Abstract
We investigated the long-term kidney and cardiovascular outcomes of patients with chronic kidney disease (CKD) after COVID-19. Our retrospective cohort consisted of 834 CKD patients with COVID-19 and 6,167 CKD patients without COVID-19 between 3/11/2020 to 7/1/2023. Multivariate competing risk regression models were used to estimate risk (as adjusted hazard ratios (aHR) with 95% confidence intervals (CI)) of CKD progression to a more advanced stage (Stage 4 or 5) and major adverse kidney events (MAKE), and risk of major adverse cardiovascular events (MACE) at 6-, 12-, and 24-month follow up. Hospitalized COVID-19 patients at 12 and 24 months (aHR 1.62 95% CI[1.24,2.13] and 1.76 [1.30, 2.40], respectively), but not non-hospitalized COVID-19 patients, were at higher risk of CKD progression compared to those without COVID-19. Both hospitalized and non-hospitalized COVID-19 patients were at higher risk of MAKE at 6-, 12- and 24-months compared to those without COVID-19. Hospitalized COVID-19 patients at 6-, 12- and 24-months (aHR 1.73 [1.21, 2.50], 1.77 [1.34, 2.33], and 1.31 [1.05, 1.64], respectively), but not non-hospitalized COVID-19 patients, were at higher risk of MACE compared to those without COVID-19. COVID-19 increases the risk of long-term CKD progression and cardiovascular events in patients with CKD. These findings highlight the need for close follow up care and therapies that slow CKD progression in this high-risk subgroup.
Similar content being viewed by others
Introduction
Patients with chronic kidney disease (CKD) are at significantly higher risk of adverse outcomes after COVID-19, including increased rates of hospitalization, critical illness, and mortality compared to those without CKD1,2. This increased vulnerability is due to several factors associated with both CKD and COVID-19. CKD is characterized by immune system dysfunction due to circulating uremic toxins and increased inflammation, which impairs the body’s ability to respond to stress and increases susceptibility to severe infections3. Similarly, severe COVID-19 also causes systemic inflammation and release of pro-inflammatory cytokines, which promote organ injury4. Dysregulated immune responses because of severe COVID-19 may also lead to prolonged illness.
Acute kidney injury (AKI) is common in severe COVID-19 and patients with CKD are at increased risk of AKI compared to those without CKD. Observational studies have estimated that 15–48% of individuals with COVID-19 associated AKI have underlying CKD5,6,7,8. Conversely, consequences of AKI include permanent loss of kidney function, development or progression of CKD. A multicenter study of 235 patients with CKD who developed hospital AKI observed that nearly 30% developed end stage kidney disease (ESKD) requiring dialysis over 5 year follow up9.
Patients with CKD are also at increased risk of major adverse cardiovascular events (MACE) and major adverse kidney events (MAKE) compared to the general population10,11,12. CKD promotes hypertension, dyslipidemia, and vascular calcification, which increases the risk of adverse cardiovascular events such as myocardial infarction and stroke. Additionally, underlying cardiovascular disease is a risk factor for CKD progression due to reduced blood flow to the kidneys, causing ischemic injury.
Although acute outcomes of patients with CKD and COVID-19 have been well-described13,14,15,16, long-term kidney and cardiovascular outcomes among COVID-19 patients with CKD have not been fully elucidated. For the reasons stated above, this subgroup may be at increased risk of accelerated kidney function decline and major adverse kidney and cardiovascular events long after resolution of SARS-CoV-2 infection17,18.
The objective of our study was to assess the long-term outcomes of patients with CKD up to 24 months after COVID-19 compared to patients with CKD without a diagnosis of COVID-19. Specifically, we evaluated the risk of CKD progression to a more advanced stage and the risk of major adverse kidney events (MAKE) and major adverse cardiovascular events (MACE).
Materials and methods
Data source and extraction
This study was approved by the Einstein-Montefiore Institutional Review Board (#2021–13,658) with an exemption for informed consent and a Health Insurance Portability and Accountability Act (HIPPA) waiver. The Montefiore Health System serves a large low-income, racially, and ethnically diverse population. Data originated from the Montefiore Health System consists of multiple hospitals and outpatient clinics located in the Bronx and its environs. De-identified health data were made available for research after standardization to the Observational Medical Outcomes Partnership (OMOP) Common Data Model (CDM) version 6. OMOP CDM represents healthcare data from diverse sources, which are stored in standard vocabulary concepts. This approach allows for the systematic analysis of disparate observational databases, including data from the electronic medical record (EMR), administrative claims, and disease classifications systems (e.g., ICD-10, SNOWMED, LOINC, etc.). Data were subsequently exported and queried as SQLite database files using the DB Browser for SQLite (version 3.12.0). To ensure data accuracy, our team performed extensive cross validation of all major variables extracted by manual chart reviews on subsets of patients. All methods were carried out in accordance with relevant guidelines and regulations, including those of stated in the “Declaration of Helsinki.” Studies using an earlier version of this large database to address different questions have been reported19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34.
The date of a patient’s first positive COVID-19 result or the first visit to the Montefiore Health System after March 1st, 2020 was used as the index date for the COVID-19 and non-COVID-19 cohorts, respectively. We excluded patients with preexisting end-stage kidney disease (ESKD) requiring dialysis, those with a previous eGFR less than 15 mL/min/1.73m2, those without outpatient creatinine values before and after index date, and those who did not meet our CKD definition.
Demographics and clinical comorbidities were extracted from electronic medical records. Demographic data included age, sex, ethnicity, and race. Chronic comorbidities included hypertension, diabetes, chronic obstructive pulmonary disease (COPD), asthma, liver disease, smoking status, heart failure, and cancer. Hospitalization status within two weeks of index date, critical illness (defined by initiation of invasive mechanical ventilation or ICU admission within two weeks of index date), and post COVID-19 mortality were also extracted. Acute kidney injury (AKI) was defined as a 1.5-fold increase in serum creatinine from baseline35,36. Creatinine values from 6 days prior to 30 days after COVID diagnosis or index date were used to define AKI.
Exposure variable
The exposure was COVID-19 positivity, defined by a positive PCR test. For regression models, CKD patients were separated into three groups: patients hospitalized with COVID-19, patients not-hospitalized with COVID-19 and patients without a COVID-19 positive test.
Outcome variables
Baseline eGFR was calculated using the 2021race-free CKD-EPI collaboration Eq37. as the mean of all eGFR values 12 months (7 to 365 days) preceding the index date. Approximately half of the cohort (51.2%) had at least 2 eGFR values in this timeframe. If there were no values within this timeframe, the mean of all eGFR values 24 months prior to index date was used.
CKD was defined as 2 consecutive eGFR readings < 60 mL/min/1.73m2 at least 90 days apart before a diagnosis of COVID-19 or the index date. CKD staging was defined using KDIGO guidelines as G1 (GFR ≥ 90 mL/min/1.73m2), G2 (GFR 60–89 mL/min/1.73m2), G3a (45–59 mL/min/1.73m2), G3b (30–44 mL/min/1.73m2), G4 (15–29 mL/min/1.73m2), and G5 (< 15 mL/min/1.73m2 or initiation of dialysis).
Progression of CKD was defined by advancing to a higher stage of CKD (e.g., those with CKD Stage 3a or 3b progressing to Stage 4, etc.) and was determined at 6, 12, and 24 months using outpatient eGFR measurements. Major adverse kidney event (MAKE) was defined as a composite of eGFR decline of ≥ 30% from baseline or progression to end-stage kidney disease (defined by either an eGFR < 15 mL/min/1.73m2 or dialysis dependence). Differences in the annual rate of eGFR change between the groups over 24 month follow up were also examined.
MACE was defined as the composite of all-cause mortality, nonfatal stroke, nonfatal myocardial infarction and non-fatal heart failure using ICD-10 codes.
Statistical analysis
All statistical analyses were performed using Python packages Statsmodels and lifeline. Frequencies and percentages for categorical variables between the 3 groups of were compared using χ2 tests. Continuous variables, expressed as means ± standard deviations, were compared between groups using ANOVA. P-values < 0.05 were considered statistically significant unless otherwise specified.
Multivariable competing risk regression (Fine gray analysis) was used to estimate the hazard ratio (HR) and 95% confidence interval (CI) of progression of CKD to Stage 4 or 5 CKD after COVID-19 at three timepoints (6, 12 and 24 months) with death as a competing risk factor. Patients were censored at death or their last follow up within the health system. Models were adjusted for demographics, comorbidities, AKI, and baseline eGFR.
Incidence of MAKE and MACE were estimated using Kaplan–Meier curves and log-rank hazard ratios (HR) with 95% CI. Cumulative incidence functions were calculated, and Multivariable Cox proportional hazards model was used to estimate HR and 95% CI, adjusting for demographics, comorbidities and baseline eGFR. Patients were censored at death or their last follow up within the health system. Differences between cumulative incidence functions were evaluated using log-rank test.
Linear mixed effects models were used to determine annual eGFR change across the entire follow up period (up to 24 months) for each group. The eGFR is treated as the dependent variable. Time from index date, COVID-19 status, and their interaction were included as the primary factors. Demographics, comorbidities, AKI, and eGFR baseline were also included in the model as covariates. A variance–covariance matrix was used to account for within-subject dependence over time, with model information criteria evaluated to select the optimal matrix structure.
Results
Baseline characteristics
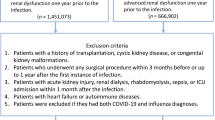
There were 56,400 patients with COVID-19 and 1,093,904 patients without COVID-19 in the Montefiore Health System from March 11, 2020, to July 1, 2023. After exclusions, there were a total of 13,319 COVID-19 positive and 125,146 COVID-19 negative patients (Fig. 1). Of the COVID-19 positive patients, 834 (6.3%) had pre-existing CKD. Of the COVID-19 negative patients, 6,167 (4.9%) had pre-existing CKD.
Table 1 summarizes the demographics and comorbidities grouped by COVID-19 status. CKD patients with COVID-19 were younger, a higher proportion were Hispanics, and a lower proportion were Black compared to those without COVID-19 (p < 0.05). Sex distribution was similar between groups. CKD patients with COVID-19, had higher prevalences of hypertension, diabetes, COPD, asthma, liver disease, heart failure, cancer, and obesity compared to CKD patients without COVID-19. CKD patients with COVID-19 had a lower but similar baseline eGFR (45.1 mL/min/1.73m2 ± 9.6 vs 46.5 mL/min/1.73m2 ± 9.2). Sixty-four percent of CKD patients with COVID-19 were hospitalized due to COVID-19 and 1.3% of CKD patients with COVID-19 had acute critical illness due to COVID-19. There was no statistical difference in mortality between CKD patients with and without COVID-19 (3.1% vs 2.3%, p = 0.12).
Risk of progression to a higher CKD stage
Figure 2 shows CKD stages at baseline, 6-, 12- and 24-months post index date. A higher proportion of CKD patients with COVID-19 progressed to a more advanced CKD stage compared to those without COVID-19. The number of outpatient eGFR measurements after the index date was similar among CKD patients with versus without COVID-19 (5.0 ± 5.0 vs 4.8 ± 6.1, p = 0.13).
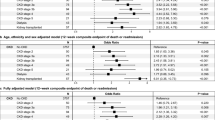
Table 2 shows the results of multivariable regression analysis for progression to Stage 4 or 5 CKD at 6-, 12- and 24-months post index date. CKD patients hospitalized with COVID-19 were not at increased risk of progression to a more advanced CKD stage at 6 months (aHR 1.05 [0.78, 1.42]), but were at increased risk of CKD progression at 12 and 24 months (aHR 1.62 [1.24,2.13], and 1.76 [1.30, 2.40], respectively), compared to non-COVID-19 patients. There was no difference in progression to a more advanced CKD stage among non-hospitalized COVID-19 versus non-COVID-19 patients. The adjusted HRs for covariates for CKD progression are detailed in Supplemental Table 1. For reference, univariable regression results for CKD progression are shown in Supplemental Table 2.
To explore the contribution of AKI to outcomes, multivariable regression analysis for CKD progression excluding patients with AKI was performed (Supplemental Table 3). The overall findings are consistent with those reported above. Among the non-AKI cohort, CKD patients hospitalized with COVID-19 were not at increased risk of progression to a higher CKD stage at 6 months (aHR 1.23 [0.89, 1.69]) but were at increased risk of CKD progression at 12 and 24 months (aHR 1.72 [1.29,2.30] and 2.04 [1.50, 2.78], respectively) compared to non-COVID-19 patients. There were no differences in progression to a higher CKD stage between non-hospitalized COVID-19 and non-COVID-19 patients who did not develop AKI.
Risk of MAKE
Figure 3 shows the cumulative incidence of MAKE stratified by COVID-19 hospitalization status. The median follow-up time was 24 months. CKD patients hospitalized for COVID-19 had a higher incidence of MAKE compared to non-hospitalized CKD patients with COVID-19 (p < 0.001) and non-COVID-19 patients (p < 0.001). Non-hospitalized COVID-19 also had a higher incidence of MAKE compared to non-COVID-19 patients (p < 0.001).
Table 3 shows the multivariable regression analysis for MAKE at 6-, 12- and 24-months. Hospitalized COVID-19 patients were at increased risk of MAKE compared to non-COVID-19 patients at 6-, 12- and 24-months (aHR 2.94 [2.28,3.79], 2.24 [1.81,2.76], and 2.03 [1.70,2.42], respectively). Non-hospitalized COVID-19 patients were also at higher risk compared to non-COVID-19 patients at 6-, 12- and 24-months (aHR 1.90 [1.31,2.78], 1.81 [1.35,2.42]), and 1.53 [1.18,1.99], respectively). Notably, the risk of MAKE decreased over time.
Annual eGFR decline
CKD patients with COVID-19 experienced a faster annual eGFR decline of −2.12 mL/min/1.73 m2 (95%CI [−1.64,2.50], p < 0.001) compared to CKD patients without COVID-19 who had an annual eGFR decline of −1.12 mL/min/1.73 m2 (95%CI [−1.01, −1.23], p < 0.001).
Risk of MACE
Figure 4 shows the cumulative incidence of MACE stratified by COVID-19 hospitalization status over a median follow-up time of 24 months. Overall, CKD patients hospitalized for COVID-19 had a higher incidence of MACE compared to non-hospitalized CKD patients with COVID-19 (p < 0.001) and non-COVID-19 patients (p < 0.001). There was no difference in MACE between non-hospitalized COVID-19 versus non-COVID-19 patients (p = 0.47).
Table 4 shows the multivariable regression analysis for MACE at 6-, 12- and 24-months. Hospitalized COVID-19 patients were at increased risk of MACE compared to non-COVID-19 patients at 6-, 12- and 24-months (aHR 1.73 [1.21, 2.50], 1.77 [1.34, 2.33], and 1.31 [1.05, 1.64], respectively) compared to non-COVID-19 patients. Notably, the risk of MACE was highest at 6 and 12 months and decreased over time. Non-hospitalized COVID-19 were at increased risk of MACE compared to non-COVID-19 patients at 6 and 12 months (aHR 1.74 [1.07, 2.83], 1.72 [1.17, 2.53] respectively) but not at 24 months (aHR 1.03 [0.73,1.44]). The adjusted HRs for covariates are detailed in Supplemental Table 4.
Hospitalization duration on outcomes
There were 31.1% (166/533) of hospitalized COVID-19 patients hospitalized for 7 or more days. Supplemental Table 5 shows the impact of hospitalization duration on MACE and MAKE. COVID-19 patients hospitalized for 7 or more days were at increased risk of MAKE compared to COVID-19 patients hospitalized for less than 7 days at 6-, 12- and 24-months (aHR 1.86 [1.45,2.39], 1.94 [1.51,2.49], and 2.00 [1.55,2.58], respectively). COVID-19 patients hospitalized for 7 or more days were at increased risk of MACE compared to COVID-19 patients hospitalized for less than 7 days at 6-,12- and 24-months (aHR 1.94 [1.25,3.01], 1.95 [1.32,2.89], and 1.88 [1.32,2.67], respectively).
Discussion
This study examined the long-term outcomes of patients with CKD up to 24 months after COVID-19 in a diverse population in the Bronx that was hit hard by early pandemic and subsequent surges. Only hospitalized COVID-19 patients with CKD had increased risk of CKD progression and MACE compared to those without COVID-19. Both hospitalized and non-hospitalized COVID-19 patients with CKD had higher risk of MAKE compared to those without COVID-19. To our knowledge, this is the first study to investigate long-term kidney and cardiovascular outcomes after COVID-19 among hospitalized and non-hospitalized non-dialysis CKD patients.
The risk of progression to a more advanced CKD stage among patients hospitalized with COVID-19 was larger or comparable with other CKD risk factors, underscoring the relatively high risk of COVID-19 had on CKD progression even after adjustment for AKI. These observations suggest that the severity of COVID-19 disease contributes to CKD progression. Consistent with the literature, baseline eGFR, hypertension, diabetes, smoking, and heart failure were independently associated with CKD progression38.
Numerous studies have reported kidney outcomes after hospitalized patients with COVID-19 were discharged. Among 1,726,683 patients from the Saint Louis VA system, COVID-19 survivors had a 1.62 higher risk of > 50% eGFR decline at 6 months across non-hospitalized, hospitalized, and ICU patients39. A multicenter study of 2,212 patients with long COVID-19 symptoms for more than 3 months in British Columbia, Canada observed that the overall cohort had a 3.39% reduction from baseline eGFR within a year40. Another multicenter study of 12,891 hospitalized patients from the 4CE consortium observed that patients who developed AKI at the time of COVID-19 had persistent elevation of creatinine (> 125% of baseline) 12 months after infection8. Other studies have similarly observed that there is incomplete recovery of kidney function up to 16 months after infection in patients with COVID-19 who developed AKI22,41,42,43. In comparison, Aklilu et al. reported that survivors of hospitalization with COVID-AKI experience lower rates of MAKE and mortality compared with patients with AKI associated with other illnesses (including influenza). The authors speculated that those who survive a COVID-19 complicated by AKI may have inherent unmeasured characteristics that are associated with favorable longer-term outcomes. While we observed a higher risk of MAKE among patients with COVID-19 compared to those without COVID-19, this may be because our cohort that was composed only of patients with pre-existing CKD who are a subgroup at higher risk of rapid kidney function decline compared to those with higher eGFR levels.
CKD progression may be due to persistent activation of the immune system and inflammation following COVID-1944,45,46,47,48. Inflammation is a known risk factor for incident and progressive CKD. We surmise that systemic inflammation as a consequence of COVID-19 promotes glomerulosclerosis and tubulointerstitial fibrosis49. Though unproven, direct kidney injury may also result from viral infection of the kidney or precipitation of immune-mediated glomerulonephritis50.
The risk for MACE in CKD patients hospitalized for COVID-19 attenuated over time suggesting that the contribution of COVID-19 as a risk factor decreased over time. A higher incidence of cardiovascular events has been reported following other respiratory infections. For example, influenza has been associated with an elevated risk of myocardial infarction and stroke, especially within the first few weeks after infection51,52,53. Systemic inflammation as a result of viral infection promotes endothelial dysfunction and destabilizes atherosclerotic plaques, making them prone to rupture, resulting in acute myocardial infarction or stroke54,55. Moreover, respiratory infections can alter autonomic nervous system function, leading to increased sympathetic activity, tachycardia and hypertension. These changes increase oxygen demand and can precipitate acute coronary syndrome56. Viral-associated inflammation and immune activation also causes a hypercoagulable state, increasing the risk of thrombotic events57. This underscores the need for close follow up after viral infections in patients with cardiometabolic risk factors for therapies aimed at cardiovascular risk reduction.
Pandemic circumstance
Finally, it is important to note that, beyond the direct or indirect effects of COVID-19 on the outcomes described above, the social impact in the early pandemic—such as psychological stress, unhealthy diet, interrupted care, and limited access to healthcare—could also contribute to CKD progression and cardiovascular events58,59,60. Populations with lower socioeconomic status, like ours in an inner-city setting, may be particularly vulnerable to these factors, although this hypothesis was beyond the scope of our study to test.
Strengths and limitations
Strengths of our study include the long follow-up time of a large diverse cohort, time to event analyses for risk of MAKE and MACE. Our results were consistent across sensitivity analyses for CKD patients with and without AKI.
However, there are notable limitations. First, this is a single health system study. Larger, multi-center studies are needed to improve generalizability. Second, vaccine status, which could affect outcomes, was not reliably recorded and therefore vaccine status was not analyzed61. Third, albuminuria is an important predictor of CKD progression but only 14% of our cohort had albuminuria data so we did were unable to use this as a covariate in our models. Fourth, since this is an observational study with real-world data, there was a lack of standardized follow up, tracking of exposures after discharge and our findings are limited to patients who returned to our health system. Although patient records included those who returned for any medical reason, including but not limited to routine office visits, patients who came to our health system may have had more severe COVID-19 and thus might not be representative of the general population at large. Fifth, we only considered the first COVID positive test and did not investigate the effects of multiple infections. COVID-19 status could be misclassified if patients were tested positive elsewhere but did not register in our health system. Sixth, we did not analyze outcomes with respect to various treatments. This was because each patient could have undergone many different treatments and our sample size did not have the power to adjust for these covariates.
Conclusions
Patients with underlying CKD who are hospitalized for COVID-19 are at increased risk of poor long-term adverse kidney and cardiovascular outcomes. These findings highlight the importance of comprehensive follow-up care to slow CKD progression and prevent cardiovascular events in this high-risk subgroup.
Data availability
Data used is available from the corresponding author upon reasonable request.
References
Khatri, M. et al. Outcomes among Hospitalized Chronic Kidney Disease Patients with COVID-19. Kidney360 2, 1107–1114, https://doi.org/10.34067/KID.0006852020 (2021).
Gibertoni, D. et al. COVID-19 incidence and mortality in non-dialysis chronic kidney disease patients. PLoS ONE 16, e0254525. https://doi.org/10.1371/journal.pone.0254525 (2021).
Syed-Ahmed, M. & Narayanan, M. Immune Dysfunction and Risk of Infection in Chronic Kidney Disease. Adv Chronic Kidney Dis 26, 8–15. https://doi.org/10.1053/j.ackd.2019.01.004 (2019).
Gustine, J. N. & Jones, D. Immunopathology of Hyperinflammation in COVID-19. Am J Pathol 191, 4–17. https://doi.org/10.1016/j.ajpath.2020.08.009 (2021).
Chawla, L. S., Eggers, P. W., Star, R. A. & Kimmel, P. L. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med 371, 58–66. https://doi.org/10.1056/NEJMra1214243 (2014).
Jewell, P. D. et al. COVID-19-related acute kidney injury; incidence, risk factors and outcomes in a large UK cohort. BMC Nephrol 22, 359. https://doi.org/10.1186/s12882-021-02557-x (2021).
Fisher, M. et al. AKI in Hospitalized Patients with and without COVID-19: A Comparison Study. J Am Soc Nephrol 31, 2145–2157. https://doi.org/10.1681/ASN.2020040509 (2020).
Tan, B. W. L. et al. Long-term kidney function recovery and mortality after COVID-19-associated acute kidney injury: An international multi-centre observational cohort study. EClinicalMedicine 55, 101724. https://doi.org/10.1016/j.eclinm.2022.101724 (2023).
Wu, V. C. et al. Acute-on-chronic kidney injury at hospital discharge is associated with long-term dialysis and mortality. Kidney Int 80, 1222–1230. https://doi.org/10.1038/ki.2011.259 (2011).
Matsushita, K. et al. Epidemiology and risk of cardiovascular disease in populations with chronic kidney disease. Nat Rev Nephrol 18, 696–707. https://doi.org/10.1038/s41581-022-00616-6 (2022).
Del Vecchio, L. et al. COVID-19 and cardiovascular disease in patients with chronic kidney disease. Nephrol Dial Transplant 39, 177–189. https://doi.org/10.1093/ndt/gfad170 (2024).
Matsushita, K. et al. Incorporating kidney disease measures into cardiovascular risk prediction: Development and validation in 9 million adults from 72 datasets. EClinicalMedicine 27, 100552. https://doi.org/10.1016/j.eclinm.2020.100552 (2020).
Flythe, J. E. et al. Characteristics and Outcomes of Individuals With Pre-existing Kidney Disease and COVID-19 Admitted to Intensive Care Units in the United States. Am J Kidney Dis 77, 190–203 e191, https://doi.org/10.1053/j.ajkd.2020.09.003 (2021).
Coca, A. et al. Outcomes of COVID-19 Among Hospitalized Patients With Non-dialysis CKD. Front Med (Lausanne) 7, 615312, https://doi.org/10.3389/fmed.2020.615312 (2020).
Gok, M. et al. Chronic kidney disease predicts poor outcomes of COVID-19 patients. Int Urol Nephrol 53, 1891–1898. https://doi.org/10.1007/s11255-020-02758-7 (2021).
Mohamed, N. E. et al. Association between chronic kidney disease and COVID-19-related mortality in New York. World J Urol 39, 2987–2993. https://doi.org/10.1007/s00345-020-03567-4 (2021).
Schmidt-Lauber, C. et al. Kidney outcome after mild to moderate COVID-19. Nephrol Dial Transplant 38, 2031–2040. https://doi.org/10.1093/ndt/gfad008 (2023).
Al-Aly, Z., Bowe, B. & Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med 28, 1461–1467. https://doi.org/10.1038/s41591-022-01840-0 (2022).
Lu, J. Y. et al. Incidence of new-onset in-hospital and persistent diabetes in COVID-19 patients: comparison with influenza. EBioMedicine 90, 104487. https://doi.org/10.1016/j.ebiom.2023.104487 (2023).
Lu, J. Y., Hou, W. & Duong, T. Q. Longitudinal prediction of hospital-acquired acute kidney injury in COVID-19: a two-center study. Infection 50, 109–119. https://doi.org/10.1007/s15010-021-01646-1 (2022).
Lu, J. Y. et al. Clinical predictors of recovery of COVID-19 associated-abnormal liver function test 2 months after hospital discharge. Sci Rep 12, 17972. https://doi.org/10.1038/s41598-022-22741-9 (2022).
Lu, J. Y. et al. Long-term outcomes of COVID-19 survivors with hospital AKI: association with time to recovery from AKI. Nephrol Dial Transplant https://doi.org/10.1093/ndt/gfad020 (2023).
Lu, J. Q. et al. Clinical predictors of acute cardiac injury and normalization of troponin after hospital discharge from COVID-19. EBioMedicine, 103821, https://doi.org/10.1016/j.ebiom.2022.103821 (2022).
Dell’Aquila, K. et al. Incidence, characteristics, risk factors and outcomes of diabetic ketoacidosis in COVID-19 patients: Comparison with influenza and pre-pandemic data. Diabetes Obes Metab https://doi.org/10.1111/dom.15120 (2023).
Xu, A. Y., Wang, S. H. & Duong, T. Q. Patients with prediabetes are at greater risk of developing diabetes 5 months postacute SARS-CoV-2 infection: a retrospective cohort study. BMJ Open Diabetes Res Care 11, e003257. https://doi.org/10.1136/bmjdrc-2022-003257 (2023).
Zhang, V., Fisher, M., Hou, W., Zhang, L. & Duong, T. Q. Incidence of New-Onset Hypertension Post-COVID-19: Comparison With Influenza. Hypertension 80, 2135–2148. https://doi.org/10.1161/HYPERTENSIONAHA.123.21174 (2023).
Feit, A. et al. Long-term clinical outcomes and healthcare utilization of sickle cell disease patients with COVID-19: A 2.5-year follow-up study. Eur J Haematol 111, 636–643, https://doi.org/10.1111/ejh.14058 (2023).
Eligulashvili, A. et al. COVID-19 Patients in the COVID-19 Recovery and Engagement (CORE) Clinics in the Bronx. Diagnostics (Basel) 13, 119, https://doi.org/10.3390/diagnostics13010119 (2022).
Lu, J. Y. et al. Characteristics of COVID-19 patients with multiorgan injury across the pandemic in a large academic health system in the Bronx. New York. Heliyon 9, e15277. https://doi.org/10.1016/j.heliyon.2023.e15277 (2023).
Lu, J. Y. et al. Outcomes of Hospitalized Patients With COVID-19 With Acute Kidney Injury and Acute Cardiac Injury. Front Cardiovasc Med 8, 798897. https://doi.org/10.3389/fcvm.2021.798897 (2021).
Eligulashvili, A. et al. Long-term outcomes of hospitalized patients with SARS-CoV-2/COVID-19 with and without neurological involvement: 3-year follow-up assessment. PLoS Med 21, e1004263. https://doi.org/10.1371/journal.pmed.1004263 (2024).
Eligulashvili, A. et al. Patients with unmet social needs are at higher risks of developing severe long COVID-19 symptoms and neuropsychiatric sequela. Sci Rep 14, 7743. https://doi.org/10.1038/s41598-024-58430-y (2024).
Peng, T. et al. Incidence, characteristics, and risk factors of new liver disorders 3.5 years post COVID-19 pandemic in the Montefiore Health System in Bronx. PLoS One 19, e0303151, https://doi.org/10.1371/journal.pone.0303151 (2024).
Mehrotra-Varma, S. et al. Patients with type 1 diabetes are at elevated risk of developing new hypertension, chronic kidney disease and diabetic ketoacidosis after COVID-19: Up to 40 months’ follow-up. Diabetes Obes Metab 26, 5368–5375. https://doi.org/10.1111/dom.15900 (2024).
Ad-hoc working group of, E. et al. A European Renal Best Practice (ERBP) position statement on the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury: part 1: definitions, conservative management and contrast-induced nephropathy. Nephrol Dial Transplant 27, 4263–4272, https://doi.org/10.1093/ndt/gfs375 (2012).
Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120, c179-184. https://doi.org/10.1159/000339789 (2012).
Inker, L. A. et al. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N Engl J Med 385, 1737–1749. https://doi.org/10.1056/NEJMoa2102953 (2021).
Hannan, M. et al. Risk Factors for CKD Progression: Overview of Findings from the CRIC Study. Clin J Am Soc Nephrol 16, 648–659. https://doi.org/10.2215/CJN.07830520 (2021).
Bowe, B., Xie, Y., Xu, E. & Al-Aly, Z. Kidney Outcomes in Long COVID. J Am Soc Nephrol 32, 2851–2862. https://doi.org/10.1681/ASN.2021060734 (2021).
Atiquzzaman, M. et al. Long-term effect of COVID-19 infection on kidney function among COVID-19 patients followed in post-COVID-19 recovery clinics in British Columbia. Canada. Nephrol Dial Transplant 38, 2816–2825. https://doi.org/10.1093/ndt/gfad121 (2023).
Sarwal, A. et al. Renal recovery after acute kidney injury in a minority population of hospitalized COVID-19 patients: A retrospective cohort study. Medicine (Baltimore) 101, https://doi.org/10.1097/MD.0000000000028995 (2022).
Lumlertgul, N. et al. Acute kidney injury prevalence, progression and long-term outcomes in critically ill patients with COVID-19: a cohort study. Ann Intensive Care 11, 123. https://doi.org/10.1186/s13613-021-00914-5 (2021).
Strohbehn, I. A. et al. Acute Kidney Injury Incidence, Recovery, and Long-term Kidney Outcomes Among Hospitalized Patients With COVID-19 and Influenza. Kidney Int Rep 6, 2565–2574. https://doi.org/10.1016/j.ekir.2021.07.008 (2021).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. Lancet 395, 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5 (2020).
Wang, D. et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan. China. JAMA 323, 1061–1069. https://doi.org/10.1001/jama.2020.1585 (2020).
Guo, T. et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 5, 811–818. https://doi.org/10.1001/jamacardio.2020.1017 (2020).
Shi, S. et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J 41, 2070–2079. https://doi.org/10.1093/eurheartj/ehaa408 (2020).
Shi, S. et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan. China. JAMA Cardiol 5, 802–810. https://doi.org/10.1001/jamacardio.2020.0950 (2020).
Hewitson, T. D., Holt, S. G. & Smith, E. R. Progression of Tubulointerstitial Fibrosis and the Chronic Kidney Disease Phenotype - Role of Risk Factors and Epigenetics. Front Pharmacol 8, 520. https://doi.org/10.3389/fphar.2017.00520 (2017).
Long, J. D., Strohbehn, I., Sawtell, R., Bhattacharyya, R. & Sise, M. E. COVID-19 Survival and its impact on chronic kidney disease. Transl Res 241, 70–82. https://doi.org/10.1016/j.trsl.2021.11.003 (2022).
Kwong, J. C. et al. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection. N Engl J Med 378, 345–353. https://doi.org/10.1056/NEJMoa1702090 (2018).
Boehme, A. K., Luna, J., Kulick, E. R., Kamel, H. & Elkind, M. S. V. Influenza-like illness as a trigger for ischemic stroke. Ann Clin Transl Neurol 5, 456–463. https://doi.org/10.1002/acn3.545 (2018).
Warren-Gash, C., Blackburn, R., Whitaker, H., McMenamin, J. & Hayward, A. C. Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Respir J 51, https://doi.org/10.1183/13993003.01794-2017 (2018).
Haidari, M. et al. Influenza virus directly infects, inflames, and resides in the arteries of atherosclerotic and normal mice. Atherosclerosis 208, 90–96. https://doi.org/10.1016/j.atherosclerosis.2009.07.028 (2010).
Naghavi, M. et al. Influenza infection exerts prominent inflammatory and thrombotic effects on the atherosclerotic plaques of apolipoprotein E-deficient mice. Circulation 107, 762–768. https://doi.org/10.1161/01.cir.0000048190.68071.2b (2003).
Skaarup, K. G., Modin, D., Nielsen, L., Jensen, J. U. S. & Biering-Sorensen, T. Influenza and cardiovascular disease pathophysiology: strings attached. Eur Heart J Suppl 25, A5–A11. https://doi.org/10.1093/eurheartjsupp/suac117 (2023).
Ackermann, M. et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med 383, 120–128. https://doi.org/10.1056/NEJMoa2015432 (2020).
Quinones, J. & Hammad, Z. Social Determinants of Health and Chronic Kidney Disease. Cureus 12, e10266. https://doi.org/10.7759/cureus.10266 (2020).
Vanholder, R. et al. Inequities in kidney health and kidney care. Nat Rev Nephrol 19, 694–708. https://doi.org/10.1038/s41581-023-00745-6 (2023).
Hall, Y. N. Social Determinants of Health: Addressing Unmet Needs in Nephrology. Am J Kidney Dis 72, 582–591. https://doi.org/10.1053/j.ajkd.2017.12.016 (2018).
Roushani, J. et al. Clinical Outcomes and Vaccine Effectiveness for SARS-CoV-2 Infection in People Attending Advanced CKD Clinics: A Retrospective Provincial Cohort Study. Clin J Am Soc Nephrol 18, 465–474. https://doi.org/10.2215/CJN.0000000000000087 (2023).
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Contributions
J.Y. Lu and J.Y. Lu – concept and design, collected data, analyzed data, created tables and figures, drafted paper S. Wang – concept and design, edited paper K.S. Duong, S. Henry – collected data M.C. Fisher – concept and design, edited paper T.Q. Duong – concept and design, supervised, edited paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, J.Y., Lu, J.Y., Wang, S. et al. Long term outcomes of patients with chronic kidney disease after COVID-19 in an urban population in the Bronx. Sci Rep 15, 6119 (2025). https://doi.org/10.1038/s41598-025-90153-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90153-6
Keywords
This article is cited by
-
Mortality comparison between the COVID-19 Omicron variant and influenza among patients with end-stage kidney disease: a nationwide population-based retrospective cohort study
Clinical and Experimental Nephrology (2026)
-
Long COVID and the kidney
Nature Reviews Nephrology (2025)
-
Long-term renal consequences of COVID-19. Emerging evidence and unanswered questions
International Urology and Nephrology (2025)