Abstract
Breast cancer remains the most prevalent malignancy among women worldwide. Emerging evidence suggests that trace elements, particularly selenium (Se) and mercury (Hg), may contribute to breast cancer pathogenesis. This study aimed to evaluate whether variations in Se and Hg levels in biological matrices are associated with breast cancer stage, related hematological changes and mammographic density. A case–control study was conducted including 285 histologically confirmed breast cancer patients and 215 age-matched controls. Biological samples (scalp hair and blood) were analyzed via atomic absorption spectrometry. Normality was tested (Shapiro–Wilk); parametric (t test, ANOVA) or nonparametric (Mann–Whitney U test, Kruskal–Wallis) tests were applied accordingly, with Tukey/Dunn post hoc corrections. Compared with controls, breast cancer patients presented significantly lower Se levels and higher Hg levels across all stages. For example, the Se concentration in Stage IV hair was 0.25 µg/g (95% CI 0.23–0.27) and that in control hair was 1.59 µg/g (95% CI 1.54–1.64) (t = − 46.2, p < 0.001; Hedges g = − 5.12). The hair Hg concentration was 4.31 µg/g (95% CI 4.24–4.38) vs. 1.19 µg/g (95% CI 1.17–1.21) (t = 84.7, p < 0.001; Hedges g = + 7.05). The blood Se concentration decreased progressively from 220.0 ± 8.2 µg/L in the controls to 51.3 ± 5.8 µg/L in Stage IV (p < 0.001), whereas the blood Hg concentration rose from 0.97 ± 0.05 to 2.94 ± 0.11 µg/L (p < 0.001). Hemoglobin levels also decreased with stage (12.7 ± 1.2 g/dL for controls vs. 5.62 ± 0.38 g/dL for Stage IV patients, p < 0.001). These findings demonstrate a consistent association between low Se and high Hg levels and advanced breast cancer stage and hematological decline. Notably, Se levels fell below the 70 µg/L GPx3 sufficiency threshold, whereas hair Hg levels exceeded the 2 µg/g toxicological guidance threshold, underscoring the clinical relevance of Se. While causal inference is limited, these results suggest that Se and Hg imbalances may serve as biomarkers for progression. These findings should be interpreted in light of international data where Se deficiency is rare, highlighting population-specific risks.
Similar content being viewed by others
Introduction
Breast cancer is the most commonly diagnosed malignancy among women worldwide and represents a growing global public health concern, especially in low- and middle-income countries. In 2020, it accounted for approximately 2.3 million new cases and 685,000 deaths, with projections indicating a continued increase in incidence by 2040 (World Health Organization, 2023)1. This global increase reflects demographic shifts, changes in reproductive behavior, and heightened exposure to environmental and lifestyle-related risk factors.
In Pakistan, breast cancer is the most prevalent cancer among women, accounting for 34.6% of all female malignancies and the highest incidence rate in Asia2. Projections estimate a 60.7% increase in the number of breast cancer cases in Karachi by 2025 compared with 2015, with an alarming 130.6% increase anticipated among women aged 30–34 years3,4. This trend is driven by a complex interplay of demographic expansion, genetic predisposition, and socioeconomic barriers to early detection and treatment.
In the Pakistani population, significant risk factors include advanced age, early onset of menarche, nulliparity, obesity, physical inactivity, and low socioeconomic status5,6. Genetic predispositions, such as BRCA mutations and high rates of consanguinity, further contribute to the disease burden, yet a significant portion of familial risk remains unexplained7. Socioeconomic and cultural determinants, particularly stigma, limited awareness, and inadequate access to diagnostic services, significantly contribute to late-stage presentation and elevated mortality rates6.
Mammographic density (MD), defined as the proportion of fibroglandular to fatty tissue in the breast, is both a major risk factor and barrier to detection. A high MD is associated with a four- to sixfold increase in breast cancer risk8,9 and reduces mammographic sensitivity from 85% in fatty breasts to less than 60% in extremely dense breasts10,11,12,13. This “masking effect” leads to delayed diagnosis14,15,16. This reduced sensitivity complicates screening accuracy and treatment planning.
The prevalence of high MD is notably elevated among Pakistani women. One study reported that 56.9% of women had BI-RADS category 3 or 4 density17, whereas another reported a 62.4% prevalence among women under 45 years of age18. Among patients with breast cancer, 76.7% were classified as BI-RADS category B or C19. Risk factors for high MD include younger age, lower BMI, hormonal exposure, and a history of benign breast disease20,21,22. Biologically, a high MD reflects an abundance of stromal and epithelial tissue, which can promote tumorigenesis through mechanical stiffness, collagen deposition, and a proinflammatory microenvironment23,24. Inflammatory mediators such as MCP-1, TNF-α, and TGF-β are elevated in dense breast tissue, potentially contributing to local immune activation and DNA damage25. Genetic factors, such as polymorphisms in estrogen metabolism and inflammatory pathways, are also implicated in regulating MD26.
Environmental and trace elements have been investigated in relation to breast cancer. Se, an essential micronutrient, has antioxidant, anti-inflammatory, and antiproliferative effects and may modulate oxidative stress and estrogen signaling27,28,29,30, although these findings are context dependent. However, few studies have examined Se and Hg together in relation to breast cancer stage or mammographic characteristics. In contrast, Hg is a known toxicant capable of generating reactive oxygen species (ROS), inducing DNA damage, and disrupting endocrine signaling. Hg exposure has been associated with increased cancer risk, although data specific to breast cancer are still emerging31,32. A significant biological interaction occurs between Se and Hg, wherein Se can form biologically inert complexes with Hg, potentially neutralizing its toxicity33,34,35,36. This antagonism highlights the need to study these elements in tandem, especially in populations with elevated environmental exposure. Nevertheless, evidence from South Asia, particularly Pakistan, remains limited, and most available studies have focused solely on serum concentrations without assessing mammographic density or hematologic parameters. Se exerts its biological effects primarily through selenoproteins that maintain cellular redox homeostasis. In particular, glutathione peroxidase-4 (GPX4) detoxifies membrane lipid hydroperoxides and thereby restrains ferroptosis, a cell death program increasingly implicated in breast cancer biology37. Similarly, thioredoxin reductases (TrxR1/TrxR2) regenerate the thioredoxin system to support nucleotide synthesis and antioxidant defense38. In contrast, Hg binds with high affinity to selenol and thiol groups and directly inhibits these enzymes, most notably TrxR—thereby weakening peroxide detoxification and amplifying oxidative stress39. Furthermore, systemic selenium delivery depends on selenoprotein P (SELENOP) and its receptors LRP8/ApoER2 and megalin/LRP2; disruption of this axis diminishes selenoprotein activity40. Finally, because Hg can sequester Se in inert Hg–Se complexes, the Se: Hg balance is biologically relevant; however, a simple “>1:1 molar ratio” rule is an oversimplification and does not guarantee protection in humans41. Se and Hg interact through complex biochemical mechanisms that influence oxidative balance and detoxification. Mercury binds to selenol and thiol groups, inhibiting antioxidant enzymes such as thioredoxin reductase (TrxR) and glutathione peroxidase (GPx), whereas Se mitigates toxicity by forming inert Hg–Se complexes that promote excretion (Fig. 1).
Selenium–mercury antagonism relevant to this study (author-created). First, Hg can bind cysteine/selenocysteine sites in TrxR and GPx, reducing enzyme activity and antioxidant capacity. Second, Se can form inert Hg–Se complexes, supporting sequestration and excretion. Third, when the Se concentration is low, Hg tends to accumulate, and oxidative stress increases. Together, these interactions explain why the Se: Hg balance is biologically linked to our endpoints (stage, mammographic density, and hematology). Abbreviations: GPx = glutathione peroxidase; TrxR = thioredoxin reductase; Se = selenium; Hg = mercury; Sec = selenocysteine; GSH = reduced glutathione. Adopted from65.
Guided by this framework, we aimed to address these gaps. We measured Se and Hg in blood and scalp hair from women with breast cancer and age-matched healthy controls in Sindh, Pakistan, and evaluated associations with (i) clinical stage (T-I to T-IV), (ii) mammographic density (BI-RADS categories), and (iii) hematologic indices (hemoglobin, red blood cell [RBC] count, hematocrit, MCV, MCH, MCHC, ferritin, and TIBC). We hypothesized that lower Se and higher Hg would be associated with a more advanced stage, greater mammographic density, and less favorable hematologic profiles, which is consistent with impaired selenoenzyme activity and heightened oxidative stress.
Materials and procedures
Study design and ethics
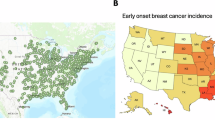
This case‒control study was conducted between 2021 and 2023 to evaluate the associations of Se and Hg concentrations in biological samples with breast cancer progression and mammographic density. A total of 285 histologically confirmed female breast cancer patients and 215 healthy age-matched women were recruited from hospitals and screening centers across Sindh Province (Fig. 2). Ethical approval for this study was obtained from the National Center of Excellence in Analytical Chemistry (NCEAC), University of Sindh. Written informed consent was obtained from all participants prior to inclusion. Certified hospital oncologists and radiologists performed the clinical evaluations, diagnoses, and imaging assessments, whereas the analytical procedures were conducted at the NCEAC laboratory.
Distribution of study participants and baseline characteristics. (a) Sample distribution showing the proportions of controls (n = 215) and patients with breast cancer (n = 285). (b) Tumor stage distribution among breast cancer patients (T-I to T-IV). (c) Comparison of the mean age (in years) between controls and breast cancer patients. (d) Comparison of the mean body mass index (BMI, kg/m²) between controls and breast cancer patients. The data are presented as the means ± SDs. p values were obtained via Welch’s t test.
Participants and sample size justification
An a priori power analysis (G*Power 3.1) assumed two-group mean differences (independent samples, two-tailed), α = 0.05, power (1 − β) = 0.80, and effect sizes in the medium–large range (Cohen’s d ≈ 0.5–0.8) reported for Se/Hg contrasts in oncology cohorts. Under these assumptions, ≥ 200 participants per group were needed. The final analytic sample (patients = 285; controls = 215) exceeded this threshold, providing ≥ 80% power to detect stagewise differences in elemental and hematologic indices.
Inclusion and exclusion criteria
Women aged 35–79 years with a histologically confirmed diagnosis of breast cancer and no mineral supplementation within the preceding 3.5 months were eligible for the patient group. Healthy women of similar age and regional background with no history of cancer or chronic illness were selected as controls. The exclusion criteria included prior chemotherapy, radiotherapy, or hormonal therapy; coexisting chronic disease (e.g., renal, hepatic, or autoimmune); prior malignancy; or incomplete clinical or biospecimen data.
Sample collection and Preparation
Scalp hair and venous blood samples were collected from participants following a detailed protocol from previous studies29,42,43,44,45,46,47,48,49,50,51. The samples were stored at -20 °C to prevent metal contamination. For biochemical analyses, 4–5 mL of venous blood was used following standard procedures52. Hair samples from the occipital region were washed with nonionic detergent and deionized water and oven dried. Blood was drawn via acid-washed polypropylene tubes to minimize contamination. The apparatus used was based on methodologies from previous studies42,44,51. A Milestone microwave oven (model Rotar MPR-300/12S) and Hitachi model 180–50 were used for the measurements, and the parameters are listed in Supplementary Table S1. Sample preparation was performed in a Pel microwave oven (model PMO23), and the solutions were stored in acid-washed PTFE containers.
Trace element analysis
Selenium and mercury levels were measured via atomic absorption spectrometry (AAS). Selenium was determined via graphite furnace AAS (PerkinElmer AAnalyst 700), whereas mercury was quantified via cold vapor AAS via a Hydride Generation System HGA-900. Calibration was performed with certified multielement standard solutions. All reagents were of analytical grade and procured from Merck and Sigma‒Aldrich.
Clinical evaluation and staging
Cancer staging was performed according to the American Joint Committee on Cancer (AJCC) TNM classification, which is based on tumor size, lymph node involvement, and metastasis. Patients were grouped into four clinical stages: T-I, T-II, T-III, and T-IV. Imaging techniques such as mammography, CT scans, ultrasound, and positron emission tomography (PET) were used for diagnostic confirmation. Mammographic density was classified via the Breast Imaging Reporting and Data System (BI-RADS), with dense breast tissue considered a risk factor for delayed tumor detection. Hospital oncologists and radiologists completed diagnostic procedures and imaging interpretations; the research team analyzed the anonymized clinical reports and elemental data.
Hematological and biochemical analysis
Hematological parameters, including hemoglobin (Hb), red blood cell count (RBC), hematocrit (HCT), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), and white blood cell (WBC) count, were measured via an automated hematology analyzer. Iron-related markers, including serum ferritin and total iron-binding capacity (TIBC), were assessed via standard immunoassay and colorimetric methods.
Statistical analysis
Group-level summary statistics (means, SDs, n) were calculated, and each cancer stage (T-I–T-IV) was compared with that of controls via Welch’s t tests. We reported the mean difference (Δ), t statistics, degrees of freedom (df), two-sided p value, 95% confidence interval (CI) for Δ, and effect sizes (Cohen’s d and Hedges’ g). The false discovery rate within analytic families (elements and hematology) was controlled via the Benjamini–Hochberg procedure. Group mean ± SD plots and stage-coded scatterplots were generated. All analyses were conducted via SPSS v25 and Python (scipy/statsmodels), with α = 0.05.
Results
Patient demographics and clinical characteristics
We analyzed 285 female breast cancer patients and 215 age-matched healthy controls (Fig. 2). The mean age of the patients was 51.7 ± 9.4 years, whereas that of the controls was 50.8 ± 8.9 years (t = 0.81, p = 0.42, 95% CI − 0.9 to 2.7; Hedges g = 0.10). The tumor stages were T-I (n = 25, 8.8%), T-II (n = 38, 13.3%), T-III (n = 105, 36.8%), and T-IV (n = 117, 41.1%) (Fig. 2). More than 60% of early-stage patients (T-I/T-II) had dense breasts (BI-RADS c/d), which is consistent with reduced screening sensitivity and delayed detection (Supplementary Figure S1). The clinical presentation evolves with stage painless lumps in early disease and nipple retraction/skin dimpling/palpable lymphadenopathy in advanced stages (Supplementary Figure S2). The diagnoses are confirmed by FNAC and/or core biopsy with multimodal imaging (ultrasound, mammography, CT; Supplementary Figure S3).
Elemental analysis of selenium and mercury
We compared the Se and Hg concentrations in the scalp hair and blood of healthy controls and breast cancer patients across stages T-I to T-IV (Fig. 3; Table 1). In the controls, the Se concentration was 1.59 ± 0.29 µg/g in the hair and 220.0 ± 8.19 µg/L in the blood, whereas the Hg concentration was 1.19 ± 0.09 µg/g in the hair and 0.97 ± 0.05 µg/L in the blood. In contrast, patients exhibited a stage-related decline in Se and a concomitant increase in Hg. In stage T-I, the Se concentration decreased to 0.45 ± 0.09 µg/g in hair and 125.1 ± 5.35 µg/L in blood, whereas the Hg concentration increased to 2.85 ± 0.21 µg/g in hair and 2.15 ± 0.35 µg/L in blood. By stage T-IV, Se reached 0.25 ± 0.01 µg/g in hair and 51.3 ± 5.75 µg/L in blood, whereas Hg rose to 4.31 ± 0.15 µg/g in hair and 2.94 ± 0.11 µg/L in blood. These stagewise patterns are displayed in Fig. 3 and summarized in Supplementary Table S2.
Se and Hg levels in blood and scalp hair across clinical stages of breast cancer. (A) Blood Se; (B) Blood Hg; (C) Hair Se; (D) Hair Hg. The bars represent the means ± SDs for controls and patients with stage T-I to T-IV breast cancer. The dashed reference lines indicate functional or toxicological thresholds (70 µg/L = GPx3 sufficiency; 100–120 µg/L = SELENOP zone; 2 µg/g = Hg guidance). The data show progressive Se depletion and Hg elevation with advancing stage. The dashed reference lines indicate commonly cited levels: blood Se 70 µg/L (approximately GPx3 sufficiency), 100–120 µg/L (SELENOP saturation), and hair Hg 2 µg/g (population guidance)55,57,66.
Inferential comparisons (Table 1) confirmed that these differences were statistically significant and large in magnitude. Compared with that in control hair, Se was lower by − 1.34 µg/g (95% CI − 1.399–−1.281; Welch’s t ≈ − 45.2; p = 1.78 × 10⁻⁶⁶; Hedges g = − 5.05), whereas Hg was greater by + 3.12 µg/g (95% CI 3.05–3.19; t ≈ 91.8; p = 2.88 × 10⁻³¹; Hedges g = + 30.1). Comparable stage-versus-control results for T-I, T-II, and T-III patients are provided in Table 1 and Supplementary Table S2, and all comparisons remained significant after false discovery rate adjustment.
From a clinical perspective, blood Se in advanced disease patients (T-III/T-IV) falls within or below the functional sufficiency range of approximately 70–120 µg/L, which is consistent with potential impairment of selenoprotein activity. In parallel, hair Hg exceeded the 2 µg/g guidance level across all cancer stages, indicating elevated exposure or accumulation. Taken together, these findings clearly reveal a shift toward selenium deficiency and mercury overload with advancement. Consistent with this pattern, the scatterplots in Fig. 4 illustrate a pronounced inverse relationship between Se and Hg across matrices, which is most evident in the higher stages.
Stagewise correlation between selenium and mercury levels in breast cancer patients. Scatter plots showing selenium vs. mercury concentrations in (a) blood (µg/L) and (b) scalp hair (µg/g), color-coded by disease stage (Controls, T-I, T-II, T-III, T-IV). A strong inverse pattern is evident, particularly in advanced-stage patients, supporting antagonistic interactions between these trace elements.
Hematological and iron-related parameters
Compared with controls, patients with breast cancer presented substantial abnormalities in hematologic indices (Fig. 5; Table 2; Supplementary Table S3). Hemoglobin decreased from 12.7 ± 1.21 g/dL in the controls to 5.62 ± 0.38 g/dL in stages T-IV (Δ = −7.08 g/dL; Welch’s t = − 78.94; df = 281.5; p < 1 × 10⁻¹⁶; Hedges g = − 7.06). Red blood cells declined from 4.02 ± 0.30 × 10¹²/L to 1.35 ± 0.17 × 10¹²/L (Δ = −2.67 × 10¹²/L; t = − 103.49; df = 329.4; p < 1 × 10⁻¹⁶; g = − 10.18). Additional measures decreased progressively with stage: hematocrit from 41.9 ± 1.05% to 17.9 ± 1.26%, mean corpuscular volume from 93.6 ± 1.45 fL to 58.5 ± 1.99 fL, mean corpuscular hemoglobin from 30.7 ± 0.62 pg to 11.9 ± 0.98 pg, and mean corpuscular hemoglobin concentration from 34.8 ± 0.59 g/dL to 16.5 ± 1.51 g/dL (all p < 1 × 10⁻¹⁶, with large effect sizes; Table 2) In contrast, the levels of iron-related markers increased from 53.9 ± 5.15 ng/mL to 165.0 ± 7.41 ng/mL (Δ = +111.1 ng/mL; t = 144.31; df = 178.3; p < 1 × 10⁻¹⁶; g = 18.35), and the total iron-binding capacity increased from 293.0 ± 9.52 µg/100 mL to 685.0 ± 26.9 µg/100 mL (Δ = +392.0 µg/100 mL; t = 152.51; df = 132.0; p < 1 × 10⁻¹⁶; g = 22.10) (Table 2). All stage-versus-control comparisons remained significant after false discovery rate adjustment. From a clinical perspective, these findings indicate that progressively severe, inflammation-associated, iron-restricted anemia worsens with advancing disease stage.
Hematological and iron metabolism parameters in breast cancer patients versus controls. (A) Hemoglobin (Hb), (B) red blood cell count (RBC), (C) serum ferritin, and (D) total iron-binding capacity (TIBC) are shown as the means ± SDs for controls and patients with breast cancer stratified by stage (T-I to T-IV). The normal physiological ranges are shaded in light color bands (Hb: 12–15 g/dL; RBC: 3.8–4.8 × 10¹²/L; ferritin: 30–150 ng/mL; TIBC: 250–450 µg/100 mL). Hematological indices decreased with advancing stage, whereas ferritin and TIBC increased, which is consistent with inflammation-associated iron-restricted erythropoiesis.
Frequency and extent of axillary lymph node metastases in female patients with breast cancer on the basis of pathological evaluation
Supplementary Table S4 summarizes multimodal findings relevant to axillary lymph node (ALN) involvement, including mammography, core biopsy pathology, and cross-sectional and nuclear imaging. On mammography, the background parenchyma was predominantly fatty/glandular. A suspicious soft-tissue density in the upper-outer quadrant of the right breast, with associated enlarged axillary lymph nodes, was assessed as BI-RADS 4, prompting core needle (tru-cut) biopsy. Core biopsy confirmed invasive (infiltrating) ductal carcinoma, with minimal tubular formation (3/3), marked nuclear pleomorphism (3/3), and numerous mitoses (3/3). Lymphocytic infiltration, fibrosis, and desmoplastic stroma were present, and the grade was assigned according to the Nottingham (Bloom–Richardson) system. Contrast-enhanced CT revealed heterogeneously enhancing right-breast mass with spiculated margins, architectural distortion, skin thickening, and nipple retraction. Right axillary lymphadenopathy was present (largest node ~ 1.4 cm with loss of fatty hilum), which was consistent with metastatic ALN involvement. Abdominal ultrasound revealed a large complex lesion (13.0 × 12.7 cm) in the umbilical/hypogastric region suspicious for a mesenteric mass; this finding was nonbreast and was documented for completeness. Skeletal scintigraphy (Tc-99 m MDP) revealed focal uptake in the skull requiring correlation and background degenerative changes in the dorsolumbar spine and peripheral joints. Collectively, the imaging and pathology findings support locoregional disease with metastatic right axillary lymphadenopathy and highlight the utility of integrated diagnostic assessment (mammography, histopathology, cross-sectional imaging, and nuclear medicine) in staging and treatment planning (Supplementary Table S4). From a clinical perspective, the concordant evidence of invasive ductal carcinoma with pathologic‒radiologic signs of axillary node involvement favors management along a node-positive pathway (systemic therapy consideration, targeted axillary staging, and individualized locoregional control), whereas nonbreast incidental findings (degenerative changes, possible mesenteric mass) should be correlated separately to avoid confounding breast-specific staging.
Discussion
In this case–control study, we observed a clear stage-related imbalance in trace elements among women with breast cancer. Selenium (Se) levels were progressively lower, and mercury (Hg) levels were markedly higher from stage T-I to T-IV compared with healthy controls, in both blood and scalp hair samples. This trend was consistent across all comparisons and remained statistically significant after correction for multiple testing. These results suggest that breast cancer progression is associated with increasing oxidative stress and reduced antioxidant defense, driven by the opposing biological roles of Se and Hg. Selenium is an essential trace element that supports antioxidant defense and redox balance through its role in selenoproteins, including glutathione peroxidases (GPx) and thioredoxin reductases (TrxR)53,54. These enzymes prevent oxidative damage to lipids, proteins, and DNA, which is crucial for maintaining cellular homeostasis and preventing malignant transformation. Mercury, in contrast, is a toxic heavy metal that binds to selenol and thiol groups in proteins, thereby inhibiting GPx and TrxR activities and increasing reactive oxygen species (ROS) production39. The mechanistic relationship between these elements is illustrated in Fig. 1. Mercury not only inhibits Se-dependent enzymes but also forms stable Hg–Se complexes, such as mercury selenide (HgSe), which reduce mercury toxicity and enhance its excretion. When Se is insufficient, this detoxification pathway becomes less effective, allowing Hg to accumulate in tissues. Thus, Se deficiency may intensify mercury-induced oxidative stress, while Hg exposure may further deplete functional Se reserves, creating a vicious cycle that contributes to cancer progression55. Our statistical findings support these mechanisms. Hair Se decreased from 1.59 µg/g in controls to 0.25 µg/g in stage T-IV patients, while hair Hg increased from 1.19 µg/g to 4.31 µg/g. Similarly, blood Se dropped from 220 µg/L to 51.3 µg/L, and blood Hg rose from 0.97 µg/L to 2.94 µg/L. These large and consistent differences (p < 0.0001; Hedges g > 2 for Se, > 10 for Hg) show a robust association between Se–Hg imbalance and disease severity. The inverse Se–Hg trend observed in both matrices supports the hypothesis that the two elements are biochemically linked and jointly influence redox homeostasis55,56,57. Hematologic parameters also changed significantly with cancer stage. Patients with T-III and T-IV disease had lower hemoglobin and red-cell indices and higher ferritin and TIBC levels than controls, consistent with inflammation-associated, iron-restricted erythropoiesis58. This pattern suggests a systemic response to chronic oxidative stress and inflammation, which are known to suppress erythropoietin production and iron availability. Such anemia contributes to fatigue, poor functional status, and reduced quality of life in advanced breast cancer patients59. The biological plausibility of these findings is further supported by previous studies showing that Hg interferes with antioxidant and immune functions, while adequate Se levels help maintain redox balance and immune competence39,54. Population studies have also reported that Se status varies widely across regions depending on soil content, diet, and supplementation policies. For instance, Se deficiency is common in some parts of China and Eastern Europe, while intake is generally adequate in North America60,61. Conversely, mercury exposure is more frequent in coastal and riverine communities that rely heavily on seafood or engage in artisanal gold mining62,63. These global differences make it difficult to establish universal Se/Hg thresholds for cancer prevention or management. Recent clinical reports also note that overt Se deficiency can be uncommon during therapy and that supplementation may risk overdosing without monitoring64. Differences in timing (pretreatment vs. on-treatment), background exposure, and matrices (hair vs. serum/plasma) may explain various observations. In our study, advanced-stage means fell at or below functional sufficiency, whereas controls were high, supporting context-specific monitoring rather than routine supplementation. Clinically, many patients with advanced disease in our study had Se concentrations at or below the lower functional range (~ 70 µg/L) and hair Hg values above the WHO/UNEP guidance limit of 2 µg/g55. Although this study does not propose definitive diagnostic cut-offs, these levels could serve as practical indicators for closer monitoring, dietary counseling, and environmental exposure assessment. Integrating trace element testing with routine hematology and imaging may improve risk stratification, particularly in low-resource settings where late-stage presentation is common.
Future research should include prospective cohorts and interventional studies that measure dietary intake, exposure sources, and functional selenoprotein activity (e.g., GPX4, TrxR)37,40. Mechanistic studies on ferroptosis and oxidative signaling could clarify whether the Se–Hg imbalance contributes directly to cancer progression. Clinical trials assessing controlled Se supplementation and Hg reduction strategies, with biochemical monitoring, may help determine whether modifying these exposures improves outcomes.
In summary, this study provides evidence of a strong stage-related Se–Hg imbalance in women with breast cancer, supported by both statistical and biological findings. Selenium depletion and mercury accumulation appear to worsen with disease progression, possibly through redox disruption and enzyme inhibition. These results highlight the importance of integrating environmental and nutritional assessments into breast cancer prevention and management, particularly in regions with low Se intake or high Hg exposure.
Limitations and implications
This study has several limitations. First, the case–control design cannot establish causation or the timing of exposure relative to disease development. Second, detailed individual data on diet (including fish intake), environmental exposure, and mercury speciation were not available; therefore, residual confounding may remain, and full multivariable adjustment was not possible. Third, blood and hair samples represent different exposure periods and mercury forms, which limits direct comparison between them. Fourth, the hospital-based sample from a single region may limit generalizability to other populations. Fifth, functional biomarkers such as selenoprotein activity (e.g., GPX4, TrxR) and ferroptosis markers were not measured, which restricts mechanistic interpretation. Finally, the clinical thresholds discussed here should be considered indicative reference points rather than diagnostic cut-offs until validated in prospective studies.
Future research should include prospective cohort studies with standardized exposure assessments, including dietary intake, fish consumption, and mercury speciation. Adjusted regression or survival models are needed to identify independent associations, and validation studies (e.g., ROC analysis) should test whether blood Se < 70 µg/L and hair Hg > 2 µg/g can improve risk prediction. Mechanistic investigations measuring selenoprotein activity and ferroptosis pathways, along with carefully designed interventions to optimize Se status and reduce Hg exposure, may help determine whether modifying these factors can improve patient outcomes.
Conclusions
In this case-control study, Se levels decreased while mercury Hg levels increased from stage T-I to T-IV in blood and scalp hair, accompanied by progressive anemia with lower hemoglobin and RBC indices, and higher ferritin/TIBC. The findings suggest lower Se may reduce antioxidant defenses, while higher Hg increases toxic stress, though remaining associative. Blood Se levels within 70–120 µg/L and hair Hg above 2 µg/g may indicate need for follow-up, counseling, and supportive care. Prospective studies should confirm these thresholds and test whether improving Se status and reducing Hg exposure improve outcomes.
Data availability
This manuscript is currently available as a preprint on Research Square with the DOI: https://doi.org/10.21203/rs.3.rs-3469503/v1. Please note that the preprint has not undergone formal peer review by a journal. The work is licensed under a CC BY 4.0 License and has gained attention within the scientific community.
References
Sedeta, E. T., Jobre, B. & Avezbakiyev, B. Breast cancer: Global patterns of incidence, mortality, and trends. JCO. 41 (16_suppl), 10528–10528 https://doi.org/10.1200/JCO.2023.41.16_suppl.10528 (2023).
Khalid, S. et al. Epidemiology and risk factors of breast cancer: a global perspective on incidence, mortality, and prevention strategies, Biol. Clin. Sci. Res. J. 2024 (1), 1465 https://doi.org/10.54112/bcsrj.v2024i1.1465 (2024).
Zaheer, R. & Fatima, K. Health education in preventing breast cancer among rural women of pakistan: A Quasi-Experimental study. PJPH 12 (3), 132–136. https://doi.org/10.32413/pjph.v12i3.1043 (2022).
Zaheer, S., Shah, N., Maqbool, S. A. & Soomro, N. M. Estimates of past and future time trends in age-specific breast cancer incidence among women in Karachi, pakistan: 2004–2025. BMC Public. Health. 19 (1), 1001. https://doi.org/10.1186/s12889-019-7330-z (2019).
Asif, H. M. et al. Prevalence, risk factors and disease knowledge of breast cancer in Pakistan. Asian Pac. J. Cancer Prev. 15 (11), 4411–4416. https://doi.org/10.7314/APJCP.2014.15.11.4411 (2014).
Ullah Khan, N., Khan, B. M., Azam, I. & Hayat, A. Current situation of breast cancer in Pakistan and the dire need of early diagnosis. CTO 4 (2), 01–17. https://doi.org/10.32350/cto.42.01 (2024).
Shaukat, U., Ismail, M. & Mehmood, N. Epidemiology, major risk factors and genetic predisposition for breast cancer in the Pakistani population. Asian Pac. J. Cancer Prev. 14 (10), 5625–5629. https://doi.org/10.7314/apjcp.2013.14.10.5625 (2013).
Lynge, E., Vejborg, I., Andersen, Z., von Euler-Chelpin, M. & Napolitano, G. Mammographic density and screening sensitivity, breast cancer incidence and associated risk factors in Danish breast cancer screening. J. Clin. Med. 8 (11). https://doi.org/10.3390/jcm8112021 (2019).
Harvey, J. A. & Bovbjerg, V. E. Quantitative assessment of mammographic breast density: relationship with breast cancer risk. Radiology 230 (1), 29–41. https://doi.org/10.1148/radiol.2301020870 (2004).
Rainey, L. et al. The impact of alcohol consumption and physical activity on breast cancer: the role of breast cancer risk. Int. J. Cancer. 147 (4), 931–939. https://doi.org/10.1002/ijc.32846 (2020).
Yaghjyan, L., Colditz, G. A. & Wolin, K. Physical activity and mammographic breast density: a systematic review. Breast Cancer Res. Treat. 135 (2), 367–380. https://doi.org/10.1007/s10549-012-2152-z (2012).
Mathur, A. & Taurin, S. What influence does mammographic density have on breast cancer occurrence? Expert Rev. Anticancer Ther. 22 (5), 445–447. https://doi.org/10.1080/14737140.2022.2065985 (2022).
Tajerian, M. N. et al. Artemisia: validation of a deep learning model for automatic breast density categorization. J. Med. Artif. Intell. 4, 5–5. https://doi.org/10.21037/jmai-20-43 (2021).
Ahern, T. P. et al. Lifestyle, behavioral, and dietary risk factors in relation to mammographic breast density in women at high risk for breast cancer. Cancer Epidemiol. Biomarkers Prev. 30 (5), 936–944. https://doi.org/10.1158/1055-9965.EPI-20-1567 (2021).
Vachon, C. M., Kuni, C. C., Anderson, K., Anderson, V. E. & Sellers, T. A. Association of mammographically defined percent breast density with epidemiologic risk factors for breast cancer (United States). Cancer Causes Control. 11 (7), 653–662. https://doi.org/10.1023/a:1008926607428 (2000).
Colin, C., Prince, V. & Valette, P. J. Can mammographic assessments lead to consider density as a risk factor for breast cancer? Eur. J. Radiol. 82 (3), 404–411. https://doi.org/10.1016/j.ejrad.2010.01.001 (2013).
Fatima, K., Mohsin, F., Rao, M. O. & Alvi, M. I. Mammographic breast density in Pakistani Women, factors affecting It, and Inter-Observer variability in assessment. Cureus 13 (3), e14050. https://doi.org/10.7759/cureus.14050 (2021).
Shamsi, U., Afzal, S., Shamsi, A., Azam, I. & Callen, D. Factors associated with mammographic breast density among women in Karachi Pakistan. BMC Womens Health. 21 (1), 438. https://doi.org/10.1186/s12905-021-01538-4 (2021).
Sajjad, B. et al. Correlation of breast density grade on mammogram with diagnosed breast cancer: A retrospective Cross-Sectional study. Cureus 14 (7), e27028. https://doi.org/10.7759/cureus.27028 (2022).
Johansson, A. et al. Characterization of benign breast diseases and association with age, hormonal factors, and family history of breast cancer among women in Sweden. JAMA Netw. Open. 4 (6), e2114716. https://doi.org/10.1001/jamanetworkopen.2021.14716 (2021).
Rice, M. S. et al. Mammographic density and breast cancer risk: a mediation analysis. Breast Cancer Res. 18 (1), 94. https://doi.org/10.1186/s13058-016-0750-0 (2016).
Schnitt, S. J. Benign breast disease and breast cancer risk: morphology and beyond. Am. J. Surg. Pathol. 27, 836–841. https://doi.org/10.1097/00000478-200306000-00017 (2003).
Huo, C. W. et al. High mammographic density is associated with an increase in stromal collagen and immune cells within the mammary epithelium. Breast Cancer Res. 17 (1), 79. https://doi.org/10.1186/s13058-015-0592-1 (2015).
Archer, M., Dasari, P., Evdokiou, A. & Ingman, W. V. Biological mechanisms and therapeutic opportunities in mammographic density and breast cancer risk. Cancers (Basel). 13 (21). https://doi.org/10.3390/cancers13215391 (2021).
Ironside, A. J. & Jones, J. L. Stromal characteristics May hold the key to mammographic density: the evidence to date. Oncotarget 7 (21), 31550–31562. https://doi.org/10.18632/oncotarget.6912 (2016).
Pettersson, A. & Tamimi, R. M. Breast density and breast cancer risk: Understanding of biology and risk. Curr. Epidemiol. Rep. 1 (3), 120–129. https://doi.org/10.1007/s40471-014-0018-0 (2014).
Demircan, K. et al. Matched analysis of Circulating selenium with the breast cancer selenotranscriptome: a multicentre prospective study. J. Transl Med. 21 (1), 658. https://doi.org/10.1186/s12967-023-04502-y (2023).
Irum Khalid, T. H. J. In-Silico Identification of Anticancer Compounds; Ligand-Based Pharmacophore Approach against EGFR Involved in Breast Cancer. Advances in Breast Cancer Research. 10, 120–132 (2021).
Unar, A. & Chanihoon, G. Q. Correlations between environmental enteropathy and anemia in pediatric patients under five years: an investigation of lead exposure. Res. Sq. https://doi.org/10.21203/rs.3.rs-3446865/v1 (2023).
Chanihoon, G. Q., Afridi, H. I., Talpur, F. N., Kazi, T. G. & Baig, J. A. Interaction between essential (zn) and toxic (cd) elements in different stages of female breast cancer patients, resident in different cities of sindh, Pakistan. Biol. Trace Elem. Res. 200 (3), 1117–1126. https://doi.org/10.1007/s12011-021-02757-4 (2022).
Coradduzza, D. et al. Heavy metals in biological samples of cancer patients: a systematic literature review. Biometals. 37 (4), 803–817 https://doi.org/10.1007/s10534-024-00583-4 (2024).
Florea, A. M. & Büsselberg, D. Metals and breast cancer: risk factors or healing agents? J. Toxicol. 2011, 159619 https://doi.org/10.1155/2011/159619 (2011).
Castriotta, L. et al. The role of mercury, selenium and the Se-Hg antagonism on cognitive neurodevelopment: A 40-month follow-up of the Italian mother-child PHIME cohort. Int. J. Hyg. Environ. Health. 230, 113604. https://doi.org/10.1016/j.ijheh.2020.113604 (2020).
Fenga, C. Occupational exposure and risk of breast cancer. Biomed. Rep. 4 (3), 282–292. https://doi.org/10.3892/br.2016.575 (2016).
Wolff, M. S. & Toniolo, P. G. Environmental organochlorine exposure as a potential etiologic factor in breast cancer. Environ. Health Perspect. 103 (Suppl 7), 141–145. https://doi.org/10.1289/ehp.95103s7141 (1995).
Wolff, M. S. & Weston, A. Breast cancer risk and environmental exposures. Environ. Health Perspect. 105 (Suppl 4), 891–896. https://doi.org/10.1289/ehp.97105s4891 (1997).
Ge, A. et al. Mechanism of ferroptosis in breast cancer and research progress of natural compounds regulating ferroptosis. J. Cell. Mol. Med. 28 (1), e18044. https://doi.org/10.1111/jcmm.18044 (2024).
DeAngelo, S. L., Győrffy, B., Koutmos, M. & Shah, Y. M. Selenoproteins and tRNA-Sec: regulators of cancer redox homeostasis. Trends Cancer. 9 (12), 1006–1018. https://doi.org/10.1016/j.trecan.2023.08.003 (2023).
Pires, V., Bramatti, I., Aschner, M., Branco, V. & Carvalho, C. Thioredoxin reductase inhibitors as potential antitumors: mercury compounds efficacy in glioma cells. Front. Mol. Biosci. 9, 889971. https://doi.org/10.3389/fmolb.2022.889971 (2022).
Saito, Y. Selenium transport mechanism via Selenoprotein P-Its physiological role and related diseases. Front. Nutr. 8, 685517. https://doi.org/10.3389/fnut.2021.685517 (2021).
Tinggi, U. & Perkins, A. V. Selenium status: its interactions with dietary mercury exposure and implications in human health. Nutrients 14 (24). https://doi.org/10.3390/nu14245308 (2022).
Unar, A., Afridi, H. I., Ali, A., Ali, N. & Qureshi, T. Determination of electrolytes and trace elements in biological samples from patients with altered semen parameters: a correlational analysis. Biol. Trace Elem. Res. 203 (3), 1383–1394. https://doi.org/10.1007/s12011-024-04281-7 (2025).
Unar, A., Sahito, O. & Afridi, H. Determining the toxic elements in cannabinoid and opioid drugs and their impact on addicts’ health. Res. Sq. https://doi.org/10.21203/rs.3.rs-3565706/v1 (2023).
Unar, A. et al. Determination of toxic elements in cannabinoid and opioid drugs and their impact on addicts’ health: A comparative study. Biol. Trace Elem. Res. 202 (12), 5339–5347. https://doi.org/10.1007/s12011-024-04096-6 (2024).
Afridi, H. I. et al. Effect of lead on the skin and health of female dermatitis patients through cosmetics. Journal Ayub Med. Coll. Abbottabad-Pakistan 35, (1) 88–94.https://doi.org/10.55519/JAMC-01-11442 (2023).
Ning, J. et al. The importance of monitoring endocrine-disrupting chemicals and essential elements in biological samples of fertilizer industry workers. Environ. Res. 231 (Pt 2), 116173. https://doi.org/10.1016/j.envres.2023.116173 (2023).
Unar, A. et al. Mitigating marine hazardous contaminants: A sustainable management perspective. Chemosphere 338, 139292. https://doi.org/10.1016/j.chemosphere.2023.139292 (2023).
Chanihoon, G. Q. et al. Selenium and mercury concentrations in biological samples from patients with COVID-19. J. Trace Elem. Med. Biol. 73, 127038. https://doi.org/10.1016/j.jtemb.2022.127038 (2022).
Li, Y. et al. Environmental impact of endocrine-disrupting chemicals and heavy metals in biological samples of petrochemical industry workers with perspective management. Environ. Res. 231 (Pt 2), 115913. https://doi.org/10.1016/j.envres.2023.115913 (2023).
Chanihoon, G. Q. et al. Determination of enzyme Q10 level in Pakistani female patients with breast cancer. Chin. J. Anal. Chem. 50 (3), 100061. https://doi.org/10.1016/j.cjac.2022.100061 (2022).
Chanihoon, G. Q. et al. Determining the level of essential elements in patients with ewing sarcoma: A correlation. Environ. Res. 211, 113035. https://doi.org/10.1016/j.envres.2022.113035 (2022).
Imran Afridi, Hassan et al. “Essential trace and toxic elemental concentrations in biological samples of male adult referent and Eunuch subjects.” Clinica chimica acta; international journal of clinical chemistry 529 96–103.https://doi.org/10.1016/j.cca.2022.02.010 (2022).
Mehdi, Y., Hornick, J. L., Istasse, L. & Dufrasne, I. Selenium in the environment, metabolism and involvement in body functions. Molecules. 18 (3), 3292–3311 https://doi.org/10.3390/molecules18033292 (2013).
Rayman, M. P. Selenium and human health. Lancet. 379 (9822), 1256–1268 https://doi.org/10.1016/S0140-6736(11)61452-9 (2012).
Hurst, R. et al. Establishing optimal selenium status: results of a randomized, double-blind, placebo-controlled trial. Am. J. Clin. Nutr. 91 (4), 923–931. https://doi.org/10.3945/ajcn.2009.28169 (2010).
Branco, V. et al. Impaired cross-talk between the thioredoxin and glutathione systems is related to ASK-1 mediated apoptosis in neuronal cells exposed to mercury. Redox Biol. 13, 278–287. https://doi.org/10.1016/j.redox.2017.05.024 (2017).
Alexander, J. & Olsen, A. K. Selenium - a scoping review for nordic nutrition recommendations 2023. Food Nutr. Res. 67 https://doi.org/10.29219/fnr.v67.10320 (2023).
Weiss, G. & Goodnough, L. T. Anemia of chronic disease. N Engl. J. Med. 352 (10), 1011–1023. https://doi.org/10.1056/NEJMra041809 (2005).
Cella, D., Lai, J. S., Chang, C. H., Peterman, A. & Slavin, M. Fatigue in cancer patients compared with fatigue in the general united States population. Cancer 94 (2), 528–538. https://doi.org/10.1002/cncr.10245 (2002).
Kieliszek, M., Bano, I. & Zare, H. A comprehensive review on selenium and its effects on human health and distribution in middle Eastern countries. Biol. Trace Elem. Res. 200 (3), 971–987. https://doi.org/10.1007/s12011-021-02716-z (2022).
Nuryanty, C. D., Riani, E., Abidin, Z., Sutjahjo, S. H. & Riyadi, A. Mercury use in the artisanal and small-scale gold mining from 2001 to 2021: a review. Toxicol. Environ. Chem. 106, 1–10. https://doi.org/10.1080/02772248.2024.2406188 (2024).
Gibb, H. & O’Leary, K. G. Mercury exposure and health impacts among individuals in the artisanal and small-scale gold mining community: a comprehensive review. Environ. Health Perspect. 122 (7), 667–672. https://doi.org/10.1289/ehp.1307864 (2014).
Donkor, A. K., Ghoveisi, H. & Bonzongo, J. C. J. Use of metallic mercury in artisanal gold mining by amalgamation: A review of Temporal and Spatial trends and environmental pollution. Minerals 14 (6), 555. https://doi.org/10.3390/min14060555 (2024).
Altmayer, L. A. et al. A plea for monitoring serum selenium levels in breast cancer patients: selenium deficiency is rare during the first year of Therapy, and selenium supplementation is associated with elevated risk of overdosing. Nutrients 16 (13). https://doi.org/10.3390/nu16132134 (2024).
Jorge, A. O. S. et al. Oct., Protection of selenium against methylmercury in the human body: A comprehensive review of biomolecular interactions, in IECBM 2024, Basel Switzerland, p. 8, (2024). https://doi.org/10.3390/blsf2024035008
United Nations Environment Programme. Guidance on monitoring of mercury and mercury compounds to support evaluation of the effectiveness of the Minamata Convention (UNEP/MC/COP.4/INF/12). (2021).
Acknowledgements
This project was funded by The Research Institute/ Center Supporting Program (RICSP-25-3), King Saud University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
All the authors contributed equally to this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the National Center of Excellence in Analytical Chemistry, University of Sindh, Jamshoro, for studies involving humans.
Informed consent Statement
Informed consent was obtained from all the subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Unar, A., Chanihoon, G.Q., Bashir, M.S. et al. Trace element imbalances in selenium and mercury in relation to mammographic density and breast cancer progression: a case‒control study. Sci Rep 15, 39173 (2025). https://doi.org/10.1038/s41598-025-24373-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-24373-1