Abstract
Medical devices (MDs) play a critical role in healthcare delivery while also bringing potential medical risks and unintended harms to patients. Although government regulation is well recognized as a critical and essential function for ensuring the safety of MDs in many countries, the supplementary role that hospitals play is often neglected. This paper constructs a tripartite evolutionary game model involving the government, hospitals, and MDs enterprises to explore their strategic behaviors of MDs regulation in healthcare delivery. We performed theoretical analysis and numerical simulations to examine the stability of stakeholders’ strategy selections. Our results reveal that: (1) Evolutionarily stable strategy (ESS) can be reached under specific revenue conditions for the government, hospitals, and MDs enterprises. (2) Penalty intensities largely affect the convergence rates of hospital strict management and enterprise quality improvement strategies. (3) Whistleblowing is an efficient factor to influence strategy selections of the hospital and MDs enterprise. Based on these findings, we propose policy recommendations to enhance MDs regulation effectiveness, including encouraging hospitals’ engagement in regulation, promoting whistleblowing with more public participation, balancing penalty systems, and strengthening multi-party cooperation.
Similar content being viewed by others
Introduction
Past decades have witnessed rapid development of health technologies, especially in the diagnosis and treatment of diseases which largely depend on the application of medical devices (MDs)1,2. MDs are any instrument, apparatus, machine, appliance, implant, reagent for in vitro use, software, material, or related article used for a specific medical purpose3. They are playing a critical role in saving lives by providing innovative healthcare solutions for clinical practices4. As reported by the BCC Research, the global market of MDs technologies is valued at $639.1 billion in 2021 and is expected to reach about $953.4 billion in 2027. However, while promoting the progress and innovation of health technologies, MDs also posing potential medical risks and unintended harms to patients due to the reason of low product quality, improper use, immature technology, etc5,6,7. According to the report from the ECRI (Emergency Care Research Institute) of the United States, MDs-induced hazards accounted for over half of the "Top 10 Health Technology Hazards for 2023".
Guaranteeing the safety throughout the lifespan of the MDs requires government’s continuous supervision and administration. Government regulation is well recognized as a critical and essential function of ensuring the effective use of MDs and minimizing the health risks and potential medical harms in many countries7,8,9. Over the past decades, MDs regulation has grown increasingly complex, with more regulatory pathways and greater variations in the evidence and controls required for authorization10. At the same time, the expanding market scale and increasing sophistication of MDs have presented mounting challenges to the regulation of numerous governments including China. According to the report of the National Medical Products Administration of China, in 2022, the number of investigated and punished MDs law cases reached approximately 33,594. Among them, 1,481 cases were from manufacturing enterprises, 14,570 from sales enterprises, and 16,277 from users such as health institutions. In 2022, the National Medical Device Adverse Event Monitoring Information System in China received 694,866 reports of MDs adverse events. Of these, 607,551 reports were submitted by users, accounting for 87.43% of the total number of reports. According to the public data of the U.S. Food and Drug Administration, in 2022, a total of 2,063,469 adverse events of MDs were disclosed in the United States. Among them, 97.77% were reported voluntarily by manufacturers, while the reporting proportion of users was 0.21%. According to public data of Australia Therapeutic Goods Administration, in 2022, there were a total of 5,832 MDs-related adverse events. Among these, the number of reports submitted by manufacturers and suppliers was 5,297, accounting for 90.83%. There were 267 reports from users, accounting for 4.58%.
Actually, ensuring the safety of MDs should not be simply considered as the inherent responsibility of the government alone. Hospitals play a dual role in MDs safety as both users and potential regulators. Although not formally empowered with regulatory authority, hospitals can exert significant influence through management measures. For instance, when encountering low-quality products, hospitals can implement measures such as returning purchased goods, terminating supply contracts. The decisions of hospitals may indirectly affect the quality management of suppliers11. This dual role creates a complex dynamic in the MDs safety management system. On one hand, hospitals have strong incentives to ensure device quality for patient safety and risk minimization. On the other hand, implementing strict management incurs substantial costs, including personnel training, management software, and quality control systems12,13,14. These cost burdens may lead hospitals to reduce their management investment and rely excessively on government supervision. Therefore, the key research questions become how policy mechanisms can be designed to: 1) Optimize the balance between government regulation and hospital management; 2) Create effective incentives for hospitals to actively participate in MDs management and monitoring in health services delivery; and 3) Establish efficient coordination mechanisms among stakeholders in MDs regulation.
The rest of this paper is organized as follows. In Section "Literature review", the relevant literatures and practices on evolutionary game theory and MDs regulation are reviewed and summarized. Section “Assumptions and game model” introduces the assumptions and construction process of the tripartite evolutionary game model. Section “Model analysis” analyzes the strategy stability of stakeholders. Section “Numerical simulation and analysis” conducts numerical simulation to validate the model analysis results. Section “Conclusion and policy suggestions” concludes the findings, proposes policy recommendations and discusses limitations and future research directions.
Literature review
Evolutionary game theory
Game theory is a mathematical approach to study decision-making strategies and their interactions among stakeholders. It has become increasingly important in many research fields including economic, regulation policies, etc15. Traditional game theory assumes that players are completely rational and capable of making optimal decisions. However, in the real world, decision-makers have limited information and knowledge. Evolutionary game theory overcomes these limitations by combining game theory analysis with dynamic evolutionary processes. It characterizes decision-makers as having bounded rationality16, assuming they: 1) have limited information; 2) can learn and adapt their strategies; and 3) gradually adjust towards optimal strategies through an evolutionary process. After decades of development, evolutionary game theory has become a useful tool for strategy analysis and has been widely applied in various fields, such as health care17,18, port and shipping systems19, and low-carbon technological innovation20. In the MDs regulation research, we think that evolutionary game theory is particularly suitable for several reasons. Firstly, the complex interactions between government, hospitals, and enterprises in MDs regulation are bounded rationality rather than perfect rationality. Secondly, the theory can effectively model the impact of various factors (including penalties, costs and benefits) on strategy evolution. Thirdly, the approach can analyze interaction of strategies and behavioral adaptations among stakeholders. These characteristics make it an ideal framework for analyzing the MDs regulation strategies in healthcare delivery.
Current practices in MDs post-market regulation
MDs regulation, particularly post-market regulation, has become a key component of the global regulatory practices. Different countries have established diverse approaches to monitor the post-marketing safety and performance of MDs21. The FDA’s post-market surveillance (PMS) system of the United States is built for adverse event reporting and the data is collected via the Manufacturer and User Facility Device Experience (MAUDE) database. And the FDA may require post-marketing studies to address specific safety issues for high-risk MDs22. The European Union has issued the new Medical Device Regulation (MDR) to strengthen its post-market regulation. Under this regulation, MDs manufacturers are required to actively and systematically collect post-market data and submit Periodic Safety Update Reports (PSURs). Besides, the European Union performs specific Post-market Clinical Follow-up (PMCF) activities for MDs with limited clinical data21. Japan has developed Good Vigilance Practice (GVP) and Good Post-marketing Study Practice (GPSP) ordinances to regulate the safety of MDs. A special characteristic of Japan’s regulation system is its comprehensive post-marketing all-case surveillance requirement, which makes manufacturers gather data from all patients utilizing their MDs in Japan22. Meanwhile, China has constructed Adverse Drug Reaction Monitoring System (ADRS) to monitor the safety of post-market MDs. In addition, several national regulations and measures (such as "Regulations on the Supervision and Administration of Medical Devices") have been issued these years to clarify the scope and responsibilities of field supervision agencies across various levels (from manufacturing facilities to healthcare institutions)23.
These different approaches demonstrate the differences in post-market strategies of MDs in different countries and regions. The United States emphasizes adverse event reporting and post-market studies, while the European Union focuses on systematic data collection and regular safety update reporting by manufacturers. In contrast, Japan’s comprehensive all-case surveillance is a thorough but resource-intensive approach; and China uses a hybrid model of adverse event monitoring combined with field inspections21.
Evolutionary game analysis in medical products regulation
Recent years have seen increasing application of evolutionary game theory to medical products regulation. Zhang and Zhu investigated drug safety supervision under government reward-punishment mechanisms, and found that strengthening governmental measures can promote enterprise compliance and reduce third-party testing agencies’ rent-seeking behaviors24. Xu and Zhu examined how government regulation and media coverage influence pharmaceutical companies, revealing that both penalties and public supervision can improve drug quality25. Yang et al. studied pharmaceutical cold chain transportation through a multiparty game model, demonstrating the importance of balanced reward-punishment mechanisms26. Rong and Zhu analyzed collusion between pharmaceutical companies and medical institutions, finding that an increase in patient complaints can effectively suppress such behavior27. Huang et al. examined the quality control of COVID-19 test kit, revealing how illegal incentives and regulatory costs impact government decisions28. Liu et al. studied household MDs recycling strategies, showing stable equilibria emerge under dynamic punishment/subsidy schemes29. Although many researchers considered the stakeholders’ decision making in the production and marketing stage of medical products, limited attention was paid to the regulation of MDs used in health services delivery. Furthermore, while substantial evidence has proved the government’s dominant position in medical products regulation, few studies explore the active role that hospitals can and should play within the regulatory framework.
Compared with previous researches, this study has the following innovations. Firstly, given the shortage of exploration on the regulation strategy selection of MDs used in health services delivery, we consider the interaction effects of main stakeholders in the context of health services delivery and construct a tripartite evolutionary game model involving the government, hospital, and MDs enterprise. Secondly, unlike other studies that commonly regard hospitals as regulated objects, we consider the indirect “regulation effects” of hospital on the MDs enterprises and analyze their decision-making strategies. Thirdly, considering that whistleblowing of illegal behaviors is encouraged by many governments in regulatory practices, we incorporate the monitoring and supplementary role of whistleblowing into the game model. Finally, the parameters of our model are comprehensively verified through multiple real-world sources, such as enterprise financial data, hospital operational records, empirical studies, and government regulatory documents. This enhances the practical relevance of the model.
Assumptions and game model
In China’s healthcare system, the government is both market regulator and healthcare system administrator, which is responsible for policy-making and market regulation. Likewise, the hospital acts as health service providers and front-line medical quality controller. By contrast, the MDs enterprise supplies medical products for patients and the quality of products is under the supervision of government regulation and hospital management. In this paper, the tripartite evolutionary game framework is established mainly based on real-world regulation practice. According to the "Regulations for the Supervision and Administration of Medical Devices" of China, the government regulatory authorities have explicit supervision requirements and penalties for both MDs suppliers and hospitals. Furthermore, in 2021, the Chinese government issued "Measures for the Administration of Clinical Use of Medical Devices", which explicitly specified hospitals’ responsibilities in MDs regulation and management. This regulation framework provides a solid foundation for our model.
The selection of parameters in our model was guided by actual regulation practices and existing management mechanisms to reflect the real-world regulation context of MDs in health services delivery. The parameter values were determined based on real-world data and empirical studies, and were validated through multiple sources including systematic industry consultation, statistical analysis of national monitoring data, and actual administrative enforcement cases, etc. Figure 1 illustrates the tripartite relationship: The government regulates both hospitals and enterprises through penalties. Hospitals influence enterprises through procurement decisions. Enterprises supply MDs while balancing quality and cost. In this complex regulatory network, each party’s decisions directly affect others’ strategies.
Model assumptions
Assumption 1
The three parties, MDs enterprise, hospital, and government, are bounded rational players in this evolutionary game. Their strategy sets are: MDs enterprise: {supply high-quality MDs (probability \(x\)), supply low-quality MDs (probability \(1-x\))}; hospital: {conduct strict management (probability \(y\)), conduct loose management (probability \(1-y\))}; government: {perform active regulation (probability \(z\)), perform passive regulation (probability \(1-z\))}, where \(0\le x,y,z\le 1\).
Assumption 2
For MDs enterprise strategic choices: Basic sales revenue (\(Re0\)) and supplying costs (\(Ce1\) for high-quality, \(Ce2\) for low-quality, \(Ce1>Ce2\)) reflect market conditions. Low-quality products create medical risk (\(Ch2\)) for hospitals. If detected supplying low-quality products, enterprises face: Revenue loss due to the termination of supply relationship (\(Pe1\)) and government fines (\(Pe2\)). According to Article 27 of the "Measures for the Administration of Clinical Use of Medical Devices", when quality issues arise, hospitals can stop using problematic MDs. This action can exert a substantial influence on enterprises’ revenue through the termination of supply relationships, which can be regarded as an effective market-based supervision mechanism that complements government regulation.
Assumption 3
For hospital strategic choices: Strict management incurs costs including personnel, software, and quality control systems (\(Ch1\)). If a hospital conducts loose management and is detected, it will face government penalties (\(Ph1\)), as stated in China’s "Regulations for the Supervision and Administration of Medical Devices", which explicitly states supervision requirements and penalties for healthcare institutions.
Assumption 4
For government strategic choices: Active regulation generates social benefits (\(G\)) but requires regulatory costs (\(Cg1\)). When enterprises supply low-quality products and hospitals conduct loose management, it creates potential patient harm and social impact (\(Cg2\)), as evidenced by international MDs adverse events involving severe injuries, deaths, and substantial economic and credibility losses (e.g., the Impella heart pump recall issued by U.S. FDA in 2024 led to 49 deaths and 129 serious injuries). Government gains social benefits (\(Rg1\)) when enterprises and hospitals perform positively.
Assumption 5
Public whistleblowing: Probability of detecting enterprise supply low-quality MDs (\(a\)) and hospital conduct loose management (\(b\)), where \(0\le a,b\le 1\). Government provides rewards (\(S1,S2\)) for valid reports. Rewards are less than expected penalties: \(aPe2>S1\), \(bPh1>S2\).
The abovementioned parameters and their meanings are shown in Table 1.
Game model
According to the above assumptions, the payoff matrix of the tripartite evolutionary game of MDs regulation is shown in Table 2.
-
(1)
When MDs enterprise supplies high-quality products (\(x\)):
-
1)
If hospital conducts strict management (\(y\)):
MDs enterprise receives: \(Re0-Ce1\) (basic revenue minus costs of supply high-quality products)
Hospital receives: \(-Ch1\) (strict management cost)
Government receives: \(G+Rg1-Cg1\) if perform active regulation (\(z\)), or \(Rg1\) if perform passive regulation (\(1-z\)).
-
2)
If hospital conducts loose management (\(1-y\)):
MDs enterprise receives: \(Re0-Ce1\).
Hospital receives:\(-Ph1\) if government performs active regulation, or \(-bPh1\) if government performs passive regulation.
Government receives: \(G+Ph1-Cg1\) if performs active regulation, or \(bPh1-S2\) if perform passive regulation.
-
1)
-
(2)
When MDs enterprise supplies low-quality products (\(1-x\)):
-
1)
If hospital conducts strict management (\(y\)):
MDs enterprise receives: \(Re0-Ce2-Pe1-Pe2\) under government active regulation, or \(Re0-Ce2-Pe1-aPe2\) under government passive regulation.
Hospital receives: \(-Ch1-Ch2\) (strict management cost plus medical risks).
Government receives: \(G+Pe2\) if perform active regulation, or \(aPe2-S1\) if perform passive regulation.
-
2)
If hospital conducts loose management (\(1-y\)):
MDs enterprise receives: \(Re0-Ce2-Pe2\) under government active regulation, or \(Re0-Ce2-aPe2\) under government passive regulation.
Hospital receives: \(-Ph1-Ch2\) if government performs active regulation, or \(-bPh1-Ch2\) if government performs passive regulation.
Government receives: \(G+Pe2+Ph1+Cg1-Cg2\) under government active regulation, or \(aPe2+bPh1-S1-S2-Cg2\) under government passive regulation.
-
1)
Model analysis
Strategy stability analysis of MDs enterprise
Based on the payoff matrix, the expected returns of MDs enterprise supplying high or low quality MDs are as follows respectively.
And the average expected return of MDs enterprise is
The replication dynamic equation of strategy selection for MDs enterprise can be expressed as
The first order derivative of \(x\) is
According to the stability principle of differential equation, the condition of MDs enterprise selecting stable strategy is \(F(x)=0\) and \(\frac{dF(x) }{dx}<0\).
If \(F(x)=0\), there are three solutions:
-
When \(y=y1\), \(\frac{dF(x)}{dx}=0\), then \(x\) is always in a stable state.
-
When \(y>y1\), \(\frac{dF(0)}{dx}>0\), \(\frac{dF(1)}{dx}<0\), then \(x=1\) is an evolutionarily stable strategy (ESS).
-
When \(y<y1\), \(\frac{dF(0)}{dx}<0\), \(\frac{dF(1)}{dx}>0\), then \(x=0\) is an ESS.
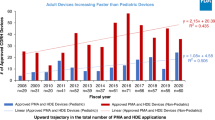
Phase diagram of MDs enterprise strategy evolution is depicted in Fig. 2.
Strategy stability analysis of hospital
Based on the payoff matrix, for the hospital, the expected return of selecting “conduct strict management” is
The expected return of the choosing “conduct loose management” is
Thus, the average expected return of hospital strategy selection is
The replication dynamic equation for hospital strategy selection is
The first order derivative of \(y\) is
According to the differential equation stability principle, the condition of hospital selecting stable strategy is \(F(y)=0\) and \(\frac{dF(y) }{dy}<0\).
If \(F(y)=0\), there are three solutions:
-
When \(z=z1\), \(\frac{dF(y)}{dy}=0\), then \(y\) is always in a stable state.
-
When \(z>z1\), \(\frac{dF(0)}{dy}>0\), \(\frac{dF(1)}{dy}<0\), then \(y=1\) is an ESS.
-
When \(z<z1\), \(\frac{dF(0)}{dy}<0\), \(\frac{dF(1)}{dy}>0\), then \(y=0\) is an ESS.
Phase diagram of hospital strategy evolution is shown in Fig. 3.
Strategy stability analysis of government
From the payoff matrix, the expected returns of government selecting “perform active regulation” and “perform passive regulation” can be marked as \(U31\) and \(U32\)
So, the average expected return of government strategy selection can be expressed as
The replication dynamic equation for government strategy selection is
The first order derivative of \(z\) is
According to the differential equation stability principle, the condition of government selecting stable strategy is \(F(z)=0\) and \(\frac{dF(z) }{dz}<0\).
If \(F(z)=0\), there are three solutions:
-
$$\begin{gathered} z1 = 0, z2 = 1, \hfill \\ x1 = - \left[ {G + S1 + \left( {1 - a} \right)Pe2 + \left( {1 - y} \right) Cg1 + \left( {1 - y} \right)S2 + \left( {1 - b} \right)\left( {1 - y} \right) Ph1} \right] \hfill \\ \quad \quad\;/\left[ {\left( {y - 2} \right)Cg1 - S1 - \left( {1 - a} \right)Pe2} \right] \hfill \\ \end{gathered}$$
-
When \(x=x1\), \(\frac{dF(z)}{dz}=0\), then \(z\) is always in a stable state.
-
When \(x>x1\), \(\frac{dF(0)}{dz}<0\), \(\frac{dF(1)}{dz}>0\), then \(z=0\) is an ESS.
-
When \(x<x1\), \(\frac{dF(0)}{dz}>0\), \(\frac{dF(1)}{dz}<0\), then \(z=1\) is an ESS.
Phase diagram of government strategy evolution is shown in Fig. 4.
Strategy stability analysis of tripartite evolutionary game
The equilibrium points can be calculated if \(F(x)=0\), \(F(y)=0\), and \(F(z)=0\). According to the Eqs. (4), (9) and (14), 8 pure strategy Nash equilibrium points can be obtained: \(E1(\text{0,0},0)\), \(E2(\text{1,0},0)\), \(E3(\text{0,1},0)\), \(E4(\text{0,0},1)\), \(E5(\text{1,1},0)\), \(E6(\text{1,0},1)\), \(E7(\text{0,1},1)\), \(E8(\text{1,1},1)\).
The Jacobian matrix of the tripartite evolutionary game system is
where \(J11\) to \(J33\) can be expressed as as follows:
According to Lyapunov’s first method (indirect method), if all eigenvalues of the Jacobian matrix have negative real parts, the equilibrium point is asymptotically stable. If at least one of the eigenvalues of Jacobian matrix has a positive real part, the equilibrium point is an unstable point30. We calculated the eigenvalue \(\lambda 1\), \(\lambda 2\) and \(\lambda 3\) and analyzed the asymptotic stability condition of each equilibrium point (Table 3). For point \(E1\), eigenvalue \(\lambda 3=Cg1+G+Pe2(1-a)+Ph1(1-b)+S1+S2>0\), so \(E1\) is an unstable point. For point \(E3\), \(\lambda 2=G+Pe2(1-a)+S1>0\), so \(E3\) is an unstable point. Therefore, the remaining \(E2(\text{1,0},0)\), \(E4(\text{0,0},1)\), \(E5(\text{1,1},0)\), \(E6(\text{1,0},1)\), \(E7(\text{0,1},1)\), \(E8(\text{1,1},1)\) may be theoretically possible ESS.
Take equilibrium point \(E5(1,1,0)\) as example, we prove its existence, local uniqueness, and analysis its stability conditions.
-
(1)
Existence of \(E5\) equilibrium point
For \(E5(1,1,0)\), we need to verify that it satisfies \(F(x)=F(y)=F(z)=0\):
-
From \(F(x)=x(1-x)[y(Pe1+Pe2)-Ce1+Ce2]=0\), at \(\text{x}=1\), \(\text{F}(\text{x})=0\) is satisfied.
-
From \(F(y)=y(1-y)[z(Ph1-bPh1)+bPh1-Ch1]=0\), at \(y=1\), \(F(y)=0\) is satisfied.
-
From \(F(z)=z(1-z)[Cg1-G+x(Rg1-aPe2-Ph1)+y(Ph1-bPh1)] =0\), at \(z=0\), \(F(z)=0\) is satisfied.
Therefore, \(E5(1,1,0)\) is indeed an equilibrium point of the model.
-
(2)
Local uniqueness analysis for \(E5\)
At \(E5=(\text{1,1},0)\), the partial derivatives are
Therefore, the Jacobian matrix \(J(E5)\) is
The determinant of \(J(E5)\) is
When \(det(J)\ne 0\), by the implicit function theorem, \(E5\) is locally unique.
-
(3)
Stability analysis for \(E5\)
Using Lyapunov’s first method, we analyze the eigenvalues of \(J(E5)\):
For \(E5\) to be asymptotically stable, we need:
-
1)
\(\lambda 1<0:G-Cg1<0\)
-
2)
\(\lambda 2<0:Ch1-bPh1<0\)
-
3)
\(\lambda 3<0:Ce1-Ce2-Pe1-aPe2<0\)
These give the stability conditions for \(E5\):
-
\(Cg1>G\) (Government condition)
-
\(Ch1<bPh1\) (Hospital condition)
-
\(Ce1-Ce2<Pe1+aPe2\) (MDs enterprise condition)
These conditions can be interpreted in the following realistic ways:
-
1)
For government: When enterprises supplying high-quality products and hospitals implementing strict management, the cost of active regulation (\(Cg1\)) exceeds its social benefits (\(G\)), making passive regulation a more rational choice.
-
2)
For hospitals: The strict management cost (\(Ch1\)) must be less than the expected penalties (\(bPh1\)).
-
3)
For MDs enterprises: The cost difference between supply high and low quality MDs (\(Ce1-Ce2\)) must be less than the penalties and revenue loss (\(Pe1+aPe2\)).
Inference 1
The government’s regulatory strategy is influenced by the cost–benefit relationship of active regulation. When \(Cg1>G\), indicating that regulation costs exceed the social benefits gained from active regulation, the government will tend toward passive regulation. Conversely, when \(Cg1<G\), suggesting that the social benefits outweigh the costs of active regulation, the government will select active regulation strategy.
Inference 2
The equilibrium strategy of hospital depends on the relationship between punishment intensity and strict management costs. Specifically, when \(Ch1>bPh1\), indicating that the expected punishment for loose management is less than the cost of conducting strict management, hospitals will stabilize at the loose management strategy. Conversely, if \(Ch1<bPh1\), meaning that the expected punishment through whistleblowing exceeds the cost of implementing strict management, hospitals will choose strict management strategy.
Inference 3
The enterprise’s equilibrium strategy is determined by the balance between quality-related costs and potential penalties. When \(Ce1-Ce2>Pe1+aPe2\), meaning the expected total punishment (penalties and revenue loss) is insufficient to offset the cost difference between supplying high and low quality products, MDs enterprise will choose to supply low-quality products. However, when \(Ce1-Ce2<Pe1+aPe2\), indicating that the expected punishment through both direct regulation and whistleblowing exceeds the cost savings from supplying low-quality products, enterprise will select the strategy of supplying high-quality products.
Numerical simulation and analysis
Data collection and parameter validation
In order to validate our theoretical analysis and ensure the practicality of the evolutionary game model, we conducted comprehensive real-world data collection and validation on the parameter values. MATLAB 2016b software was employed to perform numerical simulations based on real-world data. Table 4 presents the parameter settings and their validation methods. The values of parameters are from multiple real-world sources including financial records from MDs suppliers, operational data from hospitals, government regulatory documents, and large-scale empirical studies. These parameters are validated through systematic industry consultation, statistical analysis of national monitoring data, and actual administrative enforcement cases.
-
(1)
MDs enterprise parameters: The values of basic revenue (\(Re0\)) and supply costs (\(Ce1,Ce2\)) were from financial data of Enterprise M, a MDs supplier to Hospital S. The parameters were validated through systematic consultation with other enterprises and were referenced to industry standards. For instance, the value difference between basic revenue and cost of supplying high-quality products (\(Re0-Ce1=30\)) represents 30% of basic revenue rate of a MDs supplier. This is supported by real-world examples: Mindray Medical reported a profit margin of about 33% in 2023. In contrast, in a case of counterfeit intervertebral foramen endoscope, the profit margin of supplier reached about 67.5%.
-
(2)
Hospital parameters: Strict management costs (\(Ch1\)), medical risks (\(Ch2\)) and (\(Pe1\)) were based on actual operational data from hospital S. \(Ch1\) encompasses personnel costs, equipment procurement, and third-party testing fees, and was validated through systematic consultation with other hospitals of the comparable size. \(Ch2\) was validated through empirical research results and \(Pe1\) was validated through consultation with other hospitals of comparable size.
-
(3)
Government parameters: The values of regulatory parameters (\(G,Cg1, Cg2, Rg1\)) were obtained from literature review and actual regulatory documents. For example, the social benefit parameter \(G\) has been referenced to a study regarding vaccine quality supervision. Their validation was through real government regulation investment cases and documented enforcement cases. Penalty parameters (\(Pe2, Ph1\)) were set according to national regulation documents and validated through real administrative cases.
-
(4)
Whistleblowing parameters: The whistleblowing-related parameters were set based on national statistics and national market supervision measures. For example, the reward parameters (\(S1, S2\)) were determined as 3% of unqualified and confiscated amounts according to national market supervision measures. The detection probabilities (\(a, b\)) were set at 0.05 based on statistical data from China’s supervision system during 2021–2023 (whistleblowing cases accounted for about 5%).
Since we primarily investigate the role of hospitals in MDs regulation, equilibrium point \(E5(\text{1,1},0)\) is selected to conduct numerical simulation. Based on real-world data collection, the values of parameters are as set follows:
Parameter sensitivity analysis
Impact of initial strategies on evolution
Firstly, we investigate how random initial strategies affect model evolution. Figure 5 demonstrates that after 50 iterations, under random initial values \((x,y,z)\), the system consistently converges to equilibrium point \(E5(\text{1,1},0)\).
Secondly, we explore how different initial values influence the evolutionary paths.
-
(1)
Impact of initial enterprise strategy (\(x\))
In order to examine the convergence trend of \(y\) and \(z\) with different initial \(x\) values, we set \(y=z=0.05\), and change the value of \(x\) from 0.2 to 0.8. Figure 6a shows that higher initial \(x\) values accelerate \(y\)’s convergence to 1. This suggests that hospitals are more likely to implement strict management when enterprises show stronger initial tendency of providing high-quality products. As shown in Fig. 6b, when \(z<0.6\), initial \(x\) values have negligible impact; When \(z\ge 0.6\), higher initial \(x\) values accelerate \(z\)’s convergence to 0. This indicates that stronger MDs enterprise quality commitment promotes government’s transition to passive regulation.
-
(2)
Impact of initial hospital strategy (\(y\))
For the purpose of examining the convergence trend of \(x\) and \(z\) with different initial \(\text{y}\) values, we set \(x=z=0.05\), and change the value of \(y\) from 0.2 to 0.8. Figure 6c demonstrates that higher initial \(y\) values accelerate \(x\)’s convergence to 1. This indicates that higher initial possibilities of hospital strict management promote MDs enterprise supply high-quality products. Figure 6d shows that when \(\text{z}<0.6\), \(z\)’s evolution is insensitive to \(\text{y}\), while when \(\text{z}\ge 0.6\), higher initial \(\text{y}\) values accelerate \(z\)’s convergence to stable state. This suggests that hospital active management facilitates government’s strategic adjustment.
-
(3)
Impact of initial government strategy (\(z\))
When setting \(x=y=0.05\) and changing \(z\) from 0.2 to 0.8, Fig. 6e and f demonstrate positive correlations between initial \(z\) values and the evolution of \(x\) and \(y\). This indicates that higher initial government active regulation probability promotes positive strategies from both enterprises (supply high-quality products) and hospitals (conduct strict management).
Impact of \({\varvec{a}}\) and \({\varvec{b}}\) on evolution
-
(1)
Impact of \(a\) on evolution
With the aim of investigating the impact of the probability of detecting low-quality products via whistleblowing (\(a\)) on model’s evolution, we set \(a\) = 0.05, 0.15, 0.25 and 0.35, and while letting other variables remain constant at initial values. The simulation results show that the increase in \(a\) value decelerate the evolution of government strategy (\(z\)) to the stable point 0. This indicates that higher probability of detecting enterprises’ low-quality products through whistleblowing delays government’s turning to passive regulation (Fig. 7).
-
(2)
Impact of \(b\) on evolution
Similarly, we set \(b\) = 0.05, 0.15, 0.25 and 0.35, and let other parameters remain at initial values. The results demonstrate that the increase in \(b\) value decreases the evolution speed of \(z\) to 0. This suggests that higher probability of detecting hospital’s loose management through whistleblowing slows down government’s strategy of transition to passive regulation (Fig. 8).
Impact of \({P}{e}1\), \({P}{e}2\) and \({P}{h}1\) on evolution
-
(1)
Impact of \(Pe1\) on evolution
In order to analyze \(Pe1\)’s effect on evolution, we set \(Pe1\) = 20, 40, 60 and 80. Figure 9 shows that when \(Pe1\) increases from 20 to 80, the evolution speed of both enterprise’s strategy (\(x\)) and hospital’s strategy (\(y\)) turning to 1 rises. This indicates that a greater amount of revenue loss for MDs enterprises promotes both high-quality product supply and strict hospital management.
-
(2)
Impact of \(Pe2\) on evolution
When examining the effect of \(Pe2\) on evolution, we set the values as 200, 400, 600 and 800. As depicted in Fig. 10, larger \(Pe2\) values accelerate the evolution of enterprise strategy (\(x\)) to 1. In addition, with the increases of \(Pe2\), the government strategy (\(z\)) first increases and then converges to 0 more quickly. This suggests that stronger government penalties effectively promote enterprise quality improvement and also allow government itself transition to passive regulation faster.
-
(3)
Impact of \(Ph1\) on evolution
The effects of \(Ph1\) on evolution are analyzed using \(Ph1\) = 200, 400, 600 and 800. Figure 11 shows that higher \(Ph1\) values speed up hospital strategy evolution to 1. The government strategy (\(z\)) exhibits an initial rise followed by convergence to 0, and this process is accelerated as \(Ph1\) increases. This indicates that stronger government punishment promotes both strict hospital management and eventual government itself passive regulation.
Impact of \({{C}}{{h}}1\), \({{C}}{{e}}1\), \({{C}}{{g}}1\) and \({{G}}\) on evolution
-
(1)
Impact of \(Ch1\) on evolution
In order to analyze the impact of \(Ch1\) on evolution, we set \(Ch1\) values as 5, 10, 15 and 20. Figure 12 reveals that higher \(Ch1\) values slow down hospital strategy evolution to 1. This suggests that increased management costs delay hospitals’ adoption of strict management strategy.
-
(2)
Impact of \(Ce1\) on evolution
We set \(\text{Ce}1\) = 50, 60, 70 and 80 to examine the influence of \(\text{Ce}1\) on evolution. As shown in Fig. 13, when the values of \(\text{Ce}1\) increase, the evolution speed of the enterprise strategy towards 1 slows down. This implies that higher quality costs delay the quality improvement of enterprises, though they do not prevent it from happening.
-
(3)
Impact of \(Cg1\) on evolution
We examine \(Cg1\)’s effect on evolution by setting values 15, 20, 25 and 30. Figure 14 demonstrates that higher \(Cg1\) values accelerate government strategy evolving to 0, which suggests that increased regulatory costs promote the government’s strategy towards passive regulation.
-
(4)
Impact of \(G\) on evolution
For analyzing the influence of \(G\) on evolution, we determine its value as \(G\) = 5, 10, 15 and 20. Figure 15 shows that larger \(G\) values slow down government strategy evolution to 0, which indicates that higher social benefits delay government’s strategy towards passive regulation.
Conclusion and policy suggestions
Conclusions
Given the rapid growth of the MDs market and increasing complexity of healthcare technologies, regulatory authorities worldwide face mounting challenges in ensuring MDs safety and effectiveness. Considering that no study researched the regulation behavior strategy of MDs used in health services delivery by far, under the assumption of stakeholders’ bounded rationality behaviors, we established a tripartite evolutionary game model involving the government, hospital, and MDs enterprise. Our tripartite evolutionary game model provides novel insights into the complex dynamics of MDs regulation in health services delivery. The model results demonstrate how different stakeholders’ strategies evolve and interact, which has both theoretical significance and practical value.
Based on our analysis, several key conclusions can be drawn. At first, ESS can be reached under specific revenue conditions for stakeholders. Taking equilibrium point \(E5\) as an example, when \(Cg1>G, Ch1<bPh1, Ce1-Ce2<Pe1+aPe2\), the system reaches a stable state where government performs passive regulation, hospital conducts strict management, and enterprise supplies high-quality products. This finding is in line with an actual case in China. Specifically, according to the publicly available data from China’s MDs adverse event monitoring reports, in 2019, user institutions’ report submissions accounted for 90.27% of the total reports. However, this proportion dropped to 85.03% in 2020. After the implementation of "Measures for the Clinical Use Management of Medical Devices" in 2021, which clearly specified the supervision and management responsibilities of medical institutions in health services delivery, the proportion gradually rose to 87.55% in 2021, 88.37% in 2022, and 90.52% in 2023 respectively.
Secondly, initial strategy probabilities significantly influence the evolution paths and convergence rate of the model. Our simulation results show that when MDs enterprise and hospital are more likely to choose positive strategies (i.e., enterprise supply high-quality products and hospital conducts strict management), the government more quickly evolves toward passive regulation. This reflects that when both MDs enterprise and hospital demonstrate strong quality commitment, reduced MDs quality risks allow the government to gradually adopt a more passive regulatory strategy.
Thirdly, penalty intensities significantly affect the convergence rates of hospital management and enterprise quality improvement strategies. Our results show that increased penalties from both government (\(Pe2, Ph1\)) and hospital (\(Pe1\)) accelerate the evolution toward stable strategies. When government increases penalties on enterprises, they more quickly adopt supplying high-quality products strategy. Similarly, when enterprise revenue losses increase, the hospital implements strict management practices more rapidly. This implies that appropriate penalties can effectively guide the behavior of stakeholders. This finding is consistent with the results of other researches, thus confirming the role of penalties imposed by the government29,35 and the hospital36 in the regulation of medical products.
Fourthly, whistleblowing plays an important supplementary role in monitoring the safety of MDs. The simulation results indicate that higher whistleblowing detection probabilities (\(a, b\)) encourage the government to adopt passive regulation. This suggests that effective whistleblowing systems can partially substitute for direct government supervision, thereby reducing regulatory costs while maintaining MDs quality. This finding also implies that investing in whistleblowing mechanisms (such as increasing the whistleblowing channels, raising the amount of rewards) could be a cost-effective approach to enhance regulatory efficiency. This aligns with the current trend where many countries are strengthening their whistleblowing systems in MDs regulation37,38.
Policy suggestions
According to the research findings, several policy suggestions are proposed for future MDs regulation research and practice.
-
(1)
The government should attach importance to the key role of hospital in the supervision of MDs used in health services delivery. As reported by the National Health Commission of China government, there are about 37,000 hospitals in China. Given such a large number of hospitals and the vast usage of MDs, it is challenging to achieve effective regulation of MDs in health services delivery solely through the government’s efforts. Therefore, while promoting the implementation of relevant official management measures, the government also needs to establish a reward mechanism for hospitals that perform well in MDs management, thereby further motivating hospitals to actively engage in the regulation process.
-
(2)
The government should raise the public’s awareness of policies and regulations related to MDs safety. In fact, in many countries, including China, the public’s awareness rate of MDs-related regulations is relatively low. According to the report by National Medical Products Administration of China, the investigated and punished MDs law cases through whistleblowing only accounted for about 5.7% in 2022. There is enormous potential for regulating MDs by leveraging the power of the public. The government should enhance policy publicity and increase the intensity of rewards to stimulate the public’s enthusiasm in participating in MDs regulations.
-
(3)
The government should set a reasonable level of penalties. For MDs enterprises, light punishment fails to achieve the expected deterrent effect, while harsh penalties will impose excessive pressure on MDs enterprises, thereby affecting the supply of MDs and the development of MDs industry. In addition, harsh penalties may also easily lead to the situation of "punishment replacing management", that is to say, government regulators prefer to punish rather than manage. In the future, the government should focus on preventing illegal activities through effective supervision and management.
-
(4)
Our findings also highlight the importance of enhancing cooperation between hospitals and MDs enterprises. This can be achieved by establishing regular communication channels for feedback and quality improvement, implementing joint training programs for MDs safety and correct usage, and creating shared platforms for reporting and monitoring MDs performance.
Limitations and future research directions
Limitations
Our study has several limitations. Firstly, while our evolutionary game model investigates the main factors influencing MDs regulation in healthcare delivery, the model does not fully consider other factors such as market competition intensity, rapid technological advancements, and evolving industry standards, which may influence the strategy evolution to some extent. Secondly, our analysis concentrates on three primary stakeholders. However, in practice, there are also other participants that may play an important role in MDs regulation including patients, medical insurance institutions, quality inspection organizations, etc. Comprehensive models involving these participants would provide more reliable research findings. Lastly, our model only considers the regulation of MDs in healthcare delivery. However, the regulation of MDs during the registration, production, and marketing processes can have an impact on the quality of MDs used in hospitals and the decisions of stakeholders. For example, strict registration requirements can ensure the safety and effectiveness of MDs, while poor production management may lead to quality flaws. These are crucial for the extrapolation of our study results.
Future research directions
We propose several promising directions for future research. Firstly, future models should incorporate potential influencing factors including market competition mechanisms and technological evolution. This can better reflect how market competition and technological innovations impact stakeholders’ behavioral strategies and regulatory outcomes. Secondly, future studies should construct more comprehensive game models that integrate patients, medical insurance institutions, and quality inspection organizations into the consideration, which can more effectively investigate the strategy behaviors that are more in line with the actual environment of MDs regulation. Thirdly, empirical validation of theoretical results across healthcare systems of different countries and regions should be highly valued. This could provide comparative evidence for analyzing stakeholder’s behavior strategies on regulatory outcomes.
Data availability
The data that support the findings of this study are available from the authors on reasonable request.
References
Rodriguez, N. M., Burleson, G., Linnes, J. C. & Sienko, K. H. Thinking beyond the device: An overview of human- and equity-centered approaches for health technology design. Annu. Rev. Biomed. Eng. 25, 257–280. https://doi.org/10.1146/annurev-bioeng-081922-024834 (2023).
Smith, V. et al. Defining the clinician’s role in early health technology assessment during medical device innovation - a systematic review. BMC Health Serv. Res. 19(1), 1–14. https://doi.org/10.1186/s12913-019-4305-9 (2019).
Hubner, S. et al. The evolving landscape of medical device regulation in east, central, and Southern Africa. Glob. Health Sci. Pract. 9(1), 136–148. https://doi.org/10.9745/GHSP-D-20-00578 (2021).
Bianchini, E. & Mayer, C. C. Medical device regulation: Should we care about it?. Artery Res. 28(2), 55–60. https://doi.org/10.1007/s44200-022-00014-0 (2022).
Mooghali, M., Ross, J. S., Kadakia, K. T. & Dhruva, S. S. Characterization of US Food and Drug Administration Class I recalls from 2018 to 2022 for moderate- and high-risk medical devices: A cross-sectional study. Med. Dev. Evid. Res. https://doi.org/10.2147/MDER.S412802 (2023).
Wunnava, S., Miller, T. A. & Bourgeois, F. T. Improving FDA postmarket adverse event reporting for medical devices. BMJ Evid. Based Med. 28(2), 83–84. https://doi.org/10.1136/bmjebm-2021-111870 (2023).
Bretthauer, M., Gerke, S., Hassan, C., Ahmad, O. F. & Mori, Y. The new European medical device regulation: Balancing innovation and patient safety. Ann. Intern. Med. 176(6), 844–848. https://doi.org/10.7326/M23-0454 (2023).
Nasir, N., Molyneux, S., Were, F., Aderoba, A. & Fuller, S. S. Medical device regulation and oversight in African countries: A scoping review of literature and development of a conceptual framework. BMJ Glob. Health 8(8), e012308. https://doi.org/10.1136/bmjgh-2023-012308 (2023).
Brownscombe, J. J. Australian medical device regulation during COVID-19: Has the Australian regulatory framework for medical devices been effective during the COVID-19 pandemic?. J. Law Med. 28(3), 745–759 (2021).
Darrow, J. J., Avorn, J. & Kesselheim, A. S. FDA regulation and approval of medical devices: 1976–2020. JAMA 326(5), 420–432. https://doi.org/10.1001/jama.2021.11171 (2021).
Baulac, S. In the business of medicine: Why hospitals should be subject to the theory of strict liability as any other seller. Ave Maria L. Rev. 20, 192 (2022).
Grennan, M., Kim, G. H., McConnell, K. J. & Swanson, A. Hospital management practices and medical device costs. Health Serv. Res. 57(2), 227–236. https://doi.org/10.1111/1475-6773.13898 (2022).
Li, J., Mao, Y. & Zhang, J. Construction of medical equipment maintenance network management platform based on big data. Front. Phys. 11, 28. https://doi.org/10.3389/fphy.2023.1105906 (2023).
Arab-Zozani, M., Imani, A., Doshmangir, L., Dalal, K. & Bahreini, R. Assessment of medical equipment maintenance management: Proposed checklist using Iranian experience. Biomed. Eng. Online 20(1), 49. https://doi.org/10.1186/s12938-021-00885-5 (2021).
Marden, J. R. & Shamma, J. S. Game theory and control. Annu. Rev. Control Robot. Auton. Syst. 1(1), 105–134. https://doi.org/10.1146/annurev-control-060117-105102 (2018).
Yuan, Y., Du, L., Luo, L. & Cui, L. Allocation strategy of medical supplies during a public health emergency: A tripartite evolutionary game perspective. Sci. Rep. 13(1), 9571. https://doi.org/10.1038/s41598-023-36000-y (2023).
Tao, C. et al. How to promote the hierarchical diagnosis and treatment system: A tripartite evolutionary game theory perspective. Front. Psychol. 13, 1081562. https://doi.org/10.3389/fpsyg.2022.1081562 (2023).
Zhang, Z., Song, X. & Shi, Y. Evolutionary game analysis of behavior strategies of multiple stakeholders in an elderly care service system. Int. J. Environ. Res. Public Health 20(5), 4263. https://doi.org/10.3389/fpsyg.2022.1081562 (2023).
Xu, L. et al. Evolutionary game analysis on behavior strategies of multiple stakeholders in maritime shore power system. Ocean Coast. Manag. 202, 105508. https://doi.org/10.1016/j.ocecoaman.2020.105508 (2021).
Shi, T., Han, F., Lan, C., Shi, J. & Xiao, H. Study on value Co-creation and evolution game of low-carbon technological innovation ecosystem. J. Clean. Prod. https://doi.org/10.1016/j.jclepro.2023.137720 (2023).
Badnjević, A. et al. Post-market surveillance of medical devices: A review. Technol. Health Care 30, 1315–1329. https://doi.org/10.3233/THC-220284 (2022).
Gomes, K. L. G. et al. Post-marketing authorisation safety and efficacy surveillance of advanced therapy medicinal products in Brazil, the European Union, the United States and Japan. Cytotherapy 25, 1113–1123. https://doi.org/10.1016/j.jcyt.2023.06.005 (2023).
Chen, Y. J. et al. A comparative study of medical device regulations: US, Europe, Canada, and Taiwan. Ther. Innov. Regul. Sci. 24, 1–8. https://doi.org/10.1177/2168479017716712 (2020).
Zhang, S. & Zhu, L. Coregulation supervision strategy of drug enterprises under the government reward and punishment mechanism. Complexity 2021, 1–16. https://doi.org/10.1155/2021/5865299 (2021).
Xu, Y. & Zhu, L. Pharmaceutical enterprises drug quality strategy Moran analysis considering government supervision and new media participation. Front. Public Health 10, 1079232. https://doi.org/10.3389/fpubh.2022.1079232 (2023).
Yang, Z., Zhao, K. & Guo, Q. Mathematical problems in engineering pharmaceutical cold chain transportation decision making under the government’s reward-penalty mechanism: A perspective of evolutionary game theory. Math. Probl. Eng. https://doi.org/10.1155/2022/1555042 (2022).
Rong, J. & Zhu, L. Cleaner production quality regulation strategy of pharmaceutical with collusive behavior and patient feedback. Complexity 125, 1–15. https://doi.org/10.1155/2020/1920523 (2020).
Huang, Z., Wang, X., Feng, Z. & Chen, B. Regulating the product quality of COVID-19 antigen testing reagents: A tripartite evolutionary game analysis under China’s legal framework. Front. Public Health 10, 1060079. https://doi.org/10.3389/fpubh.2022.1060079 (2023).
Liu, Z., Lang, L., Li, L., Zhao, Y. & Shi, L. Evolutionary game analysis on the recycling strategy of household medical device enterprises under government dynamic rewards and punishments. Math. Biosci. Eng. 18(5), 6434–6451. https://doi.org/10.3934/mbe.2021320 (2021).
Zhang, L. et al. Governance mechanisms for chronic disease diagnosis and treatment systems in the post-pandemic era. Front. Public Health 10, 1023022. https://doi.org/10.3389/fpubh.2022.1023022 (2022).
Shen, Y. et al. Analysis of the characteristics and risk factors affecting the judgment results of medical damage liability disputes in 3172 second-instance and retrial cases in China. Hum. Resour. Health 21(1), 53. https://doi.org/10.1186/s12960-023-00832-6 (2023).
Zhang, T. Analysis of influencing factors of compensation amount for liability for medical malpractice and construction of multiple linear regression model: An empirical analysis based on 5928 cases. Hainan Medical University (2023) (in Chinese).
Seabury, S. A., Helland, E. & Jena, A. B. Medical malpractice reform: Noneconomic damages caps reduced payments 15 percent, with varied effects by specialty. Health Aff. 33(11), 2048–2056. https://doi.org/10.1377/hlthaff.2014.0492 (2014).
Xie, R. et al. Four-party evolutionary game analysis of supervision for vaccine quality in major epidemics. J. Intell. Fuzzy Syst. 42(6), 5695–5714. https://doi.org/10.3233/JIFS-212146 (2022).
Fan, D. et al. Safety regulation enforcement and production safety: The role of penalties and voluntary safety management systems. Int. J. Prod. Econ. 248, 108481. https://doi.org/10.1016/j.ijpe.2022.108481 (2022).
Malmir, B., Dehghani, S., Jahantigh, F. F. et al. A new model for supply chain quality management of hospital medical equipment through game theory. In Proceedings of the 6th International Conference on Information Systems, Logistics and Supply Chain, ILS 1–9 (2016).
Hashimoto, T., Ozaki, A. & Tanimoto, T. Whistleblowing and misconduct at large pharmaceutical firms. JAMA 325(13), 1331. https://doi.org/10.1001/jama.2021.0573 (2021).
Motarjemi, Y. Whistleblowing: An essential element of public health and food safety management. In Food Safety Management 1089–1107 (Academic Press, 2023).
Acknowledgements
This paper was supported by Fundamental Research Funds for the Central Universities of China (Grant Number WK9110000014).
Author information
Authors and Affiliations
Contributions
G.T. and Q.G. contributed equally in designing and drafting the manuscript and they are co-first authors, C.H. contributed in manuscript revision and refinement.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tong, G., Geng, Q. & Hu, C. Evolutionary game analysis on the regulation of medical devices used in health services delivery. Sci Rep 14, 31429 (2024). https://doi.org/10.1038/s41598-024-83068-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-83068-1