Abstract
Chordomas are rare, aggressive tumors of the axial skeleton with limited treatment options. Genetic alterations in SMARCB1, a tumor suppressor gene, have been implicated in poorly differentiated chordomas, but their role in typical and chondroid subtypes remains unclear. This study examined 42 chordoma samples (26 typical, 16 chondroid) for SMARCB1 genetic alterations, expression patterns, and associated pathways. SMARCB1 knockdown experiments were conducted in chordoma cell lines, followed by comprehensive transcriptome analysis. No exonic SMARCB1 mutations were identified, but heterozygous loss was observed in 3/26 typical chordomas. SMARCB1 expression positively correlated with patient survival and epithelial-mesenchymal markers. Functional studies revealed that SMARCB1 knockdown significantly enhanced cell proliferation, migration, and invasion. Transcriptome analysis demonstrated enrichment of MYC targets, E2F targets, and cell cycle pathways in SMARCB1-low samples, while cellular adhesion pathways were downregulated. Notably, SLPI, LBH, and LOXL2 were significantly downregulated in SMARCB1-low samples. SMARCB1 plays an important role in chordoma progression, influencing prognosis and cellular behavior, despite infrequent genetic alterations. Its effects on key oncogenic pathways and cellular plasticity suggest potential for targeted therapies. These findings provide new insights into chordoma biology and lay the groundwork for developing SMARCB1-based prognostic tools and personalized treatment strategies.
Similar content being viewed by others
Introduction
Chordomas are rare malignant tumors that arise from notochordal remnants along the axial skeleton—predominantly the skull base (~ 35%), sacrococcygeal region (~ 50%), and vertebral column (~ 15%)—and account for only 1–4% of all bone malignancies1. Their aggressive behavior, high local-recurrence rate, and resistance to conventional chemotherapy and radiotherapy present substantial clinical challenges2,3,4. Surgical resection with wide margins remains the mainstay of treatment, yet anatomical constraints frequently preclude complete excision; population-based analyses indicate a median survival of just 8.3 years5,6.
Histologically, chordomas are divided into typical, chondroid, and poorly differentiated variants7,8. Although generally considered low- to intermediate-grade tumors, they exhibit recurrence rates up to 85% and metastasis in up to 40% of cases, underscoring the need for a deeper understanding of their molecular underpinnings.
Genomic and epigenomic studies have highlighted SMARCB1 (SNF5/BAF47/INI1)—a core subunit of the SWI/SNF chromatin-remodeling complex—as a key tumor-suppressor gene located at chromosome 22q11.29. SMARCB1 loss defines a spectrum of SMARCB1-deficient neoplasms, including rhabdoid tumors and epithelioid sarcoma10,11,12,13,14. In poorly differentiated chordomas, SMARCB1 inactivation is well established, yet its status in typical and chondroid subtypes remains incompletely characterized. Elucidating how partial or complete loss of SMARCB1 alters chromatin state, cell-cycle control, and lineage plasticity may clarify subtype-specific biology and therapeutic vulnerabilities.
Here, we analyze SMARCB1 genomic status, protein expression, and downstream pathways across typical and chondroid chordomas, and functionally dissect the consequences of SMARCB1 knockdown in chordoma cell models. By defining the molecular and phenotypic impact of SMARCB1 loss, we aim to identify actionable pathways and refine prognostic stratification for chordoma patients.
Results
Histological and survival characteristics of chordoma subtypes
Our cohort consisted of 42 chordoma patients, comprising 26 cases of typical chordoma and 16 cases of chondroid chordoma. Among typical chordoma patients, there were 18 males and 8 females, with a mean age of 50.85 ± 13.94 years. The chondroid chordoma group included 13 males and 3 females, with a mean age of 49.94 ± 13.15 years. Statistical analysis revealed no significant differences in age (P = 0.618) or sex distribution (P = 0.835) between the two subtypes.
Histological examination revealed distinct features. Typical chordoma (Fig. 1A,C) displayed a lobulated architecture with characteristic physaliphorous cells embedded in a myxoid stroma. These cells exhibited abundant vacuolated cytoplasm and small nuclei. In contrast, chondroid chordoma (Fig. 1B,D) showed areas of cartilaginous differentiation interspersed with typical chordoma features. The chondroid regions contained lacunae-like spaces populated by chondrocyte-like cells.
Histopathological features and survival analysis of typical and chondroid chordomas. (A–D) Representative hematoxylin and eosin (H&E) stained sections of typical (A, C) and chondroid (B, D) chordomas. (A, C) Typical chordoma showing a lobulated architecture with characteristic physaliphorous cells embedded in a myxoid stroma. (B, D) Chondroid chordoma displaying areas of cartilaginous differentiation interspersed with typical chordoma features. Scale bars: 250 µm (A, B) and 50 µm (C, D). (E, F) Kaplan–Meier survival curves comparing typical (blue) and chondroid (red) chordoma subtypes. (E) Progression-free survival (PFS) and (F) overall survival (OS) analyses. Dotted lines represent 95% confidence intervals. Median PFS: 120 months (typical) versus 109 months (chondroid), P = 0.605. Median OS: 120 months (typical) versus 118 months (chondroid), P = 0.652. n = 26 typical and 16 chondroid chordomas.
Survival analysis comparing typical and chondroid chordoma subtypes revealed subtle differences in patient outcomes. Kaplan–Meier curves for progression-free survival (PFS) (Fig. 1E) showed a median PFS of 120 months for typical chordoma versus 109 months for chondroid chordoma (P = 0.605). Similarly, overall survival (OS) data (Fig. 1F) indicated a median OS of 120 months for typical chordoma compared to 118 months for chondroid chordoma (P = 0.652). While these trends suggest a slight prognostic advantage for patients with typical chordoma, the differences did not reach statistical significance.
Genetic variations in chordoma samples
Genetic analysis of chordoma samples revealed several single nucleotide polymorphisms (SNPs) in the SMARCB1 gene. Sanger sequencing chromatograms (Fig. 2A) identified eight intronic SNPs: rs11090285 (c.-117C > T), rs183324088 (g.9699C > T), rs5751738 (g.21526G > T), rs5760032 (g.21578C > T), rs2070457 (g.34750C > A), rs5844569 (g.43510_43511dupAA), rs17003998 (g.51904G > A), and rs9612452 (g.35095G > A). Notably, no exonic mutations causing coding changes were detected. Further analysis revealed that none of these SNPs were flagged as clinically associated (minor allele frequency < 1%) in the SNP Database (dbSNP151).
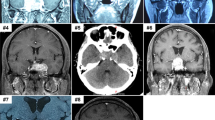
Genetic alterations in SMARCB1 in chordoma samples. (A) Representative Sanger sequencing chromatograms showing eight intronic single nucleotide polymorphisms (SNPs) identified in the SMARCB1 gene. Arrows indicate the position of each SNP. (B, C) Fluorescence in situ hybridization (FISH) analysis of SMARCB1 copy number. Nuclei are DAPI-stained. (B) Heterozygous loss of SMARCB1 in three typical chordoma cases. (C) Normal SMARCB1 copy number in chordoma cells, showing two red (SMARCB1 probe) and two green (CEN22q) signals per nucleus. Scale bars: 10 µm.
Fluorescence in situ hybridization (FISH) analysis provided insights into SMARCB1 copy number alterations in chordoma cells. Figure 2B shows predominantly normal copy numbers, with most nuclei displaying 2 red and 2 green signals. However, heterozygous loss of SMARCB1 was detected in three cases of typical chordoma (Fig. 2C), while no such loss was observed in chondroid chordomas. Tumors with SMARCB1 loss exhibited low expression of the SMARCB1 protein. Due to the limited number of cases with SMARCB1 loss, survival analysis for this specific subgroup was not feasible.
SMARCB1 expression correlates with patient outcomes and EMT markers
Immunohistochemical analysis revealed differential SMARCB1 expression patterns in chordoma samples, with significant implications for patient prognosis and tumor characteristics. Using a semiquantitative scoring method, SMARCB1 expression ranged from 0 to 12. Based on an average SMARCB1 immunoreactive score cutoff value of 8.2, tumor samples were categorized into two groups (Fig. 3A). The high SMARCB1 expression group (immunoreactive score ≥ 9) contained 23 samples, while the low SMARCB1 expression group (immunoreactive score ≤ 8) comprised 19 samples.
SMARCB1 expression correlates with patient outcomes and EMT markers in chordomas. (A) Representative immunohistochemical staining of SMARCB1 in typical and chondroid chordomas, showing high and low expression patterns. Scale bars: 50 µm. (B) Kaplan–Meier survival curves stratified by SMARCB1 expression levels. Left: Progression-free survival (PFS). Right: Overall survival (OS). High SMARCB1 expression (red) is associated with significantly better outcomes compared to low SMARCB1 expression (blue). Dotted lines represent 95% confidence intervals. Median PFS: 120 months (high) vs. 52 months (low), P = 0.006. Median OS: 134 months (high) vs. 109 months (low), P = 0.017. n = 23 high expression and 19 low expression samples. (C) Representative immunohistochemical staining of EMT markers (E-cadherin, N-cadherin, cytokeratin, and vimentin) in chordoma samples with high and low SMARCB1 expression. Scale bars: 50 µm.
Survival analysis demonstrated a strong correlation between SMARCB1 expression levels and patient outcomes. Kaplan–Meier curves for progression-free survival (Fig. 3B, left) showed significantly better outcomes for patients with high SMARCB1 expression (median PFS: 120 months vs. 52 months, P = 0.006). This trend was mirrored in the overall survival data (Fig. 3B, right), where high SMARCB1 expression was again associated with improved survival rates (median OS: 134 months vs. 109 months, P = 0.017).
Further immunohistochemical analysis revealed associations between SMARCB1 expression and key markers of epithelial-mesenchymal transition (EMT) (Fig. 3C). As the representative images show, samples with high SMARCB1 expression exhibited stronger staining for E-cadherin, N-cadherin, cytokeratin, and vimentin compared to samples with low SMARCB1 expression. This pattern suggests that SMARCB1 expression positively correlates with the expression of both epithelial (E-cadherin, cytokeratin) and mesenchymal (N-cadherin, vimentin) markers in chordoma tissues.
SMARCB1 knockdown promotes aggressive cellular behavior
Functional studies using SMARCB1 knockdown in chordoma cell lines revealed its role in regulating multiple aspects of tumor cell behavior. Western blot analysis confirmed the efficacy of SMARCB1 knockdown, with shSMARCB1 cells showing markedly reduced SMARCB1 protein levels compared to Wildtype and shNC (negative control) conditions (Fig. 4A).
SMARCB1 knockdown promotes aggressive cellular behavior in chordoma cells. (A) Western blot analysis of SMARCB1 expression in wildtype, shNC, and shSMARCB1 chordoma cells. SMARCB1 protein levels are substantially reduced in shSMARCB1 cells compared to controls. (B) CCK8 proliferation assay comparing shNC and shSMARCB1 cells over 72 h. shSMARCB1 cells show significantly increased proliferation from 24h onwards. (C) IncuCyte real-time cell proliferation assay over 100 h. shSMARCB1 cells demonstrate markedly accelerated growth compared to shNC controls. (D) Flow cytometry analysis of cell cycle distribution. Left: Representative DNA content histograms. Right: Quantification of cell cycle phases. shSMARCB1 cells exhibit an increased G0/G1 population and decreased G2/M population relative to shNC. (E) Transwell migration assay. Left: Representative images of migrated cells stained with crystal violet. Right: Quantification of migrated cell numbers. shSMARCB1 cells show significantly enhanced migratory capacity. (F) Transwell invasion assay. Left: Representative images of invaded cells stained with crystal violet. Right: Quantification of invaded cell numbers. shSMARCB1 cells display markedly increased invasive potential. (G) Wound healing assay. Left: Representative phase-contrast images of wound closure at 0-, 24-, 48-, and 72-h post-scratch. Right: Quantification of wound area over time. shSMARCB1 cells exhibit wound closure at a rate comparable to shNC controls. (B–G) Data are presented as mean ± s.d. n.s., not significant; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001 (unpaired two-tailed Student’s t-test).
CCK8 proliferation assays (Fig. 4B) demonstrated significantly increased cell proliferation in shSMARCB1 cells compared to shNC controls. This effect became particularly pronounced at 48h and 72h timepoints (P < 0.0001), indicating that SMARCB1 knockdown enhances chordoma cell proliferation. The IncuCyte real-time cell proliferation assay (Fig. 4C) further corroborated these findings, showing a consistently higher proliferation rate in shSMARCB1 cells over a 50-h period.
Flow cytometry-based cell cycle analysis (Fig. 4D) revealed substantial alterations in cell cycle distribution following SMARCB1 knockdown. In shNC cells, the distribution was 60.61% in G0/G1, 20.89% in S, and 18.23% in G2/M phases. In contrast, shSMARCB1 cells showed a marked shift with 41.44% in G0/G1, 20.60% in S, and 38.02% in G2/M phases. This shift indicates a significant decrease in G0/G1 phase cells (P < 0.01) and a concomitant increase in G2/M phase cells (P < 0.001), suggesting accelerated cell cycle progression in the absence of SMARCB1.
Migration and invasion assays (Fig. 4E,F) revealed dramatically enhanced cellular motility and invasiveness following SMARCB1 knockdown. Quantification showed an approximately fivefold increase in migration (P < 0.0001) and a 2.5-fold increase in invasion capacity (P < 0.0001) for shSMARCB1 cells compared to shNC controls.
Wound healing assays (Fig. 4G) showed only a slight difference in migration between shSMARCB1 and shNC cells. At 24, 48, and 72 h, shSMARCB1 cells exhibited marginally faster wound closure compared to shNC cells, but the difference was modest and statistically insignificant.
Transcriptome analysis reveals SMARCB1-associated pathways
Comprehensive transcriptome analysis uncovered the broader molecular landscape associated with SMARCB1 expression in chordoma. Principal Component Analysis (PCA) (Fig. 5A) demonstrated clear separation between SMARCB1-high (negative) and SMARCB1-low (positive) samples, indicating distinct gene expression profiles associated with SMARCB1 status. The first principal component (PC1) explained 72.7% of the variance, highlighting the substantial impact of SMARCB1 expression on overall gene expression patterns.
Transcriptome analysis reveals SMARCB1-associated pathways in chordoma. (A) Principal Component Analysis (PCA) plot showing distinct clustering of SMARCB1-high (negative, red) and SMARCB1-low (positive, blue) chordoma samples. PC1 explains 72.7% of the total variance. (B) Volcano plot of differentially expressed genes between SMARCB1-high and SMARCB1-low samples. Blue dots represent significantly down-regulated genes, red dots represent significantly uP-regulated genes (log2 fold change cutoff: 1, P-value cutoff: 0.05). (C) Gene Set Enrichment Analysis (GSEA) of hallmark gene sets, showing significant enrichment of MYC targets, E2F targets, and G2M checkpoint pathways in SMARCB1-low samples. NES: Normalized Enrichment Score. (D) GSEA of Gene Ontology (GO) Biological Process terms, highlighting enrichment of cell cycle-related processes and negative enrichment of cellular adhesion processes in SMARCB1-low samples. (E) GSEA of KEGG pathways, demonstrating enrichment of DNA replication and cell cycle pathways, and negative enrichment of tight junction and adherens junction pathways in SMARCB1-low samples. (C–E) The running enrichment score for each gene set is shown at the top of each panel, and the vertical bars below represent individual genes in the gene set, colored by their correlation with the SMARCB1-low phenotype (red: positive, blue: negative).
Differential gene expression analysis, visualized in the volcano plot (Fig. 5B), identified several significantly modulated genes. Notable down-regulated genes in SMARCB1-low samples included SLPI (encoding secretory leukocyte protease inhibitor, involved in immune response), LBH (transcriptional regulator implicated in development and cell cycle control), LOXL2 (lysyl oxidase-like 2, involved in extracellular matrix remodeling and metastasis), FGM1 (phosphate metabolism regulator), and KRT4 (keratin 4, an epithelial structural protein). Conversely, uP-regulated genes, though less pronounced, included MIR1144, MIRLET7I, and MIR6729, all of which are microRNAs that may play roles in post-transcriptional regulation of gene expression.
Gene Set Enrichment Analysis (GSEA) revealed significant enrichment of key cellular pathways and processes associated with SMARCB1 status. Hallmark gene set analysis (Fig. 5C) showed strong enrichment of MYC targets V1 (NES = 3.27, P < 0.001) and V2 (NES = 3.00, P < 0.001), indicating activation of the MYC oncogenic pathway, which regulates cell growth and proliferation. E2F targets (NES = 2.98, P < 0.001) and G2M checkpoint (NES = 2.04, P < 0.001) gene sets were also enriched in SMARCB1-low samples, suggesting enhanced cell cycle progression and division.
Gene Ontology (GO) Biological Process analysis (Fig. 5D) highlighted enrichment of DNA replication (NES = 2.49, P < 0.001), cell cycle G2/M transition (NES = 1.39, P = 0.01), and positive regulation of cell cycle process (NES = 1.35, P = 0.01) in SMARCB1-low samples. Conversely, processes related to cellular organization and adhesion showed negative enrichment, including tight junction organization (NES = − 1.67, P = 0), regulation of gap junction assembly (NES = − 1.88, P = 0), focal adhesion assembly (NES = − 2.02, P < 0.001), and regulation of cell–cell adhesion (NES = − 2.31, P < 0.001).
KEGG pathway analysis (Fig. 5E) further emphasized the enrichment of DNA replication (NES = 2.54, P < 0.001) and cell cycle (NES = 1.75, P < 0.001) pathways in SMARCB1-low samples. Additionally, tight junction (NES = − 1.94, P < 0.001) and adherens junction (NES = − 2.00, P < 0.001) pathways showed significant negative enrichment, aligning with the GO analysis results and supporting the role of SMARCB1 in maintaining cellular adhesion and organization.
Discussion
Our investigation into the role of SMARCB1 in chordoma pathogenesis reveals a complex interplay between genetic alterations, epigenetic regulation, and cellular behavior, with implications for patient outcomes and potential therapeutic strategies. This study not only corroborates previous findings on SMARCB1’s tumor suppressor function but also uncovers novel insights specific to chordoma biology, particularly in typical and chondroid subtypes.
SMARCB1, a core subunit protein in the ATP-dependent SWI/SNF chromatin remodeling complex, has been recognized as a potent tumor suppressor. The significance of SMARCB1 in tumor biology was first highlighted in 1990 when deficiency of the SMARCB1 gene was identified in three cases of atypical teratoid/rhabdoid tumors15. Since then, various genetic alterations, including somatic mutations and deletions, as well as aberrant expression of the SMARCB1 protein, have been identified in a wide range of tumors16,17,18,19. Kohashi and colleagues have categorized SMARCB1-deficient tumors into three groups: (1) complete loss of SMARCB1 expression, commonly seen in malignant rhabdoid tumors, epithelioid sarcoma, pancreatic undifferentiated rhabdoid carcinomas, and carcinomas of the sinonasal or gastrointestinal tract; (2) mosaic patterns of SMARCB1 protein expression, usually affecting schwannomatosis, gastrointestinal stromal tumors, and ossifying fibromyxoid tumors; and (3) reduced SMARCB1 expression, which was identified in synovial sarcomas14. Interestingly, while SMARCB1 loss has been well-established in other tumor types such as atypical teratoid/rhabdoid tumors (AT/RTs) and epithelioid sarcomas, the mechanisms of SMARCB1 inactivation in chordomas appear to be distinct. Unlike AT/RTs, where biallelic inactivating mutations are common, SMARCB1 loss in chordomas has been predominantly associated with epigenetic silencing or genomic deletions rather than point mutations20. This suggests that different tumor types may employ various mechanisms to inactivate SMARCB1, highlighting the complexity of SMARCB1-related oncogenesis.
In 2010, Mobley et al. first reported loss of SMARCB1 expression in poorly differentiated chordomas. Their study, which included 4 poorly differentiated chordomas, identified deletion of SMARCB1 in 3 of them using FISH probes. Importantly, sequencing of all nine SMARCB1 exons in all four cases revealed no point mutations10.
In 2014, Yadav et al. observed loss of SMARCB1 in 4 pediatric chordomas with atypical histomorphological features, again finding no point mutations10. In the same year, Choy et al. performed a focused genetic analysis using matrix-assisted laser desorption/ionization-time of flight mass spectrometry. They found deletion at the SMARCB1 locus in 3 of 4 chordoma samples and identified a point mutation (R40*) in 2 samples, although the pathological subtype of these chordomas was not specified21,22. Also in 2014, Renard et al. reported two cases of undifferentiated chordoma with loss of the SMARCB1 gene, while Chavez et al. described a 2-year-old girl with anaplastic chordoma showing loss of SMARCB1 expression on IHC staining23,24.
In 2016, Hasselblatt et al. conducted a comprehensive analysis of 7 poorly differentiated chordomas, performing IHC, FISH, and SMARCB1 sequencing. All of these tumors showed loss of SMARCB1 expression, but no point mutations were identified11. In 2017, Cha et al. reported two additional cases of poorly differentiated chordoma with loss of SMARCB1 expression13. In the same year, Antonelli et al. analyzed 8 pediatric chordomas (7 typical and 1 poorly differentiated) using IHC and SMARCB1 sequencing. They found loss of SMARCB1 expression in 4 of the 8 cases25. Genetic analysis identified missense mutations (c.154A > G and c.682A > G) in 2 cases and a nonsense mutation (c.364G > T) in the poorly differentiated chordoma12,25. The largest series to date was reported by Shih et al. in 2018, describing 19 cases of poorly differentiated chordomas with SMARCB1 loss26.
Our study builds upon this growing body of literature, focusing on typical and chondroid chordomas, which have been less extensively studied in terms of SMARCB1 alterations. We found that typical chordomas and chondroid chordomas exhibited similar prognoses, consistent with previous findings in intracranial chordomas27. This suggests that chondroid differentiation may not significantly affect the biological behavior of chordomas.
Our genetic analysis revealed 8 SNPs in the introns of SMARCB1, but importantly, we found no exonic mutations that would cause coding changes. This is consistent with most previous studies on chordomas, suggesting that mutational alterations in the SMARCB1 gene may not be common in chordomas, especially in chondroid subtypes10,11,21. The few reported missense/nonsense mutations in the SMARCB1 gene in chordomas appear to be the exception rather than the rule12,22. The frequency of SMARCB1 loss in our study (3/42; 7.1%) was notably lower than that reported in poorly differentiated chordomas10,11,13,26. This discrepancy suggests that SMARCB1 loss may be associated with the degree of differentiation in chordomas. However, while high SMARCB1 expression correlates with better prognosis, the absence of coding mutations coupled with the presence of intronic SNPs suggests a more nuanced regulatory mechanism at play. This finding aligns with emerging concepts of “shallow” or “partial” loss of function in cancer genes, where subtle modulations in expression levels, rather than complete loss, drive oncogenesis28.
The heterozygous loss of SMARCB1 observed exclusively in typical chordomas, but not in chondroid variants, is particularly intriguing. This subtype-specific alteration hints at divergent evolutionary paths in chordoma development, possibly reflecting the cell of origin or the tumor microenvironment’s influence. It’s conceivable that chondroid chordomas maintain SMARCB1 expression as a vestige of their cartilaginous differentiation, whereas typical chordomas might benefit from SMARCB1 reduction to enhance plasticity and invasiveness. This hypothesis warrants further investigation through single-cell sequencing and lineage tracing experiments.
Our functional studies revealed another intriguing pattern of SMARCB1's influence on chordoma cell behavior. While SMARCB1 knockdown significantly enhanced cell proliferation, as evidenced by CCK8 and IncuCyte assays, its effects on cell migration were less pronounced, particularly in wound healing assays. This discrepancy suggests that SMARCB1 may primarily regulate proliferative capacity rather than migratory potential in chordoma cells.
The observed increase in proliferation can be attributed, at least in part, to the alterations in cell cycle distribution following SMARCB1 knockdown. Our flow cytometry analysis demonstrated a marked shift from G0/G1 to G2/M phase in shSMARCB1 cells, indicating accelerated cell cycle progression. This finding aligns with the known role of SMARCB1 as a component of the SWI/SNF chromatin remodeling complex, which has been implicated in maintaining cell identity and regulating lineage plasticity, and is crucial for cell cycle regulation29. The loss of SMARCB1 may lead to dysregulation of key cell cycle checkpoint genes, particularly those involved in the G2/M transition. This cell cycle perturbation could explain the enhanced proliferative capacity observed in our functional assays, highlighting SMARCB1's role as an important regulator of cell division in chordoma cells. Future studies incorporating rescue experiments—such as re-expression of SMARCB1 in knockdown models—will be important to confirm the specificity and reversibility of these phenotypes.
Also noteworthy is the strong enrichment of MYC targets and E2F targets in SMARCB1-low samples. This suggests that SMARCB1 loss may drive chordoma progression in part through activation of these key oncogenic pathways. The enrichment of DNA replication and cell cycle-related processes further supports the pro-proliferative effect of SMARCB1 loss observed in our functional studies. However, the relationship between SMARCB1 and these oncogenic pathways may be more complex than simple repression. Recent studies have shown that SMARCB1 loss can lead to both activation and repression of target genes, depending on the cellular context and the specific genomic loci involved. In chordoma, SMARCB1 might act as a “rheostat” for MYC and E2F activity, fine-tuning their output to maintain cellular homeostasis. Its loss could disrupt this balance, leading to unopposed activation of proliferative programs.
The downregulation of SLPI in SMARCB1-low samples is particularly noteworthy. Beyond its role in immune modulation, SLPI has long been shown to inhibit NF-κB activity30. Given that NF-κB signaling is a known driver of chordoma growth, SMARCB1 loss might promote tumor progression not only through direct effects on proliferation and EMT but also by alleviating SLPI-mediated NF-κB inhibition31. This creates a potential feedback loop where SMARCB1 loss enhances NF-κB signaling, further driving SMARCB1 downregulation. Whether SMARCB1-deficient chordomas exhibit increased sensitivity to immune checkpoint blockade, such as anti-PD-1 therapy, remains to be determined and represents a promising avenue for future investigation.
The effects of SMARCB1 modulation on chordoma biology present both challenges and opportunities for therapeutic intervention. Direct restoration of SMARCB1 function remains elusive, necessitating alternative approaches. One promising avenue is the exploitation of synthetic lethality. The concept of “SWI/SNF synthetic lethality” has gained traction in other SMARCB1-deficient cancers32. In chordoma, targeting residual SWI/SNF complexes or their antagonists (e.g., PRC2 complex) could selectively kill SMARCB1-deficient cells. Our transcriptome data suggesting activation of MYC and E2F pathways provides a rationale for exploring inhibitors of these networks, such as BET inhibitors or CDK4/6 inhibitors, particularly in SMARCB1-low tumors.
The potential influence of SMARCB1 on the tumor immune microenvironment, as hinted by SLPI downregulation, opens up intriguing possibilities for immunotherapy. Recent studies have shown that SWI/SNF-deficient cancers often harbor increased tumor mutational burden and neoantigen load33. While chordomas are generally considered immunologically “cold” tumors, SMARCB1 loss might create a more immunogenic phenotype. Combining immune checkpoint inhibitors with epigenetic modulators to enhance antigen presentation could be a promising strategy, especially in SMARCB1-low chordomas. This is also important, because role of SMARCB1 in chordomas also seems to differ from its function in others, like rhabdoid tumors (RTs) and epithelioid sarcomas. In these tumors, re-expression of SMARCB1 often leads to rapid growth arrest and senescence, mediated by p16INK4A induction. In contrast, studies have shown that most chordomas lack p16INK4A expression due to genetic inactivation34. This difference may explain why SMARCB1 re-expression alone might not be sufficient to halt chordoma growth and suggests that additional therapeutic strategies may be necessary for effective treatment.
While our study provides valuable insights into the role of SMARCB1 in chordomas, several limitations should be addressed in future research. First, although our cohort size is significant for a rare tumor like chordoma, larger studies are needed to validate our findings and further explore the prognostic value of SMARCB1 expression. Second, while we demonstrated the functional impact of SMARCB1 knockdown in vitro, in vivo studies are needed to fully elucidate the role of SMARCB1 in tumor initiation and progression. Development of animal models that recapitulate SMARCB1 loss in chordomas would be invaluable for this purpose. Third, our study focused primarily on SMARCB1 expression levels, but future research should explore the mechanisms regulating SMARCB1 in chordomas. Epigenetic profiling (DNA methylation, histone modifications, chromatin accessibility) is crucial to understand the regulatory mechanisms governing SMARCB1 expression in chordoma. Applying single-cell multi-omics approaches, including RNA-seq, ATAC-seq, and spatial transcriptomics, to chordoma samples could reveal the heterogeneity of SMARCB1 expression within tumors and its relationship to cellular states and spatial organization. The strong prognostic value of SMARCB1 expression suggests its potential as a biomarker. Developing liquid biopsy assays to detect SMARCB1 alterations (e.g., circulating tumor DNA methylation) could enable non-invasive monitoring of disease progression and treatment response. Investigations into potential interactions with other members of the SWI/SNF complex may also prove useful. Lastly, while our transcriptome analysis revealed several SMARCB1-associated pathways, functional validation of these pathways and their potential as therapeutic targets is needed. Preclinical studies evaluating the efficacy of targeting these pathways in SMARCB1-deficient chordomas could pave the way for new treatment strategies.
Materials and methods
Patients and tumor specimens
This study was conducted with approval from the Institutional Review Board of Peking University Third Hospital. A total of 26 patients with typical chordoma and 16 patients with chondroid chordoma were enrolled. Clinical profiles and tumor specimens were collected from all participants after obtaining written informed consent.
Cell culture
MUG-Chor1 (ATCC CRL-3219) cells were purchased from ATCC (Manassas, VA, USA). The cells were cultured and maintained in a 4:1 ratio combination of Iscove’s Modified Dulbecco’s Medium (Invitrogen, Gibco, UK) and RPMI-1640 Medium (Invitrogen, Gibco, UK) supplemented with 10% Fetal Bovine Serum (Vazyme, CN), 1% GlutaMAX (Invitrogen, Gibco, UK), and 100 μg/ml Normocin (InvivoGen, FR). Cells were cultured on tissue culture plates and flasks coated with Cell coating working solution (Cellverse, CN). The cells were incubated in a humidified incubator at 37 °C and under 5% CO2 conditions.
Lentivirus packaging and infection
RNAi targeting SMARCB1 was designed using the Sigma Mission system. The si-SMARCB1 sequence was 5′-ACGGAGCATCTCAGAAGATTG-3′, and the NC sequence was 5′-GCGCGATAGCGCTAATAATTT-3′. Oligo DNA was synthesized (Tsingke, CN), and double-stranded DNA was prepared through annealing. To produce PLVX-shSMARCB1 and PLVX-shNC, the DNA was inserted into the PLVX-shRNA vector using the restriction enzymes BamHI and EcoRI. Both vectors were then transformed into E. coli DH5α, and positive clones were picked to expand the culture. The plasmids were extracted using the FastPure Plasmid Mini Kit (Vazyme, CN) and sent for Sanger sequencing (Tsingke,CN). Plasmids with correct sequences were then selected for viral packaging. The PLVX-shNC/shSMARCB1, psPAX2, and pMD2.G lentiviral vectors were transfected into 293T cells using Transfec reagent (Lablead, CN) in a 4:3:1 ratio for lentiviral packaging. Lentiviruses were purified using the Universal Virus Concentration Kit (Beyotime, CN) and stored in a -80°C freezer until use.
MUG-Chor1 cells were seeded into pre-coated 6-well plates at a density of 4 × 105 cells per well. After the cells adhered, the medium was aspirated, and the lentivirus was added to complete medium mixed with 10 μg/ml Polybrene (Yeasen, CN) for infection. After 72 h, the cells were screened using complete medium containing puromycin, and the culture was maintained by halving the concentration of puromycin after the control cells had been killed.
Cell proliferation
Cell proliferation was evaluated using the IncuCyte S3 platform and the CCK-8 assay. MUG-Chor1 cells were seeded at a density of 5000 cells per well in pre-coated 96-well plates. After cell attachment, phase contrast images were captured using the IncuCyte S3 platform (Sartorius, GRE). Four sets of phase contrast images were taken from distinct regions within each well at 3-h intervals using a 10X objective. The IncuCyte S3 image analysis software was configured to detect cell edges and calculate confluence as a percentage. Additionally, cell viability was assessed using the CCK-8 assay. MUG-Chor1 cells were seeded at 5000 cells per well in pre-coated 96-well plates. Every 24 h, the medium was aspirated and replaced with fresh medium containing the CCK-8 reagent (Vazyme, CN). After incubating for 3 h, cell absorbance at 450 nm was measured using a microplate reader.
Wound healing
MUG-Chor1 cells were seeded at a density of 6 × 105 cells per well in pre-coated 6-well plates. Once the cells were attached and reached over 90% confluence, a sterile 200 μl pipette tip was used to create a scratch in the cell monolayer. After washing the wells three times with PBS, the medium was replaced with serum-free medium, and the cells were incubated. Images of the scratch area were captured at 0 h, and additional images were taken every 24 h to monitor the rate of scratch closure.
Transwell assay
Cell migration was evaluated using 8 μm 24-well chambers (Corning, USA). The cell suspension containing 5 × 104 cells (without FBS) was placed in the top chambers, and DMEM with 10% FBS was added to the bottom chambers. Following 48 h of incubation at 37 °C with 5% CO2, the migrated cells were fixed with 4% paraformaldehyde for 20 min and stained with 0.1% crystal violet for 20 min. The stained cells were counted under a microscope (Leica, GRE).
For cell invasion assessment, the same chambers were used as in the migration assay, but they were pre-coated with Matrigel (Lablead, CN). The cell suspension containing 1 × 105 cells was used, and all other procedures were performed as described for the migration assay.
Flow cytometry
Flow cytometry analysis was performed to detect cell cycle distribution. Briefly, MUG-Chor1 cells were seeded into pre-coated 60 mm culture dishes at a density of 1 × 106 cells per dish. When the cells were > 80% confluent, they were digested with 0.25% trypsin, centrifuged to obtain the cellular precipitate, and the precipitate was resuspended with 300 μl of pre-cooled PBS. The suspension was slowly dripped into 700 μl of pre-cooled anhydrous ethanol and fixed at 4 °C overnight. Next, cells were centrifuged for 5 min at 3000 rpm. The pellet was resuspended in 1 mL of PBS and centrifuged again at 3000 rpm for 5 min. This step was repeated twice. Finally, the pellet was resuspended in 0.5 mL of PI staining solution (KeyGen, CN) and kept in the dark at 37 °C for 60 min. Samples were analyzed using a CytoFLEX S flow cytometer (Beckman, USA). The percentage of cells in G1, S, and G2-M phases were counted using Modfit and compared using Prism 9.3.
Western blot
MUG-Chor1 cells were lysed with RIPA buffer (Beyotime, CN) containing protease inhibitor (Applygen, CN). Following protein quantification using Bradford kits (Lablead, CN), 20 μg of protein were separated on 10% SDS gels and transferred to PVDF membranes (0.45 μm; Merck Millipore, USA). Membranes were blocked at room temperature with 5% skim milk for 1 h. The membranes were incubated with primary antibodies at 4 °C overnight, including anti-SMARCB1 antibody (Proteintech, USA) and anti-β-ACTIN antibody (Proteintech, USA). After incubation with HRP-conjugated secondary antibodies (Beyotime, CN) for 1 h at room temperature, proteins were visualized using the ECL imaging system (Tanon, China).
Data collection and preprocessing
GSE217999 was downloaded from the Gene Expression Omnibus (GEO) database34. The GEO data was generated using the Illumina HiSeq 4000 platform. We obtained the raw count data and annotated the probes according to Human.GRCh38.p13, as well as performed TPM conversion. Data for UM-Chor1 and CH-22 were extracted from the TPM matrix for subsequent analysis. The ggbiplot package was used to create a PCA plot to visualize the data distribution.
Differential expression gene analysis
The R package “limma” was used to estimate differentially expressed genes35. Genes with P-value < 0.05 and log2 fold change > 1 found by limma were identified as differentially expressed. Volcano plots of DEGs were visualized using the R package “EnhancedVolcano”36. In the volcano plot, DEGs with log2Foldchange < -1 and P-value < 0.05 were considered downregulated, while those with log2Foldchange > 1 and P-value < 0.05 were considered upregulated. The top 5 uP- and down-regulated genes are labeled in the figure.
Gene set enrichment analysis
To explore the potential signaling pathways and biological functions between SMARCB1 positive and negative groups, we performed gene set enrichment analysis (GSEA) based on MSigDB collections using the R package “clusterProfiler”37. The different transcriptional profiles were identified and sorted by log2 fold change using limma. GSEA was then performed on these transcriptional profiles, and enrichment was assessed using normalized enrichment score (NES) as a metric of enrichment. False discovery rate (FDR) < 0.25 and adjusted P-value < 0.05 were considered statistically significant.
Immunohistochemical (IHC) staining
IHC staining was performed on 4-μm-thick formalin-fixed paraffin-embedded tissue sections using antibodies directed against SMARCB1 (monoclonal EPR20189, 1:500, Abcam, Cambridge, MA, USA), E-cadherin (monoclonal 4A2, 1:1000, Abcam), cytokeratin (polyclonal, 1:200, Abcam), N-cadherin (monoclonal 8C11, 1:1000, Abcam), and vimentin (monoclonal RV203, 1:200, Abcam). IHC results were scored semiquantitatively according to the methods proposed by Sinicrope et al. [15]. The percentage of positive cells was scored as 0 (0–4% of tumor cells stained), 1 (5–25%), 2 (26–50%), 3 (51–75%), or 4 (> 75%). Immunoreactivity intensity was graded as 0 (no expression), 1 (weak expression), 2 (moderate expression), or 3 (intense expression). The final score, ranging from 0 to 12, was calculated by multiplying these two parameters.
To ensure consistency and reduce subjectivity in immunohistochemical interpretation, two authors (WL and SL), both with prior experience in IHC analysis, independently evaluated all specimens. Their assessments were concordant in all but one case, which was reviewed and resolved by a third author (CY) to reach consensus.
Gene sequence analysis
Genomic DNA was extracted from frozen tissue samples using a QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) and from paraffin-embedded samples using a GeneRead DNA FFPE Kit (Qiagen) according to the manufacturer’s instructions. Primers were designed using OLIGO Primer Analysis Software (version 7, Molecular Biology Insights, Cascade, CO, USA) and synthesized by Sangon Biological Technology (Shanghai, China). All annotated exons and adjacent introns of the SMARCB1 (NM_003073) gene were amplified and sequenced.
Fluorescence in situ hybridization (FISH)
FISH was performed on formalin-fixed, paraffin-embedded sections using SMARCB1/CEN22q probes (Abnova, Taipei, Taiwan). Deparaffinization, dehydration, pretreatment, protease treatment, and hybridization were conducted according to the manufacturer’s protocol. For each specimen, 200 interphase nuclei were analyzed. Heterozygous deletion was defined as greater than 30% of nuclei showing signal loss10.
Knockdown of SMARCB1 in chordoma cell lines
Human typical chordoma cell lines U-CH1 (American Type Culture Collection [ATCC] CRL-3217) and MUG-Chor1 (ATCC CRL-3219) were purchased from ATCC (Manassas, VA, USA) and cultured with the recommended media and under the recommended conditions. SMARCB1 knockdown was achieved by transfecting shRNA targeting SMARCB1 into chordoma cells using Lipofectamine 2000 (Invitrogen, CA, USA). Western blotting was performed to assess the expression of SMARCB1.
After 48 h of incubation, cell proliferation was evaluated using a Cell Proliferation/Cytotoxicity Assay Kit (Cell Counting Kit-8, Dojindo Laboratories, Kumamoto, Japan), measuring optical density (OD) at 450 nm. Cell apoptosis was assessed by flow cytometry using an Annexin V-fluorescein isothiocyanate (FITC)/propidium iodide (PI) Apoptosis Detection Kit (Dojindo Laboratories). Cell cycle analysis was performed using a PI/RNase Staining Cell Cycle Assay Kit (Dojindo Laboratories). All experiments were conducted in triplicate.
Statistical analysis
Statistical analyses were performed using SPSS software 25.0 (IBM, Armonk, NY, USA) and GraphPad Prism 8.0 (GraphPad, La Jolla, CA, USA). Progression-free survival (PFS) was defined as the interval between the first operation and the date of tumor progression or tumor-related death. Overall survival (OS) was defined as the interval between the first operation and the date of death from any cause. PFS and OS were estimated using the Kaplan–Meier method and compared using the log-rank test. Semiquantitative expression levels of SMARCB1 were analyzed using the Mann–Whitney U test and Spearman correlation analysis. Independent data from cell assays were analyzed using unpaired Student’s t-tests.
Conclusions
Our study reveals the genetic characteristics and expression patterns of SMARCB1 in typical and chondroid chordomas, where heterozygous loss of SMARCB1 is relatively uncommon. However, SMARCB1 expression is strongly linked to patient survival and plays a strong role in regulating aggressive cellular behavior. Transcriptome analysis identified key SMARCB1-associated pathways, particularly the activation of MYC and E2F targets. The predominance of epigenetic silencing over mutations in SMARCB1 inactivation underscores the complexity of chordoma biology. These insights lay the groundwork for the development of SMARCB1-based prognostic tools and personalized therapies, with promising prospects for synthetic lethality approaches and immunotherapies targeting SMARCB1-deficient tumors.
Data availability
The data reported in this paper have been deposited in the GenBase38 in National Genomics Data Center39, Beijing Institute of Genomics, Chinese Academy of Sciences/China National Center for Bioinformation, under accession number C_AA103182.1 to C_AA103183.1 that is publicly accessible at https://ngdc.cncb.ac.cn/genbase.
References
Kim, J. W. et al. Maximum surgical resection and adjuvant intensity-modulated radiotherapy with simultaneous integrated boost for skull base chordoma. Acta Neurochir. (Wien) 159(10), 1825–1834. https://doi.org/10.1007/s00701-016-2909-y (2017).
Meng, T. et al. Molecular targeted therapy in the treatment of chordoma: A systematic review. Front. Oncol. 9, 30. https://doi.org/10.3389/fonc.2019.00030 (2019).
Gulluoglu, S., Turksoy, O., Kuskucu, A., Ture, U. & Bayrak, O. F. The molecular aspects of chordoma. Neurosurg. Rev. 39(2), 185–196 (2016).
Naka, T. et al. Expression of c-MET, low-molecular-weight cytokeratin, matrix metalloproteinases-1 and-2 in spinal chordoma. Histopathology 54(5), 607–613 (2009).
Choi, P. J., Oskouian, R. J. & Tubbs, R. S. The current understanding of MicroRNA’s therapeutic, diagnostic, and prognostic role in chordomas: A review of the literature. Cureus https://doi.org/10.7759/cureus.3772 (2018).
Lee, I. J., Lee, R. J. & Fahim, D. K. Prognostic factors and survival outcome in patients with chordoma in the United States: a population-based analysis. World Neurosurg. 104, 346–355. https://doi.org/10.1016/j.wneu.2017.04.118 (2017).
Dutta, S. W. et al. Particles versus photons for the treatment of chordoma. Cochrane Database Syst. Rev. 12, CD013224 (2018).
Akiyama, T. et al. Analysis of the infiltrative features of chordoma: The relationship between micro-skip metastasis and postoperative outcomes. Ann. Surg. Oncol. 25(4), 912–919 (2018).
Allard, F. D., Bell, D. & Stelow, E. B. Cytopathologic features of SMARCB1 (INI-1)-deficient sinonasal carcinoma. Cancer Cytopathol. 126(8), 567–574 (2018).
Mobley, B. C. et al. Loss of SMARCB1/INI1 expression in poorly differentiated chordomas. Acta Neuropathol. 120(6), 745–753. https://doi.org/10.1007/s00401-010-0767-x (2010).
Hasselblatt, M. et al. Poorly differentiated chordoma with SMARCB1/INI1 loss: A distinct molecular entity with dismal prognosis. Acta Neuropathol. 132(1), 149–151. https://doi.org/10.1007/s00401-016-1574-9 (2016).
Antonelli, M. et al. SMARCB1/INI1 involvement in pediatric chordoma: A mutational and immunohistochemical analysis. Am. J. Surg. Pathol. 41(1), 56–61. https://doi.org/10.1097/PAS.0000000000000741 (2017).
Cha, Y. J. et al. Poorly differentiated chordoma with loss of SMARCB1/INI1 expression in pediatric patients: A report of two cases and review of the literature. Neuropathology 38(1), 47–53. https://doi.org/10.1111/neup.12407 (2018).
Kohashi, K. & Oda, Y. Oncogenic roles of SMARCB1/INI1 and its deficient tumors. Cancer Sci. 108(4), 547–552. https://doi.org/10.1111/cas.13173 (2017).
Biegel, J. A., Rorke, L. B., Packer, R. J. & Emanuel, B. S. Monosomy 22 in rhabdoid or atypical tumors of the brain. J. Neurosurg. 73(5), 710–714. https://doi.org/10.3171/jns.1990.73.5.0710 (1990).
Versteege, I. et al. Truncating mutations of hSNF5/INI1 in aggressive paediatric cancer. Nature 394(6689), 203–206. https://doi.org/10.1038/28212 (1998).
Wilson, B. G. & Roberts, C. W. SWI/SNF nucleosome remodellers and cancer. Nat. Rev. Cancer 11(7), 481–492. https://doi.org/10.1038/nrc3068 (2011).
Margol, A. S. & Judkins, A. R. Pathology and diagnosis of SMARCB1-deficient tumors. Cancer Genet. 207(9), 358–364 (2014).
Zhang, L., Fan, S., Liu, H. & Huang, C. Targeting SMARCAL1 as a novel strategy for cancer therapy. Biochem. Biophys. Res. Commun. 427(2), 232–235 (2012).
Malgulwar, P. B. et al. Downregulation of SMARCB1/INI1 expression in pediatric chordomas correlates with upregulation of miR-671–5p and miR-193a-5p expressions. Brain Tumor Pathol. 34(4), 155–159. https://doi.org/10.1007/s10014-017-0295-7 (2017).
Yadav, R. et al. Prognostic value of MIB-1, p53, epidermal growth factor receptor, and INI1 in childhood chordomas. Neuro Oncol. 16(3), 372–381. https://doi.org/10.1093/neuonc/not228 (2014).
Choy, E. et al. Genotyping cancer-associated genes in chordoma identifies mutations in oncogenes and areas of chromosomal loss involving CDKN2A, PTEN, and SMARCB1. PLoS ONE 9(7), e101283. https://doi.org/10.1371/journal.pone.0101283 (2014).
Renard, C., Pissaloux, D., Decouvelaere, A. V., Bourdeaut, F. & Ranchère, D. Non-rhabdoid pediatric SMARCB1-deficient tumors: Overlap between chordomas and malignant rhabdoid tumors?. Cancer Genet. 207(9), 384–389 (2014).
Chavez, J. A., Nasir, D. U., Memon, A. & Perry, A. Anaplastic chordoma with loss of INI1 and brachyury expression in a 2-year-old girl. Clin. Neuropathol. 33(6), 418–420 (2014).
Antonelli, M. et al. SMARCB1/INI1 involvement in pediatric chordoma: A mutational and immunohistochemical analysis. Am. J. Surg. Pathol. 41(1), 56–61 (2017).
Shih, A. R. et al. Clinicopathologic characteristics of poorly differentiated chordoma. Mod. Pathol. 31(8), 1237 (2018).
Forsyth, P. A. et al. Intracranial chordomas: A clinicopathological and prognostic study of 51 cases. J. Neurosurg. 78(5), 741–747. https://doi.org/10.3171/jns.1993.78.5.0741 (1993).
Fito-Lopez, B., Salvadores, M., Alvarez, M. M. & Supek, F. Prevalence, causes and impact of TP53-loss phenocopying events in human tumors. BMC Biol. 21(1), 92. https://doi.org/10.1186/s12915-023-01595-1 (2023).
Mittal, P. & Roberts, C. W. M. The SWI/SNF complex in cancer: Biology, biomarkers and therapy. Nat. Rev. Clin. Oncol. 17(7), 435–448. https://doi.org/10.1038/s41571-020-0357-3 (2020).
Taggart, C. C. et al. Secretory leucoprotease inhibitor binds to NF-kappaB binding sites in monocytes and inhibits p65 binding. J. Exp. Med. 202(12), 1659–1668. https://doi.org/10.1084/jem.20050768 (2005).
Trucco, M. M. et al. A novel chordoma xenograft allows in vivo drug testing and reveals the importance of NF-κB signaling in chordoma biology. PLoS ONE 8(11), e79950. https://doi.org/10.1371/journal.pone.0079950 (2013).
Sasaki, M. & Ogiwara, H. Synthetic lethal therapy based on targeting the vulnerability of SWI/SNF chromatin remodeling complex-deficient cancers. Cancer Sci. 111(3), 774–782. https://doi.org/10.1111/cas.14311 (2020).
Wang, D. et al. SWI/SNF complex genomic alterations as a predictive biomarker for response to immune checkpoint inhibitors in multiple cancers. Cancer Immunol. Res. 11(5), 646–656. https://doi.org/10.1158/2326-6066.Cir-22-0813 (2023).
Walhart, T. A. et al. SMARCB1 loss in poorly differentiated chordomas drives tumor progression. Am. J. Pathol. 193(4), 456–473. https://doi.org/10.1016/j.ajpath.2022.12.012 (2023).
Ritchie, M. E. et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucl. Acids Res. 43(7), e47. https://doi.org/10.1093/nar/gkv007 (2015).
EnhancedVolcano: Publication-ready volcano plots with enhanced colouring and labeling. Updated 2024.
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: An R package for comparing biological themes among gene clusters. OMICS 16(5), 284–287. https://doi.org/10.1089/omi.2011.0118 (2012).
Bu, C. et al. GenBase: A nucleotide sequence database. Genom. Proteom. Bioinform. https://doi.org/10.1093/gpbjnl/qzae047 (2024).
Database Resources of the National Genomics Data Center. China national center for bioinformation in 2024. Nucleic Acids Res. 52(D1), D18-d32. https://doi.org/10.1093/nar/gkad1078 (2024).
Acknowledgements
We thank the Center of Basic Medical Research at Peking University Third Hospital’s Institute of Medical Innovation and Research for providing the necessary equipment and research space essential for part of this study.
Funding
This work was supported by the National Natural Science Foundation of China (82371319 to CY), Beijing Nova Program (20230484356 and 20240484699 to CY), Beijing Natural Science Foundation (7222217 and L246046 to CY), AO Spine Research Start-up Grant (AOS-Startup-21-016 to CY), Peking University Clinical Scientist Training Program supported by "The Fundamental Research Funds for the Central Universities" (BMU2024-PYJH017 to CY), Capital Health Research and Development of Special Fund (2022-4-40918 to CY), Research Project of Peking University Third Hospital in State Key Laboratory of Vascular Homeostasis and Remodeling (2024-VHR-SY-06 to CY), Digital and Humanities Project supported by "The Fundamental Research Funds for the Central Universities" (7101503232 to CY), and Peking University Third Hospital Clinical Key Project (BYSYZD2021023 to CY).
Author information
Authors and Affiliations
Contributions
Study conception and design: CY. Writing- Original draft preparation: WL, MR. Data collection, analysis, and visualization: WL, MR, SL, YX, YD, YW, JY. Writing- Reviewing and Editing: WL, MR, CY. Supervision: CY, JY.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Peking University Third Hospital.
Informed consent
Informed consent was obtained from all subjects and/or their legal guardians prior to their participation in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, W., Regmi, M., Liu, S. et al. SMARCB1 orchestrates cellular plasticity and oncogenic pathways in typical and chondroid chordomas. Sci Rep 15, 19942 (2025). https://doi.org/10.1038/s41598-025-04508-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04508-0