Abstract
Pevonedistat, a potent NEDD8-activating enzyme inhibitor, has shown preclinical promise in overcoming platinum resistance and enhancing antitumor activity. This phase I study investigated the recommended dose (RD) and tolerability of pevonedistat in combination with capecitabine plus oxaliplatin (CapeOX) as third-line or later treatment in patients with unresectable advanced or recurrent gastric cancer (AGC). The study included a dose-finding cohort for determining the RD and an expansion cohort for assessing the efficacy and safety at the RD. Twelve patients were enrolled between April 2019 and September 2021. Dose-limiting toxicities (DLTs), including grade 2/3 aspartate transaminase/alanine transaminase (AST/ALT) elevation and treatment delays, occurred in the initial 2 patients at level 1 (20 mg/m2). After protocol amendment, no DLTs were observed at level 0 (15 mg/m2), which was determined as the RD. Common adverse events were decreased platelet count (67%), nausea (58%), and AST/ALT elevation (58%). A partial response was achieved in 2 patients (17%) and disease control was achieved in 8 (67%). Median overall survival was 9.3 months and progression-free survival was 4.4 months. Pevonedistat plus CapeOX was well tolerated and showed promising efficacy as salvage-line chemotherapy for AGC.
Similar content being viewed by others
Introduction
Gastric cancer ranks as the fifth most common cancer globally and the fifth leading cause of cancer-related mortality, with 968,784 new cases and 660,175 deaths recorded in 20221. Despite recent declines in mortality, gastric cancer still ranks third for cancer-related deaths in Japan2. Systemic chemotherapy is the standard treatment for unresectable advanced or recurrent gastric cancer (AGC) and is aimed at relieving symptoms and prolonging survival. However, the prognosis remains poor, with a reported median survival of around 15 months3,4,5,6.
The Japanese treatment guideline for gastric cancer recommends irinotecan, nivolumab, and trifluridine/tipiracil as third-line or later chemotherapy for HER2-negative AGC7,8,9 and trastuzumab deruxtecan as an additional option for HER2-positive AGC10. Nivolumab and trifluridine/tipiracil showed overall survival (OS) benefits in patients after failure of ≥ 2 chemotherapy regimens in the pivotal Phase III trials. However, the response rates were low (10% or less), and approximately half of the patients experienced disease progression as the best response, resulting in median progression-free survival (PFS) of only a few months. Therefore, development of more effective third-line treatments is necessary.
Neddylation is the process via which the ubiquitin-like protein NEDD8 (neural precursor cell expressed developmentally down-regulated protein 8) is conjugated to target proteins, and primarily activates the SCF complex (Skp, Cullin, F-box containing complex). This complex, which is activated in various cancers, regulates cell growth by degrading target proteins via the proteasome11,12,13,14,15. Inhibition of this pathway leads to accumulation of CDT1 (Cdc10-dependent transcript 1), which can cause over-replication of DNA and chromosomal instability16. Considering the importance of the NEDD8 pathway for the growth and survival of cancer cells, targeting of the NEDD8-activating enzyme (NAE) to disrupt proteasome-dependent protein degradation is a potential therapeutic approach in the treatment of cancer.
Pevonedistat (MLN4924, TAK-924) is a first-in-class NAE inhibitor that was initially developed for hematologic malignancies17,18,19,20,21,22. Preclinical studies have shown that pevonedistat also significantly suppresses the growth of gastric cancer cells23. Furthermore, pevonedistat may overcome oxaliplatin resistance by breaking down the protein complexes involved in DNA repair, which are essential for the resistance mechanism triggered by platinum-based agents24.
In Japan, S-1 is widely used in combination with oxaliplatin as the first-line treatment for AGC. S-1 and capecitabine are both classified as fluoropyrimidines, but have different mechanisms of action. In a Phase II trial of capecitabine plus cisplatin for patients with AGC and early relapse after adjuvant therapy with S-1, the response rate was 26.7%, suggesting that switching from a fluoropyrimidine to another drug provides some benefit25. It has been speculated that capecitabine in combination with oxaliplatin (CapeOX) could be a third-line option for AGC if resistance to oxaliplatin can be overcome. Moreover, pevonedistat in combination with CapeOX can be expected to have synergistic efficacy for AGC that is refractory to platinum-based chemotherapy.
The primary objectives of this study were to determine the recommended dose (RD) and pharmacokinetics of pevonedistat when used in combination with CapeOX. The secondary objectives were to assess the efficacy of this combination in Japanese patients with AGC after failure of chemotherapy containing fluoropyrimidines, platinum, and a taxane. The exploratory objective was to investigate the relationship between the molecular biological profile of proteins and the therapeutic effect of this combination chemotherapy. CapeOX is widely accepted as a standard first-line regimen for patients with AGC due to its established efficacy and manageable safety profile. This combination is endorsed by major international guidelines, such as NCCN and ESMO, and is commonly utilized as the backbone therapy in clinical studies26,27. In the future, first-line combinations that include pevonedistat may become a viable approach.
Study design
This multicenter, open-label, Phase I study included a dose-finding cohort for determining the RD based on the incidence of dose-limiting toxicities (DLTs) and an expansion cohort for assessing efficacy and safety in patients receiving the RD. Exploratory translational research was performed in both cohorts. A standard “3 + 3” dose escalation design was used in the dose-finding cohort. After determination of the RD in this cohort, additional patients were enrolled into the expansion cohort until 10 patients received the RD of pevonedistat, including those in the dose-finding cohort.
The study was approved by the institutional review board of National Cancer Center and Cancer Institute Hospital of Japanese Foundation for Cancer Research, and conducted in accordance with all applicable regulatory requirements, Good Clinical Practice standards, and the Declaration of Helsinki. All patients provided written informed consent. The study was registered on 10/May/2019 in the Japan Registry of Clinical Trials (jRCT2031190020).
Patients
Inclusion criteria were as follows: age ≥ 20 years; Eastern Cooperative Oncology Group performance status of 0–1; unresectable or recurrent gastric or gastroesophageal junction adenocarcinoma; ≥ 1 measurable lesion as defined by the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.128; ≥ 2 prior lines of chemotherapy; refractory to or intolerant of fluoropyrimidines (5-fluorouracil, capecitabine, or S-1) and platinum (cisplatin or oxaliplatin) as first-line treatment and taxanes as second-line treatment; adequate hematologic, hepatic, and renal function; and no massive ascites extending to the upper abdomen beyond the pelvic cavity or requiring drainage. Major exclusion criteria included recent or concurrent malignancy (within the past 5 years, except for definitively cured early-stage tumors), evidence of central nervous system metastasis, intolerance to capecitabine or oxaliplatin, coagulation abnormalities (prothrombin time [PT] or activated partial thromboplastin time [aPTT] > 1.5 times the upper limit of normal [ULN]); and a left ventricular ejection fraction of < 50%.
Treatment
In both cohorts, the treatment schedule started with a single dose of pevonedistat as the lead-in phase which was followed by the combination phase, which consisted of triplet chemotherapy with pevonedistat, capecitabine, and oxaliplatin (Supplemental Fig. 1). In the lead-in phase, pevonedistat was administered as monotherapy on day 1, and an endoscopic biopsy was collected on day 2 for the translational research component. In the combination phase, the first cycle of combination chemotherapy was started on the same day in the following week to allow for a 7-day interval after the single dose of pevonedistat in the lead-in phase. In the combination phase, oxaliplatin (130 mg/m2) was administered on day 1, capecitabine (1000 mg/m2/day orally twice daily with an interval of approximately 12 h between doses) for 14 days, and pevonedistat on days 1, 3, and 5 of a 3-week cycle, which was continued until the patient met the criteria for discontinuation. The dose level in the dose-finding phase is shown in Supplemental Fig. 2.
DLT and the recommended dose
DLT was assessed from the first dose of pevonedistat in the lead-in phase until day 35 or the day of initiation of cycle 2, whichever came first. An adverse event for which a causal link with the protocol treatment could be ruled out was not regarded as DLT. DLT was defined as any of the following adverse events: (1) grade 4 neutropenia lasting for ≥ 7 days; (2) grade 3 febrile neutropenia; (3) grade 4 thrombocytopenia lasting for ≥ 7 days; (4) grade 3 thrombocytopenia with bleeding; (5) platelet count < 10,000/mm3 at any time; (6) grade ≥ 3 PT or aPTT elevation in the absence of anticoagulation therapy; (7) grade ≥ 2 PT or aPTT elevation associated with clinically significant bleeding (e.g., in the central nervous system or gastrointestinal tract); (8) grade 4 non-hematologic toxicity (except for increased alkaline phosphatase, increased gamma-glutamyl transferase, hyperglycemia, hypercalcemia, hypocalcemia, hypernatremia, hyponatremia, hyperkalemia, hypokalemia, hypomagnesemia, hypophosphatemia, hypercholesterolemia, hypertriglyceridemia, and nausea/vomiting/diarrhea that improved to grade ≤ 2 within 72 h); (9) increased aspartate transaminase (AST) or increased alanine transaminase (ALT) > 5–20 × the ULN) lasting for ≥ 8 days; (10) elevations of transaminases (> 3–5 × the ULN) and bilirubin (> 1.5–3 × the ULN) lasting for ≥ 3 days between doses of pevonedistat; (11) any adverse event that caused the number of pevonedistat doses to be reduced to < 3 by day 15 in the first cycle or discontinuation; (12) any adverse event that caused a dose delay in cycle 2 for ≥ 21 days; (13) any adverse event that caused the relative dose intensity of capecitabine in cycle 1 to be reduced to < 60% of the planned dose; and (14) any adverse event that required discontinuation of the protocol treatment before cycle 2 because of adverse events other than (1) to (10). The RD was essentially the maximum dose at which DLT was observed in no more than 1 of 6 patients enrolled in the dose-escalation phase of the study. The RD was finally determined referring not only to the incidence of DLTs but also to all available information about the adverse events observed in the second or later cycles.
Assessments
Adverse events were evaluated according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0. The objective response rate, OS, PFS, disease control rate, and change in tumor burden (percent change in the sum of target lesion diameters) over time assessed by the site investigators according to RECIST version 1.128.
Exploratory translational research
To compare the pharmacokinetics of pevonedistat in the lead-in phase (pevonedistat monotherapy) with those in the combination phase, 3-mL blood samples were collected from patients enrolled in the dose-finding cohort at the following time points: before and 2, 4, and 6 h after the pevonedistat dose on day 1, day 2 (24 h post-dose) and day 3 (48 h post-dose) during the lead-in phase and at the same time points during the combination phase in cycle 1. Plasma pevonedistat concentrations were measured using Good Laboratory Practice-validated liquid chromatography/tandem mass spectrometry methods at QPS Holdings (Newark, DE, USA).
Chromatin licensing and DNA replication factor 1 (CDT1) expression was evaluated by immunohistochemistry using the monoclonal antibody for CDT1 (ab202067; Abcam, Cambridge, UK). Tumor tissue samples were analyzed using the Oncomine Comprehensive Assay-Plus (OCA Plus; Sigma-Aldrich, Burlington, MA, USA) for detection of mutations and copy number variants in more than 500 genes (Thermo Fisher Scientific, Waltham, MA, USA).
Statistical analysis
Although this study was initially planned to enroll 10 patients in the expansion cohort, the protocol was amended such that patient enrollment was terminated after 10 patients had started the protocol treatment at the RD because of the decision by Takeda Pharmaceutical Company to discontinue the development of pevonedistat (date of decision: September 1, 2021).
The sample size of 10 patients at the RD was determined based on futility. The first stage of Simon’s two-stage design was used to calculate the probability of early termination assuming a threshold response rate of ≤ 10%, whereby the probability of a true response rate being ≤ 10% would be 0.74 when the number of responders is ≤ 1 in the 10 patients.
The statistical analysis plan was developed and finalized before the database was locked. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Twelve patients were enrolled between August 28, 2019 and September 24, 2021 and received ≥ 1 dose of the study drug. The patient background characteristics are shown in Table 1. Median age was 67 years (range 37–75). Eight patients (66.7%) were male, 5 (41.7%) had an Eastern Cooperative Oncology Group performance status of 1, 1 (8.3%) had gastroesophageal junction adenocarcinoma with Siewert type III, 10 (83.3%) had intestinal-type tumors, 4 (33.3%) had metastases in ≥ 2 organs, and 2 (16.7%) were HER2-positive. Two patents had previously received trastuzumab-containing chemotherapy, 10 had received ramucirumab-containing chemotherapy, 2 had received irinotecan, and 7 had received nivolumab.
DLTs and the maximum tolerated dose
Two patients were enrolled to receive pevonedistat 20 mg/m2 (dose level 1). These patients experienced grade ≥ 2 elevations in ALT and AST during cycle 1, which led to a delay in starting cycle 2, so no further patients were enrolled for dose level 1. Thereafter, the protocol was amended to add lower dose levels of pevonedistat, namely, 15 mg/m2 (level 0) and 10 mg/m2 (level -1) (Supplemental Figs. 2 and 3).
Because no DLT was observed in the 6 patients enrolled at 15 mg/m2 (dose level 0), 4 patients were enrolled in the expansion cohort. Finally, the maximum tolerated dose of pevonedistat in combination with CapeOX was determined to be 15 mg/m2.
Safety
All 12 patients experienced ≥ 1 adverse event, and 7 (58.3%) experienced grade 3 adverse events (Table 2). Common adverse events of any grade with an incidence of > 50% were decreased platelet count (66.7%), increased AST (58.3%), ALT (58.3%), decreased neutrophil count (58.3%), nausea (58.3%), anemia (58.3%), and anorexia (58.3%). Grade 3 drug-related adverse events with an incidence of > 20% were anemia (4 patients, 33.3%) and increased AST (3 patients, 25.0%).
Treatment interruptions were required in the 2 patients who received pevonedistat at 20 mg/m2. Additionally, 1 of these patients receiving pevonedistat at 20 mg/m2 required a dose reduction. Three serious adverse events (hematuria, n = 1; decreased appetite, n = 1; and abdominal abscess requiring discontinuation of the protocol treatment, n = 1) occurred at a pevonedistat dose of 15 mg/m2 (level 0) and were judged to be related to the protocol treatment. None of the adverse events were fatal.
Pharmacokinetics of pevonedistat
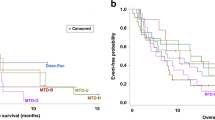
Eight patients in the dose-finding cohort (20 mg/m2, n = 2; 15 mg/m2, n = 6) were evaluable for pharmacokinetics. The plasma pevonedistat concentrations are shown in Fig. 1 and the pharmacokinetic parameters are summarized in Table 3. There was no appreciable difference in the pharmacokinetics of pevonedistat between monotherapy in the lead-in phase and combination therapy with CapeOX.
Plasma concentrations of pevonedistat in the lead-in phase (pevonedistat alone) and in the second cycle of pevonedistat plus CapeOX combination therapy in 8 patients enrolled in the dose-finding cohort. The plasma concentrations of pevonedistat after administration were measured in 8 patients to compare the pharmacokinetics of pevonedistat when administered alone and when administered in combination with CapeOX.
Efficacy
Details of the best response to treatment are summarized in Supplemental Table 1, and the waterfall plot is shown in Fig. 2. No patient obtained a complete response (CR), 2 achieved a partial response (PR), and 7 achieved stable disease (SD). The objective response rate (CR + PR) was 16.7% (95% confidence interval [CI] 2.09–48.41). The disease control rate (CR + PR + SD) was 75.0% (95% CI 42.81–94.51).
Water-fall plot showing the best percentage change in tumor size from baseline in individual patients. Each bar represents a single patient, with bars extending downward indicating reduction in tumor size and bars extending upwards indicating tumor growth. Patients who received pevonedistat at a dose of 20 mg/m2 (level 1) are indicated in red and those who received 15 mg/m2 (level 0) are indicated in blue.
As of the data cut-off date (April 30, 2022), all 12 patients had experienced progression based on the investigator’s assessment or had died, with a median PFS of 4.41 months (95% CI 1.91–5.79). One patient was still alive at the data cut-off point and was censored. The median OS time was 9.33 months (95% CI 5.46–11.0) (Fig. 3).
Change in CDT1 expression and genomic profile in endoscopic biopsy samples
Supplemental Table 2 shows the biomarker test results and treatment outcomes for each patient. Immunohistochemical evaluation of CDT1 levels was performed in all 12 patients. CDT1 expression was increased in 9 of the 12 post-treatment tumor biopsy samples (Fig. 4). No correlation was observed between increased CDT1 expression and treatment efficacy. Gene mutation analysis was performed using pre-treatment samples; however, no association was found between gene alterations, tumor mutational burden, and survival.
Expression of CDT1. CDT1 regulates DNA replication and is a biomarker of the pharmacodynamics of pevonedistat. Representative images of formalin-fixed paraffin-embedded gastric cancer tumor biopsies obtained during endoscopy from a patient treated with pevonedistat at a dose of 15 mg/m2 (level 0). Samples were collected at screening and post-dose on day 2 in cycle 1 and stained for CDT1. Arrows indicate examples of areas containing CDT1-positive cells. The scale bar represents 250 µm.
Discussion
Pevonedistat has been evaluated as monotherapy and in combination with other chemotherapy agents in various malignancies, but there have been no studies of pevonedistat in AGC. This is the first Phase I study of pevonedistat in combination with CapeOX as third-line or later treatment in patients with AGC. Although 2 patients experienced increased transaminase levels as DLT at dose level 1 (20 mg/m2), no DLTs were observed in any of the 10 patients enrolled at dose level 0 (15 mg/m2). Therefore, the RD of pevonedistat when used in combination with CapeOX was estimated to be 15 mg/m2, which is lower than the RD of 20–25 mg/m2 determined when pevonedistat was combined with chemotherapy in Phase II trials for other cancers29,30,31,32. In other clinical studies, NEDD8 inhibitors in combination with chemotherapy have caused liver dysfunction, manifesting as elevated liver enzymes such as AST and ALT. Hepatotoxicity has also been reported in the studies involving other NEDD8 inhibitors, particularly when used in combination with chemotherapy agents29,30,32,33,34,35. Furthermore, hepatic sinusoidal abnormalities, which are a type of veno-occlusive disease, have frequently been observed in patients receiving oxaliplatin36,37,38,39. There have also been occasional reports of hepatotoxicity with capecitabine40,41,42. It has been speculated that overlap of the toxicities associated with pevonedistat, capecitabine, and oxaliplatin might result in the RD of pevonedistat being smaller when it is administered in combination with CapeOX. Treatment interruptions and dose reductions were observed at a pevonedistat dose of 20 mg/m2 but not at 15 mg/m2. One patient discontinued the protocol treatment because of an abdominal abscess, and the remaining 9 patients were able to continue until disease progression. Therefore, pevonedistat at 15 mg/m2 in combination with CapeOX is considered feasible.
A previous study found that pevonedistat tended to reach a higher plasma concentration when it was administered in combination with carboplatin and paclitaxel than when it was administered as monotherapy30. However, in that study, historical pharmacokinetic data were used as the comparator for monotherapy, whereas our study compared the pharmacokinetics of pevonedistat administered as monotherapy (the lead-in cohort) with those when it was administered in combination with CapeOX (the combination cohort) in the same patients. Our results indicate that the pharmacokinetics of pevonedistat were not affected by combination with CapeOX.
The objective response rate when pevonedistat was administered in combination with CapeOX was 16.67% (95% CI 2.09–48.41), indicating that the predefined futility criteria (≤ 1/10) could be rejected. Median PFS was 4.41 months (95% CI 1.91–5.79), median OS was 9.33 months (95% CI 5.46–11.0), and the disease control rate was 75%. Three agents, namely, irinotecan, nivolumab, and trifluridine/tipiracil, are available for third-line or later treatment of AGC. While these treatments are generally tolerable, they have limited efficacy, with response rates of around 10% and more than 50% of patients experiencing disease progression as their best response, resulting in a median PFS of only a few months9,43,44. The combination of pevonedistat and CapeOX as a third-line or later treatment in this study yielded promising results comparable with those previously reported for oxaliplatin-based regimens used in salvage-line chemotherapy45,46,47,48,49,50.
Our post-treatment tumor biopsies showed both the presence of a pevinedistat-NEDD8 adduct and an increase in the cullin–RING ligase substrates NRF2 and CDT1. Immunohistochemistry revealed increased expression of CDT1 in 9 of 12 tumor biopsy samples on the day following a single dose of pevonedistat, which was thought to result from stabilization of the protein following the decrease in CDL activity in response to NAE inhibition by pevonedistat. The following 8 genes have been reported to be induced by pevonedistat through NAE inhibition: ATF3, GCLM, GSR, MAG1, NQO1, SLC7A11, SRXN1, and TXNRD120. Although these genes are considered to be pharmacodynamic markers of NAE inhibition, we did not find any association between gene mutations, tumor mutation burden, and efficacy. We are currently investigating molecular biological profiles related to the therapeutic effect of pevonedistat and CapeOX combination therapy using a proteome we have developed and deep phosphoproteome analysis51,52.
Conclusion
Pevonedistat at a RD of 15 mg/m2 administered intravenously on days 1, 3, and 5 in combination with CapeOX was well tolerated in patients with AGC. CDT1 expression was increased in 9 of 12 patients (75%). Pevonedistat plus CapeOX shows promising efficacy as salvage-line chemotherapy in patients with AGC.
Data availability
All included data is available from the corresponding author on reasonable request.
References
The GLOBOCAN 2022 database on the Global Cancer Observatory website. https://gco.iarc.fr/. (Accessed 24 November 2024).
Vital Statistics Japan (Ministry of Health, Labour and Welfare).
Yamada, Y. et al. Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naïve patients with advanced gastric cancer. Ann. Oncol. 26(1), 141–148 (2015).
Janjigian, Y. Y. et al. First-line nivolumab plus chemotherapy for advanced gastric, gastroesophageal junction, and esophageal adenocarcinoma: 3-year follow-up of the phase III CheckMate 649 trial. J. Clin. Oncol. 42(17), 2012–2020 (2024).
Boku, N. et al. Nivolumab plus chemotherapy in patients with HER2-negative, previously untreated, unresectable, advanced, or recurrent gastric/gastroesophageal junction cancer: 3-year follow-up of the ATTRACTION-4 randomized, double-blind, placebo-controlled, phase 3 trial. Gastric Cancer 27(6), 1287–1301 (2024).
Rha, S. Y. et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for HER2-negative advanced gastric cancer (KEYNOTE-859): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 24(11), 1181–1195 (2023).
Hironaka, S. et al. Randomized, open-label, phase III study comparing irinotecan with paclitaxel in patients with advanced gastric cancer without severe peritoneal metastasis after failure of prior combination chemotherapy using fluoropyrimidine plus platinum: WJOG 4007 trial. J. Clin. Oncol. 31(35), 4438–4444 (2013).
Kang, Y. K. et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 390(10111), 2461–2471 (2017).
Shitara, K. et al. Trifluridine/tipiracil versus placebo in patients with heavily pretreated metastatic gastric cancer (TAGS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 19(11), 1437–1448 (2018).
Shitara, K. et al. Trastuzumab deruxtecan in previously treated HER2-positive gastric cancer. N. Engl. J. Med. 382(25), 2419–2430 (2020).
Nakayama, K. I. & Nakayama, K. Ubiquitin ligases: cell-cycle control and cancer. Nat. Rev. Cancer 6(5), 369–381 (2006).
Jia, L. & Sun, Y. SCF E3 ubiquitin ligases as anticancer targets. Curr. Cancer Drug Targets 11(3), 347–356 (2011).
Sun, Y. E3 ubiquitin ligases as cancer targets and biomarkers. Neoplasia 8(8), 645–654 (2006).
Li, H. et al. Inactivation of SAG/RBX2 E3 ubiquitin ligase suppresses KrasG12D-driven lung tumorigenesis. J. Clin. Invest. 124(2), 835–846 (2014).
Sun, Y. & Li, H. Functional characterization of SAG/RBX2/ROC2/RNF7, an antioxidant protein and an E3 ubiquitin ligase. Protein Cell 4(2), 103–116 (2013).
Karakaidos, P. et al. Overexpression of the replication licensing regulators hCdt1 and hCdc6 characterizes a subset of non-small-cell lung carcinomas: synergistic effect with mutant p53 on tumor growth and chromosomal instability–evidence of E2F–1 transcriptional control over hCdt1. Am. J. Pathol. 165(4), 1351–1365 (2004).
Soucy, T. A. et al. An inhibitor of NEDD8-activating enzyme as a new approach to treat cancer. Nature 458(7239), 732–736 (2009).
Swords, R. T. et al. Pevonedistat (MLN4924), a First-in-Class NEDD8-activating enzyme inhibitor, in patients with acute myeloid leukaemia and myelodysplastic syndromes: a phase 1 study. Br. J. Haematol. 169(4), 534–543 (2015).
Milhollen, M. A. et al. MLN4924, a NEDD8-activating enzyme inhibitor, is active in diffuse large B-cell lymphoma models: rationale for treatment of NF-{kappa}B-dependent lymphoma. Blood 116(9), 1515–1523 (2010).
Shah, J. J. et al. Phase I Study of the Novel Investigational NEDD8-Activating Enzyme Inhibitor Pevonedistat (MLN4924) in patients with relapsed/refractory multiple myeloma or lymphoma. Clin. Cancer Res. 22(1), 34–43 (2016).
Swords, R. T. et al. Expanded safety analysis of pevonedistat, a first-in-class NEDD8-activating enzyme inhibitor, in patients with acute myeloid leukemia and myelodysplastic syndromes. Blood Cancer J. 7(2), e520 (2017).
Swords, R. T. et al. Pevonedistat, a first-in-class NEDD8-activating enzyme inhibitor, combined with azacitidine in patients with AML. Blood 131(13), 1415–1424 (2018).
Lan, H. et al. Neddylation inhibitor MLN4924 suppresses growth and migration of human gastric cancer cells. Sci. Rep. 6, 24218 (2016).
Marteijn, J. A. et al. Understanding nucleotide excision repair and its roles in cancer and ageing. Nat. Rev. Mol. Cell. Biol. 15(7), 465–481 (2014).
Nishikawa, K. et al. A phase II trial of capecitabine plus cisplatin (XP) for patients with advanced gastric cancer with early relapse after S-1 adjuvant therapy: XParTS-I trial. Gastric Cancer 21(5), 811–818 (2018).
Kim, G. M. et al. A randomized phase II trial of S-1-oxaliplatin versus capecitabine-oxaliplatin in advanced gastric cancer. Eur. J. Cancer 48(4), 518–526 (2012).
Wang, G. et al. Efficacy and safety of oxaliplatin-based regimen versus cisplatin-based regimen in the treatment of gastric cancer: a meta-analysis of randomized controlled trials. Int. J. Clin. Oncol. 24(6), 614–623 (2019).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45(2), 228–247 (2009).
Bhatia, S. et al. A phase I study of the investigational NEDD8-activating enzyme inhibitor pevonedistat (TAK-924/MLN4924) in patients with metastatic melanoma. Invest. New Drugs 34(4), 439–449 (2016).
Lockhart, A. C. et al. Phase Ib study of pevonedistat, a NEDD8-activating enzyme inhibitor, in combination with docetaxel, carboplatin and paclitaxel, or gemcitabine, in patients with advanced solid tumors. Invest. New Drugs 37(1), 87–97 (2019).
Handa, H. et al. Pevonedistat in East Asian patients with acute myeloid leukemia or myelodysplastic syndromes: a phase 1/1b study to evaluate safety, pharmacokinetics and activity as a single agent and in combination with azacitidine. J. Hematol. Oncol. 15(1), 56 (2022).
Foster, J. H. et al. Phase 1 study of NEDD8 activating enzyme inhibitor pevonedistat in combination with chemotherapy in pediatric patients with recurrent or refractory solid tumors (ADVL1615). Eur. J. Cancer 209, 114241 (2024).
Zhou, X. et al. Phase 1 study to evaluate the effects of rifampin on pharmacokinetics of pevonedistat, a NEDD8-activating enzyme inhibitor in patients with advanced solid tumors. Invest. New Drugs 40(5), 1042–1050 (2022).
Qin, A. et al. A phase II trial of pevonedistat and docetaxel in patients with previously treated advanced non-small-cell lung cancer. Clin. Lung Cancer 25(2), 128–134 (2024).
Yamamoto, N. et al. A first-in-human, phase 1 study of the NEDD8 activating enzyme E1 inhibitor TAS4464 in patients with advanced solid tumors. Invest. New Drugs 39(4), 1036–1046 (2021).
Rubbia-Brandt, L. et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann. Oncol. 15(3), 460–466 (2004).
Vauthey, J. N. et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J. Clin. Oncol. 24(13), 2065–2072 (2006).
Aloia, T. et al. Liver histology and surgical outcomes after preoperative chemotherapy with fluorouracil plus oxaliplatin in colorectal cancer liver metastases. J. Clin. Oncol. 24(31), 4983–4990 (2006).
Robinson, S. M. et al. Chemotherapy-associated liver injury in patients with colorectal liver metastases: a systematic review and meta-analysis. Ann. Surg. Oncol. 19(13), 4287–4299 (2012).
Hussein, M. & Jensen, A. B. Drug-induced liver injury caused by capecitabine: a case report and a literature review. Case Rep. Oncol. 16(1), 378–384 (2023).
Gurzu, S. et al. Lethal cardiotoxicity, steatohepatitis, chronic pancreatitis, and acute enteritis induced by capecitabine and oxaliplatin in a 36-year-old woman. Diagn. Pathol. 8, 150 (2013).
Chin, S. N., Kim, T. K. & Siu, L. L. Hepatic steatosis secondary to capecitabine: a case report. J. Med. Case Rep. 4, 227 (2010).
Nishimura, T. et al. Irinotecan monotherapy as third-line treatment for advanced gastric cancer refractory to fluoropyrimidines, platinum, and taxanes. Gastric Cancer 20(4), 655–662 (2017).
Boku, N. et al. Nivolumab in previously treated advanced gastric cancer (ATTRACTION-2): 3-year update and outcome of treatment beyond progression with nivolumab. Gastric Cancer 24(4), 946–958 (2021).
Tsuji, K. et al. Modified FOLFOX-6 therapy for heavily pretreated advanced gastric cancer refractory to fluorouracil, irinotecan, cisplatin and taxanes: a retrospective study. Jpn. J. Clin. Oncol. 42(8), 686–690 (2012).
Kondoh, C. et al. Salvage chemotherapy with the combination of oxaliplatin, leucovorin, and 5-fluorouracil in advanced gastric cancer refractory or intolerant to fluoropyrimidines, platinum, taxanes, and irinotecan. Gastric Cancer 21(6), 1050–1057 (2018).
Kim, Y. S. et al. Oxaliplatin, 5-fluorouracil and leucovorin (FOLFOX-4) combination chemotherapy as a salvage treatment in advanced gastric cancer. Cancer Res. Treat. 42(1), 24–29 (2010).
Kim, D. Y. et al. Phase II study of oxaliplatin, 5-fluorouracil and leucovorin in previously platinum-treated patients with advanced gastric cancer. Ann. Oncol. 14(3), 383–387 (2003).
Suh, S. H. et al. Oxaliplatin with biweekly low dose leucovorin and bolus and continuous infusion of 5-fluorouracil (modified FOLFOX 4) as a salvage therapy for patients with advanced gastric cancer. Cancer Res. Treat. 37(5), 279–283 (2005).
Seo, H. Y. et al. Treatment outcomes of oxaliplatin, 5-FU, and leucovorin as salvage therapy for patients with advanced or metastatic gastric cancer: a retrospective analysis. Cancer Chemother. Pharmacol. 63(3), 433–439 (2009).
Shoji, H. et al. Phosphoproteomic subtyping of gastric cancer reveals dynamic transformation with chemotherapy and guides targeted cancer treatment. Cell. Rep. 43(10), 114774 (2024).
Muraoka, S. et al. Comprehensive proteomic profiling of plasma and serum phosphatidylserine-positive extracellular vesicles reveals tissue-specific proteins. iScience 25(4), 104012 (2022).
Acknowledgements
We would like to thank the patients and their families, as well as the investigators and participating study teams, for making this study possible. We thank FiveRings Co., Ltd. for their invaluable support in conducting the clinical trial.
Funding
This study is supported by Takeda Pharmaceutical Company Limited.
Author information
Authors and Affiliations
Contributions
All authors participated in planning and writing the protocol of this study. Hirokazu Shoji and Narikazu Boku wrote the draft of the manuscript. The manuscript was reviewed by Daisuke Takahari, Akira Ooki, Kengo Nagashima, Hidekazu Hirano, Natsuko Okita, and Jun Adachi. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Hirokazu Shoji reports honoraria from Ono Pharmaceutical and Bristol Myers Squibb, and research grants from Ono Pharmaceutical and Takeda Pharmaceuticals. Daisuke Takahari reports grants from Taiho Pharmaceutical, Ono Pharmaceutical, Eli Lilly, Chugai Pharmaceutical, Bristol-Myers Squibb, and Daiichi Sankyo. Akira Ooki reports honoraria from Bristol-Myers Squibb, Astellas Pharma, Merck Serono, Taiho Pharmaceutical, Daiichi Sankyo, Ono Pharmaceutical, and MSD. Hidekazu Hirano reports honoraria from Bristol-Myers Squibb, Chugai Pharmaceutical, Novartis, Taiho Pharmaceutical, Fujifilm Pharmaceuticals, Teijin Pharma, and Ono Pharmaceutical. Kengo Nagashima reports consulting fees from SENJU Pharmaceutical Co., Ltd., Toray Industries, Inc., Kowa Company, Ltd., and Eli Lilly. Kensei Yamaguchi reports honoraria from Bristol Myers Squibb KK, Eli Lilly Japan KK, Taiho Pharmaceutical Co., Ltd., and Ono. Ken Kato reports consulting fees from Ono Pharmaceutical, Bristol-Myers Squibb, BeiGene, Novartis Pharma, AstraZeneca, Roche, Bayer Yakuhin, Merck & Co, Merck Biopharma, and Janssen Pharmaceutical, reports honoraria from Bristol-Myers Squibb, and Ono Pharmaceutical and reports participation on a Data Safety Monitoring Board or Advisory Board of Ono Pharmaceutical, Chugai Pharmaceutical, Bristol-Myers Squibb, and Merck & Co. Narikazu Boku reports honoraria from Bristol-Myers Squibb, Ono Pharmaceutical, Taiho Pharmaceutical, Daiichi Sankyo, and Eli Lilly, reports participation on a Data Safety Monitoring Board or Advisory Board of Kyowa Kirin, and research grants from Takeda Pharmaceuticals. All other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shoji, H., Takahari, D., Ooki, A. et al. Phase I study of pevonedistat combined with capecitabine and oxaliplatin in patients with platinum-refractory advanced gastric cancer. Sci Rep 16, 692 (2026). https://doi.org/10.1038/s41598-025-30367-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-30367-w