Abstract
Medication-related osteonecrosis of the jaw is currently classified only by clinical staging, with no imaging-based qualitative classification available. To establish foundational data for a new classification method that could help guide treatment decisions and predict prognosis, this study investigated the computed tomography findings commonly observed in patients with medication-related osteonecrosis of the jaw and their frequencies. Computed tomography scans from 784 patients across 19 medical institutions were analyzed for the presence of osteolysis, sequestrum separation, periosteal reactions, mixed-type osteosclerosis, and the bone-within-bone appearance. Clinical factors associated with each finding were also examined. Osteolysis appeared as localized in 55.1% of cases, extended in 27.7%, and advanced in 13.8%. In contrast, 3.4% of patients showed no osteolysis. This non-osteolytic pattern was more common among patients treated with denosumab. Sequestrum separation was seen in 34.7% of patients, most frequently among those with osteoporosis. Periosteal reactions were observed in 5.9% of cases as the attached type, 12.4% as the gap type, and 5.6% as the irregular type. Mixed-type osteosclerosis occurred in 31.9% of cases, most often in the mandibles of patients with malignant tumors. The bone-within-bone appearance was observed in 3.1% of cases. Patients with sequestrum separation had more favorable treatment outcomes. In contrast, those without osteolysis and those with periosteal reactions, mixed-type osteosclerosis, or bone-in-bone appearance were more likely to have poorer outcomes. This multicenter study clarified the prevalence of several key computed tomography features in medication-related osteonecrosis of the jaw, highlighting their potential relevance to clinical outcomes. These findings lay the groundwork for future research into their prognostic and therapeutic implications to support the development of a new imaging-based classification system.
Similar content being viewed by others
Introduction
Medication-related osteonecrosis of the jaw (MRONJ) is a serious adverse event associated with antiresorptive agents. Although conservative treatment was initially recommended for MRONJ, surgical intervention is now widely recognized to yield better outcomes1. However, discussion regarding the most appropriate surgical approaches remains limited.
Current diagnostic and staging systems, such as the American Association of Oral and Maxillofacial Surgeons (AAOMS) staging system2, are based exclusively on clinical findings such as bone exposure and the extent of disease progression, but they do not incorporate imaging features. However, computed tomography (CT) frequently reveals diverse patterns, including osteolysis, sequestrum separation, periosteal reactions, and bone sclerosis, which may reflect the biological behavior of lesions. Despite their potential clinical relevance, these imaging findings have not been systematically evaluated or integrated into classification systems. Establishing an imaging-based framework is therefore an important step toward improving treatment selection and prognostic assessment in MRONJ.
Computed tomography (CT) imaging of MRONJ reveals a wide range of findings. Common features include osteolysis, sequestrum separation, and bone sclerosis3,4. We previously reported that periosteal reactions are frequently observed5 and can be classified into three types: attached type, gap type, and irregular type6,7. Additional patterns include mixed-type osteosclerosis characterized by numerous small hypodense areas within dense sclerotic bone8, minimal osteolysis accompanied by prominent periosteal reaction9, and extensive bone marrow necrosis without any apparent osteolysis10,11,12.
When selecting treatment for MRONJ, both the biological characteristics of the lesion (qualitative diagnosis) and the extent of disease progression (quantitative diagnosis) must be considered. However, current MRONJ classification systems are limited to staging that reflects only the degree of progression. Given the diverse imaging findings associated with MRONJ, we propose a new qualitative classification based on imaging features and plan to test whether this classification method is useful for selecting treatment options and predicting prognosis. This study aimed to assess the frequency of these imaging findings in a large multicenter cohort to provide foundational data for developing such a classification system. Establishing an imaging-based classification system for MRONJ is expected to support treatment selection, improve prognostic assessment, and contribute to a better understanding of disease pathogenesis.
Results
Patient characteristics
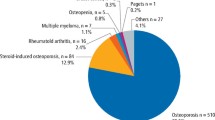
A total of 784 patients from 19 hospitals were enrolled (Table 1). The cohort included 207 men and 577 women. The primary lesion site was the maxilla in 214 patients and the mandible in 570. The underlying disease was osteoporosis in 473 patients and malignancy in 311. CT findings at the time of the initial examination were reviewed for all patients.
CT findings and associated factors
Localized, extended, and advanced types of osteolysis were observed in 432, 217, and 108 patients, respectively. In contrast, MRONJ without osteolysis—referred to as non-osteolysis MRONJ—was identified in 27 patients (3.4%; Table 2). Multivariate analysis revealed that non-osteolysis MRONJ was significantly more common among patients treated with denosumab (p = 0.036; Table 3).
Sequestrum separation was observed in 34.7% of patients (Table 2). This finding was significantly more common in older patients (p = 0.008), those with maxillary lesions (p = 0.014), those with osteoporosis (p < 0.001), and those who had taken a drug holiday from ARAs (p = 0.013). Sequestrum separation was also significantly associated with long-term ARA therapy (p = 0.002; Table 3).
Periosteal reactions were present in approximately one-third of cases. Specifically, 15.9% of patients exhibited the attached type, 12.4% the gap type, and 5.6% the irregular type (Table 2). The presence of periosteal reaction was significantly associated with the absence of steroid use (p = 0.005), advanced disease stage (p < 0.001), low white blood cell count (p = 0.005), high lymphocyte count (p = 0.005), and low albumin levels (p = 0.017; Table 3).
Mixed-type osteosclerosis was observed in 31.9% of patients (Table 2). Its occurrence was significantly associated with mandibular lesions, malignancy, elevated white blood cell count, and low albumin levels (Table 3).
The bone-within-bone appearance was rare, observed in only 3.1% of patients. Its development was significantly associated with drug holidays and advanced disease stage (Table 3).
CT findings and treatment outcomes
The relationship between CT findings and treatment outcomes is summarized in Table 4. Although patients with osteolysis had a better prognosis than those without, the difference was not statistically significant (odds ratio [OR] = 0.537, p = 0.169). In contrast, patients with sequestrum separation had a significantly higher cure rate (OR = 0.551, p < 0.001). Periosteal reactions were significantly associated with a higher relapse rate (OR = 1.736, p < 0.001), and mixed-type osteosclerosis was also a significant negative prognostic factor (OR = 1.581, p = 0.004). Moreover, patients with a bone-within-bone appearance had significantly poorer outcomes (OR = 3.586, p = 0.011).
Discussion
In this multicenter study of 784 patients with MRONJ from 19 institutions, we evaluated the frequency of key CT findings, including osteolysis, sequestrum separation, periosteal reactions, mixed-type osteosclerosis, and bone-within-bone appearance. We further analyzed associations between these imaging features and clinical factors such as age, underlying disease, antiresorptive agent use, and MRONJ stage. Notably, sequestrum separation was associated with favorable treatment outcomes, whereas non-osteolytic lesions, periosteal reactions, mixed-type osteosclerosis, and bone-within-bone appearance were linked to poorer prognosis. These results provide a comprehensive overview of CT characteristics in a large cohort and form a foundation for the development of a novel imaging-based classification system for MRONJ.
According to the AAOMS 2014 diagnostic criteria and staging system, the diagnosis of MRONJ is based solely on clinical findings, such as exposed bone, and does not incorporate imaging features. However, cases with extensive bone marrow necrosis but no bone exposure have been reported, highlighting the need to establish imaging-based diagnostic approaches for MRONJ10,11,12. In many diseases, including cancer, classification systems typically reflect both the extent of progression (e.g., staging) and the biological nature of the lesion (e.g., histology), and both inform treatment decisions. Although MRONJ has a stage classification, no system exists to classify the biological characteristics of the lesion. Given this gap, we considered imaging findings could not only aid in diagnosing MRONJ but also serve to classify lesion type and guide treatment selection and prognosis. To generate foundational data for such a system, we analyzed the frequency of CT findings across a large cohort of patients.
Although we used the AAOMS staging system, which is the most widely applied internationally, we recognize that alternative classifications incorporating both clinical and radiographic features, such as the SIPMO-SICMF Italian position paper13, exist. Our multicenter CT dataset provides foundational evidence that may support the future development of MRONJ classification systems integrating imaging features with clinical findings.
Osteolysis is a common finding in patients with MRONJ and often guides the choice of surgical technique. However, recent reports have described non-osteolytic MRONJ, which appears more frequently in patients receiving high-dose denosumab and is associated with poorer outcomes10,11,12. In the present study, non-osteolytic MRONJ was observed in 27 patients (3.4%) and was significantly more common among those treated with denosumab.
Sequestrum separation was present in approximately one-third of patients and was more frequent in older individuals with osteoporosis. It occurred more often in the maxilla than in the mandible and was associated with long-term ARA therapy. Although not evaluated in this study, Morishita et al. reported that sequestrum separation was more common in advanced lesions and in patients with primary osteoporosis who were not immunocompromised14.
Periosteal reactions are rare in bacterial osteomyelitis and even less common in radiation-induced osteomyelitis15. In contrast, they occur more frequently in MRONJ. Kojima et al. were the first to report periosteal reactions as a poor prognostic factor4. Soutome et al. classified them into three types—attached type, gap type, and irregular type—and noted that the latter two represent infectious lesions that should be included within the resection margin6,7. We have also described a rare variant, the periosteal reaction-dominant type, characterized by minimal or no osteolysis but extensive periosteal reaction9. The bone-within-bone appearance is a distensible osteolytic lesion with sequestrum separation and prominent central bone sclerosis following a prolonged course of MRONJ. It may represent an advanced form of the gap-type periosteal reaction7.
Bone sclerosis is a common finding in MRONJ. Suyama et al. reported that dense bone sclerosis may contain multiple small hypodense areas, referred to as mixed-type osteosclerosis8. Although CT cannot clearly differentiate whether these hypodense areas represent infection or residual bone marrow, their pathogenesis is becoming better understood. Real-time polymerase chain reaction has detected bacterial presence, and these lesions have been linked to postoperative relapse7 as well as histopathological evidence of inflammation12.
MRONJ presents with diverse imaging findings, and no standardized treatment has been established. Conservative therapy was previously recommended as first-line management, but recent studies have shown the superiority of surgical approaches1. Conservative treatment may lead to symptom resolution or prolonged stability, but in some cases, lesions rapidly worsen. Kojima et al. reported that in patients with periosteal reactions, conservative treatment often results in lesion progression over a short period, making surgical intervention preferable16. Even when surgery is selected, no consensus exists regarding the extent of bone resection or the optimal surgical technique17,18,19. In head and neck cancer, treatment is guided not only by stage but also by tumor characteristics—such as histological type (e.g., squamous cell carcinoma, adenocarcinoma) and, in the case of squamous cell carcinoma, the degree of differentiation (well, moderately, or poorly differentiated). In contrast, treatment decisions for MRONJ have not considered the biological behavior of lesions. To improve outcomes and preserve quality of life in MRONJ, we believe a new classification system is needed to describe the biological nature of these lesions and guide treatment selection.
The findings of this study also have clinical implications. For example, sequestrum separation observed on CT was associated with better treatment outcomes, suggesting that this feature may guide surgical decision-making. Conversely, periosteal reactions and bone-within-bone appearance were linked to poor prognosis, indicating that such imaging findings may alert clinicians to more aggressive disease requiring tailored management. Furthermore, while the AAOMS classification remains the most widely used system, our results suggest that the integration of imaging features could enhance diagnostic accuracy and prognostic stratification. The present multicenter data may thus serve as a foundation for developing future MRONJ classification systems that combine clinical and radiographic criteria, moving beyond purely clinical definitions.
This study has several limitations. Although MRONJ presents with a wide range of imaging findings, the lack of a standardized treatment approach across centers in this multicenter observational study limited our ability to evaluate the relationship between specific imaging findings and treatment outcomes. Nevertheless, as no similar large-scale studies exist, this analysis provides valuable estimates of the frequency of each imaging feature. The results suggest that sequestrum separation is associated with a favorable prognosis, whereas non-osteolytic MRONJ, periosteal reactions, and mixed-type osteosclerosis may indicate poorer outcomes. We intend to conduct a more detailed investigation of treatment strategies and clinical courses to develop a new classification system for MRONJ that can better inform treatment selection and prognosis.
In summary, this multicenter study identified the frequency of key CT findings in MRONJ, including osteolysis, sequestrum separation, periosteal reactions, mixed-type osteosclerosis, and bone-within-bone appearance. These data provide a foundation for further analysis of how imaging features relate to clinical outcomes. Building on these results, we plan to develop a qualitative classification system that can help guide treatment decisions and improve prognostic assessment in patients with MRONJ.
Methods
Patients
Patients with MRONJ who presented to any of the 19 participating institutions between January 1, 2011, and December 31, 2021, were included in the study. Inclusion criteria were: (1) diagnosis of MRONJ according to the AAOMS 2014 criteria, (2) availability of CT imaging within 1 month of the first visit, and (3) age ≥ 18 years. Exclusion criteria were: (1) history of radiation therapy to the jaws or metastatic disease to the jaws, (2) incomplete clinical data or absence of evaluable CT images, and (3) inability to confirm MRONJ diagnosis according to AAOMS criteria. CT scans obtained from the date of the first visit up to one month afterward were included, and all scans were performed prior to any surgical intervention to ensure that the images represented untreated MRONJ lesions at the time of diagnosis.
Data extracted from medical records included sex, age, lesion location, underlying disease (osteoporosis or malignancy), presence of diabetes, steroid use, type of antiresorptive agent (ARA) therapy, duration of ARA administration and drug holiday, relevant blood test results (white blood cell count, lymphocyte count, creatinine, and albumin levels), MRONJ stage, treatment method, and outcome. A drug holiday was defined as cessation of antiresorptive therapy for at least one month prior to diagnosis. The duration of drug holidays was recorded, and the same definition was applied to both bisphosphonate and denosumab users. Treatment methods were divided into conservative and surgical treatments. Conservative treatment was defined as symptomatic management without surgical removal of necrotic bone, including administration of antibiotics, analgesics, oral rinses, and local irrigation. Surgical treatment was defined as operative procedures involving removal of necrotic bone, such as sequestrectomy, curettage, or partial resection of the affected jaw. Treatment outcomes were classified into two categories: healing and non-healing. Healing was defined as the complete resolution of all clinical symptoms, including exposed bone, pain, swelling, and purulent discharge. Cases in which any of these findings persisted were classified as non-healing. Radiographic changes such as osteolysis or periosteal reaction were not required for the definition of healing.
CT findings
All CT images were obtained using helical (fan-beam) CT scanners. Cone-beam CT was not used in this study because it provides less diagnostic information for MRONJ compared with helical CT.
CT images were interpreted by two oral and maxillofacial radiologists or dentists. Multiple meetings were held among the participating research institutions to standardize the diagnostic criteria for key imaging features of MRONJ, including osteolysis, sequestrum separation, periosteal reactions, mixed-type osteosclerosis, and bone-within-bone appearance20. CT images were independently assessed by oral and maxillofacial surgeons at each institution. When discrepancies occurred, final evaluations were reached by consensus. Although formal statistical testing for inter-rater agreement was not performed, all images were reviewed on medical-grade diagnostic monitors under standard clinical lighting conditions. When multiple lesions were present in the same patient, the most severe lesion was consistently selected for imaging assessment. In cases with bilateral lesions in the same jaw, the more advanced site was recorded. Although CT models and imaging parameters varied across institutions, evaluations were based on images acquired in bone mode, reviewed in both horizontal and frontal sections. CT findings were classified as follows:
-
(1)
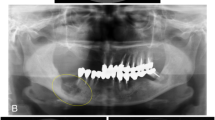
Osteolysis (Fig. 1).
Classified based on the extent of bone resorption in the maxilla and mandible:
(−): No osteolysis.
Localized type
Bone marrow or cortical osteolysis does not extend:
-
(1)
To the wall of the maxillary sinus, or
-
(2)
To the level of the superior border of the mandibular canal.
Extended type
Bone marrow or cortical osteolysis extends:
-
(1)
To the wall of the maxillary sinus, or
-
(2)
To the level of the superior border of the mandibular canal.
Advanced type
Bone marrow or cortical osteolysis extends:
-
(1)
Beyond the maxillary bone, involving the adjacent zygomatic bone, or
-
(2)
Beyond the level of the inferior border of the mandibular canal.
Note: In the anterior mandible, the reference point is the line connecting the mental foramina.
Classification of mandibular osteolysis (A–C) and maxillary osteolysis (D–F).(A) Localized type, not extending to the mandibular canal (arrow). (B) Extendedtype, reaching the mandibular canal (arrow). (C) Advanced type, extending to thelower portion of the mandibular canal (arrow). (D) Localized type, not extending tothe floor of the maxillary sinus (arrow). (E) Extended type, reaching the floor of themaxillary sinus (arrow). (F) Advanced type, extending beyond the maxillary bone,such as to the zygomatic bone (arrow).
-
(2)
Sequestrum separation (Fig. 2).
Defined as ≥ 90% separation of the sequestrum:
(−): No sequestrum separation.
(+): Sequestrum separation observed.
Classified by the presence and morphology of periosteal new bone formation:
(−): No periosteal reaction.
Attached type—new bone is formed parallel to the mandible, without a gap.
Gap type—new bone is formed parallel to the mandible, separated by a gap.
Irregular type—new bone is formed with an irregular shape.
Defined as multiple distinct hypodense areas within dense sclerotic bone:
(−): No mixed-type osteosclerosis.
(+): Mixed-type osteosclerosis observed.
Characterized by an expansile lytic lesion containing a dense central sequestrum, resembling a “bone-within-bone” pattern:
(−): No bone-within-bone appearance.
(+): Bone-within-bone appearance observed.
Statistical analysis
Statistical analysis was performed using SPSS version 26.0. The frequency of each CT finding was described, and correlations between imaging findings and clinical factors were evaluated. The chi-square test or Mann–Whitney U test was used to compare the distribution of each variable between groups. Associations between CT findings and treatment outcomes were assessed using the chi-square test, with cases classified as cured if all symptoms had resolved and non-cured otherwise. We did not investigate the details of the treatment methods in this study, and therefore did not calculate healing rates according to treatment type. A two-sided p-value < 0.05 was considered statistically significant for all analyses.
Ethics
This study was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects issued by the Ministry of Health, Labor, and Welfare of Japan. The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Nagasaki University Hospital (approval number: 22080804). The IRB approved the use of an opt-out method via the websites of the participating hospitals and granted a waiver of individual informed consent, as permitted under the national ethical guidelines for non-invasive observational studies. All patient-identifiable information was removed prior to analysis.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hayashida, S. et al. Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: a multicenter retrospective study with propensity score matching analysis. J. Bone Min. Res. 32, 2022–2029. https://doi.org/10.1002/jbmr.3191 (2017).
Ruggiero, S. L. et al. American association of oral and maxillofacial surgeons position paper on medication-related osteonecrosis of the jaw–2014 update. J. Oral Maxillofac. Surg. 72, 1938–1956 (2014).
Ruggiero, S. L. et al. American association of oral and maxillofacial surgeons’ position paper on medication-related osteonecrosis of the jaws—2022 update. J. Oral Maxillofac. Surg. 80, 920–943. https://doi.org/10.1016/j.joms.2022.02.008 (2022).
Yoneda, T. et al. Antiresorptive agent-related osteonecrosis of the jaw: position paper 2017 of the Japanese allied committee on osteonecrosis of the jaw. J. Bone Min. Metab. 35, 6–19. https://doi.org/10.1007/s00774-016-0810-7 (2017).
Kojima, Y. et al. Clinical significance of periosteal reaction as a predictive factor for treatment outcome of medication-related osteonecrosis of the jaw. J. Bone Min. Metab. 37, 913–919. https://doi.org/10.1007/s00774-019-00994-1 (2019).
Soutome, S. et al. Effect of periosteal reaction in medication-related osteonecrosis of the jaw on treatment outcome after surgery. J. Bone Min. Metab. 39, 302–310. https://doi.org/10.1007/s00774-020-01154-6 (2021).
Soutome, S. et al. Periosteal reaction of medication-related osteonecrosis of the jaw (MRONJ): clinical significance and changes during Conservative therapy. Support Care Cancer. 29, 6361–6368. https://doi.org/10.1007/s00520-021-06214-9 (2021).
Suyama, K. et al. Bone resection methods in medication-related osteonecrosis of the jaw in the mandible: an investigation of 206 patients undergoing surgical treatment. J. Dent. Sci. 19, 1758–1769. https://doi.org/10.1016/j.jds.2023.10.007 (2024).
Otsuru, M. et al. Imaging findings and treatment outcomes of a rare subtype of medication-related osteonecrosis of the jaw. J. Bone Min. Metab. 40, 150–156. https://doi.org/10.1007/s00774-021-01267-6 (2022).
Sakamoto, Y., Sawada, S. & Kojima, Y. Medication-related osteonecrosis of the jaw without osteolysis on computed tomography: a retrospective and observational study. Sci. Rep. 13, 12890. https://doi.org/10.1038/s41598-023-39755-6 (2023).
Kojima, Y., Sawada, S. & Sakamoto, Y. Medication-related osteonecrosis of the lower jaw without osteolysis on computed tomography images. J. Bone Min. Metab. 42, 27–36. https://doi.org/10.1007/s00774-023-01484-1 (2024).
Ohnuma, M. et al. Potential relationship among CT and MRI imaging, histological findings, and treatment outcomes in patients with medication-related osteonecrosis of the jaw undergoing segmental mandibulectomy—a retrospective study. J. Dent. Sci. 20, 1523–1531. https://doi.org/10.1016/j.jds.2024.12.020 (2025).
Bedogni, A. et al. Italian position paper (SIPMO-SICMF) on medication-related osteonecrosis of the jaw (MRONJ). Oral Dis. 30, 3679–3709 (2024).
Morishita, K. et al. Relationship between drug holiday of the antiresorptive agents and surgical outcome of medication-related osteonecrosis of the jaw in osteoporosis patients. Sci. Rep. 12, 11545. https://doi.org/10.1038/s41598-022-15720-7h (2022).
Kün-Darbois, J. D. & Fauvel, F. Medication-related osteonecrosis and osteoradionecrosis of the jaws: update and current management. Morphologie 105, 170–187. https://doi.org/10.1016/j.morpho.2020.11.008 (2021).
Kojima, Y. et al. Factors exacerbating clinical symptoms and CT findings in patients with medication-related osteonecrosis of the jaw receiving Conservative therapy: a multicenter retrospective study of 53 cases. Int. J. Environ. Res. Public. Health. 19, 7854. https://doi.org/10.3390/ijerph19137854 (2022).
Okuyama, K. et al. Surgical strategy for medication-related osteonecrosis of the jaw (MRONJ) on maxilla: a multicenter retrospective study. J. Dent. Sci. 16, 885–890. https://doi.org/10.1016/j.jds.2020.12.007 (2021).
Otsuru, M. et al. A preliminary clinical study of segmental mandibulectomy on medication-related osteonecrosis of the jaw. J. Dent. Sci. 17, 444–450. https://doi.org/10.1016/j.jds.2021.07.029 (2022).
Sawada, S. et al. Treatment and outcome of maxillary sinusitis associated with maxillary medication-related osteonecrosis. J. Oral Maxillofac. Surg. Med. Pathol. 33, 408–415. https://doi.org/10.1016/j.ajoms.2021.01.012 (2021).
Fatterpekar, G. M. et al. Bone-within-bone appearance: a red flag for bisphosphonate-associated osteonecrosis of the jaw. J. Comput. Assist. Tomogr. 35, 553–556. https://doi.org/10.1097/RCT.0b013e318227a81d (2011).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology: M.O., M.U. Data curation, formal analysis, and investigation: K.O., T.H., Y.Y., E.K., N.U., S.S., S.R., M.U., H.N., K.I., E.I., S.Y., T.S., Y.M., Y.S., M.K., T.H., Y.K., T.K., M.S., A.T., M.U. Writing-original draft: M.O. Writing-review and editing: M.U. Supervision and project administration: M.U.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Institutional Review Board of Nagasaki University Hospital (approval number: 22080804) and was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Biological Research Involving Human Subjects issued by the Ministry of Health, Labor, and Welfare of Japan..
Patient consent statement
In accordance with Japanese law, individual informed consent was not required for this non-invasive observational study. All patient-identifiable information was removed, and an opt-out option was provided by publishing the research plan on the websites of the participating hospitals, as instructed by the Institutional Review Board of Nagasaki University Hospital.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Otsuru, M., Omori, K., Hasegawa, T. et al. A multicenter study of CT findings in medication-related osteonecrosis of the jaw. Sci Rep 15, 40152 (2025). https://doi.org/10.1038/s41598-025-23915-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-23915-x