Abstract
This study aims to explore the effect of implant apex design, osteotomy preparation, intraosseous depth and bone quality on immediate implant placement insertion torque and establish a more sophisticated decision model with multi-factor analysis based on machine learning for improving the success rate of immediate implant placement. Six implant replicas of each of the three implant systems with different implant apex design were placed in polyurethane foam block with different densities(soft, medium and hard) via two osteotomy preparation protocols (normal preparation and undersized preparation) at different implant intraosseous depths (3 mm, 5 mm and 7 mm). The insertion torque for each implant was recorded and subsequently analyzed using one-way and four-way ANOVA. Prediction models of insertion torque were then constructed using multiple linear regression (MLR) and decision tree regression (DTR) analyses based on multi-factors. These machine learning models were evaluated and compared for their predictive accuracy and performance. The influencing factors of immedate implant placement insertion torque are ranked as follows: bone quality, intraosseous depth, osteotomy preparation protocol, and implant apex design. Both two machine learning preoperative prediction models (MLR and DTR) showed high accuracy in insertion torque prediction, with the latter’s R2 reaching as high as 0.951. This research is of significant reference value for optimizing clinical decision-making, improving the success rate of immediate implant placement, and enhancing the efficiency of doctor-patient communication. In addition, this study further refined the evaluation framework for implant performance, rendering it more comprehensive and standardized.
Similar content being viewed by others
Introduction
Immediate implant placement at the time of tooth extraction is increasing in popularity for shortening the treatment period, reducing the number of surgeries interventions and trauma. Studies have validated the feasibility of this technique. Survival rates are similar between immediate and delayed placement, if enough primary stability of the implant was obtained in the residual bone of the tooth extraction socket1. However, bone defects and rugged bone morphology after tooth extraction make it more difficult for implants to achieve enough primary stability than delayed implant placement2. Decision-making regarding patient eligibility for immediate implant placement, choice of surgical technique, and selection of implant type largely relies on the doctor’s clinical experience. Preoperative misjudgment may result in suboptimal clinical outcomes. Consequently, developing a comprehensive and scientifically rigorous assessment method is crucial. Such a method would enable a more accurate analysis and prediction of immediate implant success rates for patients, aid clinicians in clinical decision-making, and enhance communication between doctors and patients.
Primary stability refers to the initial mechanical fixation of an implant within the bone immediately following placement. It is instrumental in achieving osseointegration by minimizing micromotion and averting fibrous encapsulation. This primary or mechanical stability transitions into secondary or biologic stability through the process of osseointegration, which involves bone remodeling around the implant3. Insertion torque was used to evaluates the primary stability of implants by recording the final torque value during implant insertion using torque wrench or surgical motor4. Optimal insertion torque is considered to facilitate bone cell differentiation. Low insertion torque may result in micro-movements, fibrous tissue formation, and premature implant failure. While high insertion torque values could potentially induce excessive peri-implant bone remodeling, buccal soft tissue recession, and increased bone resorption5. Thus, the prediction of insertion torque serves as a valuable metric for assessing the success rate of implant treatment.
Previous studies have identified factors that influence the insertion torque of implant, including the macro-design of implant, surgical technique of osteotomy preparation, bone quality of implant site, etc.5,6,7. It is important to note that the majority of these studies are conducted within the context of delayed implant placement. However, achieving the required bone volume for full-length implant placement is often impractical in clinical settings due to anatomical constraints and patient-specific factors. Therefore, it is essential to simulate the conditions of immediate implant placement and subsequently reassess the factors that affect the insertion torque. Current studies on insertion torque typically isolate single factors, which, while informative, do not fully represent the combined effect of multiple interrelated factors in clinical settings. Effective clinical decision-making requires a holistic consideration of these factors for planning surgeries, selecting techniques, and choosing implants. Single-factor assessments are often insufficient for accurate preoperative decisions, especially for inexperienced doctors, and may increase patient risks8. Hence, there’s an urgent need for an advanced decision-making model that considers a comprehensive analysis of multiple factors.
Creating a decision model based on multi-factor analysis is challenging due to the complex interactions and individual influences of these factors on outcomes. This process requires extensive sample data and sophisticated statistical methods. Machine learning-based artificial intelligence, particularly through in vitro research, can facilitate the development of such a model.
Hence, the focus of this research is to investigate the effects and co-effect of various implant apex designs, bone densities, implant intraosseous depths, and osteotomy preparation protocols on the implant insertion torque required for prior to making decisions of immediate implant surgery, and to construct machine learning preoperative prediction model for immediate implant insertion torque.
Materials and methods
Implants and polyurethane foam blocks
Three different Nobel implant systems characterized with different apex designs were used in the present in vitro study, including Nobel Active, Nobel Parallel CC and Nobel Replace CC. The study evaluated the performance of three distinct dental implant apex designs: the Nobel Active implant has tapered apex with deep thread and long cutting edge. Nobel Parallel CC has tapered apex with shallow thread and long cutting edge. Nobel Replace CC has tapered apex with shallow thread and no cutting edge (Table 1).
The polyurethane block (Sawbones Europe AB, Malmö, Sweden) represents an alternative to animal or corpse bone and exhibits common mechanical properties according to standards defined by the manufacturer (ASTM F-1839-08), which reduces the variables, alterations, and deformations found using cadaver bone or in animal bone. In this study, polyurethane blocks with three densities (15, 20, 30 pounds per cubic feet (pcf)) were used to simulate soft, medium, hard bone respectively5,8,9.
Experimental procedure
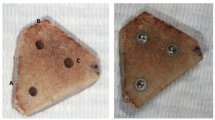
Six implant replicas of each of the three implant systems (Nobel Active, Nobel Parallel CC and Nobel Replace CC) were placed in each of the three densities of polyurethane foam block (15, 20 and 30pcf) with two osteotomy preparation protocols (normal preparation and undersized preparation) at three implant intraosseous depths (3 mm, 5 mm and 7 mm) (Fig. 1).
The procedure of normal preparation was performed according to the manufacturer, while the procedure of undersized preparation reduced the use of the terminal drill on the basis of normal preparation procedure. Drill stop ring was used to control the preparation depth at 3 mm, 5 mm and 7 mm. All implants were inserted self-tapping with an implant drill unit set on a maximum torque of 70 N·cm (iChiropo™, Bien-Air Dental SA, Bienne, Switzerland). A time-torque curve was registered for each implant site, which was used to extract the maximal insertion torque (Max IT ) in N·cm for each site (Fig. 2). All surgical procedures were performed by the same experienced surgeon who had inserted more than 1500 dental implants. Ethics approval was not required for this in vitro study.
Statistical analysis
Mean Max IT ± standard deviations (SD) were calculated. Due to the Max ITs were not normally distributed, the raw data of Max ITs were transformed with Box-cox transformation for subsequent analysis. Box-cox (Max IT)=(Max IT × λ + 1)1/λ, λ = 0.3.Then the data were further processed by statistical using SPSS 29.0. The sample size were calculated using G*Power software (version 3.1.9.7) and leveraging a linear model calculation method. The parameters employed consisted of a power level of 0.95, an alpha level of 0.05, an effect size of d = 0.15, and 4 predictors. These parameters pointed to a need for a minimum of 169 samples. A total of 324 samples (n = 6) were adopted in this study. The effect of implant apex design, intraosseous depth, bone quality and osteotomy preparation on the Max IT was analyzed using one-way ANOVA and four-way ANOVA with post hoc Bonferroni analysis. Then the significant factors were analyzed by multiple linear regression analysis to establish a prediction model for insertion torque. A decision tree regression model was constructed for predicting implant insertion torque based on machine learning methods using SPSSPRO. 70% of the raw data were utilized as the training set for model construction, while the remaining 30% of the raw data served as the validation set to assess the model’s performance. Compare the predictive indicators of the two models, including MSE (Mean Squared Error), RMSE (Root Mean Squared Error), MAE (Mean Absolute Error), MAPE (Mean Absolute Percentage Error), and R² (Coefficient of Determination), to evaluate the predictive power of both models. Statistical significance was analyzed with p < 0.05 considered significant.
Results
Table 2 presents the means and means and standard deviations of Max IT for simulated immediate implant placement situation. The ANOVA analysis revealed that all these factors (implant apex design, intraosseous depth, bone quality and osteotomy preparation) significantly affected Max IT values (Table 3). The interaction between osteotomy preparation protocol and intraosseous depth (p = 0.629), among implant apex design, intraosseous depth and bone quality (p = 0.430), and among osteotomy preparation protocol, intraosseous depth and bone quality (p = 0.328) was not significant, while other interactions were significant (p < 0.05) (Table 3).
From the analysis of the results of the F-test, it can be concluded that the P-value of significance is 0.000*** and identified all the variables (Implant Apex Design, Osteotomy preparation protocol, Intraosseous depth and Bone quality) as predictors of Max IT (Table 4); For the collinearity of variables, all VIFs are less than 10, so the model does not have multi collinearity issues. The multiple linear regression models showed fair fitting with R2 (R2 = 0.839) greater than 0.80, indicating the model is good fit. Based on the multiple linear regression equation, Box-cox (Max IT) = -1.631 + 2.629×Bone Quality (Hard) + 0.6519×Bone Quality (Medium) + 0.7089×Implant Apex Design (Nobel Active) + 0.2699×Implant Apex Design (Nobel Parallel CC) + 1.3499×Osteotomy preparation protocol (Undersized) + 0.75×Intraosseous Depth.
The analysis was conducted using the SPSSPRO software, where the data was divided into a training set and a validation set in a 7:3 ratio, and the predictive evaluation metrics of the decision tree model were calculated. Training set: MSE = 10.937, RMSE = 3.307, MAE = 2.364, MAPE = 18.197, R2 = 0.959. Validation set: MSE = 13.309, RMSE = 3.648, MAE = 2.915, MAPE = 24.732, R2 = 0.951. Following the same method, we calculated other evaluation metrics for the multiple linear regression model: MSE = 35.361, RMSE = 5.946, MAE = 4.447, MAPE = 33.639, R2 = 0.839 (Table 5). The true values of the validation set, predictions from the MLR (Multiple Linear Regression) model, and predictions from the Decision Tree Regression model were included in a line chart with the highest implant torque as the vertical axis to compare their fit, as shown in Fig. 3. The predictions from the Decision Tree Regression model fit the true values more closely, indicating that the predictive power of the Decision Tree Regression model is superior to that of the MLR model. Table 6 presents “insertion torque performance” of Nobel implant system under different conditions based on decision tree model established in this study.
Discussion
Practicality and advancement of the decision model base on multi-factor analysis
Preoperative prediction of insertion torque is essential for clinical decision-making. Currently, preoperative assessment of insertion torque in immediate implant placement remains a relatively understudied area. Some studies have established predictive models based on single factors, such as implant macrogeometries10, bone density11, drilling protocols12, etc. However, the reference value for complex clinical situations is limited by the approach of considering only single factors. In this study, four factors including implant apex design, osteotomy preparation, intraosseous depth, and bone quality were simultaneously considered, and a predictive model was established using multiple linear regression analysis, which yielded a high R-value of 0.839. The model established in this study exhibits greater scientific rigor and advanced characteristics, providing enhanced guidance for clinical practice.
In this study, we initiated the evaluation from an intraosseous depth of 3 mm, as our preliminary experiments revealed that depths of 1–2 mm were insufficient to achieve an insertion torque of over 10 N·cm. To better study the effect of intraosseous depth on insertion torque, intraosseous depths of 5 mm and 7 mm were set to simulate actual application scenarios. Our results indicated that when the intraosseous depth is 3 mm, employing a combination of deep-threaded implants featuring long cutting edges, along with undersized preparation, becomes essential to ensure optimal insertion torque. Nevertheless, it is important to recognize that with medium- to low-density bone, the method struggles to achieve an optimal insertion torque of over 25 N·cm. In the literature, an implant torque of at least 25 N·cm is widely accepted as the threshold criterion for immediate loading13.
Our findings indicated that the use of undersized preparation significantly enhances the insertion torque of implants, regardless of bone quality, implant design, or depth of insertion. Literature suggests that an insertion torque exceeding 50 N·cm is considered excessive and may heighten the risk of thermal bone damage and resorption12,13. Notably, at an intraosseous depth of 7 mm in hard bone conditions, the insertion torque achieved with undersized preparation surpassed 50 N·cm, irrespective of implant apex design, thus it is necessary to adopt the conventional osteotomy preparation protoco rather than the undersized preparation technique.
For immediate implant placement, only the intraosseous portion of the implant can affect the insertion torque. Therefore, the impplant apex design should be also considered as a significant factor for immediate implant placement. Studies have demonstrated that implant apex with deep and dense threads are more beneficial for increasing bone-implant contact and obtaining high insertion torque. In addition, implant apex with cutting edge have good self-tapping ability, allowing them to be more easily inserted in undersized implant beds11,14,15,16,17. The results of this study are generally consistent with the aforementioned research. However, it is worth noting that the implants with Tapered/Deep thread/Long cutting edge apex designs demonstrate their advantages primarily in hard bone and when using undersized preparation technique.
The current consensus is that there is a positive correlation between bone quality and insertion torque6. The results of this study also support this consensus that bone quality is the most significant influencing factor, compared to osteotomy preparation protocols, intraosseous depth and implant apex design. In addition, this study found that with an intraosseous depth of 3 mm, achieving an insertion torque of 25 N·m is only possible in cases of hard bone when using an implant with deep threads and cutting edges at the apex, and employing the undersized preparation technique. While in soft bone condition, even with an intraosseous depth of 7 mm, employing the undersized preparation technique along with an implant featuring deep threads and cutting edges at the apex, it was not possible to achieve a torque greater than 25 N·m, which is the minimum implant torque requirement for immediate loading9.
Based on our research findings, these four factors are crucial in influencing implant torque, while the clinical outcomes reflect the combined effects of these factors. Isolating the analysis of each factor independently would lead to misjudgments of the results. However, the establishment of a comprehensive analysis model incorporating multiple factors undoubtedly presents significant challenges. In addition to traditional statistical methods, artificial intelligence and machine learning algorithms, such as decision tree regression, can also be utilized in predictive model construction. Decision tree regression models are notable for their capacity to manage small sample sizes effectively. Moreover, they offer excellent visualization and transparent decision-making processes, distinguishing them from other ‘black-box’ models18. In this study, we developed a decision tree regression model for predictive purposes, achieving an R-value of 0.951, which exceeds that of the multiple linear regression model. This suggests that the decision tree regression model offers superior predictive accuracy for the insertion torque in immediate implant placement. With the rapid advancement of artificial intelligence, the medical field has emerged as a prominent domain for AI applications. Leveraging extensive medical data, AI technology holds the promise to aid clinicians in making more precise decisions regarding disease diagnosis, treatment planning, and patient risk assessment, thereby enhancing the quality and efficiency of healthcare services.
A more sophisticated decision model for clinical application guidance
If postoperative implant insertion torque is inadequate, it is necessary to forgo immediate loading and consider submerged healing instead. However, for immediate implant placement, insufficient soft tissue volume can complicate achieving complete wound closure required for submerged healing. Hence, preoperative prediction of insertion torque is essential for clinical decision-making.In actual clinical scenarios, the factors mentioned in this study often cannot be simultaneously optimized. However, we can optimize some adjustable factors according to the actual situation to accurately control the insertion torque and maximize the success rate of the implant. Assuming we only have Nobel Replace CC implants available with tapered/ shallow thread/ no cutting edge apex design, and the patient suffers from osteoporosis, but the mandibular molar to be extracted has a bone height greater than 7 mm from the inferior alveolar nerve canal, we can adopt an undersized osteotomy technique and ensure that the intraosseous depth of implant is at least 7 mm. By doing so, we can achieve an insertion torque close to 25 N·cm (Table 2). Furthemore, if the insertion torque still cannot be increased to a safe range within the scope of various factors that can be optimized, then we should not recommend the patient to adopt the immediate implant placement. This is of significant reference value for optimizing clinical decision-making, improving the success rate of implants, and enhancing the efficiency of doctor-patient communication.
A more comprehensive and standardized evaluation system can be established
Currently, many implant manufacturers claim that their products can achieve good primary stability (or insertion torque), but this is not rigorous. Based on the insertion torque prediction model established in this study, except for the intrinsic factors of the implant, it is also necessary to consider the actual clinical application scenarios, such as intraosseous depth of the implant, bone quality of the implant site, and the osteotomy preparation protocol. Based on the results of this study, we propose the concept of “implant insertion torque performance”. Manufacturers can calculate the insertion torque of the implant under different clinical scenarios using the prediction model of this study, and list specific values and reasonable osteotomy preparation protocol in the implant instruction manual for reference by clinical doctors. As shown in Table 6, taking the Nobel implant system as an example, we have sorted out its “insertion torque performance” table according to the prediction model established in this study, which can greatly improve the safety and success rate of implant surgery and increase the decision-making efficiency of doctors. At the same time, in this way, the primary stability (or insertion torque performance) provided by different brands of implants will be more comparable.
The present study has certain limitations. Firstly, it is an in vitro investigation utilizing a standardized model, which may not entirely replicate the complex bone conditions encountered in clinical settings14. Secondly, the diameter of the implants was not included in the study, despite being reported in numerous studies as one of the factors influencing the insertion torque of implants15. Thirdly, surgeon’s inexperience may be another elements for low insertion torque17.
Conclusion
The following conclusions are drawn from the results of this in vitro experimental study: In the context of immediate implant placement, the factors influencing implant insertion torque are ranked in the following order: bone quality, intraosseous depth, osteotomy preparation protocol, and implant apex design. Both traditional on multiple linear regression and novel machine learning models have demonstrated the capability to construct highly accurate predictive models for preoperative decision-making regarding the feasibility of immediate implant surgery. The methodologies employed in this study standardize the assessment of ‘insertion torque performance’ across different dental implant systems, thereby facilitating more precise decision-making.
Data availability
Data are available from the corresponding author (Runheng Liu: liurh28@mail.sysu.edu.cn) upon reasonable request.
References
Garcia-Sanchez, R. et al. Comparison of clinical outcomes of immediate versus delayed placement of dental implants: A systematic review and meta-analysis. Clin. Oral Implants Res. 33(3), 231–277 (2022).
Koh, R. U., Rudek, I. & Wang, H. L. Immediate implant placement: Positives and negatives. Implant Dent. 19(2), 98–108 (2010).
Javed, F. et al. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 5(4), 162–167 (2013).
Watanabe, T. et al. Insertion torque and periotest values are important factors predicting outcome after orthodontic miniscrew placement. Am. J. Orthod. Dentofacial Orthop 152(4), 483–488 (2017).
Stoilov, M., Shafaghi, R., Stark, H. et al. Influence of implant macro-design, -length, and -diameter on primary implant stability depending on different bone qualities using standard drilling protocols-an in vitro analysis. J. Funct. Biomater. 14(9) (2023).
Marquezan, M. et al. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin. Oral Implants Res. 23(7), 767–774 (2012).
Comuzzi, L., Tumedei, M., Di Pietro, N. et al. A Comparison of conical and cylindrical implants inserted in an in vitro post-extraction model using low-density polyurethane foam blocks. Materials (Basel) 16(14) (2023).
Dura Haddad, C., Andreatti, L., Zelezetsky, I. et al. Primary stability of implants inserted into polyurethane blocks: Micro-CT and analysis in vitro. Bioengineering (Basel) 11(4) (2024).
Mohlhenrich, S. C. et al. Compensating for poor primary implant stability in different bone densities by varying implant geometry: A laboratory study. Int. J. Oral Maxillofac. Surg. 44(12), 1514–1520 (2015).
Degidi, M., Daprile, G. The use of an artificial intelligence-driven novel tool for the evaluation of dental implants primary stability and immediate loading feasibility: An in vitro pilot study. Int. J. Oral Maxillofac. Implants 1–17 (2023).
Xiao, Y. et al. Correlation between peri-implant bone mineral density and primary implant stability based on artificial intelligence classification. Sci. Rep. 14(1), 3009 (2024).
Sakai, T. et al. Development of artificial intelligence model for supporting implant drilling protocol decision making. J. Prosthodont. Res. 67(3), 360–365 (2023).
Weigl, P. & Strangio, A. The impact of immediately placed and restored single-tooth implants on hard and soft tissues in the anterior maxilla. Eur. J. Oral Implantol. 9(Suppl 1), S89–S106 (2016).
Liu, R. et al. The influence of guide stabilizers and their application sequences on trueness and precision of surgical guides in free end situations: An in vitro analysis. Clin. Oral Implants Res. 35(3), 294–304 (2024).
Gottlow, J. & Sennerby, L. Influence of diameter and length on primary stability in various implant site densities—an in vitro study in polyurethane blocks. Clin. Implant Dent. Relat. Res. 26(2), 327–332 (2024).
Degidi, M., Daprile, G. The use of an artificial intelligence-driven novel tool for the evaluation of dental implants primary stability and immediate loading feasibility: An in vitro pilot study. Int. J. Oral Maxillofac. Implants 1–17 (2023).
Degidi, M., Daprile, G. & Piattelli, A. Determination of primary stability: A comparison of the surgeon’s perception and objective measurements. Int. J. Oral Maxillofac. Implants 25(3), 558–561 (2010).
Rousseau, S., Polachek, I. S. & Frenkel, T. I. A machine learning approach to identifying pregnant women’s risk for persistent post-traumatic stress following childbirth. J. Affect. Disord. 296, 136–149 (2022).
Acknowledgements
This work was financially supported by National Natural Science Foundation of China (82301036, 82201012), Guangdong Basic and Applied Basic Research Foundation (2022A1515110088), Guangdong Natural Science Foundation of China (2024A1515011661).
Author information
Authors and Affiliations
Contributions
G.L. and S.D. contributed to methodology, investigation, formal analysis, writing origninal draft and writing review & editing. R.L., Y.L. and Q.L. contributed to methodology and visualization. S.W. contributed to validation. Z.C. contributed to conceptualization, methodology, validation, supervision and writing review & editing. R.L. contributed to conceptualization, methodology, software, data curation, investigation, funding acquisition and writing review & editing. All authors gave final approval and agreed to be accountable for all aspects of the work. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, G., Deng, S., Liu, R. et al. Precise multi-factor immediate implant placement decision models based on machine learning. Sci Rep 15, 5143 (2025). https://doi.org/10.1038/s41598-025-89814-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-89814-3