Abstract
In Tunisia, cervical cancer ranks as the 14th most common cancer, largely driven by high-risk of Human Papillomavirus (HPV) types, notably HPV 16 and 18. Current screening efforts are limited, with only 17% of all women aged 35-60 undergoing Pap-smear testing. The introduction of the HPV vaccine in 2025 through the national school vaccination program, targeting girls aged 11-12, is expected to reduce the burden of cervical cancer. However, alongside vaccination, enhanced screening strategies are essential for early detection and prevention of HPV-related cancers. Aim This study aims to assess the cost-effectiveness of different HPV screening strategies in Tunisia, specifically examining the combination of varying HPV screening frequencies and a vaccination program targeting girls aged 11-12. The objective is to determine the most cost-efficient screening strategy to complement vaccination efforts in reducing cervical cancer incidence. A cost-effectiveness analysis was conducted from the perspective of the Tunisian healthcare system using the HPVsim model, a multi-agent-based simulation tool that captures HPV transmission dynamics and cervical cancer progression. Four approaches were compared: (1) maintaining the current Pap-smear screening strategy combined with vaccination; (2) introducing HPV DNA testing once between ages 35-40; (3) introducing HPV DNA testing twice between ages 35-45, with a 5-year interval; and (4) introducing HPV DNA testing every 5 years for women aged 35-60. All approaches were combined with the vaccination program. Screening coverage rates of 15%, 25%, 33%, 50%, and 70% were tested for each approach. Primary outcomes included the number of cancer cases averted, total intervention costs, and cost increase per cancer case averted. Academic literature and existing evidence were included on the demographic variables, cervical cancer incidence and mortality, treatment costs, vaccine delivery costs and other model parameters. All interventions resulted in substantial reductions in cervical cancer cases, with decreases ranging from 41% to 59% in cumulative cases between 2025 and 2090. The most intensive approach, involving HPV DNA testing every 5 years for women aged 35-60, achieved the largest reduction, with a 59% decrease in cumulative cervical cancer cases by 2090, although it also incurred the highest costs. The least costly option, which retained current Pap-smear testing alongside vaccination, reduced cervical cancer cases by 41%. Although the introduction of HPV DNA testing significantly increases costs, a high frequency of screening allows for quicker public health benefits. The scenario combining vaccination and maintaining current screening practices is found to be the most cost-effective for the Tunisian context. If the price of the HPV DNA test is reduced to $9 USD, the most frequent testing strategy would become the most cost-effective option, offering both high effectiveness and financial viability. Lowering the cost of HPV DNA testing could make more frequent screening financially sustainable, providing greater public health benefits. These findings offer valuable guidance for decision-makers in shaping future strategies for cervical cancer prevention in Tunisia.
Similar content being viewed by others
Introduction
Human Papillomavirus (HPV) is a group of viruses transmitted through sexual contact, infecting the epithelial cells of the skin and mucous membranes, HPV infections can lead to benign conditions like genital warts and, over time, to precancerous or cancerous lesions, particularly uterine cervical cancer1.
In Africa, despite ongoing efforts to enhance prevention and treatment, cervical cancer continues to be a major concern due to socioeconomic challenges, restricted healthcare access, and insufficient awareness2. To address this, the World Health Organization (WHO) has launched the “90-70-90” initiative, which aims to globally eliminate cervical cancer by vaccinating 90% of girls against HPV before age 15, screening 70% of women at ages 35 and 45, and treating 90% of women with cervical disease3. This strategy is supported by awareness campaigns, international collaborations, and funding to bolster health systems in developing countries.
The WHO advocates for HPV screening as a key tool for early detection of cervical cancer, particularly in low- and middle-income countries. The guidelines recommend that women start screening at age 30 and continue at regular intervals, typically every 5 to 10 years, depending on the type of test and previous results4. In Tunisia, opportunistic or spontaneous cytology screening is available for women aged 35 to 59, with low coverage, at approximately 15%.
As a result, there is growing interest in adopting the HPV DNA test, which offers automation and ease of processing. Although this test primarily detects HPV types 16 and 18, it could significantly increase screening coverage. HPV DNA test prices vary by manufacturer (Hologic Aptima, GenProbe Aptima, BD Onclarity, CareHPV) and region (low-income coutries, middle-income countries) from $5 to $100 (https://supply.unicef.org/s0001704.html). Given the high cost of testing, it is essential to evaluate screening frequency and coverage alongside vaccination efforts.
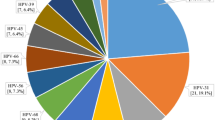
In Tunisia, HPV types 16 and 18 are the most common genotypes linked to cervical infections and cancers, with other high-risk types such as HPV 31, 45, 51, and 56 also prevalent5. Cervical cancer is the \(14^{th}\) most common cancer, representing 2% of cancers in Tunisia in 20226. Beginning in 2025, vaccination will be integrated into the existing school-based immunization program in Tunisia, using the bivalent vaccine to target girls aged 11 to 12. With a school enrollment rate of 92% and an estimated coverage rate of 97% within the school vaccination program, the overall vaccine coverage is projected to reach approximately 87%7. A 90% coverage rate is used as an upper-bound scenario to provide a benchmark for assessing the potential impact under the most optimistic conditions.
A cost-effectiveness analysis was conducted to compare various HPV vaccination strategies, demonstrating that CECOLIN is the most cost-effective option, particularly when cross-protection is considered7. Given that Tunisia does not have a strict willingness-to-pay (WTP) threshold for assessing cost-effectiveness, the authors evaluated the probability of vaccines being cost-effective across a range of possible WTP thresholds, up to 0.3 times the national GDP per capita. Notably, CECOLIN showed a 100 % probability of being cost-effective at a WTP threshold of $200, equivalent to 5% of Tunisia’s national GDP per capita, when compared to no vaccination.
The goal of this work is to identify the most cost-efficient screening strategy to complement vaccination efforts. We will use the multi-agent-based model HPVsim, which integrates social interaction dynamics, HPV transmission, and its progression to cervical cancer.
The document presents a cost-effectiveness analysis of combined HPV vaccination and screening strategies in Tunisia. The section details the use of the HPVsim model for simulation, including descriptions of intervention scenarios, costs, and outcomes. It covers demographic, biological, and social parameters, focusing on varying screening frequencies and vaccine coverage. The section compares the effectiveness of different strategies in reducing HPV infections and cervical cancer cases. Finally, section concludes the document.
Results
We simulated the maintenance of the current cervical cancer screening process,which relies on opportunistic cytology screening for women aged 35 to 608, while simultaneously introducing routine vaccination for girls aged 11–12 (see Figure 1b and 1a in red). The simulation projected a reduction in both HPV infections and cervical cancer cases by 65% and 75%, respectively, by the year 2090. We also evaluated alternative strategies defined by scenarios 2, 3 and 4. By 2090, Scenario 2, which introduced HPV DNA testing at a frequency of one test for women aged 35–40 plus routine vaccination, showed reductions in HPV infections and cervical cancer cases by 62-69% and 75-77%, respectively (see Figures 1b and 1a in blue). Scenario 3, which introduced HPV DNA testing at a frequency of two tests for women aged 35–45 plus routine vaccination, showed reductions in HPV infections and cervical cancer cases by 62-68% and 74-77%, respectively (see Figures 1b and 1a in yellow). Finally, Scenario 4, which introduced HPV DNA testing at a frequency of every 5 years for women aged 35–60 plus routine vaccination, showed reductions in HPV infections and cervical cancer cases by 63-66% and 75-80%, respectively (see Figures 1b and 1a in green). The slight upward trend observed at the beginning of the curves for scenarios 1 and 2 in Figure 1b (red and blue, respectively) is due to the convex shape of the Baseline curve, which shows a continuous and accelerating increase in yearly cancer cases. In contrast, the scenario curves are concave, initially increasing but then declining due to vaccination and/or screening interventions. As the model is stochastic, smoothing them against the Baseline causes this effect. The minor upward peak, under 5%, is negligible.
Although all scenarios resulted in almost similar reductions in HPV infections and cervical cancer cases by 2090, the rate of decrease differed across scenarios. The more frequent is the screening, the steeper the decline in the annual cancer cases curve. For instance, the annual cancer cases curve for Scenario 1 begins its downward trend from 2040, for Scenario 2 from 2040, for Scenario 3 from 2035, and for Scenario 4 almost immediately from 2025 (see Figure 1b). However we don’t notice any considerable difference in the rate of decrease of HPV infections between all scenarios. For further examination, supplementary analysis was conducted to study the effect of HPV-DNA test introduction by comparing the reduction in HPV infections and cervical cancer cases of scenarios 2-4 which include the HPV DNA test to the scenario 1 which doesn’t include the introduction of HPV DNA test. For reduction in HPV infections there are no notable differences between scenarios 2-4 as all the curves are within −9% and +1% difference margin (see Figure 2a). As for reduction in cancer cases there are notable differences as the more frequent the screening, the more we notice the effect of the introduction of HPV-DNA test; for instance in scenario 2 where the HPV-DNA test is conducted at a rate of once in a lifetime there is barely any noticeable effect when compared to scenario 1 which doesn’t include the introduction of HPV-DNA test as reduction of cancer cases of scenario 2 compared to scenario 1 is always nearing 0%; between −6% and +4% (see Figure 2b), in scenario 3 where the HPV DNA test is conducted at a rate of twice in a lifetime, the reduction of cancer cases when compared to scenario 1 is, also, always nearing 0%; between −5% and +0%, and in scenario 4 where the HPV DNA test is conducted at a rate of every 5 years, the absolute reduction of cancer cases when compared to scenario 1 reaches a maximum of 22%. We observe that over longer time horizons, particularly by the year 2090, the outcomes will be primarily influenced by vaccination rates, as the impact of introducing the HPV-DNA test diminishes, and by 2090, all scenarios become equivalent.
The annual reduction in HPV infections and cancer cases for scenarios (1-4), compared to the baseline scenario. For scenarios (2-4), the curves represent the average reductions across various coverage rates tested, with the shaded areas indicating the range of minimum and maximum values (min-max envelope) resulting from different coverage rates. The boxplots display the thickness of the min-max envelope, reflecting the variability due to the different coverage rates tested for each strategy. Scenario 1 (red): maintaining the current screening strategy coupled with vaccination; Scenario 2 (blue): introducing the HPV DNA test at a frequency of one screening between ages 35 and 40, coupled with vaccination; Scenario 3 (yellow): introducing the HPV DNA test at a frequency of two screenings spaced 5 years apart between ages 35 and 45, coupled with vaccination; Scenario 4 (green): introducing the HPV DNA test at a frequency of every 5 years for women aged 35-60, coupled with vaccination.
The annual reduction in HPV infections and cancer cases for scenarios (1-4), compared to the scenario 1. For scenarios (2-4), the curves represent the average reductions across various coverage rates tested, with the shaded areas indicating the range of minimum and maximum values (min-max envelope) resulting from different coverage rates. The boxplots display the thickness of the min-max envelope, reflecting the variability due to the different coverage rates tested for each strategy. Scenario 2 (blue): introducing the HPV DNA test at a frequency of one screening between ages 35 and 40, coupled with vaccination; Scenario 3 (yellow): introducing the HPV DNA test at a frequency of two screenings spaced 5 years apart between ages 35 and 45, coupled with vaccination; Scenario 4 (green): introducing the HPV DNA test at a frequency of every 5 years for women aged 35-60, coupled with vaccination.
In a second analysis, we examined the percentage of cumulative cancer cases averted from 2025 to 2090 across these different scenarios. Results indicate that the more frequent is the screening, the higher the percentage of cumulative cancer cases averted. We should note that varying the screening coverage rate within the same scenario had little influence on the outcome in terms of cancer reduction, as there was no significant difference in the mean percentage of cumulative cancer cases averted (see Figure 3). Scenario 1 resulted in a reduction of cumulative cancer cases from 2022 to 2090 by 42%. In scenario 2 the mean percentage of cumulative cancer reduction varies between 40% and 44%. In Scenario 3 the mean percentage of cumulative cancer reduction varies between 43% and 46%. Finally, in Scenario 4 the mean percentage of cumulative cancer reduction varies between 53% and 59% (see Figure 3).
The figure presents the cumulative cancer cases averted percentage for each scenario compared to the baseline scenario. Error bars are the 90th and 10th percentile, boxes are the 75th and 25th percentiles, horizontal lines in each box is the mean. Scenario 1 is maintaining the current screening strategy coupled with vaccination; Scenario 2 is introducing the HPV DNA test at a frequency of one screening during a lifetime at the age between 35 and 40, coupled with vaccination; Scenario 3 is introducing the HPV DNA test at a frequency of two screenings during a lifetime spaced 5 years apart at the age between 35 and 45, coupled with vaccination; Scenario 4 is introducing HPV DNA test at a frequency of every 5 years for women aged between 35 and 60, coupled with vaccination.
A similar analysis and comparison was conducted having as a reference scenario the no-interventions scenario where we exclude any form of screening or treatment, even the already existing interventions, can be found in the appendix.
Cost analysis reveals that scenarios incorporating HPV DNA testing are significantly more expensive compared to Scenario 1, which retains the less-costly Pap-smear test. Figure 4 shows that costs escalate with greater coverage rates within each scenario which is contrary to what we noted on the effect of increasing coverage rate on reducing cancer cases. We also notice that Scenarios 1 and 2 are cost-saving, suggesting that these two scenarios are less expensive than the Baseline Scenario therefore adapting one of these two strategies will actually generate positive revenue.
The figure presents the cost increase in percentage for each scenario compared to the baseline scenario. Error bars are the 90th and 10th percentile, boxes are the 75th and 25th percentiles, horizontal line in each box is the mean. Scenario 1 is maintaining the current screening strategy coupled with vaccination; Scenario 2 is introducing the HPV DNA test at a frequency of one screening during a lifetime at the age between 35 and 40, coupled with vaccination; Scenario 3 is introducing the HPV DNA test at a frequency of two screenings during a lifetime spaced 5 years apart at the age between 35 and 45, coupled with vaccination; Scenario 4 is introducing HPV DNA test at a frequency of every 5 years for women aged between 35 and 60, coupled with vaccination.
Combining cost and efficacy data, we compared the cost increase per cancer case averted for each scenario to the average GDP between 2025 and 2090. The cost-effectiveness analysis reveals that all strategies 1-4 falls within the “cost-effective” range, (see Figure 5a) as all scores are under the three times the average GDP per capita from 2025 to 2090 threshold. Furthermore, strategies 1-2 have negative cost-effectiveness scores meaning that adapting one of these strategies is cheaper than having no intervention at all. Scenario 3 is emerging as “very cost effective” because its scores are between zero and one times the average GDP per capita. Finally Scenario 4 is emerging as “cost effective” because its scores are between one times and three times the average GPD per capita.
A sensitivity analysis was conducted to explore the feasibility of strategy 4 that includes screening at a rate of every 5 years for women aged between 35 and 60. Our findings suggest that at a price of 8.00USD for the HPV-DNA test, all scenarios are cost-saving whatever the coverage rate is (see Figures 5b and 5c), this suggests that adapting any of the scenarios is cheaper than the Baseline scenario. In this case, Scenario 4, which includes vaccination for girls aged 11–12 and HPV DNA screening every 5 years for women aged 35–60, specifically at a coverage rate of 70%, emerging as the most favorable due to its highest reduction in cancer cases (see Figure 3). And these observations persist if we consider the price to be 5.00USD reported in this article9 (see Figure 5c) See appendix for a description of all results.
The figure illustrates the cost-effectiveness defined as the cost increase per cancer case averted for all the screening strategies across all the tested coverage rates of screening at different prices of the HPV DNA test. Error bars are the 90th and 10th percentile, boxes are the 75th and 25th percentiles, and horizontal lines in each box represent the mean. The dotted horizontal lines represent the “cost-effective” range defined as a score between one and three times the average GDP per capita between 2025 and 2090. Scenario 1 is maintaining the current screening strategy coupled with vaccination; Scenario 2 is introducing the HPV DNA test at a frequency of one screening during a lifetime at the age between 35 and 40, coupled with vaccination; Scenario 3 is introducing the HPV DNA test at a frequency of two screenings during a lifetime spaced 5 years apart at the age between 35 and 45, coupled with vaccination; Scenario 4 is introducing HPV DNA test at a frequency of every 5 years for women aged between 35 and 60, coupled with vaccination.
Discussion
The association between cervical cancer and the HPV genome was first identified in 1983, marking a turning point in cervical cancer research10. Since then, significant progress has been made in the fight against the disease. However, after the HPV vaccine was approved for clinical use in June 2006, the focus of the scientific and medical community shifted from the simple prevention of cervical cancer to the ambitious goal of eliminating it11.
Our current study demonstrated that the most cost-effective strategy for the Tunisian context towards that goal, involves introducing routine HPV vaccination with the bivalent vaccine for girls aged 11 to 12 years, achieving a 87% coverage rate, while maintaining the current screening strategy using Pap-smear tests for women aged 35 to 65 years with a 1% coverage rate. This approach is projected to reduce cumulative cervical cancer cases by 41% between 2025 and 2090. By 2090, the reduction in cancer cases is expected to reach 76% compared to the baseline scenario without vaccination. Although strategies that include HPV DNA screening method coupled with vaccination are also cost-effective. Regarding screening tools, our findings align with those of Chen M-K et al., who demonstrated that annual Pap smear testing yields the highest gain in life years when compared to HPV DNA testing12. This could be explained by the fact that Pap smear screening not only detects early-stage invasive cervical carcinoma but also prevents the malignant transformation of precursor lesions. Additionally, the cost of Pap smear testing is lower than that of HPV DNA testing, making it a more cost-effective option. On the other hand, the WHO recommends HPV DNA based screening, as it is less prone to human errors and also suitable for all settings, areas, and countries13. Moreover, cost-effectiveness studies done in other low and middle income countries (LMIC) including India, Kenya, Peru, South Africa and Thailand confirm the efficacy of HPV DNA screening and its cost effectiveness in these areas14.
The divergence between these findings highlights the importance of considering country-specific factors when choosing screening strategies. Differences in healthcare infrastructure, the availability of healthcare professionals, gross domestic product (GDP), and the population’s acceptance of certain screening tools all play critical roles in determining the most suitable approach for each country. In Tunisia, despite the low coverage rate due to limited capacity of labs to process tests, the geographical distribution is good across the country with 2085 primary care centers distributed throughout the 24 governorates
When it comes only to the number of cancer cases, our results shows that maintaining the current screening strategy with existing coverage rates in Tunisia or introducing intensive screening based on the HPV DNA test yields similar outcomes by the end of our time horizon when compared to the introduction of the HPV DNA test. Actually, the key difference lies in the time required to achieve these results and the deployed costs. The strategy involving intensive HPV DNA screening significantly accelerates the reduction in cervical cancer cases, leading to earlier public health benefits’ range although being costlier than the first scenario. As explained by Castaneda-Orjuela et al, the decision making process in the public health field should be a comprehensive process valuing consequences beyond the health system, including the population well-being15.
Our study has several notable strengths. First of all, the HPVsim model was parameterized to closely align with Tunisian demographic and behavioral parameters, as well as the prevalence of HPV in the country. This customization ensures that the model accurately reflects the unique characteristics of the Tunisian population. Secondly, the model was rigorously calibrated to produce predictions that closely match real-world data, such as the distribution of HPV genotypes in 2013 and the annual incidence of cervical cancer cases between 2020 and 2022. This calibration process enhances our confidence in the relevance and reliability of the results within the Tunisian context. Lastly, all the scenarios and their variations were developed in close collaboration with experts in vaccination and HPV screening from the Pasteur Institute of Tunis. Their insights, suggestions, and feedback were invaluable in ensuring that the study’s questions were pertinent to real-world challenges. This collaboration significantly contributes to the practical applicability of our findings, aiding in shaping the decision-making process regarding HPV vaccination and screening strategies in Tunisia.
Our study also has several limitations that should be taken into account. Firstly, we did not explore all possible HPV screening tests available on the market, nor did we consider every potential screening target or routine vaccination target and coverage. This decision was made to focus on strategies that were most relevant to Tunisian policymakers at the time of the study. Secondly, we did not incorporate the effects of migration or HIV infections into our model. This omission could potentially lead to an overestimation of the vaccine’s effectiveness. Thirdly, The model assumes constant sensitivity and specificity of the HPV test for detecting HSIL, whereas these parameters actually vary depending on the duration of infection and the lesion progression dynamics. This approach overlooks the fact that the test’s clinical specificity is partly affected by women who are HPV-positive but have not yet developed HSIL. As a result, the model may underestimate the preventive effectiveness of HPV-based screening, particularly in strategies involving more frequent testing. Nevertheless, we think that despite these limitations, the overall conclusion of the study should remain robust as the most cost-effective strategy identified would likely remain the same, though the exact efficacy score might differ. Lastly, when calculating costs, we assumed a constant discount rate of 3% throughout the entire simulation period, extending until 2090. While this is a simplified assumption, it’s a common assumption used in many studies of cost-effectiveness analysis in public health16,17,18,19,20 as it’s recommended by the Second Panel on Cost-Effectiveness in Health and Medicine21.
Models can be categorized by the following criteria: (a) Randomness: Deterministic models use pre-determined rates for events such as HPV acquisition and clearance, resulting in consistent outcomes, while stochastic models incorporate randomness, leading to varying results with each run. (b) Structure Level: Individual-based models simulate events for each person, capturing individual variability, whereas aggregate models group individuals into compartments, reducing internal variability. (c) Interaction: Dynamic models consider herd immunity by modeling infection risk based on the number of infectious individuals, reflecting changes over time. In contrast, static models assume a constant infection rate and do not account for herd immunity. HPVSim is a dynamic, stochastic multi-agent model that explicitly incorporates both vaccination and screening, along with complex social sexual interactions22. This integration of multiple factors makes it an ideal choice for our study, providing a detailed and realistic simulation of HPV transmission dynamics and preventive measures. It is worth noting that similar models exist, such as those by23,24. However these models, HPVsim included, do not consider certain criteria such as equity and acceptability. In the aftermath of the COVID pandemic, vaccine hesitancy has become a significant threat to global health25. Experts are increasingly recommending that the acceptability of vaccines and screening tools be included in health economic evaluations, which was not done in this study26.
Methods
Study design
We conducted an economic evaluation through a cost-effectiveness analysis of combined vaccination and screening strategies tailored to the Tunisian context. This analysis was approached from a healthcare system perspective using the multi-agent model HPVsim. The analysis was reported according to the Consolidated Health Economic Evaluation Reporting Standards statement.
Modelling
HPVSim is a software package developed that provides flexibility for creating agent-based models to simulate HPV transmission and cervical disease progression22. The simulations generated using HPVSim feature a population of agents who interact via sexual networks, over which multiple co-circulating HPV genotypes can be transmitted. Persistent infections can lead to cervical dysplasia, which may spontaneously regress or progress to invasive cervical cancer. HPVSim can also simulate the effects of interventions, including vaccination, screening, and treatment.
By default, simulations run with HPVsim include genotypes 16, 18, and a pooled group consisting of all other high-risk types. In Tunisia, studies5 has shown that many high-risk genotypes such as HPV 31, 35, 39, 52, 56, 58 and 58 are prevalent in the population. Therefore we modified to the HPVsim code to include these additional high-risk genotypes. A detailed description on genotype identification is available in the appendix.
The model parameters are categorized into three categories: demographic parameters, obtained from the World Bank and the National Institute of Statistics in Tunisia (https://www.ins.tn/taxonomy/term/113), biological parameters related to HPV transmission and progression to cervical cancer, and social parameters related to sexual behavior. The latter were obtained from a survey conducted by the Tawhida Ben Cheikh Association on a stratified cluster sample of unmarried Tunisians aged 18 to 3027. The details about HPVsim parametrization and a table with parameter and their references is provided in the appendix.
Unknown model parameter values were evaluate by model calibration using data on HPV genotype prevalence in Tunisia in 2012 national survey5,5 and yearly cancer cases from 202028 and 20226. The method used was Adam29. Details on the calibration methodology is provided in the appendix.
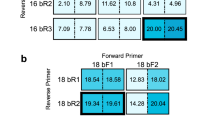
We used evidence to estimate the level of protection of Bivalent HPV vaccine against the HPV genotypes that are prevalent in Tunisia30,31 (genotypes 16, 18, 31, 35, 39, 52, 56, 58 and 58). This information was used to update the cross-protection matrix of the vaccine in the HPVsim model. The appendix provides the updated cross-protection matrix.
Intervention scenarios
In January 2024, the Ministry of Health in Tunisia announced plans to introduce the HPV vaccine into the national school vaccination program starting in 2025. The vaccine will be administered to girls in their 6th year of primary school (i.e. 11-12 years old). With a vaccination coverage rate of approximately 97% in school settings and a school enrollment rate of 92%, the program is expected to provide widespread protection against HPV. A prior cost-effectiveness analysis on vaccine selection suggested that the bivalent vaccine, priced under 10.5 USD, is a cost-efficient choice7.
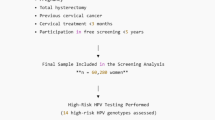
Currently, cervical cancer screening in Tunisia is estimated to cover 15% of women aged 35 to 6032 which translates to approximately an annual screening probability of 1.33%, calculation details to derive this annual probability of screening from the overall coverage are provided in the appendix. The screening is conducted using the Pap-smear cytology test.. Women who test positive for high-risk HPV types are referred for further evaluation through colposcopy and biopsy, where precancerous lesions can be identified and then treated. A detailed description of the screening and treatment process is provided in the appendix. The low screening coverage is mainly due to the limited capacity of laboratories to process Pap-smear tests. Consequently, there is growing interest in increasing coverage by introducing the HPV DNA test, which can be automated and processed without manual intervention.
For this study, we aim to evaluate the costs and benefits of the following four scenarios: maintaining the current screening strategy coupled with vaccination (Scenario 1); introducing the HPV DNA test at a frequency of one screening during a lifetime between the ages of 35 and 40, coupled with vaccination (Scenario 2); introducing the HPV DNA test at a frequency of two screenings during a lifetime spaced 5 years apart between the ages of 35 and 45, coupled with vaccination (Scenario 3); and finally, introducing the HPV DNA test at a frequency of every 5 years for women aged 35 to 60, coupled with vaccination (Scenario 4). For every scenario that includes the introduction of the HPV DNA test, we assumed a gradual rollout beginning in 2030, with the desired final coverage rate being reached in 2035, thereby fully replacing the Pap-smear test. We tested different targeted coverage rates: 15%, 25%, 33%, 50%, and 70%.
These scenarios will be compared to a Baseline scenario defined as follows: maintaining the current screening strategy with a 1% screening rate per year for women aged 35 to 60 years, without introducing any modifications to the screening methodology or rate, and without introducing vaccination.
For all scenarios, including the Baseline scenario, we assumed that 90% of those who test positive for HPV would follow up with colposcopy and biopsy, and 90% of those diagnosed with precancerous lesions would receive appropriate treatment. This assumption includes a 10% drop-off at each stage to approximately represent those who do not continue treatment. We also suppose that vaccination will be integrated into the existing school vaccination program using the bivalent vaccine, targeting girls aged 11 to 12, at an estimated coverage rate of 87% starting in 2025.
Costs
All costs are of 2024 adjusted with a 3% discount rate applied for future years. The bivalent vaccine was priced at 10.25USD per dose7. This cost includes delivery and implementation costs (e.g. necessary infrastructure, logistics, personnel, refrigeration units, etc...). The treatment cost for cervical cancer was estimated at 2463.00USD per case33, the cost has been applied to all cancer cases, assuming that all cancers are being treated. Additionally, the costs for pap-smear test, colposcopy and pre-cancer treatments, including excision and ablation, were based on the official CNAM Hospital Price Template at 6.50USD, 6.80USD, 18.00USD, and 18.00USD, respectively. CNAM is the National Health Insurance Fund, established to manage health insurance systems and provide coverage for medical expenses for Tunisian citizens. Finally the HPV DNA test was estimated at 29.00USD per test based on expert consultation. All costs are summarized in Table cost in the appendix.
Outcomes
The simulations were run from 1990 to 2090 to compute the full effects of transmission dynamics and intervention outcomes, with each scenario being simulated 10 times for each coverage rate. The primary outcomes of HPVsim include the yearly number of HPV cases, cancer cases, vaccine doses administered, tests performed, colposcopies conducted, and pre-cancer treatments administered. These outcomes were collected from 2025 to 2090. The yearly cancer cases and HPV infections from HPVsim were fitted using a 5th degree polynomial for smoothing; this was applied across all 10 replicates for each coverage rate in each scenario. Costs were calculated by multiplying the yearly HPVsim outcomes of each medical intervention by its corresponding unit price, assuming that all cervical cancer cases would receive treatment. This was also applied across all 10 replicates for each coverage rate in each scenario.
We performed random sampling on the data for averted HPV infections (yearly and cumulative), averted cancer cases (yearly and cumulative), increased costs (yearly and cumulative), and cost-effectiveness as follows: We selected a group of 3 replicates from the 10 replicates of a given coverage rate in each scenario and then averaged the results. This process was repeated 60 times for each coverage rate in every scenario. To determine the averted cancer cases of each replicate, we calculated the reduction in cancer cases compared to the average of the baseline scenario. We assessed the associated cost increase of each replicate by comparing the cost to the average of the baseline scenario. We defined cost-effectiveness using the following criteria: a scenario is considered highly cost-effective if the increased cost per cancer case averted is less than one times the average per capita Tunisian gross domestic product (GDP); cost-effective if it is between one and three times the average GDP; and not cost-effective if it exceeds three times the average GDP. The per capita Tunisian GDP is estimated to be 3895USD in 202334, discounted by 3% every year from 2025 to 2090 and then the average was calculated.
Data availability
The datasets used and/or analysed during the current study available on github https://github.com/IPT-BIMS/hpvsim_tunisia.git. Our study does not involve any experimental procedures on human subjects or the use of human tissue samples. Additionally, the participant data used in this study were sourced from a publicly available database.
References
IARC Working Group. Human Papillomaviruses, vol. 90 of IARC Monographs on the Evaluation of Carcinogenic Risks to Humans (WHO, 2007).
Word Health Organisation (WHO). HPV in Africa. https://www.afro.who.int/health-topics/cervical-cancer
Geneva: World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. WHO global strategy (2020).
World Health Organization (WHO) WHO recommends DNA testing as a first-choice screening method for cervical cancer prevention. Sept 2021. https://www.who.int/europe/news/item/11-09-2021-who-recommends-dna-testing-as-a-first-choice-screening-method-for-cervical-cancer-prevention
Ardhaoui, M. et al. The Prevalence, Genotype Distribution and Risk Factors of Human Papillomavirus in Tunisia: A National-Based Study. Viruses 14, 1–15. https://doi.org/10.3390/v14102175 (2022).
Ferlay, J. et al. Global Cancer Observatory: Cancer Today (2022).
Laraj, O. et al. Human papillomavirus vaccination at the national level in Tunisia: a cost-effectiveness analysis using a comparative modeling study. medRxiv https://doi.org/10.1101/2024.09.17.24313756 (2024).
Khiari, H., Makni, K., Meddeb, K., Jaidane, O. & Hsairi, M. Cost-effectiveness of Human Papillomavirus (HPV) Vaccination in Tunisia: A Modelling Study. BMJ Open 14, e085462. https://doi.org/10.1136/bmjopen-2024-085462 (2024).
Inturrisi, F. & and, J. B. Pricing of hpv tests in italian tender-based settings. Journal of Medical Economics 25, 762–768, https://doi.org/10.1080/13696998.2022.2082777 (2022). PMID: 35616231,
Frazer, I. H. The HPV Vaccine Story. ACS Pharmacol and Transitional Science 2, 210–212 (2019).
Markowitz, L. E. & Schiller, J. T. Human Papillomavirus Vaccines. The Journal of Infectious Diseases 224, S367–S378 (2021).
Chen, M.-K., Hung, H.-F., Duffy, S., Yen, A.M.-F. & Chen, H.-H. Cost-effectiveness analysis for Pap smear screening and human papillomavirus DNA testing and vaccination. Journal of Evaluation in Clinical Practice 17, 1050–1058 (2011).
Word Health Organisation (WHO). HPV Screening.
Woo, Y. L., Gravitt, P., Khor, S. K., Ng, C. W. & Saville, M. Accelerating action on cervical screening in lower- and middle-income countries (LMICs) post COVID-19 era’’. Preventive Medicine 144, 106294 (2021).
Castañeda-Orjuela, C., García-Molina, M. & De la Hoz-Restrepo, F. Is There Something Else Beyond Cost-Effectiveness Analysis for Public Health Decision Making?. Value in Health Regional Issues 23, 1–5. https://doi.org/10.1016/j.vhri.2019.09.009 (2020).
Zou, Z. et al. Domestic HPV vaccine price and economic returns for cervical cancer prevention in China: a cost-effectiveness analysis. The Lancet Global Health 8, e1335–e1344. https://doi.org/10.1016/S2214-109X(20)30277-1 (2020).
Su, S. et al. Cost-effectiveness of universal screening for chronic hepatitis B virus infection in China: an economic evaluation. The Lancet Global Health 10, e278–e287. https://doi.org/10.2139/ssrn.3848518 (2022).
Waterlow, N. R. et al. The potential cost-effectiveness of next generation influenza vaccines in England and Wales: A modelling analysis. Vaccine 41, 6017–6024. https://doi.org/10.1016/j.vaccine.2023.08.031 (2023).
Wondimu, A., Postma, M. J. & van Hulst, M. Cost-effectiveness analysis of quadrivalent and nonavalent human papillomavirus vaccines in Ethiopia. Vaccine 40, 2161–2167. https://doi.org/10.1016/j.vaccine.2022.02.080 (2022).
Palmer, M. R. et al. The impact of alternate HPV vaccination and cervical screening strategies in Japan: a cost-effectiveness analysis. The Lancet Regional Health - Western Pacific 44, 101018. https://doi.org/10.1016/j.lanwpc.2024.101018 (2024).
Sanders, G. D. et al. Recommendations for Conduct, Methodological Practices, and Reporting of Cost-effectiveness Analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA 316, 1093–1103. https://doi.org/10.1001/jama.2016.12195 (2016).
Stuart, R. M. et al. HPVsim: An agent-based model of HPV transmission and cervical disease. PLOS Computational Biology 20, 1–17. https://doi.org/10.1371/journal.pcbi.1012181 (2024).
Bonneault, M. et al. Contact patterns and HPV-genotype interactions yield heterogeneous HPV-vaccine impacts depending on sexual behaviors: An individual-based model. Epidemics 39, 100584. https://doi.org/10.1016/j.epidem.2022.100584 (2022).
van Schalkwyk, C., Moodley, J., Welte, A. & Johnson, L. F. Estimated impact of human papillomavirus vaccines on infection burden: The effect of structural assumptions. Vaccine 37, 5460–5465. https://doi.org/10.1016/j.vaccine.2019.06.013 (2019).
Nuwarda, R. F., Ramzan, I., Weekes, L. & Kayser, V. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines (Basel) 10 (2022).
Bishai, D., Brenzel, L. & Padula, W. Handbook of Applied Health Economics in Vaccines (Oxford University Press, 2023).
Chekir, H. & Belhadj, H. Enquête sur la recomposition des valeurs en rapport avec la sexualité, la santé sexuelle et reproductive et la relation de genre https://groupe-tawhida.org/ (2023).
Bruni, L. et al. Human Papillomavirus and Related Diseases in Tunisia. Summary Report 10 March 2023. Tech. Rep., ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre) (2023).
Kingma, D. P. & Ba, J. Adam: A Method for Stochastic Optimization, 2017. arxiv:1412.6980.
Malagón, T. et al. Cross-protective efficacy of two human papillomavirus vaccines: A systematic review and meta-analysis. The Lancet Infectious Diseases 12, 781–789. https://doi.org/10.1016/S1473-3099(12)70187-1 (2012).
Saeki, Y. et al. Effectiveness of prophylactic HPV vaccines against cervical abnormalities and HPV infection in Japan: The J-HERS 2021 multicenter study. Journal of Medical Virology 96, https://doi.org/10.1002/jmv.29413 (2024).
Khiari, H., Makni, K., Meddeb, K., Jaidane, O. & Hsairi, M. Cost-effectiveness of human papillomavirus (hpv) vaccination in tunisia: a modelling study. BMJ Open https://doi.org/10.1136/bmjopen-2024-085462 (2024).
Garci, M. Cancer du col de l’utérus: étude épidémiologique multicentrique. MD thesis, School of Medecine (2020).
The World Bank. GDP per capita (current US$) - Tunisia (2024). https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=TN
Acknowledgements
Authors would like to thank the reviewers for their thoughtful comments and valuable suggestions. Their feedback has greatly contributed to improving the clarity, rigor, and overall quality of our work. This work was supported by Bill & Melinda Gates Foundation [INV-059607] through AMAX (African Modeling and Analytics Academy for Women) project and by Vaccine Impact Modelling Consortium (VIMC). Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission. At the time of analysis, the VIMC was jointly funded by Gavi, the Vaccine Alliance, and the Bill & Melinda Gates Foundation (grant numbers INV-034281 and INV-009125/OPP1157270).
Author information
Authors and Affiliations
Contributions
AL conducted the simulations, performed result analysis, as well as contributed to article drafting. BB, HT assisted in data collection and contributed to writing the discussion draft. AG, EE, RS and SRR provided recommendations and suggestions for conceiving the simulations. RS and SRR reviewed the first draft of the article. OL helped with data analysis. AK, HA and SBM provided supervision, with SBM also contributing to the methodology and article drafting.
Corresponding author
Ethics declarations
Ethical approval
This study does not involve any experimental procedures on human participants or the use of human tissue samples. The data used were sourced from publicly available databases, and no additional ethical approval was required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lahdhiri, A., Benzina, B., Ennaifer, E. et al. HPV DNA screening and vaccination strategies in Tunisia. Sci Rep 15, 27916 (2025). https://doi.org/10.1038/s41598-025-13423-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-13423-3