Abstract
Cancer treatment using systemic therapy and radiotherapy may cause post-therapy complications, resulting in increased unplanned hospitalisation. The evidence on such complications, their impact on unplanned hospitalisations, and associated costs is scant in Australia. We aimed to estimate the prevalence of post-therapy complications, evaluate their impact on unplanned hospitalisation, length of stay (LOS) and investigate the associated medical costs. A retrospective cohort study was conducted among 8,633 cancer patients (1.03 million emergency hospital admissions) in Victoria, Australia from July 2006 to June 2020, from the Australian healthcare system perspective. Multivariate generalised linear regression models were employed to estimate the adjusted association between post-therapy complications and clinical characteristics with hospital LOS and associated hospitalisation medical costs. Approximately 52% of patients were male with an average patient age of 59.9 years. Annually, post-therapy complications leading to unplanned hospitalisations increased by 7.25%, outpacing the growth in overall hospitalisation admissions, which was 5.66% for overall hospitalisation admissions. A significant proportion of patients (71%) experienced multiple complications, with the most common being anemia (26%), sepsis (15%), nausea and vomiting (14%), and neutropenia (11%). Patients undergoing combined systemic and radiotherapy exhibited higher odds of post-therapy complications (OR = 8.24, 95%CI: 7.48 to 9.08) compared with those who only received systemic therapy. Mean hospital stay among patients who experienced post-therapy complications was 2.23 days per admission (360 days per patient), an extra 1.72 days per admission [95%CI: 1.68 to 1.76; 354 days per patient, 95%CI: 336 to 371 days] longer than patients without complications (0.51 days per admission and 6.48 days per patients). Overall, per-admission medical hospitalisation costs among patients with post-therapy complications were $8,791 higher than for patients who did not experience complications ($11,418 vs. $2,627 per admission, 95%CI: $8,685 to $8,897). Per-patient costs for unplanned hospitalisation due to post-therapy complications were significantly $1.82 million higher among patients than those without complications ($1.86 million vs. $33,599 per patient, 95%CI: $1.71 million to $1.94 million). The cost and hospitalisation stay (in days) varied by the type of therapy and cancer type. The study results indicate that post-therapy complications in cancer patients varied by the type of cancer and increased over the study period, leading to longer unplanned hospital stays and higher hospitalisation medical costs. The results highlight the need for better-customized treatment delivery strategies to address this burden and optimise resources in cancer care.
Similar content being viewed by others
Introduction
Cancer continues to be a major global health challenge1, contributing to the disease burden worldwide, including in Australia where it accounts for approximately 17% of the total disease burden in 20222. In 2023, about 165,000 Bangladeshi were diagnosed with cancer, facing a mortality rate of 195 per 100,000 individuals3. These numbers are projected to rise dramatically by 2044, with incidence and mortality rates expected to by 51% and 36%, respectively. The economic impact of cancer is also substantial, with expenditures reaching AU$10.1 billion in 2016, representing 8.6% of total disease expenditures in Australia4. The cost associated with hospital admissions for cancer treatments, including systemic therapy and radiotherapy, significantly contributes to this financial burden.
Advances in cancer treatment over the last decade have improved patient outcomes significantly5. Around 323,000 cancer patients in Australia receive systemic therapy or radiotherapy annually, with around 160,000 patients receiving both6,7, which are essential components of cancer treatment protocols. These modalities not only enhance quality of life but also extend overall survival8. However, the effectiveness of these treatments varies based on the severity of the disease9, and is not without risks10,11. Notably, severe post-therapy complications often lead to unplanned hospitalisations, straining healthcare resources. A study highlighted that 90% of cancer patients hospitalised after emergency visits suffered from post-therapy complications, with a significant impact on hospital length of stay (LOS) and associated costs12.
Despite the benefits, systemic therapy and radiotherapy can lead to adverse effects13,14,15 such as sepsis, neutropenia, and pneumonia14,15,16,18, necessitating hospital care14, particularly for older adults and advanced-stage patients16. These complications not only exacerbate patient suffering but also interrupt ongoing cancer treatment, potentially derailing therapeutic outcomes13,19. Additionally, these unplanned hospitalisations represent a heavy economic burden on patients, families14, and the healthcare system, with the primary treatment phase alone costing over $6 billion annually20.
The growing prevalence of cancer and the consequential increase in therapy-related complications underscore the need for comprehensive research to inform clinical and policy decisions. To our knowledge, there is currently no clear evidence-based research at a local or national level in Australia that examines the diversity of emergency admissions and inpatient care based on the cancer type and stage. In addition, evidence on post-therapy complications is limited in Australia which could help develop an oncology care model and reflect the reality of cancer care in the Australian healthcare system. To address this evidence gap, this study aimed to estimate the incidence of post-therapy complications due to systemic therapy and radiotherapy complications, measure their impact on hospitalisations, including LOS, and estimate that associated hospitalisation costs and factors associated hospitalisation among cancer patients in Victoria, Australia.
We hypothesise that different post-therapy complications occurring from systemic therapy and radiotherapy have significant impacts on healthcare systems, resulting in longer unplanned hospital LOS and higher hospitalisation medical costs, with some potential factors contributing more significantly than others.
Methods
Study design and setting
A retrospective cohort study was conducted in Victoria, Australia, to investigate the post-therapy complications of systemic therapy and radiotherapy among cancer patients over a 14-year period (2006–2020). This study analysed administrative health data of the admitted patients to comprehensively examine treatment-related complications, and hospitalisation events, and their associated medical costs from the Australian healthcare system perspective. Patient demographics, clinical characteristics, clinical and administrative details for admitted episode of care records were extracted from linked data source (i.e., Victorian Admitted Episodes Dataset, VAED) from 2006 to 2020. The VAED provides a comprehensive dataset of the causes, effects and nature of illness, and the usage of health services in Victoria.
Study population
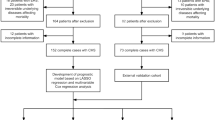
The study population included patients at their first cancer diagnosis, even if they were diagnosed with multiple types of cancer. The study included patients who fulfilled the following criteria: (i) having a diagnosis of any cancer (only considered the first cancer diagnosis), (ii) have received systemic therapy and/or radiotherapy between 2006 and 2020, and (iii) have complete medical record data available, including ‘International Classification of Diseases (ICD) 10th version (ICD-10) codes or Australian Classification of Health Intervention (ACHI) codes for treatment. The records of cancer patients who could not meet these criteria were excluded from the analysis (Fig. 1). Systemic therapy and radiotherapy were defined based on available data (ACHI codes or ICD-10codes, see Appendix Table A1). In addition, we excluded patients who experienced post cancer-therapy related complications more than 5 years after the first date of therapy.
Outcome measures
This study considered outcome measures: (i) post-therapy complication status, (ii) unplanned LOS in days due to post-therapy complications, and (iii) associated hospitalisation costs, valued in Australian dollars.
Hospital length of stay (LOS)
Unplanned hospital LOS for post-cancer treatment-related therapy was defined as the number of days from hospital admission to discharge. Therefore, the LOS was calculated as the discharge date minus the hospital admission date for both patients with treatment-related complications and without complications. We calculated a LOS for each admission. If a patient did not experience any cancer-therapy related complications, their hospital admission was solely for post-cancer treatment-related therapy. Then after, the comparative analysis of LOS between these two groups (complication vs. non-complication) were conducted. We have detailed the hospitalisation process in Fig. 1.
Hospitalisation costs for post-therapy complications
From the perspective of the Australian healthcare system, the medical costs associated with hospitalisation are calculated based on a unit of measurement known as ‘National Weighted Activity Units (NWAUs)’, which are assigned to each inpatient hospital admission21. NWAUs are used as the standard unit of measurement of hospital activity in Australia, against which the ‘National Efficient Price (NEP)’ is applied, and ‘activity-based funding (ABF)’ is provided to hospitals. To calculate the total hospitalisation medical cost for each admission, the NWAU for that admission is multiplied by the NEP, which is currently AU$ 5,134 per national weighted activity unit for the fiscal year 2019-20, to determine the cost to the healthcare system. Admitted acute ABF costs were calculated based on the AR-DRG classification related to systemic therapy and radiotherapy-related complications. National cost weights as determined by the ‘Independent Hospital Pricing for each AR-DRG code’ were then applied to determine admitted acute hospital costs22. Each patient’s hospitalisation medical cost comprised the total cost of an admitted acute ABF AR-DRG presentation. Costs were reported as mean and rounded to the nearest whole Australian dollars (AU$), using the 2020 reference year22.
Measure of post-therapy complications Occurrence of systemic therapy and radiotherapy-related complications, which were defined according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM) codes was the main exposure variables in the study (Appendix Table A2). We considered any post-therapy complications that emerged subsequent to the first administration date of systemic therapy or radiotherapy. The prevalence of treatment-related complications was calculated based on the most reported complications. In addition, the status of post-therapy complications was categorised as follows: 1 indicates patients who reported at least one therapy (i.e., systemic therapy and/or radiotherapy) related complication during the post-therapy period and reported on subsequent hospitalisation, while 0 indicates patients who did not report any such complication.
Covariates
Relevant covariates with a known or hypothesised association with the exposure variables or outcomes of interest (unplanned hospital LOS and hospitalisation medical costs) were identified from published literature14,19,23,25,26,27,28,29,30,31. Several covariates were included in regression models to answer each research question as outlined below. Sociodemographic factors were ascertained, including age (categorised as 18–25 years; 26–35 years; 36–45 years; 46–55 years; 56–65 years; >65 years), sex (male or female), Indigenous status, and year of cancer diagnosis.
Statistical considerations
In the descriptive analyses, patient’s characteristics were presented using frequencies, n (%) for categorical variables or mean (standard deviation, SD) for continuous data. A single imputation approach was applied to replace missing data with a single predicted value for estimating hospitalisation medical costs, such as the mean for a given case32. Continuous nature of data (i.e. unplanned hospital LOS in days and associated hospitalisation costs) was presented as mean with SD and mean differences between the two groups (with and without a diagnosis of post-therapy complications). The univariate analysis consisted of a non-parametric bootstrapping approach (with 1,000 replications) through a Generalised Linear Models (GLM) to assess the statistical significance of differences with 95% confidence intervals [CIs] in unplanned hospital LOS days [or hospitalisation medical costs]. For categorical data, the chi-square test was used to compare the post cancer therapy-related complications status (present or absent), by patients’ characteristics.
For the univariate and multivariable analyses, the estimation approach was based on the nature of the outcome variables in each model. Unadjusted and adjusted associations were estimated between unplanned hospital LOS (or hospitalisation medical costs) and the main exposure variables using the GLM with a log-link, gamma distribution, and robust estimates of variance. In addition, a logistic regression model was used to determine the association between post-therapy complications and patients’ characteristics. The reference group selected was the lower risk category of covariates. All statistical significance was considered as p-value < 0.05. All analyses were performed using the statistical software Stata/BE 18. This study has reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement for cohort studies33. All methods were carried out in accordance with relevant national guidelines and institutional regulations.
Results
Characteristics of the study population
A total of 8,633 patients with cancer were included in this study (Table 1). The mean age of the patients was 59 years, and approximately 65% of them were 56 years or older, and 52% were male. Most patients (98%) were not of Aboriginal or Torres Strait background. About 92% of patients received systemic therapy and 4.33% of them received radiotherapy, whereas 4% of the participants received both systemic therapy and radiotherapy (Table 1). Between 2006 and 2020, there were 1,035,294 hospital admissions associated with these patients, out of which 1,004,036 were identified as being associated with post-therapy complications (Appendix Table A3).
Diagnosis of post-therapy complications due to systemic therapy and radiotherapy
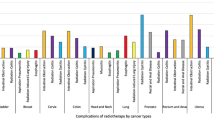
The most common complications were reported as follows: anemia at 26%, sepsis at 15%, nausea and vomiting at 14%, neutropenia at 11% and pneumonia at 9% (Fig. 2).
A significant majority of hospital admissions (94%; n = 945,846) were associated with post-cancer therapy complications among patients undergoing systemic therapy (Appendix Table A3). Notably, patients who received both systemic therapy and radiotherapy exhibited an 8.24-fold increase in the odds of experiencing post-therapy-related complications (OR = 8.24, 95% CI: 7.48 to 9.08, p < 0.001) compared with those who received systemic therapy alone. The odds of having post-therapy complications varied significantly with cancer type. Patients with acute lymphoblastic leukemia (OR = 16.99, 15.42 to 18.71), multiple myeloma (OR = 9.72, 9.00 to 10.5), melanoma (OR = 3.62, 3.20 to 4.09) showed the highest odds of complications. Increased odds were also noted for cancers of the kidney (OR = 3.54, 2.85 to 4.40), Hodgkin lymphoma (OR = 2.97, 2.75 to 3.20), esophageal cancer (OR = 2.43, 1.96 to 3.10), non-Hodgkin lymphoma (OR = 2.19, 2.06 to 2.33), and stomach cancer (OR = 2.30, 1.81 to 2.91) (Appendix Table A3).
Approximately41% of female patients experienced at least one post-therapy complication. Compared to male patients, female patients had 16% lower odds of developing complications (OR = 0.84, 0.81 to 0.86). The odds of experiencing post-cancer therapy increased significantly with patient age (p < 0.001, Table 1). Patients aged 56 to 65 years had a 1.44-fold higher odd (OR = 1.44, 1.28 to 1.62), and or those older than 65 years had a 1.51-fold higher odd (OR = 1.99, 1.77 to 2.25) compared to were found to be 1.51 times more likely to experience post-therapy complications that the younger counterparts. Moreover, approximately 62% of post-therapy complications associated with this age group. There was a notable decline in the prevalence of post-therapy complications from 31% in 2006–2009 to 10% in 2016–2018.
Distribution of hospitalisation length of stay (LOS) in days and hospitalisation medical costs
Patients experiencing post-therapy complications had a significantly longer mean hospital stay, with 2.23 days per admission (Table 2), equating to 360 days per patient (Table 3), compared to those without complications, who had 0.51 days per admission and a total of 6.48 days per patient. This difference in LOS resulted in an additional 1.72 days per admission (95%CI: 1.68 to 1.76) and 354 days per patient (336 to 371).
Patients undergoing both systemic therapy and radiotherapy with complications also exhibited extended hospital LOS, with a mean difference of 1.38 days, resulting in 354 days per patient as opposed to 19.87 days per patients for those without complications. Male patients with complications had a longer LOS of 2.29 days compared to 0.54 days for those without, showing a significant difference of 1.72 days per admission (p < 0.001).
Patients with post-therapy complications incurred substantially higher hospitalisation costs, averaging AU$11,418 per admission in stark contrast to AU$2,627 for those without complications. This difference led to an excess cost of AU$8,791 per admission (8,685 to 8,897; p < 0.001; Table 4).
Per-patient costs for unplanned hospitalisation due to complications were dramatically higher at $1.82 million compared to AU$33,599 for those without complications, with a confidence interval ranging from AU$1.71 million to AU$1.94 million (Table 5). Cost disparities were also notable in patients receiving systemic therapy alone or in combination with radiotherapy, with those having complications incurring AU$11,335 and AU$12,279 per admission, respectively, significantly higher than those without complications (AU$2,371 and AU$5,281 per admission, respectively). Male patients with post-therapy complications faced an average hospitalisation cost of AU$11,729 per admission, significantly higher by AU$2,806 than those without complications (AU$ 8923 per admission). This trend was similar among female patients. Over time, hospitalisation costs have increased notably, with expenses for patients with complications tripling from AU$10,642 per admission in 2006–2009 to AU$27,930 per admission in 2019–2020 (Table 4).
Factors associated with length of stay (LOS) in days per admission and hospitalisation medical costs
Table 6 presents the results of two different models for analysing hospitalisation LOS and the associated costs per admission. Potential variables were adjusted based on qualified variables from the unadjusted explorations (Appendix Table A4). The regression analysis revealed that patients who had complications after therapy had a significantly longer hospital LOS (β = 1.30, 1.25 to 1.35) and higher medical costs (β = 1.29, 1.26 to 1.33). However, the results varied depending on the patient’s characteristics and of the specific cancer diagnosis. For instance, patients aged 65 and above had a significantly longer hospital LOS per admission (β = 0.37, 0.33 to 0.40) and higher hospitalisation medical costs (β = 0.36, 0.34 to 0.39) compared with younger patients aged 18 to 25 years.
Discussion
This study provides a comprehensive analysis of post-therapy complications among cancer patients, highlighting significant increases in hospitalisation length of stay (LOS) and medical costs. Notably, 72% of patients developed complications post-systemic and/or radiation therapy, predominantly manifesting as anemia, sepsis, nausea and vomiting, and neutropenia. The types of cancer most frequently associated with these complications were acute lymphoblastic leukemia, multiple myeloma, melanoma, kidney, Hodgkin lymphoma, esophageal cancer, non-Hodgkin lymphoma, and stomach among the participants. Patients experiencing post-therapy complications had an average increase in hospital LOS by 1.72 additional days, reflecting unplanned extensions beyond their initial treatment plans. These patients also faced significantly higher hospitalisation costs, with additional expenses averaging AU$8,791 compared to those without complications.
Our analysis revealed that patients who underwent both systemic therapy and radiotherapy had an 8.24 times higher chance of experiencing post-therapy complications compared with those who only received systemic therapy. These findings are consistent with previous studies that also showed a correlation between receiving cancer therapies and post-therapy complications34,36,37. This increased risk might be attributable to the cumulative toxic effects of multiple therapies on patient health, as suggested in other studies34,36,37. This comparative insight is crucial for healthcare providers in strategising care to mitigate these risks, particularly in treatments involving multiple therapy modalities38.
This study highlighted the significance of post-therapy and revealed that patients who experienced complications, such as prolonged following therapy, had significantly longer unplanned hospital stays and compared with those who did not experience any complications. This finding is consistent with published data that indicates patients with post-therapeutic complications have longer hospital stays and higher treatment costs12,14,18,19,39. These results reinforce the critical need for effective monitoring and management of patients during and after cancer treatment to mitigate the risks associated with post-therapy complications. Such complications not only impose a substantial economic burden on patients and the healthcare system but also potentially delay ongoing cancer treatment40, adversely affecting patient outcomes. It is imperative that healthcare providers implement robust strategies for early identification and management of potential complications. Assessing factors such as performance status, organ function, comorbidity, and patient frailty can guide clinicians in tailoring treatment plans that minimise the risk of adverse effects18,34,41. Moreover, proper communication with patients about the potential for hospitalisations and other treatment-related adverse events is essential. Providing detailed information helps patients make informed decisions about their treatment options, balancing the benefits against the risks. This approach can significantly improve the quality of care, reduce the impact on healthcare resources, and enhance the overall quality of life for patients and their caregivers.
Treatment-related complications, including anemia, sepsis, and neutropenia that occur after systemic and radiotherapy, have been found to be associated with longer hospitalisation stay per admission. Cancer patients undergoing active treatment are often immunocompromised, which makes them more susceptible to sepsis leading to mortality. Previous studies show that cancer patients have a higher incidence of severe sepsis, which results in increased hospitalisation and mortality14,18. For example, cancer patients with severe sepsis stayed in hospital for almost three times as long as cancer patients without severe sepsis14,18. Anemia is also prevalent among cancer patients and can lead to longer hospitalisation in the oncology unit31,42. These occurrences can adversely impact overall survivorship, quality of life, and increase length of hospital stay43. Neutropenia is another severe complication of chemotherapy among cancer patients. Patients who experience neutropenia mostly have longer hospitalisation periods44. Another study found that neutropenia is a life-threatening toxic effect of chemotherapy that can be responsible for longer hospital LOS39. However, the toxicity profile of each cancer treatment modality varies according to dosages, treatment duration, and patient characteristics. These findings highlight the need to manage these complications effectively with supportive measures at home or by increasing outpatient monitoring. Furthermore, it underlines the importance of preventing hospitalisation due to therapy-related complications to optimise patient outcomes. While the reasons for prolonged LOS without complications were not directly examined in this study. However, previous studies indicated that factors including pain, infection and dyspnea can influence hospitalisation14,24,31,41,45.
Study strengths and limitations
The main strength of this study was the use of a large cohort of cancer patients from Victoria, Australia. Data was extracted from administrative linked data sources, including the Victorian Admitted Episodes Dataset, for the period between 2006 and 2020. These administrative datasets are based on hospital data compiled by individual public and private hospitals through two hospital networks in Victoria, Australia. This study conducted a 14-year longitudinal analysis among medically diagnosed cancer patients, allowing the identification of trends and changes in the burden of post-therapy complications over time. By capturing associations, this analysis aids in understanding how therapy practices and patient health outcomes have evolved. It is important to note that while this study identifies associations, it does not establish causality between treatment practices and patient outcomes. This study adopted a comprehensive approach by investigating complications from several aspects, including clinical characteristics, hospitalisation, and healthcare system costs from the Australian healthcare system perspective. This multifaceted exploration improves the understanding of the complexities surrounding post-therapy complications.
This study has some limitations such as data was collected from only two hospital networks in metropolitan Victoria. However, it is important to note that the results may not be fully representative of the entire state and might be biased towards a particular population. To ensure accurate and reliable results, a more comprehensive study would be required, which would involve collecting data from a state-wide cancer registry and including data from all state hospitals. By doing so, we can ensure that our findings are based on extensive and diverse data, and that we can make confident and reliable conclusions. The study was conducted from the Australian healthcare system perspective and assessed the direct medical costs of unplanned hospitalisation due to post-therapy complications in cancer patients. However, patients who experience post-therapy complications may also incur greater indirect costs, such as psychological stress, reduced productivity in daily activities, and increased time off from work and additional care burdens on their family members. In order to perform rigorous explorations for the economic analysis of post-therapy complications, healthcare utilisation data, including Medicare claims through the Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Schedule (PBS) claims data, is required. Unfortunately, we were unable to capture all aspects of healthcare use and assess the long-term economic impact of these cancer patients due to a lack of data access and funding. The substantial group size imbalance, with the majority of patients receiving systemic therapy only, may have impacted the precision of estimates, and this limitation should be considered when interpreting the findings. We acknowledge that the stages of cancer among patients may significantly influence the choice of treatment modalities and subsequent risk of complications, which may not be fully captured by the analysis of this specific subgroup within our study. Moreover, the study considered post-therapy complications according to the study design and research questions, while cancer patients may also be diagnosed with non-cancer chronic comorbid conditions or diseases, which may contribute to a higher disease burden and hospitalisation events. However, we acknowledge that the inclusion of performance status, comorbidity indices, frailty, and organ function could enrich the analysis, providing a more nuanced understanding of risk factors associated with post-therapy complications and their economic impact. The absence of these variables in our analysis is indeed a limitation, as it could affect the depth of risk stratification and potentially influence the interpretation of our findings. Therefore, future research is required using a similar study design that captures all relevant aspects of healthcare use in an economic assessment to provide robust evidence for policymakers and stakeholders. In addition, we recommend that future clinical studies with larger subsets of patients receiving combined therapies be conducted to validate and expand upon these findings.
Implications and key recommendations
The research findings have several policy implications for the Australian healthcare system, addressing various aspects of cancer care and post-therapy complications. This study proposes some key recommendations:
-
(1)
Develop risk stratification models to accurately identify patients at a higher risk of post-therapy complications. This should focus on factors such as age, gender, health conditions, and specific cancer types. Implement targeted interventions for these high-risk groups to ensure early detection, monitoring, and effective management of complications.
-
(2)
Given the observed higher risk of complications among patients receiving both systemic therapy and radiotherapy—despite the small size of this subgroup—, it is prudent to advocate, for a more cautious approach. We recommend the implication of tailored treatment protocols for these patients, which include enhanced monitoring and coordinated care. These protocols should focus on active surveillance, early detection, and prompt management of potential complications. This approach may help mitigate the risks associated with combined treatment modalities and improve patient outcomes.
-
(3)
Establish strategies for continuous monitoring and enhancement of the quality of cancer care. Consistently assess the occurrence of post-therapy complications, evaluate the impact on hospitalisation, and adjust healthcare practices accordingly. This could involve regular assessments and incorporating lessons learned into clinical guidelines.
Conclusion
This study provides evidence of the economic impact of post-therapy complications and associated unplanned hospitalisation on cancer patients and the healthcare system. The research offers a compilation of the most reported complications, highlighting the prevalence of anemia, sepsis, nausea and vomiting, neutropenia, pneumonia, and acute kidney failure. This information is essential for adopting or introducing interventions that may mitigate and effectively manage these specific complications in cancer care. The study also revealed that post-therapy complications significantly increase unplanned hospitalisation LOS and associated hospitalisation medical costs. This underscores the importance of effective management of post-therapy complications to optimise the use of healthcare resources.
Data availability
The data underlying this article will be shared upon reasonable request to the corresponding author.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer. J. Clin. 71, 209–249 (2021).
Australian Institute of Health and Welfare and Australian Government. Australian Burden of Disease Study 2023. Cat. No: BOD 39, Australian Government (2023).
Australian Institute of Health and Welfare and Australian Government. Cancer data in Australia. Overview of cancer in Australia. 2023. https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/overview-of-cancer-in-australia-2023 (Accessed 23 November 2023) (2023).
Australian Institute of Health and Welfare. Health System Expenditure on cancer and Other Neoplasms in Australia, 2015–16. Cancer Series no. 131. Cat. no. CAN 142 (AIHW, 2021).
Elmore, L. W. et al. Blueprint for cancer research: critical gaps and opportunities. Cancer J. Clin. 71, 107–139 (2021).
Tervonen, H. E., Creighton, N., Zhao, G. W., Ng, M. & Currow, D. C. Capture of systemic anticancer therapy use by routinely collected health datasets. Public Health Res. Pract. 30, 3–6 (2020).
Australian Institute of Health and Welfare. Radiotherapy in Australia 2018–19 (2020).
de Boer, S. M. et al. Adjuvant chemoradiotherapy versus radiotherapy alone in women with high-risk endometrial cancer (PORTEC-3): patterns of recurrence and post-hoc survival analysis of a randomised phase 3 trial. Lancet Oncol. 20, 1273–1285 (2019).
Shahjalal, M. et al. Assessing health related quality of life among cancer survivors during systemic and radiation therapy in Bangladesh: a cancer specific exploration. BMC Cancer. 23, 1–13 (2023).
Toale, K. M., Johnson, T. N. & Ma, M. Q. Chemotherapy-Induced Toxicities. In: (eds Todd, K. H. & Thomas, C. R.) Oncologic Emergency Medicine: Principles and Practice. Geneva, Switzerland: Springer; 381–406. (2016).
FitzGerald, T. J. et al. Treatment toxicity: Radiation. In: (eds Todd, K. H. & Thomas, C. R.) Oncologic Emergency Medicine: Principles and Practice. Springer, Cham; 663–677. (2021).
Adelson, K. B., Dest, V., Velji, S., Lisitano, R. & Lilenbaum, R. Emergency department (ED) utilization and hospital admission rates among oncology patients at a large academic center and the need for improved urgent care access. J. Clin. Oncol. 32(30_suppl), 19 (2014).
Brooks, G. A. et al. A clinical prediction model to assess risk for chemotherapy- related hospitalization in patients initiating palliative chemotherapy. JAMA Oncol. 1, 441–447 (2016).
Jairam, V. et al. Treatment-related complications of systemic therapy and radiotherapy. JAMA Oncol. 5, 1028–1035 (2019).
Hong, A. M. et al. The benefit for radiotherapy at specialised sarcoma centres: a systematic review and clinical practice guidelines from the Australia and New Zealand Sarcoma Association. Radiother. Oncol. 177, 158–162 (2022).
Manzano, J. G. M., Luo, R., Elting, L. S., George, M. & Suarez-Almazor, M. E. Patterns and predictors of unplanned hospitalization in a population-based cohort of elderly patients with GI cancer. J. Clin. Oncol. 32, 3527–3533 (2014).
Rocha, P. H. P. et al. Adverse radiation therapy effects in the treatment of head and neck tumors. Radiographics 42, 806–821 (2022).
Williams, M. D. et al. Hospitalized cancer patients with severe sepsis: analysis of incidence, mortality, and associated costs of care. Crit. Care. 8, 1–8 (2004).
O’Neill, C. B. et al. Hospitalizations in older adults with advanced cancer: the role of chemotherapy. J. Oncol. Pract. 12, e138–e148 (2016).
Goldsbury, D. E. et al. Health services costs for cancer care in Australia: estimates from the 45 and up study. PLoS One. 13, e0201552 (2018).
IHPA. National Weighted Activity Unit (NWAU) calculators 2019-20. Independent Hospital Pricing Authority (IHPA)-National Efficient Price Determination. (2020).
IHPA. National efficient price determination 2018-19. Independent Hospital Pricing Authority (IHPA). (2018).
Andrianopoulos, N., Jolley, D., Evans, S. M., Brand, C. A. & Cameron, P. A. Application of variable life adjusted displays (VLAD) on victorian admitted episodes dataset (VAED). BMC Health Serv. Res. ;12. (2012).
Rivera, D. R. et al. Trends in adult cancer-related emergency department utilization: an analysis of data from the nationwide emergency department sample. JAMA Oncol. 3, e172450 (2017).
Berecki-Gisolf, J., Fernando, T. & D’Elia, A. Trends in mortality outcomes of hospital-admitted injury in Victoria, Australia 2001–2021. Sci. Rep. 13, 1–9 (2023).
Dulisse, B. et al. A retrospective study of the clinical and economic burden during hospitalizations among cancer patients with febrile neutropenia. J. Med. Econ. 16, 720–735 (2013).
Haffty, B. G. Long-term results of hypofractionated radiation therapy for breast cancer. Breast Dis. 21, 267–268 (2010).
Albano, D. et al. Imaging side effects and complications of chemotherapy and radiation therapy: a pictorial review from head to toe. Insights into Imaging. 12, 1–28 (2021).
Chin, V. et al. Chemotherapy and radiotherapy for advanced pancreatic cancer. Cochrane Database of Systematic Reviews. CD011044:1–168. (2018).
Minami-Shimmyo, Y. et al. Risk factors for treatment-related death associated with chemotherapy and thoracic radiotherapy for lung cancer. J. Thorac. Oncol. 7, 177–182 (2012).
Saxena, A. et al. Hospitalization rates for complications due to systemic therapy in the United States. Sci. Rep. 11, 1–7 (2021).
Gabrio, A., Mason, A. J. & Baio, G. Handling missing data in within-trial cost-effectiveness analysis: a review with future recommendations. PharmacoEconomics - Open. 1, 79–97 (2017).
von Elm, E. et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J. Clin. Epidemiol. 61, 344–349 (2008).
Rabello, L. S. C. F. et al. Clinical outcomes and microbiological characteristics of severe pneumonia in cancer patients: a prospective cohort study. PLoS ONE. 10, 1–13 (2015).
Zhou, X. H., Melfi, C. A. & Hui, S. L. Methods for comparison of cost data. Ann. Intern. Med. 127, 752–756 (1997).
Olson, R. et al. Population-based comparison of two feeding tube approaches for head and neck cancer patients receiving concurrent systemic-radiation therapy: is a prophylactic feeding tube approach harmful or helpful? Support. Care Cancer. 21, 3433–3439 (2013).
Mohan, G., P, A. H. T., Narayanasamy, J. J. A. M. S. D. K. & Vellingiri, A. Recent advances in radiotherapy and its associated side effects in cancer—a review. Scandinavian J. Rheumatol. Supplement. 80, 1–10 (2019).
Warde, P. et al. Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial. Lancet 378, 2104–2111 (2011).
Caggiano, V., Weiss, R. V., Rickert, T. S. & Linde-Zwirble, W. T. Incidence, cost, and mortality of neutropenia hospitalization associated with chemotherapy. Cancer 103, 1916–1924 (2005).
Abdelfatah, E., Ramos-Santillan, V., Cherkassky, L., Cianchetti, K. & Mann, G. High risk, high reward: Frailty in colorectal cancer surgery is associated with worse postoperative outcomes but equivalent long-term oncologic outcomes. Sci. Rep. 30, 2035–2045 (2023).
Hassett, M. J. et al. Chemotherapy-related hospitalization among community cancer center patients. Oncologist 16, 378–387 (2011).
Seshadri, T. et al. The Australian cancer anaemia survey: a snapshot of anaemia in adult patients with cancer. Med. J. Aust. 182, 453–457 (2005).
Doni, L. et al. The impact of anemia on quality of life and hospitalisation in elderly cancer patients undergoing chemotherapy. Crit. Rev. Oncol. Hematol. 77, 70–77 (2011).
Nguyen, M., Jacobson, T., Torres, J. & Wann, A. Potential reduction of hospital stay length with outpatient management of low-risk febrile neutropenia in a regional cancer center. Cancer Rep. 4, 2–5 (2021).
Mahumud, R. A. et al. Systemic therapy and radiotherapy related complications and subsequent hospitalisation rates: a systematic review. BMC Cancer. 24 (1), 826 (2024).
Author information
Authors and Affiliations
Contributions
All authors critically reviewed earlier versions of the draft and approved the final manuscript. RAM and OW conceived the paper. RAM, OW, KA, JG, MS, PKD, and MPM developed the analysis plan. RAM did the analysis and wrote the initial draft. RAM, MS, PKD, MPM, KA, JG, AMNR, MGH, SKM, KNK, SHC and OW contributed to the write up and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
To ensure compliance with ethical standards and participant confidentiality, we obtained ethical approval from the ‘Royal Melbourne Hospital Human Research Ethics Committee’ (approval # 202201/1). The data were de-identified to maintain anonymity prior to analysis. Due to the retrospective nature of the study, Royal Melbourne Hospital Human Research Ethics Committee waived the need of obtaining informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mahumud, R.A., Shahjalal, M., Dahal, P.K. et al. Emerging burden of post-cancer therapy complications on unplanned hospitalisation and costs among Australian cancer patients: a retrospective cohort study over 14 years. Sci Rep 15, 4709 (2025). https://doi.org/10.1038/s41598-025-89247-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-89247-y
Keywords
This article is cited by
-
Assessing inequalities in health utility scores among cancer patients undergoing systemic and radiation therapy
Health and Quality of Life Outcomes (2025)