Abstract
Establishing normal values of left atrial (LA) phasic strains and strain rates is essential for distinguishing between normal and abnormal functions, determining the degree of abnormality, and understanding the clinical significance of reported values in pediatrics. This meta-analysis aimed to establish normal values of two-dimensional speckle-tracking echocardiography (2DSTE)-derived LA phasic strains and strain rates in the pediatric population and identify the sources of inter-study heterogeneity for these values. A comprehensive search of PubMed, Scopus, and Embase databases was conducted using keywords such as “left atrial/left atrium,” “strain/speckle/deformation,” and “echocardiography” combined with pediatric age categories. Inclusion criteria comprised English-language human studies involving healthy subjects under 18 years of age. Subjects were categorized as neonates (up to 1 month), infants (1–12 months), and children (1–18 years). A random-effects model was applied to determine 2DSTE-derived LA strains and strain rates, and a meta-regression analysis was performed to investigate inter-study heterogeneity. Our analysis included 17 studies involving 1448 healthy subjects. For children, the mean values of LA strains during the reservoir, conduit, and contraction phases were 47.3% (95% CI 42.5–52.1%), 32.8% (95% CI 27.8–37.8%), and 12% (95% CI 10.0–14.1%), respectively. The mean values for LA strain rates were 2.4 s−1 (95% CI 1.1–3.8 s−1), 4.3 s−1 (95% CI 0.6–8.0 s−1), and 2.4 s−1 (95% CI 0.4–4.5 s−1), respectively. Inter-study heterogeneity for 2DSTE-derived LA phasic strains and strain rates was attributed to factors such as the number of study participants, publication year, software utilized, gating methods, the number of analyzed segments, the geographical region of the study, and heart rate. This study established the normal range of 2DSTE-derived LA phasic strains and strain rates. Additionally, inter-study heterogeneity was found to be influenced by various demographic, physiologic, and methodological factors.
Similar content being viewed by others
Introduction
The left atrium (LA) performs three phasic functions: reservoir, conduit, and contraction. These functions play crucial roles in regulating left ventricular (LV) filling and performance. LA phasic strains and strain rates can be used to evaluate these functions1. Two-dimensional speckle-tracking echocardiography (2DSTE) is a feasible, reproducible, and noninvasive tool that offers greater accuracy in measuring these parameters than conventional tissue Doppler imaging2.
In adults, LA phasic strains and strain rates are recognized as reliable echocardiographic indicators of LV systolic and diastolic dysfunction1. Moreover, these indicators have proven to be effective diagnostic parameters for assessing LV filling pressure and diastolic and systolic function in pediatric patients3.
Numerous studies have examined LA phasic strains and strain rates across pediatric age groups and populations, including those with normal and abnormal conditions4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19. These parameters have been identified as robust and sensitive prognostic factors for different pediatric age categories with various heart diseases, such as dilated, restrictive, and hypertrophic cardiomyopathies10,12,20,21,22,23. LA strains during the reservoir and contraction phases have been found to correlate with subtle LV systolic dysfunction in children with thalassemia. In contrast, LA strains during the reservoir and conduit phases have been linked to post-chemotherapy LV dysfunction17,18. Similarly, an association has been observed in acute conditions, such as post-COVID-19 multisystem inflammatory syndrome3. Chronic conditions have also demonstrated an association with LA mechanical impairment, as indicated by reports of subclinical LA mechanical dysfunction in children with transplanted hearts and those with chronic systemic diseases, such as diabetes mellitus and chronic kidney disease12,23,24.
Assessing pediatric LV diastolic function using echocardiography presents a challenge, as research suggests that diastolic parameters used in the adult population may not be suitable or practical for pediatric populations18,25. Additionally, the availability of age-related normal echocardiographic values for children has restricted the identification of diastolic dysfunction to a small subset of patients, while adult guidelines for assessing diastolic dysfunction have proven insufficient in identifying and classifying diastolic dysfunction in pediatric populations18.
Establishing the normal ranges of LA phasic strains and strain rates is essential for their application in pediatric populations. Although previous studies have investigated this topic, they have generally involved relatively small sample sizes. To our knowledge, no systematic review has been conducted on normal 2DSTE-derived LA phasic strains and strain rates in healthy pediatric populations. Thus, the primary objective of this study was to collect and analyze existing research on the normal range of 2DSTE-derived LA phasic strains and strain rates in children.
Methods
Search profile
We conducted multiple searches in PubMed, Scopus, and Embase databases through October 2023. Our search targeted specific keywords related to pediatric age categories, the LA, strains, speckle tracking, and echocardiography. (See Supplement 1 for details.) Only studies published in English were considered for this analysis. To ensure a comprehensive review, we also manually examined the references of identified studies to locate any additional relevant research. We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to maintain a systematic approach26.
Study selection
Studies were included in this analysis if they met the following criteria: (1) assessment of the pediatric LA using 2DSTE or velocity vector imaging, and (2) inclusion of a control group consisting of healthy individuals without cardiovascular diseases or risk factors. Studies were excluded if they focused on (1) preterm infants, (2) individuals over 18 years of age, (3) children with very high or very low body mass indices, or (4) animal subjects. Additionally, conference articles, case reports, editorials, letters to the editor commenting on published articles, review articles, articles without abstracts, and studies utilizing the same data set were excluded from the analysis. For articles that appeared to include participants over 18 years of age, corresponding authors were contacted via email for clarification. Studies were excluded if the authors failed to respond or justify the inclusion of participants beyond the specified age range. Age categorization was based on current standards27 with minor modifications: subjects up to 1 month of age were classified as neonates, those between 1 and 12 months as infants, and individuals between 1 and 18 years as children. This classification was applied to accommodate varying age classifications across different studies and address the limited research on the 2DSTE of the LA. Studies involving subjects between the ages of 5 and 18 years were also included to maximize the extraction of relevant findings. Some studies did not clearly define the age categories of excluded participants. In such cases, studies were included if the majority of subjects (or all but one) fell within a single age category based on the estimated mean and standard deviation of age. For studies that conducted two 2DSTE examinations within a single period, only the results from the first echocardiographic examination were included in the analysis. One study was excluded due to the absence of descriptions of the healthy group and uncertainty regarding the measurements performed by the researchers. To maintain consistency and accuracy, three groups of cardiologists (R.H. and T.H.; P.S. and R.M.; and N.T. and F.F.) independently evaluated the titles and abstracts of the selected studies after removing duplicates. Each group assessed one-third of the studies. A.H. reviewed all titles and abstracts. EndNote X9 (Clarivate, 2013, Philadelphia, PA) was used for reference management by the research groups. Any discrepancies between A.H. and each group of researchers were resolved through consensus after discussion. Afterward, each member of the cardiologist groups (R.H., T.D., P.S., R.M., N.T., and F.F.) reviewed the full texts of the selected studies based on their abstracts. Subsequently, A.H. independently re-evaluated the results of each group. The final selection of studies was determined through consensus between each group and A.H., ensuring that the selected studies met the predefined inclusion criteria and quality standards.
Data collection
Two cardiologist groups (R.H. and P.S. and R.M. and F.F.) independently assessed half of the full content of the eligible studies. They extracted demographic characteristics, clinical information, and echocardiographic data (particularly indicators of LA phasic functions) from the healthy control groups in each study. T.D. and N.T., followed by A.H., then cross-checked the data collected by each group. Any discrepancies between the three researchers were addressed through discussion and consensus. Studies suspected of using overlapping data sets were excluded from the analysis.
Statistical analysis
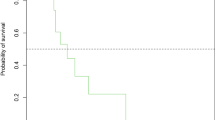
A random-effects model was employed to calculate the mean and 95% confidence interval (CI) for LA strains and strain rates. Cochran’s Q test (P-value < 0.1) was applied to assess inter-study heterogeneity, and I2 statistics were used to measure inter-study inconsistency. The results of each LA strain and strain rate were presented as forest plots, with the absolute values of LA strains and strain rates reported.
Meta-regression was conducted to assess how demographic, clinical, and echocardiographic variables contributed to the heterogeneity of the normal range for each LA strain value and strain rate. Subgroup analysis was conducted based on the geographical region of each study.
Publication bias was assessed using Begg’s test (P-value < 0.05). Stata software, Release 16 (College Station, TX: StataCorp LLC), was used for statistical analyses. The quality of the selected studies was evaluated using the Downs and Black method28, which is a frequently employed tool in similar meta-analyses29,30.
Two groups (R.H. and P.S. and R.M. and F.F.) independently appraised the quality of the selected studies. Disagreements were resolved through discussions between N.T. and each group member. A.H. subsequently re-evaluated the quality of the studies and finalized them through consultations with N.T.
Results
Figure 1 illustrates the PRISMA flowchart of the study. The final search on October 10, 2023, yielded 1652, 223, and 247 studies from PubMed, Scopus, and Embase, respectively. (See Supplement 1 for details.) After the removal of duplicates, 1727 studies were screened based on their abstracts. Seventy-eight studies were selected for full-text evaluation (Supplementary Table 1), and 17 studies were included in the final analysis. Table 1 summarizes the characteristics of the included studies. Table 2 presents the distribution of studies and related cases across different age categories (children, a subgroup of children aged 5–18 years, infants, and neonates) and 2DSTE-derived LA phasic strains and strain rates. Limited research was available on neonates, infants, and phasic strain rates in children, particularly in the subgroup of children aged 5 to 18 years.
Normal values of LA phasic strains and strain rates
Table 3; Figs. 2, 3, 4, 5, 6 and 7 display the mean normal values with 95% CIs, inter-study heterogeneity (represented by Q and associated P-values), and inconsistency (measured as I2) of 2DSTE-derived LA phasic strains and strain rates in children through forest plots. Additionally, Table 3 includes the mean normal values with 95% CIs for these markers in neonates, infants, and children aged 5 to 18 years. Significant inter-study heterogeneity and inconsistency were observed in studies examining LA phasic strains and strain rates in children. Nonetheless, the limited number of studies precluded the calculation of these parameters for infants, neonates, and the LA phasic strain rate in children aged 5 to 18 years.
Meta-regression analysis results
Meta-regression analysis was performed exclusively on studies involving children (Table 4).
Reservoir function markers
No significant inter-study heterogeneity was observed for longitudinal strains during the reservoir phase (LASr). However, the type of software used (B = 0.25, P-value = 0.033) and the number of analyzed segments (B = 0.35, P-value < 0.001) were identified as sources of inter-study heterogeneity for the peak longitudinal strain rate during the reservoir phase (pLASRr).
Conduit function markers
The type of software used (B = 2.07, P-value = 0.005) was identified as a source of inter-study heterogeneity for longitudinal strains during the conduit phase (LAScd). Additionally, the gating method (PP interval vs. RR interval) (B = 2.62, P-value = 0.012) and the number of analyzed segments (B = 0.72, P-value < 0.001) contributed to inter-study heterogeneity for the peak longitudinal strain rate during the conduit phase (pLASRcd).
Contraction function markers
The year of publication (B = − 0.57, P-value = 0.006) contributed to inter-study heterogeneity for longitudinal strains during the contraction phase (LASct). Further, the number of cases (B = − 0.03, P-value = 0.027), heart rate (B = 0.12, P-value = 0.023), and the number of analyzed segments (B = 0.37, P-value = 0.002) were identified as sources of inter-study heterogeneity for peak longitudinal strains during the contraction phase (pLASct).
Subgroup analysis by geographical regions and children aged 5–18 years
In the subgroup analysis, the mean normal values of 2DSTE-derived LA phasic strains and strain rates were compared across different geographical regions: East Asia, Europe, the Middle East, and North America. A statistically significant difference was found among LA phasic strains based on the geographical region (P-value < 0.001). Supplementary Tables 2 and Supplementary Figs. 1–6 provide the corresponding table and forest plots for these findings. Due to the limited number of studies on strain rates, only forest plots are presented in Supplementary Figs. 4–6. Moreover, LA phasic strains and strain rates in children aged 5–18 years are presented in Table 3 and Supplementary Figs. 7, 8 and 9. A statistically significant difference was observed in LA phasic strains within this age subgroup based on the geographical region (P-value < 0.001), as shown in Supplementary Figs. 10–12. However, only forest plots are provided for strain rates in Supplementary Figs. 12–15 owing to the scarcity of studies.
Quality of studies
All selected studies met more than 50% of the defined criteria. Sixteen studies (94%) fulfilled seven or more criteria (with one study meeting 10 criteria), and one study (5%) satisfied six criteria. All studies provided objective definitions, outcomes, characteristics of control groups, descriptions of confounders, key findings, and strain imaging protocols. Reproducibility analyses were conducted in all studies except one. In all studies, echocardiographers were not blinded to outcomes. (See Supplementary Table 3 for details.)
Publication bias
Begg’s test for publication bias assessment revealed nonsignificant results for the following LA phasic function parameters: LASr (P-value = 0.843), LAScd (P-value = 0.368), LASct (P-value = 0.348), pLASRr (P-value = 0.308), pLASRcd (P-value = 0.296), and pLASRct (P-value > 0.999).
Discussion
2DSTE provides a comprehensive examination of atrial phasic myocardial deformation and global atrial phasic function within a single cardiac cycle. LA phasic function components play a role in regulating LV filling and are likely impacted by LV diastolic properties and performance. LA reservoir function is synchronous with LV systole, while LA conduit function corresponds to LV early diastole, during which the LV fills with blood stored in the LA, and diastasis allows for passive blood flow from the pulmonary veins into the LV. LA contractile function significantly contributes to LA emptying and LV filling during the late diastolic phase31,32.
Assessing LV diastolic function in pediatric patients remains challenging. Still, LA myocardial deformation analysis using 2DSTE is a promising and feasible approach to improve our understanding and classification of diastolic dysfunction in children and adolescents. Moreover, a significant correlation has been observed between LA myocardial deformation parameters and invasive LV end-diastolic pressure measurements10.
LA strains and strain rates are useful in evaluating cardiac dysfunction in pre-adolescent athletes engaged in endurance sports7 and children with cardiomyopathies10, simple and complex congenital heart diseases4,33, valvular heart diseases34, Kawasaki disease8, or obesity6.
Previous meta-analyses have established normal range values for left and right ventricular STE-derived deformation markers in pediatric populations35,36. Nonetheless, there is a paucity of information on normal values for 2DSTE-derived LA strains and strain rates. Accurate interpretation of 2DSTE measurements in the context of LA strains and strain rates should account for both maturational changes in LA myocardium and age-specific reference values for LA phasic functions5. Unfortunately, the current literature provides limited information on the pediatric population in this area. Researchers have highlighted that diastolic parameters derived from adult studies lack sufficient discriminatory power when applied to pediatric populations25,37.
In this study, we present for the first time the normal values of 2DSTE-derived LA phasic strains and strain rates, serving as indices of LA phasic functions through meta-analyses in pediatrics. We also emphasize the ongoing knowledge gap regarding normal ranges for 2DSTE-derived LA phasic strains and strain rates in this population. The limited data on pediatric populations forced us to draw upon adult-related literature to interpret our findings in some instances. We aimed to provide a solid foundation for future research into pediatric LA phasic functions under physiological and pathological conditions by establishing these normal values.
Source of heterogeneity
Studies investigating the association of LA mechanical deformation indices with age have yielded conflicting results, with some reporting no correlation and others finding weak or moderate associations5,9,11,14. The majority of changes appear to occur during the first two years of life5. Furthermore, one study reported that the association between age and LA mechanical deformation indices disappeared after adjusting for LA volume14. Our meta-analysis findings align with the observations made by Jimbo et al.,11 as we did not identify age as a source of heterogeneity. Nevertheless, it is important to consider the limited number of studies included in our analysis.
Our meta-analysis did not identify sex as a source of heterogeneity. Although the impact of sex on LA mechanical deformation indices in pediatric populations remains understudied, one investigation found associations between some indices and sex in univariate analysis; however, these associations were not significant in multivariable analysis14.
Previous studies have reported associations between body surface area and LA mechanical deformation indices9,14. Be that as it may, these correlations were weak, and in one study, the association disappeared in multivariable analysis when LA volume was taken into consideration14. In our meta-analysis, body surface area was not identified as a source of heterogeneity.
Studies in pediatric populations have suggested a correlation between heart rate and LA strains and strain rates5. Our meta-analysis, however, did not demonstrate a statistical correlation between heart rate and LA mechanical deformation indices, except for pLASRct. This finding chimes with a study conducted on adult populations, which reported a nonsignificant effect of heart rate on LA mechanical deformation38. Nevertheless, tachycardia and the resulting decrease in diastolic time might be the primary factors contributing to increased LA strain rates (more so than LA strains) in younger children11. The limited availability of studies providing data on LA strain rates in our review could account for the discrepancies observed in our findings.
The impact of hypertension on LA phasic function remains understudied, although the effect of hypertension on reducing the global longitudinal strain of the LV has been reported39. Our meta-analysis did not identify blood pressure as a source of heterogeneity, likely because we only included studies with healthy subjects who had normal blood pressure ranges.
Our findings demonstrated that the software used for analysis contributed to inter-study heterogeneity, in line with previous studies that have compared different software programs for evaluating 2DSTE-derived deformation indices40,41,42.
Our findings indicated that the number of analyzed segments represented another source of heterogeneity. The EACVI/ASE/Industry Task Force43 advocated for standardizing deformation imaging and supported phasic strain and strain rate measurements in apical four-chamber views, along with the biplane measurement of these markers. Thus, it is reasonable to assume that analyzing more segments for the 2DSTE of the LA would provide more comprehensive information.
Our findings identified publication year and sample size as sources of inter-study heterogeneity, which may indirectly reflect the experience level of operators performing 2DSTE assessments30.
Zero reference points (the R or P-wave of electrocardiography), also known as gating, emerged as a source of inter-study heterogeneity in LA strain rates. Although gating is employed for the LA strain curve, it is not used for the LA strain rate curve. Consequently, we believe these results could be due to chance, given the limited number of studies available on LA strain rates.
Our findings identified the geographical region as an additional source of inter-study heterogeneity. The diverse racial and ethnic backgrounds of children living in East Asia, Europe, the Middle East, and North America may account for the differences in normal values of myocardial deformation across the selected studies. These variations could be related to disparities in nutritional status among these populations44,45,46.
The subgroup analysis of children aged 5–18 years revealed minimal differences when compared with the overall children group. This finding is consistent with previous studies, which reported a weak association between age and LA phasic strains, suggesting that age might not be an independent predictor of LA phasic strains5,9,11,14.
Publication bias
Our study did not reveal any publication bias; however, this result should be considered in the context of the limited number of available studies on our selected topics, particularly LA strain rates. To reduce the likelihood of overlooking relevant studies, we employed a balanced hierarchy approach when conducting our systematic review.
Although our study establishes a normal range for 2DSTE-derived LA phasic strains and strain rates in children, our findings should be viewed as preliminary due to the limited number of available studies. Nonetheless, these results provide a valuable reference range for researchers and clinicians who seek to assess LA phasic function for various purposes, such as evaluating improvements after disease-related deterioration. Our study also highlights the significant knowledge gap regarding the normal range of 2DSTE-derived LA phasic function markers in pediatric populations, particularly neonates and infants.
Study limitations
Our systematic review included 17 studies with 1448 participants, a sample size that may not be considered substantial. The scarcity of research on neonates and infants underscores the need for further investigation across all pediatric age groups. The presence of multiple sources of heterogeneity in our study may be attributed to the cross-sectional or observational designs of the included studies, which lacked randomization47. Additionally, the expertise level of operators performing 2DSTE, which was not reported in the selected studies, may have influenced our results. Concordant with other studies, we analyzed the provided data without considering the specific details of each study’s patient population. Furthermore, although we employed a predesigned quality assessment checklist, subjective factors may still have influenced the evaluation process29,48.
Conclusion
This systematic review established normal ranges of LA phasic strains and strain rates in children, as well as LA phasic strains in a subgroup of children aged 5 to 18 years. The normal ranges were found to be broad, with minimal differences observed between the overall children group and the subgroup of children aged 5 to 18 years regarding LA phasic strain. Methodological factors, along with geographic region and heart rate, were identified as the primary sources of inter-study heterogeneity. These normal ranges serve as a valuable resource for clinicians to identify abnormal results, while future studies are warranted to establish narrower and more precise reference values.
Data availability
Data is provided within supplementary information files.
References
Nagueh, S. F. & Khan, S. U. Left atrial strain for assessment of left ventricular diastolic function: focus on populations with normal LVEF. JACC Cardiovasc. Imaging. 16, 691–707. https://doi.org/10.1016/j.jcmg.2022.10.011 (2023).
Kupczyńska, K., Mandoli, G. E., Cameli, M. & Kasprzak, J. D. Left atrial strain - a current clinical perspective. Kardiol Pol. 79, 955–964. https://doi.org/10.33963/KP.a2021.0105 (2021).
Minocha, P. K. et al. Strain in children with MIS-C and acute COVID-19. Ann. Pediatr. Cardiol. 15, 459–466. https://doi.org/10.4103/apc.apc_93_22 (2022).
Khoo, N. S. et al. The assessment of atrial function in single ventricle hearts from birth to Fontan: a speckle-tracking study by using strain and strain rate. J. Am. Soc. Echocardiogr. 26, 756–764. https://doi.org/10.1016/j.echo.2013.04.005 (2013).
Kutty, S. et al. Functional maturation of left and right atrial systolic and diastolic performance in infants, children, and adolescents. J. Am. Soc. Echocardiogr. 26, 398–409e2. https://doi.org/10.1016/j.echo.2012.12.016 (2013).
Mahfouz, R. A., Gomma, A., Goda, M. & Safwat, M. Relation of left atrial stiffness to insulin resistance in obese children: Doppler strain imaging study. Echocardiography. 32, 1157–1163. https://doi.org/10.1111/echo.12824 (2015).
D’Ascenzi, F. et al. Atrial chamber remodelling in healthy pre-adolescent athletes engaged in endurance sports: a study with a longitudinal design. The CHILD study. Int. J. Cardiol. 223, 325–330. https://doi.org/10.1016/j.ijcard.2016.08.231 (2016).
Kang, S. J., Ha, J., Hwang, S. J. & Kim, H. J. Long term outcomes of left atrial reservoir function in children with a history of Kawasaki disease. J. Cardiovasc. Ultrasound. 26, 26–32. https://doi.org/10.4250/jcu.2018.26.1.26 (2018).
Cantinotti, M. et al. Left and right atrial strain in healthy caucasian children by two-dimensional speckle-tracking echocardiography. J. Am. Soc. Echocardiogr. 32, 165–168e3. https://doi.org/10.1016/j.echo.2018.10.002 (2019).
Sabatino, J. et al. Left atrial strain to identify diastolic dysfunction in children with cardiomyopathies. J. Clin. Med. 8, 1243. https://doi.org/10.3390/jcm8081243 (2019).
Jimbo, S. et al. Normal reference values for left atrial strains and strain rates in school children assessed using two-dimensional speckle-tracking echocardiography. Heart Vessels. 35, 1270–1280. https://doi.org/10.1007/s00380-020-01594-0 (2020).
Ifuku, M. et al. Left atrial dysfunction and stiffness in pediatric and adult patients with type 1 diabetes mellitus assessed with speckle tracking echocardiography. Pediatr. Diabetes. 22, 303–319. https://doi.org/10.1111/pedi.13141 (2021).
Matsubara, D. et al. Longitudinal assessment of cardiac outcomes of multisystem inflammatory syndrome in children associated with covid-19 infections. J. Am. Heart Assoc. 11, e023251. https://doi.org/10.1161/JAHA.121.023251 (2022).
Aristizábal-Duque, C. H. et al. The assessment of myocardial longitudinal strain in a paediatric Spanish population using a new software analysis. J. Clin. Med. 11, 3272. https://doi.org/10.3390/jcm11123272 (2022).
Chang, H. Y. et al. Subclinical changes in left heart structure and function at preschool age in very low birth weight preterm infants. Front. Cardiovasc. Med. 9, 879952. https://doi.org/10.3389/fcvm.2022.879952 (2022).
Ficial, B. et al. Feasibility, reproducibility and reference ranges of left atrial strain in preterm and term neonates in the first 48 h of life. Diagnostics (Basel). 12, 350. https://doi.org/10.3390/diagnostics12020350 (2022).
Luo, S. L., Deng, Y., Lan, W. F., Yang, Y. H. & Dai, P. Echocardiographic evaluation of left atrial strain for predicting iron overload in pediatric patients with β-thalassemia with preserved ejection fraction. Int. J. Cardiovasc. Imaging. 39, 895–906. https://doi.org/10.1007/s10554-022-02788-5 (2023).
Chen, J. et al. Assessment of left heart dysfunction to predict doxorubicin cardiotoxicity in children with lymphoma. Front. Pediatr. 11, 1163664. https://doi.org/10.3389/fped.2023.1163664 (2023).
Sabatino, J. et al. Mid- and long-term atrio-ventricular functional changes in children after recovery from COVID-19. J. Clin. Med. 12, 186. https://doi.org/10.3390/jcm12010186 (2022).
Zuckerberg, J. C. et al. Left atrial stiffness and strain are novel indices of left ventricular diastolic function in children: validation followed by application in multisystem inflammatory syndrome in children due to COVID-19. Eur. Heart J. Cardiovasc. Imaging. 24, 1241–1251. https://doi.org/10.1093/ehjci/jead087 (2023).
Sun, B. J. & Park, J. H. Echocardiographic measurement of left atrial strain - A key requirement in clinical practice. Circ. J. 86, 6–13. https://doi.org/10.1253/circj.CJ-21-0373 (2021).
Jhaveri, S. et al. Left atrial strain and function in pediatric hypertrophic cardiomyopathy. J. Am. Soc. Echocardiogr. 34, 996–1006. https://doi.org/10.1016/j.echo.2021.04.014 (2021).
Loar, R. W. et al. Left atrial strain correlates with elevated filling pressures in pediatric heart transplantation recipients. J. Am. Soc. Echocardiogr. 33, 504–511e1. https://doi.org/10.1016/j.echo.2019.11.004 (2020).
Doan, T. T. et al. Left ventricular strain and left atrial strain are impaired during hemodialysis in children. Int. J. Cardiovasc. Imaging. 37, 3489–3497. https://doi.org/10.1007/s10554-021-02350-9 (2021).
Recher, M. et al. Assessment of left-ventricular diastolic function in pediatric intensive-care patients: a review of parameters and indications compared with those for adults. World J. Pediatr. 17, 21–30. https://doi.org/10.1007/s12519-020-00369-x (2021).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372, n71. https://doi.org/10.1136/bmj.n71 (2021).
Williams, K. et al. Standard 6: age groups for pediatric trials. Pediatrics. 129, S153–S160. https://doi.org/10.1542/peds.2012-0055I (2012).
Downs, S. H. & Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health. 52, 377–384. https://doi.org/10.1136/jech.52.6.377 (1998).
Truong, V. T. et al. Normal ranges of left ventricular strain by three-dimensional speckle-tracking echocardiography in adults: a systematic review and meta-analysis. J. Am. Soc. Echocardiogr. 32, 1586–1597e5. https://doi.org/10.1016/j.echo.2019.07.012 (2019).
Pathan, F., D’Elia, N., Nolan, M. T., Marwick, T. H. & Negishi, K. Normal ranges of left atrial strain by speckle-tracking echocardiography: a systematic review and meta-analysis. J. Am. Soc. Echocardiogr. 30, 59–70e8. https://doi.org/10.1016/j.echo.2016.09.007 (2017).
Jain, V. et al. Contemporary narrative review on left atrial strain mechanics in echocardiography: cardiomyopathy, valvular heart disease and beyond. Cardiovasc. Diagn. Ther. 11, 924–938. https://doi.org/10.21037/cdt-20-461 (2021).
Yuda, S. Current clinical applications of speckle tracking echocardiography for assessment of left atrial function. J. Echocardiogr. 19, 129–140. https://doi.org/10.1007/s12574-021-00519-8 (2021).
Suzuki, K. et al. Influence of percutaneous occlusion of atrial septal defect on left atrial function evaluated using 2D speckle tracking echocardiography. Int. Heart J. 61, 83–88. https://doi.org/10.1536/ihj.19-173 (2020).
Shakti, D. et al. Left atrial size and function in patients with congenital aortic valve stenosis. Am. J. Cardiol. 122, 1541–1545. https://doi.org/10.1016/j.amjcard.2018.07.027 (2018).
Jashari, H. et al. Normal ranges of left ventricular strain in children: a meta-analysis. Cardiovasc. Ultrasound. 13, 37. https://doi.org/10.1186/s12947-015-0029-0 (2015).
Levy, P. T. et al. Normal ranges of right ventricular systolic and diastolic strain measures in children: a systematic review and meta-analysis. J. Am. Soc. Echocardiogr. 27https://doi.org/10.1016/j.echo.2014.01.015 (2014). 549 – 60, e3.
Xiang, X., Zhu, X., Zheng, M. & Tang, Y. Comparison of two echocardiography-based methods for evaluating pediatric left ventricular diastolic dysfunction. Front. Pediatr. 11, 1206314. https://doi.org/10.3389/fped.2023.1206314 (2023).
Sun, B. J. et al. Normal reference values for left atrial strain and its determinants from a large Korean multicenter registry. J. Cardiovasc. Imaging. 28, 186–198. https://doi.org/10.4250/jcvi.2020.0043 (2020).
Demircan, T. et al. Evaluation of left ventricular functions by speckle-tracking echocardiography in coarctation patients. Echocardiography. 38, 410–416. https://doi.org/10.1111/echo.14993 (2021).
Pathan, F. et al. Left atrial strain: a multi-modality, multi-vendor comparison study. Eur. Heart J. Cardiovasc. Imaging. 22, 102–110. https://doi.org/10.1093/ehjci/jez303 (2021).
Ferkh, A. et al. Inter-vendor comparison of left atrial strain using layer specific strain analysis. Int. J. Cardiovasc. Imaging. 37, 1279–1288. https://doi.org/10.1007/s10554-020-02114-x (2021).
Wang, Y. et al. Left atrial strain reproducibility using vendor-dependent and vendor-independent software. Cardiovasc. Ultrasound. 17, 9. https://doi.org/10.1186/s12947-019-0158-y (2019).
Badano, L. P. et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur. Heart J. Cardiovasc. Imaging. 19, 591–600. https://doi.org/10.1093/ehjci/jey042 (2018).
Russo, C. et al. Race-ethnic differences in subclinical left ventricular systolic dysfunction by global longitudinal strain: a community-based cohort study. Am. Heart J. 169, 721–726. https://doi.org/10.1016/j.ahj.2015.02.011 (2015).
Parke, K. S. et al. Ethnic differences in cardiac structure and function assessed by MRI in healthy south Asian and white European people: a UK Biobank Study. J. Cardiovasc. Magn. Reson. 26, 100001. https://doi.org/10.1016/j.jocmr.2023.100001 (2024).
El Amrousy, D. et al. Myocardial function using two dimension speckle-tracking echocardiography in children with celiac disease. Eur. J. Pediatr. 183, 947–954. https://doi.org/10.1007/s00431-023-05343-z (2024).
Delgado-Rodríguez, M. Systematic reviews of meta-analyses: applications and limitations. J. Epidemiol. Community Health. 60, 90–92. https://doi.org/10.1136/jech.2005.035253 (2006).
Levy, P. T. et al. Reference ranges of left ventricular strain measures by two-Dimensional Speckle-Tracking Echocardiography in children: a systematic review and Meta-analysis. J. Am. Soc. Echocardiogr. 29, 209–225e6. https://doi.org/10.1016/j.echo.2015.11.016 (2016).
Author information
Authors and Affiliations
Contributions
Authorship: Conception: A.H., A.J.Work design: A.H., T.D., R.M., N.T., R.H., P.S., F.F.Data acquisition: A.H., T.D., R.M., N.T., R.H., P.S., F.F.Analysis: A.J., A.H.Interpretation of data: A.H., T.D., R.M., N.T., R.H., P.S., F.F., A.J.Drafting of the manuscript: A.H., T.D., R.M., N.T., R.H., P.S., F.F.Substantive revision of the manuscript: A.H., T.D., R.M., N.T., R.H., P.S., F.F., A.J.Approved submitted version: A.H., T.D., R.M., N.T., R.H., P.S., F.F.All the authors agree both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated and resolved and the resolution is documented in the literature.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Davarpasand, T., Jalali, A., Mohseni-Badalabadi, R. et al. Normal ranges of left atrial phasic strains and strain rates by 2D speckle-tracking echocardiography in pediatrics: a systematic review and meta-analysis. Sci Rep 14, 25888 (2024). https://doi.org/10.1038/s41598-024-76411-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-76411-z