Abstract
Patients with end stage renal disease (ESRD) are at high risk of developing upper tract urothelial carcinoma (UTUC). Due to high recurrence rate of UTUC in contralateral kidney and ureter, and high risk of complications related to surgery and anesthesia, whether it’s necessary to remove both kineys and ureters at one time remains in debate. We utilized Taiwanese UTUC Registry Database to valuate the difference of oncological outcomes and perioperative complications between patients with ESRD with unilateral and bilateral UTUC receiving surgical resection. Patients with ESRD and UTUC were divided into three groups, unilateral UTUC, previous history of unilateral UTUC with metachronous contralateral UTUC, and concurrent bilatetral UTUC. Oncological outcomes, perioperative complications, and length of hospital stays were investiaged. We found that there is no diffence of oncological outcomes including overall survival, cancer specific survival, disease free survival and bladder recurrence free survival between these three groups. Complication rate and length of hospital stay are similar. Adverse oncological features such as advanced tumor stage, lymph node involvement, lymphovascular invasion, and positive surgical margin would negatively affect oncological outcomes.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a prevalent disease that affects up to 14.9% of the population in the United States. Approximately 2% progresses to end-stage renal disease (ESRD) within the CKD population1. Renal replacement therapy (RRT), including peritoneal dialysis, hemodialysis, or transplantation, is indicated for ESRD in this population group1. The United States Renal Data System reported a global estimate of 2.6 million patients who received RRT in 2010. The number of individuals receiving RRT is estimated to double by 2030, with the anticipated increase in ESRD2.
Several risk factors for upper tract urothelial carcinoma (UTUC) have been proposed, including smoking, aristolochic acid, and arsenic intoxication, as well as patients with ESRD receiving RRT3,4. The cumulative incidence rates of UTUC increase as the patients progress to ESRD and start receiving dialysis, and the standardized incidence ratio increases to > 20–30 times in the first year of dialysis3. Possible mechanisms behind the high incidence of urothelial carcinoma in patients with ESRD include decreased urinary washout, uremia, chronic bladder irritation, and bladder involution5. Taiwan has the highest prevalence and incidence of ESRD with a higher survival rate of patients undergoing dialysis, and its incidence and prevalence have been increasing from 2010 to 20186,7. Moreover, Taiwan reported a higher UTUC incidence compared to other geographical regions, encompassing approximately 20–25% of all urothelial tumors8.
The standard treatment for patients with localized high-risk UTUC patients includes radical nephroureterectomy (RNU). However, UTUC is associated with an increased risk of recurrence of 22–47% in the bladder and 2–5% over the contralateral upper tract after treatment9. A previous series has demonstrated poor renal function as an independent predictive factor for contralateral recurrence in patients with UTUC. Patients with ESRD demonstrated almost 3 times the risk of developing contralateral recurrence10. If cancer progressing to metastatic disease, the survival rate is poor and patients with ESRD and metastatic UC have limited systemic treatment options, mainly immune checkpoint inhibitors since their renal function are poor and tend to be chemotherapy ineligible11,12,13. Some evidences and prognosis-predicting tools, such as Royal Marsden Hospital Score, have shown that patients with ESRD were associated with a higher risk of perioperative complications, postoperative mortality, and cardiovascular events and poor cancer prognosis14,15. Anesthesia and operation time were both predictive of postoperative major cardiac events (MACE)16,17.
In this study, we aimed to evaluate the oncological outcomes and perioperative complications of patients with ESRD with unilateral UTUC, recurrent contralateral UTUC, and synchronous bilateral UTUC as well as assess the potential role of prophylactic contralateral nephroureterectomy.
Results
Figure 1 shows the enrollment flowchart. The Taiwanese UTUC database consisted of 6131 individuals when we initiated this study. First, patients not receiving RNU (N = 881) were excluded. Among the remaining 5250 patients, 647 have EDRD receiving RRT. An additional 71 patients were excluded due to missing key information. Finally, this study included 576 patients with ESRD who had received RNU. Unilateral, sequential unilateral, and bilateral RNU accounted for 413, 99, and 64 cases, respectively.
Table 1 demonstrates the demographic data. The mean follow-up period was 45.1, 47.3, and 43.1 months, respectively. The mean age at diagnosis was in the 60 s, with female dominance in each group. The sequential RNU group demonstrated a higher percentage of frequent chemical exposure (p = 0.003). No significant difference in terms of other risk factors of UTUC (tobacco smoking, herbal supplements, arsenic water intake, and frequent hair-dying) and comorbidities was found between each group.
Table 2 exhibits the details of surgical parameters in each group. No difference was found in RNU types. The bilateral RNU group demonstrated a higher percentage of transperitoneal approach. Additionally, a significant difference in the type of bladder cuff resection was found between the three groups. Surgical margin status revealed no difference. Severe complications of Clavien-Dindo class III or higher were < 10% in each group and indicated no difference between groups. Median postoperative hospital stay is 8–9 days without difference between groups.
Table 3 lists the pathological features of each group. The bilateral RNU group demonstrated a significantly higher rate of multicentric tumor (p < 0.001) but smaller tumor size (p = 0.044). No difference in pathological tumor and lymph node stage was found between the three groups. The unilateral RNU group revealed a lower percentage of previous history or concurrent bladder UC (p < 0.001) than the other two groups. The bilateral RNU group exhibited a higher rate of carcinoma in situ (p = 0.023).
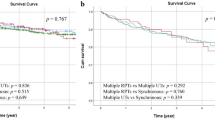
We initially investigated the association of demographic data, surgical parameters, and pathological features with OS, CSS, DFS, and BRFS using a univariant regression model to evaluate factors related to prognostic outcomes (Supplementary Table S1). Factors with statistical significance in each outcome were further analyzed using a multivariant regression model (Table 4). Older age, pathological tumor stage of > T2, positive lymphovascular invasion (LVI), and positive surgical margin were associated with worse OS. Additionally, these factors were associated with worse CSS except for age. Pathological tumor stages of > T3, positive lymph node metastasis, positive LVI, and positive surgical margin were associated with worse DFS. Positive LVI was related to worse BRFS. Unilateral, sequential, or bilateral UTUCs were not adverse factors of any prognostic outcomes (Fig. 2).
Discussion
This retrospective cohort study comprising 576 patients with UTUC who received curative-intent nephroureterectomy revealed no significant difference in the OS, CSS, DFS, and BRFS among the three groups. The univariate analysis generated 10 significantly associated factors when analyzing the possible prognostic factor for OS in this cohort. Multivariate analysis revealed age, pathological T-stage, LVI, and surgical margin to be significantly associated with the OS of these patients. In this study, we provide sufficient evidence to reveal that even patients with ESRD and unilateral UTUC receiving radical nephroureterctomy and encountering tumor recurrence in the contralateral upper urinary tract, the oncological outcomes are not different from those without recurrence. Moreover, the perioperative complications and hospital stay length are not different between patients receiving once or twice nephroureterctomy. Our findings suggest that it may not be necessary to perform prophylactic ipsilateral RNU for patients with ESRD and unilateral UTUC.
Nephroureterectomy is the primary treatment for patients with UTUC. A previous study revealed that patients who received nephroureterectomy demonstrated a better 5-year OS than those who did not receive such treatment despite the aforementioned risks, and such results remained even after adjusting for confounding factors18. If radical surgical resection is not performed for ESRD patients, standard alternative treatment of concurrent chemo-radiation therapy is not feasible due to poor renal function. Immune checkpoint inhibitors might be an another option, but there are potential adverse effects in ESRD patients and response rate and survival benefits remain unpredictable19,20,21,22. The benefit of surgery raises another question on the extent and the magnitude of the surgery. Different surgical operations have been proposed, including ipsilateral nephroureterectomy, bilateral nephroureterectomy, and complete urinary tract extirpation18,23. However, the efficacy and safety of the different surgical approaches remain debatable.
Urothelial carcinoma carries a multifocal nature, with any primary urothelial carcinoma as a risk factor for developing another urinary tract tumor24. A higher recurrence rate was observed in patients with ESRD with UTUC. Thus, extensive surgery of bilateral nephroureterectomy and even cystectomy have been proposed in this group of patients to achieve oncological benefit25,26,27. A previous study has analyzed patients with ESRD with bladder urothelial carcinoma and revealed that cystectomy with concurrent nephroureterectomy carries a better 5-year survival rate compared with cystectomy alone. A possible role of concurrent nephroureterectomy in improving survival benefits was noted28. Additionally, another study revealed that one-stage bilateral nephroureterectomy avoids 19.7% of subsequent contralateral nephroureterectomy within 2 years in patients on dialysis with UTUC18. Meanwhile, another study demonstrated no superior oncological outcome with one-stage complete urinary tract extirpation23. Thus, the potential beneficial role of preventive nephroureterectomy and cystectomy remains unknown. Our results also showed that there is no difference regarding the survival of unilateral UTUC without or without contralateral recurrence UTUC.
Radical nephroureterectomy itself is associated with morbidity and mortality. The operation was associated with 12.2–18.6% of 30-day overall complications and 11.3–18.2% of serious complications. Additionally, a study reported a 1% 30-day mortality rate29. A more extensive surgery with preventive contralateral nephroureterectomy and even cystectomy may pose an increased perioperative risk of complication24. Moreover, patients with ESRD carry higher perioperative and mortality risks compared to those without ESRD. This increased risk was demonstrated in both noncardiac and cardiac perioperative stages. Factors, including time of operation and anesthesia and the use of colloid and crystalloid, were more effective factors in the prediction model of postoperative complications in patients with ESRD16. One-stage complete urinary tract exenteration was associated with a higher risk of perioperative complication compared to multistage surgery30. Meanwhile, another study reported comparable safety in the unilateral and bilateral nephroureterectomy groups with no significant difference in blood loss and morbidity rate31. However, longer operative time and longer hospital stays remained. In this study, we found that there is no difference of perioperative complications between patients with once or twice RNU at different timepoints.
A possible stratification of the patients into different risk groups may generate a more specific population fit for the extensive and preventive operation, with the limited role of preventive contralateral nephroureterectomy seen in the cohort. Previous studies have analyzed prognostic factors in patients with UTUC using clinical, surgical, and pathological factors, and molecular markers, and have developed several predictive tools32,33. Pathological factors with tumor grade, tumor stage, carcinoma in situ, LVI, and lymph node invasion were considered prognostic factors32. A study then analyzed patients with ESRD with UTUC and revealed age at dialysis as an independent mortality predictor34. In this study, we have further analyzed possible poor prognostic factors for overall survival in patients with ESRD with UTUC. Multivariate analysis revealed age, pathological T-stage, LVI, and surgical margin to be significantly associated with a worse OS. Additionally, LVI was associated with CSS, DFS, and BRFS. A previous study revealed LVI as an independent predictive factor of poor survival in patients with UTUC35. A systemic review and meta-analysis of 17 trials has further revealed LVI as a poor prognostic factor in DFS and CSS36. A recent study used propensity score-weighted analysis to eliminate possible confounding factors and revealed that LVI remains a significant predictive factor of poor metastatic-free survival, CSS, and OS in patients with UTUC37. We further analyzed its prognostic value in patients with ESRD with UTUC. A possible risk classification may stratify the ESRD cohorts into different risk groups with the incorporation of these factors. A potential oncological benefit in a more extensive, and preventive surgery may be observed for those at a higher risk of poor prognosis.
This cohort study has some strengths. We used the UTUC database, obtained data from multiple medical centers, and included a fair number of patients with a rather homogenous population comprised of mainly Asians. Additionally, the baseline characteristics of the three groups were similar, including, ECOG, age, tumor size, TNM stage, etc. Different survival curves were incorporated into the analysis, and comparable results were seen among the three groups. However, as with other retrospective studies, our study has some limitations. First, Its retrospective design poses selection bias. Second, some information, including the indications for different operation groups, could not be retrieved and analyzed due to the use of the UTUC database. These factors may result in potential bias. Third, we aimed to analyze the role of nephroureterectomy, but the incorporation of cystectomy in the analysis may better clarify the role of preventive operation.
In conclusion, the role of preventive contralateral nephroureterectomy in patients with ESRD remains debatable with the potential oncologic benefit and possible increased risk for perioperative morbidity and mortality. Our study included 576 patients with ESRD with UTUC and revealed no difference in oncological outcome in terms of OS, CSS, DFS, and BRFS between the unilateral, subsequent contralateral, and one-stage bilateral nephroureterectomy group. Preventive contralateral RNU may not be necessary for every patient with ESRD and unilateral UTUC. Risk stratification showed that patients with advanced tumor stage, lymph node involvement, and lymphovascular invasion may encountered worse survival rate, and preventive contralateral RNU may be applied to these patients.
Methods
Ethical considerations
The Institutional Review Board (IRB) of Chang Gung Memorial Hospital approved this study (IRB No. 202100079B0). This is an observational retrospective study used electrical medical records and identification information from individuals was delinked in the database. Informed consent was waived by the Institutional Review Board (IRB) of Chang Gung Memorial Hospital. All methods were performed in accordance with the relevant guidelines and regulations for research involving human participants.
Patient population
The Taiwanese UTUC Registry Database was used to retrieve the study data which collected clinical information of patients with UTUC from 19 participating Taiwanese Hospitals (Taipei Tzu Chi Hospital; Hualien Tzu Chi Hospital; Kaoshiung Medical University Hospital; Ditmanson Medical Foundation Chia-Yi Christian Hospital; Chang Gung Memorial Hospital, Linkou; Chang Gung Memorial Hospital, Chiayi; E-Da Hospital; Kaohsiung Veterans General Hospital; Taichung Veterans General Hospital; China Medical University Hospital; Taipei City Hospital; National Taiwan University Hospital; Taipei Medical University-Shuang Ho Hospital; Chi Mei Medical Center; Taiwan Adventist Hospital; Cardinal Tien Hospital; Far Eastern Memorial Hospital; Taipei Medical University Hospital; Mackay Memorial Hospital). The database was stored in the Taipei Tzu Chi Hospital Urology Research Study Group. Clinical information, including demographic data, cancer stage, surgical and medical treatment details, and disease outcomes, were recorded. The database included patients diagnosed with UTUC from July 1988 to July 2023. Information on curative surgeries for these patients was available from March 28, 2001, to February 8, 2023. The UTUC database included > 6000 patients at the date of data retrieval.
Patients diagnosed with ESRD receiving RRT were retrieved from the database, whereas those who had not received RNU or with missing data were excluded from the study. We categorized these patients into three groups according to RNU sequence: unilateral RNU: patients having one side UTUC and received only one side RNU; sequential unilateral RNU: patients receiving one side RNU for previous UTUC diagnosis and received contralateral RNU at present due to newly diagnosed UTUC; bilateral RNU: patients having synchronous bilateral UTUC and receiving bilateral RNU in one surgery.
Investigation parameters and outcomes
Demographic data, including age at diagnosis, gender, Eastern Cooperative Oncology Group (ECOG) performance status, UTUC risk factors, and comorbidities, were recorded. Perioperative parameters include surgical types (open, hand-assisted laparoscopic, pure laparoscopic, or robot-assisted) and approaches (transperitoneal or retroperitoneal), resection margin status, surgical complications, and length of hospital stay. Additionally, detailed pathological variables were recorded. Demographic, perioperative, and pathological parameters were investigated to evaluate the impact of prognostic outcomes, including overall survival (OS), cancer-specific survival (CSS), disease-free survival (DFS), and bladder recurrence-free survival (BRFS).
Statistical method
Some missing data were inevitable due to the complexity and long period of data collection. The statistical analysis was conducted for available data only. Differences between groups were compared using a two-sample Pearson Chi-square for categorical variables. The Kolmogorov–Smirnov test was used to evaluate continuous variables for normality. Univariable and multivariable binary logistic regression was performed for clinical and pathological parameters to assess their association with recurrence. The Kaplan–Meier estimator was used to estimate the rates of prognostic outcomes, and the stratified log-rank test was used to compare the survival curves. The Cox proportional hazard model was selected to evaluate the effect of the surgical approaches on the prognostic outcomes, alone and after potential confounder adjustments. All statistical assessments were two-tailed and considered statistically significant as p-values of < 0.05. IBM Statistical Package for the Social Sciences version 26 was used for statistical analyses.
Data availability
The data is available upon reasonable request to the corresponding author.
References
Gupta, R. et al. Epidemiology of end-stage kidney disease. Semin. Vasc. Surg. 34(1), 71–78 (2021).
Thurlow, J. S. et al. Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am. J. Nephrol. 52(2), 98–107 (2021).
Wang, S.-M. et al. Increased upper and lower tract urothelial carcinoma in patients with end-stage renal disease: A nationwide cohort study in Taiwan during 1997–2008. BioMed Res. Int. 2014, 149750 (2014).
Wang, S. M. et al. Increased risk of urothelial cancer in young and middle aged patients with end-stage renal disease. J. Formos. Med. Assoc. 114(1), 52–57 (2015).
Chang, C. H. et al. Renal diagnosis of chronic hemodialysis patients with urinary tract transitional cell carcinoma in Taiwan. Cancer 109(8), 1487–1492 (2007).
Lai, T. S. et al. Trends in the incidence and prevalence of end-stage kidney disease requiring dialysis in Taiwan: 2010–2018. J. Formos. Med. Assoc. 121(Suppl 1), S5-s11 (2022).
Wu, B. S. et al. Mortality rate of end-stage kidney disease patients in Taiwan. J. Formos. Med. Assoc. 121(Suppl 1), S12-s19 (2022).
Soria, F. et al. Epidemiology, diagnosis, preoperative evaluation and prognostic assessment of upper-tract urothelial carcinoma (UTUC). World J. Urol. 35(3), 379–387 (2017).
EAU Guidelines. Edn. Presented at the EAU Annual Congress Milan 2023. ISBN 978-94-92671-19-6.
Huang, P. C. et al. High incidence of and risk factors for metachronous bilateral upper tract urothelial carcinoma in Taiwan. Int. J. Urol. 13(7), 864–869 (2006).
Rizzo, A. et al. Peripheral neuropathy and headache in cancer patients treated with immunotherapy and immuno-oncology combinations: The MOUSEION-02 study. Expert Opin. Drug Metab. Toxicol. 17(12), 1455–1466 (2021).
Rizzo, A. et al. Pembrolizumab in patients with advanced upper tract urothelial carcinoma: a real-world study from ARON-2 project. Clin. Exp. Metastasis. 6, 66 (2024).
Rizzo, A. et al. Expression of programmed cell death ligand 1 as a predictive biomarker in metastatic urothelial carcinoma patients treated with first-line immune checkpoint inhibitors versus chemotherapy: A systematic review and meta-analysis. Eur. Urol. Focus 8(1), 152–159 (2022).
Sahin, T. K. et al. Prognostic significance of the Royal Marsden Hospital (RMH) Score in patients with cancer: A systematic review and meta-analysis. Cancers 16(10), 1835 (2024).
Guven, D. C. et al. The association between albumin levels and survival in patients treated with immune checkpoint inhibitors: A systematic review and meta-analysis. Front. Mol. Biosci. 9, 1039121 (2022).
Jeong, Y. S. et al. Prediction of postoperative complications for patients of end stage renal disease. Sensors 21(2), 66 (2021).
Go, A. S. et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 351(13), 1296–1305 (2004).
Huang, C. E. et al. Nephroureterectomy increase 5 year survival in patients on dialysis with upper urinary tract urothelial carcinoma. Oncotarget 8(45), 79876–79883 (2017).
Mollica, V. et al. Current strategies and novel therapeutic approaches for metastatic urothelial carcinoma. Cancers 12(6), 1449 (2020).
Monteiro, F. S. M. et al. Efficacy of immune checkpoint inhibitors combinations as first-line systemic treatment in patients with advanced urothelial carcinoma: A systematic review and network meta-analysis. Crit. Rev. Oncol. Hematol. 196, 104–321 (2024).
Santoni, M. et al. Real-world effectiveness of pembrolizumab as first-line therapy for cisplatin-ineligible patients with advanced urothelial carcinoma: The ARON-2 study. Cancer Immunol. Immunother. 72(9), 2961–2970 (2023).
Fiala, O. et al. Use of concomitant proton pump inhibitors, statins or metformin in patients treated with pembrolizumab for metastatic urothelial carcinoma: Data from the ARON-2 retrospective study. Cancer Immunol. Immunother. 72(11), 3665–3682 (2023).
Huang, Y. C. et al. Treatment strategy for dialysis patient with urothelial carcinoma. Diagnostics 11(11), 66 (2021).
Zein, M. et al. Concurrent radical cystectomy and nephroureterectomy indications and outcomes: A systematic review and comparative analysis. Ther. Adv. Urol. 15, 17562872231171756 (2023).
Huang, Y. C. et al. Perioperative complications and mortality in patients with urothelial carcinoma and end-stage renal disease undergoing one-stage complete urinary tract extirpation. Ann. Surg. Oncol. 25(2), 573–581 (2018).
Wu, C. F. et al. Different treatment strategies for end stage renal disease in patients with transitional cell carcinoma. J. Urol. 171(1), 126–129 (2004).
Wang, T. Y. et al. High incidence and recurrence of transitional cell carcinoma in Taiwanese patients with end-stage renal disease. Nephrology 16(2), 225–231 (2011).
Tseng, S. F. et al. Long-term outcome of radical cystectomy in ESDR patients with bladder urothelial carcinoma. Int. Urol. Nephrol. 43(4), 1067–1071 (2011).
Levy, A. et al. Perioperative complications and adverse sequelae of radical nephroureterectomy. Transl. Androl. Urol. 9(4), 1853–1859 (2020).
Ou, C. H. et al. Long-term outcomes of complete urinary tract exenteration for dialysis patients with urothelial cancer. Int. Urol. Nephrol. 49(4), 623–627 (2017).
Zhang, Q. et al. Bilateral nephroureterectomy versus unilateral nephroureterectomy for treating de novo upper tract urothelial carcinoma after renal transplantation: A comparison of surgical and oncological outcomes. Clin. Med. Insights Oncol. 15, 11795549211035540 (2021).
Lughezzani, G. et al. Prognostic factors in upper urinary tract urothelial carcinomas: A comprehensive review of the current literature. Eur. Urol. 62(1), 100–114 (2012).
Mbeutcha, A. et al. Prognostic factors and predictive tools for upper tract urothelial carcinoma: A systematic review. World J. Urol. 35(3), 337–353 (2017).
Hung, P. H. et al. Urothelial carcinoma in patients with advanced kidney disease: A 12-year retrospective cohort survey. Am. J. Med. Sci. 342(2), 148–152 (2011).
Novara, G. et al. Prognostic role of lymphovascular invasion in patients with urothelial carcinoma of the upper urinary tract: An international validation study. Eur. Urol. 57(6), 1064–1071 (2010).
Ku, J. H. et al. Lymphovascular invasion as a prognostic factor in the upper urinary tract urothelial carcinoma: A systematic review and meta-analysis. Eur. J. Cancer 49(12), 2665–2680 (2013).
Chang, Y. L. et al. The prognostic impact of lymphovascular invasion for upper urinary tract urothelial carcinoma: A propensity score-weighted analysis. Medicine 102(15), e33485 (2023).
Author information
Authors and Affiliations
Contributions
Study conception and design were done by YC Tsai, ST Pang, and PH Lin. Material preparation, data collection were performed by TC Lin, GH Chen, CC Yeh, HL Ke, WM Li, Marcelo C and SH Lo. Data analysis were performed by SH Wu, CY Huang, CH Chen and WR Lin. The first draft of the manuscript was written by TC Lin and all authors commented on previous versions of the manuscript. PH Lin supervised and revised the final version of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, TC., Chen, GH., Yeh, CC. et al. No difference in oncological outcomes and perioperative complications between patients with ESRD with unilateral and bilateral UTUC receiving radical nephroureterectomy. Sci Rep 14, 17766 (2024). https://doi.org/10.1038/s41598-024-68872-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-68872-z