Abstract
To explore the value of cytogenetic risk stratification combined with minimal residual disease (MRD) status in predicting the therapeutic efficacy and prognosis for multiple myeloma (MM). From January 2017 to December 2023, 73 cases of newly diagnosed MM were recruited. Cytogenetic risks were stratified according to the results of fluorescence in situ hybridization (FISH); MRD status and clinical data were analyzed. The progression-free survival (PFS) and overall survival (OS), and their influencing factors were evaluated. During the median follow-up period of 30 (4–65) months, the median progression-free survival (PFS) and overall survival (OS) were 38 (95% CI 29.7, 46.3) months and 55 (95% CI 45.9, 64.1) months, respectively. In our cohort, the 3-year PFS rate was 51.0% and the 3-year OS rate was 71.0%. According to the MRD status, 31 MM patients were assigned to the MRD-positivity group and 42 to the MRD-negativity group. Significant differences were detected in the median PFS (30 months vs. 45 months, χ2 = 7.747, P = 0.005) and OS (34 months vs. 59 months, χ2 = 8.683, P = 0.003) between groups. Subgroup analyses based on the cytogenetic risk stratification (standard risk [SR] and high risk [HR]) showed that MM patients in the SR/MRD-negativity subgroup did not reach the median PFS and OS, and the median PFS (42 months vs. 33 months, P = 0.093) and OS (59 months vs. 42 months, P = 0.703) were similar between the SR/MRD-positivity and HR/MRD-negativity subgroups. In comparison to the HR/MRD-negativity subgroup, the median PFS (20 months vs. 33 months, P = 0.031) and OS (33 months vs. 42 months, P = 0.032) were significantly shorter in the HR/MRD-positivity group. Multivariate analysis showed that MRD-positivity was an independent risk factor for PFS (HR 2.874, 95% CI 1.452, 5.689; P = 0.008) and OS (HR 3.504, 95% CI 1.599, 7.676; P = 0.002) of MM. MRD status is a powerful prognostic indicator of PFS and OS in MM, but its performance is inferior to cytogenetic risk stratification. More high-risk cytogenetic abnormalities (HRCAs) indicate a worse prognosis of MM, while MRD-negativity improves HRCA-associated prognosis of MM. We recommend a risk stratification by assessing MRD status combined with HRCAs in MM patients, thus favoring the design of individualized treatment.
Similar content being viewed by others
Introduction
Multiple myeloma (MM), a malignant clonal tumor developing from plasma cells, features a globally increasing incidence, a high recurrence rate and an incurability1,2. Current treatments only aim to relieve complications and improve the quality of life by a long-term suppression on cancer cells3. Due to science advances over the past two decades, new treatments have significantly increased the remission rate and survival rate4,5. However, high-risk (HR) MM patients gain inferior benefits on the progression-free survival (PFS) and overall survival (OS) than standard-risk (SR) MM patients5. MM associated with high-risk cytogenetic abnormality (HRCA) has still a poor prognosis6. Therefore, a more reliable index, rather than the stringent complete response (sCR), is urgently needed to assess the treatment outcome of MM.
Minimal residual disease (MRD) can be measured, and its negativity is associated with a better outcome of MM1. MRD-directed therapy has caught wide interests among MM researchers7. Importantly, MRD-negativity can dilute partial effects of HRCA on the poor prognosis of MM8, and MRD status, as an index, may offer valuable information to guide the individualized treatment9. In real-world studies, the prognostic value of cytogenetic risk stratification combined with MRD status in MM has been rarely reported. As indicated by the Mayo Stratification of Myeloma and Risk-adapted Therapy (mSMART), MM patients can be classified into SR and HR, both of which can be based on to guide treatment and management decisions.
In the present study, cytogenetic risk stratification was performed according to the results of fluorescence in situ hybridization (FISH), and MRD status was measured in MM patients. We then explored the value of their combination in predicting the prognosis. Our findings are expected to provide references for decision-making in clinical MM treatment.
Methods
Subjects
From January 2017 to December 2023, we recruited a total of 73 patients diagnosed as having new-onset MM by the International Myeloma Working Group (IMWG) criteria 2014 10, at the Department of Hematology of the First People’s Hospital of Lianyungang. Their demographic data, baseline characteristics, and laboratory indexes were collected. The present study was approved by the Ethics Committee of the First People’s Hospital of Lianyungang (No. KY-20240110001-02) and all methods were performed in accordance with in accordance with the Declaration of Helsinki. Informed consent was obtained from all individual participants or their legal representatives. Here, extramedullary lesions in MM referred to either bone-related extramedullary masses or those outside of the bone marrow.
FISH
Cytogenetic analysis was performed in all patients prior to FISH. Briefly, CD138+ cells were sorted from the bone marrow specimens. Cytogenetic features, including p53 deletions, 1q21 amplification, 13q14 deletions and IgH rearrangements, were detected. FISH analyses of t(4;14), t(4;14) and t(14;16) were additionally conducted in MM patients harboring IgH rearrangements. According to the European Myeloma Network (EMN), a positive result was defined by the 20% of cut-off values for 1q21 amplification and del(17p), and 10% of cut-off values for t(4;14), t(4;14) and t(14;16).
As proposed by mSMART 3.0, MM patients carrying del(17p), t(4;14), t(14;16) and 1q21 amplification were classified into the HR category, otherwise into the SR category11. We did not perform FISH analysis of t(14;20) in the present study, due to the extremely low detection rate of 1% in MM patients4.
MRD detection
MRD in bone marrow specimens was detected by the Euroflow next-generation flow cytometry via examining an immunophenotyping panel of CD117, CD19, CD20, CD269, CD27, CD28, CD45, CD56, CD81, CyIgλ, CyIgκ, CD38 and CD138. MRD negativity was determined by a 10‒5 threshold of abnormal plasma cells in the bone marrow.
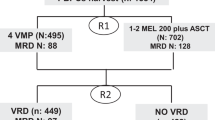
Treatment regimens
MM patients were determined as qualified or disqualified for a stem cell transplant according to their pre-treatment ages and physical conditions. MM patients in the categories of SR and HR were given corresponding treatment regimens. Following an induction therapy, MM patients in the SR and HR groups were subdivided into MRD-negativity (< 10‒5) and MRD-positivity subgroups (≥ 10‒5)12.
Induction therapy was applied to all MM patients, including regimens consisting of a proteasome inhibitor (PI) and other drugs, and those composing a PI, an immunomodulatory drug (IMiD) and/or other drugs. The former included the VAD (Bortezomib + Epirubicin + Dexamethasone), VCD (Bortezomib + Cyclophosphamide + Dexamethasone) and VD (Bortezomib + Dexamethasone); and the latter included the VRD (Bortezomib + Lenalidomide + Dexamethasone), VTD (Bortezomib + Thalidomide + Dexamethasone), PI + IMiD + anti-CD38 monoclonal antibody, and D-VRd (Bortezomib + Lenalidomide + Dexamethasone).
Efficacy evaluation
The efficacy was evaluated after four cycles of induction therapies by the IMWG response criteria and classified into sCR, complete remission (CR), very good partial response (VGPR), partial response (PR), minor response (MR), stable disease (SD) and progressive disease (PD)12. The overall response ratio (ORR) was the sum of the ratios of sCR, CR, VGPR and PR.
Follow-up
Follow-up was conducted by reviewing the electronic medical records, outpatient re-examinations and telephone contact. As of December 31, 2023, the follow-up reached a median period of 30 (4–65) months. The interval from the start of treatment to disease progression, recurrence, death or the final follow-up visit was recorded as PFS. OS was defined as the time from diagnosis to death or the final follow-up visit.
Statistical analysis
Statistical analysis was performed using SPSS 26.0 and Graphpad Prism 8.0. Enumeration data were expressed as n (%), and differences between groups were analyzed by the Chi-square test or Fisher’s exact test. Kaplan-Meier curves were plotted to assess the survival, and the differences between the two groups were analyzed by the Log-rank test. A Cox proportional hazards model was performed to identify relationships between clinical data and prognosis of MM. P < 0.05 was considered as statistically significant.
Results
Baseline characteristics of MM patients
Of the 73 patients with newly diagnosed MM were 48 (65.8%) males and 25 (34.2%) females. There were 35 (47.9%) cases younger than 65 years and 38 (52.1%) older than 65 years, with a median onset age of 66 (45–81) years. They were divided into the SR (n = 33) and HR (n = 40) groups based on the cytogenetic risk stratification.
Hypercalcemia (Ca > 2.65 mmol/L), impaired renal function (creatinine > 177 µmol/L), anemia (hemoglobin ≤ 100 g/L), osteolytic lesions, extramedullary lesions, elevated lactate dehydrogenase (> 245 U/L), elevated β2-microglobulin (≥ 5.5 mg/L), low albumin (< 35 g/L), and thrombocytopenia (platelet count < 125 × 109/L) were detected in 8 (10.9%), 21 (28.8%), 50 (68.5%), 57 (78.1%), 11 (15.1%), 12 (16.4%), 28 (38.4%), 48 (65.7%) and 21 (28.8%) cases, respectively.
Diagnosed based on immunoglobulin types, 39 (53.4%) cases were diagnosed as IgG MM, 16 (21.9%) as IgA MM, 16 (21.9%) of light-chain only, and 2 (2.7%) as non-secretory myeloma. Determined by the bone marrow plasma cell (BMPC) percentage at diagnosis, 13 (17.8%) MM patients had a BMPC% exceeding 60%, and 60 (82.2%) lower than 60%.
Between the SR and HR groups, no significant differences were observed in sex, age, clinical manifestations, types of MM and BMPC% values (all P > 0.05, Table 1).
MM staging and treatment regimens
The Durie-Salmon staging system classified 73 MM patients into stage I (2/73, 2.7%), stage II (9/73, 12.4%) and stage III (62/73, 84.9%). Categorized by the International Staging System (ISS), 10 (13.7%), 32 (43.8%) and 31 (42.5%) cases were in stages I, II and III, respectively. The Revised International Staging System (R-ISS) divided them into stage I (7/73, 9.6%), stage II (52/73, 71.2%) and stage III (14/73, 19.2%). We determined no significant differences among the results of three staging methods for MM between SR and HR groups (all P > 0.05, Table 2), except the R-ISS (χ2 = 13.812, P = 0.001, Table 2).
All patients were treated by induction therapies, with 42 (57.5%) cases managed by a PI-based regimen, 25 (34.2%) with the PI + IMiD regimen, and 6 (8.2%) intervened with PI + IMiD + anti-CD38 monoclonal antibody. A total of 16 MM patients received stem cell transplant. The proportions of MM patients treated with various regimens of induction therapies and whether they under transplantation were comparable between SR and HR groups (all P > 0.05, Table 3).
Cytogenetic risk stratification of MM patients
Cytogenetic profiling showed 36 (49.3%) cases of 1q21 amplification, 5 (6.8%) of del(17p), 10 (13.7%) of t(4;14), 2 (2.7%) of t(14;16) and 11 (15.1%) of t(11;14). Among them, 33 (45.2%), 27 (37.0%) and 13 (17.8%) MM patients carried 0, 1, and 2 HRCA, respectively. Cytogenetic abnormalities were depicted in Supplementary Table S1 online.
Clinical efficacy
Of the 73 MM patients, CR showed in 33 (45.2%) cases, sCR in 24 (32.9%) cases, VGPR in 18 (24.7%) cases, PR in 20 (27.4%) cases and SD in 2 (2.7%) cases, yielding an ORR of 97.3%. Of the 16 MM patients treated with stem cell transplant, CR, VGPR and PR before transplantation were observed in 6, 4 and 6 cases, respectively. After transplantation, PR was improved to CR in 3 cases, and VGPR to CR in 2 cases. The ratio of CR plus sCR was significantly higher in MM patients treated with stem cell transplant than in their counterparts (χ2 = 4.586, P = 0.032, see Supplementary Table S2 online).
Among MM patients carrying 1 HRCA, CR appeared in 11 cases, VGPR in 6 cases and PR in 10 cases. Among MM patients carrying 2 HRCAs, CR appeared in 5 cases, VGPR in 3 cases, PR in 3 cases and SD in 2 cases. Among MM patients lacking HRCA, CR appeared in 17 cases, VGPR in 9 cases and PR in 7 cases. The distributions of these outcomes were comparable among the three groups (χ2 = 0.994, P = 0.610, see Supplementary Table S2 online).
Correlation of MRD status with the cytogenetic risk stratification and clinical outcome of MM
MRD negativity was detected in 42 (57.5%) MM patients, with a median time to MRD negativity of 9.5 (2.5–20) months following induction therapy. Of them, CR appeared in 24 cases (57.1%) who had shown MRD negativity at the first time of measurement, including sCR in 20 cases (47.6%). Of the remaining 19 cases (43.9%) failing to achieve CR, 4 gained CR after the consolidation therapy and second-line therapy. Only 5 cases of CR were found in the MRD positivity group. The ratio of CR was significantly higher in the MRD negativity group than the MRD positivity group (66.7% vs. 16.1%, χ2 = 18.391, P < 0.001, Table 4).
Among the 16 MM patients treated with stem cell transplant, 12 (75.0%) cases showed MRD negativity, involving 10 cases of CR. Only 1 (25.0%) case of CR was found in MRD-positive MM patients treated with stem cell transplant. Although the ratio of CR was much higher in the MRD negativity group of MM patients treated with stem cell transplant than in the MRD positivity group, no significant difference was detected (P = 0.063, see Supplementary Table S2 online).
Except for the ratio of MM patients with BMPC ≥ 60% (χ2 = 4.638, P = 0.031) and CR/sCR (χ2 = 18.391, P < 0.001), the remaining demographic data, clinical manifestations, immunoglobin types (M-protein), staging, treatment regimens, HRCA and treatment of stem cell transplantation were comparable between MRD-negativity and MRD-positivity groups (all P > 0.05, Table 4).
No significant difference was detected in the MRD-negativity ratio between SR and HR groups (63.6% vs. 52.5%, χ2 = 0.918, P = 0.338, Table 4). The distributions of clinical responses (Supplementary Fig. S1A) and HRCAs (Supplementary Fig. S1B) in MRD-negativity and MRD-positivity groups are shown in Supplementary Fig. S1 online.
Correlation of MRD status with the prognosis of MM
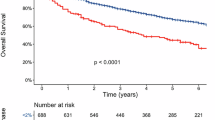
Overall, 73 MM patients were followed up with a median period of 30 (4–65) years, with a median PFS of 38 (95% CI 29.7, 46.3) months and a median OS of 55 (95% CI 45.9, 64.1) months. The 3-year PFS and OS rates were 51.0% and 71.0%, respectively (Fig. 1).
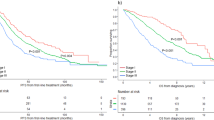
Divided by the cytogenetic risk stratification, the median PFS and OS did not reach in the SR group, but reached 28 (95% CI 20.3, 35.7) months and 39 (95% CI 31.8, 46.2) months in the HR group, respectively. The 3-year PFS (85% vs. 23%, χ2 = 30.916, P < 0.001) and 3-year OS (88% vs. 57%, χ2 = 13.990, P < 0.001) were significantly higher in the SR group than in the HR group (Fig. 2A, B). There were significant differences in the median PFS (not reached vs. 33 months vs. 17 months, χ2 = 73.314, P < 0.001) and OS (not reached vs. 44 months vs. 30 months, χ2 = 33.864, P < 0.001) in MM patients carrying 0, 1 and ≥ 2 HRCA (Fig. 2C, D). A greater number of HRCAs indicated a worse prognosis of MM.
Divided by the MRD status, the median PFS was significantly longer in the MRD-negativity group than in the MRD-positivity group (45 [95% CI 35.0, 54.9] months vs. 30 [95% CI 21.9, 38.0] months, χ2 = 7.747, P = 0.005), with a 3-year PFS of 65.0% and 33.0%, respectively (Fig. 3A). Consistently, a significantly longer median OS was detected in the MRD-negativity group than in the MRD-positivity group (59 [95% CI 43.2, 74.8] months vs. 34 [95% CI 26.8, 41.2] months, χ2 = 8.683, P = 0.003). The 3-year OS was 88.0% in the MRD-negativity group and 50.0% in the MRD-positivity group (Fig. 3B).
Subgroup analyses on the survival of MM patients. A, B The median PFS (A) and OS (B) in MM patients divided by the MRD status. (C, D) The median PFS (C) and OS (D) in MM patients divided by the cytogenetic risk stratification combined with the MRD status. (E, F) The median PFS (E) and OS (F) in MM patients divided by the clinical response combined with the MRD status.
Subgroup analyses were further conducted based on the cytogenetic risk stratification in the MRD-negativity and MRD-positivity groups. The longest PFS (not reached) and OS (not reached) were observed in the SR/MRD-negativity subgroup. In MRD-negative MM patients, the median PFS (33 months vs. not reached, P < 0.001) and OS (42 months vs. not reached, P = 0.003) in the HR/MRD-negativity subgroup were significantly inferior to those in the SR/MRD-negativity subgroups. However, MM patients in the SR/MRD-positivity subgroup did not gain more survival benefits than those in the HR/MRD-negativity group (median PFS: 33 months vs. 42 months, P = 0.093; median OS: 42 months vs. 59 months, P = 0.703). The median PFS (20 months vs. 33 months, P = 0.031) and OS (33 months vs. 42 months, P = 0.032) were significantly shorter in the HR/MRD-positivity subgroup than in the HR/MRD-negativity subgroup (Fig. 3C, D). Overall, MRD negativity partially overcame the deleterious influence of HRCA on the prognosis of MM.
Furthermore, MM patients in the MRD-negativity and MRD-positivity groups were subdivided according to CR (Fig. 3E, F). In the MRD-negativity group, the median PFS (not reached vs. 34 months, P = 0.226) and OS (not reached vs. 59 months, P = 0.156) were similar in individuals having achieved either CR or not. The median PFS was not reached in MM patients with CR from either MRD-negativity or MRD-positivity groups; but the median OS was significantly inferior in CR/MRD-positivity subgroup than tin he CR/MRD-negativity subgroup (33 months vs. not reached, P = 0.014). Collectively, MRD status was more sensitive than the clinical response in predicting the prognosis of MM.
Prognostic factors of MM
Univariate analysis showed that age, BMPC%, R-ISS, clinical response, cytogenetic profile and MRD status significantly influenced the PFS in MM patients (all P < 0.05); and clinical response, cytogenetic profile and MRD status were significantly related to the OS (all P < 0.05). Multivariate analysis further identified that cytogenetic profile and MRD status were risk factors for both the PFS and OS in MM patients (all P < 0.05, Table 5).
Discussion
In our cohort of 73 MM patients, ORR was achieved in 97.3% (71/73) and MRD-negativity in 57.5% (42/73). More favorable survival outcomes were observed in MRD-negative MM patients than in the MRD-positivity group, which is consistent with previous real-world findings13,14,15. Cox regression further confirmed that the MRD status and cytogenetic profile were prognostic factors for MM. Although the prognostic potential of MRD status in MM was not superior to cytogenetic risk stratification, MRD-negativity partially compensate for the adverse influence of HRCA on MM and offered prognostic benefits to those failed to achieve CR.
The proportion of MM patients reaching CR was significantly higher in the MRD-negativity group than in the MRD-positivity group (66.7% vs. 16.1%), revealing a close relationship between CR and MRD-negativity in MM13. However, MRD-negativity did not synchronize with CR in neither the incidence nor the duration in MM patients, which is consistent with previous findings16,17,18,19,20. Such a phenomenon could be attributed to fact that the half-life of M-protein may last longer than the time for tumor cells to perish following the induction therapy, local distribution of tumor cells, and variations in clinical samples, detections and thresholds. Our data showed no significant differences in the median PFS and OS in MRD-negative MM patients with CR or not. On the contrary, the median OS was inferior in the CR/MRD-positivity subgroup than in the CR/MRD-negativity subgroup. The PFS and OS were comparable between patients showing negative MRD status and CR, suggesting the clinical significance of the MRD status in assessing the outcome of MM21,22,23.
Clinical trials and real-world studies have validated that stem cell transplantation is a major factor contributing to MRD negativity in MM patients13,14,24,25,26. In the present study, stem cell transplantation was found to have no influences on the MRD status, probably due to the small sample size. Notably, the MRD-negativity ratio was significantly higher in MM patients receiving stem cell transplant than the ineligible individuals. The median PFS and OS were longer in MRD-negative MM patients treated with stem cell transplant, although significant differences were not detectable.
HRCA is an established risk for the prognosis of MM, but its negative influence on PFS and OS could be partially offset by a negative MRD status6. Paiva et al.27 have reported a significantly lower MRD-negativity ratio in HR MM patients than in the SR group, whereas the 3-year PFS is similar between HR and SR MM patients with a negative MRD status. Inconsistently, the Myeloma XI trial has proved the unfavorable outcomes of PFS and OS caused by HRCA, even in MRD-negative MM patients28. A long-term follow-up of the IFM 2009 trial has reported a poor PFS in HR patients, and similar PFSs between SR and HR patients who achieve a negative MRD status at the end of the maintenance therapy29. The PETHEMA/GEM2012MENOS65 study has shown better outcomes in the HR group of MRD-negative MM patients than in the SR group30。Overall, the influence of HRCA on the prognosis of MM may not equal to that of the MRD negativity1,29. In our study, the MRD-negativity ratio differed between the SR and HR groups, and MM patients possessing a combination of SR and negative MRD benefited the most. Although in a negative MRD status, MM patients in the cytogenetic category of HR suffered from an inferior survival than the SR category. Taken together, a long-term negative MRD status could partially offset the influence of HRCA on MM prognosis, although its prognostic potential in MM might not outperform that of cytogenetic risk stratification29.
Double-hit/triple-hit MM patients, possessing 2 or 3 cytogenetic abnormalities, present an extremely poor prognosis31. The disease-progression rate of MM and recurrence rate of MRD increase in individuals carrying a minimum of 2 HRCAs32. A negative MRD status can be referred to make clinical decisions following stem cell transplant, and predict the survival of MM patients with extremely high risks of cytogenetic abnormalities33. A retrospective study suggests that MRD negativity achieved prior to stem cell transplantation significantly improves PFS and OS in triple-hit MM patients34. Generally, we believed that a negative MRD in HR MM patients achieved and/or maintained by sufficient individualized treatments favors a satisfactory outcome35. Besides, stem cell transplantation can be postponed in SR MM patients carrying a MRD negative status. Both the MRD status and cytogenetic classification can be introduced into clinical decision-making33.
The following limitations in the present study should be noted. First, this was a retrospective study with a small sample size. Second, we did not perform a dynamic monitoring of MRD, and a persistent MRD-negativity status may possess a stronger prognostic value in MM. Third, MRD measurements and patient compliance can be influenced by multiple factors like local economic level and healthcare resources, which may ignite the passion of researchers in the future.
Taken together, risk stratification can be performed in MM patients by measuring the MRD status and the cytogenetic profiles, thus offering valuable references to guide clinical management and improve the prognosis of MM.
Data availability
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
References
Mohty, M., Avet-Loiseau, H., Malard, F. & Harousseau, J. L. Potential future direction of measurable residual disease evaluation in multiple myeloma. Blood 142, 1509–1517. https://doi.org/10.1182/blood.2023020284 (2023).
Malard, F. et al. Multiple myeloma. Nat. Rev. Dis. Primers. 10 https://doi.org/10.1038/s41572-024-00529-7 (2024).
Cowan, A. J. et al. Diagnosis and management of multiple myeloma: A review. JAMA 327, 464–477. https://doi.org/10.1001/jama.2022.0003 (2022).
Rajkumar, S. V. Multiple myeloma: 2024 update on diagnosis, risk-stratification, and management. Am. J. Hematol. 99, 1802–1824. https://doi.org/10.1002/ajh.27422 (2024).
Zamagni, E., Barbato, S. & Cavo, M. How I treat high-risk multiple myeloma. Blood 139, 2889–2903. https://doi.org/10.1182/blood.2020008733 (2022).
Liang, D. et al. Clinical outcome of induction treatment in the era of novel agents and the impact of the number of high-risk cytogenetic abnormalities (HRA) on prognosis of patients with newly diagnosed multiple myeloma (NDMM): insights from a multicenter study. Cancer Med. 13, e70270. https://doi.org/10.1002/cam4.70270 (2024).
Zhou, H. X. & Chen, W. M. Minimal residual disease assessment and progress in multiple myeloma. Zhonghua Xue Ye Xue Za Zhi. 45, 203–208. https://doi.org/10.3760/cma.j.cn121090-20230728-00036 (2024).
Cavo, M. et al. Prognostic value of minimal residual disease negativity in myeloma: combined analysis of POLLUX, CASTOR, ALCYONE, and MAIA. Blood 139, 835–844. https://doi.org/10.1182/blood.2021011101 (2022).
Szalat, R., Anderson, K. & Munshi, N. Role of minimal residual disease assessment in multiple myeloma. Haematologica 109, 2049–2059. https://doi.org/10.3324/haematol.2023.284662 (2024).
Rajkumar, S. V. et al. International myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 15, e538–548. https://doi.org/10.1016/S1470-2045(14)70442-5 (2014).
Rajkumar, S. V. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am. J. Hematol. 95, 548–567. https://doi.org/10.1002/ajh.25791 (2020).
Kumar, S. et al. International myeloma working group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 17, e328–e346. https://doi.org/10.1016/s1470-2045(16)30206-6 (2016).
Wang, J. et al. Real-world prognostic significance of attaining minimal residual disease negativity in newly diagnosed multiple myeloma. Discov Oncol. 15, 38. https://doi.org/10.1007/s12672-024-00891-8 (2024).
Tao, Y. et al. Real-world advantage and challenge of post-autologous stem cell transplantation MRD negativity in high-risk patients with double-hit multiple myeloma. BMC Cancer. 24, 406. https://doi.org/10.1186/s12885-024-12077-0 (2024).
Munshi, N. C. et al. A large meta-analysis establishes the role of MRD negativity in long-term survival outcomes in patients with multiple myeloma. Blood Adv. 4, 5988–5999. https://doi.org/10.1182/bloodadvances.2020002827 (2020).
Yee, A. J. & Raje, N. Minimal residual disease in multiple myeloma: why, when, where. Hematol. Am. Soc. Hematol. Educ. Program 37–45, (2021). https://doi.org/10.1182/hematology.2021000230 (2021).
Paiva, B., San-Miguel, J. & Avet-Loiseau, H. MRD in multiple myeloma: does CR really matter? Blood 140, 2423–2428. https://doi.org/10.1182/blood.2022016170 (2022).
Landgren, O. et al. EVIDENCE meta-analysis: evaluating minimal residual disease as an intermediate clinical end point for multiple myeloma. Blood 144, 359–367. https://doi.org/10.1182/blood.2024024371 (2024).
Ding, H. et al. Minimal residual disease in multiple myeloma: current status. Biomark. Res. 9 https://doi.org/10.1186/s40364-021-00328-2 (2021).
Charalampous, C. & Kourelis, T. Minimal residual disease assessment in multiple myeloma patients: minimal disease with maximal implications. Front. Oncol. 11, 801851. https://doi.org/10.3389/fonc.2021.801851 (2021).
Munshi, N. C. et al. Association of minimal residual disease with superior survival outcomes in patients with multiple myeloma: a meta-analysis. JAMA Oncol. 3, 28–35. https://doi.org/10.1001/jamaoncol.2016.3160 (2017).
Popat, R. et al. Using depth of response to stratify patients to front line autologous stem cell transplant: results of the phase II PADIMAC myeloma trial. Br. J. Haematol. 193, e19–e22. https://doi.org/10.1111/bjh.17391 (2021).
Lahuerta, J. J. et al. Depth of response in multiple myeloma: a pooled analysis of three PETHEMA/GEM clinical trials. J. Clin. Oncol. 35, 2900–2910. https://doi.org/10.1200/JCO.2016.69.2517 (2017).
Sun, Q. et al. Prognostic significance of the stage at which an MRD-Negative status is achieved for patients with multiple myeloma who received ASCT. Front. Oncol. 12, 776920. https://doi.org/10.3389/fonc.2022.776920 (2022).
Voorhees, P. M. et al. Daratumumab, lenalidomide, bortezomib, and dexamethasone for transplant-eligible newly diagnosed multiple myeloma: the GRIFFIN trial. Blood 136, 936–945. https://doi.org/10.1182/blood.2020005288 (2020).
Rocchi, S., Zannetti, B. A., Marconi, G. & Lanza, F. Multiple myeloma: the role of autologous stem cell transplantation in the era of immunotherapy. Cells 13 https://doi.org/10.3390/cells13100853 (2024).
Paiva, B. et al. Measurable residual disease by next-generation flow cytometry in multiple myeloma. J. Clin. Oncol. 38, 784–792. https://doi.org/10.1200/JCO.19.01231 (2020).
de Tute, R. M. et al. Minimal residual disease after autologous stem-cell transplant for patients with myeloma: prognostic significance and the impact of Lenalidomide maintenance and molecular risk. J. Clin. Oncol. 40, 2889–2900. https://doi.org/10.1200/jco.21.02228 (2022).
Perrot, A. et al. Minimal residual disease negativity using deep sequencing is a major prognostic factor in multiple myeloma. Blood 132, 2456–2464. https://doi.org/10.1182/blood-2018-06-858613 (2018).
Goicoechea, I. et al. Deep MRD profiling defines outcome and unveils different modes of treatment resistance in standard- and high-risk myeloma. Blood 137, 49–60. https://doi.org/10.1182/blood.2020006731 (2021).
Ozga, M. et al. Concomitant 1q + and t(4;14) influences disease characteristics, immune system, and prognosis in double-hit multiple myeloma. Blood Cancer J. 13, 167. https://doi.org/10.1038/s41408-023-00943-2 (2023).
Costa, L. J. et al. Carfilzomib, Lenalidomide, and dexamethasone with minimal residual disease response-adapted therapy in newly diagnosed multiple myeloma. J. Clin. Oncol. 40, 2901–2912. https://doi.org/10.1200/JCO.21.01935 (2022). Daratumumab.
Ramasamy, K. et al. Measurable residual disease testing in multiple myeloma routine clinical practice: a modified Delphi study. Hemasphere 7, e942. https://doi.org/10.1097/HS9.0000000000000942 (2023).
Pasvolsky, O. et al. Outcomes of autologous stem cell transplantation in patients with ultra-high-risk multiple myeloma. Transpl. Cell. Ther. 29, 757–762. https://doi.org/10.1016/j.jtct.2023.08.031 (2023).
Nishimura, K. K. et al. Long-term outcomes after autologous stem cell transplantation for multiple myeloma. Blood Adv. 4, 422–431. https://doi.org/10.1182/bloodadvances.2019000524 (2020).
Acknowledgements
We gratefully acknowledge Dr Yongke Cao for his expert assistance in improving the clarity and quality of the English language in this manuscript.
Funding
This study was funded by the Science and Technology Project in Lianyungang City (No. SF2313) and the Science and Technology Development Fund of Xuzhou Medical University Affiliated Hospital (No. XYFM202328).
Author information
Authors and Affiliations
Contributions
JP M, YW and LD Z contributed to the study conceptualization. JP M managed the data collection, analyzed the data and wrote the main manuscript text. LG X, H Z, YX Z, T J, ZM C, and LN Z participated in the patient data collection. HQ W provided the laboratory test data. Y W, LD Z provided the consultancy, corrections, and comments. Y W and J W reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Ethics Committee of the First People’s Hospital of Lianyungang (No. KY-20240110001-02), and informed consent was obtained prior to the experiment.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mao, J., Xue, L., Wang, H. et al. Cytogenetic risk stratification combined with minimal residual disease status influences the therapeutic outcome and prognosis of multiple myelomas. Sci Rep 15, 12545 (2025). https://doi.org/10.1038/s41598-025-97125-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97125-w
Keywords
This article is cited by
-
Genomic Alterations in Multiple Myeloma: A Comprehensive Landscape
Indian Journal of Hematology and Blood Transfusion (2025)