Abstract
Cortisol, a key biomarker of hypothalamus–pituitary–adrenal (HPA) axis activity, is central to early stress regulation and neurodevelopment. While prior studies have linked maternal and infant cortisol to child outcomes, less is known about their synchrony during early infancy, a time of rapid neuroendocrine development. In this longitudinal study, we examined cortisol coupling and the correlation with maternal adverse childhood experiences (ACEs) in 305 mother–infant dyads from São Paulo, Brazil. Salivary cortisol was collected at ~ 1 month (32.3 days) and 6 months postpartum. We assessed intra- and interindividual cortisol dynamics and coupling using bivariate latent change score modeling. Maternal and infant cortisol were positively correlated at baseline (r = 0.319, p < 0.001) and at 6 months (r = 0.208, p = 0.003), suggesting early attunement that diminishes over time. Mothers and infants showed negative self-feedback, where higher baseline cortisol predicted smaller changes (mothers: B = -0.654; infants: B = -0.615; both p < 0.001). Maternal ACEs predicted elevated maternal cortisol at baseline (B = 0.126, p = 0.026) but did not affect the rate of change. These findings reveal early HPA synchrony and gradual decoupling, and highlight the lasting effects of maternal adversity on postpartum stress physiology.
Similar content being viewed by others
Introduction
Adverse childhood events (ACEs) encompass physical, sexual, and psychological abuse, neglect, poverty, and parental mental illness1 and have been robustly linked to long-term alterations in mental health and behavior2,3,4,5,6. These early life adversities initiate neurobiological cascades that contribute to both functional and structural changes in brain regions critical for emotion regulation and stress response, including the prefrontal cortex, amygdala, and hippocampus7,8,9,10,11. Such alterations may underlie the psycho-emotional vulnerabilities observed in individuals with high ACE exposure and shape physiological regulation across generations. Building on this framework, the current study investigates (1) whether maternal and infant cortisol levels are linked during early infancy and (2) whether maternal ACEs relate to postpartum cortisol regulation and mother–infant synchrony.
The effects of ACEs extend beyond the directly affected individual and can impact the next generation, resulting in the intergenerational transmission of trauma12,13,14,15,16. This transmission can be associated with offspring development from the gestational period through postpartum, increasing the risk of mental disorders and metabolic diseases, among other outcomes14,17,18. The mechanisms underlying the intergenerational transmission of trauma are diverse, including genetic, hormonal, intrauterine environment, and neurobiological alterations15,19,20.
The impacts of ACEs on the hypothalamic–pituitary–adrenal (HPA) axis, one of the body’s central stress-response systems, are well established21,22,23,24,25,26. The HPA axis orchestrates physiological responses to threat and supports homeostasis by releasing corticotropin-releasing hormone (CRH), which stimulates adrenocorticotropic hormone (ACTH) secretion from the pituitary. ACTH then promotes cortisol release from the adrenal cortex, enabling broad systemic effects on metabolism, immunity, and neurodevelopment27,28,29. Dysregulation of this axis, as frequently observed in individuals exposed to early adversity, has implications for lifelong stress reactivity and health outcomes.
Stressors, such as unpredictability, uncontrollability, and social evaluation, increase cortisol levels, which typically return to baseline once the stressor subsides30,31,32. In contrast, ACEs are linked to chronic dysregulation of the HPA axis – in both hypo- or hyper-regulation22, affecting cortisol regulation across the lifespan33. According to Hosseini-Kamkar and colleagues34, HPA axis calibration follows an inverted U-shaped curve, with severe adversity leading to downregulation and milder stress to increased cortisol output. ACEs are also related with heightened HPA axis sensitivity during adulthood21. Women with elevated lifetime cortisol levels maintain higher levels during pregnancy, potentially increasing fetal exposure to stress17,24,35.
Under typical conditions, fetal exposure to maternal cortisol is regulated by the placental 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2) enzyme, which inactivates cortisol to cortisone, buffering the fetus from maternal glucocorticoid fluctuations36,37. However, 11β-HSD2 expression is reduced in pregnancies affected by elevated psychosocial stress, anxiety, or depression38 and this down regulation appears more pronounced in women with a history of ACEs, potentially increasing fetal cortisol exposure earlier in gestation39.
Glucocorticoids, such as cortisol, play a significant role in the development of the central nervous system, affecting emotional regulation and cognitive function. Physiological increases in cortisol levels during pregnancy are necessary for normative brain development and behavioral regulation40. Conversely, excessive exposure to cortisol during critical developmental periods appears to be detrimental to fetal neurodevelopment, with strong links to psychopathology later in life3,4,5,6,41,42,43.
Postnatally, maternal cortisol remains critical for infant development44, with cortisol related to cortisol regulation and temperament45,46,47. Children’s stress-regulatory systems are still developing, and caregivers play an important role in externally regulating their child’s stress response and helping them respond adaptively to stress and challenge48. Maternal exposure to ACEs has been associated with lower breast milk cortisol at 6 weeks and a blunted increase from weeks 2 to 1249, suggesting greater cortisol dysregulation as a function of an adverse environment50. However, research on circulating cortisol has yielded different results. Studies found that experiencing early life adversity was associated with alterations in diurnal cortisol rhythms across pregnancy51,52. Additionally, women who reported early life adversity had a larger cortisol awakening response than those who did not experience adversity at 2–6 months postpartum53. These findings underscore the complex role of maternal ACEs and HPA axis function and regulation, particularly during pregnancy and early postpartum, in the intergenerational transmission of adversities and may contribute to the fetal programming of infant stress physiology. Studies found that experiencing early life adversity was associated with alterations in diurnal cortisol rhythms across pregnancy51,52, and women reporting experiencing early life adversity had a larger awakening response than those who did not experience adversity at 2–6 months postpartum53. These findings underscore the role of maternal ACEs and HPA axis function and regulation, particularly during pregnancy and early postpartum, in the intergenerational transmission of adversities and may contribute to the fetal programming of infant stress physiology.
Physiological synchrony is a concept referring to the association between a specific measure of physiological activity in a caregiver and the same measure in their child, typically in response to a task or in a particular context. This core idea is measured and discussed using various related terms, such as concordance, attunement, coregulation, and coordination54,55,56. Within this framework, "synchrony," "concordance," and “attunement” generally denote a positive relationship where physiological activity moves in the same direction for both individuals. Conversely, terms like "negative attunement," "discordance," and “asynchrony” specifically denote a negative association where one individual’s physiological activity increases while the other’s decreases48.
Neuroendocrine, immune, and metabolic systems mediate the impact of maternal mental health on offspring, in physiological synchrony within the mother–infant dyad57. During pregnancy and the neonatal period, shared environments promote alignment of HPA axis activity between mothers and their children58,59. Studies have shown attunement in cortisol levels and diurnal rhythms within dyads, particularly between mothers and infants aged 7.8 to 17.4 months60. Correlations in cortisol were stronger for mother–infant pairs than father–infant pairs61, likely due to genetic, environmental, and emotional proximity. Maternal affective states are mirrored in infant physiology, while infant cues reciprocally are linked to maternal regulation, supporting a dynamic biobehavioral feedback system within the dyad62. This physiological synchrony and intergenerational transfer of adversity are hypothesized to be fundamentally mediated by epigenetic mechanisms. Specifically, epigenetic mechanisms, such as DNA methylation and changes in chromatin structure, have been implicated as a means by which environmental factors, like ACEs and stress, can shape gene expression and are thought to produce long-term health consequences in mothers and offspring63,64. In rats, stress situations have epigenetic effects that alter the methylation status of the NGFI-A binding site in a region of the Nr3c1 promoter responsible for control of hippocampal glucocorticoid receptor (GR) expression, and, in sum, results in decreased methylation of the NGFI-A consensus binding site, increased negative HPA feedback stress regulation64. In this way, our group found a negative association between maternal ACEs and miRNA expression (hsa-miR-582-3p) in umbilical cord blood samples65. High expression of hsa-miR-582-3p has been shown to negatively regulate the HPA axis through the modulation of glucocorticoid receptors66, and consequently, lower levels of this miRNA in newborns could lead to higher cortisol levels.
Biobehavioral synchrony reflects coordinated HPA axis activity within the mother–infant dyad in response to stress, and is thought to represent a biological expression of shared emotional and behavioral states67,68,69,70. While physiological attunement is commonly associated with positive outcomes, it may also occur in dysregulated forms. Mothers and infants can synchronize around both adaptive and maladaptive stress responses71. Specifically, parent–child physiological synchrony is beneficial by providing a scaffold from which children can develop independent regulatory skills72,73. Conversely, synchronous physiological activity can also be detrimental by potentially exaggerating the experience of stress between two individuals74,75. For instance, Fuchs (2017)76 found that cortisol awakening response (CAR) synchrony was present only in mother–child dyads with a history of maltreatment. These findings suggest that maternal ACEs may contribute to this maladaptive form of physiological attunement, thereby increasing the likelihood of intergenerational transmission of dysregulated stress physiology19,20,43,77,78,79.
Evidence suggests that HPA axis attunement may begin prenatally, with maternal cortisol levels during pregnancy accounting for approximately 30% of the variability in fetal cortisol80. Elevated maternal cortisol, particularly in the morning and afternoon, has been associated with increased infant cortisol reactivity and impaired stress recovery postnatally81,82,83. This physiological synchrony persists into the postpartum period, maintained through continuous behavioral and biological interactions84. However, maternal histories of childhood maltreatment have been linked to disrupted regulation in offspring, including lower baseline cortisol43 and prolonged elevated cortisol responses to stress85. These dyads also show reduced cortisol concordance, suggesting that early adversity in mothers may impair the transmission of adaptive stress regulation to the next generation43,79,85.
Cortisol levels among family members reflect not only genetic factors but also shared environmental factors86. As infants grow, their stress-response systems stabilize, and early mother–child interactions help shape enduring patterns of HPA axis regulation87. During infancy, cortisol is modulated by social input, particularly maternal behavior50,88. However, as children form relationships beyond the home, the maternal role wanes. The preschool period represents a sensitive window for cortisol consolidation and the development of stress regulation and resilience87. Thus, analyses of maternal-infant HPA axis dynamics must account for developmental stage, as regulatory patterns evolve rapidly over the first year of life87.
While prior research has demonstrated physiological attunement between maternal and infant cortisol levels, most studies have focused on dyads with infants older than 12 months67,68, with limited attention to earlier developmental stages (younger than 5 months)85,89. To address this gap, the present study examines mother–infant salivary cortisol attunement at 1 and 6 months postpartum—a period marked by rapid maturation of the infant stress-response system. We also assess changes in cortisol over time and evaluate the correlation between maternal exposure to ACEs and cortisol regulation in both mothers and their infants.
We hypothesize that maternal and infant cortisol levels will be positively correlated, consistent with early physiological attunement. We further hypothesize that greater maternal ACE exposure will be associated with disrupted cortisol regulation in the dyad (both mother and infant) during early infancy, which will in turn affect the development and stress response of the infant HPA axis.
Methods
Participants
Participants were drawn from the Mother Influences on Child Neurobehavioral Development (Healthy MiNDS) cohort study in Brazil90, a longitudinal study investigating the effects of maternal ACEs on offspring behavior, neurodevelopment, and associated biological mechanisms underlying intergenerational transmission. Maternal inclusion criteria were: residence in high-risk, low-resource areas of Guarulhos or São Paulo (São Paulo state, Brazil); reliance on the Brazilian public healthcare system (Sistema Único de Saúde); age between 18 and 38 years; gestational age of 25–39 weeks at enrollment; and the ability to read, understand, and provide written informed consent.
Mothers were excluded if they presented with high-risk pregnancies; severe psychiatric disorders (e.g., schizophrenia, bipolar disorder, persistent delusional disorder, obsessive–compulsive disorder, dementia, or suicidal ideation); history of traumatic brain injury, epilepsy treatment, or neurosurgery; decompensated medical conditions requiring intensive care; use of illicit substances (excluding cannabis); or active infections including toxoplasmosis, rubella, cytomegalovirus, herpes, or others.
Participants were enrolled at birth following maternal consent to participate in the study. Offspring were excluded if they met any of the following criteria: prematurity (< 37 weeks’ gestation), low birth weight (< 2.5 kg), 5-min Apgar score < 7, admission to a neonatal intensive care unit, or diagnosis of kernicterus or congenital metabolic disorders. The final sample comprised 325 mother–infant dyads recruited from the low-risk population of the Healthy MiNDS cohort.
This research protocol received approval from the Institutional Review Board (IRB) at Duke University (Pro00110664) and Columbia University/New York State Psychiatric Institute (7927). In Brazil, it was sanctioned by the National Research Ethics Committee (CONEP; 78,018,417.2.0000.5505) and the Research Ethics Committee of Universidade Federal de São Paulo (CEP; 1200/2017). All procedures were conducted in compliance with applicable guidelines and regulations.
Each participant in the study received comprehensive information regarding the study’s objectives and methodologies. Written informed consent was obtained for participation, including for their newborns, following the principles established in the Helsinki Declaration.
Procedures
Maternal ACEs, race, maternal educational level, and socioeconomic status
Maternal ACEs were assessed during pregnancy using the CDC-Kaiser ACE Study Questionnaire1,91, administered at enrollment. This instrument evaluates adverse experiences before the age of 18 through 10 dichotomous items (“yes”/“no”), covering physical, emotional, and sexual abuse, neglect, and household dysfunction (e.g., domestic violence, substance use, mental illness, or parental separation). The total ACE score, ranging from 0 to 10, is the sum of affirmative responses, with higher scores reflecting greater cumulative exposure to childhood adversity.
Participants were asked to self-report their race, their infant’s race, and their educational attainment. Socioeconomic status was assessed using the ABEP92 (Associação Brasileira de Empresas de Pesquisa) scale, the official method for socioeconomic stratification in Brazil, which is based on household income, ownership of goods, and educational level of the head of household. The ABEP scale produces a total score ranging from 0 to 50, with classes approximately distributed as follows: A1 (45–50; $4745.29; 0.6%), A2 (41–44; value not reported), B1 (36–40; $2094.47; 1.1%), B2 (31–35; $1047.62; 7.9%), C1 (26–30; $572.96; 21.1%), C2 (15–25; $324.70; 36.0%), and D/E (0–14; $133.66; 33.4%). These values illustrate the socioeconomic diversity of the participants, spanning the range from the highest-income and highest-score class (A1) to the lowest-income and lowest-score groups (D/E).
Saliva sample collection
Saliva samples for cortisol measurement were collected from mothers and infants between 2–6 weeks postpartum (baseline) in the morning (7:00 am-12:00 pm) following their arrival at the university. Follow-up samples were collected when the infants reached 6 months of age, both in the morning and afternoon (8:30 a.m. to 6:00 p.m.), at the participants’ home.
Cortisol follows a circadian rhythm, peaking 20–30 min after awakening (the cortisol awakening response—CAR) and declining throughout the day to its lowest level 2–3 h after sleep onset93. Notably, Khoury85 found that saliva collection time was negatively correlated with maternal cortisol levels, but not with infant cortisol levels.
The saliva was collected using Salivette® (Sarstedt) tubes, placing the cotton swab under the tongue for 2–3 min. Mothers provided samples in Falcon tubes. All samples were centrifuged at 4,000 g for 15 min, aliquoted into microtubes, and stored in −80 °C freezers until the analysis.
Measures
Measurement of salivary cortisol level
The enzyme-linked Immunosorbent Assay (ELISA) (DRG® Salivary Cortisol ELISA – SLV-2930 – MARBURG/Germany) was used to measure salivary cortisol levels based on the principle of competitive binding. This method utilizes wells coated with a monoclonal (mouse) antibody that targets an antigenic site on the cortisol molecule. Endogenous cortisol from the sample competes with a cortisol-peroxidase conjugate for binding to the antibody. After incubation, any unbound conjugate was washed away. The amount of peroxidase conjugate bound was inversely proportional to the cortisol level in the sample. Following the addition of the substrate solution, the intensity of the developed color was inversely proportional to the cortisol level in the sample. The results were presented as “absorbance obtained” and “final concentration of cortisol” in the analyzed sample.
Statistical analysis
As an initial analysis, ordinary paired t-tests (6 months vs. baseline and mother vs. offspring) were conducted, along with Pearson correlations and partial correlations, to examine the nature of association within and between dyads over time. Standardized effect sizes are reported according to Cohen94, with the effect size for paired t-tests calculated using the standard deviation of the differences.
Subsequently, using the mother–offspring dyad data, the bivariate latent change score (BLCS) model was employed to investigate the concept of cross-domain coupling95. This model allowed us to assess the extent to which changes in salivary cortisol levels in offspring after 6 months (such as Δ [6 months − baseline]) are correlated with the initial maternal salivary cortisol level. Additionally, it quantified the changes in the salivary cortisol levels of both the offspring and mother between baseline and 6 months and their relationship with their respective baseline levels.
BLCS model with two-time points is a just-identified model fitting the data perfectly with zero degrees of freedom; therefore, no fit indices are reported. Detailed theoretical background on the BLCS model is provided in earlier works96,97, and Mplus and Lavaan syntaxes are presented in Supplementary Material 1.
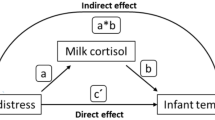
The main parameters of interest here are the following (presented in Fig. 1 and Fig. 2):
-
•The cross-domain coupling (shown in orange), represented by single-headed arrows.
-
•The self-feedback (shown in purple),
-
•The correlated change in cortisol levels (shown in yellow as a double-headed arrow), reflecting the degree to which changes in maternal and child salivary cortisol co-occur, after accounting for the coupling pathway.
-
•The mother-child correlation in cortisol levels at baseline (shown in blue as a double-headed arrow)
The raw values for the dyad cortisol were winsorized at the 5th and 95th percentile and log-transformed as conducted by Lawes98. Winsorization reduces the effect of extreme outliers by capping values at specified percentiles rather than removing them (unlike trimming), preserving the sample size (i.e., unlike deletion of outliers), reducing variance and skewness caused by extreme values. The log-transformation is used to normalize positively skewed data (common for hormone concentrations like cortisol) and stabilize variance. As a consequence, it makes the distribution more symmetric (closer to normality) and mitigates heteroscedasticity, facilitating linear modeling assumptions (e.g., regression).
Both raw and transformed salivary measures were presented, as the dispersion for offspring has not been described in the literature, to our knowledge.
Missing data were addressed using the full-information maximum likelihood approach based on the missing at-random mechanism99. Robust maximum likelihood estimation was applied because the transformed cortisol measures were not normally distributed.
Given the variation in the timing of cortisol data collection, and the known effect of cortisol levels based on the time of the day100, the BLCS model was adjusted to account for the timing of sample collection. This adjustment involves correlations between all initial cortisol measures and time, while also treating time as a predictor for the latent score change (see Supplementary Material 1 for the syntax and refer to the gray arrows and squares in Fig. 1).
Lastly, embedded in the BLCS model, we evaluated the correlation between ACEs and the cortisol baseline levels of the dyad and the latent change scores. Because this model is overidentified, we can assess its model fit (such as the comparative Fit Index, root mean squared error of approximation, and Tucker–Lewis index). We adopted the suggested cutoffs101 to determine whether the model’s fit was good or acceptable.
The racial diversity brought in the context of our study is not coming from a WEIRD (western, educated, industrialized, rich democracies) scenario102. Our hypothesis accounted for all variables, such as type of delivery and breastfeeding. These factors, among others, relate directly to the characterization of our study sample.
Results
The mean maternal age was 27.30 years old (± 5.13), with an average of 3.53 ACEs. Infants were, on average, 32.32 days old at baseline and 203.22 days (approximately 6.77 months) at the 6-month follow-up. At least 39.5% of the mothers had completed high school. The majority of the sample (65.1%) identified as non-white, and 69.4% belonged to socioeconomic strata (classes DE and C2). More than half of the births were vaginal deliveries (61.4%). Detailed demographic characteristics are presented in Table 1.
From baseline to six months postpartum, salivary cortisol levels significantly declined in both mothers and their infants, with a greater reduction observed in maternal levels. For mothers, both raw (M = –0.381, 95% CI [–0.537, –0.224]) and winsorized log-transformed values (M = –0.433, 95% CI [–0.590, –0.274]) showed significant decreases. Similarly, infants exhibited significant reductions over time in both raw (M = –0.173, 95% CI [–0.319, –0.026]) and winsorized values (M = –0.195, 95% CI [–0.341, –0.048]). Full results are presented in Table 2.
Mother–offspring cortisol levels are positively correlated, with stronger associations observed at baseline (r = 0.319, p < 0.001) than at six months (r = 0.208, p = 0.003). At baseline, correlations were moderate and statistically significant, while at six months, the correlations weakened but remained statistically significant. Correlations were controlled for the time of saliva collection to account for diurnal variation in cortisol levels. Detailed correlation and p-values for both raw and winsorized data are provided in Table 3.
Standardized effect sizes (Cohen’s d) for differences in cortisol levels between mothers and their offspring at baseline and six months, based on both raw and winsorized (WL) data, are presented in Table 4. Across all conditions, offspring exhibited higher cortisol levels than their mothers.
The figures present the four main parameters of interest in their standardized form (i.e., standardized regression coefficients and Pearson’s correlations) taking into account the time when the cortisol was collected for Fig. 1 and full model where ACEs’ baseline cortisol levels and latent change score are adjusted for time when cortisol was collected, mother’s and offspring’s age in Fig. 2. A significance level of 0.05 was adopted, and the significant paths are indicated using solid lines for easier visualization.
Under the full adjusted model and full-information maximum likelihood approach for dealing with missing data, the baseline correlation between mother–offspring cortisol levels was significant (r = 0.319, 95% CI = 0.212–0.425), indicating a medium-sized effect94. In contrast, the correlation between changes in cortisol levels over time within the dyad was smaller (r = 0.145, 95% CI = 0.001 to 0.289), and the difference between these two correlations was statistically significant (Wald test (1) = 4.664, p = 0.0308). These results suggest a stronger synchrony in cortisol levels at baseline compared to changes over time. See Fig. 1 and 2 for a visual representation of the BCLS model parameters (n = 358) without and with covariates adjustment, respectively.
ACEs significantly predicted maternal baseline cortisol levels (B = 0.126, p = 0.026), while all other paths from ACEs to cortisol outcomes were not statistically significant. Importantly, the effect sizes of the other model paths remained unchanged after including ACEs and covariates (mothers’ and offsprings’ age). The model was overidentified and demonstrated excellent fit (χ2(6) = 7.727, p = 0.2588; CFI = 0.981 and TLI = 0.915; RMSEA = 0.028, 90% CI = 0.000 to 0.078; RMSEA p = 0.705). These models fit and findings are derived from the model represented in Fig. 2.
The raw and winsorized values of salivary cortisol for mothers and their offspring at baseline and at 6 months are presented in Fig. 3.
Box plots display the raw and winsorized cortisol values distribution for mothers and their offspring at baseline and six months postpartum. Legend: MrB = Mother row baseline cortisol, Mr6 = mother raw six-month cortisol, OrB = offspring raw baseline cortisol, Or6 = offspring raw six months cortisol, MwlB = Mother winsorized and log-transformed baseline cortisol, Mwl6 = mother winsorized and log-transformed six-month cortisol, OwlB = offspring winsorized and log-transformed baseline cortisol, Owl6 = offspring winsorized and log-transformed six-months cortisol.
Only the self-feedback paths were statistically significant and showed negative, similarly sized effects, indicating that higher baseline cortisol levels were associated with greater decreases over time for both mothers and offspring. Conversely, individuals with lower baseline cortisol levels showed increases over time. This pattern suggests a regulatory effect toward the mean in both groups (Fig. 4). In contrast, the cross-domain coupling paths were not statistically significant and had minimal effect sizes, indicating no meaningful correlation between one dyad member’s cortisol trajectory with the others.
Supplementary Material 1 presents all estimated unstandardized and standardized parameters, including their confidence intervals. It also details the factors that were included as covariates in our model: maternal age, ethnicity, education, SES, ACEs, and maternal mental health (GAD7, PHQ9, PSS, EPDS, and resilience). However, none of these covariates correlated with the presented results, except for maternal ACEs.
Consistent with expectations for longitudinal studies, the research experienced participant loss during data collection, with 344 dyads’ saliva samples collected at baseline and 203 samples retained at 6-month follow-up (243 dyads performed the collection, but in 40 cases there was insufficient saliva volume to perform the cortisol analysis). To assess potential attrition bias, we compared the profile of participants who completed the follow-up to those who did not. No significant differences were observed across key maternal characteristics, including age (mean 27.6 vs. 26.9 years; t = −1.38; p = 0.17), number of ACEs (mean 3.61 vs. 3.45; t = −0.61; p = 0.54), or SES score (mean 20.16 vs. 19.71; t = −0.63; p = 0.53). Likewise, the distribution of maternal race did not differ significantly (χ2 = 3.18; p = 0.53), and while a non-significant trend was observed for maternal education (χ2 = 13.92; p = 0.053), it was not statistically significant. These findings suggest that the participant loss at the 6-month follow-up did not introduce substantial bias in the main maternal characteristics, thereby supporting the representativeness of the retained sample. Important to note that the results derived from the full adjusted model analysed data from 350 dyads due to the full-information maximum likelihood approach, as described in the statistical analysis subheading.
Discussion
Our findings indicate that maternal ACEs were associated with elevated salivary cortisol levels in mothers during the neonatal period, but this association was not sustained at six months postpartum. This temporal pattern may reflect the heightened physiological and psychological demands of the early postpartum period, particularly for women with a history of childhood adversity. Prior research suggests that early-life stress can recalibrate the HPA axis, increasing baseline activity and reactivity to stress103,104. Chronic exposure to elevated cortisol during development may disrupt glucocorticoid receptor sensitivity, resulting in long-term alterations to stress regulation27.
The first three months following birth involve significant lifestyle and circadian disruptions, including sleep deprivation, hormonal shifts associated with breastfeeding, and increased caregiving demands. These stressors may disproportionately impact mothers with elevated vulnerability due to ACEs, exacerbating HPA axis activation47,49,53,105,106. Circadian misalignment and sensitivity to daily stressors may contribute to transient elevations in maternal cortisol, particularly in those with heightened affective reactivity and limited regulatory capacity.
Interestingly, our results diverge from prior work showing blunted cortisol responses in mothers with higher ACE exposure49. However, that study examined a low-risk sample characterized by low adversity and substantial partner involvement, which may buffer the physiological effects of early adversity. Conversely, a study evaluating adolescent mothers from a high-risk Brazilian birth cohort project found that lifetime trauma history was associated with maternal salivary cortisol at 12 months postpartum107. Taken together, our findings underscore the importance of contextual and temporal factors in shaping the relationship between maternal ACEs and HPA axis activity during the postpartum period. Factors such as exposure to current stress, family environment, socioeconomic issues, and social support are crucial in mitigating or exacerbating the effects of early exposure to adversity on HPA axis regulation and cortisol levels107,108.
We observed a significant decline in maternal salivary cortisol concentrations from the neonatal period (3.59 ± 3.48 ng/mL) to six months postpartum (2.31 ± 2.27 ng/mL), consistent with established patterns of elevated cortisol during late pregnancy and during labor109,110. This trajectory reflects the physiological tapering of maternal HPA axis activity following childbirth.
Uniquely, our study examined mother-infant cortisol synchronicity at two critical developmental stages: 1) during the neonatal period (~ 1 month of age) and again at 6 months. While prior research has assessed maternal and infant cortisol levels independently, few studies have addressed their physiological coupling in the early postpartum months, and none, to our knowledge, have done so longitudinally from the neonatal stage onward. By capturing this dyadic cortisol dynamic across time, our findings provide novel insight into the temporal emergence and evolution of mother–infant HPA axis synchrony, a mechanism increasingly recognized as central to biobehavioral regulation in early development.
We observed a significant positive correlation between maternal and infant salivary cortisol levels at both the neonatal stage (r = 0.319, p < 0.001) and at 6 months postpartum (r = 0.208, p = 0.003), with stronger synchrony in the early postnatal period. This finding is consistent with evidence suggesting that mothers and infants exhibit physiological, emotional, and behavioral attunement from birth onward59,62,111. Such synchrony is thought to originate during gestation, when maternal and fetal systems are coupled through shared neuroendocrine pathways112. Maternal cortisol, for example, has been shown to correlate with levels in both amniotic fluid and fetal cord blood113,114, providing a route for the programming of infant stress responses. In line with this, Nazzari and coworkers115 reported that higher maternal cortisol awakening response (CAR) during pregnancy predicted a flatter infant cortisol response to stress in the neonatal period. However, findings remain mixed; in a later study, antenatal diurnal cortisol levels were not associated with stress reactivity in 3-month-old infants116. Collectively, these results suggest that maternal–infant physiological coupling is dynamic and may be strongest immediately after birth, potentially shaped by both prenatal exposures and early caregiving contexts.
The observed decrease in cortisol synchrony from the neonatal period to 6 months may reflect developmental changes following birth. As the direct physiological coupling between mother and fetus is disrupted postnatally, and as the infant’s central nervous system matures, dyadic cortisol attunement naturally declines. This pattern is consistent with prior evidence suggesting that cortisol synchrony is sustained not only by biological embedding but also by shared environments and co-regulated routines61,86,117,118. Notably, studies have found that parent–child adrenocortical synchrony depends on the amount of time spent together, underscoring the role of behavioral and contextual factors in shaping physiological alignment61,117,118.
Our sample comprised mothers with a mean of 3.6 ACEs, a rate notably higher than that reported in studies from high-income settings119,120. This elevated exposure to early adversity may partially account for the high level of dyadic cortisol attunement observed, particularly at baseline. Consistent with this interpretation, Hibel and collaborators121 reported that mothers and infants exposed to family violence exhibited greater physiological synchrony during stress, compared to non-exposed dyads. Similarly, heightened cortisol concordance has been observed in dyads facing elevated psychosocial risk or environmental threat67. Furthermore, our findings align with those from a São Paulo birth cohort project, a high-risk group characterized by chronic stress and residents primarily living in slums. Liu and colleagues108 found a strong correlation between maternal and infant hair cortisol sampled at 12 months in this cohort. The high degree of maternal-infant cortisol synchrony observed in these two high-risk studies, relative to findings from other mother-infant studies, strongly suggests that context plays an important role in the synchrony of maternal and infant cortisol. However, this association may be non-linear. Khoury85 found that maternal history of childhood maltreatment moderated the relationship between maternal and infant cortisol: while low-maltreatment dyads exhibited positive cortisol associations, high-maltreatment dyads did not. Interestingly, in that study, maternal and infant cortisol levels remained highly correlated at 4 months of age, suggesting that developmental timing and maternal history interact to shape the dynamics of HPA axis co-regulation. Our findings align with this literature, indicating that maternal early-life adversity may enhance mother–infant physiological synchrony during early infancy, particularly under conditions of elevated caregiving demands. However, in high-risk circumstances (such as those involving high socioeconomic risk, maltreatment, or insecure attachment), synchrony was not associated with better interaction quality or child functioning. This suggests that, under conditions of elevated risk, synchrony may instead act as an additional risk factor in the intergenerational transmission of the effects of stress and trauma122.
Finally, we investigated whether baseline cortisol levels in mothers and their infants predicted their own cortisol levels six months later, focusing on intraindividual change, termed here as self-feedback. We found that higher baseline cortisol levels were associated with greater reductions over time in both mothers and infants, whereas lower initial levels tended to increase.
These findings align with established models of HPA axis regulation, in which cortisol secretion activates a negative feedback loop through glucocorticoid receptor (GR) binding, restoring baseline levels following stress exposure123. During pregnancy, however, sustained activation of the HPA axis results in elevated cortisol, which typically normalizes postpartum124.
Under chronic stress, reduced GR sensitivity can impair this negative feedback mechanism, leading to HPA dysregulation and glucocorticoid resistance125. While our data revealed typical feedback patterns in cortisol recovery across the postpartum period, maternal ACEs did not significantly moderate this self-feedback dynamic. This suggests that ACE-related disruptions in HPA function may be more pronounced in acute stress reactivity than in basal feedback processes. However, our results do indicate that ACEs correlates with maternal cortisol concentrations during the neonatal period, consistent with the hypothesis that early adversity sensitizes the HPA axis, rendering it more reactive to environmental stressors encountered later in life126. In line with this, mothers with early trauma have shown elevated basal cortisol levels across the day, potentially reflecting a hyperresponsive HPA axis53. Importantly, while we focused on cortisol as an index of HPA function, other mechanisms – including ACTH levels and epigenetic modifications of GR expression – likely contribute to the regulation of this system and warrant future investigation.
Our results should also be interpreted in light of several limitations. First, maternal ACEs were assessed retrospectively, introducing potential recall bias. Second, our design relied on naturally occurring variation in cortisol levels rather than experimental stress paradigms, which limits causal inference.
Statistically, although it is possible to test a BLCS model with a minimum of two time points, but there are critics of this use given that two time point models, like the latent change score here presented are unlikely to capture individual differences reliably because of relatively little shared variance with the true generating scores and lower reliabilities127; consequently there is an attenuation of relationships that individual trajectories would exhibit with other phenomena128. Some insights and suggestions for two-time points are given by Brandmaier129, where some factors are study duration and the influence of adding an extra measurement occasion could influence the precision to estimate individual differences in linear slopes; however, there are always practicalities and logistics related to such precision gain as costs and adherence of the participants.
Lastly, there was inherent variation in the timing of saliva collection for both mothers and infants, which may have affected the measured cortisol values. This timing variability was primarily observed in the six-month follow-up collections, which were performed at the participants’ homes, according to their provided schedule. To mitigate these effects, collection time was included as a covariate in the statistical analyses.
Despite these limitations, our study offers several strengths. We included a racially and socioeconomically diverse cohort of mothers, predominantly Black and mixed-race women from under-resourced urban communities in Brazil, a population often underrepresented in developmental psychobiology. In this context, it is known that exposure to childhood adversity affects racial minorities and low-income communities, who are more likely to experience systemic and community adversities130. Moreover, we assessed mother-infant cortisol levels at two critical time points—during the neonatal period and at six months postpartum—an approach rarely undertaken in prior studies. Most prior research on maternal and infant cortisol has focused on post-stress reactivity, often using maternal self-collection at home51,115,116,131,132,133,134,135. In contrast, our data were collected at rest and under controlled conditions by trained researchers, ensuring procedural consistency across all participants. The resulting cortisol values are in line with those reported in previous studies43,111,116,136,137, supporting the validity and robustness of our protocol.
In summary, our findings highlight the enduring role of maternal ACEs, particularly in the context of early parenting and biological attunement with the infant. We demonstrated that maternal early adversity is associated with elevated cortisol in the neonatal period and that maternal and infant cortisol levels are significantly synchronized at early stages of development. These patterns highlight potential pathways for intergenerational transmission of stress biology and suggest critical windows for intervention to promote long-term health and developmental outcomes in vulnerable populations.
Data availability
The raw data supporting the findings of this study are available from the corresponding author (AJ) upon request. Raw data are not publicly available due to restrictions in the written consent signed by the participants of our study.
Abbreviations
- ACEs:
-
Adverse childhood experiences
- HPA:
-
Hypothalamic–pituitary–adrenal
References
Felitti, V. J. et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am. J. Prev. Med. 14, 245–258 (1998).
Hughes, K. et al. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2, e356–e366 (2017).
Doi, S., Fujiwara, T. & Isumi, A. Association between maternal adverse childhood experiences and mental health problems in offspring: An intergenerational study. Dev. Psychopathol. 33, 1041–1058 (2021).
Esteves, K., Gray, S. A. O., Theall, K. P. & Drury, S. S. Impact of physical abuse on internalizing behavior across generations. J. Child Fam. Stud. 26, 2753–2761 (2017).
McDonnell, C. G. & Valentino, K. Intergenerational effects of childhood trauma: Evaluating pathways among maternal ACEs, perinatal depressive symptoms, and infant outcomes. Child Maltreat. 21, 317–326 (2016).
Moog, N. K. et al. Intergenerational transmission of the effects of maternal exposure to childhood maltreatment in the USA: A retrospective cohort study. Lancet Public Health 8, e226–e237 (2023).
Zhang, J., Wiecaszek, P., Sami, S. & Meiser-Stedman, R. Association between panic disorder and childhood adversities: A systematic review and meta-analysis. Psychol. Med. 53, 2585–2595 (2023).
McLaughlin, K. A., Weissman, D. & Bitrán, D. Childhood adversity and neural development: A systematic review. Annu. Rev. Dev. Psychol. 1, 277–312 (2019).
Teicher, M. H., Samson, J. A., Anderson, C. M. & Ohashi, K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat. Rev. Neurosci. 17, 652–666 (2016).
Machlin, L. et al. Distinct associations of deprivation and threat with alterations in brain structure in early childhood. J. Am. Acad. Child Adolesc. Psychiatry 62, 885-894.e3 (2023).
Schäfer, J. L. et al. Threat and deprivation are associated with distinct aspects of cognition, emotional processing, and psychopathology in children and adolescents. Dev. Sci. 26, e13267 (2023).
Cooke, J. E., Racine, N., Pador, P. & Madigan, S. Maternal adverse childhood experiences and child behavior problems: A systematic review. Pediatrics 148, e2020044131 (2021).
Ma, X. et al. Mediators and moderators in the relationship between maternal childhood adversity and children’s emotional and behavioural development: A systematic review and meta-analysis. Psychol. Med. 52, 1817–1837 (2022).
Scorza, P. et al. Research Review: Intergenerational transmission of disadvantage: Epigenetics and parents’ childhoods as the first exposure. J. Child Psychol. Psychiatry 60, 119–132 (2019).
Yehuda, R. & Lehrner, A. Intergenerational transmission of trauma effects: Putative role of epigenetic mechanisms. World Psychiatry Off. J. World Psychiatr. Assoc. WPA 17, 243–257 (2018).
Santana, V. O. et al. Sex-specific association between maternal childhood adversities and offspring’s weight gain in a Brazilian cohort. Sci. Rep. 15, 2960 (2025).
Bowers, M. E. & Yehuda, R. Intergenerational transmission of stress in humans. Neuropsychopharmacology 41, 232–244 (2016).
Demers, C. H., Aran, Ö., Glynn, L. M. & Davis, E. P. Prenatal programming of neurodevelopment: Structural and functional changes. In Prenatal stress and child development 193–242 (Springer International Publishing, 2021).
Buss, C. et al. Intergenerational transmission of maternal childhood maltreatment exposure: Implications for fetal brain development. J. Am. Acad. Child Adolesc. Psychiatry 56, 373–382 (2017).
Moog, N. K. et al. Intergenerational effect of maternal exposure to childhood maltreatment on newborn brain anatomy. Biol. Psychiatry 83, 120–127 (2018).
Heim, C. Pituitary-Adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA 284, 592 (2000).
Brindle, R. C., Pearson, A. & Ginty, A. T. Adverse childhood experiences (ACEs) relate to blunted cardiovascular and cortisol reactivity to acute laboratory stress: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 134, 104530 (2022).
Iob, E., Baldwin, J. R., Plomin, R. & Steptoe, A. Adverse childhood experiences, daytime salivary cortisol, and depressive symptoms in early adulthood: A longitudinal genetically informed twin study. Transl. Psychiatry 11, 420 (2021).
Moog, N. K. et al. Maternal exposure to childhood trauma is associated during pregnancy with placental-fetal stress physiology. Biol. Psychiatry 79, 831–839 (2016).
Barrett, J. & Fleming, A. S. Annual research review: All mothers are not created equal: Neural and psychobiological perspectives on mothering and the importance of individual differences. J. Child Psychol. Psychiatry 52, 368–397 (2011).
Loman, M. M. & Gunnar, M. R. Early experience and the development of stress reactivity and regulation in children. Neurosci. Biobehav. Rev. 34, 867–876 (2010).
Gunnar, M. R. & Quevedo, K. Early care experiences and HPA axis regulation in children: A mechanism for later trauma vulnerability. Prog. Brain Res. 167, 137–149 (2007).
Lupien, S. J., McEwen, B. S., Gunnar, M. R. & Heim, C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat. Rev. Neurosci. 10, 434–445 (2009).
Munck, A., Guyre, P. M. & Holbrook, N. J. Physiological functions of glucocorticoids in stress and their relation to pharmacological actions*. Endocr. Rev. 5, 25–44 (1984).
Jezova, D. & Herman, J. P. Stress and stress-related disease states as topics of multi-approach research. Stress 23, 615–616 (2020).
Romanova, Z. et al. Testosterone but not cortisol concentrations in hair correlate between mothers and their prepubertal children under real-life stress conditions. Psychoneuroendocrinology 143, 105844 (2022).
Zorn, J. V. et al. Cortisol stress reactivity across psychiatric disorders: A systematic review and meta-analysis. Psychoneuroendocrinology 77, 25–36 (2017).
Kalmakis, K. A., Meyer, J. S., Chiodo, L. & Leung, K. Adverse childhood experiences and chronic hypothalamic–pituitary–adrenal activity. Stress 18, 446–450 (2015).
Hosseini-Kamkar, N., Lowe, C. & Morton, J. B. The differential calibration of the HPA axis as a function of trauma versus adversity: A systematic review and p-curve meta-analyses. Neurosci. Biobehav. Rev. 127, 54–135 (2021).
Swales, D. A. et al. Exposure to traumatic events in childhood predicts cortisol production among high risk pregnant women. Biol. Psychol. 139, 186–192 (2018).
Beitens, I. Z., Bayard, F., Ances, I. G., Kowarski, A. & Migeon, C. J. The metabolic clearence rate, blood production, interconversion and transplacental passage of cortisol and cortisone in pregnancy near term. Pediatr. Res. 7, 509–519 (1973).
Brown, R. W. et al. The ontogeny of 11 beta-hydroxysteroid dehydrogenase type 2 and mineralocorticoid receptor gene expression reveal intricate control of glucocorticoid action in development. Endocrinology 137, 794–797 (1996).
Jahnke, J. R., Terán, E., Murgueitio, F., Cabrera, H. & Thompson, A. L. Maternal stress, placental 11β-hydroxysteroid dehydrogenase type 2, and infant HPA axis development in humans: Psychosocial and physiological pathways. Placenta 104, 179–187 (2021).
George, J., Muzik, M. & Townsel, C. Placental cortisol dysregulation in mothers with experiences of childhood adversity: Potential mechanisms and clinical implications. J. Clin. Med. 13, 2020 (2024).
Kapoor, A., Dunn, E., Kostaki, A., Andrews, M. H. & Matthews, S. G. Fetal programming of hypothalamo-pituitary-adrenal function: Prenatal stress and glucocorticoids. J. Physiol. 572, 31–44 (2006).
Cook, F. et al. Infant regulation and child mental health concerns: A longitudinal study. Pediatrics 143, e20180977 (2019).
Bierer, L. M. et al. Elevation of 11β-hydroxysteroid dehydrogenase type 2 activity in Holocaust survivor offspring: Evidence for an intergenerational effect of maternal trauma exposure. Psychoneuroendocrinology 48, 1–10 (2014).
Brand, S. R. et al. The impact of maternal childhood abuse on maternal and infant HPA axis function in the postpartum period. Psychoneuroendocrinology 35, 686–693 (2010).
Hinde, K. Lactational programming of infant behavioral phenotype. In Building babies: Primate development in proximate and ultimate perspective 187–207 (New York, NY, 2012).
Grey, K. R., Davis, E. P., Sandman, C. A. & Glynn, L. M. Human milk cortisol is associated with infant temperament. Psychoneuroendocrinology 38, 1178–1185 (2013).
Nolvi, S. et al. Human milk cortisol concentration predicts experimentally induced infant fear reactivity: Moderation by infant sex. Dev. Sci. 21, e12625 (2018).
Glynn, L. M. et al. Postnatal maternal cortisol levels predict temperament in healthy breastfed infants. Early Hum. Dev. 83, 675–681 (2007).
DePasquale, C. E. A systematic review of caregiver–child physiological synchrony across systems: Associations with behavior and child functioning. Dev. Psychopathol. 32, 1754–1777 (2020).
Vacaru, S. V., Brett, B. E., Eckermann, H. & De Weerth, C. Determinants of maternal breast milk cortisol increase: Examining dispositional and situational factors. Psychoneuroendocrinology 158, 106385 (2023).
Tarullo, A. R. & Gunnar, M. R. Child maltreatment and the developing HPA axis. Horm. Behav. 50, 632–639 (2006).
Epstein, C. M., Houfek, J. F., Rice, M. J. & Weiss, S. J. Integrative review of early life adversity and cortisol regulation in pregnancy. J. Obstet. Gynecol. Neonatal. Nurs. 50, 242–255 (2021).
Rinne, G. R., Hartstein, J., Guardino, C. M. & Dunkel Schetter, C. Stress before conception and during pregnancy and maternal cortisol during pregnancy: A scoping review. Psychoneuroendocrinology 153, 106115 (2023).
Gonzalez, A., Jenkins, J. M., Steiner, M. & Fleming, A. S. The relation between early life adversity, cortisol awakening response and diurnal salivary cortisol levels in postpartum women. Psychoneuroendocrinology 34, 76–86 (2009).
Saxbe, D. E. et al. Relative influences: Patterns of HPA axis concordance during triadic family interaction. Health Psychol. 33, 273–281 (2014).
Skoranski, A. M., Lunkenheimer, E. & Lucas-Thompson, R. G. The effects of maternal respiratory sinus arrhythmia and behavioral engagement on mother-child physiological coregulation. Dev. Psychobiol. 59, 888–898 (2017).
Suveg, C. et al. Symptoms and synchrony: Mother and child internalizing problems moderate respiratory sinus arrhythmia concordance in mother–preadolescent dyads. Dev. Psychol. 55, 366–376 (2019).
Garafova, A. et al. Bridging the mood and stress hormone levels between mothers and their babies: The study design and first preliminary results. Acta Psychol. (Amst.) 238, 103977 (2023).
Davis, E. P. & Sandman, C. A. The timing of prenatal exposure to maternal cortisol and psychosocial stress is associated with human infant cognitive development. Child Dev. 81, 131–148 (2010).
Saxbe, D. E. et al. HPA axis linkage in parent–child dyads: Effects of parent sex, autism spectrum diagnosis, and dyadic relationship behavior. Dev. Psychobiol. 59, 776–786 (2017).
Bright, M. A., Granger, D. A. & Frick, J. E. Do infants show a cortisol awakening response?. Dev. Psychobiol. 54, 736–743 (2012).
Stenius, F. et al. Comparisons between salivary cortisol levels in six-months-olds and their parents. Psychoneuroendocrinology 33, 352–359 (2008).
Voegtline, K. M., Dhaurali, S., Wainger, J. & Lauzon, S. Ontogeny of the Dyad: the relationship between maternal and offspring neuroendocrine function. Curr. Psychiatry Rep. 24, 297–306 (2022).
Oberlander, T. F. et al. Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics 3, 97–106 (2008).
Sharma, R. et al. Maternal–fetal stress and DNA methylation signatures in neonatal saliva: An epigenome-wide association study. Clin. Epigenetics 14, 87 (2022).
Micali, D. et al. hsa-miR-582-3p in umbilical cord blood is negatively associated with maternal exposure to childhood maltreatment. Epigenomics 16, 1273–1286 (2024).
Imrich, R. et al. Adrenal function in rheumatoid arthritis: A correlation with disease activity. Arthritis Res. Ther. 14, P27 (2012).
Atkinson, L. et al. Maternal sensitivity and infant and mother adrenocortical function across challenges. Psychoneuroendocrinology 38, 2943–2951 (2013).
Laurent, H. K., Ablow, J. C. & Measelle, J. Taking stress response out of the box: Stability, discontinuity, and temperament effects on HPA and SNS across social stressors in mother–infant dyads. Dev. Psychol. 48, 35–45 (2012).
Sethre-Hofstad, L. Attunement of maternal and child adrenocortical response to child challenge. Psychoneuroendocrinology 27, 731–747 (2002).
Van Bakel, H. J. A. & Riksen-Walraven, J. M. Adrenocortical and behavioral attunement in parents with 1-year-old infants. Dev. Psychobiol. 50, 196–201 (2008).
Bernard, N. K., Kashy, D. A., Levendosky, A. A., Bogat, G. A. & Lonstein, J. S. Do different data analytic approaches generate discrepant findings when measuring mother–infant HPA axis attunement?. Dev. Psychobiol. 59, 174–184 (2017).
Lougheed, J. P. & Hollenstein, T. Arousal transmission and attenuation in mother–daughter dyads during adolescence. Soc. Dev. 27, 19–33 (2018).
Wass, S. V. et al. Parents mimic and influence their infant’s autonomic state through dynamic affective state matching. Curr. Biol. 29, 2415-2422.e4 (2019).
Waters, S. F., West, T. V., Karnilowicz, H. R. & Mendes, W. B. Affect contagion between mothers and infants: Examining valence and touch. J. Exp. Psychol. Gen. 146, 1043–1051 (2017).
Waters, S. F., West, T. V. & Mendes, W. B. Stress contagion: Physiological covariation between mothers and infants. Psychol. Sci. 25, 934–942 (2014).
Fuchs, A., Moehler, E., Resch, F. & Kaess, M. The effect of a maternal history of childhood abuse on adrenocortical attunement in mothers and their toddlers. Dev. Psychobiol. 59, 639–652 (2017).
Dixon, L., Hamilton-Giachritsis, C. & Browne, K. Attributions and behaviours of parents abused as children: A mediational analysis of the intergenerational continuity of child maltreatment (Part II). J. Child Psychol. Psychiatry 46, 58–68 (2005).
Fuchs, A., Möhler, E., Resch, F. & Kaess, M. Impact of a maternal history of childhood abuse on the development of mother–infant interaction during the first year of life. Child Abuse Negl. 48, 179–189 (2015).
Fuchs, A., Möhler, E., Resch, F. & Kaess, M. Sex-specific differences in adrenocortical attunement in mothers with a history of childhood abuse and their 5-month-old boys and girls. J. Neural Transm. 123, 1085–1094 (2016).
Gitau, R., Fisk, N. M., Teixeira, J. M. A., Cameron, A. & Glover, V. Fetal hypothalamic-pituitary-adrenal stress responses to invasive procedures are independent of maternal responses1. J. Clin. Endocrinol. Metab. 86, 104–109 (2001).
Davis, E. P., Glynn, L. M., Waffarn, F. & Sandman, C. A. Prenatal maternal stress programs infant stress regulation. J. Child Psychol. Psychiatry 52, 119–129 (2011).
Gutteling, B. M., Weerth, C. D. & Buitelaar, J. K. Prenatal stress and children’s cortisol reaction to the first day of school. Psychoneuroendocrinology 30, 541–549 (2005).
Gutteling, B. M., De Weerth, C. & Buitelaar, J. K. Short communicationmaternal prenatal stress and 4–6 year old children’s salivary cortisol concentrations pre- and post-vaccination. Stress 7, 257–260 (2004).
Feldman, R. From biological rhythms to social rhythms: Physiological precursors of mother-infant synchrony. Dev. Psychol. 42, 175–188 (2006).
Khoury, J. E., Beeney, J., Shiff, I., Bosquet Enlow, M. & Lyons-Ruth, K. Maternal experiences of childhood maltreatment moderate patterns of mother–infant cortisol regulation under stress. Dev. Psychobiol. 63, 1309–1321 (2021).
Schreiber, J. et al. Environmental influences on family similarity in afternoon cortisol levels: Twin and parent–offspring designs. Psychoneuroendocrinology 31, 1131–1137 (2006).
Gunnar, M. R. & Donzella, B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology 27, 199–220 (2002).
Hostinar, C. E. & Gunnar, M. R. Future directions in the study of social relationships as regulators of the HPA axis across development. J. Clin. Child Adolesc. Psychol. 42, 564–575 (2013).
Crockett, E. E., Holmes, B. M., Granger, D. A. & Lyons-Ruth, K. Maternal disrupted communication during face-to-face interaction at 4 months: Relation to maternal and infant cortisol among at-risk families. Infancy 18, 1111–1134 (2013).
Micali, D. et al. The intergenerational impact of maternal childhood adversity on child behavior and neurodevelopment: The healthy MiNDS protocol. Int. J. Methods Psychiatr. Res. 34, e70031 (2025).
Pereira, F. G. & Viana, M. C. Adaptação transcultural do adverse childhood experiences international questionnaire. Rev. Saúde Pública 55, 79 (2021).
ABEP - Associação Brasileira de Empresas de Pesquisa. Critério Brasil: Critério de Classificação Econômica Brasil. at <https://www.abep.org/criterio-brasil> (2019).
Doman, J., Thompson, S., Grochocinski, V., Jarrett, D. & Kupfer, D. J. A computer algorithm to determine the nadir and rise time in nocturnal cortisol secretion. Psychoneuroendocrinology 11, 359–366 (1986).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences. Taylor and Francis. (2013).
Kievit, R. A., Fuhrmann, D., Borgeest, G. S., Simpson-Kent, I. L. & Henson, R. N. A. The neural determinants of age-related changes in fluid intelligence: A pre-registered, longitudinal analysis in UK Biobank. Wellcome Open Res. 3, 38 (2018).
McArdle, J. J. & Nesselroade, J. R. Longitudinal data analysis using structural equation models. (American Psychological Association. https://doi.org/10.1037/14440-000 (2014).
Steyer, R., Eid, M. & Schwenkmezger, P. Modeling True Intraindividual Change: True Change as a Latent Variable. Preprint at https://doi.org/10.23668/PSYCHARCHIVES.12718 (1997).
Lawes, M., Hetschko, C., Schöb, R., Stephan, G. & Eid, M. Unemployment and hair cortisol as a biomarker of chronic stress. Sci. Rep. 12, 21573 (2022).
Enders, C. & Bandalos, D. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct. Equ. Model. Multidiscip. J. 8, 430–457 (2001).
Kirschbaum, C. et al. Cortisol and behavior: 2. Application of a Latent state-trait model to salivary cortisol. Psychoneuroendocrinology 15, 297–307 (1990).
Schermelleh-Engel, K., Moosbrugger, H. & Müller, H. Evaluating the Fit of Structural Equation Models: Tests of Significance and Descriptive Goodness-of-Fit Measures. Preprint at https://doi.org/10.23668/PSYCHARCHIVES.12784 (2003).
Gurven, M. D. & Lieberman, D. E. WEIRD bodies: Mismatch, medicine and missing diversity. Evol. Hum. Behav. Off. J. Hum. Behav. Evol. Soc. 41, 330–340 (2020).
Isenhour, J., Speck, B., Conradt, E., Crowell, S. E. & Raby, K. L. Examining the implications of contextual stress and maternal sensitivity for infants’ cortisol responses to the still face paradigm. Psychoneuroendocrinology 166, 107059 (2024).
Ellis, B. J. & Boyce, W. T. Biological sensitivity to context. Curr. Dir. Psychol. Sci. 17, 183–187 (2008).
Gay, C. L., Lee, K. A. & Lee, S.-Y. Sleep patterns and fatigue in new mothers and fathers. Biol. Res. Nurs. 5, 311–318 (2004).
Brunton, P. J., Russell, J. A. & Douglas, A. J. Adaptive responses of the maternal hypothalamic-pituitary-adrenal axis during pregnancy and lactation. J. Neuroendocrinol. 20, 764–776 (2008).
Wiley, K. S. et al. A preliminary investigation of associations between traumatic events experienced during pregnancy and salivary diurnal cortisol levels of brazilian adolescent mothers and infants. Am. J. Hum. Biol. 37, e70004 (2025).
Liu, H. et al. Cavum septum pellucidum and first-episode psychosis: A meta-analysis. PLoS ONE 12, e0177715 (2017).
Pofi, R. & Tomlinson, J. W. Glucocorticoids in pregnancy. Obstet. Med. 13, 62–69 (2020).
Trainer, P. J. Corticosteroids and Pregnancy. Semin. Reprod. Med. 20, 375–380 (2002).
Provenzi, L. et al. The dual nature of hypothalamic-pituitary-adrenal axis regulation in dyads of very preterm infants and their mothers. Psychoneuroendocrinology 100, 172–179 (2019).
Uvnäs-Moberg, K., Arn, I. & Magnusson, D. The psychobiology of emotion: the role of the oxytocinergic system. Int. J. Behav. Med. 12, 59–65 (2005).
Glover, V., Bergman, K., Sarkar, P. & O’Connor, T. G. Association between maternal and amniotic fluid cortisol is moderated by maternal anxiety. Psychoneuroendocrinology 34, 430–435 (2009).
Stirrat, L. I. et al. Glucocorticoids are lower at delivery in maternal, but not cord blood of obese pregnancies. Sci. Rep. 7, 10263 (2017).
Nazzari, S. et al. Beyond the HPA-axis: Exploring maternal prenatal influences on birth outcomes and stress reactivity. Psychoneuroendocrinology 101, 253–262 (2019).
Nazzari, S., Fearon, P., Rice, F., Molteni, M. & Frigerio, A. Maternal caregiving moderates the impact of antenatal maternal cortisol on infant stress regulation. J. Child Psychol. Psychiatry 63, 871–880 (2022).
Mörelius, E., Broström, E. B., Westrup, B., Sarman, I. & Örtenstrand, A. The stockholm neonatal family-centered care study: Effects on salivary cortisol in infants and their mothers. Early Hum. Dev. 88, 575–581 (2012).
Mörelius, E., Örtenstrand, A., Theodorsson, E. & Frostell, A. A randomised trial of continuous skin-to-skin contact after preterm birth and the effects on salivary cortisol, parental stress, depression, and breastfeeding. Early Hum. Dev. 91, 63–70 (2015).
Bellis, M. A., Hughes, K., Leckenby, N., Perkins, C. & Lowey, H. National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Med. 12, 72 (2014).
McKenna, B. G. et al. Infant epigenetic aging moderates the link between Black maternal childhood trauma and offspring symptoms of psychopathology. Dev. Psychopathol. https://doi.org/10.1017/S0954579423001232 (2023).
Hibel, L. C., Granger, D. A., Blair, C. & Cox, M. J. The Family Life Project Key Investigators. Intimate partner violence moderates the association between mother–infant adrenocortical activity across an emotional challenge. J. Fam. Psychol. 23, 615–625 (2009).
Thomas, J. C., Letourneau, N., Campbell, T. S. & Giesbrecht, G. F. Apron Study Team. Social buffering of the maternal and infant HPA axes: Mediation and moderation in the intergenerational transmission of adverse childhood experiences. Dev. Psychopathol. 30, 921–939 (2018).
Karin, O. et al. A new model for the HPA axis explains dysregulation of stress hormones on the timescale of weeks. Mol. Syst. Biol. 16, e9510 (2020).
Magiakou, M. A. et al. Hypothalamic corticotropin-releasing hormone suppression during the postpartum period: Implications for the increase in psychiatric manifestations at this time. J. Clin. Endocrinol. Metab. 81, 1912–1917 (1996).
Cohen, S. et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc. Natl. Acad. Sci. 109, 5995–5999 (2012).
Koss, K. J. & Gunnar, M. R. Annual research review: Early adversity, the hypothalamic–pituitary–adrenocortical axis, and child psychopathology. J. Child Psychol. Psychiatry 59, 327–346 (2018).
Parsons, S. & McCormick, E. M. Limitations of two time point data for understanding individual differences in longitudinal modeling — What can difference reveal about change?. Dev. Cogn. Neurosci. 66, 101353 (2024).
Liu, K. Measurement error and its impact on partial correlation and multiple linear regression analyses1. Am. J. Epidemiol. 127, 864–874 (1988).
Brandmaier, A. M., Lindenberger, U. & McCormick, E. M. Optimal two-time point longitudinal models for estimating individual-level change: Asymptotic insights and practical implications. Dev. Cogn. Neurosci. 70, 101450 (2024).
SmithBattle, L., Loman, D. G., Yoo, J. H., Cibulka, N. & Rariden, C. Evidence for revising the adverse childhood experiences screening tool: A scoping review. J. Child Adolesc. Trauma 15, 89–103 (2022).
Duffy, K. A. et al. Sex differences in stress-induced cortisol response among infants of mothers exposed to childhood adversity. Biol. Psychiatry 96, 876–885 (2024).
Chasson, M., Khoury, J., Bosquet Enlow, M. & Lyons-Ruth, K. Maternal caregiving moderates relations between maternal childhood maltreatment and infant cortisol regulation. J. Child Psychol. Psychiatry. https://doi.org/10.1111/jcpp.14171 (2025).
Bublitz, M. H., Bourjeily, G., Vergara-Lopez, C. & Stroud, L. R. Momentary stress, cortisol, and gestational length among pregnant victims of childhood maltreatment: A pilot study. Obstet. Med. 9, 73–77 (2016).
Bublitz, M. H. & Stroud, L. R. Maternal history of child abuse moderates the association between daily stress and diurnal cortisol in pregnancy: A pilot study. Stress 16, 706–710 (2013).
Hantsoo, L., Kornfield, S., Anguera, M. C. & Epperson, C. N. Inflammation: A proposed intermediary between maternal stress and offspring neuropsychiatric risk. Biol. Psychiatry 85, 97–106 (2019).
Reid, B. M., Sokol, N., Aubuchon-Endsley, N. L. & Stroud, L. R. Maternal prenatal cortisol and the interaction of income and pre-pregnancy body mass index are independently associated with newborn cortisol. Dev. Psychobiol. 65, e22354 (2023).
Thayer, Z. M. & Kuzawa, C. W. Early origins of health disparities: Material deprivation predicts maternal evening cortisol in pregnancy and offspring cortisol reactivity in the first few weeks of life. Am. J. Hum. Biol. 26, 723–730 (2014).
Acknowledgements
We extend our gratitude to all families, especially mothers and their infants, for their participation.
Funding
This study was mainly funded by both the National Institute of Mental Health (NIMH; R01 MH121070-01A1) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; Research Support Foundation of the State of São Paulo; 2019/21612–0 and 2021/04819–0), as part of a partnership between both agencies.
Author information
Authors and Affiliations
Contributions
ACR, CD, JP, and AJ contributed to study conception and design, material preparation, and data collection/analysis, and prepared the first draft of the manuscript. HCM, ME, VOS, and IS contributed to material preparation, data collection/analysis, and prepared the first draft of the manuscript. LPR and ACCM contributed to material preparation and data collection/analysis. All authors commented on previous versions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramos, A.C., Cogo-Moreira, H., Eid, M. et al. Mother infant cortisol levels and maternal childhood adversity. Sci Rep 15, 44746 (2025). https://doi.org/10.1038/s41598-025-28548-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-28548-8