Abstract
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a globally widespread chronic liver condition that may progress to severe liver diseases, including advanced liver fibrosis. The high-sensitivity C-reactive protein-to-high-density lipoprotein cholesterol (hs-CRP/HDL-C) index may be a potential indicator for MASLD and advanced liver fibrosis, given its relevance to inflammation and plasma lipids. In this study, the hs-CRP/HDL-C index was investigated in relation to prevalent MASLD and advanced liver fibrosis. The study analyzed secondary data from the National Health and Nutrition Examination Survey (NHANES) 2017–2018 database. The hs-CRP/HDL-C index was calculated by the quotient of hs-CRP and HDL-C. Multiple logistic regression models, Cochran-Armitage trend tests, smooth curve fitting, threshold effect analyses, and stratified analyses were used to evaluate whether the hs-CRP/HDL-C index associated with MASLD and advanced liver fibrosis. The study cohort comprised 3684 participants, of whom 1268 (34.42%) were diagnosed with MASLD and 156 (12.28%) with advanced liver fibrosis. Logistic analyses adjusted for covariates revealed positive associations of the hs-CRP/HDL-C index with MASLD and advanced liver fibrosis, consistent across all subgroups. Smooth curve fitting and threshold effect analyses revealed nonlinear relationships of hs-CRP/HDL-C index with MASLD and advanced liver fibrosis, with inflection points at 0.8 for MASLD and 1.2 for advanced liver fibrosis. Additionally, significant interactions were observed between MASLD and covariates such as gender, smoking status, chronic kidney disease (CKD), and cancer. Similarly, the hs-CRP/HDL-C index exhibited positive correlations with advanced liver fibrosis across diverse subgroups, with notable interactions related to cancer. MASLD and advanced liver fibrosis were associated with hs-CRP/HDL-C index, indicating its potential utility as a clinical marker for these conditions.
Similar content being viewed by others
Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD), defined by pathological lipid deposits in the liver without excessive alcohol intake, poses a formidable challenge to public health1,2. On a global scale, it affects 30% of individuals, making it a foremost chronic liver condition3. Particularly in the United States, 80–100 million individuals grapple with MASLD, which imposes a staggering annual economic burden surpassing $103 billion4. This affliction is regularly linked to various metabolic dysfunctions, especially type 2 diabetes, hypertension, and cardiovascular disorders. MASLD can evolve into metabolic dysfunction-associated steatohepatitis (MASH), progress into stages of liver fibrosis, culminate in cirrhosis, and potentially lead to liver cancer5. The implications of MASLD heighten mortality risks from liver-related diseases, cardiovascular complications and malignant tumors6,7. This underscores the crucial importance of prompt detection and meticulous monitoring of prevalent MASLD and liver fibrosis. Such measures are essential to steer effective management strategies and therapeutic decisions8. While liver biopsy remains the definitive method for identifying and grading liver fibrosis, its invasive nature, high costs, and associated risks render it less desirable9,10,11. Hence, there is a compelling need for non-invasive techniques that accurately assess the severity of MASLD and liver fibrosis, offering a safer, cost-effective alternative.
The high-sensitivity C-reactive protein-to-high-density lipoprotein cholesterol (hs-CRP/HDL-C) ratio is emerging as a valuable composite index. It is recognized for its potential as a clinical marker for cardiovascular diseases due to its simplicity, practicality, and clinical relevance12. Central to pathogenesis of MASLD is inflammation, which can trigger oxidative stress, lipid peroxidation and the activation of immune cells. Hs-CRP has been identified as predictive indicators for MASLD13,14. Conversely, HDL-C is inversely linked with MASLD prevalence, underscoring its pivotal interaction in the disease trajectory15,16. Despite the emerging usage of the hs-CRP/HDL-C index, its relationship with MASLD and advanced liver fibrosis remains unclear. A comprehensive exploration into how this index correlates with MASLD and advanced liver fibrosis could unravel vital insights, potentially guiding future research directions.
To our knowledge, the exploration of these associations within a population-based framework remains uncharted. Therefore, we employed data sourced from the National Health and Nutrition Examination Survey (NHANES) 2017–2018 to scrutinize the associations of hs-CRP/HDL-C index with MASLD and advanced liver fibrosis.
Materials and methods
Study population
The NHANES was conducted to assess the general and nutritional health conditions of Americans. Annually, around 5,000 people are included in this survey from a sample representing the entire nation. The survey gathers five distinct types of data: demographic profiles, dietary habits, physical examinations, lab tests, and personal questionnaires. Each dataset is freely available to the public.
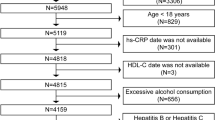
This investigation drew on data from the NHANES 2017–2018 cycle to probe the link between the hs-CRP/HDL-C index and MASLD, along with advanced liver fibrosis. It focused on adults aged ≥ 18 years who underwent vibration-controlled transient elastography (VCTE) within this NHANES cycle, a technique deployed to measure liver stiffness indicative of MASLD and liver fibrosis. Exclusions were made for pregnant women, individuals positive for hepatitis B/C serological markers, those with a physician’s diagnosis of hepatitis B/C, participants with history of excessive alcohol intake (indicated by standard drinks more than 14 for women or more than 21 for men per week), those suffering from terminal renal failure (defined as having an estimated glomerular filtration rate (eGFR) less than 15 mL/min/1.73 m2), and participants missing hs-CRP or HDL-C data. 3,685 participants were ultimately involved in this research, with comprehensive details regarding the selection criteria illustrated in Fig. 1.
Measurement of the hs-CRP/HDL-C index
Hs-CRP levels were quantified using a particle-enhanced turbidimetric immunoassay. HDL-C levels were measured through a specific endpoint reaction, with the resulting product measured by photometry at a wavelength of 600 nm. For this study, the hs-CRP/HDL-C index was calculated as the quotient of hs-CRP (mg/L) and HDL-C (mg/dL/1000).
Assessment of MASLD and advanced liver fibrosis
The identification of liver steatosis was conducted through the controlled attenuation parameters (CAP) of Fibroscan devices, boasting an AUROC value of 0.96 as outlined in earlier literature17. Liver stiffness evaluations were achieved utilizing a noninvasive VCTE technique, which deliver a precise quantification of liver fibrosis18. Within the NHANES data framework, 4266 participants underwent VCTE assessments utilizing the FibroScan 502 V2 Touch model at mobile examination centers. Drawing from existing research, liver steatosis was diagnosed when CAP reached or exceeded 285 dB/m19, and advanced liver fibrosis was identified when VCTE readings reached or exceeded 12 kPa20. MASLD was defined by the presence of liver steatosis in conjunction with metabolic dysfunction, while excluding other potential causes of hepatic fat accumulation. To establish metabolic dysfunction, patients must meet at least one of the following criteria2,21: (1) a body mass index (BMI) of 25 kg/m2 or higher, or a waist circumference exceeding 94 cm in men or 80 cm in women; (2) fasting blood glucose levels of 100 mg/dL or above, hemoglobin A1c values of 5.7% or greater, a prior diagnosis of type 2 diabetes, or current diabetes treatment; (3) blood pressure readings of 130/85 mmHg or above, or ongoing antihypertensive therapy; (4) triglyceride levels of 150 mg/dL or greater, or being under lipid-lowering treatment; and (5) low high-density lipoprotein cholesterol (HDL-C) levels, with thresholds set at below 40 mg/dL for men and below 50 mg/dL for women, or active treatment for dyslipidemia.
Covariates
Demographic details such as age, gender, race, poverty-to-income ratio, marital status, and education level were meticulously gathered by trained NHANES interviewers during in-person dialogues utilizing the Computer-Assisted Personal Interviewing (CAPI) system and the Family and Sample Person Demographics questionnaires. Body mass index (BMI) was calculated by the quotient of body weight (in kilograms) and height squared (in meters squared) based on physical measurements from NHANES assessments. According to standard classifications, a BMI < 25 kg/m2 was categorized as normal or underweight, 25 ≤ BMI < 30 kg/m2 as overweight, and BMI ≥ 30 kg/m2 as obesity22,23.
Diabetes mellitus (DM) identification in participants hinged on either a doctor’s diagnosis, self-reported use of insulin, usage of blood sugar-lowering medication, or laboratory indicators including an HbA1c reaching or exceeding 6.5% and a fasting glucose level reaching or exceeding 126 mg/dL24.
Hypertension classification was derived from participants’ self-reported history or usage of prescription medication for high blood pressure. Cardiovascular disease (CVD) status was determined by affirmative responses to physician-diagnosed conditions such as coronary heart disease, heart attack, congestive heart failure, or stroke. Chronic kidney disease (CKD) was flagged for individuals with an eGFR < 60 mL/min/1.73 m2, calculated using the IDMS-traceable MDRD Study formula. Smoking status was segmented into non-smokers, former smokers, and current smokers based on lifetime cigarette consumption and current smoking habits. Individuals who had smoked less than 100 cigarettes in their lifetime were categorized as non-smokers, those who had smoked more than 100 cigarettes but were not actively smoking were classed as former smokers, and those who smoked more than 100 cigarettes were defined as current smokers. Biochemical profiles, including measurements for aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, serum total cholesterol, and triglycerides were compiled from the NHANES laboratory data.
Statistical analyses
The statistical analyses for this investigation utilized the NHANES database with an intricate sampling design. To mirror national demographics accurately, all calculations were weighted according to the protocols of the National Center for Health Statistics (NCHS). Whereas categorical variables were represented by raw counts and weighted proportions, continuous variables were expressed as weighted averages and standard deviations. Differences between groups were identified utilizing either the Student’s t-test or chi-squared test, contingent on the type and distribution of the data. We investigated the relationship between the hs-CRP/HDL-C index and prevalent MASLD, along with advanced liver fibrosis through multivariate logistic regression analyses. Model 1 remained unadjusted, Model 2 incorporated adjustments for demographic elements (age, gender, race, poverty-to-income ratio, marital status, education level), and Model 3 expanded adjustments to include additional variables like smoking status, obesity, DM, hypertension, and histories of CVD, CKD, and cancer. Furthermore, we conducted a Cochran-Armitage trend test to examine the dose-response relationships of the hs-CRP/HDL-C index with MASLD and advanced liver fibrosis. The hs-CRP/HDL-C index was divided into quartiles for subgroup analyses and interaction tests, using the first quartile as a reference. Additionally, generalized additive models (GAM) and smooth curve fitting were applied, controlling for all covariates, to examine potential non-linear relationships. When non-linear relationships were identified, segmented regression models were utilized to assess threshold effects. Stratification by various covariates allowed us to investigate potential variations in these associations.
All statistical analyses were performed utilizing EmpowerStats 4.2 and R 4.3.2. Statistical significance was defined as P < 0.05.
Results
Baseline characteristics
The characteristics of the study sample are presented in Table 1. The participants had an average age of 48.55 years, with 48.02% male and 51.98% female. The majority of participants were non-Hispanic whites (64.56%) and non-smokers (62.64%). The average BMI was 29.50 kg/m2. Subjects with MASLD exhibited markedly elevated levels of AST, ALT, albumin, triglycerides, hs-CRP, and the hs-CRP/HDL-C index in comparison to those without MASLD. Conversely, higher average levels of HDL-C were observed in subjects free from MASLD. Similarly, participants without advanced liver fibrosis displayed significantly reduced average concentrations of AST, ALT, albumin, hs-CRP, and the hs-CRP/HDL-C index, while maintaining elevated levels of HDL-C, in contrast to those suffering from advanced liver fibrosis.
The associations of hs-CRP/HDL-C index with MASLD and advanced liver fibrosis
The study findings indicated an increased occurrence of MASLD and advanced liver fibrosis in participants with an elevated hs-CRP/HDL-C index (Table 2). These associations were found to be statistically significant in the unadjusted model (Model 1) and adjusted models (Model 2 and Model 3). After adjusting for potential confounders, an increase in the hs-CRP/HDL-C index was autonomously and notably linked to higher odds of MASLD (OR = 1.82, 95% CI: 1.15–2.87) and advanced liver fibrosis (OR = 1.68, 95% CI: 1.03–2.75). Each additional unit in the hs-CRP/HDL-C index was linked to a 82% rise in the likelihood of MASLD and a 68% increase in the odds of advanced liver fibrosis.
Cochran-Armitage trend test results indicated substantial linear correlations between the hs-CRP/HDL-C index and MASLD, along with advanced liver fibrosis. In comparison to the first quartile group, there were higher odds in the second, third, and fourth quartiles. These associations were statistically significant in Models 1, 2, and 3.
To assess the reliability and stability of the logistic regression analyses findings, the generalized additive model (GAM) analyses were performed, controlling for all covariates. The smooth curve fitting depicted in Fig. 2 illustrated nonlinear associations of the hs-CRP/HDL-C index with MASLD and advanced liver fibrosis, presenting two inverted U-shaped curves. The threshold effect analyses revealed inflection points at 0.8 for MASLD and 1.2 for advanced liver fibrosis (Table 3).
Subgroup analyses and interaction tests
Gender, race, education level, smoking status, DM, history of CVD, CKD, and cancer were used as stratification variables to observe the effect size trend, and two forest plots of data were generated (Figs. 3 and 4). Positive associations were found between the hs-CRP/HDL-C index and MASLD in all subgroups. There were significant interactions between MASLD and gender, smoking status, CKD, and cancer. Furthermore, there were positive correlations observed in various subgroups between the hs-CRP/HDL-C index and advanced liver fibrosis. Additionally, advanced liver fibrosis showed a significant interaction with cancer.
Discussion
Based on stringent selection standards, 3685 participants were recruited in this retrospective study. This study found that the hs-CRP/HDL-C index is positively related to MASLD, along with advanced liver fibrosis. Specifically, for each incremental rise in the hs-CRP/HDL-C index, MASLD odds increased by 82%, and the likelihood of advanced liver fibrosis escalated by 68% in a comprehensively adjusted model. Dose-response in these associations was underscored through trend tests. Furthermore, nonlinear relationships of hs-CRP/HDL-C index with MASLD and advanced liver fibrosis were identified. The threshold effect analyses indicated inflection points at 0.8 for MASLD and 1.2 for advanced liver fibrosis. Stratified analyses and interaction trials showed statistical variations across different strata in the correlation between the hs-CRP/HDL-C index and MASLD, along with advanced liver fibrosis. These findings suggest that the hs-CRP/HDL-C index may be a potential clinical marker for MASLD and advanced liver fibrosis.
Persistent inflammation is the major contributor to the progression of MASLD, potentially advancing from mere fatty degeneration to MASH, severe liver fibrosis, cirrhosis, and eventually culminating in end-stage liver disease and hepatocarcinoma25. The inflammatory response in MASLD is multifaceted, involving hepatic lipid metabolism, gut microbiome-derived signals, activation of pattern recognition receptors such as toll-like receptor 4 (TLR4), and adipose tissue-liver crosstalk, which together create a feed-forward loop of inflammation and fibrosis26. Hs-CRP, an easily quantifiable marker of inflammation, has been demonstrated in various studies to correlate with the risk of developing MASLD27,28,29. Furthermore, liver biopsy studies have demonstrated that inflammation in acinar or portal areas independently correlated with the emergence of advanced fibrosis in MASH30. These studies suggested that inflammation plays a pivotal role in predicting MASLD and its progression to fibrosis and cirrhosis on a histological level.
Notably, research has indicated impaired lipid metabolism may be another key link in the incidence and development of MASLD. Zhang and his team noted a markedly negative correlation between HDL -C and liver attenuation parameter (a metric of fat content) across their entire study cohort, with individuals afflicted with MASLD exhibiting higher average levels of plasma LDL-C31. As supporting evidence, Janac et al. observed a gradual decline in HDL-C levels as the fatty liver disease index increased32. Adding to this body of evidence, Yozgat et al.33 and Karami et al.34 identified that patients with MASLD exhibited significantly lower HDL-C levels than those without the disease. Moreover, Bril et al. observed a consistent pattern of reduced HDL-C among MASLD patients in comparison to controls, applicable to both non-obese and obese groups35. Despite the absence of research on HDL-C in relation to advanced liver fibrosis, the outcomes of the aforementioned studies offered robust and dependable evidence to elucidate the findings of this research.
The potential mechanisms behind the associations of the hs-CRP/HDL-C index with MASLD and advanced liver fibrosis remain unclear currently and possibly involve various mechanisms. Initially, the multitude of damages induced by hepatic lipid accumulation (secretion of adipokines, inflammation, lipotoxicity, and disturbances in glucose and lipid metabolism) could collaboratively pave the path from MASLD to MASH and cirrhosis36,37. Furthermore, HDL-C is known to exhibit biological properties such as reverse cholesterol transport, antioxidant activity, anti-inflammatory effects, and cellular protection38,39. A decline in HDL-C levels and the subsequent diminishment of its biological characteristics could be a reason for the heightened risk of MASLD and advanced liver fibrosis. As an inflammation-lipid composite biomarker, the hs-CRP/HDL-C index could serve as a novel and practical marker for identifying MASLD and advanced liver fibrosis, empowering clinicians with a straightforward tool to determine if a patient needs further diagnostic procedures like Fibroscan or abdominal ultrasound.
Advantages and limitations
This study showcases several pronounced advantages. Firstly, the NHANES database, renowned for its stringent quality control, offers a comprehensive national perspective. Secondly, meticulous adjustments were made for confounding covariates, aiming to diminish the bias impacts on the outcomes. Thirdly, to unearth any population-specific disparities in the associations of the hs-CRP/HDL-C index with MASLD and advanced liver fibrosis, subgroup analyses were meticulously conducted. However, some limitations warrant attention. Firstly, the study’s temporal scope is restricted to data from 2017 to 2018 due to the availability of MASLD and advanced liver fibrosis data. Secondly, despite the inclusion of multiple covariates, the exclusion of all potential confounding factors remains unattainable. Thirdly, diagnoses of MASLD and advanced liver fibrosis hinged on questionnaire surveys, lacking the precision of imaging diagnostics. Additionally, NHANES data, grounded in self-reported questionnaires, inherently bear recall bias. Lastly, the cross-sectional nature of this study precludes the establishment of clear causal relationship between the hs-CRP/HDL-C index and the prevalence of MASLD and advanced liver fibrosis.
Conclusion
In summary, this study discovered that the hs-CRP/HDL-C index correlates with the prevalence of MASLD as well as advanced liver fibrosis, indicating that the hs-CRP/HDL-C index may be able to serve as a clinical marker for evaluating MASLD along with advanced liver fibrosis.
Data availability
The data from the NHANES study that underpin the conclusions of this research are freely accessible via the provided URL: https://www.cdc.gov/nchs/nhanes/index.htm.
References
Sattar, N., Forrest, E. & Preiss, D. Non-alcoholic fatty liver disease. Bmj 349, g4596 (2014).
Rinella, M. E. et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 79 (6), 1542–1556 (2023).
Younossi, Z. M. et al. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology 77 (4), 1335–1347 (2023).
Younossi, Z. M. et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology 64 (5), 1577–1586 (2016).
Powell, E. E., Wong, V. W. & Rinella, M. Non-alcoholic fatty liver disease. Lancet 397 (10290), 2212–2224 (2021).
Tan, D. J. H., Ng, C. H., Muthiah, M. D., Loomba, R. & Huang, D. Q. Clinical features and outcomes of NAFLD-related hepatocellular carcinoma - authors’ reply. Lancet Oncol. 23 (6), e244 (2022).
Targher, G., Byrne, C. D. & Tilg, H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut 69 (9), 1691–1705 (2020).
Friedman, S. L., Neuschwander-Tetri, B. A., Rinella, M. & Sanyal, A. J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 24 (7), 908–922 (2018).
Seth, S. et al. Audit of medical (non-targeted) liver biopsy specimen quality, pathology reporting and effect on patient management. J. Clin. Pathol. 75 (7), 498–502 (2022).
Androutsakos, T. et al. Liver biopsy: to do or not to do - a single-center study. Dig. Dis. 41 (6), 913–921 (2023).
Khalifa, A. & Rockey, D. C. The utility of liver biopsy in 2020. Curr. Opin. Gastroenterol. 36 (3), 184–191 (2020).
Gao, Y. et al. The predictive value of the hs-CRP/HDL-C ratio, an inflammation-lipid composite marker, for cardiovascular disease in middle-aged and elderly people: evidence from a large national cohort study. Lipids Health Dis. 23 (1), 66 (2024).
Kumar, R. et al. Association of high-sensitivity C-reactive protein (hs-CRP) with non-alcoholic fatty liver disease (NAFLD) in Asian indians: a cross-sectional study. J. Family Med. Prim. Care. 9 (1), 390–394 (2020).
Huang, J., Wang, M., Wu, Y., Kumar, R. & Lin, S. Serum high-sensitive C-reactive protein is a simple indicator for all-cause among individuals with MAFLD. Front. Physiol. 13, 1012887 (2022).
Tang, Z. et al. Sex, Age, and BMI modulate the Association of Physical Examinations and Blood Biochemistry Parameters and NAFLD: a retrospective study on 1994 cases observed at Shuguang Hospital, China. Biomed. Res. Int. 2019, 1246518 (2019).
Hoekstra, M. & Van Eck, M. High-density lipoproteins and non-alcoholic fatty liver disease. Atheroscler Plus. 53, 33–41 (2023).
Pu, K. et al. Diagnostic accuracy of controlled attenuation parameter (CAP) as a non-invasive test for steatosis in suspected non-alcoholic fatty liver disease: a systematic review and meta-analysis. BMC Gastroenterol. 19 (1), 51 (2019).
Hashemi, S. A., Alavian, S. M. & Gholami-Fesharaki, M. Assessment of transient elastography (FibroScan) for diagnosis of fibrosis in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Casp. J. Intern. Med. 7 (4), 242–252 (2016).
Karlas, T. et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J. Hepatol. 66 (5), 1022–1030 (2017).
Sterling, R. K. et al. Evaluating noninvasive markers to identify Advanced Fibrosis by Liver Biopsy in HBV/HIV co-infected adults. Hepatology 71 (2), 411–421 (2020).
EASL-EASD-EASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD): Executive Summary. Diabetologia. (2024).
Visser, M., Bouter, L. M., McQuillan, G. M., Wener, M. H. & Harris, T. B. Elevated C-reactive protein levels in overweight and obese adults. Jama 282 (22), 2131–2135 (1999).
Appropriate body-mass. Index for Asian populations and its implications for policy and intervention strategies. Lancet 363 (9403), 157–163 (2004).
Rayburn, W. F. Diagnosis and classification of diabetes mellitus: highlights from the American Diabetes Association. J. Reprod. Med. 42 (9), 585–586 (1997).
Marjot, T., Moolla, A., Cobbold, J. F., Hodson, L. & Tomlinson, J. W. Nonalcoholic fatty liver disease in adults: current concepts in etiology, outcomes, and management. Endocr. Rev. ;41(1). (2020).
Schwärzler, J., Grabherr, F., Grander, C., Adolph, T. E. & Tilg, H. The pathophysiology of MASLD: an immunometabolic perspective. Expert Rev. Clin. Immunol. 20 (4), 375–386 (2024).
Yeniova, A. O. et al. High-sensitivity C-reactive protein is a strong predictor of non-alcoholic fatty liver disease. Hepatogastroenterology 61 (130), 422–425 (2014).
Nigam, P. et al. Non-alcoholic fatty liver disease is closely associated with sub-clinical inflammation: a case-control study on Asian indians in North India. PLoS One. 8 (1), e49286 (2013).
Duan, Y. et al. Association of Inflammatory Cytokines with non-alcoholic fatty liver disease. Front. Immunol. 13, 880298 (2022).
Argo, C. K., Northup, P. G., Al-Osaimi, A. M. & Caldwell, S. H. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J. Hepatol. 51 (2), 371–379 (2009).
Zhang, Y. et al. The liver steatosis severity and lipid characteristics in primary biliary cholangitis. BMC Gastroenterol. 21 (1), 395 (2021).
Janac, J. et al. The association between lecithin-cholesterol acyltransferase activity and fatty liver index. Ann. Clin. Biochem. 56 (5), 583–592 (2019).
DeFilippis, A. P. et al. Nonalcoholic fatty liver disease and serum lipoproteins: the multi-ethnic study of atherosclerosis. Atherosclerosis 227 (2), 429–436 (2013).
Karami, S. et al. Association of anti-oxidative capacity of HDL with subclinical atherosclerosis in subjects with and without non-alcoholic fatty liver disease. Diabetol. Metab. Syndr. 13 (1), 121 (2021).
Bril, F. et al. Hepatic steatosis and insulin resistance, but not Steatohepatitis, promote atherogenic dyslipidemia in NAFLD. J. Clin. Endocrinol. Metab. 101 (2), 644–652 (2016).
Tilg, H. & Moschen, A. R. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology 52 (5), 1836–1846 (2010).
Buzzetti, E., Pinzani, M. & Tsochatzis, E. A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 65 (8), 1038–1048 (2016).
Kosmas, C. E. et al. High-density lipoprotein (HDL) functionality and its relevance to atherosclerotic cardiovascular disease. Drugs Context. 7, 212525 (2018).
Zhang, L., Shi, Y., Liang, B. & Li, X. An overview of the cholesterol metabolism and its proinflammatory role in the development of MASLD. Hepatol. Commun. ;8(5). (2024).
Acknowledgements
The authors express profound gratitude towards both the dedicated investigators and the engaged participants of the NHANES database for their invaluable contributions to this research. We extend our heartfelt thanks to the creators of EmpowerStats for their pivotal support and advanced analytical tools that greatly enhanced our study.
Author information
Authors and Affiliations
Contributions
BL and XQ were responsible for study design, data collection, data analysis, and drafting the manuscript. JH contributed to data interpretation and provided valuable feedback throughout the research process. YL assisted in creating visual representations of the data and contributed to the editing of the manuscript. HS offered scholarly oversight and guidance throughout the study. JM and YC contributed to the research direction and played a significant role in the subsequent revisions of the manuscript. All authors have reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, B., Qiu, X., Huang, J. et al. Nonlinear associations of the hs-CRP/HDL-C index with metabolic dysfunction-associated steatotic liver disease and advanced liver fibrosis in US adults: insights from NHANES 2017–2018. Sci Rep 15, 4029 (2025). https://doi.org/10.1038/s41598-025-88685-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88685-y
Keywords
This article is cited by
-
Association between hs-CRP/HDL-C ratio and risk of prediabetes or diabetes: a cross-sectional study based on NHANES 2015–2023
BMC Endocrine Disorders (2025)
-
S-shaped association between hs-CRP/HDL-C index and overweight/obesity in children and adolescents: a population-based study
European Journal of Medical Research (2025)