Abstract
To investigate the association between dietary microbes intake and sedentary behavior with mortality risk in hypertensive adults in the United States. This study uses data from hypertensive individuals included in the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018. The relationship between live-microbe intake, sedentary time, and mortality risk among hypertensive individuals is preliminarily explored using Kaplan–Meier curves. Cox proportional hazards models are employed to analyze the associations separately and jointly, followed by subgroup analyses and sensitivity analysis to assess model stability. The study enrolled 10,036 participants with hypertension, among whom 1599 deaths occurred, including 512 cardiovascular disease-related deaths. Initial Kaplan–Meier curve analysis revealed that hypertensive individuals with both low intake of dietary live microbes and prolonged sedentary time had significantly higher mortality risk. Subsequent Cox proportional hazards model analysis demonstrated that high dietary microbial intake combined with reduced sedentary time were associated with lower mortality risk in hypertensive patients. Joint effect analysis suggested that maintaining proper dietary microbial eating habit may mitigate the adverse health effects of chronic sedentary behavior in this population. Subgroup and sensitivity analyses confirmed the stability of these findings across most examined conditions. The mortality risk in hypertensive individuals due to low intake of dietary live microbes and prolonged sedentary behavior is cumulative. Consuming foods rich in dietary microbes may help reduce the mortality risk associated with sedentary behavior in hypertensive populations.
Similar content being viewed by others
Introduction
Hypertension is one of the most common chronic diseases worldwide, significantly impacting both quality of life and life expectancy for affected populations1. Epidemiological data indicate that the prevalence of hypertension continues to rise due to lifestyle changes and population aging. According to the World Health Organization (WHO), approximately 1.3 billion people globally suffer from hypertension, with around 10 million deaths each year attributed to hypertension and its complications2. Reducing mortality risk among hypertensive individuals has therefore become a pressing issue in public health. In this context, sedentary behavior and live-microbe dietary intake are increasingly recognized as lifestyle factors that may exacerbate or improve hypertension prognosis.
In the development process of modern society today, sedentary behavior has already evolved into an extremely common lifestyle pattern. Especially in the contexts of daily work and leisure activities, the daily sedentary duration of most individuals significantly exceeds their activity time3,4. Numerous studies have shown that this prolonged sedentary state is regarded as a high-risk factor for a series of chronic diseases such as cardiovascular diseases, diabetes, and cancer5,6, and there exists a close and complex internal relationship with the overall health outcomes of the population. Some research reports have pointed out that prolonged and continuous sedentary behavior can lead to the impairment of vascular endothelial function. Under the sedentary state, the normal metabolism and functional regulation of vascular endothelial cells are disrupted, resulting in the imbalance of the synthesis and release of vasoactive substances. The release of vasodilatory substances such as nitric oxide decreases, while the secretion of vasoconstrictive substances such as endothelin-1 relatively increases, thereby causing the impairment of vascular dilation function7,8. At the same time, sedentary behavior can significantly enhance insulin resistance, interfere with glucose and lipid metabolism, and trigger metabolic syndrome9,10,11, further accelerating the process of atherosclerosis and exacerbating the progression of hypertension. In addition, under the sedentary state, the sympathetic nerve remains in a relatively excited state continuously, and the vascular tension increases, thus further raising the blood pressure and increasing the pressure load on the cardiovascular system12,13. Given the numerous adverse effects of the above-mentioned sedentary behavior on patients with hypertension, reducing sedentary time has been widely and unanimously recommended as one of the key components of lifestyle interventions for patients with hypertension. By changing this unhealthy lifestyle habit, it is expected to improve the vascular function, metabolic status, and blood pressure control of patients with hypertension, and thus enhance their overall health level.
Enhancing the dietary intake of live microorganisms has emerged as another noteworthy lifestyle intervention in recent years, demonstrating unique potential in modulating gut microbiota and promoting cardiovascular health14. Dietary microorganisms are microbes consumed via food or supplements that can positively impact human health, such as probiotics and other functional microorganisms. They can be categorized into colonizing strains (such as Bifidobacterium longum and Lactiplantibacillus plantarum) and non-colonizing strains (including Lactobacillus delbrueckii subsp. bulgaricus and Bacillus subtilis var. natto) based on their intestinal colonization capacity15,16,17. For hypertensive patients, these two microbial categories exert synergistic therapeutic effects through distinct but complementary mechanisms. Colonizing strains persistently adhere to the intestinal epithelium, competitively inhibiting the proliferation of pro-inflammatory bacteria like Escherichia and Proteus, while stimulating the production of neuroactive and anti-inflammatory metabolites such as short-chain fatty acids (SCFAs) and polysaccharide A. These microbial-derived molecules not only enter systemic circulation to improve vascular endothelial function, but also act as key signaling molecules in the gut-brain axis. By modulating enteric nervous system activity and vagal afferent pathways, colonizing strains indirectly influence central regulation of blood pressure18,19,20,21. Transient gut microbes exert dual health benefits: Their metabolites can cross the blood–brain barrier or activate enteroendocrine cells to regulate neurotransmitter (serotonin, dopamine, acetylcholine) synthesis, thereby fine-tuning autonomic nervous function for physiological regulation like blood pressure control. Simultaneously, they transiently improve the gut microenvironment (pH modulation, mucus secretion) to create favorable niches for beneficial commensals, amplifying their health-promoting effects. These transient interactions yield sustained benefits even post-clearance22,23. Notably, in sedentary hypertensive patients, these microbial strains demonstrate synergistic effects in preserving intestinal ecosystem homeostasis while improving metabolic health. They enhance motility in hypokinetic intestines induced by sedentarism, prevent dysbiosis-related barrier impairment, and reduce endotoxin translocation24,25. By modulating gut microbiota locally and extending to systemic metabolic and neural regulation, dietary microorganisms collectively improve glucose homeostasis, uric acid balance, and lipid profiles, thereby mitigating sedentarism-aggravated metabolic syndrome components contributing to hypertension pathogenesis26,27,28.
However, most of the current studies are derived from animal experiments. The actual effects and mechanisms of dietary microorganisms on the health of hypertensive individuals in the human population are still unclear. Moreover, due to the similarities and differences in the gut microbiota between animals and humans, as well as the completely different living habits between humans and animals, the research results are also limited in terms of promotion and applicatio29. Therefore, there is still a lack of large-scale population studies to confirm the long-term effectiveness of different live-microbe dietary intakes and reducing sedentary time intervention in the management of hypertension. Meanwhile, the comprehensive impact of the two on the mortality risk of hypertensive individuals is still unclear, and the relevant clinical research data are relatively limited. To address this issue, this study conducts research through the large-scale clinical data of the NHANES database, systematically evaluating the comprehensive impact of sedentary behavior and differential intake of dietary live microbes on the health of patients with hypertension, in order to deepen the understanding of the roles of sedentary behavior and dietary microorganisms in the mortality risk of hypertensive individuals, provide a scientific basis for the lifestyle management of patients with hypertension, and offer a reference for formulating more targeted public health intervention strategies.
Materials and methodology
This study utilizes data from the NHANES database, conducted by the National Center for Health Statistics (NCHS) in the United States. NHANES is a comprehensive survey designed to collect representative information on the health and nutrition of the U.S. civilian population, including demographics, socioeconomic factors, diet, and health-related issues. To ensure sample diversity, NHANES employs a stratified, multistage sampling method to select participants from across the nation. The study protocol received approval from the NCHS Research Ethics Review Board of the Centers for Disease Control and Prevention, and all participants provided written informed consent. Further details are available on the NHANES website.
Inclusion and exclusion criteria for participants
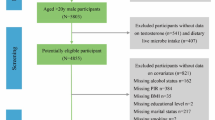
This study utilized participant data from 1999 to 2018, available on the NHANES website. Hypertensive patients were identified based on self-reported responses to questions about a physician’s diagnosis of hypertension, the use of antihypertensive medications, and the average of three blood pressure measurements (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg). A total of 15,008 hypertensive individuals were initially identified. Participants under the age of 20, those lacking data on sedentary behavior, dietary intake, survival status, or key covariates were excluded. Ultimately, 10,036 eligible participants were included in the study. The screening process is detailed in Fig. 1.
Assessment of live-microbe dietary intake and sedentary behavior
Previous studies have indicated that sterile or pasteurized foods contain very low levels of live microorganisms, unpeeled fresh fruits and vegetables contain moderate levels, and unprocessed fermented foods generally contain high levels of live microorganisms. Thus, this study estimated dietary intake of live microbes using 24-h dietary recall data. Foods were categorized by microbial content as low (104 CFU/g), moderate (104–107 CFU/g), or high (> 107 CFU/g) levels of dietary microbes. Based on food consumption, participants were divided into three groups: a low live-microbe dietary intake group (all foods with low levels of live microbes), a moderate live-microbe dietary intake group (foods including moderate levels of live microbes, excluding high levels), and a high live-microbe dietary intake group (foods including high levels of live microbes). This classification approach has been reported and applied in several studies30,31,32.
Sedentary behavior was assessed through the Global Physical Activity Questionnaire (GPAQ), conducted by trained interviewers at a mobile examination center. Participants were asked, “How much time do you spend sitting each day during work, home, commuting, or social activities? This includes time at a desk, in a car or on public transportation, reading, playing cards, watching television, or using a computer. ” Based on responses, and in line with previously published studies, sedentary time was temporarily classified into three levels: < 5 h/day, 5–8 h/day, and > 8 h/day33,34. Subsequent studies will utilize statistical algorithms to adjust sedentary time thresholds for specific population subgroups based on individualized health risk profiles.
Assessment of mortality
The NCHS linked NHANES data with NDI data using identifiers such as Social Security numbers and birth dates to obtain survival status information, with follow-up ending on December 31, 2019. If no match was found in the NDI, the participant was considered to be alive. The causes of death for survivors were classified according to the International Classification of Diseases, 10th Revision (ICD-10). Cardiovascular-related mortality in this study included rheumatic heart disease, hypertensive heart disease, ischemic heart disease, pulmonary heart disease, cardiomyopathy, endocarditis, as well as cerebral hemorrhage and cerebral infarction, with relevant ICD codes I00-I09, I11, I13, I20-I51, I60-I69.
The covariates included in this study
This study accounted for multiple covariates that could influence the relationship between dietary live microbes, sedentary behavior, and risks of cardiovascular and all-cause mortality. These variables encompassed a range of demographic characteristics within the study population, including age, gender, race, education level, income-to-poverty ratio, and BMI, as well as lifestyle factors such as smoking and alcohol consumption, and health conditions such as diabetes, coronary heart disease, depression, kidney disease, and cancer. Demographic characteristics and lifestyle habits were collected via questionnaires, while disease diagnoses were based on physician diagnosis, laboratory tests, and relevant medication use. Depression was diagnosed using a PHQ-9 score greater than 10. In the sensitivity analysis, the consumption amount of salt, the intake of dietary fiber, the usage of probiotics within 30 days, and the Healthy Eating Index (HEI)35 were also analyzed.
Statistical analyses
The statistical analysis in this study strictly adhered to the design methodology recommended by the NHANES database, applying appropriate weights for each study parameter. Continuous variables with a normal distribution were expressed as mean ± standard deviation, while non-normally distributed continuous variables were represented by the median, and categorical variables were presented as percentages. Initially, the Kaplan–Meier method was used to explore the preliminary effects of dietary live microbe intake and sedentary time on all-cause and cardiovascular mortality among hypertensive participants. Subsequently, Cox proportional hazards regression models were employed to further assess the specific impact of dietary live microbes and sedentary behavior on all-cause and cardiovascular mortality, with results presented as hazard ratios (HR) and 95% confidence intervals (CI). To examine the nonlinear relationship between sedentary time and mortality risk among hypertensive individuals, we used a restricted cubic spline (RCS) model, determining critical inflection points through segmented stepwise fitting. Based on these inflection points, participants were grouped for combined analysis according to sedentary time and levels of dietary live microbe intake. Three regression models were constructed for this analysis: Model 1, unadjusted for confounding factors; Model 2, adjusted for demographic characteristics, including age, gender, race, education level, PIR, and marital status; and Model 3, further adjusted for health-related variables, including BMI, alcohol consumption, smoking, diabetes, coronary heart disease, chronic kidney disease, cancer, and depression. Subgroup analyses and Sensitivity analysis were conducted to confirm the robustness and consistency of the findings within specific populations.In the sensitivity analysis, the consumption amount of salt, the intake of dietary fiber, the usage of probiotics within 30 days, and the HEI were also analyzed. For missing covariate data, the primary approach was complete case deletion. All statistical analyses were conducted using R software (version 4.3.1), with a two-sided P < 0.05 considered statistically significant.
Results
Demographic and clinical attributes of participants
After screening, this study ultimately included 10,036 hypertensive participants from the NHANES 1999–2018 data, comprising 5091 men and 4945 women, with 1599 cases of all-cause mortality and 512 cases of cardiovascular mortality. According to the study objectives, participants were divided into three groups based on the level of dietary live microbes. It was observed that individuals with high live-microbe dietary intake tended to have higher incomes, lower BMI, higher educational attainment, and lower risks of diabetes, kidney disease, heart disease, depression, and cancer. Additionally, those with high live-microbe dietary intake had lower risks of cardiovascular and all-cause mortality. However, we also observed that hypertensive individuals with prolonged sedentary behavior tended to consume diets high in live microbes (see Table 1).
The Kaplan–Meier curves between live-microbe dietary intake and sedentary behavior with mortality
To preliminarily explore the clinical significance of live-microbe dietary intake and sedentary time in the prognosis of hypertensive individuals, this study used Kaplan–Meier analysis to assess the association between these factors and all-cause and cardiovascular mortality. Based on prior research, dietary live microbes eating habits were categorized into three levels: low, medium, and high. Sedentary time was also divided into three levels: < 5 h/day, 5–8 h/day, and > 8 h/day. Results indicated a significant association between live-microbe dietary intake and all-cause and cardiovascular mortality in hypertensive individuals. Those with low live-microbe dietary intake had a higher risk of all-cause (PALL = 0.001) and cardiovascular (PCVD = 0.020) mortality, while those with high eating habit showed lower mortality risks. Additionally, sedentary behavior impacted long-term prognosis, with individuals who sat for less than 5 h/day having the lowest mortality risk (PALL < 0.001). However, those with 5–8 h/day and > 8 h/day sedentary time displayed similar survival curves, suggesting that the current sedentary classification may not be optimally accurate for hypertensive populations. Detailed results are shown in Fig. 2.
Kaplan–Meier analysis of the impact of live-microbe dietary intake and sedentary behavior on mortality in hypertensive patients: (A) live-microbe dietary intakes and ALL-cause mortality risk (B) live-microbe dietary intakes and CVD-cause mortality risk (C) Sedentary behavior and ALL-cause mortality risk (D) Sedentary behavior and CVD-cause mortality risk.
Cox proportional hazards regression analysis of live-microbe dietary intake and sedentary behavior with mortality
To further investigate the impact of live-microbe dietary intake and sedentary behavior on long-term prognosis, we employed Cox proportional hazards models to examine these factors separately. Results revealed that both sedentary behavior and live-microbe dietary intake remained closely associated with mortality risk in hypertensive individuals. Specifically, sedentary duration was significantly related to mortality risk: for each additional unit of sedentary time, all-cause and cardiovascular mortality risks increased by 6% and 6.5%, respectively. Compared to individuals with less than 5 h of sedentary time, those with over 8 h had significantly higher mortality risks (PALL < 0.0001, PCVD = 0.013). Using individuals with low live-microbe dietary intake as a reference, those with medium and high microbe intake showed significantly lower mortality risks (Pmiddle−ALL < 0.001, Phigh−ALL = 0.019, Pmiddle−CVD = 0.002). Details are provided in Tables 2 and 3.
The nonlinear relationship between sedentary time and mortality risk
After performing K–M and Cox proportional hazard analyses, we identified a potential nonlinear relationship between sedentary duration and mortality, suggesting that the current sedentary behavior classifications may not be optimal for hypertensive populations. Therefore, we utilized RCS curves to depict the nonlinear association between sedentary time and mortality risk in hypertensive individuals. After adjusting for relevant covariates, a “U-shaped” relationship was observed between sedentary duration and all-cause mortality risk, while no nonlinear association was found with cardiovascular mortality (see Fig. 3 for details). Using segmented stepwise fitting to calculate the inflection point between sedentary time and mortality risk, we identified 4.1 h as the threshold for both cardiovascular and all-cause mortality. Different effect values for all-cause mortality were observed before and after this 4.1-h threshold (P for interaction < 0.011), with mortality risk progressively increasing for individuals with sedentary time exceeding 4.1 h. Furthermore, a linear relationship may exist between sedentary time and cardiovascular mortality risk, with a statistically significant effect becoming more pronounced after 4.1 h (see Table 4 for details).
Joint association of live-microbe dietary intake and sedentary behavior with mortality
To explore the combined impact of live-microbe dietary intake and sedentary behavior on hypertensive individuals, we further divided sedentary behavior into two groups: those with sedentary time greater than 4.1 h and those with less than 4.1 h. Similarly, dietary live microbe intake was classified into low, medium, and high intake groups for joint analysis. Using the group with sedentary time above 4.1 h and the lowest dietary microbe intake as the reference (highest mortality risk), we found that hypertensive individuals with sedentary time under 4.1 h had significantly lower mortality risk, regardless of their level of dietary microbe intake, compared to those with sedentary time above 4.1 h. Moreover, both medium and high levels of dietary microbes were associated with lower mortality risk for both sedentary and non-sedentary hypertensive individuals, with nearly universal improvement observed across all subgroups in the non-sedentary population. In the sedentary group, dietary microbe intake significantly reduced cardiovascular mortality (HRCVD: 0.717 [0.566, 0.909]). Although statistical significance for dietary microbe intake improving overall sedentary mortality risk was not observed in the remaining groups, a trend toward reduced mortality risk was evident (P for trend < 0.05). Detailed results are presented in Table 5, and Fig. 4 illustrates the effect relationship between each group and mortality risk.
Subgroup analysis
To assess the stability of the prognostic impact of sedentary behavior and dietary microbe intake on hypertensive individuals across different populations, we conducted a subgroup analysis. The results showed no significant interaction effects across different genders, BMI categories, ages, lifestyle habits, cardiovascular, and depression status, indicating that our findings remain consistent across various populations. Further subgroup analyses on live-microbe dietary intake and sleep disorders, along with detailed subgroup analysis results, can be found in Tables S1 and S2.
Sensitivity analysis
Considering the potential impacts of salt, dietary fiber, probiotics, and healthy eating habits on the long-term prognosis of sedentary individuals with hypertension, this study conducted relevant sensitivity analyses. The key adjustments included the daily salt intake, dietary fiber intake, the use of probiotic supplements in the past 30 days, and the Healthy Eating Index (HEI). The results showed that even after adjusting for these covariates, the dietary habit with intake of dietary microorganisms could still reduce the mortality risk of sedentary individuals with hypertension. Therefore, the research findings are still very robust. Detailed results are presented in Table 6.
Discussion
This study analyzed data from 10,036 hypertensive participants (5,091 males and 4,945 females) collected by NHANES between 1999 and 2018, including 1,599 all-cause deaths and 512 cardiovascular deaths. Preliminary Kaplan–Meier analysis of sedentary behavior and dietary live microbe intake revealed that both factors were significantly associated with mortality risk in this population. Specifically, prolonged sedentary time correlated with higher mortality risk, while participants with low dietary microbial intake also demonstrated elevated mortality. To further investigate the long-term prognostic impact of these lifestyle factors, we employed Cox proportional hazards models, which confirmed their significant associations with clinical outcomes in hypertensive patients. Notably, joint analysis demonstrated that increased dietary microbial intake may attenuate the elevated mortality risk associated with sedentary behavior. Our findings suggest an intriguing protective strategy: hypertensive individuals with sedentary lifestyles may potentially reduce health risks through appropriate consumption of live microbe-rich foods.
While the combined effects of dietary microorganisms and sedentary behavior on hypertensive patients’ prognosis require further investigation, current research has elucidated their potential interactions through complex metabolic, immunological, and neural regulatory networks, which substantiate our findings. The protective effects of dietary microorganisms on health are primarily manifested in the cardiovascular system and multiple other aspects. Firstly, natural ACE-inhibitory peptides in fermented foods (such as nattokinase and lactic acid bacteria metabolites) can specifically bind to angiotensin-converting enzyme, inhibiting the conversion of angiotensin I to angiotensin II while reducing bradykinin degradation, thereby significantly improving vascular function and exerting cardioprotective effects36,37. Secondly, dietary patterns rich in microorganisms can promote the proliferation of beneficial gut microbiota (such as Lactobacillus and butyrate-producing bacteria)38, which ferment dietary fibers to produce various SCFAs (including butyrate and propionate). These metabolites possess multi-level physiological regulatory functions: at the local vascular level, they can directly enhance the activity of nitric oxide synthase in vascular endothelial cells, thereby maintaining vasodilation39; at the central nervous regulatory level, these short-chain fatty acids can modulate the activity of the hypothalamic–pituitary–adrenal axis through the bidirectional communication system of the gut-brain axis, suppressing excessive sympathetic excitation and reducing cardiac afterload40,41,42. More importantly, these short-chain fatty acids can promote the synthesis of tight junction proteins in intestinal epithelial cells, enhancing the integrity of the intestinal barrier while improving intestinal motility, effectively preventing the entry of intestinal endotoxins and pro-inflammatory factors into the circulation, thereby alleviating systemic low-grade inflammation. This anti-inflammatory effect plays a crucial role in preventing vascular endothelial injury and the development of atherosclerosis43,44.
In contrast, sedentary behavior disrupts gut microbiota equilibrium and elevates cardiovascular risk through multiple mechanisms. Prolonged sitting slows intestinal motility and reduces blood circulation, leading to abnormal increases in intestinal oxygen partial pressure that suppress the proliferation of beneficial bacteria like Bifidobacterium and Lactobacillus while promoting overgrowth of opportunistic pathogens, thereby exacerbating gut dysbiosis45,46,47,48,49. This microbial imbalance not only impairs short-chain fatty acid production50,51,52 but also compromises intestinal barrier integrity, allowing bacterial toxins and inflammatory factors to enter systemic circulation. This process triggers chronic low-grade inflammation, further activating the renin–angiotensin–aldosterone system (RAAS) and exacerbating insulin resistance, creating a vicious cycle of blood pressure elevation53,54. Crucially, reduced muscle activity from sedentariness decreases secretion of specific myokines (particularly irisin, brain-derived neurotrophic factor) that normally enhance intestinal epithelial mitochondrial function to optimize anaerobic bacterial environments. These myokines also regulate rhythmic intestinal motility and mucus secretion via the enteric-vagal nerve axis, preventing pathogenic bacterial overcolonization55,56. Additionally, lack of muscle contraction reduces anti-inflammatory myokine secretion (such as IL-10, IL-15) while visceral fat accumulation promotes macrophage infiltration, elevating proinflammatory factors like TNF-α and IL-1β that aggravate vascular endothelial damage and disrupt blood pressure regulation57,58. Collectively, this findings of this study are supported by numerous previous studies, demonstrating that combining dietary intake of live microbe-rich foods with reduced sedentary behavior produces synergistic health benefits for hypertensive patients. These results provide clinically actionable nutritional approaches for managing hypertension through targeted dietary modifications.
Nevertheless, several noteworthy findings in this study warrant further discussion. While high dietary microbial intake significantly reduced all-cause mortality risk in hypertensive patients when analyzed independently, restricted cubic spline (RCS) curve analysis stratified by sedentary status revealed a paradoxical pattern: sedentary individuals derived benefits from moderate microbial intake but showed no significant improvement with high intake. This complex phenomenon may involve multisystem interactions. For instance, prolonged sedentary behavior slows intestinal transit, while substantial supplementation with dietary microbe-rich foods may lead to excessive accumulation of microbial metabolites in the colon that surpass optimal physiological thresholds. This can result in altered pH, osmotic diarrhea, and erosion of the mucus layer, ultimately compromising intestinal barrier integrity59,60. Furthermore, chronic sedentariness-induced low-grade inflammation and reduced microbial diversity impair the gut ecosystem’s capacity to regulate high microbial loads, predisposing to dysbiosis47. Intriguingly, our baseline data also showed that while all hypertensive participants averaged 6 h of daily sitting time, those in the high microbial intake group actually had the longest sedentary duration (6.8 h). This apparent contradiction may reflect compensatory dietary patterns among sedentary office workers who frequently consume probiotic beverages (specifically yogurt, kombucha, kefir)61,62,63, potentially masking some sedentary risks. Furthermore, in wealthier participants exhibiting both prolonged sedentariness and high microbial intake, elevated salt consumption (may primarily stem from certain high-salt fermented food varieties such as salt-rich kimchi, high-sodium natto, or brine-pickled cucumbers)64 appears to counteract microbial benefits, ultimately resulting in similar HEI scores across medium and high intake groups. Conversely, lower-income individuals showed more physical activity but poorer diets (relying on processed/canned foods with minimal fruit intake), yielding higher mortality risk despite less sedentarism, as evidenced by their lower Healthy Eating Index (HEI) scores65,66,67. These counterbalancing effects likely contributed to the non-significant joint association between sedentarism and microbial intake on mortality outcomes. Based on these findings, we propose a dual intervention strategy for sedentary hypertensive patients: combining eating live microbe-containing foods with regular exercise to synergistically restore gut motility and microbial diversity (rather than solely increasing microbial intake). This integrated approach may optimize vascular function, suppress inflammatory cascades, and reestablish autonomic balance, offering a positive solution for long-term hypertension management.
In summary, our study possesses several notable strengths. We are the first to systematically investigate the combined effects of varying dietary live microbe intake levels and sedentary behavior on mortality risk in hypertensive populations, demonstrating an additive cumulative risk from both low microbial intake and prolonged sedentariness. Importantly, our application of threshold analysis to redefine sedentary behavior thresholds offers improved characterization of activity patterns in this hypertensive population. Therefore, this study provides valuable insights for hypertensive individuals with sedentary occupations (such as office workers, programmers, truck drivers). It suggests that incorporating foods rich in dietary microbes such as yogurt, kimchi, and kefir may serve as an effective dietary intervention to complement their health management. However, several limitations must be acknowledged. First, while our classification of dietary live microbes follows established expert consensus cited in numerous studies, the lack of precise microbial quantification in food items may introduce classification bias. Second, the NHANES dietary data collection relies on self-reported questionnaires, which are susceptible to recall bias regarding both food intake and sedentary time estimation. These methodological constraints necessitate validation through subsequent studies. Furthermore, as our analysis focused on the U.S. population with distinct genetic, lifestyle, healthcare and socioeconomic characteristics compared to other regions, global generalization of these findings requires caution. While our results suggest potential benefits of dietary microbial supplementation for sedentary hypertensive individuals, more robust evidence is needed to conclusively establish the relationship between live microbe consumption, sedentary behavior and mortality risk.
Conclusion
The mortality risk in hypertensive individuals due to low intake of dietary live microbes and prolonged sedentary behavior is cumulative. Consuming foods rich in dietary microbes may help reduce the mortality risk associated with sedentary behavior in hypertensive populations.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- NCHS:
-
National Center for Health Statistics
- BMI:
-
Body Mass Index
- PIR:
-
Price-to-income ratio
- SB:
-
Sedentary behavior
- CKD:
-
Chronic kidney disease
- NHANES:
-
National Health and Nutrition Examination Survey
- CVD-cause:
-
Cardiovascular disease-caused mortality
- ALL-cause:
-
All reasons-caused mortality
- HR:
-
Hazard ratios
- CI:
-
Confidence intervals
References
Zhou, B., Perel, P., Mensah, G. A. & Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 18, 785–802. https://doi.org/10.1038/s41569-021-00559-8 (2021).
World Health Organization. Global Report on Hypertension: The Race Against a Silent Killer (World Health Organization, 2023).
Bailey, D. P. Sedentary behaviour in the workplace: Prevalence, health implications and interventions. Br. Med. Bull. 137, 42–50. https://doi.org/10.1093/bmb/ldaa039 (2021).
Babey, S. H., Hastert, T. A. & Wolstein, J. Adolescent sedentary behaviors: Correlates differ for television viewing and computer use. J. Adolesc. Health. 52, 70–76. https://doi.org/10.1016/j.jadohealth.2012.05.001 (2013).
Hermelink, R. et al. Sedentary behavior and cancer—an umbrella review and meta-analysis. Eur. J. Epidemiol. 37, 447–460. https://doi.org/10.1007/s10654-022-00873-6 (2022).
Li, X., Ma, H., Zhou, T. & Qi, L. Replacing sedentary behavior time with physical activities, recommended physical activity, and incident coronary heart disease. Mayo Clin. Proc. 98, 111–121. https://doi.org/10.1016/j.mayocp.2022.06.031 (2023).
van Deel, E. D., Octavia, Y., de Waard, M. C., de Boer, M. & Duncker, D. J. Exercise training has contrasting effects in myocardial infarction and pressure overload due to divergent endothelial nitric oxide synthase regulation. Int. J. Mol. Sci. 19, 1968. https://doi.org/10.3390/ijms19071968 (2018).
Hasegawa, N. et al. Effects of different exercise modes on arterial stiffness and nitric oxide synthesis. Med. Sci. Sports Exerc. 50, 1177–1185. https://doi.org/10.1249/MSS.0000000000001567 (2018).
Engin, B. et al. Sedentary time is independently related to adipose tissue insulin resistance in adults with or at risk of type 2 diabetes. Med. Sci. Sports Exerc. 55, 1548–1554. https://doi.org/10.1249/MSS.0000000000003193 (2023).
La Favor, J. D. et al. Microvascular endothelial dysfunction in sedentary, obese humans is mediated by NADPH oxidase: Influence of exercise training. Arterioscler. Thromb. Vasc. Biol. 36, 2412–2420. https://doi.org/10.1161/ATVBAHA.116.308339 (2016).
Tjurin, P. et al. Cross-sectional associations of sedentary behavior and sitting with serum lipid biomarkers in midlife. Med. Sci. Sports Exerc. 54, 1261–1270. https://doi.org/10.1249/MSS.0000000000002916 (2022).
Subramanian, M. & Mueller, P. J. Altered differential control of sympathetic outflow following sedentary conditions: Role of subregional neuroplasticity in the RVLM. Front. Physiol. 7, 290. https://doi.org/10.3389/fphys.2016.00290 (2016).
Mueller, P. J. Influence of sedentary versus physically active conditions on regulation of plasma renin activity and vasopressin. Am. J. Physiol. Regul. Integr. Comp. Physiol. 295, R727–R732. https://doi.org/10.1152/ajpregu.00144.2008 (2008).
Abenavoli, L. et al. Gut microbiota and obesity: A role for probiotics. Nutrients 11, 2690. https://doi.org/10.3390/nu11112690 (2019).
Culp, E. J., Nelson, N. T., Verdegaal, A. A. & Goodman, A. L. Microbial transformation of dietary xenobiotics shapes gut microbiome composition. Cell 187, 6327-6345.e20. https://doi.org/10.1016/j.cell.2024.08.038 (2024).
Liu, M. et al. Lipid-lowering, antihypertensive, and antithrombotic effects of nattokinase combined with red yeast rice in patients with stable coronary artery disease: A randomized, double-blinded, placebo-controlled trial. Front. Nutr. 11, 1380727. https://doi.org/10.3389/fnut.2024.1380727 (2024).
Shah, A. B. et al. Probiotic significance of Lactobacillus strains: A comprehensive review on health impacts, research gaps, and future prospects. Gut. Microbes. 16, 2431643. https://doi.org/10.1080/19490976.2024.2431643 (2024).
O’Donnell, J. A., Zheng, T., Meric, G. & Marques, F. Z. The gut microbiome and hypertension. Nat. Rev. Nephrol. 19, 153–167. https://doi.org/10.1038/s41581-022-00654-0 (2023).
Kyoung, J. & Yang, T. Depletion of the gut microbiota enhances the blood pressure-lowering effect of captopril: Implication of the gut microbiota in resistant hypertension. Hypertens Res. 45, 1505–1510. https://doi.org/10.1038/s41440-022-00921-4 (2022).
Kong, C. Y. et al. Probiotic yogurt blunts the increase of blood pressure in spontaneously hypertensive rats via remodeling of the gut microbiota. Food Funct. 12, 9773–9783. https://doi.org/10.1039/d1fo01836a (2021).
Gómez-Contreras, A. et al. Dietary intake of table olives exerts antihypertensive effects in association with changes in gut microbiota in spontaneously hypertensive rats. Food Funct. 14, 2793–2806. https://doi.org/10.1039/d2fo02928f (2023).
Młynarska, E. et al. Gut microbiota and gut-brain axis in hypertension: Implications for kidney and cardiovascular health-a narrative review. Nutrients 16, 4079. https://doi.org/10.3390/nu16234079 (2024).
Qu, S. et al. Gut microbiota modulates neurotransmitter and gut-brain signaling. Microbiol. Res. 287, 127858. https://doi.org/10.1016/j.micres.2024.127858 (2024).
Lai, H. et al. Effects of dietary fibers or probiotics on functional constipation symptoms and roles of gut microbiota: A double-blinded randomized placebo trial. Gut. Microbes. 15, 2197837. https://doi.org/10.1080/19490976.2023.2197837 (2023).
Shen, F. et al. Ligilactobacillus acidipiscis YJ5 modulates the gut microbiota and produces beneficial metabolites to relieve constipation by enhancing the mucosal barrier. Food Funct. 15, 310–325. https://doi.org/10.1039/d3fo03259k (2024).
Zhu, W. et al. Priestia megaterium ASC-1 Isolated from pickled cabbage ameliorates hyperuricemia by degrading uric acid in rats. Microorganisms. 12, 832. https://doi.org/10.3390/microorganisms12040832 (2024).
Song, X. et al. The gut microbiota-brain axis: Role of the gut microbial metabolites of dietary food in obesity. Food Res. Int. 153, 110971. https://doi.org/10.1016/j.foodres.2022.110971 (2022).
Kim, D. W. et al. Effects of kimchi intake on the gut microbiota and metabolite profiles of high-fat-induced obese rats. Nutrients 16, 3095. https://doi.org/10.3390/nu16183095 (2024).
Amato, K. R. et al. Variable responses of human and non-human primate gut microbiomes to a Western diet. Microbiome. 3, 53. https://doi.org/10.1186/s40168-015-0120-7 (2015).
Gu, S. et al. The relationship between dietary intake of live microbes and insulin resistance among healthy adults in the US: A cross-sectional study from NHANES 2003–2020. Sci Rep. 14, 17666. https://doi.org/10.1038/s41598-024-68243-8 (2024).
Huo, X. et al. Association of dietary live microbe intake with frailty in US adults: Evidence from NHANES. J. Nutr. Health Aging. 28, 100171. https://doi.org/10.1016/j.jnha.2024.100171 (2024).
Yan, K. et al. Higher dietary live microbe intake is associated with a lower risk of sarcopenia. Clin. Nutr. 43, 1675–1682. https://doi.org/10.1016/j.clnu.2024.05.030 (2024).
Chang, Q. et al. Replacement of sedentary behavior with various physical activities and the risk of all-cause and cause-specific mortality. BMC Med. 22, 385. https://doi.org/10.1186/s12916-024-03599-2 (2024).
Sun, Y. et al. Replacement of leisure-time sedentary behavior with various physical activities and the risk of dementia incidence and mortality: A prospective cohort study. J. Sport Health Sci. 12, 287–294. https://doi.org/10.1016/j.jshs.2022.11.005 (2023).
Xu, G., Ma, E., Zhang, W. & Feng, B. Association between healthy eating index-2015 total and metabolic associated fatty liver disease in Americans: A cross-sectional study with US. National health and nutrition examination survey. Front. Nutr. 11, 1427619. https://doi.org/10.3389/fnut.2024.1427619 (2025).
Vukic, V. R. et al. In silico identification of milk antihypertensive di- and tripeptides involved in angiotensin I-converting enzyme inhibitory activity. Nutr. Res. 46, 22–30. https://doi.org/10.1016/j.nutres.2017.07.009 (2017).
Yamamoto, N., Maeno, M. & Takano, T. Purification and characterization of an antihypertensive peptide from a yogurt-like product fermented by Lactobacillus helveticus CPN4. J. Dairy Sci. 82, 1388–1393. https://doi.org/10.3168/jds.S0022-0302(99)75364-6 (1999).
Xiong, R. G. et al. Health benefits and side effects of short-chain fatty acids. Foods. 11, 2863. https://doi.org/10.3390/foods11182863 (2022).
Robles-Vera, I. et al. Protective effects of short-chain fatty acids on endothelial dysfunction induced by angiotensin II. Front. Physiol. 11, 277. https://doi.org/10.3389/fphys.2020.00277 (2020).
Robles-Vera, I., Toral, M. & Duarte, J. Microbiota and hypertension: Role of the sympathetic nervous system and the immune system. Am. J. Hypertens. 33, 890–901. https://doi.org/10.1093/ajh/hpaa103 (2020).
Bartolomaeus, H. et al. Short-chain fatty acid propionate protects from hypertensive cardiovascular damage. Circulation 139, 1407–1421. https://doi.org/10.1161/CIRCULATIONAHA.118.036652 (2019).
Richards, E. M., Li, J., Stevens, B. R., Pepine, C. J. & Raizada, M. K. Gut microbiome and neuroinflammation in hypertension. Circ. Res. 130, 401–417. https://doi.org/10.1161/CIRCRESAHA.121.319816 (2022).
Cheng, S. et al. The probiotic fermented milk of Lacticaseibacillus paracasei JY062 and Lactobacillus gasseri JM1 alleviates constipation via improving gastrointestinal motility and gut microbiota. J. Dairy Sci. 107, 1857–1876. https://doi.org/10.3168/jds.2023-24154 (2024).
Rothman, A. M. et al. Effects of interleukin-1β Inhibition on blood pressure, incident hypertension, and residual inflammatory risk: A secondary analysis of CANTOS. Hypertension 75, 477–482. https://doi.org/10.1161/HYPERTENSIONAHA.119.13642 (2020).
Aya, V., Flórez, A., Perez, L. & Ramírez, J. D. Association between physical activity and changes in intestinal microbiota composition: A systematic review. PLoS ONE 16, e0247039. https://doi.org/10.1371/journal.pone.0247039 (2021).
Aya, V., Jimenez, P., Muñoz, E. & Ramírez, J. D. Effects of exercise and physical activity on gut microbiota composition and function in older adults: A systematic review. BMC Geriatr. 23, 364. https://doi.org/10.1186/s12877-023-04066-y (2023).
Pérez-Prieto, I., Plaza-Florido, A., Ubago-Guisado, E., Ortega, F. B. & Altmäe, S. Physical activity, sedentary behavior and microbiome: A systematic review and meta-analysis. J Sci Med Sport. 27, 793–804. https://doi.org/10.1016/j.jsams.2024.07.003 (2024).
Castellanos, N. et al. Key bacteria in the gut microbiota network for the transition between sedentary and active lifestyle. Microorganisms. 8, 785. https://doi.org/10.3390/microorganisms8050785 (2020).
Xia, W. J. et al. Antihypertensive effects of exercise involve reshaping of gut microbiota and improvement of gut-brain axis in spontaneously hypertensive rat. Gut. Microbes. 13, 1–24. https://doi.org/10.1080/19490976.2020.1854642 (2021).
Carey, R. A. & Montag, D. Exploring the relationship between gut microbiota and exercise: Short-chain fatty acids and their role in metabolism. BMJ Open Sport Exerc. Med. 7, e000930. https://doi.org/10.1136/bmjsem-2020-000930 (2021).
van de Wouw, M. et al. Short-chain fatty acids: Microbial metabolites that alleviate stress-induced brain-gut axis alterations. J. Physiol. 596, 4923–4944. https://doi.org/10.1113/JP276431 (2018).
Zhu, Q., Jiang, S. & Du, G. Effects of exercise frequency on the gut microbiota in elderly individuals. Microbiologyopen. 9, e1053. https://doi.org/10.1002/mbo3.1053 (2020).
Mizoguchi, R. et al. Impact of gut microbiome on the renin-aldosterone system: Shika-machi super preventive health examination results. Hypertens. Res. 46, 2280–2292. https://doi.org/10.1038/s41440-023-01334-7 (2023).
Li X, Xia Y, Song X, Xiong Z, Ai L, Wang G. Probiotics intervention for type 2 diabetes mellitus therapy: a review from proposed mechanisms to future prospects. Crit. Rev. Food Sci. Nutr. (2024): https://doi.org/10.1080/10408398.2024.2387765.
Pinkas, M. & Brzozowski, T. The role of the myokine irisin in the protection and carcinogenesis of the gastrointestinal tract. Antioxidants 13, 413. https://doi.org/10.3390/antiox13040413 (2024).
Li, C., Cai, Y. Y. & Yan, Z. X. Brain-derived neurotrophic factor preserves intestinal mucosal barrier function and alters gut microbiota in mice. Kaohsiung J. Med. Sci. 34, 134–141. https://doi.org/10.1016/j.kjms.2017.11.002 (2018).
Parsons, T. J. et al. Physical activity, sedentary behavior, and inflammatory and hemostatic markers in men. Med. Sci. Sports Exerc. 49(3), 459–465. https://doi.org/10.1249/MSS.0000000000001113 (2017).
Lynch, G. M., Murphy, C. H., Castro, E. M. & Roche, H. M. Inflammation and metabolism: The role of adiposity in sarcopenic obesity. Proc. Nutr. Soc. 16, 1–13. https://doi.org/10.1017/S0029665120007119 (2020).
Tian, Z., Zhuang, X., Luo, M., Yin, W. & Xiong, L. The propionic acid and butyric acid in serum but not in feces are increased in patients with diarrhea-predominant irritable bowel syndrome. BMC Gastroenterol. 20, 73. https://doi.org/10.1186/s12876-020-01212-3 (2020).
Kamath, P. S., Phillips, S. F. & Zinsmeister, A. R. Short-chain fatty acids stimulate ileal motility in humans. Gastroenterology 95, 1496–1502. https://doi.org/10.1016/s0016-5085(88)80068-4 (1988).
Li, S. et al. Innovative beverage creation through symbiotic microbial communities inspired by traditional fermented beverages: Current status, challenges and future directions. Crit. Rev. Food Sci. Nutr. 64, 10456–10483. https://doi.org/10.1080/10408398.2023.2225191 (2024).
Pyo, Y., Kwon, K. H. & Jung, Y. J. Probiotic functions in fermented foods: Anti-viral, immunomodulatory, and anti-cancer benefits. Foods. 13, 2386. https://doi.org/10.3390/foods13152386 (2024).
de Souza, H. F. et al. Water kefir in co-fermentation with Saccharomyces boulardii for the development of a new probiotic mead. Food Sci. Biotechnol. 33, 3299–3311. https://doi.org/10.1007/s10068-024-01568-2 (2024).
Liu, L. et al. Traditional fermented soybean products: Processing, flavor formation, nutritional and biological activities. Crit. Rev. Food Sci. Nutr. 62, 1971–1989. https://doi.org/10.1080/10408398.2020.1848792 (2022).
Cunha, S. C., Alves, R. N., Fernandes, J. O., Casal, S. & Marques, A. First approach to assess the bioaccessibility of bisphenol A in canned seafood. Food Chem. 232, 501–507. https://doi.org/10.1016/j.foodchem.2017.04.006 (2017).
Franchi, C. et al. Inverse association between canned fish consumption and colorectal cancer risk: Analysis of two large case-control studies. Nutrients 14, 1663. https://doi.org/10.3390/nu14081663 (2022).
Yao, H. et al. Sex differences in association of healthy eating pattern with all-cause mortality and cardiovascular mortality. BMC Public Health 24, 2363. https://doi.org/10.1186/s12889-024-19883-y (2024).
Acknowledgements
We acknowledge NHANES databases for providing their platforms and contributing meaningful datasets.
Funding
This study was supported by The National Natural Science Foundation of China (No. 82474494), the National Key Research and Development Program of China (No. 2022YFC3500102), the Beijing Municipal Science and Technology Development Funding Program of Traditional Chinese Medicine (No. JJ-2020-69), and High Level Chinese Medical Hospital Promotion Project (No. HLCMHPP2023065). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Writing the first draft of the manuscript, statistical analyses, data organization, writing review, and editing : XC Huang, LS Hu .Research, statistical analyses, and editing: C Meng, X Xia, YY Liu Design research, supervision, editing, review, revision of the manuscript, and funding: J Li. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing of interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval and consent to participate
The data supporting the results of this study are available in NHANES database. Our analysis was conducted on the basis of publicly available data, and previous subjects signed an informed consent form. Thus, our research does not require renewed informed consent from participants or ethical approval from the NCHS Research Ethics Review Board. More detailed information can be obtained from the official NHANES website. (https://www.cdc.gov/nchs/nhanes/irba98.htm).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, X., Hu, L., Li, J. et al. Dietary intake of live microbes mitigates the mortality risk associated with sedentary behavior in US hypertensive individuals. Sci Rep 15, 16483 (2025). https://doi.org/10.1038/s41598-025-01122-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01122-y