Abstract
The cerebral biomarkers, neurofilament light chain (NfL), amyloid-β, tau, and neuron specific enolase (NSE) reflect a wide spectrum of neurological damage in the brain and spinal cord. With this study, we aimed to assess whether these biomarkers hold any potential diagnostic value for the three most common canine neurological diseases. Canines suffering from meningoencephalitis of unknown origin (MUO), brain tumors, and selected non-infectious myelopathies were included. For each diagnosis, we analyzed these biomarkers in the cerebrospinal fluid collected via cranial puncture from the cisterna magna. Elevated levels of CSF tau, NfL, and NSE were observed in MUO, with all three biomarkers being intercorrelated. Tau and NSE were increased while amyloid-β was decreased in dogs suffering from tumors. In contrast, no biomarker changes were observed in dogs with myelopathies. Covariates such as age, sex, or castration had minimal impact. CSF biomarkers may reflect molecular changes related to MUO and tumors, but not to non-infectious myelopathies. The combination of NfL, tau, and NSE may represent useful biomarkers for MUO as they reflect the same pathology and are not influenced by age.
Similar content being viewed by others
Introduction
To date, the diagnosis neurological disorders of the central nervous system (CNS) constitutes a considerable challenge for human and veterinary medicine1,2,3. Thorough clinical evaluation and structural imaging are an essential part of diagnostic algorithms for human CNS disorders. Yet, especially in earlier stages of neurodegenerative disorders, these tools are insufficient to diagnose diffuse processes such as neurodegeneration4, and do not allow the assessment of the underlying pathophysiological changes that are responsible for the observed atrophy and neurological deficits, with negative impact on both drug research5,6 and clinical practice. Identification of fluid biomarkers (either in cerebrospinal fluid or blood) which would be specific for individual neurological diseases and disease related pathologies has significantly contributed to drug development, early detection and monitoring of neurodegenerative conditions like Alzheimer’s Disease7, and could improve the diagnostic accuracy of brain disorders in veterinary practice as well, via complementing established diagnostic algorithms that are based on clinical assessment and structural imaging. Given the fact that canine disorders such as meningoencephalitis of unknown origin (MUO) are often fatal if left untreated8,9, accurate diagnosis is imperative to allow timely intervention, achieve remission, and increase survival10. In some instances, MUO is not readily distinguishable via established methodologies, it is worthwhile to consider other tools that could be incorporated in the arsenal of the veterinary clinician—such as fluid biomarkers. These are widely used for the diagnostics and prognostics of human neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease, or multiple sclerosis11,12. Tau and amyloid-β in the cerebrospinal fluid (CSF) represent cornerstone biomarkers for Alzheimer’s disease diagnostics, displaying very high specificity and sensitivity13,14,15, while NfL in the blood reflects disease activity and therapeutic efficacy in multiple sclerosis16; ultimately, studies on CSF biomarkers have led to the development of corresponding assays for blood biomarkers7, which are substantially less invasive, and more practical as well. In contrast, fluid biomarkers are used only marginally in veterinary practice with the notable exception of spinal cord injury prognostication17,18; most studies evaluating their diagnostic utility are focused predominantly on a single biomarker in one specific neurological disorder19,20,21,22. So far, only a few studies utilized a combined panel of biomarkers to diagnose neurological disorders, with main focus on assay sensitivity, specificity, and cut-offs to improve diagnostic accuracy23. Noteworthy exceptions include studies such as work done by Olby et al., to identify predictors of recovery from spinal cord injury24.
Based on initial feasibility assessment and review of literature18,22,25,26, four CSF biomarkers—tau, amyloid-β, NSE, and NfL—appeared to be the most suitable for a multi-marker study in dogs. In the present study, we tested these markers in the CSF of canines with non-infectious neurological disorders such as MUO, brain tumors, and selected non-infectious myelopathies. We analyzed their levels, and their ability to distinguish between the individual diagnoses.
Material and methods
Study design/case selection
CSF samples evaluated during the study were collected between September 2019 and June 2021. Client-owned dogs were recruited consecutively during the study at referral neurology clinics in Slovakia. CSF sampling were performed by experienced veterinary neurologists.
Diagnosis
Each patient underwent clinical and neurological examination with complete hematology and biochemistry assessment (concentrations of total protein, glucose, urea, creatinine, ALT, and ALP were measured).
Diagnosis of presumptive Meningoencephalitis of Unknown Origin (MUO) was made in accordance to previously described criteria27 based on clinical symptoms, neurological deficits and magnetic resonance imaging (MRI); for a case to be defined as MUO at least part of the suspected inflammatory lesion had to be located intracranially. A total of 47 dogs were diagnosed with (MUO), 19 dogs with (mostly intra-axial, N = 15) brain tumors (TUMORS) and 29 dogs with other non-infectious CNS diseases—Myelopathies and conditions leading to CSF flow abnormalities (Chiari malformation—CM, Syringomyelia—SM, Myelitis—M) were pooled for the purpose of this study under one experimental group called myelopathies (CM/SM/M); this should be considered a ‘miscellaneous’ group as there are differences between these three disorders. Cases of Steroid-Responsive Meningitis-Arteritis (SRMA) were excluded from the study. As owners were unwilling to let healthy dogs undergo anesthesia and CSF sampling, 66 dogs with Idiopathic Epilepsy (IE) were used as the control group instead (CTRL). See Table 1 for cohort characteristics.
Where indicated, the geographically most common infectious CNS diseases (Canine Distemper Virus, Tick-borne encephalitis, Anaplasmosis, Ehrlichiosis, Neosporosis, Toxoplasmosis) were excluded via CSF analysis in an external laboratory (Laboklin, Germany). In the cases where this could not be performed due to the financial restraints of the owners, a presumptive MUO diagnosis was made on the base of the satisfactory clinical response to systemic immunomodulatory treatment.
The presumptive diagnosis of tumors was based on MRI in accordance with previously described MR features of various tumors28,29. A definitive diagnosis was not possible, as tumour biopsy was deemed to be too invasive, and henceforth was declined by the owners.
Diagnoses of presumptive non-infectious myelopathies (CM/SM/M) were made in accordance with previously described criteria27,30,31,32. Presumptive diagnosis was made on the base of the signalment, breed predisposition, neurological deficits, laboratory workup, MRI findings and results of CSF analysis. In some cases, infectious CNS diseases were excluded via the analysis of CSF in the external laboratory.
Diagnosis of idiopathic epilepsy was made based on a history of two or more unprovoked epileptic seizures occurring at least 24 h apart, age at epileptic seizure onset of between six months and six years, unremarkable inter-ictal physical and neurological examination, no significant abnormalities on blood tests and urinalysis, and unremarkable fasting and post-prandial bile acids, MRI of the brain and CSF analysis33.
Collection of cerebrospinal fluid
Patients were anesthetized at veterinary clinics (premedication with opioids—butorfanol (Butomidor 10mg/ml, Richter Pharma AG, Wels, Austria), induction with propofol (Proposure 10mg/ml, Axience, Pantin, France), maintenance with isoflurane (IsoFlo 100% w/w, Zoetis, Prague, Czech Republic) with endotracheal intubation. CSF was collected via cranial puncture from the cerebellomedullar cistern (cisterna magna) in accordance with previously described technique34.
For each CSF sample, protein concentration, total nucleated cell count (TNCC) and differential cell count were assessed. Protein concentration was identified by Pandy´s reaction and TNCC was determined by Fuchs-Rosenthal counting chamber. In cases of CSF blood contamination during collection, a corrected estimate of the TNCC was done by subtracting one total nucleated cell for every 500 red blood cells34,35,36,37. When possible, differential cell counts were based on 100 cells counted from slides prepared from cytocentrifugation. Abnormal CSF was defined by the presence of pleocytosis or an abnormal CSF differential cell count. The cut-off value for a pleocytosis was TNCC over 5 cells/µL34,38,39. Remaining CSF samples were centrifuged at 1600 g for 10 min., frozen in polypropylene tubes (Sarstedt, Germany) at − 20 °C for ~ 2 months, transferred on dry ice, and stored at − 80 °C until analysis.
Measurement of protein concentration in CSF
The levels of Amyloid Beta-42 (Aβ42), total Tau (t-Tau, HTAU), Neuron-Specific Enolase (NSE) and neurofilament-light chain (NfL) in CSF were measured using commercially available single-parameter ELISA kits: Aβ42 by INNOTEST® β-AMYLOID(1–42)25, t-Tau by INNOTEST® hTAU Ag (both Fujirebio, Gent, Belgium)18, NSE by Neuron Specific Enolase ELISA (ALPCO, Salem, USA)26 and NfL by NF-light® ELISA (Umman Diagnostics, Umea, Sweden)22 according to the manufacturer recommendation (see Supplementary Table 1). Measurements were done in duplicates. Post-analysis evaluation was done by GraphPad Prism 8 (GraphPad Software, CA, USA).
Statistical analysis
Data processing and statistical analyses were performed in the R version 4.2.2 programming environment40. All alternative hypotheses were two-sided and statistical tests were performed at a significance level equal to 0.05. All empirical confidence intervals (CI) are Wald-type, 95%, and two-sided. All p-values and CIs are reported without correction for multiplicity, i.e., without adjustment.
Since measurements of all concentrations of four CSF proteins were done in duplicates, these were averaged, and these arithmetic averages were used in the subsequent statistical analyses. If one or both values were above the upper limit, the upper limit value was used., e.g., for Amyloid β1-42 “ > 4238”, Total tau “ > 2198.5”, Neurofilament-light chain “ > 40,000” (no upper limit for Neuron-specific enolase). To handle outliers, the concentrations were winsorized for each CSF protein and diagnosis using the Tukey quartile rule on both sides of the distribution (owing to symmetry), i.e., the values smaller than the first quartile minus 1.5 times of the interquartile range (IQR) and greater than the third quartile plus 1.5 times of the IQR were set at these limits.
The characteristics of the sample were calculated for each diagnosis and epileptic controls for sex (number of females and males), age (in years, median and range), and concentrations of the four CSF proteins (sample size n, mean, standard deviation). For CSF proteins, the CIs for expected values are also given. In cases where the lower limit of CI is below zero, it is truncated to zero. The distributions of concentrations of the four CSF proteins were visualized using boxplots.
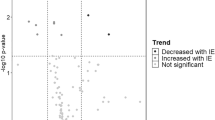
The effect of interest was the mean difference between all diagnoses and epileptic controls and all pairs of diagnoses. The null hypothesis mean difference is equal to zero was tested against the alternative hypothesis mean difference is not equal to zero by the two-sample Student t-test with Welch degrees of freedom for mean difference41. The results are summarized numerically as mean difference, standard deviations of mean difference, t-statistics, degrees of freedom, p-value, lower and upper bound of 95% CI for mean difference. The mean differences and the CIs of the mean difference were also visualized graphically.
Furthermore, the mean difference was adjusted by age, castration, and sex using of linear regression models as follows:
-
1.
concentration ~ diagnosis + age,
-
2.
concentration ~ diagnosis + sex,
-
3.
concentration ~ diagnosis + castration.
The results were summarized numerically and graphically as above but using least-squares marginal mean differences, i.e., adjusted mean differences42. All regression coefficients and effects, and their variances were estimated by ordinary least squares algorithm.
The linear association between the concentrations of all four CSF proteins was assessed using the Pearson correlation coefficient. The null hypothesis the correlation coefficient is equal to zero was tested against the alternative hypothesis the correlation coefficient is not equal to zero by Fisher z-test43. The results were summarized numerically by Pearson correlation coefficient, lower and upper bound of 95% CI for a correlation coefficient calculated using Fisher z-transformation, z-statistics, and p-value.
To assess the diagnostic ability of all four CSF proteins to distinguish the diagnoses or diagnoses from epileptic controls, the receiver operating characteristic (ROC) analysis was used44. The results were summarized numerically by area under the curve (AUC), lower and upper bound of 95% CI for an AUC, cut-off point, optimal sensitivity and specificity with respective lower and upper bound of 95% CI calculated using logit transformation. If the optimal sensitivity or specificity is equal to zero or one, related 95% CI is not reported. The ROCs were also visualized graphically.
Results
Study sample and cohorts
A total of 161 dogs (72 females, 89 males, median age 7.0 years, age range 0.5–16.0 years) were evaluated. General characteristics of the study cohorts, and descriptive statistics of biomarker levels are presented in Table 1. An illustration is provided in Fig. 1.
An overview of breeds is provided in Supplement 1.
The effect of covariates on The CSF biomarkers in canine neurological diseases
The mean Aβ1-42 concentration was significantly different between the epileptic control group and MUO (mean difference − 236.44, 95% CI − 471.66, − 1.21; SD difference 90.55; p = 0.04831), or tumors (mean difference − 577.49, 95% CI − 893.84, − 261.15; SD difference 121.78; p = 0.00003). There was no significant difference of Aβ1-42 concentration in CSF of the CM/SM/M group compared to epileptic controls (mean difference − 12.86, 95% CI − 290.58, − 264.87; SD difference 106.91; p = 0.99938). The tumors group also displayed significantly decreased CSF Aβ1-42 compared to the MUO (mean difference 341.05, 95% CI 9.19, 672.92; SD difference 127.75; p = 0.04147) and CM/SM/M (mean difference 564.64, 95% CI 201.41, 927.86; SD difference 139.83; p = 0.00049) group (Fig. 2A). Adjustment for age reduced the difference between MUO and epileptic controls group (mean difference − 213.35, 95% CI − 446.34, 19.65; SD difference 89.69; p = 0.09) and MUO and tumors group to non-significant levels (mean difference 273.97, 95% CI − 60.83, 608.77; SD difference 128.88; p = 0.150) (Fig. 2B). Adjustment for sex reduced the difference between MUO and epileptic controls group to non-significant levels (mean difference − 233.27, 95% CI − 472.26, 5.72; SD difference 91.98; p = 0.06) ((Fig. 2C).and adjustment for castration reduced the difference between MUO and epileptic controls group to non-significant levels (mean difference − 235.58, 95% CI − 473.39, 2.31; SD difference 91.56; p = 0.053) (Fig. 2D).
Comparisons of CSF biomarkers between diagnostic groups, with and without covariate adjustment. (A) No adjustment, (B) adjustment for age, (C) adjustment for sex, (D) adjustment for castration. See Supplement for details. Forrest plots show 95% CI for differences; CIs that do not include 0 denote significant differences, and are highlighted in red.
There was a significant increase of NfL in MUO (mean difference 20,354.98, 95% CI 11,564.60, 29,144.36; SD difference 3370.13; p ˂ 0.0001) when compared to epileptic controls. In contrast, the NfL concentration in CSF did not show significant differences between the epileptic control group and CM/SM/M (mean difference 10,046.08, 95% CI − 4.97, 20,097.12; SD difference 3853.89; p = 0.05016) or tumors group (mean difference 4781.13, 95% CI − 5656.63, 15,218.90; SD difference 4002.17; p = 0.63151). Except for the MUO vs. tumors comparison (mean difference 15,573.85, 95% CI 4314.42, 26,833.27; SD difference 4317.22; p = 0.00258), we did not observe any difference in mean NfL concentration between diagnoses (Fig. 2B). Adjustment for age increased the difference between CM/SM/M and epileptic control group to slight significant levels (mean difference 10,365.82, 95% CI 285.62, 20,446.03; SD difference 3864.55; p = 0.04137) (Fig. 2B). No effects of sex and castration were observed (Fig. 2C and D).
There was a significant increase in NSE concentration in Tumors (mean difference 52.08, 95% CI 23.90, 80.27; SD difference 10.81; p = 0.00003) when compared with the epileptic control group. No difference was found between MUO vs. epileptic controls (mean difference 16.69, 95% CI − 7.05, 40.42; SD difference 9.10; p = 0.26320) or CM/SM/M vs. epileptic controls (mean difference 15.29, 95% CI − 11.39, 41.97; SD difference 10.23; p = 0.44418). We found a significant increase in NSE in the tumors group when compared to MUO (mean difference − 35.40, 95% CI − 65.80, − 5.00; SD difference 11.66; p = 0.01552) or CM/SM/M (mean difference − 39.80, 95% CI − 69.55, − 4.04; SD difference 12.56; p = 0.02110). Adjustment for age reduced the difference between CM/SM/M and tumors group to non-significant levels (mean difference − 31.93, 95% CI − 67.45, 3.59; SD difference 13.62; p = 0.09429) (Fig. 2B). Effect of sex and castration were not observed (Fig. 2C and D).
We observed a significant increase of total tau in MUO (mean difference 51.47, 95% CI 30.99, 71.94; SD difference 7.88; p ˂ 0.0001) and tumors (mean difference 37.15, 95% CI 9.61, 64.68; SD difference 10.60; p = 0.00333) when compared to the epileptic control group. No significant difference was found between CM/SM/M and epileptic controls (mean difference 17.20, 95% CI − 6.38, 40.77; SD difference 9.08; p = 0.23454). We found a significant increase in total tau in the MUO when compared to CM/SM/M (mean difference 34.27, 95% CI 9.13, 59.41; SD difference 9.68; p = 0.00294). No differences between other diagnoses were observed. Effect of age, sex and castration were not observed (Fig. 2B–D). Detailed statistical results are listed in the supplement.
Correlation analyses of CSF biomarkers within diagnoses
In MUO and tumors there was a strong positive correlation between all biomarkers of brain injury (tau, NfL and NSE), but not with amyloid β. In the CM/SM/M group, only total tau and NfL were correlated (see Table 2).
Specificity and sensitivity of individual biomarkers in canine neurological disorders
MUO vs epileptic controls
Total tau discriminated MUO from epileptic controls (AUC 0.84 [95% CI 0.74, 0.90], cut-off 35.67 pg/mL) 80% optimal sensitivity (95% CI 0.65, 0.90) and 74% optimal specificity (95% CI 0.27, 0.96); NfL (AUC 0.90 [95% CI 0.79, 0.95], cut-off 3625.4 pg/mL) with 70% optimal sensitivity (95% CI 0.52, 0.84) and 100% optimal specificity; NSE (AUC 0.67 [95% CI 0.53, 0.78], cut-off 21.52 pg/mL), with 70% optimal sensitivity (95% CI 0.48, 0.86) and 65% optimal specificity (95% CI 0.38, 0.84); Aβ1-42 (AUC 0.65 [95% CI 0.54, 0.75], cut-off 1471.28 pg/mL), with 49% optimal sensitivity (95% CI 0.33, 0.65) and 88% optimal specificity (95% CI 0.61, 0.97) (Fig. 3A).
Sensitivity and specificity of Aβ1-42, NfL, NSE and total tau biomarkers for the differentiation between diagnostic groups. Sensitivity and specificity of biomarkers to distinguish between the control group with Idiopathic Epilepsy (controls) and individual diagnoses (MUO, tumors, CM/SM/M) (A–C), among diagnoses (D–F), and individual diagnoses vs. the other two (G–I) is shown. MUO = Meningoencephalitis of Unknown Origin; CM/SM/M, Chiari malformation = CM, Syringomyelia = SM, Myelitis = M; sensitivity = optimal sensitivity (TPF); specificity = optimal specificity (1 − FPF).
Tumors vs epileptic controls
Aβ1-42 discriminated tumors from epileptic controls (AUC 0.86 [95% CI 0.71, 0.94], cut-off 1444.75 pg/mL), with 79% optimal sensitivity (95% CI 0.55, 0.92) and 91% optimal specificity (95% CI 0.26, 1); total tau protein (AUC 0.86 [95% CI 0.71, 0.94], cut-off 48.45 pg/mL), with 74% optimal sensitivity [95% CI 0.49, 0.89] and 94% optimal specificity [95% CI 0.32, 1]); NSE (AUC 0.86 [95% CI 0.71, 0.94], cut-off 19.15 pg/mL), with 100% optimal sensitivity and 58% optimal specificity [95% CI 0.44, 0.71]); NfL (AUC 0.94 [95% CI 0.8, 0.98], cut-off 2837.45 pg/mL), with 83% optimal sensitivity (95% CI 0.55, 0.95) and 90% optimal specificity (95% CI 0.53, 0.99) (Fig. 3B).
CM/SM/M vs epileptic controls
NfL discriminated CM/SM/M from epileptic controls (AUC 0.73 [95% CI 0.57, 0.84], cut-off 2911.43 pg/mL), with 50% optimal sensitivity (95% CI 0.29, 0.71) and 92% optimal specificity (95% CI 0.02, 1); Aβ1-42 (AUC 0.49 [95% CI 0.36, 0.62], cut-off 1486.58 pg/mL), with 74% optimal sensitivity (95% CI 0.53, 0.88) and 14% optimal specificity (95% CI 0.03, 0.47); total tau protein (AUC 0.66 [95% CI 0.53, 0.77], cut-off 54.16 pg/mL), with 31% optimal sensitivity (95% CI 0.17, 0.50) and 100% optimal specificity; NSE (AUC 0.66 [95% CI 0.50, 0.79], cut-off 19.62 pg/mL), with 76% optimal sensitivity (95% CI 0.51, 0.91) and optimal specificity 58% (95% CI 0.27, 0.84) (Fig. 3C).
MUO vs tumors
Aβ1-42 discriminated MUO from tumors (AUC 0.71 [95% CI 0.56, 0.82], cut-off 1315.65 pg/mL) 69% optimal sensitivity (95% CI 0.47, 0.85) and 74% optimal specificity (95% CI 0.41, 0.92); NfL (AUC 0.63 [95% CI 0.46, 0.77], cut-off 14,134.72 pg/mL) with 47% optimal sensitivity (95% CI 0.30, 0.64) and 100% optimal specificity; NSE (AUC 0.71 [95% CI 0.55, 0.84], cut-off 51.02 pg/mL), with 73% optimal sensitivity (95% CI 0.40, 0.92) and 72% optimal specificity (95% CI 0.43, 0.90); total tau protein(AUC 0.52 [95% CI 0.37, 0.67], cut-off 46.38 pg/mL), with 47% optimal sensitivity (95% CI 0.28, 0.67) and 79% optimal specificity (95% CI 0.44, 0.95) (Fig. 3D).
MUO vs CM/SM/M
Aβ1-42 discriminated MUO from CM/SM/M (AUC 0.65 [95% CI 0.52, 0.77], cut-off 1471.95 pg/mL) 49% optimal sensitivity (95% CI 0.29, 0.70) and 82% optimal specificity (95% CI 0.54, 0.94); NfL (AUC 0.67 [95% CI 0.50, 0.80], cut-off 4821.3 pg/mL) with 63% optimal sensitivity (95% CI 0.42, 0.80) and 70% optimal specificity (95% CI 0.26, 0.94); NSE (AUC 0.50 [95% CI 0.34, 0.65], cut-off 103.32 pg/mL), with 80% optimal sensitivity (95% CI 0.58, 0.92) and 10% optimal specificity (95% CI 0.01, 0.59); total tau protein (AUC 0.68 [95% CI 0.55, 0.79], cut-off 31.80 pg/mL), with 91% optimal sensitivity (95% CI 0.70, 0.98) and 41% optimal specificity (95% CI 0.20, 0.66) (Fig. 3E).
CM/SM/M vs tumors
Aβ1-42 discriminated CM/SM/M from tumors (AUC 0.87 [95% CI 0.73, 0.94], cut-off 1309.08 pg/mL) 89% optimal sensitivity (95% CI 0.63, 0.97) and 74% optimal specificity (95% CI 0.36, 0.93); NfL (AUC 0.62 [95% CI 0.43, 0.78], cut-off 3379.07 pg/mL) with 60% optimal sensitivity (95% CI 0.37, 0.79) and 78% optimal specificity (95% CI 0.10, 0.99); NSE (AUC 0.74 [95% CI 0.56, 0.87], cut-off 40.00 pg/mL), with 67% optimal sensitivity (95% CI 0.26, 0.92) and 78% optimal specificity (95% CI 0.49, 0.93); total tau protein(AUC 0.69 [95% CI 0.53, 0.82], cut-off 44.40 pg/mL), with 66% optimal sensitivity (95% CI 0.37, 0.86) and 79% optimal specificity (95% CI 0.47, 0.94) (Fig. 3F).
CM/SM/M vs MUO, tumors
Aβ1-42 discriminated CM/SM/M for other two clinical diagnosis (AUC 0.72 [95% CI 0.58, 0.82], cut-off 1471.95 pg/mL, with 82% optimal sensitivity [95% CI 0.56, 0.94], and 58% optimal specificity [95% CI 0.38, 0.75]); total tau protein (AUC 0.68 [95% CI 0.55, 0.79], cut-off 42.47 pg/mL, with 66% optimal sensitivity [95% CI 0.42, 0.84], and 69% optimal specificity [95% CI 0.49, 0.84]); NfL (AUC 0.65 [95% CI 0.49, 0.78], cut-off 3379.07 pg/mL, with 60% optimal sensitivity [95% CI 0.35, 0.81], and 73% optimal specificity [95% CI 0.42, 0.91]); NSE (AUC 0.59 [95% CI 0.44, 0.73], cut-off 40.00 pg/mL, with 67% optimal sensitivity [95% CI 0.38, 0.87], 54% optimal specificity [95% CI 0.33, 0.74]) (Fig. 3G).
Tumors vs MUO, CM/SM/M
Aβ1-42 discriminated tumors from other clinical diagnoses (AUC 0.77 [95% CI 0.61, 0.87], cut-off 1309.08 pg/mL, with 74% optimal sensitivity [95% CI 0.43, 0.91], and 76% optimal specificity [95% CI 0.58, 0.89]); NSE (AUC 0.73 [95% CI 0.56, 0.85], cut-off 51.02 pg/mL, with 72% optimal sensitivity [95% CI 0.45, 0.89], and 73% optimal specificity [95% CI 0.41, 0.91]); total tau protein (AUC 0.59 [95% CI 0.44, 0.73], cut-off 46.38 pg/mL, with 79% optimal sensitivity [95% CI 0.51, 0.93], and 54% optimal specificity [95% CI 0.33, 0.74]); NfL (AUC 0.53 [95% CI 0.38, 0.68], cut-off 14,134.72 pg/mL, with 100% optimal sensitivity and 38% optimal specificity [95% CI 0.26, 0.52]) (Fig. 3H).
MUO vs CM/SM/M, tumors
Aβ1-42 discriminated MUO from other two clinical diagnosis (AUC 0.51 [95% CI 0.39, 0.62], cut-off 1198.47 pg/mL, with 20% optimal sensitivity [95% CI 0.08, 0.42] and 72% optimal specificity [95% CI 0.51, 0.86]); NfL (AUC 0.65 [95% CI 0.51, 0.77], cut-off 14,134.72 pg/mL, with 47% optimal sensitivity [95% CI 0.26, 0.68] and 87% optimal specificity [95% CI 0.58, 0.97]); NSE (AUC 0.60 [95% CI 0.46, 0.72], cut-off 51.02 pg/mL, with 73% optimal sensitivity [95% CI 0.47, 0.90] and 49% optimal specificity [95% CI 0.28, 0.70]), total tau protein (AUC 0.60 [95% CI 0.48, 0.71], cut-off 31.8 pg/mL, with 91% optimal sensitivity [95% CI 0.70, 0.98], 31% optimal specificity [95% CI 0.16, 0.52] (Fig. 3I).
Discussion
In the present study, we evaluated four CSF biomarkers which are commonly used for diagnostic purposes in human neurologic disorders, and assessed their diagnostic properties in three clinically relevant canine CNS disorders. All selected biomarkers are homologous to their human counterparts3,45,46,47. Tau is an indicator of axonal and neuronal damage, with CSF levels of total tau being positively correlated with the amount of tissue damage in a wide range of CNS conditions, including neurodegenerative disorders, injury, and prionoses48. NSE is a highly specific marker for neurons and peripheral neuroendocrine cells49. Its levels correlate with neurological and functional severity of traumatic brain and spinal cord injury, brain infarctions, and neuroendocrine tumors in human patients49,50,51,52 and inflammatory diseases such as GM1 gangliosidosis, encephalitis and canine distemper in dogs53,54,55. NfL is increased in CSF proportionally to the degree of axonal damage in a variety of neurological disorders, including inflammatory, neurodegenerative, traumatic, and cerebrovascular diseases56. Amyloid-β is considered to be a biomarker specific for senile amyloid plaques in Alzheimer’s disease; in brains of aged dogs, a large number of amyloid deposits are found46,57,58,59, accompanied by a decrease of amyloid-β in CSF57,60,61. Beside amyloid-β, these biomarkers are not specific for individual underlying pathologies, though, with changes occurring in response to a range of CNS disorders and injuries.
We have focused on the most common neurological disorders, meningoencephalitis of unknown origin or etiology (MUO, MUE), brain tumors, and selected non-infectious myelopathies.
Intracranial tumors of dogs are frequently encountered in veterinary medicine62,63,64, with incidence reported as 14.5 cases per 100,000 and prevalence being higher in middle-aged to older dogs65,66,67. Current diagnostic algorithms of brain neoplasms utilize clinical examination, imaging methods (CT, MRI) and analysis of selected CSF markers67,68,69.
Interestingly, in our study, we showed a significant decrease of Aβ42 levels in the tumor group and MUO when compared to epileptic controls and other diagnoses. Aβ42 discriminated tumors from epileptic controls with 91% specificity and 79% sensitivity and MUO from epileptic controls with 88% specificity and 49% sensitivity. Age being a crucial factor in the concentration of Aβ42 in CSF, with levels initially increasing with age, then decreasing in an age-dependent fashion57,60,61, we have evaluated whether adjusting for age would explain this difference in CSF Aβ42. Despite the age difference between the MUO, tumor group and epileptic controls or other diagnoses, respectively, correcting for age did not have pronounced impact on the results. This suggests a direct link between tumors, MUO and the amyloid-β pathway. Histopathological studies in similarly aged cohorts may shed light on the molecular mechanism; with further optimization of methodology, such studies may support the inclusion of amyloid-β in diagnostic algorithms in the future.
Similarly, we saw increased levels of NSE in tumors, with NSE discriminating tumors from other diagnoses with 72% optimal sensitivity and 73% optimal specificity and from epileptic controls with 100% optimal sensitivity and 58% optimal specificity. This is not sufficient to employ NSE as a single biomarker for diagnostic purposes; including it in a biomarker panel may be feasible though.
Meningoencephalitis of unknown origin or etiology—the most frequent canine non-infectious neuroinflammatory brain condition—constitutes 5–25% of all CNS disorders in dogs70,71. Affected animals display a variety of neurological signs including seizures. The disorder can presently only be truly confirmed based on histopathology9,27,72,73. Diagnosis of probable MUO is based on clinical signs, MRI, CSF analysis and exclusion of infectious agents27,74. Given that efficacious treatment options are available, the unmet need for improved diagnostic tools that would allow timely intervention is high.
The present study shows that the investigated CSF biomarkers of neuronal and axonal damage—tau and NfL—were significantly increased in dogs with MUO. On the other hand, Aβ was significantly decreased. Interestingly, there was high inter-correlation between these three biomarkers, suggesting that they may reflect the same pathological changes. However, the diagnostic accuracy of the abovementioned biomarkers was not sufficient to reliably discriminate MUO from other diagnoses. A previous study showed significantly higher levels of NfL in MUO dogs compared to healthy controls, with high sensitivity (> 89%) and specificity (> 96%). However, the healthy cohort in said study was younger than the MUO dogs, and the analysis was not adjusted for age, limiting interpretability22.
Chiari malformation (CM) and Syringomyelia (SM) are common conditions associated with myelopathies that frequently occur in small, brachycephalic, and toy dogs75,76,77. SM may be present in more than 50% of dogs with CM78,79. By definition, CM is a malformation of the skull and cranio-cervical junction which compromises the neural parenchyma to cause pain and/or disrupt CSF circulation, which can result in SM80. SM results in the development of fluid-containing cavities within the parenchyma of the spinal cord as a consequence of abnormal cerebrospinal fluid movement80. Currently, the diagnoses of CM or SM are based on clinical symptoms and imaging (MRI, CT)81,82,83. Myelitis (M) is defined as an inflammation of spinal cord parenchyma or meningomyelitis. Prevalence in veterinary medicine is relatively rare and most often is occurred in combination with inflammatory brain disease84,85. A clinical diagnosis of myelitis is typically made by a combination of clinical presentation, MRI, CT imaging of involved part of the CNS and results of cerebrospinal fluid (CSF) analysis9,84.
Our data did not show any significant changes of selected biomarkers in myelopathies, with levels of tau, NfL, NSE and Aβ being similar to the epileptic control group. It seems that myelopathies do not cause neuronal damage which could be monitored by these biomarkers. Previously, one study on dogs with intervertebral disc herniation (IVDH) showed significantly higher CSF tau concentrations in dogs showing plegia compared to healthy dogs and dogs with paresis18, however the study did not compare dogs with IVDH to other diagnoses.
While previous studies usually employed small cohorts with a single disorder, the present study considerably expands the available evidence base by evaluating a sizable cohort of 161 dogs of a wide range of breeds and assessing multiple biomarkers in multiple disorders. This has allowed assessing the utility of these markers and their combinations in differentiating common canine CNS disorders. Overall, the observed sensitivity, specificity, and ROCs are not yet at the levels of reliable diagnostic assays; further research is necessary before these CSF markers can be incorporated in veterinary diagnostic algorithms alongside clinical and imaging assessments. In their present state, they can be useful for disease monitoring, early pathology detection in neurogenetic conditions etc. Ultimately, it is also desirable to develop blood biomarker assays for dogs, as these are far less invasive and logistically significantly more expedient—and for many biomarkers such as NfL they are highly representative of levels measured in the CSF86.
Limitations
The present study has some limitations:
-
(a)
Dogs with idiopathic epilepsy were used as a control group instead of healthy individuals, as samples were collected at neurologic referral clinics whose ethical guidelines do not allow anesthesia in healthy individuals without indications that would justify it. The group did not include individuals with refractory epilepsy.
-
(b)
The study evaluates only diagnoses which are common at Slovak veterinary neurological clinics. A wider spectrum of neurologic disorders would provide greater insight into differences in biomarker patterns between disorders.
-
(c)
The most relevant differential diagnoses, MUO and Brain Tumors, reach the high probability level only and therefore remain “presumptive/suspected”, as no confirmatory tissue diagnosis could be performed. As such, the ability of biomarkers to discriminate between diagnoses might be hindered by an inaccurate diagnosis.
-
(d)
The results of centrally sampled biomarkers (e.g., from the cisterna magna) may differ from studies where sampling was performed at lumbar level 87, limiting comparability somewhat.
Conclusions
To sum up, we investigated four biomarkers—tau, Aβ, NfL and NSE—in three canine neurological diseases. The observed diagnostic accuracy was not sufficient to use them as a routine diagnostic or screening tool; however, in the case of MUO a combination of three of them (tau, Aβ and NfL) has potential to improve diagnostic precision. Future studies are warranted to assess their prognostic and theragnostic utility in the treatment of canine MUO.
These biomarkers could also be utilized in studies of molecular pathways involved in various canine CNS diseases.
Data availability
Please contact author for data requests.
References
Sisó, S. et al. Neurodegenerative diseases in domestic animals: A comparative review. Vet. J. 171(1), 20–38 (2006).
Noble, W. & Burns, M. Challenges in neurodegeneration research. Front. Psychiatry https://doi.org/10.3389/fpsyt.2010.00007 (2010).
Prpar Mihevc, S. & Majdič, G. Canine cognitive dysfunction and Alzheimer’s disease—Two facets of the same disease?. Front. Neurosci. https://doi.org/10.3389/fnins.2019.00604 (2019).
Lombardi, G. et al. Structural magnetic resonance imaging for the early diagnosis of dementia due to Alzheimer’s disease in people with mild cognitive impairment. Cochrane Database Syst. Rev. 3(3), CD009628 (2020).
Cullen, N. C. et al. Efficacy assessment of an active tau immunotherapy in Alzheimer’s disease patients with amyloid and tau pathology: A post hoc analysis of the “ADAMANT” randomised, placebo-controlled, double-blind, multi-centre, phase 2 clinical trial. EBioMedicine 99, 104923 (2024).
Salloway, S. et al. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s disease. N. Engl. J. Med. 370(4), 322–333 (2014).
Janelidze, S. et al. Head-to-head comparison of 10 plasma phospho-tau assays in prodromal Alzheimer’s disease. Brain 146(4), 1592–1601 (2023).
Lowrie, M., Smith, P. M. & Garosi, L. Meningoencephalitis of unknown origin: Investigation of prognostic factors and outcome using a standard treatment protocol. Vet. Rec. 172(20), 527 (2013).
Cornelis, I. et al. Clinical presentation, diagnostic findings, prognostic factors, treatment and outcome in dogs with meningoencephalomyelitis of unknown origin: A review. Vet. J. 244, 37–44 (2019).
Lowrie, M. et al. Effect of a constant rate infusion of cytosine arabinoside on mortality in dogs with meningoencephalitis of unknown origin. Vet. J. 213, 1–5 (2016).
Hall, S. et al. CSF biomarkers and clinical progression of Parkinson disease. Neurology 84(1), 57–63 (2015).
Blennow, K. & Zetterberg, H. Chapter one—Fluid biomarker-based molecular phenotyping of Alzheimer’s disease patients in research and clinical settings. In Progress in Molecular Biology and Translational Science (ed. Teplow, D. B.) 3–23 (Academic Press, 2019).
Blennow, K. & Zetterberg, H. Biomarkers for Alzheimer’s disease: Current status and prospects for the future. J. Intern. Med. 284(6), 643–663 (2018).
Jack, C. R. Jr. et al. NIA-AA research framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 14(4), 535–562 (2018).
Lleó, A. et al. Longitudinal cerebrospinal fluid biomarker trajectories along the Alzheimer’s disease continuum in the BIOMARKAPD study. Alzheimers Dement. 15(6), 742–753 (2019).
Bittner, S. et al. The potential of serum neurofilament as biomarker for multiple sclerosis. Brain 144(10), 2954–2963 (2021).
Olby, N. J. et al. Prognostic factors in canine acute intervertebral disc disease. Front. Vet. Sci. 7, 596059 (2020).
Roerig, A. et al. Cerebrospinal fluid tau protein as a biomarker for severity of spinal cord injury in dogs with intervertebral disc herniation. Vet. J. 197(2), 253–258 (2013).
Toda, Y. et al. Glial fibrillary acidic protein (gfap) and anti-gfap autoantibody in canine necrotising meningoencephalitis. Vet. Record 161(8), 261–264 (2007).
Toedebusch, C. M. et al. Cerebrospinal fluid levels of phosphorylated neurofilament heavy as a diagnostic marker of canine degenerative myelopathy. J. Vet. Intern. Med. 31(2), 513–520 (2017).
Panek, W. K. et al. Plasma neurofilament light chain as a translational biomarker of aging and neurodegeneration in dogs. Mol. Neurobiol. 57(7), 3143–3149 (2020).
Yun, T. et al. Neurofilament light chain as a biomarker of meningoencephalitis of unknown etiology in dogs. J. Vet. Intern. Med. 35(4), 1865–1872 (2021).
Zhang, L. et al. Cerebrospinal fluid and blood biomarkers in the diagnostic assays of Alzheimer’s disease. J. Innov. Opt. Health Sci. 15(01), 2230001 (2022).
Olby, N. J. et al. Time course and prognostic value of serum GFAP, pNFH, and S100beta concentrations in dogs with complete spinal cord injury because of intervertebral disc extrusion. J. Vet. Intern. Med. 33(2), 726–734 (2019).
Vikartovska, Z. et al. Novel diagnostic tools for identifying cognitive impairment in dogs: Behavior, biomarkers, and pathology. Front. Vet. Sci. 7, 551895 (2020).
Samanci, Y. et al. Neuron-specific enolase levels as a marker for possible neuronal damage in idiopathic intracranial hypertension. Acta Neurol. Belg. 117(3), 707–711 (2017).
Granger, N., Smith, P. M. & Jeffery, N. D. Clinical findings and treatment of non-infectious meningoencephalomyelitis in dogs: A systematic review of 457 published cases from 1962 to 2008. Vet. J. 184(3), 290–297 (2010).
Hecht, S. & Adams, W. H. MRI of brain disease in veterinary patients part 2: Acquired brain disorders. Vet. Clin. North Am. Small Anim. Pract. 40(1), 39–63 (2010).
Wisner, E. R., Dickinson, P. J. & Higgins, R. J. Magnetic resonance imaging features of canine intracranial neoplasia. Vet. Radiol. Ultrasound 52(1 Suppl 1), S52-61 (2011).
Rusbridge, C., Greitz, D. & Iskandar, B. J. Syringomyelia: Current concepts in pathogenesis, diagnosis, and treatment. J. Vet. Intern. Med. 20(3), 469–479 (2006).
Hechler, A. C. & Moore, S. A. Understanding and treating chiari-like malformation and syringomyelia in dogs. Top. Companion Anim. Med. 33(1), 1–11 (2018).
Mariani, C. L. et al. Cerebrospinal fluid lactate in dogs with inflammatory central nervous system disorders. J. Vet. Intern. Med. 33(6), 2701–2708 (2019).
De Risio, L. et al. International veterinary epilepsy task force consensus proposal: Diagnostic approach to epilepsy in dogs. BMC Vet. Res. 11, 148 (2015).
Di Terlizzi, R. & Platt, S. R. The function, composition and analysis of cerebrospinal fluid in companion animals: Part II—Analysis. Vet. J. 180(1), 15–32 (2009).
MacNeill, A. L. et al. The effects of iatrogenic blood contamination on total nucleated cell counts and protein concentrations in canine cerebrospinal fluid. Vet. Clin. Pathol. 47(3), 464–470 (2018).
Nagendran, A. et al. Risk factors for blood-contaminated cerebrospinal fluid collection in dogs. Vet. Rec. 186(16), e8 (2020).
Hurtt, A. E. & Smith, M. O. Effects of iatrogenic blood contamination on results of cerebrospinal fluid analysis in clinically normal dogs and dogs with neurologic disease. J. Am. Vet. Med. Assoc. 211(7), 866–867 (1997).
Chrisman, C. L. Cerebrospinal fluid analysis. Vet. Clin. North Am. Small Anim. Pract. 22(4), 781–810 (1992).
Hugo, T. B., Heading, K. L. & Labuc, R. H. Canine cerebrospinal fluid total nucleated cell counts and cytology associations with the prevalence of magnetic resonance imaging abnormalities. Vet. Med. (Auckl) 5, 75–84 (2014).
R_Core_Team. R: A language and environment for statistical computing (R Foundation for Statistical Computing, 2022).
Welch, B. L. The generalization of `student’s’ problem when several different population variances are involved. Biometrika 34(1/2), 28–35 (1947).
Searle, S. R., Speed, F. M. & Milliken, G. A. Population marginal means in the linear model: An alternative to least squares means. Am. Stat. 34(4), 216–221 (1980).
Winterbottom, A. A note on the derivation of fisher’s transformation of the correlation coefficient. Am. Stat. 33(3), 142–143 (1979).
Pepe, M. S. The Statistical Evaluation of Medical Tests for Classification and Prediction (Oxford University Press, 2004).
Stylianaki, I. et al. Amyloid-beta plasma and cerebrospinal fluid biomarkers in aged dogs with cognitive dysfunction syndrome. J. Vet. Intern. Med. 34(4), 1532–1540 (2020).
Smolek, T. et al. Tau hyperphosphorylation in synaptosomes and neuroinflammation are associated with canine cognitive impairment. J. Compar. Neurol. 524(4), 874–895 (2016).
National Center for Biotechnology Information Database (NCBI).
Blomme, E. A. G. & Waring, J. F. Cerebrospinal fluid biomarkers: Exploiting advances in humans to improve veterinary care. Vet. J. 197(2), 113–114 (2013).
Isgrò, M. A., Bottoni, P. & Scatena, R. Neuron-specific enolase as a biomarker: Biochemical and clinical aspects. In Advances in Cancer Biomarkers: From biochemistry to clinic for a critical revision (ed. Scatena, R.) 125–143 (Springer, 2015).
Bandyopadhyay, S. et al. Serum neuron-specific enolase as a predictor of short-term outcome in children with closed traumatic brain injury. Acad. Emerg. Med. 12(8), 732–738 (2005).
Selakovic, V., Raicevic, R. & Radenovic, L. The increase of neuron-specific enolase in cerebrospinal fluid and plasma as a marker of neuronal damage in patients with acute brain infarction. J. Clin. Neurosci. 12(5), 542–547 (2005).
El-Maraghi, S. et al. The prognostic value of neuron specific enolase in head injury. Egypt. J. Crit. Care Med. 1(1), 25–32 (2013).
Nakamura, K. et al. Proteome analysis of cerebrospinal fluid in healthy beagles and canine encephalitis. J. Vet. Med. Sci. 74(6), 751–756 (2012).
Satoh, H. et al. Cerebrospinal fluid biomarkers showing neurodegeneration in dogs with GM1 gangliosidosis: Possible use for assessment of a therapeutic regimen. Brain Res. 1133, 200–208 (2007).
Elias, B. C., Alfieri, A. F., Navarro, I. T. & Gomes, L. A. Neuron-specific enolase as biomarker for possible neuronal damage in dogs with distemper vírus. Pesquisa Veterinária Brasileira 39(01), 47–51 (2019).
Gaetani, L. et al. Neurofilament light chain as a biomarker in neurological disorders. J. Neurol. Neurosurg. Psychiatry 90(8), 870–881 (2019).
Head, E. et al. Amyloid-β peptide and oligomers in the brain and cerebrospinal fluid of aged canines. J. Alzheimer’s Dis. 20, 637–646 (2010).
Urfer, S. R. et al. Canine Cognitive Dysfunction (CCD) scores correlate with amyloid beta 42 levels in dog brain tissue. GeroScience 43(5), 2379–2386 (2021).
Schmidt, F. et al. Detection and quantification of β-amyloid, pyroglutamyl Aβ, and tau in aged canines. J. Neuropathol. Exp. Neurol. 74(9), 912–923 (2015).
Rusbridge, C. et al. An aged canid with behavioral deficits exhibits blood and cerebrospinal fluid amyloid beta oligomers. Front. Aging Neurosci. https://doi.org/10.3389/fnagi.2018.00007 (2018).
Borghys, H. et al. Young to middle-aged dogs with high amyloid-β levels in cerebrospinal fluid are impaired on learning in standard cognition tests. J. Alzheimer’s Dis. 56(2), 763–774 (2017).
Priester, W. A. & Mantel, N. Occurrence of tumors in domestic animals. Data from 12 United States and Canadian colleges of veterinary medicine. J. Natl. Cancer Inst. 47(6), 1333–44 (1971).
Song, R. B. et al. Postmortem evaluation of 435 cases of intracranial neoplasia in dogs and relationship of neoplasm with breed, age, and body weight. J. Vet. Intern. Med. 27(5), 1143–1152 (2013).
Snyder, J. M. et al. Canine intracranial primary neoplasia: 173 cases (1986–2003). J. Vet. Intern. Med. 20(3), 669–675 (2006).
Westworth, D. et al. Choroid plexus tumors in 56 dogs (1985–2007). J. Vet. Intern. Med. 22(5), 1157–1165 (2008).
Sturges, B. et al. Magnetic resonance imaging and histological classification of intracranial meningiomas in 112 dogs. J. Vet. Intern. Med. 22(3), 586–595 (2008).
Miller, A. D., Miller, C. R. & Rossmeisl, J. H. Canine primary intracranial cancer: A clinicopathologic and comparative review of glioma, meningioma, and choroid plexus tumors. Front. Oncol. https://doi.org/10.3389/fonc.2019.01151 (2019).
Wolff, C. A. et al. Magnetic resonance imaging for the differentiation of neoplastic, inflammatory, and cerebrovascular brain disease in dogs. J. Vet. Intern. Med. 26(3), 589–597 (2012).
Bentley, R. T. Magnetic resonance imaging diagnosis of brain tumors in dogs. Vet. J. 205(2), 204–216 (2015).
Braund, K. G. Granulomatous meningoencephalomyelitis. J. Am. Vet. Med. Assoc. 186(2), 138–141 (1985).
Tipold, A. Diagnosis of inflammatory and infectious diseases of the central nervous system in dogs: A retrospective study. J. Vet. Intern. Med. 9(5), 304–314 (1995).
Coates, J. R. & Jeffery, N. D. Perspectives on meningoencephalomyelitis of unknown origin. Vet. Clin. North Am. Small Anim. Pract. 44(6), 1157–1185 (2014).
Talarico, L. R. & Schatzberg, S. J. Idiopathic granulomatous and necrotising inflammatory disorders of the canine central nervous system: A review and future perspectives. J. Small Anim. Pract. 51(3), 138–149 (2010).
Nessler, J. N. et al. Canine meningoencephalitis of unknown origin-the search for infectious agents in the cerebrospinal fluid via deep sequencing. Front. Vet. Sci. 8, 645517 (2021).
Wijnrocx, K. et al. Twelve years of chiari-like malformation and syringomyelia scanning in Cavalier King Charles Spaniels in the Netherlands: Towards a more precise phenotype. PLoS One 12(9), e0184893 (2017).
Mitchell, T. J. et al. Syringomyelia: Determining risk and protective factors in the conformation of the Cavalier King Charles Spaniel dog. Canine Genet. Epidemiol. 1(1), 9 (2014).
Park, C. et al. Syringomyelia in three small breed dogs secondary to Chiari-like malformation: Clinical and diagnostic findings. J. Vet. Sci. 10(4), 365–367 (2009).
Wolfe, K. C. & Poma, R. Syringomyelia in the Cavalier King Charles spaniel (CKCS) dog. Can. Vet. J. 51(1), 95–102 (2010).
Rusbridge, C., McFadyen, A. K. & Knower, S. P. Behavioral and clinical signs of Chiari-like malformation-associated pain and syringomyelia in Cavalier King Charles spaniels. J. Vet. Intern. Med. 33(5), 2138–2150 (2019).
Knowler, S. P., Galea, G. L. & Rusbridge, C. Morphogenesis of Canine chiari malformation and secondary syringomyelia: Disorders of cerebrospinal fluid circulation. Front. Vet. Sci. 5, 171 (2018).
Rusbridge, C., Stringer, F. & Knowler, S. P. Clinical application of diagnostic imaging of Chiari-like malformation and syringomyelia. Front. Vet. Sci. 5, 280 (2018).
Rusbridge, C. & Knowler, S. P. Inheritance of occipital bone hypoplasia (Chiari type I malformation) in Cavalier King Charles Spaniels. J. Vet. Intern. Med. 18(5), 673–678 (2004).
Lu, D. et al. Neurological signs and results of magnetic resonance imaging in 40 cavalier King Charles spaniels with Chiari type 1-like malformations. Vet. Record 153(9), 260–263 (2003).
Griffin, J. F. et al. Meningomyelitis in dogs: A retrospective review of 28 cases (1999 to 2007). J. Small Anim. Pract. 49(10), 509–517 (2008).
Tipold, A. & Stein, V. M. Inflammatory diseases of the spine in small animals. Vet. Clin. North Am. Small Anim. Pract. 40(5), 871–879 (2010).
Wojdala, A. L. et al. Trajectories of CSF and plasma biomarkers across Alzheimer’s disease continuum: Disease staging by NF-L, p-tau181, and GFAP. Neurobiol. Dis. 189, 106356 (2023).
Rostgaard, N. et al. Differential proteomic profile of lumbar and ventricular cerebrospinal fluid. Fluids Barriers CNS 20(1), 6 (2023).
Acknowledgements
Our special thanks belong to the all the dedicated veterinary professionals, breeders, pet owners and technicians for taking part in the study.
Funding
This study was supported by APVV- 18-0515 (NZ), and VEGA 2/0127/22 (TS) research grants. The funding bodies were not involved in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
T.S., P.N., N.Z., S.K., and Z.V.K. conceived and designed the study, evaluated data, and wrote the manuscript. S.K. performed statistical analysis. I.H. and V.P. collected CSF samples. J.H., E.S. performed biomarker analysis. T.S., I.H., V.P., contributed to sample processing and testing. T.S., P.N., J.H., N.Z., S.K., I.H., V.P., Z.V.K. provided critical feedback. All authors listed reviewed the manuscript and provided feedback with writing and revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
The study was approved by the Ethics Committee of the Institute of Neuroimmunology in its proceedings on 10-OCT-2018. The study was carried in accordance with the European Communities Council Directive (2010/63/EU) regarding the use of animals in research and Slovak Law for Animal Protection 377/2012 and 436/2012. Written informed consent was obtained from the owners for the participation of their animals in this study; the consent form was approved by the abovementioned Ethics Committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Smolek, T., Vince-Kazmerova, Z., Hanes, J. et al. On the utility of cerebrospinal fluid biomarkers in canine neurological disorders. Sci Rep 14, 24129 (2024). https://doi.org/10.1038/s41598-024-73812-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-73812-y