ 6.5 mmol/L or triglyceride levels ≥ 2.3 mmol/L or was taking lipid-lowering agents, the patient was considered to have hyperlipidemia. The study was approved by the ethics committee of Chonnam National University Hospital, and informed consent was obtained from all participants. The study was conducted in accordance with the Helsinki Declaration-based ethical principles for medical research involving human subjects.
Measurements
Venous blood samples were collected after overnight fasting. Cystatin C was measured using an assay from Gentian (Moss, Norway), traceable to the international calibrator ERM-DA471/IFCC42. Creatinine level was measured using the Jaffe method. Plasma galectin-3 concentrations were determined using a human galectin-3 Quantikine enzyme-linked immunosorbent assay kit (R&D Systems, Minneapolis, MN) (inter-assay coefficient of variation < 7% and intra-assay coefficient of variation < 4.0%) following the manufacturer’s instructions. Glycated hemoglobin (A1C) was assayed using ion-exchange liquid chromatography (Tosoh, Tokyo, Japan). Urinary albumin excretion was determined using the urinary albumin-to-creatinine ratio (UACR). The mean values of urinary albumin excretion were determined from two spot urine samples obtained on two consecutive mornings. Normoalbuminuria was defined as UACR < 30 mg/g, and albuminuria was ≥ 30 mg/g. eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula combining creatinine-cystatin C (eGFRcrea-cyst)43. As an alternative, eGFR was also estimated using the CKD-EPI creatinine formula (eGFRcrea)43.
Statistical analyses
The sample size was estimated using G*Power 3.1.9.244. Using a two-tailed test, the sample size was determined to detect a medium effect size (correlation coefficient) of 0.3 with α of 0.05 and a power of 0.80. The minimum sample size was estimated to be 84.
Quantitative variables are presented as the mean ± standard deviation (SD) or median (25th, 75th percentile). Qualitative variables are presented as frequencies (percentages). Differences between groups were assessed using Student's t-test and Mann–Whitney U test for parametric and nonparametric continuous variables, respectively. Chi-square test or Fisher’s exact test was used to compare categorical variables. Normal distribution was assessed using both visual inspection of histograms and the Kolmogorov–Smirnov test. Logarithmic transformation for variables with skewed distributions was conducted prior to correlation and regression analyses. Pearson’s correlation analysis was used to assess the association between plasma galectin-3 levels and eGFR. We evaluated the association between galectin-3 concentration and eGFR using a multiple linear regression model. Variables were used as covariates in the regression model if they were previously shown to relate to the risk of renal function decline2,45 and/or exhibited significant differences between patients according to median galectin-3 in either normoalbuminuria or albuminuria group. These covariates are as follows: age, body mass index, smoking, duration of diabetes, A1C, hemoglobin, hyperlipidemia, hypertension, and anti-diabetic therapy. Sex was also considered as a covariate. We adjusted for sex and age (Model 1). Model 2 included adjustments for body mass index, smoking, duration of diabetes, A1C, hemoglobin, hyperlipidemia, hypertension, and use of insulin and oral hypoglycemic agents in addition to the parameters in Model 1. In Model 3a, we adjusted for all parameters in Model 2 plus UACR as albuminuria status (yes/no). In Model 3b, we adjusted for all parameters in Model 2 plus UACR as the continuous variable. Multicollinearity was examined using the variance inflation factor. A variance inflation factor > 10 was excluded from the models. All analyses were conducted using the SPSS software version 20.0 (SPSS, Chicago, IL, USA). P significance was set at < 0.05.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Ingelfinger, J. R. & Jarcho, J. A. Increase in the incidence of diabetes and its implications. N. Engl. J. Med. 376, 1473–1474. https://doi.org/10.1056/NEJMe1616575 (2017).
Thomas, M. C. et al. Diabetic kidney disease. Nat. Rev. Dis. Primers 1, 15018. https://doi.org/10.1038/nrdp.2015.18 (2015).
Ninomiya, T. et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J. Am. Soc. Nephrol. 20, 1813–1821. https://doi.org/10.1681/ASN.2008121270 (2009).
de Zeeuw, D. Albuminuria: A target for treatment of type 2 diabetic nephropathy. Semin. Nephrol. 27, 172–181. https://doi.org/10.1016/j.semnephrol.2007.01.002 (2007).
de Zeeuw, D. et al. Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: Lessons from RENAAL. Kidney Int. 65, 2309–2320. https://doi.org/10.1111/j.1523-1755.2004.00653.x (2004).
Gerstein, H. C. et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286, 421–426. https://doi.org/10.1001/jama.286.4.421 (2001).
Solini, A. et al. Diverging association of reduced glomerular filtration rate and albuminuria with coronary and noncoronary events in patients with type 2 diabetes: The renal insufficiency and cardiovascular events (RIACE) Italian multicenter study. Diabetes Care 35, 143–149. https://doi.org/10.2337/dc11-1380 (2012).
Adler, A. I. et al. Development and progression of nephropathy in type 2 diabetes: The United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 63, 225–232. https://doi.org/10.1046/j.1523-1755.2003.00712.x (2003).
Mogensen, C. E. Microalbuminuria, blood pressure and diabetic renal disease: Origin and development of ideas. Diabetologia 42, 263–285. https://doi.org/10.1007/s001250051151 (1999).
Vistisen, D. et al. Progressive decline in estimated glomerular filtration rate in patients with diabetes after moderate loss in kidney function-even without albuminuria. Diabetes Care 42, 1886–1894. https://doi.org/10.2337/dc19-0349 (2019).
Said, S. M. & Nasr, S. H. Silent diabetic nephropathy. Kidney Int. 90, 24–26. https://doi.org/10.1016/j.kint.2016.02.042 (2016).
Klessens, C. Q. et al. An autopsy study suggests that diabetic nephropathy is underdiagnosed. Kidney Int. 90, 149–156. https://doi.org/10.1016/j.kint.2016.01.023 (2016).
Comai, G. et al. Histological evidence of diabetic kidney disease precede clinical diagnosis. Am. J. Nephrol. 50, 29–36. https://doi.org/10.1159/000500353 (2019).
Dumic, J., Dabelic, S. & Flogel, M. Galectin-3: An open-ended story. Biochim. Biophys. Acta 1760, 616–635. https://doi.org/10.1016/j.bbagen.2005.12.020 (2006).
Henderson, N. C. & Sethi, T. The regulation of inflammation by galectin-3. Immunol. Rev. 230, 160–171. https://doi.org/10.1111/j.1600-065X.2009.00794.x (2009).
Hara, A. et al. Galectin-3 as a next-generation biomarker for detecting early stage of various diseases. Biomolecules https://doi.org/10.3390/biom10030389 (2020).
Martinez-Martinez, E. et al. Galectin-3 blockade reduces renal fibrosis in two normotensive experimental models of renal damage. PLoS ONE 11, e0166272. https://doi.org/10.1371/journal.pone.0166272 (2016).
Nishiyama, J. et al. Up-regulation of galectin-3 in acute renal failure of the rat. Am. J. Pathol. 157, 815–823. https://doi.org/10.1016/S0002-9440(10)64595-6 (2000).
Desmedt, V., Desmedt, S., Delanghe, J. R., Speeckaert, R. & Speeckaert, M. M. Galectin-3 in renal pathology: More than just an innocent bystander. Am. J. Nephrol. 43, 305–317. https://doi.org/10.1159/000446376 (2016).
Ou, S. M. et al. Identification of galectin-3 as potential biomarkers for renal fibrosis by RNA-sequencing and clinicopathologic findings of kidney biopsy. Front Med. 8, 748225. https://doi.org/10.3389/fmed.2021.748225 (2021).
Cao, Z. Q., Yu, X. & Leng, P. Research progress on the role of gal-3 in cardio/cerebrovascular diseases. Biomed. Pharmacother. 133, 111066. https://doi.org/10.1016/j.biopha.2020.111066 (2021).
Saeed, M. et al. Serum galectin-3 and subsequent risk of coronary heart disease in subjects with childhood-onset type 1 diabetes: A cohort study. Diabetes Care 44, 810–816. https://doi.org/10.2337/dc20-1712 (2021).
Wang, A. et al. Serum galectin-3 and poor outcomes among patients with acute ischemic Stroke. Stroke 49, 211–214. https://doi.org/10.1161/STROKEAHA.117.019084 (2018).
Yilmaz, H., Cakmak, M., Inan, O., Darcin, T. & Akcay, A. Increased levels of galectin-3 were associated with prediabetes and diabetes: New risk factor?. J. Endocrinol. Invest. 38, 527–533. https://doi.org/10.1007/s40618-014-0222-2 (2015).
Atalar, M. N. et al. Assessment of serum galectin-3, methylated arginine and Hs-CRP levels in type 2 diabetes and prediabetes. Life Sci. 231, 116577. https://doi.org/10.1016/j.lfs.2019.116577 (2019).
Li, P. et al. Hematopoietic-derived galectin-3 causes cellular and systemic insulin resistance. Cell 167, 973–984. https://doi.org/10.1016/j.cell.2016.10.025 (2016).
Vora, A., de Lemos, J. A., Ayers, C., Grodin, J. L. & Lingvay, I. Association of galectin-3 with diabetes mellitus in the Dallas heart study. J. Clin. Endocrinol. Metab. 104, 4449–4458. https://doi.org/10.1210/jc.2019-00398 (2019).
Drechsler, C. et al. Galectin-3, renal function, and clinical outcomes: Results from the LURIC and 4D studies. J. Am. Soc. Nephrol. 26, 2213–2221. https://doi.org/10.1681/ASN.2014010093 (2015).
Rebholz, C. M. et al. Plasma galectin-3 levels are associated with the risk of incident chronic kidney disease. Kidney Int. 93, 252–259. https://doi.org/10.1016/j.kint.2017.06.028 (2018).
Tan, K. C. B. et al. Galectin-3 is independently associated with progression of nephropathy in type 2 diabetes mellitus. Diabetologia 61, 1212–1219. https://doi.org/10.1007/s00125-018-4552-z (2018).
Hodeib, H. et al. Galectin-3 as a prognostic biomarker for diabetic nephropathy. Diabetes Metab. Syndr. Obes. 12, 325–331. https://doi.org/10.2147/DMSO.S194410 (2019).
Macisaac, R. J. & Jerums, G. Diabetic kidney disease with and without albuminuria. Curr. Opin. Nephrol. Hypertens. 20, 246–257. https://doi.org/10.1097/MNH.0b013e3283456546 (2011).
Perkins, B. A., Ficociello, L. H., Roshan, B., Warram, J. H. & Krolewski, A. S. In patients with type 1 diabetes and new-onset microalbuminuria the development of advanced chronic kidney disease may not require progression to proteinuria. Kidney Int. 77, 57–64. https://doi.org/10.1038/ki.2009.399 (2010).
Dowse, G. K. et al. Prevalence and risk factors for diabetic retinopathy in the multiethnic population of Mauritius. Am. J. Epidemiol. 147, 448–457. https://doi.org/10.1093/oxfordjournals.aje.a009470 (1998).
Ritz, E. & Orth, S. R. Nephropathy in patients with type 2 diabetes mellitus. N. Engl. J. Med. 341, 1127–1133. https://doi.org/10.1056/NEJM199910073411506 (1999).
Frenay, A. R. et al. Pharmacological inhibition of galectin-3 protects against hypertensive nephropathy. Am. J. Physiol. Renal Physiol. 308, F500-509. https://doi.org/10.1152/ajprenal.00461.2014 (2015).
Chen, S. C. & Kuo, P. L. The role of galectin-3 in the kidneys. Int. J. Mol. Sci. 17, 565. https://doi.org/10.3390/ijms17040565 (2016).
Vlassara, H. Protein glycation in the kidney: Role in diabetes and aging. Kidney Int. 49, 1795–1804. https://doi.org/10.1038/ki.1996.270 (1996).
Vlassara, H. et al. Identification of galectin-3 as a high-affinity binding protein for advanced glycation end products (AGE): A new member of the AGE-receptor complex. Mol. Med. 1, 634–646 (1995).
Pugliese, G. et al. Accelerated diabetic glomerulopathy in galectin-3/AGE receptor 3 knockout mice. FASEB J. 15, 2471–2479. https://doi.org/10.1096/fj.01-0006com (2001).
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 26 Suppl 1, S5–20. https://doi.org/10.2337/diacare.26.2007.s5 (2003).
Grubb, A. et al. First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin. Chem. Lab. Med. 48, 1619–1621. https://doi.org/10.1515/CCLM.2010.318 (2010).
Inker, L. A. et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 367, 20–29. https://doi.org/10.1056/NEJMoa1114248 (2012).
Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. https://doi.org/10.3758/bf03193146 (2007).
Thomas, M. C. Anemia in diabetes: Marker or mediator of microvascular disease?. Nat. Clin. Pract. Nephrol. 3, 20–30. https://doi.org/10.1038/ncpneph0378 (2007).
Acknowledgements
This study was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea government (MSIT) (2021R1F1A1062776) and Chonnam National University Hospital Biomedical Research Institute (BCRI20014).
Author information
Authors and Affiliations
Contributions
J.O.C. designed the study, analyzed data, drafted the manuscript, and approved its final version. S.Y.P., S.B.L., and M.Y.C. contributed to the statistical analyses and interpretation of data. J.O.C., D.H.C., N. R. K., and D.J.C. acquired data. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, J.O., Park, SY., Lee, S.B. et al. Plasma galectin-3 concentration and estimated glomerular filtration rate in patients with type 2 diabetes with and without albuminuria. Sci Rep 12, 16328 (2022). https://doi.org/10.1038/s41598-022-20860-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-20860-x