Abstract
This study investigated whether intravenous administration of tumor cells killed by photodynamic therapy (PDT) with 5-aminolevulinic acid (5-ALA) had antitumor effects on distal tumors. Furthermore, a novel extracorporeal blood circulating 5-ALA/PDT system was developed. 5-ALA/PDT- (low or high irradiation) or anticancer drug–treated cells were intravenously administered to rats in a glioma cancer model. CD8+ T cell infiltration into the tumor and expression of calreticulin were examined. The cell-killing effect in the circulating PDT system and protoporphyrin IX (PpIX) accumulation were evaluated. An antitumor effect was observed only with preadministration of low-irradiated 5-ALA/PDT-treated cells and was characterized by the infiltration of CD8+ T cells into the tumor. In low-irradiated cells, several types of cell death were observed, and cell surface calreticulin expression increased over time. A method for the intravenous administration of 5-ALA/PDT-treated cells along with extracorporeal blood circulation was then developed to target hematologic malignancies. Gradually cell death in the circulating PDT system and tumor-specific PpIX accumulation was confirmed using hematopoietic tumor cells. Thus, the extracorporeal blood circulating 5-ALA/PDT system has a direct cell-killing effect and an antitumor effect via induced immune activity and illustrates a new therapeutic strategy for hematologic malignancies.
Similar content being viewed by others
Introduction
Photodynamic therapy (PDT) is a promising cancer therapy for selective killing of cancer cells while minimizing damage to normal cell1. In particular, aminolevulinic acid (5-ALA), a precursor of a PDT photosensitizer, is preferred over other treatments for certain cancers because of the high specificity and low side effects1,2. 5-ALA is metabolized into several metabolites that ultimately and specifically accumulate in tumors as protoporphyrin IX (PpIX)1. PpIX then generates cytotoxic reactive oxygen species upon exposure to light in the presence of oxygen, causing the selective killing of cancer cells3. 5-ALA/PDT has already been approved by the U.S. Food and Drug Administration and is used in the United States to treat actinic keratosis, a skin condition that can become cancerous4.
This phototoxic reaction of PpIX causes the destruction of the tumor and tumor vasculature. In addition to its direct cell-killing effects, PDT has been shown to stimulate antitumor immune responses, resulting in shrinkage of untreated tumors5,6,7. These responses are considered to be mediated by the release of tumor-associated antigens (TAA), tumor-specific antigens (TSA), and damage-associated molecular patterns (DAMPs) from cells killed by PDT, which then activate dendritic cells (DCs) and subsequently T cells8,9. This induces immunogenic cell death of residual and metastatic tumor cells. However, most of these studies have investigated responses after the treatment of solid tumors with PDT10; therefore, the clinical applicability of the antitumor immunostimulatory effects of PDT has not yet been established.
Despite the potential of PDT to stimulate an antitumor immune response, the clinical application of PDT-induced immunotherapy remains limited because of several challenges. First, the effectiveness of this strategy depends on the effective preservation and presentation of the cancer immunogenicity to immune cells. This requires a method of administering PDT-treated cells to patients while retaining the immunogenicity of TSA, which differs between individual patients, has not yet been resolved. Moreover, in most cases, antitumor immune activation by PDT-treated cells requires additional immune stimulation by using immune adjuvants, immune cells, or a combination of immune checkpoint inhibitors11,12, and PDT-treated cells alone cannot sufficiently activate an immune response. Furthermore, how the conditions of PDT-treated cells, i.e., whether they experience programed cell death or are necrotic, affects immune responses remains poorly understood. Finally, a method for efficiently and safely administering PDT-treated cells to patients has not yet been identified.
In this study, we verified for the first time whether intravenous administration of 5-ALA/PDT-treated dead cells in a rat tumor model can have an antitumor immune effect. Subsequently, we developed a device combining extracorporeal blood circulation and 5-ALA/PDT for treating hematologic cancers as a novel approach. This extracorporeal blood circulating PDT system with 5-ALA may provide a new therapeutic strategy for hematologic cancers.
Results
Antitumor immunostimulatory effect of intravenous administration of 5-ALA/PDT-treated cells
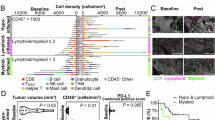
Rats in the C6 rat glioma model were intravenously administered with phosphate-buffered saline (PBS) (control group) or 5-ALA/PDT-treated C6 glioma cells three times prior to the graft. Consequently, tumors grew in the control group, whereas the tumor volume was significantly reduced in rats that received intravenous administration of 5-ALA/PDT-treated cells with low irradiation (7.5 J/cm2) (Fig. 1a,b,d). Conversely, intravenous administration of 5-ALA/PDT-treated cells with high irradiation (317 J/cm2) did not cause tumor reduction (Fig. 1c,d). Immunostaining of tumors for CD8+ T cell only showed a significant increase in intratumoral CD8+ T cells with low irradiation (Fig. 1e,f), and the number of intratumoral CD8+ T cells did not change with high irradiation (Fig. 1f). The production of interferon γ (IFN-γ) from splenic T cells in rats euthanized on day 10 tended to only increase in the low irradiation group, but not significantly (Fig. 1g). Thus, intravenous administration of 5-ALA/PDT-treated cells induced immunostimulatory and antitumor effects in vivo with low irradiation but not with high irradiation.
Antitumor immunostimulatory effect of intravenous administration of 5-ALA/PDT-treated cells. (a–c) Tumor volume changes in individual rats after allogenic C6 cell transplantation. Prior to transplantation, intravenous administration of (a) PBS (control), (b) 1 mmol/L 5-ALA/PDT-treated C6 cells with low irradiation (7.5 J/cm2), or (c) 1 mmol/L 5-ALA/PDT-treated C6 cells with high irradiation (317 J/cm2), was performed three times (day -21, -14, and -1). **p < 0.01 compared with the control group. (d) Photos of the tumors of three rats from each group taken on day 10. (e) Immunostaining of CD8+ cells in the tumors in each group. (f) The average number of CD8+ cells per field (400 ×). (g) IFN-γ level (pg/mL) in supernatants of splenocytes stimulated with C6 cells for 24 h on day 10 was detected by ELISA. Values are presented as mean (SD) **p < 0.01 compared with the control group.
5-ALA/PDT-induced cell death and calreticulin expression
5-ALA/PDT-treated cells with low or high irradiation were stained with Annexin V and propidium iodide (PI), and flow cytometric analysis was performed. As shown in Fig. 2a,c, the cells treated with low irradiation were a mixture of live cells (Annexin V- /PI-), apoptotic cells (Annexin V+/PI-), and dead cells (Annexin V+/PI+) immediately after irradiation (0 h). At 4–24 h later, these live cells and apoptotic cells disappeared, and dead cells became predominant. Conversely, most cells treated with high irradiation were found to be dead immediately after irradiation (Fig. 2b,c); therefore, these were considered necrotic cells. Flow cytometric analysis of cell surface calreticulin expression in these irradiated cells showed that the expression gradually increased in a time-dependent manner (Fig. 2d,e). In addition, the expression of calreticulin on 5-ALA/PDT-treated cells was higher immediately after irradiation (0 h) with high irradiation. However, over time (4–24 h), cells treated with low irradiation showed higher levels of calreticulin expression than those treated with high irradiation (Fig. 2e).
5-ALA/PDT-induced cell death and calreticulin expression. (A and B) Flow cytometric analysis of 5-ALA/PDT-treated cells stained with Annexin V and propidium iodide (PI) at low (a) and high irradiation (b). (c) Summary of cell death immediately (0 h) and 4 and 24 h after low or high irradiation. (d) Flow cytometric analysis of cell surface calreticulin at 0, 4, and 24 h after low or high irradiation. (e) Average of mean fluorescence intensity (MFI) of calreticulin. Values are presented as mean (SD) **p < 0.01, low irradiation versus high irradiation. N.T.: Not statistical tested because of n = 2.
Intravenous administration of anticancer drug–treated cells and calreticulin expression
We next examined whether intravenous administration of cells treated with anticancer drugs would also have antitumor effects. Rats were administrated with PBS (control group), 5-ALA/PDT with low irradiation, mitoxantrone hydrochloride (MTX)-, doxorubicin hydrochloride (DOX)-, or epirubicin hydrochloride (EPI)-treated C6 glioma cells intravenously three times prior to each graft. To eliminate the direct effects of anticancer drugs, only supernatant-free cells were administered in each group. Consequently, the pretreatment of injected cells with the three anticancer drugs failed to reduce tumor volume (Fig. 3a). Annexin V/PI staining of cells was performed to confirm the condition of the anticancer drug–treated cells for analysis via by flow cytometry (Fig. 3b). Cells treated with the three anticancer drugs were predominantly Annexin V+/PI- indicating apoptotic cells. Furthermore, unlike 5-ALA/PDT-treated cells, these anticancer drug–treated cells contained few dead cells (Annexin V+/PI+) (Fig. 3c). In addition, flow cytometric analysis of the expression of cell surface calreticulin was performed (Fig. 3d). In all three anticancer drug–treated cells, cell surface calreticulin expression was as high as that in 5-ALA/PDT-treated cells with low irradiation (Fig. 3e). This indicates that inducing antitumor effects through the intravenous administration of cells requires not only the expression of DAMPs, such as calreticulin, but also the presence of necrotic cells and other types of cell death within gradually dying cells.
Antitumor immunostimulatory effect of 5-ALA/PDT-treated cells or anticancer drug–treated cells. (a) Changes in tumor volume after allogenic C6 cell transplantation in rats with prior intravenous administration of PBS (control), 5-ALA/PDT with low irradiation–, mitoxantrone (MTX)-, doxorubicin (DOX)-, or epirubicin (EPI)-treated C6 cells (n = 3 per group). **p < 0.01 compared with the control group. (b) Flow cytometric analysis of low-irradiated 5-ALA/PDT–, MTX-, DOX-, or EPI-treated cells stained with Annexin V and PI. (c) Summary of cell death after each treatment. (d) Flow cytometric analysis of cell surface calreticulin of low-irradiated 5-ALA/PDT–, MTX-, DOX-, or EPI-treated cells. (e) Average MFI of calreticulin after each treatment. Values are presented as mean (SD) **p < 0.01, comparison with immediately (0 h) after low irradiation 5-ALA/PDT.
A novel extracorporeal blood circulating photodynamic therapy system
As mixture of necrotic cells and gradually dying cells is required to exert antitumor immunostimulatory effects, a method was required to deliver this mixture of cells intravenously; therefore, we devised and developed the extracorporeal blood circulation PDT system shown in Fig. 4a,b for clinical use. In this novel system, hematological malignancies would be the primary target disease because leukemic cells in the blood can be targeted by 5-ALA/PDT, and the device was designed to kill leukemic cells in the bloodstream by extracorporeal circulation and light irradiation. Hence, because the intensity of light at 630 nm reaching the blood is limited due to the presence of erythrocytes, we investigated the optimal cross-sectional shape of the blood circuit to achieve the cell-killing effect (Fig. 4c).
A novel extracorporeal blood circulating PDT system for treating hematopoietic malignancies. (a,b) 5-ALA was administered orally, and the blood was then circulated extracorporeally through medical tubes with a blood pump. Circulating blood is irradiated with light at 630 nm, and the treated blood is returned to the body. (c) Cross-sectional shape of the blood circuit tube.
The cell viability of TL-Om1, a human adult T cell leukemia/lymphoma (ATL) cell line, mixed with erythrocytes after 5-ALA/PDT treatment was examined in four different cross-sectional shapes (Table 1). For diameters D1 and D2, although the exact diameters cannot be shown because of confidentiality of device development, they indicate that D1 (mm) is A < B and D2 (mm) is a < b < c < d, respectively (Table 1 and Fig. 4c). In the presence of erythrocytes, the cell-killing effect was observed at irradiations of 30 J/cm2 or higher. The cell-killing effect was slight in tubes with a diameter D1 larger than B mm, but a clear decrease in cell viability was observed as diameter D1 decreased and, which was considered to be caused by erythrocytes inhibiting light transmission. Furthermore, the cell-killing effect tended to decrease as the diameter D2 increased, which was likely to the decrease in the irradiation energy density per cell as the volume in the tube increased.
Cell-killing effect in the blood circuit
Based on Table 1, a tube with a cross-section of diameter D1 = A mm and diameter D2 = c mm was selected to confirm the cell-killing effect of 5-ALA/PDT using TL-Om1 and ATN-1 cells supplemented with erythrocytes. Cell death was observed immediately after irradiation (0 h) in a 5-ALA concentration- and light intensity-dependent manner (Fig. 5a,c). Furthermore, the cell viability of these 5-ALA/PDT-treated cells continued to decrease after 24 h of irradiation (Fig. 5b,d), indicating that the cells gradually died over time. This cell death pattern was similar to that of 5-ALA/PDT-treated cells with low irradiation, which demonstrated antitumor immunostimulatory effects in the C6 rat glioma model.
Cell-killing effect in the blood circuit using 5-ALA/PDT. TL-Om1 or ATN-1 cells incubated in the presence of 5-ALA (0 to 0.5 mmol/L) were mixed with erythrocytes, flowed into tubes with a peristaltic pump, and irradiated. (a,b) Viability (%) of TL-Om1 cells immediately (0 h) and 24 h after irradiation. (c,d) Viability (%) of ATN-1 cells immediately (0 h) and 24 h after irradiation. Values are presented as mean (SD).
Intracellular PpIX accumulation in naïve T cells and various hematological tumor cells
Tumor-specific intracellular PpIX accumulation was investigated using naïve T cells and ATL cells without erythrocytes. High-performance liquid chromatography (HPLC) analysis was performed to quantify the level of intracellular PpIX. Low accumulation of intracellular PpIX was observed in naïve T cells, but a 5-ALA dose-dependent increase in intracellular PpIX was observed in the ATL cell lines (Fig. 6). In addition, as this extracorporeal blood circulating PDT system targets leukemia cells, cell lines for acute myeloid leukemia (AML), chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), non-Hodgkin’s lymphoma (NHL), and myelodysplastic syndrome (MDS) were used to confirm whether 5-ALA/PDT was effective in hematological tumors other than ATL. Consequently, 5-ALA treatment produced a dose-dependent increase in intracellular PpIX accumulation in all hematological tumor cell lines (Fig. 6).
Intracellular PpIX accumulation in various hematological tumor cells. Intracellular PpIX (mg/g protein) normalized to concentration of cellular proteins in cells incubated with 5-ALA (0–0.5 mmol/L). Naïve T cells, ATL cell lines (TL-Om1 and ATN-1), AML cell lines (HL-60, Kasumi-1, MOLM-13, and THP-1), CML cell line (KCL-22), ALL cell line (CCRF-SB), NHL cell line (HuT78), and MDS cell line (SKM-1) were evaluated. Values are presented as mean (SD).
Discussion
In this study, we demonstrate that intravenous administration of 5-ALA/PDT-treated cells in rats produced an antitumor effect. The antitumor effect was accompanied by immune activation characterized by infiltrating CD8-positive T cells into the tumor. This effect was confirmed only in low-irradiated 5-ALA/PDT-treated cells and not in high-irradiated treated cells. For intravenously administered cells, the high-irradiated cells were considered predominantly necrotic, whereas the low-irradiated cells were a mixture of necrotic and gradually dying cells. Although some live cells were observed by flow cytometry in the low-irradiated cells, no lung lesions, occurring with intravenous injection of live C6 cells, were observed at autopsy and no effect of these live cells was observed.
In addition, the expression of cell surface calreticulin was suggested to be involved in immune activation. No antitumor effect was observed in rats with any of the anticancer drug–treated cells administrated intravenously. Anticancer drug–treated cells also expressed the same level of calreticulin as those treated with PDT. However, these anticancer drug–treated cells were mostly apoptotic. This suggests that activation of antitumor immunity requires both necrotic and gradually dying tumor cells with simultaneous sustained presentation of calreticulin.
Annexin V+/PI+ cells are typically classified as necrotic but have also been reported to include necroptotic and pyroptotic cells, which arise owing to programed cell death13. However, Annexin V+/PI− cells do not include these cell types and are identified as apoptotic cells13,14. Herein, we classified Annexin V+/PI− cells as apoptotic based on previous reports. Similarly, Annexin V+/PI+ cells observed immediately after irradiation (0 h) were primarily classified as necrotic cells owing to the high cytotoxicity of 5-ALA/PDT. By contrast, gradually dying Annexin V+/PI+ cells observed at 4 and 24 h after low irradiation may also include necroptotic and pyroptotic cells in addition to necrotic cells. To further investigate the types of cell death involved in Annexin V+/PI+ cells gradually dying, we performed additional experiments with various inhibitors. Cell death caused by low irradiation showed a tendency to be suppressed by inhibitors of pyroptosis and necroptosis (Supplemental Fig. 1). In addition, a subset of Annexin V+/PI− apoptotic cells was observed in cell death induced by low irradiation. These findings suggest that cells subjected to low irradiation eliciting antitumor immune effects upon intravenous administration to rats likely include necrotic, apoptotic, pyroptotic, and necroptotic cells.
This study demonstrated that intravenous administration of 5-ALA/PDT-treated cells is an effective therapy for cancer vaccination. PDT-based cancer vaccines have been reported15,16, and PDT-treated cells are strongly indicated as antigens17. However, PDT-treated cells have previously been injected subcutaneously or peritumorally18,19,20, and whether intravenous administration could induce antitumor immune effects was unknown. Furthermore, intravenous administration of necrotic or apoptotic cells alone did not induce antitumor effects. These findings suggest the conditions necessary for immune activation. A combination of necrotic and gradually dying cells induced by low irradiation may enable the presentation of TAA and TSA through necrosis, as well as the release of DAMPs, such as calreticulin, through programed cell death (i.e., apoptosis and necroptosis). Our results are consistent with those in studies that showed that TAA and TSA were present through necrosis in cells treated with PDT, whereas DAMPs were released through apoptosis21,22. However, whether the release of DAMPs must be mediated by PDT-induced programed cell death is unclear. Further studies are required, such as injecting a mixture of apoptotic tumor cells treated with anticancer drugs and necrotic tumor cells treated with high irradiation to confirm this.
The process whereby cancer antigens are presented to antigen-presenting cells in the blood is not yet understood. However, dying cells that had been treated with 5-ALA/PDT were responsible for inducing antitumor immunity in this study. Phagocytic cells in the spleen process such dying cells, and antigen presentation may occur during this process23. Splenic DCs originate from marrow hematopoietic stem cells, specialize in antigen processing and presentation, and are key initiators and controllers of adaptive immunity24. The C6 glioma used in this study is also considered to be an immunogenic cancer cell line25. Thus, intravenous administration of cells may activate splenic DC-mediated antitumor immunity in the presence of DAMPs, inducing CD8+ T cell activation and tumor reduction.
The intravenous administration of 5-ALA/PDT-treated cells has antitumor effects, indicating the potential for a novel therapeutic approach that combines extracorporeal blood circulation and PDT. We devised and developed an extracorporeal PDT system for clinical use that targets leukemia cells (Fig. 4) by intravenously delivering a mixture necrotic and gradually dying cells. A similar concept was presented in previous reports26,27. Herein, cell-killing assays with 5-ALA/PDT were performed by circulating a mixture of erythrocytes and hematological tumor cell lines in a blood circuit with optimized tubing geometry. Consequently, a gradual state of hematological tumor cell death was achieved over a 24-h period after irradiation. We also found that irradiation in the presence of erythrocytes, which inhibits light transmission, required a higher irradiation energy density of 30 to 100 J/cm2 compared with no erythrocytes, which required 7.5 J/cm2. The accumulation of intracellular PpIX was observed in various hematological tumor cell lines, including ATL, AML, CML, ALL, NHL, and MDS. 5-ALA/PDT has been shown to kill hematological tumor cells in vitro, both in cell lines28,29,30 and in clinical samples31,32. Our study found that 0.125–0.5 mmol of 5-ALA produced high levels of PpIX accumulation and cytotoxic effects in hematological tumor cells. This concentration can be achieved in the blood by oral administration of a 20 mg/kg dose of 5-ALA, which is the approved dose as a photodiagnostic agent for glioma in humans33. Thus, an extracorporeal PDT system may be applicable to these types of leukemia.
Experimental studies have shown that PDT treatment with extracorporeal blood circulation and hematoporphyrin monomethyl ether could prolong survival in leukemic rats34, whereas PDT treatment with photodithiazine and intravascular light irradiation without extracorporeal blood circulation was reported to increase the survival rate35. In these rat studies, the systemic therapeutic effect may have been due to the direct cell-killing effect of PDT on leukemia cells. However, the direct cell-killing effect alone may not provide sufficient clinical effect in hematological malignancies where tumors occur in sites other than the peripheral blood; thus, a so-called abscopal effect, wherein the shrinkage of untreated tumors occurred concurrently with the shrinkage of tumors upon local treatment, is required6,7. In this regard, our findings indicate that blood extracorporeal 5-ALA/PDT treatment induces an antitumor effect via immune activation similar to the abscopal effect.
A form of PDT combined with extracorporeal circulation, called extracorporeal photopheresis (ECP), has been used clinically36. ECP involves ultraviolet (UV) light irradiation of buffy coat treated with 8-methoxypsoralen as a photosensitizer and has been demonstrated to have efficacy in treating mycosis fungoides, Sezary syndrome skin lesions, and distal lesions37,38. However, 8-MOP/ECP kills diseased and healthy cells without selectivity and has limited efficacy in some cases39. Therefore, several new attempts to combine UV-ECP with 5-ALA, which is considered to be safer and more tumor-selective than 8-MOP, have been reported but were targeted at immune disorders40,41. The effects of UV-ECP with 5-ALA on tumors remain unclear. The direct cell-killing and immunostimulatory effects of 5-ALA/PDT may be more promising than UV-ECP with 5-ALA as shown in this study. In terms of side effects, the accumulation of intracellular PpIX and cytotoxicity was not observed in naïve T cells treated with 5-ALA. In addition, we conducted nonclinical safety studies of this system in male and female minipigs, according to Good Laboratory Practice. The results showed no evidence of lethality, life-threatening toxicities, or irreversible findings with a single administration of 60 mg/kg 5-ALA HCl and a single irradiation of 120 J/cm2.
This study has some limitations. First, as mentioned above, the process whereby cancer antigens enter the bloodstream and activate antitumor immunity is not yet fully understood. Further studies, including those involving splenectomized rats, are required to determine whether splenic DCs are involved in tumor antigen presentation. Second, whether hematological tumor cells are as immunogenic as the C6 glioma cells was not examined in this study. However, they have been reported to be highly immunogenic in leukemias such as ATL and CML. ATL cells express sufficient levels of antigen to evoke specific T cell responses in vivo42. It has also been reported that the photooxidative changes produced by PDT result in alterations to the antigenic fingerprint, including the expression of neoantigen, render treated cancer cells more immunogenic43. Further detailed studies are required on their therapeutic efficacy against these diseases. Finally, although this study focused on the antitumor immune effects of gradually dying cells, the contribution of each cell death type (e.g., necrosis, apoptosis, necroptosis, and pyroptosis) to the antitumor immune effects in the C6 rat glioma model requires further study. A prior study revealed that 5-ALA/PDT induces necroptosis and pyroptosis, leading to antitumor effects44.
In conclusion, these results indicate that the combination of 5-ALA/PDT and extracorporeal circulation has a direct cell-killing effect and an indirect antitumor effect due to tumor immune activity. The novel extracorporeal blood circulating PDT system using 5ALA described in this study may provide a new treatment option for patients with hematological malignancies, especially immunogenic leukemia.
Materials and methods
Cells and cell cultures
The rat glioma cell line C6 was obtained from the American Type Culture Collection (ATCC). C6 cells were cultured in Ham’s F-12K medium (Thermo Fisher Scientific) containing 2.5% heat-inactivated fetal bovine serum (COSMO BIO) and antibiotics. Hematological tumor cell lines evaluated included: two ATL cell lines, TL-Om1 (provided by Dr. K. Sugamura, Miyagi Cancer Center Research Institute, Japan) and ATN-1 (RIKEN BRC); four AML cell lines, HL-60 (Cell Resource Center for Biomedical Research, Tohoku University), Kasumi-1 (ATCC), THP-1 (ATCC), and MOLM-13 (Deutsche Sammlung von Mikroorganismen und Zellkulturen GmbH); a CML cell line, KCL-22 (JCRB Cell Bank); an ALL cell line, CCRF-SB (ATCC); an NHL cell line, HuT78 (ATCC), and MDS cell line, SKM-1 (JCRB Cell Bank). Normal human peripheral blood mononuclear cells (PBMCs) were obtained from PRECISION for Medicine. Hematological tumor cell lines and PBMCs were cultured in RPMI1640 medium (NACALAI TESQUE) containing 10% heat-inactivated fetal calf serum (NICHIREI BIOSCIENCES) and antibiotics. All cells were cultured in a humidified atmosphere of 5% CO2 at 37°C.
Rat C6 glioma model and intravenous administration
Male F344 rats, 8 weeks of age at the start of the study, were purchased from Jackson Laboratory Japan, Inc. and grouped based on body weight (n = 3 to 6 per group). Prior to subcutaneous transplantation of C6 cells, 5ALA/PDT- or anticancer drug–treated C6 cells (1 × 107 cells per 0.5 mL PBS) were administered intravenously three times at an interval of one week. For 5-ALA/PDT-treated cells, C6 cells were cultured with 5-ALA hydrochloride (Sigma-Aldrich) at a final concentration of 1 mmol/L for 24 h. Cells were then washed with PBS, placed in Tygon tubes, and irradiation performed at high and low conditions (317 and 7.5 J/cm2, respectively) using an irradiation device (Otsuka Electronics) with a wavelength of 630 nm. For anticancer drug–treated cells, C6 cells were loaded with 20 μg/mL MTX, 75 μg/mL DOX, or 62.5 μg/mL EPI as final concentrations for 48 h and washed with PBS. All anticancer drugs were obtained from Sigma-Aldrich. For the control group, 0.5 mL of PBS was administered via the tail vein. The day after the third intravenous injection of 5-ALA/PDT-treated, anticancer drug–treated cells, or PBS, intact C6 cells (1 × 107 cells in 0.5 mL PBS) were subcutaneously transplanted into the left flank of the rats. All rats were euthanized with an overdose of isoflurane on day 10 (Supplemental Fig. 2). Tumor growth was assessed by measuring with a caliper every 2 days, and tumor volume was calculated as 1/6 × π × D × d2, where D = maximal tumor diameter and d = tumor diameter perpendicular to D.
All experiments were approved by the Ethics Committee for Animal Experimentation of JIMRO Co., Ltd. (approved protocol number: E-096b-2 and E-096c) and reported in accordance with ARRIVE guidelines. All animals were handled in accordance with institutional guidelines.
Flow cytometry
PDT- or anticancer drug–treated cells were stained using the FITC Annexin V Apoptosis Detection Kit I (BD Biosciences) to detect live, apoptotic, and dead cells. Cell surface calreticulin expression was assessed using FITC-conjugated anti-calreticulin polyclonal antibody (Bioss). Samples were analyzed using a FACS Calibur (BD Bioscience).
Immunostaining of CD8+ T cells
Tumor tissues were fixed in formalin and embedded in paraffin. Tissue blocks were sectioned at 4 μm and mounted on positively charged glass slides. CD8+ T cells were immunostained using a mouse monoclonal anti-CD8a antibody (Clone: OX-8, BD Bioscience) and the Avidin–Biotin Complex detection method. Slides were counterstained with hematoxylin. After dehydration, coverslips were mounted with permanent mounting medium. CD8+ T cell populations in the tumor were determined using an optical microscope (DM5000 B, Leica Microsystems). Briefly, the number of CD8+ cells was counted in three different fields at a high-power field (400 ×), and the average number of positive cells per field was calculated.
Enzyme-linked immunosorbent assay (ELISA) for IFN-γ
Splenocytes were collected from the spleens of rats 10 days after subcutaneous allogenic transplantation using Lympholyte-Rat (Cedarlane Laboratories). Splenic lymphocytes and C6 cells were mixed at a concentration of 1 × 105 cells each and cocultured in 96-well plates for 24 h. After coculture, the culture supernatant was analyzed for IFN-γ levels using an ELISA quantitation kit (R&D Systems).
Cell viability in the circulating PDT system
TL-Om1 and ATN-1 were incubated with 5-ALA hydrochloride (KIYAN PHARMA) at final concentrations of 0, 0, 0.125, 0.25, and 0.5 mmol/L for 4 h. Cells with the supernatant removed were mixed in phenol red-free culture medium with erythrocytes fractionated from human whole blood type O (COSMO BIO) to achieve a hematocrit of 50%. Cells and erythrocyte suspensions were flowed through the tubes using a peristaltic pump and irradiated at 30 and 100 J/cm2 using an irradiation device (Otsuka Electronics). After irradiation, only cells were isolated using the Dynabeads CD4 Positive Isolation Kit (Thermo Fisher Scientific). Immediately after isolation (0 h) and after 24 h of incubation, the optical density at 450/630 nm of each well was measured using the Cell Counting Kit-8 (DOJINDO). Cell viability was calculated as 100% of cells not loaded with 5-ALA.
High-performance liquid chromatography analysis of intracellular PpIX
TL-Om1, ATN-1, HL-60, Kasumi-1, MOLM-13, THP-1, KCL-22, CCRF-SB, HuT78, SKM-1, and naïve T cells were incubated with 5-ALA hydrochloride at final concentrations of 0, 0.0625, 0.125, 0.25, and 0.5 mmol/L for 4 h. Cell suspensions were centrifuged, and supernatants removed. Cells were lysed completely in 0.1 mol/L NaOH solution. An equal volume of perchloric acid/2-propanol solution (1 mol/L perchloric acid and 50% 2-propanol mixture) was added to cell lysates, and the mixture was allowed to stand for 15 min under light-shielded conditions. After centrifugation, the resulting supernatant was analyzed via HPLC. PpIX was separated using an HPLC system (LCMS8040, Shimadzu Corporation) equipped with a reverse-phase column (TSKgel ODS-100V 3 μm, 2 mm ID × 150 mm, Tosoh Corporation). Elution was started with solvent A (0.1 v/v% formic acid), followed by a linear gradient of 0%–100% solvent B (acetonitrile) in solvent A followed by 100% solvent B. PpIX was detected with a fluorospectrometer (λex = 405 nm; λdet = 630 nm), and the PpIX concentration was estimated from the area of the PpIX peak compared with a standard PpIX (Sigma-Aldrich) sample. Protein concentrations of cell lysates dissolved in NaOH were determined using the BCA Protein Assay Kit (Thermo Fisher Scientific). Intracellular PpIX (μg/g protein) was calculated as PpIX per cellular protein.
Statistical analysis
Data are presented as the mean ± SD. Statistical analysis was performed using Dunnett’s multiple comparison tests after a two-way repeated measures ANOVA (Fig. 1b,c and 3a), Tukey’s test (Fig. 1f,g and 3e) and Student’s t-test (Fig. 2e). The statistical analysis software used was EZR (Version 1.64, Saitama Medical Center, Jichi Medical University)45, which is a graphical user interface for R (The R Foundation for Statistical Computing).
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.
References
Dougherty, T. J. et al. Photodynamic therapy. J. Natl. Cancer Inst. 90, 889–905 (1998).
Morton, C. A. The emerging role of 5-ALA-PDT in dermatology: is PDT superior to standard treatments?. J. Dermatolog. Treat. 13 (1), S25–S29 (2002).
Pignatelli, P., Umme, S., D’Antonio, D. L., Piattelli, A. & Curia, M. C. Reactive oxygen species produced by 5-aminolevulinic acid photodynamic therapy in the treatment of cancer. Int. J. Mol. Sci. 24, 8964. https://doi.org/10.3390/ijms24108964 (2023).
Lang, K., Schulte, K. W., Ruzicka, T. & Fritsch, C. Aminolevulinic acid (Levulan) in photodynamic therapy of actinic keratoses. Skin Ther. Lett. 6, 1–2 (2001).
Mroz, P., Hashmi, J. T., Huang, Y. Y., Lange, N. & Hamblin, M. R. Stimulation of anti-tumor immunity by photodynamic therapy. Expert Rev. Clin. Immunol. 7, 75–91 (2011).
Thong, P. S. et al. Photodynamic-therapy-activated immune response against distant untreated tumours in recurrent angiosarcoma. Lancet Oncol. 8, 950–952 (2007).
Lou, J. et al. Repeated photodynamic therapy mediates the abscopal effect through multiple innate and adaptive immune responses with and without immune checkpoint therapy. Biomaterials 292, 121918. https://doi.org/10.1016/j.biomaterials.2022.121918 (2023).
Panzarini, E., Inguscio, V. & Dini, L. Immunogenic cell death: can it be exploited in photodynamic therapy for cancer?. BioMed Res. Int. 2013, 482160. https://doi.org/10.1155/2013/482160 (2013).
Alzeibak, R. et al. Targeting immunogenic cancer cell death by photodynamic therapy: past, present and future. J. Immunother. Cancer 9, e001926. https://doi.org/10.1136/jitc-2020-001926 (2021).
Adkins, I., Fucikova, J., Garg, A. D., Agostinis, P. & Špíšek, R. Physical modalities inducing immunogenic tumor cell death for cancer immunotherapy. Oncoimmunology 3, e968434. https://doi.org/10.4161/21624011.2014.968434 (2014).
Jung, N. C. et al. Photodynamic therapy-mediated DC immunotherapy is highly effective for the inhibition of established solid tumors. Cancer Lett. 324, 58–65 (2012).
Cramer, G. M., Moon, E. K., Cengel, K. A. & Busch, T. M. Photodynamic therapy and immune checkpoint blockade†. Photochem. Photobiol. 96, 954–961 (2020).
Yu, P. et al. Pyroptosis: mechanisms and diseases. Signal Transduct. Target Ther. 6, 128. https://doi.org/10.1038/s41392-021-00507-5 (2021).
Wang, S., Liu, Y., Zhang, L. & Sun, Z. Methods for monitoring cancer cell pyroptosis. Cancer Biol Med. 19, 398–414 (2022).
Gollnick, S. O., Vaughan, L. & Henderson, B. W. Generation of effective antitumor vaccines using photodynamic therapy. Cancer Res. 62, 1604–1608 (2002).
Kleinovink, J. W. & Ossendorp, F. Combination of photodynamic therapy and therapeutic vaccination. Methods Mol. Biol. 2451, 597–604 (2022).
Chou, W. et al. Photodynamic therapy-induced anti-tumor immunity: influence factors and synergistic enhancement strategies. Pharmaceutics 15, 2617. https://doi.org/10.3390/pharmaceutics15112617 (2023).
Zhang, H. et al. Antitumor effects of DC vaccine with ALA-PDT-induced immunogenic apoptotic cells for skin squamous cell carcinoma in mice. Technol. Cancer Res. Treat. 17, 1533033818785275. https://doi.org/10.1177/1533033818785275 (2018).
Korbelik, M. & Sun, J. Photodynamic therapy-generated vaccine for cancer therapy. Cancer Immunol. Immunother. 55, 900–909 (2006).
Korbelik, M., Stott, B. & Sun, J. Photodynamic therapy-generated vaccines: relevance of tumour cell death expression. Br. J. Cancer 97, 1381–1387 (2007).
Garg, A. D., Krysko, D. V., Vandenabeele, P. & Agostinis, P. DAMPs and PDT-mediated photo-oxidative stress: exploring the unknown. Photochem. Photobiol. Sci. 10, 670–680 (2011).
Tan, L., Shen, X., He, Z. & Lu, Y. The role of photodynamic therapy in triggering cell death and facilitating antitumor immunology. Front. Oncol. 12, 863107. https://doi.org/10.3389/fonc.2022.863107 (2022).
Bronte, V. & Pittet, M. J. The spleen in local and systemic regulation of immunity. Immunity 56, 1152. https://doi.org/10.1016/j.immuni.2023.04.004 (2023).
Merad, M., Sathe, P., Helft, J., Miller, J. & Mortha, A. The dendritic cell lineage: ontogeny and function of dendritic cells and their subsets in the steady state and the inflamed setting. Annu. Rev. Immunol. 31, 563–604 (2013).
Giakoumettis, D., Kritis, A. & Foroglou, N. C6 cell line: the gold standard in glioma research. Hippokratia 22, 105–112 (2018).
Kim, G. & Gaitas, A. Extracorporeal photo-immunotherapy for circulating tumor cells. PLoS One 10, e0127219. https://doi.org/10.1371/journal.pone.0127219 (2015).
Oka, T., Matsuoka, K. I. & Utsunomiya, A. Sensitive photodynamic detection of adult T-cell leukemia/lymphoma and specific leukemic cell death induced by photodynamic therapy: current status in hematopoietic malignancies. Cancers (Basel) 12, 335. https://doi.org/10.3390/cancers12020335 (2020).
Grebenová, D. et al. Selective destruction of leukaemic cells by photo-activation of 5-aminolaevulinic acid-induced protoporphyrin-IX. J. Photochem. Photobiol. B 47, 74–81 (1998).
Eléouet, S. et al. Heterogeneity of delta-aminolevulinic acid-induced protoporphyrin IX fluorescence in human glioma cells and leukemic lymphocytes. Neurol. Res. 22, 361–368 (2000).
Cai, J., Zheng, Q., Huang, H. & Li, B. 5-aminolevulinic acid mediated photodynamic therapy inhibits survival activity and promotes apoptosis of A375 and A431 cells. Photodiagn. Photodyn. Ther. 21, 257–262 (2018).
Oka, T. et al. Metabolic abnormalities in adult T-cell leukemia/lymphoma and induction of specific leukemic cell death using photodynamic therapy. Sci. Rep. 8, 14979. https://doi.org/10.1038/s41598-018-33175-7 (2018).
Sando, Y. et al. Author correction: 5-aminolevulinic acid-mediated photodynamic therapy can target aggressive adult T cell leukemia/lymphoma resistant to conventional chemotherapy. Sci. Rep. Sci. Rep. 11, 6420. https://doi.org/10.1038/s41598-021-86066-9 (2021).
Stummer, W., Stepp, H., Wiestler, O. D. & Pichlmeier, U. Randomized, prospective double-blinded study comparing 3 different doses of 5-aminolevulinic acid for fluorescence-guided resections of malignant gliomas. Neurosurgery 81, 230–239 (2017).
Yin, H. et al. Evaluation of the effects of systemic photodynamic therapy in a rat model of acute myeloid leukemia. J. Photochem. Photobiol. B 153, 13–19 (2015).
Wen, L. Y., Bae, S. M., Chun, H. J., Park, K. S. & Ahn, W. S. Therapeutic effects of systemic photodynamic therapy in a leukemia animal model using A20 cells. Lasers Med. Sci. 27, 445–452 (2012).
Knobler, R. et al. Extracorporeal photopheresis: past, present, and future. J. Am. Acad. Dermatol. 61, 652–665 (2009).
Zic, J. A. Extracorporeal photopheresis in the treatment of mycosis fungoides and Sézary syndrome. Dermatol. Clin. 33, 765–776 (2015).
Szodoray, P., Papp, G., Nakken, B., Harangi, M. & Zeher, M. The molecular and clinical rationale of extracorporeal photochemotherapy in autoimmune diseases, malignancies and transplantation. Autoimmun. Rev. 9, 459–464 (2010).
Christensen, E. et al. Application of photodynamic therapy with 5-aminolevulinic acid to extracorporeal photopheresis in the treatment of patients with chronic graft-versus-host disease: A first-in-human study. Pharmaceutics 13, 1558. https://doi.org/10.3390/pharmaceutics13101558 (2021).
Zhang, M., Zhao, Y., Ma, H., Sun, Y. & Cao, J. How to improve photodynamic therapy-induced antitumor immunity for cancer treatment?. Theranostics 12, 4629–4655 (2022).
Espeland, K. et al. Photodynamic effects with 5-aminolevulinic acid on cytokines and exosomes in human peripheral blood mononuclear cells from patients with Crohn’s disease. Int. J. Mol. Sci. 24, 4554. https://doi.org/10.3390/ijms24054554 (2023).
Kurihara, K. et al. Potential immunogenicity of adult T cell leukemia cells in vivo. Int. J. Cancer 114, 257–267 (2005).
Korbelik, M. Cancer vaccines generated by photodynamic therapy. Photochem. Photobiol. Sci. 10, 664–669 (2011).
Wang, L., Chelakkot, V. S., Newhook, N., Tucker, S. & Hirasawa, K. Inflammatory cell death induced by 5-aminolevulinic acid-photodynamic therapy initiates anticancer immunity. Front. Oncol. 13, 1156763. https://doi.org/10.3389/fonc.2023.1156763 (2023).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 48, 452–458 (2013).
Acknowledgements
We thank Yuko Yagihashi and Eiko Shimizu of JIMRO for their outstanding technical assistance. We thank Dr. Shiro Tochizawa of Otsuka Pharmaceutical for his invaluable assistance and suggestions. We also thank Dr. Kazuhide Ohta for his invaluable ideas.
Funding
The authors received funding from Otsuka Medical Devices Co., Ltd. The funder provided support research funds but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
H.M., M.K., Y.H., and K.K. conceived and designed the study. H.M. performed the animal experiments and K.K. supervised the study. Y.H. performed experiments with hematologic tumor cells and M.K. supervised the study. A.T., S.K., T.F., and H.A. devised and developed the extracorporeal blood circulation PDT system. H.M., M.K., and K.K. interpreted data and drafted the manuscript. M.K. wrote the manuscript. All authors carefully reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Maegawa, H., Kohashi, M., Harada, Y. et al. Antitumor immunostimulatory effect via cell-killing action of a novel extracorporeal blood circulating photodynamic therapy system using 5-aminolevulinic acid. Sci Rep 15, 1064 (2025). https://doi.org/10.1038/s41598-024-84861-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84861-8