Abstract
Fungal keratitis caused by Candida albicans (CA) is a common, disabling eye disease with a complex immune response system, affecting diagnosis, treatment, and prognosis. The specific regulatory roles and interactions of IL-36γ and pigment epithelium-derived factor (PEDF) in this disease remain largely unclarified. Additionally, the influence of miR-204-5p on the expression and anti-inflammatory functions of IL-36γ and PEDF in CA keratitis is insufficiently explored. Therefore, research focused on understanding the disease’s pathogenesis and immune regulation. Human corneal epithelial cells treated with heat-killed CA showed anti-inflammatory responses from IL36γ and PEDF, confirmed via western blot, PCR, and ELISA. Transfection of small interfering RNA and recombinant protein granules showed PEDF exerts immunoprotected regulatory mechanisms by inhibiting NF-κB via PPARγ. Analysis of multiple miRNA target gene prediction databases and literature revealed that miR-204-5p is differentially expressed in fungal keratitis. PCR and dual luciferase reporter assays confirmed that miR-204-5p directly binds to PEDF mRNA, negatively regulating IL36γ and PEDF expression. Consequently, both PEDF and IL-36 γ exhibit anti-inflammatory effects in CA keratitis. PEDF may inhibit the NF-κB signaling pathway through the PPAR γ pathway. In addition, miR-204-5p inhibits the mRNA expression of IL-36 γ and PEDF, exacerbating inflammation. This provides a theoretical basis for new methods and drug targets for the prevention and treatment of CA keratitis, and promotes the clinical application of IL-36 γ/PEDF.
Similar content being viewed by others
Introduction
Candida albicans (CA) is a common opportunistic pathogen causing fungal keratitis, which can lead to vision loss or even blindness1,2,3. This infection often occurs after eye surgery, local corticosteroid use, systemic diseases, or eye trauma 4,5. Fungal keratitis has diverse clinical manifestations and lacks specific signs, causing frequent misdiagnoses, increasing treatment challenges, disability, and blindness rates6,7,8. With the advent of global ageing, the increase in chronic diseases (cardiovascular disease and diabetes) and reduced immunity of the older population, escalate cases of retinal vascular disease and diabetic eye disease9,10. Understanding fungal keratitis pathogenesis and developing new treatment methods are essential in ophthalmology and have important clinical value and social significance.
IL-36γ, belonging to the cytokine IL-1 family, regulates inflammatory responses in various cells 11,12, including promoting the differentiation and activation of Th17 cells, influencing the occurrence and development of inflammatory diseases13,14,15. In Pseudomonas aeruginosa Keratitis, IL-36γ is crucial for immune regulation, activating NF-κB, MAPK, Erk1/2, JNK, and recruiting numerous macrophages and natural killer cells to produce inflammatory or anti-inflammatory responses16,17. In IL-36R-/- in mice with Candida albicans infected corneas, IL-17 A, IL-17 F, IL-22, and IL-23 (key cytokine levels for Th17 activation) significantly increase, intensifying the infection18. In addition, previous studies have shown that IL-36γ enhances ocular angiogenesis by promoting the vascular endothelial growth factor vascular endothelial growth factor receptor axis19. These studies show that IL-36γ plays an important role in inflammatory diseases of the eye.
PEDF is a secreted glycoprotein with multiple biological functions20. In the pathogenesis of keratitis, PEDF plays a protective role by promoting corneal nerve regeneration, inhibiting corneal neovascularization, and reducing inflammatory reactions21. PEDF inhibits inflammatory cytokine expression, including IL-1 β, IL-6, TNF-α, and IL-17 A, as seen in conditions such as dry eye syndrome22,23,24. PEDF functions by inhibiting the MAPK p38 and JNK phosphorylation in hypertonic human corneal epithelial cells (hCECs)25. PEDF nourishes corneal nerves, aiding in nerve repair after damage. PEDF inhibits corneal neovascularization, crucial for controlling pathological neovascularization in keratitis26. PEDF has antioxidant properties, improving atherosclerotic plaque stability by inhibiting macrophage inflammation response27. However, the specific role and mechanism of PEDF in fungal keratitis remain unclear. Preliminary research found that PEDF expression in hCECs significantly decreases after CA infection. Pre-treating cells with recombinant PEDF reduces cytokine levels and alleviates infection severity. Therefore, this study aimd to explore the molecular signaling pathway of PEDF in CA keratitis, and provided a new direction for the treatment of PEDF in keratitis.
MiR-204-5p is a microRNA (miRNA) involved in cell growth, differentiation, proliferation, and apoptosis28. In corneal diseases, miR-204-5p expression patterns are associated with various eye diseases, and may regulate effects via specific target genes. miR-204-5p may influence diabetes keratopathy by targeting SIRT129,30. In addition, miR-204-5p also plays an important role in corneal injury healing, maintaining blood-retinal barrier stability in a quiescent state and influencing cell apoptosis, survival, and inflammatory mediator expression in human trabecular meshwork cells31. This suggests that miR-204-5p may regulate inflammation and repair processes in corneal lesions32,33. In fungal keratitis, miR-204-5p expression is significantly lower than that in normal cornea, indicating its role in corneal defence against fungal infections34,35. This study aimed to reveal the pathogenesis and new defence pathways of fungal keratitis by regulating IL36 γ, PEDF, and miR-204-5p expression and their effects on CA keratitis, providing new clinical targets for treatment strategies.
Results
After infection with CA, hCECs showed increased IL-36 γ expression and decreased PEDF expression
After treating hCECs with CA for 0, 1, 3, 6, 9, and 18 h, inflammatory factors, IL36 γ, and PEDF in the cells and supernatant were detected. The PCR results (Fig. 1A–E) showed that the expression of inflammatory factors such as IL-1β, IL-6, CXCL-8, CCL-20, and S100a9 increased after 3 h of infection, peaking at 6 h. ELISA detection of the protein expression levels also yielded similar results (Fig. 1F–J). Western blotting results showed that after CA stimulation of hCECs, cytokine IL-1β and IL-36γ expression increased, whereas PEDF expression decreased (Fig. 1K–N).
After infection with CA, hCECs showed increased expression of IL36γ and decreased expression of PEDF. A–E PCR results show the expression levels of inflammatory cytokine IL-1β, IL-6, CXCL8, CCL20, and S100a9 in hCECs at different time points of CA infection. (n = 3). F–J ELISA results showed the expression levels of inflammatory cytokine IL-1β, IL-6, IL-8, CCL20, and S100a9 in the cell supernatant of hCECs infected with CA at different time points. (n = 3). K–N Western blot results showed the expression levels of IL-36γ and PEDF in hCECs at different time points of CA infection. (n = 3). Data are presented as the means ± SDs; *p < 0.05, **p < 0.01, ***p < 0.005 and ****p < 0.001.
PEDF and IL-36γ exert anti-inflammatory effects on CA-infected hCECs
During hCECs culturing, si-IL36γ, si-PEDF, and exogenous recombinant proteins IL-36γ and PEDF, were added separately, and their knockdown and overexpression efficiencies were detected using western blot analysis (Fig. 2A, B). Subsequently, cells were divided into the control group, si-IL36γ, rh-IL36γ, si-PEDF, and rh-PEDF groups. After CA treatment for 6 h, the expression of IL-36γ, PEDF, and downstream inflammatory factors were detected in all groups. Western blotting results showed that IL-36γ knockdown decreased PEDF expression. PEDF knockdown also decreased IL-36γ expression. IL-36γ and PEDF knockdown increased inflammatory cytokine IL-1β expression, whereas IL-36γ and PEDF overexpression decreased it (Fig. 2C and D). The PCR results (Fig. 2E) showed that inflammatory factors such as IL-1 β, IL-6, CXCL-8, CCL-20, and S100a9 increased after IL-36 γ and PEDF knockdown, and decreased after IL-36γ and PEDF overexpression. ELISA confirmed these findings (Fig. 2F). This indicated an interaction between IL-36γ and PEDF, suggesting that both play an anti-inflammatory role in CA-infected hCECs.
IL36γ and PEDF alleviate the inflammatory response of hCECs infected with CA. A, B Western blotting results validate the overexpression and knockdown efficiency of IL36γ and PEDF. (n = 3). C, D Western blotting results show IL36γ, PEDF, and IL1β expression in hCECs across different groups after 6 h of CA infection treatment. (n = 3). E PCR results showing IL1 β, IL6, CXCL8, CCL20, and S100a9 expression in hCECs across different groups after 6 h of CA infection treatment. (n = 3). F PCR results showing IL1 β, IL6, IL8, CCL20, and S100a9 expression in the supernatant of hCECs across different groups after 6 h of CA infection treatment. (n = 3). Data are presented as the mean ± SD; *p < 0.05, **p < 0.01, ***p < 0.005 and ****p < 0.001.
PEDF exerts anti-inflammatory effects in CA-infected hCECs by inhibiting the NF-KB signalling pathway via PPARγ
HCECs were divided into three groups: control, rh PDEF, and rh PDEF + GW9662, with all groups tested after 6 h of CA stimulation. The ELISA results showed that the expression of inflammatory factors TNF-α, IL-1β, and IL-6 was reduced in the rh-PEDF group, and the addition of GW9662 inhibited the anti-inflammatory effect of PEDF (Fig. 3A–C). Western blotting results showed that adding recombinant PEDF may reduce p-p65 expression and inhibit the activation of NF-KB after CA infection. Simultaneously adding GW9662 reduced the effect of PEDF (Fig. 3D–F). These results indicated that PEDF exerts an anti-inflammatory effect in hCECs infected with CA, possibly through the inhibition of the NF-KB signalling pathway by PPARγ.
PEDF inhibits the NF-κB signalling pathway via PPARγ. A–C ELISA results show the expression of inflammatory factors TNF-α, IL1β, and IL6 in the supernatant of cells across different groups. (n = 3). D–F Western blot results show P65 and P-P65 expression across different groups. (n = 3). Data are presented as the mean ± SD; *p < 0.05, **p < 0.01, ***p < 0.005 and ****p < 0.001.
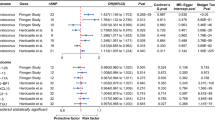
miR-204-5P inhibits the expression of IL36 γ/PEDF mRNA, exacerbating the inflammatory response caused by CA
Three miRNAs related to fungal keratitis were selected via database screening of PEDF and IL-36γ targeting miRNAs (PubMed search) (Fig. 4A). miR-204-5p may act on the mRNA of IL-36γ and PEDF and inhibit their expression (Fig. 4B). Subsequently, a series of experiments were conducted to confirm this. During hCEC culturing, the miR-204-5p mimic was added. PCR detection showed that the addition of miR-204-5P mimics significantly reduced IL-36γ and PEDF expression in cells (Fig. 4C). Subsequently, we divided the cells into three groups: control, si-IL-36γ, and si-IL-36γ + miR-204-5p inhibitor. All groups were treated with CA infection for 6 h. PCR and ELISA were used to detect PEDF, revealing that the expression of PEDF was reduced in the si-IL-36γ group compared to the control group. The addition of miR-204-5p inhibitor partially alleviated the decrease in PEDF (Fig. 4D). To further investigate the relationship among miR-204-5p, IL-36γ, and PEDF, we conducted a dual luciferase reporter assay, which showed that miR-204-5p could inhibit the expression of PEDF mRNA (Fig. 4E).
miR-204-5P inhibits the expression of IL36γ/PEDF mRNA, exacerbating the inflammatory response of CA-infected hCECs. A Intersection of miRNAs targeting IL36γ and PEDF, as identified from the database screening, with miRNAs associated specifically with fungal keratitis. B Database prediction of the binding sites of miR-204-5p with IL36γ and PEDF mRNA. C PCR detection of miR-204-5p expression. (n = 3). D PCR detection of IL36γ and PEDF expression after adding miR-204-5p. (n = 3). E PCR and ELISA detection of PEDF expression across different groups. (n = 3). F Dual luciferase reporter assay detects the effect of miR-204-5p on PEDF transcription. (n = 3). Data are presented as the mean ± SD; *p < 0.05, **p < 0.01, and ****p < 0.001.
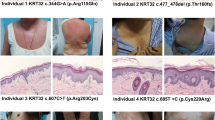
Exogenous PEDF alleviates the inflammatory response of CA-infected mouse cornea
To observe whether exogenous PEDF has affected CA keratitis pathogenesis, mouse IL-36γ was subcutaneously injected 4 h before CA infection, with BSA as a control. After 24 h of CA infection in mouse corneas, keratitis severity was evaluated via clinical scoring, and infected corneas were collected to measure fungal load, Myeloperoxidase (MPO)activity levels, and inflammatory cytokine levels. Results indicated that, compared with the control group, mice in the exogenous PEDF group had reduced corneal opacity and significantly lower clinical scores (Fig. 5A). Fungal counts decreased from 1600 to 500 CFU (Fig. 5B) in the exogenous PEDF group, and MPO activity also decreased (Fig. 5C). The ELISA results also showed that adding exogenous PEDF inhibit IL-1β, IL-6, TNF -α, and S100a9 expression and promote IL-10 expression (Fig. 5D). These results indicated that PEDF can inhibit inflammation, promote repair, and protect the cornea from excessive CA infection.
Exogenous PEDF can alleviate the inflammatory response of CA-infected mouse cornea. A Corneal slit lamp imaging and clinical scoring of corneal injuries across different groups. (n = 6). B Fungal load assessment of mouse corneas across different groups; results are expressed as CFU/per cornea. (n = 6). C MPO detection of corneas across different groups. (n = 6). D ELISA results showing the expression of inflammatory cytokines IL1β, IL6, TNFα, S100a9, and IL10 across different groups with keratitis. (n = 6). Data are presented as the mean ± SD; *p < 0.05, **p < 0.01 and ***p < 0.005.
miR-204-5p Inhibition promotes IL-36γ and PEDF expression and alleviates the inflammatory response in CA-infected mouse Corneas
To investigate the role of miR-204-5p in CA keratitis, 5 µL of miR-204-5p inhibitor was subcutaneously injected into mice cornea 24 and 4 h before CA infection. After 24 h of CA infection, keratitis severity was evaluated via clinical scoring, and infected corneas were collected for fungal load, MPO activity levels, and inflammatory cytokine detection. The experimental results showed that, compared with the control group, mice in the miR-204-5p inhibitor group had reduced corneal opacity and significantly lower clinical scores (Fig. 6A). Western blotting results showed, compared with the control group, the miR-204-5p inhibitor group increased IL-36γ and PEDF expression (Fig. 6B, C), decreased fungal count from 1500 to 700 CFU (Fig. 6D), and decreased MPO activity (Fig. 6E). The ELISA results also showed that adding the miR-204-5p inhibitor inhibited IL1β, IL6, TNF-α, and S100a9 expression and promoted IL10 expression (Fig. 6F). These results indicated that miR-204-5p inhibitors increased of IL-36γ and PEDF expression, contributing to protection against corneal CA infection.
Inhibition of miR-204-5p promotes IL36γ and PEDF expression and alleviates the inflammatory response in CA-infected mouse corneas. A Corneal slit lamp imaging and clinical scoring of corneal injuries across different groups. (n = 6). B, C Western blotting results show the effect of miR-204-5p inhibitor on IL36γ and PEDF expression. (n = 6). D Fungal load assessment performed on mouse corneas across different groups, and the results are expressed as CFU/per cornea. (n = 6). E MPO detection of corneas across different groups. (n = 6). F ELISA results show the expression of inflammatory cytokines IL1β, IL6, TNFα, S100a9, and IL10 across different groups with keratitis. (n = 6). Data are presented as the mean ± SD; *p < 0.05, **p < 0.01, and ****p < 0.001.
Discussion
This study investigated changes in specific inflammatory factors and protein expression in hCECs after CA infection, assessing their impact on inflammation. The results showed inflammatory factors such as IL-1β, IL-6, CXCL-8, CCL-20, and S100a9 were upregulated 3 h post-infection, peaking at 6 h. In addition, PEDF and IL-36γ inhibited inflammatory responses, and PEDF may exert a protective effect by inhibiting the NF-KB signalling pathway via PPARγ. miR-204-5p inhibited the expression of IL-36γ and PEDF mRNA, exacerbating the inflammatory response. In mouse models, exogenous PEDF and miR-204-5p inhibitors alleviated corneal inflammation after CA infection.
In addition, PEDF, a protein with anti-inflammatory and antioxidant properties, protects the cornea from inflammatory damage, aligning with our findings that reduced PEDF expression is associated with increased inflammation in CA-infected keratitis. Several studies have shown that PEDF can regulate the NF-κB signaling pathway through PPARγ in various diseases. For example, in dry eye disease, PEDF has been found to reduce the expression of inflammatory cytokines such as IL-1β and TNF-α by activating the NF-κB signaling pathway, thereby alleviating the inflammatory response of the ocular surface25. In diabetic nephropathy, PEDF inhibits age-induced podocyte apoptosis by regulating PPARγ and prevents advanced glycation end product-induced mesangial cell damage by blocking NF-κB activation36,37,38. These findings indicate that PEDF regulates the PPARγ and NF-κB signalling pathways in ocular diseases as well as other diseases, playing a crucial role in modulating inflammation and immune responses. In CA infection, the activation of the NF-κB signalling pathway can lead to the excessive production of inflammatory cytokines, causing tissue damage and aggravating the infection. By suppressing the NF-κB signalling pathway through PPARγ, PEDF can effectively reduce the inflammatory response, protect corneal tissue from damage, and promote the recovery of the infected cornea. This supported anti-inflammatory and antioxidant effects of PEDF in fungal keratitis. Although the role of miR-204-5p in CA has not been widely studied, miRNAs are widely recognised for regulating inflammatory responses, and our findings provided new insights into this field. In addition, the role of miR-204-5p in regulating IL-36γ and PEDF expression offers a novel perspective on miRNA’s role in keratitis. In mouse models, exogenous PEDF and miR-204-5p inhibitors significantly alleviated keratitis indicating these molecules have therapeutic potential.
Although this study provides valuable insights, it had several limitations. First, the research primarily relied on in vitro cell culture and animal models, necessitating further clinical studies to confirm the applicability of the results to human patients. Second, although we observed an interaction between IL-36γ and PEDF, the exact molecular mechanism of this interaction remains unclear. In addition, although miR-204-5p precisely regulated the mRNA site of PEDF, further research is needed to investigate other potential mechanisms of action and the regulation of IL-36γ by miR-204-5p. In addition, the results in Fig. 1 show that after CA infection of hCEC cells, PEDF expression decreases and IL-36 γ expression increases, which may be due to the disruption of the balance between the inflammatory response caused by CA infection and the body’s anti-inflammatory response. The specific reasons need further research in the later stage.
PEDF has shown significant anti-inflammatory potential in multiple studies39. For instance, in the experimental dry eye (EDE) model, the PEDF-derived short peptide 29-mer demonstrated therapeutic effects on EDE, preventing its development and accompanied by improvements in inflammatory factors such as MMP9, IL-1β, TNF-α, and IL-640. In retinal diseases, PEDF-loaded mesenchymal stem cell-derived small extracellular vesicles enhance therapeutic effects by increasing the stability and permeability of PEDF, thereby enhancing its anti-angiogenic, anti-inflammatory, and neuroprotective properties41. These findings suggest that PEDF could serve as a promising therapeutic agent for CA keratitis and other inflammatory eye diseases. Enhancing therapeutic efficacy through combined use: Given the regulatory relationship between PEDF and miR-204-5p, combining PEDF-based therapies with miR-204-5p inhibitors may produce synergistic effects. For example, exogenous administration of PEDF could directly exert anti-inflammatory effects while suppressing miR-204-5p expression. In turn, miR-204-5p inhibitors could further upregulate endogenous PEDF expression, amplifying the therapeutic outcome.
In summary, this study found that PEDF and IL-36γ exhibited an anti-inflammatory interaction in CA keratitis. PEDF may inhibit the NF-KB signalling pathway via the PPARγ pathway. In addition, miR-204-5p inhibited the expression of IL-36γ and PEDF mRNA, exacerbating inflammation. In mouse models, exogenous PEDF and miR-204-5p inhibitors alleviated keratitis after CA infection. The findings provide new insights into the molecular mechanisms of CA infection and are crucial for developing novel therapies targeting CA.
Methods
Preparation of Candida albicans solution
Liquid Sabouraud medium was prepared, sterilized at 120 °C for 15 min under high temperature and pressure, and stored at 4 °C after cooling. Shashi solid culture medium powder (45 g) was mixed with 1000 mL double distilled water and sterilized at 120 °C for 15 min under high temperature and pressure. After removal, 20 mL was poured into culture plates on a clean workbench, allowing it to solidify, air-dried for 20 min, and stored at 4 °C.
The purchased Candida albicans (CA) strain was stored at – 80 °C and revived before use. The strain was spread onto solid Sabouraud medium, cultured at room temperature for 3 d, and stored at 4 °C for later use.
Two round bottom shake flasks were filled with 6 mL of liquid Sabouraud medium each; one served as a blank and spores of CA were added to the other. Both flasks were placed on a horizontal shaker and incubated at room temperature for at least 16 h at 200 rpm.
The next day, the CA solution was transferred to a 15 mL centrifuge tube and centrifuged at 4000 rpm for 3 min, and the medium was discarded. The pellet was resuspended in 1 mL sterile PBS, the concentration was measured with a cell counter, and adjusted it 2 × 107 CFU/mL with sterile PBS.
Animals
Animal ethics
C57BL/6 mice (Male, 6–8 weeks old) were obtained from Beijing Vital River Laboratory Animal Technology. All animal experiments have been approved by the Shandong University Qilu Hospital Research Ethics Committee (Approval number: KYLL-2021 (KS) -1044). Mice are euthanized by dislocated cervical vertebrae, and the mice die within 5–10 s.
All methods were carried out in accordance with relevant guidelines and regulations. All methods are reported in accordance with ARRIVE guidelines.
Mouse pretreatment
rhPEDF pretreatment group: Four hours before infection, after anaesthesia and disinfection, mice received a 100 ng/5 µL subconjunctival injection of rhPEDF with a microinjection needle. The control group received a subconjunctival injection of 0.2% BSA in PBS (2.5 µL) above and below the eyeball.
miR-204-5p-inhibitor pretreatment group: Five microlitres of miR-204-5p-inhibitor (RNA interference) and miR-NC were injected subcutaneously 24 h and 4 h before infection, followed by CA infection for 1 d; a subconjunctival injection of 2.5 µL was administered above and below the eyeball.
Mouse CA infection
Routine ophthalmic disinfection was performed with iodine three times in the surgical area of the mouse eye. Mice were anaesthetized with a subcutaneous injection of pentobarbital sodium. After tendon and corneal reflexes disappeared, mice were placed under an ophthalmic microscope and subjected to ocular surface anaesthesia using Obukine eye drops, administered three times The conjunctival sac was rinsed three times with gentamicin solution. Using a pipette, 5 µL of pre-prepared CA mycelium suspension was dropped it onto the surgical eye.
Clinical scoring
Corneal disease was graded as described42: 0 = clear or slight opacity, partially or fully covering the pupil; 1 = slight opacity, fully covering the anterior segment; 2 = dense opacity, partially or fully covering the pupil; 3 = dense opacity, covering the entire anterior segment; and 4 = corneal perforation or phthisis.
Tissue protein extraction
RIPA lysis buffer (60 µL) was added to one corneal sample. The corneal tissue was homogenised with a magnetic bead shaker for 3 min. Thereafter the magnetic beads were removed. Ultrasonic shearing treatment was performed three times, followed by shaking on ice for 30 min. The sample was centrifuged at 15,000 rpm and 4 ℃ for 20 min, protein was obtained by collecting the supernatant. Protein samples were either stored at − 80 ℃ for future use or their concentration measured directly using the BCA method for balancing. Thereafter, 5× SDS loading buffer was added, and the protein was heated in a water bath for 10 min to denature before long-term storage at − 80 ℃.
ELISA
ELISA was performed according to the manufacturer’s instructions as follows: The sample (100 µL) was added to each well and incubated at 37 °C for 90 min. The plate was emptied and washed three times. Thereafter, the biotinylated antibody working solution was added for a 60-min incubation at 37 °C. The plate was emptied again, washed three times, and HRP enzyme conjugate working solution was incubated at 37 °C for 30 min. After discarding and washing the plate three times, 100 µL of TMB substrate solution was added to each well and incubated in the dark at 37 °C for 15 min.
Termination solution (50 µL) was added to each well, and the OD values were measured at 450 nm using an ELISA reader. A standard curve was generated based on the concentration and OD values of the standard samples, and sample concentrations were calculated using the curve equation.
MPO activity assay
A corneal sample was added to 60 µL PBS magnetic bead homogenate. Thereafter, the magnetic beads were removed. Corneal homogenate (30 µL) was mixed with 270 µL 0.5% HTAB phosphate buffer and transferred to a 1.5 mL EP tube. The EP tube was sealed and freeze-thawed three times using liquid nitrogen. After three rounds of ultrasonic shearing, the sample was centrifuged at 4000g for 15 min, and the supernatant was collected for later use. Twenty microlitres of supernatant was mixed with a 1:9 solution of o-dianisidine, and the rate of change in absorbance was measured at 460 nm within 1 min to calculate MPO activity according to the formula provided in the kit.
Corneal fungal load measurement: After MPO measurement, the remaining corneal homogenate was diluted in a gradient and plated onto Sabouraud solid culture medium. Two wells were prepared for each gradient and cultured at room temperature for 3 d. The fungal load on each cornea was calculated by counting fungi in each dish.
Cells
Cell culture
HCECs, SV40 immortalized human corneal epithelial cell lines has been ordered from Fuheng Biotechnology Co., Ltd. with the serial number FH1239, were cultured in DMEM/F12 containing 10% serum and 1% bispecific antibody. Cells were incubated at 37 ℃ in a 5% CO2 environment. For experimentation, cells were inoculated at a density of 1 × 105 cells/well in a 6-well plate and cultured in a normal growth medium until reaching 80% confluency.
CA treatment
A suspension of CA with a concentration of 2 × 107 CFU was heated in a constant temperature water bath at 100 ℃ for 10 min to inactivate the organism. After cooling, the suspension was used for stimulation experiments. For stimulation, 10 µL of the suspension was added to the culture medium in each well of a 6-well plate, achieving a final concentration of 2 × 105 CFU. After 6 h, the cell culture medium was collected, and the cells were scraped for downstream detection.
Cell protein extraction
Cells were washed three times with cold PBS, lysed with RIPA buffer, and shaken on ice for 20 min. The cell lysate was scraped from the culture container and transferred to a 1.5 mL tube. Cells were centrifuged at 14,000 rpm and 4 °C for 20 min to obtain the supernatant containing the protein.
Extraction of supernatant protein: After removing the sample supernatant, 5× SDS loading buffer was added. The mixture was boiled at 100 ℃ for 10 min, cooled, and stored at -20 ℃ for western blotting.
PCR
The cell supernatant was removed and the sample was washed three times with PBS. Sample RNA was extracted according to the manufacturer’s instructions, and reverse transcription was performed.
PPAR γ inhibitor treatment: hCEC cells with good growth were treated with 0.1% DMSO in the control group and 10 µM PPAR γ inhibitor (GW9662) in the experimental group. After incubation for 24 h, cells were stimulated with CA for 6 h to measure the expression and activity of P65/P-P65.
Transfection
When the cell density reached 70%, miR-204-5p/siR-IL36 γ/si-PEDF was transfected into hCEC or 293T cells using Lipofectamine 3000. After 6 h, the culture medium was replaced with the original medium. After 48 h, the transfected cells were used for further experiments. Transfection efficiency was validated via western blot analysis. Exogenous recombinant PEDF (CRP2287, Cohesion biosciences, Suzhou, China) was diluted with PBS to a concentration of 10 µM/µL and incubated with hCECs for 4 h before treating with CA.
Western blot analysis
Protein was separated on a 10% acrylamide gel via SDS-PAGE and transferred to a PVDF membrane. The membrane was sealed with 5% BSA at room temperature for 1 h. An antibody was applied to the membrane overnight at 4 ℃. After washing with TBST, the membrane was incubated with an appropriate secondary antibody at room temperature for 1 h. Protein bands were detected using chemiluminescent HRP substrate. The relative band densities of various proteins were analysed using ImageJ software. The complete western blot bands were shown in Figure S1 and S2.
Dual luciferase reporter assay
According to manufacturer’s instruction, 293T cells were inoculated in triplicate into a 70% confluent 96 well plate. After 24 h of culture, luciferase reporter gene and transcription factor plasmids were transfected using Lipofectamine 2000. A dual luciferase reporter kit was used to detect firefly and renal luciferase signals 48 h after transfection. The relative promoter activity was expressed as the ratio of firefly to sea kidney luciferase activity.
Bioinformatics analysis
miRWalk predicted the targeted miRNAs of IL-36 γ and PEDF. The intersection of was miRNAs were taken. miRNAs related to fungal keratitis were selected, resulting in the identification of miR204-5p.
Statistical analyses
Statistical analyses were performed using GraphPad software. One way analysis of variance is used for statistical evaluation. Student’s t-test was conducted on paired samples. All results are presented as the mean ± standard deviation (SD). A p value < 0.05 is considered statistically significant.
Data availability
The data and materials presented in this study are available upon request from the corresponding author.
References
Abbondante, S. et al. Immunity to pathogenic fungi in the eye. Semin Immunol. 67, 101753. https://doi.org/10.1016/j.smim.2023.101753 (2023).
Duan, H. J. et al. Extracellular vesicles from Candida albicans modulate immune cells function and play a protective role in fungal keratitis. Microb. Pathogenesis. 189, 106606. https://doi.org/10.1016/j.micpath.2024.106606 (2024).
Tuft, S., Stone, N. R. H., Burton, M. J., Johnson, E. M. & Borman, A. M. Antifungal susceptibility profiles for fungal isolates from corneas and contact lenses in the United Kingdom. Eye https://doi.org/10.1038/s41433-023-02719-1 (2023).
Reginatto, P. et al. Eye fungal infections: a mini review. Arch. Microbiol. 205, 236. https://doi.org/10.1007/s00203-023-03536-6 (2023).
Balasoiu, A. T., Balasoiu, M., Zlatian, O. M. & Ghenea, A. E. Bacterial and Fungal Keratitis in a Tertiary Care Hospital from Romania. Microorganisms 12, 787. https://doi.org/10.3390/microorganisms12040787(2024).
Hoffman, J. J., Burton, M. J. & Leck, A. Mycotic Keratitis-A global threat from the filamentous fungi. J. Fungi (Basel) 7. https://doi.org/10.3390/jof7040273 (2021).
Sitnova, A. V. & Svetozarskiy, S. N. Modern technologies in diagnosis of fungal keratitis (review). Sovrem Tekhnol. Med. 15, 73–84. https://doi.org/10.17691/stm2023.15.2.07 (2023).
Moramarco, A. et al. Efficacy of the Combined Intrastromal Injection of Voriconazole and Amphotericin B in Recalcitrant Fungal Keratitis. Microorganisms 12. https://doi.org/10.3390/microorganisms12050922 (2024).
Kwon, I., Talib, N. F., Zhu, J., Yang, H. I. & Kim, K. S. Effects of aging-induced obesity on the transcriptional expression of adipogenesis and thermogenic activity in the gonadal white adipose, brown adipose, and skeletal muscle tissues. Phys. Act. Nutr. 27, 39–49. https://doi.org/10.20463/pan.2023.0017 (2023).
Liu, B. et al. Lipid and glucose metabolism in senescence. Front. Nutr. 10, 1157352. https://doi.org/10.3389/fnut.2023.1157352 (2023).
Yuan, Z. C. et al. Biology of IL-36 signaling and its role in systemic inflammatory diseases. Front. Immunol. 10, 2532. https://doi.org/10.3389/fimmu.2019.02532 (2019).
Sugiura, K., Fujita, H., Komine, M., Yamanaka, K. & Akiyama, M. The role of interleukin-36 in health and disease States. J. Eur. Acad. Dermatol. https://doi.org/10.1111/jdv.19935 (2024).
Dong, H. N., Hao, Y. Q., Li, W., Yang, W. & Gao, P. IL-36 cytokines: their roles in asthma and potential as a therapeutic. Front. Immunol. 13, 13. https://doi.org/10.3389/fimmu.2022.921275 (2022).
Andoh, A. & Nishida, A. Pro- and anti-inflammatory roles of Interleukin (IL)-33, IL-36, and IL-38 in inflammatory bowel disease. J. Gastroenterol. 58, 69–78. https://doi.org/10.1007/s00535-022-01936-x (2023).
Ahmad, F. et al. Emerging role of the IL-36/IL-36R axis in multiple inflammatory skin diseases. J. Investig. Dermatol. 144, 206–224. https://doi.org/10.1016/j.jid.2023.11.004 (2024).
Gao, N., Me, R., Dai, C. Y., Seyoum, B. & Yu, F. S. X. Opposing effects of IL-1Ra and IL-36Ra on innate immune response to infection in C57BL/6 mouse corneas. J. Immunol. 201, 688–699. https://doi.org/10.4049/jimmunol.1800046 (2018).
Me, R. et al. IL-36α enhances host defense against keratitis in C57BL/6 mouse corneas. J. Immunol. 207, 2868–2877. https://doi.org/10.4049/jimmunol.2001246 (2021).
Dai, C. et al. Role of IL-36gamma/IL-36R signaling in corneal innate defense against Candida albicans keratitis. Investig. Ophthalmol. Vis. Sci. 62, 10. https://doi.org/10.1167/iovs.62.6.10 (2021).
Cho, W. J., Elbasiony, E., Singh, A., Mittal, S. K. & Chauhan, S. K. IL-36gamma augments ocular angiogenesis by promoting the vascular endothelial growth factor-vascular endothelial growth factor receptor axis. Am. J. Pathol. 193, 1740–1749. https://doi.org/10.1016/j.ajpath.2023.01.003 (2023).
Sagheer, U., Gong, J. & Chung, C. Pigment epithelium-derived factor (PEDF) is a determinant of stem cell fate: lessons from an ultra-rare disease. J. Dev. Biol. 3, 112–128. https://doi.org/10.3390/jdb3040112 (2015).
Yeh, S. I. et al. Pigment Epithelium-Derived Factor Peptide Promotes Corneal Nerve Regeneration: An In Vivo and In Vitro Study. Investig. Ophth Vis. Sci. 62, 23. https://doi.org/10.1167/iovs.62.1.23 (2021).
Chen, S. P. et al. A PEDF peptide mimetic effectively relieves dry eye in a diabetic murine model by restoring corneal nerve, barrier, and lacrimal gland function. Ocul Surf. 32, 1–12. https://doi.org/10.1016/j.jtos.2023.12.002 (2024).
Xiang, W. et al. PEDF protects retinal pigment epithelium from ferroptosis and ameliorates dry AMD-like pathology in a murine model. Geroscience 46, 2697–2714. https://doi.org/10.1007/s11357-023-01038-3 (2024).
Zhang, Q., Qi, S. A., You, J. X. & Wang, C. G. The role of retinal glial cells and related factors in macular edema. Biochem. Biophys. Res. Co 695, 149415. https://doi.org/10.1016/j.bbrc.2023.149415 (2024).
Ma, B. et al. Pigment epithelium-derived factor (PEDF) plays anti-inflammatory roles in the pathogenesis of dry eye disease. Ocul Surf. 20, 70–85. https://doi.org/10.1016/j.jtos.2020.12.007 (2021).
Chu, X. R. et al. Suppressive Role of Pigment Epithelium-derived Factor in a Rat Model of Corneal Allograft Rejection. Transplantation 108, 2072–2083. https://doi.org/10.1097/Tp.0000000000005032 (2024).
Wen, H. et al. PEDF improves atherosclerotic plaque stability by inhibiting macrophage inflammation response. Int. J. Cardiol. 235, 37–41. https://doi.org/10.1016/j.ijcard.2017.02.102 (2017).
Fan, C. et al. Circular RNA circ KMT2E is up-regulated in diabetic cataract lenses and is associated with miR-204-5p sponge function. Gene 710, 170–177. https://doi.org/10.1016/j.gene.2019.05.054 (2019).
Mobasher, M. A. et al. LncRNA LYPLAL1, miR-204-5p, and SIRT1: novel signatures for risk assessment of diabetic macrovascular complications. Sci. Rep. 14, 24154. https://doi.org/10.1038/s41598-024-75543-6 (2024).
Gao, J., Wang, Y., Zhao, X., Chen, P. & Xie, L. MicroRNA-204-5p-mediated regulation of SIRT1 contributes to the delay of epithelial cell cycle traversal in diabetic Corneas. Investig. Ophthalmol. Vis. Sci. 56, 1493–1504. https://doi.org/10.1167/iovs.14-15913 (2015).
Abbasi, M. et al. Effects of miR-204-5p modulation on PAX6 regulation and corneal inflammation. Sci. Rep. 14, 26436. https://doi.org/10.1038/s41598-024-76654-w (2024).
Wu, J. W., Zhang, D. W., Wu, J. H. & Zhang, S. H. Construction of ceRNA network and identification of hub genes in aniridia-associated keratopathy using bioinformatics analysis. Front. Genet. 13, (2022). https://doi.org/10.3389/fgene.2022.997581.
Xie, J. et al. Mir-204-5p alleviates mitochondrial dysfunction by targeting IGFBP5 in diabetic cataract. Mol. Biol. Rep. 51, 755. https://doi.org/10.1007/s11033-024-09701-4 (2024).
Boomiraj, H., Mohankumar, V., Lalitha, P. & Devarajan, B. Human corneal MicroRNA expression profile in fungal keratitis. Investig. Ophthalmol. Vis. Sci. 56, 7939–7946. https://doi.org/10.1167/iovs.15-17619 (2015).
Xu, S. B. & Hazlett, L. D. MicroRNAs in Ocular Infection. Microorganisms 7, 359. https://doi.org/10.3390/microorganisms7090359 (2019).
Ishibashi, Y. et al. PEDF inhibits AGE-induced podocyte apoptosis via PPAR-gamma activation. Microvasc. Res. 85, 54–58. https://doi.org/10.1016/j.mvr.2012.10.007 (2013).
Ide, Y., Matsui, T., Ishibashi, Y., Takeuchi, M. & Yamagishi, S. Pigment epithelium-derived factor inhibits advanced glycation end product-elicited mesangial cell damage by blocking NF-kappaB activation. Microvasc. Res. 80, 227–232. https://doi.org/10.1016/j.mvr.2010.03.015 (2010).
Dass, C. R. PEDF and its role in metabolic disease, angiogenesis, cardiovascular disease, and diabetes. Biomedicines 13 https://doi.org/10.3390/biomedicines13071780 (2025).
He, X., Cheng, R., Benyajati, S. & Ma, J. X. PEDF and its roles in physiological and pathological conditions: implication in diabetic and hypoxia-induced angiogenic diseases. Clin. Sci. (Lond). 128, 805–823. https://doi.org/10.1042/CS20130463 (2015).
Ho, T. C., Fan, N. W., Yeh, S. I., Chen, S. L. & Tsao, Y. P. The therapeutic effects of a PEDF-Derived short peptide on murine experimental dry eye involves suppression of MMP-9 and inflammation. Transl. Vis. Sci. Technol. 11, 12. https://doi.org/10.1167/tvst.11.10.12 (2022).
Fan, R. et al. Enhanced therapeutic effect of PEDF-loaded mesenchymal stem cell-derived small extracellular vesicles against oxygen-induced retinopathy through increased stability and penetrability of PEDF. J. Nanobiotechnol. 21, 327. https://doi.org/10.1186/s12951-023-02066-z (2023).
Guo, H., Gao, J. & Wu, X. Toll-like receptor 2 SiRNA suppresses corneal inflammation and attenuates Aspergillus fumigatus keratitis in rats. Immunol. Cell. Biol. 90, 352–357. https://doi.org/10.1038/icb.2011.49 (2012).
Funding
This study was supported by grants from the Youth Foundation of National Natural Science Foundation (82101088).
Author information
Authors and Affiliations
Contributions
C. D.: Conceptualization, Data curation, Methodology, Writing – original draft, Writing - review & editing, Visualization, Conceptualization, Funding acquisition. H. G.: Investigation, Software, Methodology. J. W.: Investigation, Validation. L.W.: Methodology, Investigation. L.S.: Investigation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dai, C., Guo, H., Wu, J. et al. The IL-36γ/PEDF/PPARγ signalling pathway plays an anti-inflammatory role in Candida albicans keratitis. Sci Rep 15, 31926 (2025). https://doi.org/10.1038/s41598-025-17965-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17965-4