Abstract
Insight impairment contributes significantly to morbidity in psychiatric disorders. The neurologic concept of anosognosia, reflecting deficits in metacognitive awareness of illness, is increasingly understood as relevant to psychopathology, but has been little explored in psychiatric disorders other than schizophrenia. We explored anosognosia as an aspect of insight impairment in n = 71 individuals with DSM-5 hoarding disorder. We used a standardized clutter severity measure to assess whether individuals with hoarding disorder underreport home clutter levels relative to independent examiners. We then explored whether underreporting, as a proxy for anosognosia, is predicted by clinical or neurocognitive behavioral measures. We found that individuals with hoarding disorder underreport their clutter, and that underreporting is predicted by objective severity of clutter. In an n = 53 subset of participants, we found that underreporting is predicted by altered performance on tests of cognitive control and inhibition, specifically Go/No-Go and Stroop tests. The relation of underreporting to objective clutter, the cardinal symptom of hoarding disorder, suggests that anosognosia may reflect core pathophysiology of the disorder. The neurocognitive predictors of clutter underreporting suggest that anosognosia in hoarding disorder shares a neural basis with metacognitive awareness deficits in other neuropsychiatric disorders and that executive anosognosia may be a transdiagnostic manifestation of psychopathology.
Similar content being viewed by others
Introduction
In the psychiatric literature, ‘insight’ is a complex, multidimensional construct, defined to include awareness of illness, attribution of symptoms to illness, and openness to treatment1,2. It is nonetheless of prima facie clinical relevance, influencing patients’ engagement with and benefit from care. Across diverse disorders, impaired insight has been associated with increased symptom severity, greater comorbidity, and worse prognosis3,4. Insight has been identified as a critical target of psychotherapeutic treatment5, yet there is minimal evidence to support pharmacologic or somatic treatments for impaired insight, likely reflecting the dimensional complexity of the construct, the heterogeneity of conditions in which insight may be impaired, and insufficient understanding of the basis of insight in the brain. Pathophysiologic understanding of insight in psychiatry has further emphasized its dynamic psychological nature, including affective and motivational influences on awareness and the deployment of denial as a defense6.
In the neurologic literature, impaired awareness of illness—or anosognosia—has been a focus of interest for more than a century and has been described in association with diverse disorders, including most characteristically hemiplegia after stroke, but also cortical blindness, dementias, aphasias, and amnestic disorders7,8. In contrast to the dynamic psychiatric model of ‘insight impairment,’ the term ‘anosognosia’ refers specifically to impaired awareness of illness and its symptoms. Pathophysiologic understanding of anosognosia has emphasized its neurobiological basis—the disruption to relevant cortical and subcortical circuits and substrates—particularly implicating right hemispheric areas, including prefrontal, temporoparietal, and insular cortex9,10,11,12,13.
The concept of anosognosia has increasingly been applied in the context of psychiatric illness4. While in psychiatry the term ‘anosognosia’ has been used principally in studies of schizophrenia14,15,16, research exploring the neurobiological basis of awareness deficits in psychiatric illness has increasingly supported a model in which insight reflects neurobiologically-based neurocognitive capacities. In particular, studies in schizophrenia, substance use disorders, and a limited number of other conditions have suggested that deficits in illness awareness correlate neurocognitively with deficits in aspects of executive function, particularly those related to attentional set shifting and the processing of error4,17,18. At a circuit level, awareness or insight deficits have been correlated with dysfunctional activation or connectivity of salience network components, including the anterior cingulate and insula4,18,19,20. In both the psychiatric and neurologic clinical literature, increasing emphasis on anosognosia/insight impairment as reflecting deficits in metacognitive capacity may bridge historical psychologic and neurologic explanatory models21,22. A contemporary neurocognitive model for metacognitive awareness, the Cognitive Awareness Model (CAM), similarly emphasizes the role of error-monitoring and other frontal-executive functions in facilitating awareness23,24.
In this study, we have sought to explore the neurocognitive basis of anosognosia in psychiatric illness using hoarding disorder (HD) as a highly relevant model disorder. Acquiring and saving behavior leading to excessive and impairing clutter is termed hoarding, and a diagnosis of HD is made when these behaviors are not better explained by a primary neurodegenerative, psychotic, or other condition25. Clinical literature has long emphasized manifestations of poor insight in HD26,27, and insight impairment is coded as a diagnostic specifier for HD in the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-5)25, yet significant gaps remain in understanding its disorder-specific expression, prevalence, and etiology.
No consensus instrument for assessment of insight has been applied in HD. Scores on the Brown Assessment of Beliefs Scale (BABS)28—an insight assessment instrument validated in obsessive–compulsive and related disorders (OCRDs)—correlate poorly with clinician-assessed insight in HD29. Attempts to assess the prevalence and degree of insight impairment in HD have yielded inconsistent results, likely reflecting the absence of a standardized assessment, variable samples of the HD patient population, and the inherent limitations of self-report. Studies using clinician interview30 or those asking family members31 or social service providers32 to rate the insight of individuals with hoarding behaviors have suggested rates of poor or absent insight from 55 to 85%. The historical conflation of HD and obsessive–compulsive disorder (OCD) additionally complicates estimates, yet multiple studies have described an association in OCD between hoarding symptoms and insight impairment, whether assessed via the Y-BOCS33,34,35 or BABS36,37,38.
Neurocognitive testing studies in HD have suggested that executive dysfunction, including difficulties with response inhibition and set shifting, is characteristic of the disorder39,40,41,42,43. Findings are inconsistent, however: a large study of unmedicated individuals with HD found deficits in sustained attention but no difference from controls in terms of executive function44. Neurophysiologic and imaging data is less abundant, yet aberrant activations of anterior cingulate cortex45, frontal hypoactivation during inhibitory control tasks46, and decreases in an electrophysiologic measure of error processing47 have been observed in individuals with HD relative to controls, broadly supporting a model of prefrontal dysfunction in HD. No study has explored the relationship between neurocognitive functioning and insight in HD.
In this exploratory study, we assessed data from individuals screening for participation in a clinical trial of group therapy for HD (NCT02843308) for objective indicators of anosognosia and its correlates. In particular, given that anosognosia, or minimization of clutter, has been considered a hallmark of insight impairment in HD26,27, we used a standardized pictographic rating scale of clutter, the Clutter Image Rating (CIR)48, to explore individual-level discrepancies between self-ratings of clutter made in clinic and independent examiner (IE) ratings of clutter made during a subsequent home visit. We hypothesized that subjective underreporting of clutter per CIR would be prevalent, and that underreporting would be predicted by impaired performance on neurocognitive tasks associated with attentional control or response inhibition.
Materials and methods
This study was conducted via an outpatient academic clinic. Approval was obtained for all procedures from the Stanford University Administrative Panel on Human Subjects in Medical Research (authorized to approve research under the US Department of Health and Human Services’ Office for Human Research Protections), and all participants gave informed consent. All experiments were performed in accordance with relevant guidelines and regulations.
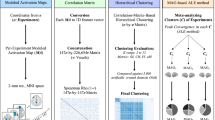
Overview and behavioral assessment of anosognosia
Demographic and clinical data were collected from participants screening for participation in a clinical treatment study of HD between October 2016 and April 2019 (Fig. 1A). Participants self-identified as seeking help with clutter and were recruited via targeted online advertisements, radio advertisements, local flyering, and word of mouth. Clinical data included self- and clinician-rated assessments performed either in clinic, via secure teleconference, or via secure web-based submission portals. After initial assessments, a home visit was scheduled during which an IE rated home clutter severity (Fig. 1B). The full n = 71 study sample includes all participants for whom both self- and home-visit IE-ratings of clutter were completed during the recruitment period.
Participant flow diagram. Data were collected from individuals screening for and enrolling in study offering clinical treatment of hoarding disorder. (A) Participants underwent clinical assessments and self-rated their home clutter levels using the Clutter Image Rating (CIR). (B) 71 participants completed an in-home evaluation during which independent evaluators (IEs) rated home clutter levels using the CIR, thus allowing a measure of anosognosia based upon the relative discrepancy of self- vs IE-rated clutter. (C) 53 participants for whom a measure of anosognosia was obtained proceeded to the clinical treatment study and completed computer-based neurocognitive testing (WebNeuro).
A quantitative behavioral measure of anosognosia was generated by evaluating the discrepancy between self-ratings of clutter made using the CIR, a validated pictographic instrument48, and objective (IE) ratings of clutter using the same instrument, as a proportion of total objective clutter score (see “Assessments” and “Statistical analysis” below).
Inclusion/exclusion
To qualify for a home visit (and thus to be included in the n = 71 study sample), participants were required to meet the following inclusion criteria: age between 18–75; primary DSM-5 HD diagnosis (assessed via the structured clinical interview (SCID) for DSM-5)49; clinically significant symptoms (defined as a Saving Inventory-Revised (SI-R) score ≥ 40)50; no or stable psychotropic medication use (defined as medication doses unchanged for > 4 weeks prior to assessment or > 8 weeks if fluoxetine); a safely accessible home in one of two neighboring counties and within 30 miles of Stanford University. Participants were excluded if they had OCD as a primary diagnosis, a current or history of psychotic disorder or bipolar disorder, a current eating disorder, or a current moderate or lifetime severe substance use disorder. Patients were additionally excluded if they had current severe depression (defined as Hamilton Depression Rating Scale (HDRS) score > 30)51, had any other medical or neuropsychiatric condition that would increase risk of participation or interfere with engagement in assigned behavioral practice tasks, were currently working with a professional organizer, or were at elevated acute eviction risk. For one participant, a full SCID was completed only after the home visit occurred; however, given the availability of both self- and IE-CIR ratings data, this individual was included in the analysis despite bipolar disorder comorbidity. Similarly, two participants who for scheduling reasons underwent a home visit prior to completing the SI-R, and who were found to have SI-R < 40 (with scores of 14 and 37), were nonetheless included in the analysis given the availability of both self- and IE-CIR ratings and diagnosis of HD per SCID.
Assessments
The CIR48 is a validated pictorial scale of clutter severity consisting of nine photographs each of an increasingly cluttered kitchen, bedroom, or living room. Each room in a home is rated by choosing the image that most closely corresponds to the level of clutter in the room, and a composite home score is generated by averaging room scores. The CIR is designed for use by both patients and clinicians. As validated, the composite CIR score has high test–retest reliability (r = 0.85 when repeated by patients with interval of < 2 months) and high inter-observer reliability (r = 0.94) when both patient and clinician are in the home being rated; correlation between asynchronous patient ratings made in the clinic and clinician ratings made in the home is less strong (r = 0.78)48, as similarly observed in an independent study of older adults (r = 0.54)52. Our data included asynchronous participant CIR ratings (self-CIR) made in clinic and independent examiner CIR ratings (IE-CIR) made during a subsequent home visit. Composite scores for both self-CIR and IE-CIR were calculated by averaging scores from only those rooms rated by both participant and IE.
The SI-R50 is a 23-item questionnaire using a 5 point (0 to 4) Likert-type scale that assesses severity of compulsive hoarding. It comprises three subscales defined by exploratory factor analysis, reflecting core domains of hoarding behavior, including Excessive Acquisition (seven items), Difficulty Discarding (seven items), and clutter (nine items). Internal consistency (Cronbach’s alpha) for the full scale in our sample was acceptable, at 0.86. Alpha values for the subscales of the SI-R were 0.7 for Difficulty Discarding, 0.88 for Clutter, and 0.79 for Excessive Acquisition.
The Saving Cognitions Inventory (SCI)53 is a 24-item questionnaire using a 7 point (1 to 7) Likert-type scale that assesses the experienced frequency of thoughts and beliefs related to possessions (e.g., “I am responsible for the well-being of this possession”). Although a measure of beliefs, not of hoarding behaviors per se, the SCI correlates strongly with measures of hoarding54. Factor analysis of SCI responses has defined four subscales, including emotional attachment (ten items), memory (five items), control (three items), and responsibility (six items)53. In our sample, internal consistency of the full scale was high (0.92). Alpha values for the subscales were 0.93 for Emotional Attachment, 0.81 for Memory, 0.68 for Control, and 0.67 for Responsibility.
Additional measures included the 17-item Hamilton Depression Rating Scale (HDRS)51, used to allow clinician-assessed rating of depression severity; the North American Adult Reading Test (NAART)55, used to estimate verbal intelligence; and the Edinburgh Handedness Inventory56 in a revised eight-item format57, used to assess handedness.
Neurocognitive testing
A subset of participants (n = 53) met criteria for clinical study enrollment and underwent neurocognitive assessment (Fig. 1C). These criteria included having at least one room IE-CIR rated ≥ 3 on home visit, and having a home deemed safe for ongoing visitation by study staff (i.e., free of mold, vermin, or structural risks).
Neurocognitive assessment of cognitive control was undertaken using a computerized test battery called WebNeuro58, which has been validated against gold-standard neuropsychological tests assessing the equivalent constructs58,59. The testing battery was completed in a single sitting of approximately 45 min. Participants were offered the opportunity to complete WebNeuro testing either at home or in a private office in the clinic. The neurocognitive domains assessed by this battery and the test used to assess them (and the equivalent test from traditional paper–pencil neuropsychological tests) include:
-
i.
Sensorimotor function; Finger Tapping test (Finger Tapping)
-
ii.
Cognitive control; Go/No-Go test (Go/No-Go)
-
iii.
Maintenance of attention; Continuous Performance test (Continuous Performance)
-
iv.
Processing speed; Switching of Attention test (Trails B)
-
v.
Decision speed; Choice Reaction Time test (Corsi Blocks)
-
vi.
Verbal learning and memory; Memory Recognition test (California Verbal Learning and Memory test)
-
vii.
Working memory; Digit Span test (Digit Span)
-
viii.
Executive function; Maze test to assess planning and response monitoring (Austin Maze)
-
ix.
Inhibition; Verbal Interference task assessing capacity to suppress conflicting information when assessing either written word or ink color (Stroop).
Individual performance on each of these behavioral tests was quantified by accuracy and reaction time relative to matched healthy norms for age, sex, and years of education (normative cohort of n = 1317)60,61. These norm-reference scores were expressed as standardized scores with a mean of 0 and standard deviation of 1, such that lower scores reflected greater impairment.
Statistical analysis
Using self- and IE-rated composite CIR scores, we generated an error metric (‘CIR-error’) for each participant that reflected the degree of under- or over-reporting. Taking the IE-CIR as ‘objective,’ we defined CIR-error as self-CIR subtracted from IE-CIR, divided by IE-CIR ((IE-CIR–self-CIR)/IE-CIR), thus capturing discrepancy in self-report in proportion to objective clutter severity. As defined, more positive scores of CIR-error reflect greater underreporting of clutter.
Means, ranges, and standard deviations were assessed for demographic, clinical, and neurocognitive variables. One-sample Student’s t-tests with µ = 0 were used to assess differences in neurocognitive performance between our HD participants and the normative population. For those variables for which our participants’ scores were not normally distributed, as per Shapiro-Wilk test, we employed a one-sample Wilcoxon Rank Sum Test. An initial alpha threshold of 0.05 was Bonferroni-adjusted for the number of independent predictors.
We assessed relationships between clinical and neurocognitive variables and CIR-error, as well as self- and IE-CIR scores themselves, using univariate linear regression with CIR-error as the dependent variable. To account for multiple comparisons, the alpha threshold was Bonferroni-adjusted for the number of independent predictors tested. Significant predictors of CIR-error were considered as possible explanatory variables in a multiple linear regression model. Proportions of variance explained are provided as adjusted R2. Instances of missing data were addressed with listwise deletion; given limited missing observations (< 4 cases per variable), the assumption that data are missing completely at random was not felt to add significant risk of bias. All statistical assessments were performed using R version 4.1.2.
Results
Sample characteristics
A demographic and clinical description of our sample population is presented in Table 1. Participants ranged in age from 24 to 75, with an average age of 57.0 (SD 10.4). Fifty-three of 71 participants (75%) in our full sample identified as female and 75% as Caucasian/White. Forty participants (60%) reported use of psychotropic medication, including 36 (54%) using antidepressant medications, and 3 (5%) using antipsychotic medications. The average SI-R score was 59.1 (range 14–86, SD 10.9), well above the thresholds of 39 or 41 suggested in the literature for diagnosis of HD62,63. Average HDRS score was 5.8 (range 0–24, SD 4.9), consistent with typically mild severity, if any, of comorbid depression. Estimated verbal intelligence quotient for the full sample was high, at 115.2 (84.1–123.9, SD 7.3), and school grades completed, recorded in the sample completing neurocognitive testing, suggest high levels of education, with 91% reporting at least 4 years of post-secondary education, and 47% reporting more than 6 years of post-secondary education. Medical comorbidity was common, with 65% reporting use of medication for somatic medical conditions.
Subjective underreporting of clutter
Self-assessed composite CIR scores averaged 3.78 (range 1.67–6.4, SD 1.14). IE-CIR scores were obtained during home visit after an average interval of 25 days (range 0–100, SD 21.5). IE-CIR scores averaged 4.22 (range 1–8.33, SD 1.39). Although self-CIR and IE-CIR scores were significantly correlated (r = 0.73 (95% CI 0.60–0.83), p < .0001), self-CIR scores were significantly lower than IE-CIR scores (difference in means 0.45 (95% CI 0.22–0.67, t(70) = 3.94, p = .0002), indicating a tendency by participants to underrate clutter during in-clinic assessment (Fig. 2A,B). The mean CIR-error score was 0.06 (range -0.75–0.60, SD 0.26) with 41 of 71 participants (58%) having positive CIR-error values (indicating underreporting of clutter), 21 of 71 participants (30%) having CIR-error score or 0.2 or greater, and three of 71 individuals (4%) scoring 0.5 or greater, representing underreporting of clutter by half.
Underreporting of clutter, a proxy for anosognosia, is common in hoarding disorder and increases with severity of clutter. (A) Independent evaluator (IE) and self-rated Clutter Image Rating (CIR) scores are correlated (solid black line), but most individuals with hoarding disorder underrate clutter relative to IE ratings (e.g., all points below the x = y dotted line). CIR-error (shading, calculated as (IE-CIR – self-CIR)/IE-CIR) represents the degree of underreporting (blue) or overreporting (red) relative to IE-CIR score. (B) Example living room images from the CIR scale (adapted with permission from Steketee and Frost79). The circled data point in panel A represents one individual with HD who self-rated their rooms on average as level ‘4’ (upper panel), whereas an IE rated the same rooms on average as level ‘6’ (lower panel). (C) Clutter underreporting (CIR-error) increases with objective clutter score (IE-CIR). (D) Clutter underreporting is not predicted by self-reported clutter (self-CIR).
Relation of underreporting to clutter severity
Univariate linear regression was used to assess IE-CIR and self-CIR as predictors of CIR-error (Table 2). CIR-error was predicted by severity of IE-assessed clutter (IE-CIR; β = 0.11 (95% CI 0.07–0.15), R2 = 0.35, p < 0.0001); the degree of clutter underreporting increased as objective clutter severity increased (Fig. 2C). This was not true for self-reported clutter: self-CIR score did not predict CIR-error (β = − 0.01 (95% CI − 0.06–0.05), R2 < 0.001, p = 0.81; Fig. 2D). The days elapsed between self-rating and in-home IE-rating also had no predictive value (β = 0.001 (95% CI − 0.002–0.004), R2 = 0.012, p = 0.37). Using a multivariate linear model, objective severity of clutter (IE-CIR) remained a significant predictor of CIR-error when controlling for age, gender, handedness, estimated IQ, depression, and use of psychotropic medication (β = 0.12 (95% CI 0.07–0.16), p < 0.0001).
Relation of clutter underreporting to clinical assessments
Other demographic and clinical variables were next assessed as predictors of CIR-error (Table 2). For the full sample, CIR-error was not predicted by age, gender, handedness, psychotropic medication use, number of current somatic medical diagnoses, or depression (HDRS). Notably, clinical measures of HD were also not predictive of CIR-error. Only the Difficulty Discarding subscale of the SI-R (SIR-DD) showed a trend toward prediction of CIR-error—however, with a negative coefficient, such that lower scores on SIR-DD predicted greater underreporting of clutter (β = − 0.02 (95% CI − 0.033 to − 0.003), R2 = 0.08, p = 0.021). The SCI and its component subscales were similarly not predictive of CIR-error.
Neurocognitive performance
Fifty-three participants completed computer-based neurocognitive testing. Demographic and clinical characteristics of this subset were like those of the full sample (Table 1). Means for normed performance on task measures are represented in Table 3. Our participants with HD showed significant differences from the reference normative population on several measures. On the Go/No-Go test, participants had slower reaction times (z = − 1.08, t(51) = − 14.9, p < 0.0001). On the Continuous Performance test, participants showed slower reaction times (z = − 1.01, t = − 6.3, p < 0.0001) and a trend toward more false negative errors (z = − 0.38, V = 495, p = 0.051), suggesting mild deficits in sustained attention. Participants showed stronger performance on a test of immediate recall than the reference population (z = 0.49, V = 1236, p < 0.0001). On the Stroop-like Verbal Interference test, HD participants were marginally faster at identifying the ink color of printed color words (z = 0.29, t = 2.13, p = 0.04), and demonstrated faster normed performance for ink-color identification relative to written color word identification (z = 0.24, t = 2.32, p = 0.02). HD participant performance did not otherwise differ from the reference population for measures of psychomotor speed, reaction time, Switching of Attention, Digit Span, or Maze completion.
Relation of clutter underreporting to neurocognitive performance
We next explored neurocognitive performance measures as independent predictors of CIR-error using univariate linear regression (Table 4). Total errors on the Go/No-Go test (β = − 0.12 (95% CI − 0.18 to − 0.05), R2 = 0.18, p = 0.002) predicted CIR-error. Differential reaction time for ink color naming vs color word reading on the Verbal Interference test (β = 0.13 (95% CI 0.04–0.22), R2 = 0.13, p = 0.010) also predicted CIR-error, however this relationship did not survive Bonferroni correction for multiple comparisons. Given the strong relationship between CIR-error and objective clutter, we additionally assessed neurocognitive variables when controlling for IE-CIR in a multivariate linear regression. This additionally suggested completion time for the Switching of Attention test (β = − 0.06 (95% CI − 0.12 to − 0.01) p = 0.032) as a predictor of CIR-error at a trend level.
Multivariate model
Considering all objective measures suggested as predictive of CIR-error, a multivariate linear model was tested incorporating objective clutter assessment (IE-CIR), Go/No-Go errors, Stroop interference by reaction time, and Switching of Attention completion time. This model revealed IE-CIR (β = 0.09 (95% CI 0.05–0.14), p < 0.001), Go/No-Go errors (β = − 0.07 (95% CI − 0.13 to − 0.01), p = 0.03), and Stroop interference (β = 0.08 (95% CI 0.01–0.16), p = 0.03) to be significant independent predictors of CIR-error, and explained 50% of the variance of CIR-error measurements. IE-CIR (β = 0.10 (95% CI: 0.04–0.15), p = 0.002), Go/No-Go errors (β = − 0.09 (95% CI − 0.15 to − 0.02), p = 0.014), and Stroop interference (β = 0.10 (95% CI 0.01–0.19), p = 0.043) remained significant independent predictors when included in a multivariate model controlling for age, gender, handedness, estimated IQ, depression, and use of psychotropic medication.
Discussion
To our knowledge, our study is the first to assess anosognosia in HD in a manner that does not rely on direct subjective impressions of family or clinician raters and the first study to explore neurocognitive correlates of insight in HD. We found that most participants in our study underrated their clutter, that the degree of underrating was correlated with severity of clutter, and that underrating was correlated with behavioral performance on specific tests of neurocognitive function.
Clutter rating discrepancies
Whether HD patients tend to underreport or overreport symptoms has been explored in prior studies48,64. Variable results when comparing self-ratings with other-ratings on diverse measures have suggested that such tendencies may be influenced by motivation or context (e.g., that participants seeking to enroll in studies might overestimate the severity of their disorder)64. In our study, however, the underreporting of clutter per self-CIR, performed in the context of screening for study participation, is inconsistent with such motivation. The correlations of this underreporting with objective clutter and with neurocognitive behavioral performance further argue against a purely social or contextual explanation for the discrepancies we observe.
Our study relies on discrepancies in CIR rating when the CIR is used as a self-report measure vs a clinician-rated measure. The close correlation of simultaneous self and clinician ratings reported in the literature suggests against gross differences in perception in individuals with HD. The time elapsed between asynchronous self- and IE-ratings in our study may suggest the possibility of interval change in clutter; yet discrepancies we observed were not correlated with inter-assessment interval. Deficits in memory or updating may explain discrepancies when HD participants perform self-rating outside of their homes, in line with observations that insight deficits in OCD are negatively correlated with verbal memory performance65 (though not consistently)66 or visual memory performance66. However, in our study, discrepancies in CIR rating were not predicted by behavioral measures of learning or memory.
The lower correlations of asynchronous (relative to synchronous) self and clinician clutter ratings observed in prior studies48,62 suggests that accuracy of clutter self-assessment, and indeed awareness itself, may be influenced by the presence of a third-party observer. This accords with what has been described in clinical literature, whereby individuals with HD may experience sudden increases in both awareness and distress when others enter their home26. Such fluctuating awareness in relation to third-party perspective may accord with findings from anosognosia in hemiplegia, schizophrenia, and dementia, in which unaware patients may be able to acknowledge deficits when exposed to evidence from a third-person perspective. This phenomenon has been modeled conceptually in dementia by invoking activation of distinct systems for autobiographical vs generic memory67.
Anosognosia as characteristic of hoarding disorder
In our study, participants’ underreporting of clutter increased with objective clutter severity, the cardinal symptom of HD, suggesting that anosognosia may reflect core pathophysiological processes of HD. The relation between underreporting of clutter (insight impairment) and objective clutter severity (behavioral outcome) may find analogy in studies of insight in cocaine use disorder, where underreporting of desire to view cocaine-related images (relative to actual choice of such images in a laboratory context) predicted past-30-day cocaine use68. Importantly, clutter underreporting had no relation to self-reported clutter severity and was not correlated with self-report scales of HD severity, with the exception of a trend-level negative correlation with the Difficulty Discarding subscale of the SI-R. Absent or anti-correlations with self-report HD severity measures might be expected if underreporting is a true proxy of anosognosia. If anosognosia is common or characteristic of HD, however, this raises nosological questions about how the disorder might best be defined or assessed, i.e., whether to emphasize behavior and behavioral impacts (e.g., acquiring, saving, or clutter) or subjective distress associated with hoarding behaviors. The absence of a correlation between clutter underreporting and subscales of the SCI—which scores strength of agreement with various beliefs related to HD—is also notable, in as much as the best-validated instrument for assessing insight in other OCRDs, the BABS, emphasizes strength of disorder-related beliefs as fundamental to ratings of insight. If, as per prior literature, insight impairment in HD is a multi-dimensional construct with both ‘unawareness’ (anosognosia) and ‘delusionality’ as component axes26,27, our proxy measure appears to capture anosognosia more so than overvalued ideation or delusionality.
Anosognosia and cognitive control
Errors on a Go/No-Go test of response inhibition most strongly predicted clutter underreporting in our sample. We are the first study to our knowledge to report Go/No-Go performance as a correlate of clinical insight, although in a neuroimaging study, decreased Go/No-Go task-based activations of cingulate and prefrontal cortex have been associated with unawareness of deficits in Alzheimer’s Disease69. As a measure of response inhibition, however, our finding is strongly consistent with replicated findings from research in psychotic disorders correlating deficits in clinical insight with deficits in Wisconsin Card Sort Test performance, and with the suggestion, based on this work, that insight impairment might reflect deficits in cognitive control and a tendency to perseverative error17. We additionally identified differential response time on a Stroop color/word task as a predictor of clutter underreporting. Correlations between Stroop performance and clinical insight impairment have been reported for OCD65 and for bipolar disorder70, on which basis insight impairment has similarly been suggested to reflect deficits in response inhibition and the processing of conflictual information. For our participants, we observed that increased clutter underreporting predicted better normalized response time performance on the ink color naming task relative to the word reading task. One speculative consideration is that insight deficits in OCRDs may correspond to deficits in the fast, ventral-stream visual pathway required for word recognition and logographic processing. Deficits in such ventral-stream processing for complex figures have been observed to correlate with insight impairment in body dysmorphic disorder71,72. Such deficits, if present in our HD participants, might be expected to slow response in the non-interference phase of our Stroop paradigm—which relies on fast reading of written color names—and yet speed performance in the interference phase of our Stroop paradigm, in as much as ‘overlearned’ word recognition might less potently interfere with ink color naming. Lastly, while below threshold for significance when included in a model with other clinical and neurocognitive predictors, we observed a trend toward impaired performance on the Switching of Attention test as a correlate of clutter underreporting, particularly when controlling for level of clutter. This is consistent with findings from OCD66,73, anorexia nervosa74, and bipolar disorder70,75, in which relative deficits in the Trail Making Test Part B have been found to correlate with impaired clinical insight. The observation that abnormalities of response inhibition, interference processing, and attention switching might correlate with insight impairment across diagnoses supports a general model in which awareness is intrinsically related to cognitive control. Conceptually, a theory of conscious awareness suggests that subjective awareness is a schematic model of attention itself, evolved to facilitate top-down control of attention76. Similarly, the CAM model for metacognitive awareness in dementia and other neurologic conditions suggests that deficits in executive error processing—required for the updating of self-concept based on sensory input—may present one pathway for the development of anosognosia23. Our data suggesting that pathological unawareness in HD correlates with deficits in cognitive control might provide a novel line of evidence in support of these general models.
Limitations and future directions
Limitations of the current study include its exploratory nature and the possibility of Type I error. Additionally, our help-seeking sample may not be representative of the broader population of individuals with HD in terms of clinical insight: our participants lived in homes that were deemed non-squalorous and safely accessible for research staff, they were predominantly older women, and half were using psychotropic medication. While we suggest CIR-error as a face-valid proxy for anosognosia in HD, as a measure of clinical insight impairment more broadly it may not be fully content-valid, in that it may not capture clinically important dimensions of insight impairment in HD, such as the tendency to misjudge the value of objects or risks of clutter, or propensity to interpersonal distortions, by which individuals offering help may be perceived as threatening26,27. We additionally do not assess test–retest reliability of our measure. Nonetheless, the fact that CIR-error correlates with a measure of behavioral severity (objective clutter) and with measures of neurocognitive function identified as correlates of insight impairment in other disorders supports the construct validity of CIR-error as a proxy for anosognosia as a component of insight impairment.
Future work could assess whether clutter underreporting correlates with neurophysiologic or neuroimaging measures of error signaling known to be aberrant in OCD77,78 and HD46,47. In particular, in as much as HD—in contrast to OCD—may be associated with diminished, rather than exaggerated error signaling46,47, it would be of interest to test whether clutter underreporting correlates negatively with error signaling. This might replicate associations between insight impairment and hypoactive error signaling seen in cocaine use disorder19 or proposed in anosognosia for hemiplegia18. Given the prevalence, morbidity, and adverse prognostic significance of insight impairment across the spectrum of neuropsychiatric illness, and given the paucity of treatment interventions specifically targeting this dimension of illness, identifying the neural basis for insight in HD and other disorders will be critical to developing more effective future treatments for mental health conditions.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available, as they contain information that could compromise the privacy of research participants.
Abbreviations
- BABS:
-
Brown Assessment of Beliefs Scale
- CI:
-
Confidence interval
- CIR:
-
Clutter Image Rating
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- HD:
-
Hoarding disorder
- HDRS:
-
Hamilton Depression Rating Scale
- IE:
-
Independent evaluator
- OCD:
-
Obsessive–compulsive disorder
- OCRD:
-
Obsessive–compulsive and related disorder
- SCI:
-
Saving Cognitions Inventory
- SCID:
-
Structured Clinical Interview for DSM-5
- SD:
-
Standard deviation
- SI-R:
-
Saving Inventory-Revised
- SI-R-DD:
-
Saving Inventory Revised, Difficulty Discarding subscale
- Y-BOCS:
-
Yale-Brown Obsessive Compulsive Scale
References
David, A. S. Insight and psychosis. Br. J. Psychiatry. 156, 798–808 (1990).
Amador, X. F. et al. Assessment of insight in psychosis. Am. J. Psychiatry. 150, 873–879 (1993).
David, A. S. The clinical importance of insight: An overview. In Insight and Psychosis: Awareness of Illness in Schizophrenia and Related Disorders 2nd edn (eds Amador, X. F. & David, A. S.) 359–392 (Oxford University Press, 2004).
Landi, P., Marazziti, D., Rutigliano, G. & Dell’Osso, L. Insight in psychiatry and neurology: State of the art, and hypotheses. Harv. Rev. Psychiatry. 24, 214–228 (2016).
Jennissen, S., Huber, J., Ehrenthal, J. C., Schauenburg, H. & Dinger, U. Association between insight and outcome of psychotherapy: Systematic review and meta-analysis. Am. J. Psychiatry. 175, 961–969 (2018).
Williams, A. R., Olfson, M. & Galanter, M. Assessing and improving clinical insight among patients “in denial”. JAMA Psychiat. 72, 303 (2015).
Langer, K. G., Levine, D. N., Babinski, J. (1914) Contribution to the study of the mental disorders in hemiplegia of organic cerebral origin (anosognosia). Translated by Langer, K. G. & Levine, D. N. Cortex. 61, 5–8 (2014).
Gainotti, G. History of Anosognosia. In History of Neuropsychology (eds Bogousslavsky, J. et al.) 75–82 (S. Karger AG, 2019)
Pia, L., Neppi-Modona, M., Ricci, R. & Berti, A. The anatomy of anosognosia for hemiplegia: A meta-analysis. Cortex 40, 367–377 (2004).
Karnath, H.-O. Awareness of the functioning of one’s own limbs mediated by the insular cortex?. J. Neurosci. 25, 7134–7138 (2005).
Orfei, M. D. et al. Anosognosia for hemiplegia after stroke is a multifaceted phenomenon: A systematic review of the literature. Brain 130, 3075–3090 (2007).
Moro, V. et al. Motor versus body awareness: Voxel-based lesion analysis in anosognosia for hemiplegia and somatoparaphrenia following right hemisphere stroke. Cortex 83, 62–77 (2016).
Lattanzio, L., Seames, A., Holden, S. K. & Buard, I. The emergent relationship between temporoparietal junction and anosognosia in Alzheimer’s disease. J. Neurosci. Res. 99, 2091–2096 (2021).
Pia, L. & Tamietto, M. Unawareness in schizophrenia: Neuropsychological and neuroanatomical findings. Psychiatry Clin. Neurosci. 60, 531–537 (2006).
Shad, M. U., Tamminga, C. A., Cullum, M., Haas, G. L. & Keshavan, M. S. Insight and frontal cortical function in schizophrenia: A review. Schizophr. Res. 86, 54–70 (2006).
Lehrer, D. S. & Lorenz, J. Anosognosia in schizophrenia: hidden in plain sight. Innov. Clin. Neurosci. 11, 10–17 (2014).
Aleman, A., Agrawal, N., Morgan, K. D. & David, A. S. Insight in psychosis and neuropsychological function: Meta-analysis. Br. J. Psychiatry. 189, 204–212 (2006).
Klein, T. A., Ullsperger, M. & Danielmeier, C. Error awareness and the insula: Links to neurological and psychiatric diseases. Front. Hum. Neurosci. 7, 14 (2013).
Moeller, S. J. et al. Functional, structural, and emotional correlates of impaired insight in cocaine addiction. JAMA Psychiat. 71, 61 (2014).
Fan, J. et al. Resting-state functional connectivity between right anterior insula and right orbital frontal cortex correlate with insight level in obsessive-compulsive disorder. NeuroImage Clin. 15, 1–7 (2017).
David, A. S., Bedford, N., Wiffen, B. & Gilleen, J. Failures of metacognition and lack of insight in neuropsychiatric disorders. Philos. Trans. R. Soc. B Biol. Sci. 367, 1379–1390 (2012).
Sunderaraman, P. & Cosentino, S. Integrating the constructs of anosognosia and metacognition: A review of recent findings in dementia. Curr. Neurol. Neurosci. Rep. 17, 27 (2017).
Agnew, S. K. & Morris, R. G. The heterogeneity of anosognosia for memory impairment in Alzheimer’s disease: A review of the literature and a proposed model. Aging Ment. Health. 2, 7–19 (1998).
Morris, R. G. & Mograbi, D. C. Anosognosia, autobiographical memory and self knowledge in Alzheimer’s disease. Cortex 49, 1553–1565 (2013).
American Psychiatric Association. Obsessive-compulsive and related disorders. In Diagnostic and Statistical Manual of Mental Disorders, 5th edn (American Psychiatric Association, 2013).
Frost, R. O., Tolin, D. F. & Maltby, N. Insight-related challenges in the treatment of hoarding. Cogn. Behav. Pract. 17, 404–413 (2010).
Worden, B. L., Di Loreto, J. & Tolin, D. F. Insight and Motivation. In The Oxford Handbook of Hoarding and Acquiring (eds Frost, R. O. & Steketee, G.) (Oxford University Press, 2014)
Eisen, J. L. et al. The brown assessment of beliefs scale: Reliability and validity. Am. J. Psychiatry. 155, 102–108 (1998).
Mataix-Cols, D., Billotti, D., de la Cruz, L. F. & Nordsletten, A. E. The London field trial for hoarding disorder. Psychol. Med. 43, 837–847 (2013).
Matsunaga, H., Hayashida, K., Kiriike, N., Nagata, T. & Stein, D. J. Clinical features and treatment characteristics of compulsive hoarding in Japanese patients with obsessive-compulsive disorder. CNS Spectr. 15, 258–266 (2010).
Tolin, D. F., Fitch, K. E., Frost, R. O. & Steketee, G. Family informants’ perceptions of insight in compulsive hoarding. Cogn. Ther. Res. 34, 69–81 (2010).
Kim, H.-J., Steketee, G. & Frost, R. O. Hoarding by elderly people. Health Soc. Work. 26, 176–184 (2001).
De Berardis, D. et al. Insight and alexithymia in adult outpatients with obsessive–compulsive disorder. Eur. Arch. Psychiatry Clin. Neurosci. 255, 350–358 (2005).
Matsunaga, H. et al. Obsessive-compulsive disorder with poor insight. Compr. Psychiatry. 43, 150–157 (2002).
Samuels, J. F. et al. Hoarding in obsessive–compulsive disorder: Results from the OCD collaborative genetics study. Behav. Res. Ther. 45, 673–686 (2007).
Ravi Kishore, V., Samar, R., Janardhan Reddy, Y. C., Chandrasekhar, C. R. & Thennarasu, K. Clinical characteristics and treatment response in poor and good insight obsessive–compulsive disorder. Eur. Psychiatry. 19, 202–208 (2004).
Jakubovski, E. et al. Dimensional correlates of poor insight in obsessive–compulsive disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 35, 1677–1681 (2011).
Torres, A. R. et al. Clinical features of obsessive-compulsive disorder with hoarding symptoms: A multicenter study. J. Psychiatr. Res. 46, 724–732 (2012).
Grisham, J. R., Brown, T. A., Savage, C. R., Steketee, G. & Barlow, D. H. Neuropsychological impairment associated with compulsive hoarding. Behav. Res. Ther. 45, 1471–1483 (2007).
Grisham, J. R., Norberg, M. M., Williams, A. D., Certoma, S. P. & Kadib, R. Categorization and cognitive deficits in compulsive hoarding. Behav. Res. Ther. 48, 866–872 (2010).
McMillan, S. G., Rees, C. S. & Pestell, C. An investigation of executive functioning, attention and working memory in compulsive hoarding. Behav. Cogn. Psychother. 41, 610–625 (2013).
Ayers, C. R. et al. Executive functioning in older adults with hoarding disorder. Int. J. Geriatr. Psychiatry. 28, 1175–1181 (2013).
Woody, S. R., Kellman-McFarlane, K. & Welsted, A. Review of cognitive performance in hoarding disorder. Clin. Psychol. Rev. 34, 324–336 (2014).
Tolin, D. F., Villavicencio, A., Umbach, A. & Kurtz, M. M. Neuropsychological functioning in hoarding disorder. Psychiatry Res. 189, 413–418 (2011).
Tolin, D. F. et al. Neural mechanisms of decision making in hoarding disorder. Arch. Gen. Psychiatry. 69, 832 (2012).
Tolin, D. F., Witt, S. T. & Stevens, M. C. Hoarding disorder and obsessive–compulsive disorder show different patterns of neural activity during response inhibition. Psychiatry Res. Neuroimaging 221, 142–148 (2014).
Mathews, C. A. et al. Error-related brain activity dissociates hoarding disorder from obsessive-compulsive disorder. Psychol. Med. 46, 367–379 (2016).
Frost, R. O., Steketee, G., Tolin, D. F. & Renaud, S. Development and validation of the clutter image rating. J. Psychopathol. Behav. Assess. 30(3), 193–203 (2008).
First, M., Williams, J., Karg, R. & Spitzer, R. Structured Clinical Interview for DSM-5— Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV) (American Psychiatric Association, 2015).
Frost, R. O., Steketee, G. & Grisham, J. Measurement of compulsive hoarding: Saving inventory-revised. Behav. Res. Ther. 42, 1163–1182 (2004).
Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 23, 56–62 (1960).
Dozier, M. E. & Ayers, C. R. Validation of the clutter image rating in older adults with hoarding disorder. Int. Psychogeriatr. 27, 769–776 (2015).
Steketee, G., Frost, R. O. & Kyrios, M. Cognitive aspects of compulsive hoarding. Cogn. Ther. Res. 27, 463–479 (2003).
Frost, R. O. & Hristova, V. Assessment of hoarding. J. Clin. Psychol. 67, 456–466 (2011).
Uttl, B. North American adult reading test: Age norms, reliability, and validity. J. Clin. Exp. Neuropsychol. 24, 1123–1137 (2002).
Oldfield, R. C. The assessment and analysis of handedness: The Edinburgh inventory. Neuropsychologia 9, 97–113 (1971).
Williams, S. M. A major revision of the Edinburgh Handedness Inventory: The EHI-8. Neuropsychologia https://doi.org/10.13140/RG.2.2.15176.55042/1 (2020).
Silverstein, S. M. et al. Development and validation of a World-Wide-Web-based neurocognitive assessment battery: WebNeuro. Behav. Res. Methods. 39, 940–949 (2007).
Paul, R. H. et al. Preliminary validity of “Integneuro”: A new computerized battery of neurocognitive tests. Int. J. Neurosci. 115, 1549–1567 (2005).
Mathersul, D. et al. Explicit identification and implicit recognition of facial emotions: II. Core domains and relationships with general cognition. J. Clin. Exp. Neuropsychol. 31, 278–291 (2009).
Williams, L. M. et al. Explicit identification and implicit recognition of facial emotions: I. Age effects in males and females across 10 decades. J. Clin. Exp. Neuropsychol. 31, 257–277 (2009).
Kellman-McFarlane, K. et al. Saving Inventory – Revised: Psychometric performance across the lifespan. J. Affect. Disord. 252, 358–364 (2019).
Tolin, D. F., Meunier, S. A., Frost, R. O. & Steketee, G. Hoarding among patients seeking treatment for anxiety disorders. J. Anxiety Disord. 25, 43–48 (2011).
DiMauro, J., Tolin, D. F., Frost, R. O. & Steketee, G. Do people with hoarding disorder under-report their symptoms?. J. Obsessive-Compuls. Relat. Disord. 2, 130–136 (2013).
Kashyap, H., Kumar, J. K., Kandavel, T. & Reddy, Y. C. J. Neuropsychological correlates of insight in obsessive-compulsive disorder: Neuropsychology of insight in OCD. Acta Psychiatr. Scand. 126, 106–114 (2012).
Manarte, L. et al. Executive functions and insight in OCD: A comparative study. BMC Psychiatry 21(1), 1–11 (2021).
Bertrand, E., Landeira-Fernandez, J. & Mograbi, D. C. Metacognition and perspective-taking in Alzheimer’s disease: A mini-review. Front. Psychol. 7, 1812 (2016).
Moeller, S. J. et al. Impaired insight in cocaine addiction: Laboratory evidence and effects on cocaine-seeking behaviour. Brain 133, 1484–1493 (2010).
Amanzio, M. et al. Unawareness of deficits in Alzheimer’s disease: Role of the cingulate cortex. Brain 134, 1061–1076 (2011).
Camelo, E. et al. Clinical and cognitive correlates of insight in bipolar disorder. Psychiatr. Q. 90, 385–394 (2019).
Kerwin, L., Hovav, S., Hellemann, G. & Feusner, J. D. Impairment in local and global processing and set-shifting in body dysmorphic disorder. J. Psychiatr. Res. 57, 41–50 (2014).
Li, W. et al. Aberrant early visual neural activity and brain-behavior relationships in anorexia nervosa and body dysmorphic disorder. Front. Hum. Neurosci. 9, 301 (2015).
Tumkaya, S. et al. Schizophrenia with obsessive-compulsive disorder and obsessive-compulsive disorder with poor insight: A neuropsychological comparison. Psychiatry Res. 165, 38–46 (2009).
Konstantakopoulos, G., Tchanturia, K., Surguladze, S. A. & David, A. S. Insight in eating disorders: clinical and cognitive correlates. Psychol. Med. 41, 1951–1961 (2011).
Dias, V. V., Brissos, S. & Carita, A. I. Clinical and neurocognitive correlates of insight in patients with bipolar I disorder in remission. Acta Psychiatr. Scand. 117, 28–34 (2008).
Graziano, M. S. A. & Webb, T. W. The attention schema theory: A mechanistic account of subjective awareness. Front. Psychol. 6, 500 (2015).
Norman, L. J. et al. Error processing and inhibitory control in obsessive-compulsive disorder: A meta-analysis using statistical parametric maps. Biol. Psychiatry. 85, 713–725 (2019).
Riesel, A. The erring brain: Error-related negativity as an endophenotype for OCD-A review and meta-analysis. Psychophysiology 56, e13348 (2019).
Steketee, G. & Frost, R. O. Treatment for Hoarding Disorder: Therapist Guide 2nd edn (Oxford University Press, 2013).
Acknowledgements
The authors thank the study participants for their collaboration in the completion of this study. They are additionally grateful to Becky Fullmer for editorial assistance and to members of the Rodriguez Translational Therapeutics Laboratory for critical reading and discussion of the manuscript.
Funding
Preparation of this work was supported in part by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs (Dr. van Roessel), the Avy L. and Roberta L. Miller Foundation (Dr. van Roessel), NIMH R01MH105461 (Dr. Rodriguez), and a Stanford Department of Psychiatry and Behavioral Sciences Innovator Award (Dr. Rodriguez).
Author information
Authors and Affiliations
Contributions
Authors P.v.R., C.S., L.W., and C.R. designed the study; P.v.R., C.M., A.V., P.M., S.A., C.S., and C.R. collected the data, P.v.R., C.M., P.M., S.A., H.S., B.J., L.W., and C.R. analyzed the data, and P.v.R., C.M., L.G., L.W., and C.R. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
In the last 3 years, Dr. Rodriguez has served as a consultant for Biohaven Pharmaceuticals and received research grant support from Biohaven Pharmaceuticals and a stipend from APA Publishing for her role as Deputy Editor at The American Journal of Psychiatry. Dr. Williams has received fees for serving on the advisory board of One Mind Psyberguide. All other authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Roessel, P.J., Marzke, C., Varias, A.D. et al. Anosognosia in hoarding disorder is predicted by alterations in cognitive and inhibitory control. Sci Rep 12, 21752 (2022). https://doi.org/10.1038/s41598-022-25532-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-25532-4