Abstract
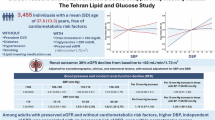
We investigated the effect of differential blood pressure (BP) levels on future end-stage renal disease (ESRD) in patients with type 2 diabetes mellitus (T2DM) and established coronary artery disease with a previous record of percutaneous coronary intervention (PCI). Using health check-up data from the Korean National Health Insurance Service (2015–2016), we analyzed 80,187 T2DM patients with a history of PCI. Patients were categorized by BP levels measured: systolic BP < 120, 120–129 (reference), 130–139, 140–149, and ≥150 mmHg; diastolic BP < 70, 70–79 (reference), 80–89, and ≥90 mmHg. Incident ESRD, defined by disease codes and renal replacement therapy initiation, was the primary outcome. Multivariate Cox proportional hazard regression assessed adjusted hazard ratios (HRs) (95% confidence intervals) by BP group. Mean age was 67.7 years; 80.9% used antihypertensives. ESRD incidence was 1.70% (1,362 patients) over 4.7 years. After adjustment for confounding factors, the HR of ESRD patients significantly and sequentially increased in the higher BP groups. Similar trends were seen with pulse pressure (PP). Subgroup analysis showed stronger BP-ESRD association in < 65-year-olds compared to those aged ≥65 years. ESRD risk linearly increased with systolic BP and had a J-shaped association with diastolic BP, with the lowest risk at 68 mmHg. Elevated BP, including PP, correlated with ESRD risk in a dose‒response manner among T2DM patients with a previous record of PCI. Strict BP control is crucial for preventing ESRD in these high-risk patients.
Similar content being viewed by others
Introduction
End-stage renal disease (ESRD) is the final phase of chronic kidney disease (CKD) and occurs as a severe chronic consequence of prolonged diabetes and hypertension, contributing significantly to the global health burden. The incidence of ESRD has been increasing worldwide, driven by the acceleration of societal aging, the exponential rise in chronic metabolic disease, and the consequent increase in life expectancy1,2. The 2019 Korean Renal Data System report revealed a continuous increase in the incidence and prevalence of ESRD, with diabetes mellitus (DM) being the most common cause of ESRD in Korea (48.4%)2. Although clinical guidelines have been widely disseminated, it is anticipated that the prevalence of ESRD will continue to rise due to these trends.
Hypertension is an important risk factor in the development and progression of cardiovascular disease (CVD) and ESRD, particularly in individuals with type 2 diabetes mellitus (T2DM). Regulating blood pressure (BP) within the desired range in individuals with hypertension and/or T2DM decreases the likelihood of cardiovascular incidents and mortality3. Furthermore, diabetes status is strongly associated with an increased risk of ESRD, emphasizing the importance of BP control in individuals with hypertension and T2DM to prevent ESRD.
The latest hypertension guidelines suggest lower BP goals for high-risk patients, including those with CKD or type 2 diabetes4. However, the optimal BP target for preventing CKD or its progression in patients with type 2 diabetes and CVD is still unknown. The Korean Society of Hypertension and the Korean Diabetes Association suggest maintaining BP below 140/90 mmHg in people with type 2 diabetes who do not have additional CVD risk factors or CVD. For individuals with T2DM who have one or more risk factors for CVD, existing CVD, CKD stage 3–5, or asymptomatic organ damage, a BP target of less than 130/80 mmHg is advised3,5,6. However, insufficient data exist on the recommended BP target to reduce progression to ESRD in individuals with coronary artery disease (CAD) and T2DM, especially those who have undergone percutaneous coronary intervention (PCI). Using the Korean National Health Insurance Service (KNHIS) database, we examined the relationships of systolic BP (SBP) and diastolic BP (DBP) with the likelihood of ESRD in individuals with T2DM who underwent PCI for CAD to determine the ability of BP to predict ESRD development.
Methods
Data sources
The KNHIS database provided the data for this nationwide cohort study7. The KNHIS database, the details of which have been previously reported8,9, is thought to represent the whole population of South Korea. All insured Korean people undergo annual or biennial health examinations that are supported by the KNHIS. The database contains information on mortality, pharmacy dispensing claims, demographics, and all medical costs for both inpatient and outpatient treatments7. We also gathered questionnaire data and laboratory test findings related to lifestyle behaviors from this dataset.
First identified were 2,612,704 T2DM individuals who were 20 years of age or older and had health examinations performed between 2015 and 2016 (the index year). We chose 83,588 individuals who had had PCI before the health check-up. We also eliminated individuals with a history of ESRD prior to the index year (n = 1,499) in order to reduce the potential effects of reverse causation and avoid confounding related to preexisting conditions. Ultimately, 80,187 subjects made up the study population after those with missing blood test results or values in the KNHIS database were excluded. The population under investigation was monitored through December 31, 2020.
The Catholic University of Korea St. Vincent’s Hospital’s Institutional Review Board gave its approval to this study (VC23ZISE0366). The requirement for informed consent from the study subjects was waived by the IRB of the Catholic University of Korea St. Vincent’s Hospital due to the retrospective study design. All methods were performed in compliance with the Declaration of Helsinki’s tenets.
Definition of T2DM, comorbidities, and clinical parameters
According to the International Statistical Classification of Diseases, Tenth Revision (ICD-10) codes E11 to E14 from the claims data, the presence of T2DM was defined as any one of the following: (1) at least one claim per year for a prescription of antidiabetic medication; or (2) fasting plasma glucose ≥ 126 mg/dL in the health examination without a prescription for antidiabetic medication10,11. The following procedure codes were used to determine the patients’ PCI status: M6551-M6554, M6561-M6566, M6572, and M657212. Hypertension was defined as a SBP of ≥140 mmHg or DBP of ≥90 mmHg recorded in the health examination or the use of antihypertensive medications combined with the ICD-10 codes (I10-13, I15)13. Dyslipidemia was defined as an ICD-10 code of E78 and a history of lipid-lowering drug use or a total serum cholesterol level ≥ 240 mg/dL recorded in the health examination database14.
According to recent guidelines15, patients with CAD are classified as very high-risk, with a recommended LDL cholesterol target of < 55 mg/dL. Based on these recommendations, we conducted Cox regression analysis to evaluate the risk of ESRD across LDL cholesterol categories: <55 (reference), 55–69, 70–99, and ≥ 100 mg/dL. Using the Modification of Diet in Renal Disease formula, an estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73 m2 was categorized as having chronic kidney disease (CKD)10. CKD stages were defined by eGFR: Stage 1 (≥ 90 mL/min/1.73 m²), Stage 2 (60–89 mL/min/1.73 m²), Stage 3a (45–59 mL/min/1.73 m²), Stage 3b (30–44 mL/min/1.73 m²), Stage 4 (15–29 mL/min/1.73 m²), and Stage 5 (< 15 mL/min/1.73 m²). The lowest 20% of socioeconomic level was considered to have a low income. The formula for calculating body mass index was weight (kg) divided by height (m2). Through the use of a questionnaire, data regarding current alcohol and smoking intake was gathered. The three categories for smoking history were current smoker, ex-smoker, and non-smoker. Based on their level of alcohol intake, participants were divided into three categories: mild drinkers (< 30 g/day), heavy drinkers (≥ 30 g/day), and nondrinkers. Regular exercise was defined as physical activity that was performed at least five times per week16.
Blood samples for the measurement of serum glucose and lipid profiles were drawn after overnight fasting. The Korean Association for Laboratory Medicine evaluated the quality of the laboratory tests, and the NHIS recognized the hospitals that took part in its health screening programs16.
Measurements and classification of BP levels
KNHIS data for brachial SBP and DBP were acquired using an automatic sphygmomanometer in a sitting position after taking the anthropometric measures and after at least 5 min of seated rest. The reported value is the average of two readings. The DBP value was subtracted from the SBP value to determine the pulse pressure (PP)8.
According to the 2023 European Society of Hypertension (ESH) guidelines for patients with coronary heart disease (CHD), diabetes, and CKD, SBP of 120–129 mmHg and DBP of 70–79 mmHg were used as reference categories4. SBP categories were < 120, 120–129, 130–139, 140–149, and ≥ 150 mmHg, and DBP categories were < 70, 70–79, 80–89, and ≥ 90 mmHg. PP categories were < 40 (reference), 40–49, 50–59, 60–69, and ≥ 70 mmHg.
Participants were further categorized into six BP groups based on the 2023 ESH guidelines4, with optimal BP serving as the reference group: (1) optimal BP (SBP < 120 mmHg and DBP < 80 mmHg), (2) normal BP (SBP 120–129 mmHg or DBP 80–84 mmHg), (3) high normal BP (SBP 130–139 mmHg or DBP 85–89 mmHg), (4) grade 1 hypertension (SBP 140–159 mmHg or DBP 90–99 mmHg), (5) grade 2 hypertension (SBP 160–179 mmHg or DBP 100–109 mmHg), and (6) grade 3 hypertension (SBP ≥ 180 mmHg or DBP ≥ 110 mmHg).
Study outcome and follow-up
The primary endpoint was incident ESRD, which was defined using a combination of ICD-10 codes (N18-19, Z49, Z94.0, and Z99.2) and a unique code (V code) that was assigned at the initiation of renal replacement therapy (hemodialysis, V001; peritoneal dialysis, V003) and/or kidney transplantation (V005) during hospitalization16. CKD stage 5 (eGFR < 15 ml/min/1.73 m²) was not included in the definition of ESRD due to variability in the timing of eGFR measurements. Instead, the initiation of RRT was used as it represents a precise and well-documented event. All medical expenses for dialysis are reimbursed using the Korean Health Insurance Review and Assessment Service database. These patients are also registered as special medical aid beneficiaries. Therefore, we identified every patient with ESRD in the entire South Korean population and analyzed the data for all patients with ESRD who started dialysis. We excluded individuals without previous CKD who had a transplant or dialysis code recorded on the same date as an acute renal failure code. Acute peritoneal dialysis patients and those receiving continuous renal replacement treatment were also not included8,16,17. The participants were followed up until one of the following occurred: a new diagnosis of ESRD, death, loss of health insurance, or end of the study (December 31, 2020).
Statistical methods
For continuous variables, the baseline characteristics are shown as means ± SEs, and for categorical variables, as percentages (standard errors, SEs). Geometric means (95% confidence intervals) are used to display variables with nonnormal distributions. The χ2 test and t test were used to evaluate baseline characteristics between the ESRD and other groups. The ESRD incidence rates are displayed as a function of 1,000 person-years. Person-years were measured starting on the day of BP measurement and ending on December 31, 2014, whichever happened first—the date of reported ESRD, loss to follow-up, or death. The reference group was the one with the lowest level of each measure, and we used multivariable Cox proportional hazards regression models to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of ESRD. We chose potential confounders based on their past connections with the risk of ESRD in our study cohort or because they were recognized risk factors for ESRD. Four models were used to examine relationships between BP category and ESRD development: Model 1 was unadjusted; Model 2 was adjusted for age and sex; Model 3 was adjusted for Model 2 plus income, body mass index, smoking, drinking, physical activity, dyslipidemia, and chronic kidney disease; and Model 4 was adjusted for Model 3 plus fasting glucose levels, use of antihypertensive medications, and length of diabetes. We assessed the cumulative incidence of ESRD by creating Kaplan-Meier curves for the whole follow-up period. To investigate variations in ESRD development by BP category, we employed the log-rank test.
The structure of the correlations between BP indices and the risk of ESRD was investigated using restricted cubic spline analysis. We determined the number of knots needed to suit the best approximate model by calculating the values of the Akaike information criterion. We then used the first or second knot as a reference and performed the Wald test to check for linearity. Because all BP indices demonstrated linear dose-dependent responses above predetermined thresholds seen in restricted cubic spline analysis and risk estimates from ordinal BP categories, we restricted the analyses to participants whose BP measurements were above the cutoff values determined from the results, and we calculated HRs and 95% CIs per 10-mmHg increment of each BP index beyond the level at which the risk increased linearly. We also carried out stratified analysis based on sex, age (less than 65 versus greater than 65), and the existence of CKD.
The provided p-values are all two-sided, and the significance level is set at less than 0.05. SAS version 9.4 was used for the statistical analyses (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics
The baseline characteristics of the participants with respect to the development of ESRD are shown in Table 1. The mean age was 67.7 years, and 80.9% of the participants were treated with antihypertensive medications. Over a mean follow-up of 4.7-years, 1,362 patients (1.7%) developed ESRD, with an incidence rate of 3.62 per 1,000 person-years.
Compared to the non-ESRD group, the ESRD group had a greater mean age (68.6 ± 8.8 years vs. 66.8 ± 9.5 years, p < 0.001), lower income status (23.2% vs. 20.4%, p = 0.0124), longer duration of diabetes (p < 0.001), higher prevalence of underlying CKD (87.8% vs. 20.7%, p < 0.001), and a greater proportion of patients with CKD stage 3 or higher (p < 0.001). Among them, 80.7% of the patients in the non-ESRD group and 93.5% of those in the ESRD group were prescribed hypertension medication, respectively. The values for mean SBP (127.8 ± 15.6 mmHg vs. 135.7 ± 18.5 mmHg, p < 0.001), mean DBP (75.6 ± 10.0 mmHg vs. 76.4 ± 11.4 mmHg, p = 0.0034), and LDL-C (75.6 ± 30.7 mg/dL vs. 83.2 ± 35.5 mg/dL, p < 0.001) were greater in the ESRD group than in the non-ESRD group. The eGFR (81.1 ± 59.1 mL/min/1.73 m2 vs. 38.9 ± 47.7 mL/min/1.73 m2, p < 0.001) was lower in the ESRD group than in the non-ESRD group. The median time between BP measurements and PCI was similar between the non-ESRD and ESRD groups, at 5.29 years (IQR: 2.61–8.44) and 5.37 years (IQR: 2.33–8.50), respectively (p = 0.60) (Table 1).
Effects of systolic or diastolic BP on the risk of ESRD in patients with T2DM who underwent PCI
Table 2 shows the multivariable Cox proportional hazard regression analysis to estimate the adjusted hazard ratio (HR) (95% CI) based on the BP groups. The incidence rate of ESRD increased according to BP in both the SBP and DBP categories. After adjustment for covariates, the HRs (95% CIs) of SBP for incident ESRD patients were 0.75 (0.63–0.90), 1.00 (reference), 1.27 (1.08–1.50), 1.88 (1.57–2.24), and 2.71 (2.29–3.20) in the < 120, 120–129, 130–139, 140–149, and ≥150 mmHg categories, respectively. For DBP, a similar trend was observed; however, the HR for DBP < 70 mmHg (1.08 [0.93–1.24]) was slightly higher than the reference group. For higher DBP categories, the adjusted HRs were 1.22 (1.07–1.41) for 80–89 mmHg and 1.80 (1.52–2.13) for ≥ 90 mmHg. PP remained significantly associated with ESRD risk in a dose-dependent manner after adjusting for multiple variables. (Table 2).
In addition, incident ESRD also increased with higher blood pressure groups. ESRD risk increased even in the normal BP range. The multivariable-adjusted HRs (95% CIs) for ESRD were 1.54 (1.31–1.81), 1.92 (1.61–2.29), 2.84 (2.38–3.39), 4.37 (3.27–5.86), and 7.45 (3.67–15.13) in the normal BP, high normal BP, grade 1, grade 2, and grade 3 hypertension groups, respectively, compared to the optimal BP group (Table 3).
We further classified the DBP levels according to SBP categories. In the SBP 140–159 mmHg group, the lowest DBP group (< 80 mmHg) had the highest HR (95% CI) of 3.20 (2.61–3.92). Moreover, compared to the normal BP group, the highest SBP (≥ 160 mmHg) and DBP (≥ 100 mmHg) groups had the highest HR (95% CI) (4.86 (3.43–6.88); Table 4).
The Kaplan-Meier curves illustrate the cumulative incidence probabilities of ESRD stratified by SBP, DBP, PP, and HTN grade. The cumulative incidence of ESRD progressively increased with higher SBP, PP levels, and HTN grades, indicating a clear positive association with ESRD risk (Fig. 1a, c and d). For DBP, a similar trend was observed; however, the DBP < 70 mmHg group showed an even higher risk not only compared to the DBP 70–79 mmHg group but also to the DBP 80–89 mmHg group, highlighting the significant impact of very low DBP on ESRD risk (Fig. 1b).
Kaplan-Meier curves for cumulative incidence of ESRD stratified by BP categories and hypertension grades. (a) SBP categories: <120 mmHg, 120–129 mmHg, 130–139 mmHg, 140–149 mmHg, and ≥ 150 mmHg, (b) DBP categories: <70 mmHg, 70–79 mmHg, 80–89 mmHg, and ≥ 90 mmHg, (c) PP categories: <40 mmHg, 40–49 mmHg, 50–59 mmHg, 60–69 mmHg, and ≥ 70 mmHg, (d) Hypertension grades based on classification: Optimal, Normal, High-Normal, HTN grade 1, HTN grade 2, and HTN grade 3. The cumulative incidence probabilities were calculated over 6 years of follow-up. ESRD: end-stage renal disease; BP: blood pressure; SBP: systolic blood pressure; DBP; PP: pulse pressure.
Restricted cubic spline analysis revealed a nonlinear relationship between all BP indices (nonlinearity, p < 0.001 for SBP, DBP, and mean arterial pressure (MAP) and p = 0.003 for PP) and the risk of ESRD, and the HRs increased in a linear dose-dependent manner beyond a certain level for each index. The association with the risk of ESRD for SBP appeared to plateau at very low levels, with the risk beginning to increase significantly around 115 mmHg (Fig. 2a). In contrast, the risk of ESRD seemed to increase with decreasing DBP at very low levels to create an overall J-shaped association (Fig. 2b). The risk of ESRD showed a J-shaped association with DBP at 68 mmHg after adjustment for covariates.
Restricted cubic spine analyses for BP and ESRD patients. The HR for incident ESRD showed a linear relationship with a baseline of 115 mmHg for SBP (a) and a J-shaped curve with a nadir at 68 mmHg for DBP (b). The shaded areas represent the 95% confidence intervals. BP: blood pressure; ESRD: end-stage renal disease; HR; hazard ratio; SBP: systolic blood pressure; DBP: diastolic blood pressure.
Subgroup analyses
In the subgroup analysis based on age, individuals under the age of 65 with a SBP ≥ 150 mmHg exhibited a higher HR (95% CI) of 3.35 (2.48–4.54) compared to those aged ≥ 65 years, who had an HR of 2.47 (2.02–3.02) (Fig. 3a). Similarly, higher DBP was associated with an increased risk of ESRD, and this association was slightly more pronounced in younger patients (HR [95% CI]: 1.92 [1.45–2.56]) compared to older patients (1.74 [1.41–2.14]) for DBP ≥ 90 mmHg. This result highlights that the relationship between elevated BP and ESRD is particularly pronounced in the population under 65 years of age (Fig. 3). Although not stated here, the risk of ESRD was also linearly correlated with PP.
Forest plots for SBP and DBP and ESRD outcomes stratified by age, sex, and CKD status. (a) HRs for ESRD outcomes according to SBP categories (< 120, 120–129, 130–139, 140–149, and ≥ 150 mmHg) stratified by age (< 65 years and ≥ 65 years), sex (male and female), and CKD status (CKD[-] and CKD[+]), (b) HRs for ESRD outcomes according to DBP categories (< 70, 70–79, 80–89, and ≥ 90 mmHg) stratified by the same subgroups. Each plot includes the HRs with 95% CIs and the p-values for interaction tests between subgroups. SBP: systolic blood pressure; DBP: diastolic blood pressure; ESRD: end-stage renal disease; CKD: chronic kidney disease; HRs: hazard ratios; CIs: confidence intervals.
In the subgroup analysis by sex, male patients demonstrated a higher ESRD risk across all BP groups compared to female patients; for instance, the HRs were 3.12 vs. 2.04 for SBP ≥ 150 mmHg, respectively. (Fig. 3).
Impact of initial CKD stages on ESRD risk
As the initial CKD stage advanced, both the incidence rate and HR for ESRD progressively increased. The most significant increases occurred between stages 3a and 3b, where the incidence rate rose sharply from 3.81 to 23.37 per 1,000 person-years, and the HRs (95% CI) in Model 4 increased from 13.85 (9.40-20.41) to 83.47 (57.17-121.88) (Supplementary Table S1).
Effect of LDL cholesterol levels on the risk of ESRD
After full adjustment for covariates, the HRs (95% CI) for ESRD progressively increased with higher LDL cholesterol levels: 1.01 (0.86–1.20) for 55–69 mg/dL, 1.26 (1.08–1.46) for 70–99 mg/dL, and 1.91 (1.62–2.25) for ≥ 100 mg/dL, compared to the reference group (< 55 mg/dL) (Supplementary Table S2).
Discussion
In this study, we investigated the association between BP levels and the risk of ESRD in patients with T2DM who had a history of PCI. Our findings demonstrated a progressive increase in ESRD risk with higher SBP levels, with the lowest risk observed in the SBP < 120 mmHg group compared to the reference (120–129 mmHg). DBP levels showed a J-shaped relationship with ESRD, where both low (< 70 mmHg) and high (≥ 80 mmHg) DBP levels were associated with increased risk compared to the reference (70–79 mmHg). Kaplan-Meier analysis revealed a higher cumulative incidence probability of ESRD with increasing SBP, PP levels, and HTN grades. Notably, the DBP < 70 mmHg group exhibited a higher incidence probability than the reference and DBP 80–89 mmHg groups, highlighting the potential risks of excessively low DBP. Subgroup analysis indicated that BP-related ESRD risk was particularly pronounced in younger patients (< 65 years), and males.
During the 4.7-year follow-up of our study, 1,362 patients (1.7%) developed ESRD, corresponding to an incidence rate of 3.62 per 1,000 person-years. This rate is consistent with those reported in other studies. For example, a nationwide cohort study in Korea observed an ESRD incidence rate of 4.14 per 1,000 person-years in patients with hypertrophic cardiomyopathy18, and another study reported a similar rate of 3.5 per 1,000 person-years in patients with coronary heart disease after cardiovascular events19.
Controlling BP within the desired range is crucial for preventing CVD, particularly in individuals with T2DM. Compared with routine treatment, intensive BP lowering was more effective at providing vascular protection20. Previous studies have shown that a decrease of approximately 10 mmHg in SBP can lead to a 20% reduction in CVD risk, a 28% decrease in heart failure risk, a 27% lower risk of stroke, and a 13% decrease in all-cause mortality3. Furthermore, high-risk patients can have added advantages from more aggressive BP reduction, even if their SBP is less than 140 mmHg20.
It’s as uncertain whether BP should be reduced to the same target level in high-risk groups to prevent ESRD in people with type 2 diabetes. A systematic review and meta-analysis of 19 trials involving 44,989 participants showed that intensive BP-lowering treatment resulted in a 14% (95% CI 4–22) reduction in major cardiovascular events, a 10% (95% CI 3–16) decrease in albuminuria, and a 19% (95% CI 0–34) decrease in retinopathy progression. In contrast, there were no significant impacts on heart failure (15% difference, 95% CI -11 to 34), cardiovascular death (9% difference, 95% CI -11 to 26), or ESRD (10% difference, 95% CI -6 to 23)21. Epidemiological studies and randomized controlled trials have shown that BP control is crucial for reducing the decline in eGFR and the risk of future ESRD22,23,24,25. However, compared to standard control (less than 140 mmHg), intensive SBP control (less than 120 mmHg) in clinical trials did not show any CKD-related benefits in diabetic patients26. Compared to the conventional treatment goal of < 140/90 mmHg, lowering BP to below the current standard of < 130/80 mmHg did not yield additional benefits for overall kidney-related outcomes when in nondiabetic patients with CKD. Moreover, stringent BP management unexpectedly showed a threefold increase in CKD incidence in the group receiving intensive SBP treatment compared to the group receiving conventional treatment27.
Conversely, some research indicates that intensive BP management is crucial for preventing ESRD. Hsu et al. reported that the probability of developing ESRD was greater in patients with DM than in those without DM and that the probability of developing ESRD increased with increasing BP compared to that in individuals with a BP below 120/80 mmHg3. The Kidney Early Evaluation Program (KEEP) study, conducted with a large community-based group of individuals with established CKD, indicated that elevated SBP appeared to be the primary factor contributing to the risk of developing ESRD. However, the increased risk of ESRD was not observable until SBP exceeded 140 mmHg instead of the recommended target of less than 130 mmHg, and the increased risk was most significant among individuals with a SBP over 150 mmHg28. A nationwide population-based cohort study revealed that elevated SBP and DBP were associated with an increased risk of developing ESRD in adult patients with DM. Younger individuals were at a particularly higher risk17.
In this study, individuals with T2DM who had undergone PCI and had higher BP levels exhibited a dose-dependent increase in the risk of ESRD episodes compared to those with reference BP levels (SBP 120–129 mmHg and DBP 70–79 mmHg). The results observed in the high-risk patient group support the current Korean Diabetes Association guidelines recommending a lower BP target (< 130/80 mmHg) for hypertensive patients with type 2 diabetes compared to the target for low-risk individuals (< 140/90 mmHg). Furthermore, the risk of ESRD was notably elevated even in individuals with BP levels classified as normal (SBP 120–129 mmHg or DBP 80–84 mmHg) compared to those with optimal BP levels (SBP < 120 mmHg and DBP < 80 mmHg).
Post-PCI DBP exhibited a J-shaped curve starting at a DBP of 68 mmHg. In individuals with CAD, having a low SBP below 120 mmHg and a low DBP below 70 mmHg is linked to a greater likelihood of cardiovascular events, known as the J-curve phenomenon29,30. Since coronary perfusion occurs during the diastolic phase, it has been thought that low diastolic pressure causes coronary perfusion to decrease, which increases the likelihood of cardiac events31. Based on these observations, maintaining a BP target near < 130/80 mmHg may provide a balance between reducing ESRD risk and minimizing the potential harms of excessively low BP32.
In older patients, frailty should be carefully considered when establishing BP goals. Excessively aggressive BP reduction in frail elderly individuals may increase the risk of adverse outcomes, such as falls, syncope, or organ hypoperfusion33,34. In our subgroup analysis, patients aged > 65 years showed a relatively lower impact of higher BP on ESRD risk compared to those aged < 65 years. Therefore, individualized BP targets based on functional status, frailty, and comorbidities are crucial for optimizing outcomes in this population.
In this investigation, PP was identified as a significant risk factor for ESRD in this high-risk group. PP is a significant index derived from SBP and DBP to assess the pulsatile element and stiffness of the arteries. PP has been identified as a standalone predictor of cardiovascular mortality and morbidity35,36. The Framingham Heart Study showed that PP was more effective than SBP and DBP in predicting the risk of congestive heart disease37. Furthermore, individuals with elevated PP show an increased likelihood of developing ESRD according to many studies37,38,39,40. Within a population-based cohort in Singapore, compared with other BP indicators, such as SBP, DBP, and MAP, PP exhibited the most robust correlation with the risk of ESRD. Arterial stiffness, as indicated by PP, may negatively impact renal function through hemodynamic and metabolic damage41,42,43. Increased aortic stiffness leads to increased pressure fluctuations and wave reflection, causing elevated pressure and flow fluctuations in the microvascular beds of the kidneys. This can result in microvascular ischemia and injury to renal tissue35,44.
Our study indicates that managing hypertension is crucial for lowering the risk of ESRD. Therefore, enhancing adherence to antihypertensive medication and lifestyle changes are essential beginning in the early stages of CKD. Less than 45% of individuals with CKD achieve the desired BP targets, and effective management typically involves the use of 3 to 4 drugs45,46. Moreover, the effective rate of BP regulation via antihypertensive medication was approximately 70% among Korean patients with T2DM in 2016, as reported in the Diabetes and Metabolism Journal and the Korean Journal of Internal Medicine47. Although more aggressive BP reduction has been associated with an increase in hypotensive events, including severe hypotension, the potential benefits of treatment in high-risk groups generally outweigh the risks. Further research is needed to refine BP targets and minimize adverse effects in this population.
Our study has several strengths, including a large sample size, nationwide cohort design, and objective method for detecting ESRD. Nevertheless, our study has several limitations. First, important variables, such as medication information, combined diabetic complications, and glycemic control status, were not analyzed. Second, we analyzed the results of a one-time BP measurement using different devices during the health examination, and detailed information—such as the equipment brand, cuff size, arm used (dominant or non-dominant), or measurement timing—was not available. However, 1-time BP measurements taken by trained personnel have been shown to correlate with average BP levels, which is an important predictor of adverse outcomes48. Third, electronic health records may include diagnostic inaccuracies. Elevated BP readings could be influenced by white coat syndrome, while masked hypertension might lead to undetected true hypertension. Similarly, fasting glucose levels may vary due to non-fasting states or steroid use. Firth, there were differences in the time between BP measurement and PCI among the participants. Finally, the population observed in this study consisted of one ethnic group. Despite these limitations, our findings have implications for optimizing the management of hypertension to reduce the risk of ESRD in established CVD patients with T2DM. Managing BP within the target range may be beneficial for patients with T2DM and a history of PCI to reduce the risk of ESRD.
In short, Korean individuals with type 2 diabetes who had previously undergone PCI and had elevated BP levels had a greater risk of ESRD than did those with normal BP. ESRD is a severe complication for people with longstanding T2DM, who also frequently experience CVD as a vascular complication. Maintaining BP within the target range and providing comprehensive treatment are important for preventing ESRD in patients with confirmed CVD and T2DM. A J-shaped association between DBP and ESRD was observed in this study, suggesting potential risks associated with excessively low DBP. While intensive BP reduction might provide benefits in specific high-risk populations, such as individuals with documented CAD who have undergone PCI, careful consideration of BP targets is necessary to balance the benefits and risks. In addition, our findings provide additional evidence that the management of hypertension may require not only reducing SBP and DBP but also maintaining PP for renal protection. Further research is needed to determine the ideal BP target for individuals with type 2 diabetes at high risk of ESRD.
Conclusions
In this nationwide population-based research, among T2DM patients who underwent PCI, higher systolic and diastolic BP as well as PP were linked in a dose-response manner to an increased the risk of developing ESRD. Stricter BP control is required in T2DM patients who underwent PCI in order to prevent ESRD.
Data availability
The datasets produced or analyzed during this research are accessible upon reasonable request from the corresponding author.
References
Himmelfarb, J., Vanholder, R., Mehrotra, R. & Tonelli, M. The current and future landscape of dialysis. Nat. Rev. Nephrol. 16, 573–585. https://doi.org/10.1038/s41581-020-0315-4 (2020).
Hong, Y. A. et al. Trends in epidemiologic characteristics of end-stage renal disease from 2019 Korean Renal Data System (KORDS). Kidney Res. Clin. Pract. 40, 52–61, doi:https://doi.org/10.23876/j.krcp.20.202 (2021).
Ettehad, D. et al. Blood pressure Lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387, 957–967. https://doi.org/10.1016/s0140-6736(15)01225-8 (2016).
Mancia, G. et al. 2023 ESH guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the European society of hypertension: endorsed by the international society of hypertension (ISH) and the European renal association (ERA). J. Hypertens. 41, 1874–2071. https://doi.org/10.1097/hjh.0000000000003480 (2023).
Correction & ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention., Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71, e136-e139, (2017). https://doi.org/10.1161/hyp.0000000000000075 (2018).
Choi, J. H. et al. 2023 Clinical practice guidelines for diabetes mellitus of the Korean diabetes association. Diabetes Metab. J. 47, 575–594. https://doi.org/10.4093/dmj.2023.0282 (2023).
Cheol Seong, S. et al. Data resource profile: the National health information database of the National health insurance service in South Korea. Int. J. Epidemiol. 46, 799–800. https://doi.org/10.1093/ije/dyw253 (2017).
Bae, E. H. et al. Association between systolic and diastolic blood pressure variability and the risk of End-Stage renal disease. Hypertension 74, 880–887. https://doi.org/10.1161/hypertensionaha.119.13422 (2019).
Lee, H. S., Nam, J. H., Oh, D. J., Ahn, H. J. & Lim, Y. J. Association between eupatilin and reduction in small bowel bleeding in aspirin users and aspirin plus acid suppressant users. Korean J. Intern. Med. 38, 484–492. https://doi.org/10.3904/kjim.2022.340 (2023).
Koh, E. S. et al. Weight change and microvascular outcomes in patients with new-onset diabetes: a nationwide cohort study. Korean J. Intern. Med. 36, 932–941. https://doi.org/10.3904/kjim.2020.121 (2021).
Yang, Y. S., Han, K., Sohn, T. S. & Kim, N. H. Young-onset type 2 diabetes in South Korea: a review of the current status and unmet need. Korean J. Intern. Med. 36, 1049–1058. https://doi.org/10.3904/kjim.2021.379 (2021).
Lee, C. W. et al. Blood pressure and mortality after percutaneous coronary intervention: a population-based cohort study. Sci. Rep. 12, 2768. https://doi.org/10.1038/s41598-022-06627-4 (2022).
Lee, J. Y. et al. Long-term cardiovascular events in hypertensive patients: full report of the Korean hypertension cohort. Korean J. Intern. Med. 38, 56–67. https://doi.org/10.3904/kjim.2022.249 (2023).
Bae, E. H. et al. Low waist circumference prior to percutaneous coronary intervention predict the risk for end-stage renal disease: a nationwide Korean population based-cohort study. Korean J. Intern. Med. 37, 639–652. https://doi.org/10.3904/kjim.2021.313 (2022).
Zeitouni, M. et al. 2019 ESC/EAS guidelines for management of dyslipidaemia: strengths and limitations. Eur. Heart J. Cardiovasc. Pharmacother. 7, 324–333. https://doi.org/10.1093/ehjcvp/pvaa077 (2021).
Bae, E. H. et al. Blood pressure prior to percutaneous coronary intervention is associated with the risk of end-stage renal disease: a nationwide population based-cohort study. Kidney Res. Clin. Pract. 40, 432–444. https://doi.org/10.23876/j.krcp.21.245 (2021).
Bae, E. H. et al. Effects of blood pressure according to age on End-Stage renal disease development in patients with diabetes: A nationwide Population-Based cohort study. Hypertension 79, 1765–1776. https://doi.org/10.1161/hypertensionaha.121.18881 (2022).
Lee, H. et al. Risk of end-stage renal disease in patients with hypertrophic cardiomyopathy: A nationwide population-based cohort study. Sci. Rep. 9, 14565. https://doi.org/10.1038/s41598-019-50993-5 (2019).
Ishigami, J. et al. Incident hospitalization with major cardiovascular diseases and subsequent risk of ESKD: implications for cardiorenal syndrome. J. Am. Soc. Nephrol. 31, 405–414. https://doi.org/10.1681/asn.2019060574 (2020).
Lv, J. et al. Effects of intensive blood pressure Lowering on cardiovascular and renal outcomes: a systematic review and meta-analysis. PLoS Med. 9, e1001293. https://doi.org/10.1371/journal.pmed.1001293 (2012).
Xie, X. et al. Effects of intensive blood pressure Lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet 387, 435–443. https://doi.org/10.1016/s0140-6736(15)00805-3 (2016).
Young, J. H. et al. Blood pressure and decline in kidney function: findings from the systolic hypertension in the elderly program (SHEP). J. Am. Soc. Nephrol. 13, 2776–2782. https://doi.org/10.1097/01.asn.0000031805.09178.37 (2002).
Rifkin, D. E. et al. Blood pressure components and decline in kidney function in community-living older adults: the cardiovascular health study. Am. J. Hypertens. 26, 1037–1044. https://doi.org/10.1093/ajh/hpt067 (2013).
Bell, E. K. et al. Blood pressure indexes and end-stage renal disease risk in adults with chronic kidney disease. Am. J. Hypertens. 25, 789–796. https://doi.org/10.1038/ajh.2012.48 (2012).
Reynolds, K. et al. A population-based, prospective study of blood pressure and risk for end-stage renal disease in China. J. Am. Soc. Nephrol. 18, 1928–1935. https://doi.org/10.1681/asn.2006111199 (2007).
Cushman, W. C. et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl. J. Med. 362, 1575–1585. https://doi.org/10.1056/NEJMoa1001286 (2010).
Beddhu, S. et al. Effects of intensive systolic blood pressure control on kidney and cardiovascular outcomes in persons without kidney disease: A secondary analysis of a randomized trial. Ann. Intern. Med. 167, 375–383. https://doi.org/10.7326/m16-2966 (2017).
Peralta, C. A. et al. Blood pressure components and end-stage renal disease in persons with chronic kidney disease: the kidney early evaluation program (KEEP). Arch. Intern. Med. 172, 41–47. https://doi.org/10.1001/archinternmed.2011.619 (2012).
Gaffney, B., Jacobsen, A. P., Pallippattu, A. W., Leahy, N. & McEvoy, J. W. The diastolic blood pressure J-Curve in hypertension management: links and risk for cardiovascular disease. Integr. Blood Press. Control. 14, 179–187. https://doi.org/10.2147/ibpc.S286957 (2021).
Böhm, M. et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet 389, 2226–2237. https://doi.org/10.1016/s0140-6736(17)30754-7 (2017).
Messerli, F. H. et al. Dogma disputed: can aggressively Lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann. Intern. Med. 144, 884–893. https://doi.org/10.7326/0003-4819-144-12-200606200-00005 (2006).
Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 39, 3021–3104. https://doi.org/10.1093/eurheartj/ehy339 (2018).
Odden, M. C., Beilby, P. R. & Peralta, C. A. Blood pressure in older adults: the importance of frailty. Curr. Hypertens. Rep. 17, 55. https://doi.org/10.1007/s11906-015-0564-y (2015).
Guasti, L. et al. Management of hypertension in the elderly and frail patient. Drugs Aging. 39, 763–772. https://doi.org/10.1007/s40266-022-00966-7 (2022).
Geng, T. T., Talaei, M., Jafar, T. H., Yuan, J. M. & Koh, W. P. Pulse pressure and the risk of End-Stage renal disease among Chinese adults in Singapore: the Singapore Chinese health study. J. Am. Heart Assoc. 8, e013282. https://doi.org/10.1161/jaha.119.013282 (2019).
Chae, C. U. et al. Increased pulse pressure and risk of heart failure in the elderly. Jama 281, 634–639. https://doi.org/10.1001/jama.281.7.634 (1999).
Franklin, S. S., Khan, S. A., Wong, N. D., Larson, M. G. & Levy, D. Is pulse pressure useful in predicting risk for coronary heart disease?? The Framingham heart study. Circulation 100, 354–360. https://doi.org/10.1161/01.cir.100.4.354 (1999).
Mitchell, G. F. et al. Arterial stiffness and cardiovascular events: the Framingham heart study. Circulation 121, 505–511. https://doi.org/10.1161/circulationaha.109.886655 (2010).
Franklin, S. S. et al. Does low diastolic blood pressure contribute to the risk of recurrent hypertensive cardiovascular disease events? The Framingham heart study. Hypertension 65, 299–305. https://doi.org/10.1161/hypertensionaha.114.04581 (2015).
Lorenzo, C., Aung, K., Stern, M. P. & Haffner, S. M. Pulse pressure, prehypertension, and mortality: the San Antonio heart study. Am. J. Hypertens. 22, 1219–1226. https://doi.org/10.1038/ajh.2009.151 (2009).
Briet, M., Boutouyrie, P., Laurent, S. & London, G. M. Arterial stiffness and pulse pressure in CKD and ESRD. Kidney Int. 82, 388–400. https://doi.org/10.1038/ki.2012.131 (2012).
Safar, M. E., Plante, G. E. & Mimran, A. Arterial stiffness, pulse pressure, and the kidney. Am. J. Hypertens. 28, 561–569. https://doi.org/10.1093/ajh/hpu206 (2015).
Warren, J. et al. Impact of Pre-Procedural blood pressure on Long-Term outcomes following percutaneous coronary intervention. J. Am. Coll. Cardiol. 73, 2846–2855. https://doi.org/10.1016/j.jacc.2019.03.493 (2019).
O’Rourke, M. F. & Safar, M. E. Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension 46, 200–204. https://doi.org/10.1161/01.Hyp.0000168052.00426.65 (2005).
Peralta, C. A. et al. Control of hypertension in adults with chronic kidney disease in the united States. Hypertension 45, 1119–1124. https://doi.org/10.1161/01.Hyp.0000164577.81087.70 (2005).
Hebert, L. A. et al. Effects of blood pressure control on progressive renal disease in Blacks and whites. Modification of diet in renal disease study group. Hypertension 30, 428–435. https://doi.org/10.1161/01.hyp.30.3.428 (1997).
Ha, K. H. & Kim, D. J. Current status of managing diabetes mellitus in Korea. Korean J. Intern. Med. 31, 845–850. https://doi.org/10.3904/kjim.2016.253 (2016).
Staessen, J. A. et al. Task force II: blood pressure measurement and cardiovascular outcome. Blood Press. Monit. 6, 355–370. https://doi.org/10.1097/00126097-200112000-00016 (2001).
Acknowledgements
We express our gratitude to the Korean National Health Insurance Service for providing access to their database. Additionally, we acknowledge the invaluable contributions of medical writers, proofreaders, and editors in the development of this manuscript.
Author information
Authors and Affiliations
Contributions
Conception or design: S.H.K., D.G.M.Acquisition, analysis, or interpretation of data: K.D.H., Y.M.P.Drafting the work or revising: S.H.K, D.G.M, H.L.K.Final approval of the manuscript: S.H.K., D.G.M., H.L.K., K.D.H., Y.M.P., J.S.Y., K.H.K., Y.J.C., H.W.K., Y.K.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical declarations
This study was approved by the Institutional Review Board of the Catholic University of Korea St. Vincent’s Hospital (IRB no. VC23ZISE0366). The requirement for informed consent from the study subjects was waived by the IRB of the Catholic University of Korea St. Vincent’s Hospital due to the retrospective study design. All methods were performed in accordance with the principles of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, H., Park, YM., Ko, SH. et al. Blood pressure levels and risk of end-stage renal disease in patients with type 2 diabetes who underwent percutaneous coronary intervention: a nationwide population-based study. Sci Rep 15, 7832 (2025). https://doi.org/10.1038/s41598-025-91835-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91835-x
Keywords
This article is cited by
-
Knowledge, Attitudes, and Practices Survey on Hypertensive Nephropathy Among Hypertensive Patients in Xinjiang, China: A Cross-Sectional Study
Journal of General Internal Medicine (2026)