Abstract
Background
The interrelationships between atrial fibrillation (AF), brain lesions and cognitive function are poorly understood. We aimed to investigate the relationship of AF with brain lesions and cognition.
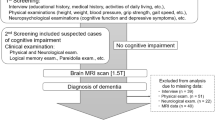
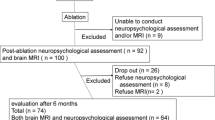
Methods
We enrolled 1,480 patients with and 959 without AF in a multicenter prospective study (Swiss-AF; NCT02105844). We assessed brain structure, and cognition using the Montreal Cognitive Assessment (MoCA). Brain magnetic resonance imaging (MRI) was performed to assess large non-cortical and cortical infarcts (LNCCI), small non-cortical infarcts (SNCI), white matter hyperintensities (WMH), and microbleeds. Using causal mediation analyses, we investigated the direct (lesion-independent) and indirect (lesion-mediated) effects of AF on cognition.
Results
Mean age in AF patients is 75.0 vs. 74.2 years in no-AF patients, 28.6% vs. 36.9% are female, and comorbidities are comparable. The prevalence of MRI-detected brain infarcts (LNCCI and/or SNCI) is 40.1% in AF patients vs. 24.0% in no-AF patients, adjusted OR (95% CI): 1.78 (1.30; 2.44), p = 0.0003. WMH (Fazekas ≥2) are more prevalent in AF patients (59.2% vs 44.4%), adjusted OR (95% CI): 2.03 (1.50; 2.77), p = 4.6e-06. The mean MoCA score is 25.3 in AF patients and 26.4 in no-AF patients. In mediation analysis, the total effect of AF on cognition is −1.05 MoCA points, decomposed into a direct effect of −0.99 and an indirect, lesion-mediated, effect of −0.06 points.
Conclusions
The prevalence of ischemic brain infarcts and WMH is higher in patients with AF than without AF despite comparable comorbidities. AF is associated with lower cognitive function, primarily through a direct effect rather than mediated by brain lesions.

Plain Language Summary
Atrial fibrillation is a common heart rhythm disorder in which there is an irregular heartbeat. It has been associated with damage to the brain and reduced cognitive function, which is the mental processes involved in thinking, learning, and processing information. However, the relationship is poorly understood. We assessed brain structure and cognitive function in people with similar characteristics that either had or did not have atrial fibrillation. We found that people with atrial fibrillation had more brain damage visible by brain imaging and lower cognitive function, compared to people without atrial fibrillation. The brain damage seen did not seem to be the main cause of the lower cognitive function. The main driver of lower cognitive function was most probably the arrhythmia itself.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. To protect participant privacy, this information is not publicly available. Supplementary Data 1 contains the source data for Fig. 3.
References
Lloyd-Jones, D. M. et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation 110, 1042–1046 (2004).
Krijthe, B. P. et al. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur. Heart J. 34, 2746–2751 (2013).
Prince, M. et al. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimers Dement 9, 63–75 (2013).
Kalantarian, S., Stern, T. A., Mansour, M. & Ruskin, J. N. Cognitive impairment associated with atrial fibrillation: a meta-analysis. Ann. Intern. Med. 158, 338–346 (2013).
Conen, D. et al. Relationships of Overt and Silent Brain Lesions With Cognitive Function in Patients With Atrial Fibrillation. J. Am. Coll. Cardiol. 73, 989–999 (2019).
Kühne, M. et al. Silent brain infarcts impact on cognitive function in atrial fibrillation. Eur. Heart J. 43, 2127–2135 (2022).
Benjamin, E. J. et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 271, 840–844 (1994).
Conen, D. et al. Influence of systolic and diastolic blood pressure on the risk of incident atrial fibrillation in women. Circulation 119, 2146–2152 (2009).
Alonso, A. et al. Blood lipids and the incidence of atrial fibrillation: the Multi-Ethnic Study of Atherosclerosis and the Framingham Heart Study. J. Am. Heart Assoc. 3, e001211 (2014).
Adelborg, K. et al. Heart failure and risk of dementia: a Danish nationwide population-based cohort study. Eur. J. Heart Fail. 19, 253–260 (2017).
Lourida, I. et al. Association of Lifestyle and Genetic Risk With Incidence of Dementia. JAMA 322, 430–437 (2019).
SPRINT MIND Investigators for the SPRINT Research Group et al. Association of Intensive vs Standard Blood Pressure Control With Cerebral White Matter Lesions. JAMA 322, 524–534 (2019).
Conen, D. et al. Design of the Swiss Atrial Fibrillation Cohort Study (Swiss-AF): structural brain damage and cognitive decline among patients with atrial fibrillation. Swiss Med. Wkly. 147, w14467 (2017).
Kirchhof, P. et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 37, 2893–2962 (2016).
Wardlaw, J. M. et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12, 822–838 (2013).
Duering, M. et al. Neuroimaging standards for research into small vessel disease-advances since 2013. Lancet Neurol 22, 602–618 (2023).
Nasreddine, Z. S. et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699 (2005).
Lange, T., Vansteelandt, S. & Bekaert, M. A simple unified approach for estimating natural direct and indirect effects. Am. J. Epidemiol. 176, 190–195 (2012).
Brambatti, M. et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circulation 129, 2094–2099 (2014).
Mitchell, L. B. et al. Prediction of stroke or TIA in patients without atrial fibrillation using CHADS2 and CHA2DS2-VASc scores. Heart Br. Card. Soc. 100, 1524–1530 (2014).
Melgaard, L. et al. Assessment of the CHA2DS2-VASc Score in Predicting Ischemic Stroke, Thromboembolism, and Death in Patients With Heart Failure With and Without Atrial Fibrillation. JAMA 314, 1030–1038 (2015).
Koene, R. J. et al. Relation of the CHA2DS2-VASc Score to Risk of Thrombotic and Embolic Stroke in Community-Dwelling Individuals Without Atrial Fibrillation (From The Atherosclerosis Risk in Communities [ARIC] Study). Am. J. Cardiol. 123, 402–408 (2019).
Mahajan, R. et al. Subclinical device-detected atrial fibrillation and stroke risk: a systematic review and meta-analysis. Eur Heart J 39, 1407–1415 (2018).
Svendsen, J. H. et al. Implantable loop recorder detection of atrial fibrillation to prevent stroke (The LOOP Study): a randomised controlled trial. The Lancet 398, 1507–1516 (2021).
Singer, D. E., Ziegler, P. D., Koehler, J. L., Sarkar, S. & Passman, R. S. Temporal Association Between Episodes of Atrial Fibrillation and Risk of Ischemic Stroke. JAMA Cardiol 6, 1364–1369 (2021).
Banerjee, G. et al. Cognitive Impairment Before Atrial Fibrillation–Related Ischemic Events: Neuroimaging and Prognostic Associations. J. Am. Heart Assoc. 9, e014537 (2020).
Gardarsdottir, M. et al. Atrial fibrillation is associated with decreased total cerebral blood flow and brain perfusion. Europace 20, 1252–1258 (2018).
Krisai, P. et al. Biomarker and cognitive decline in atrial fibrillation: a prospective cohort study. Sci. Rep. 15, 12921 (2025).
Guo, J. et al. Atrial fibrillation catheter ablation, brain glymphatic function, and cognitive performance. Eur. Heart J. ehaf036 (2025) https://doi.org/10.1093/eurheartj/ehaf036.
von Eisenhart Rothe, A. F. et al. Depression in paroxysmal and persistent atrial fibrillation patients: a cross-sectional comparison of patients enroled in two large clinical trials. Eur. Eur. Pacing Arrhythm. Card. Electrophysiol. J. Work. Groups Card. Pacing Arrhythm. Card. Cell. Electrophysiol. Eur. Soc. Cardiol. 16, 812–819 (2014).
Al-Kaisey, A. M. et al. Atrial Fibrillation Catheter Ablation vs Medical Therapy and Psychological Distress: A Randomized Clinical Trial. JAMA 330, 925–933 (2023).
Kirchhof, P. et al. Early Rhythm-Control Therapy in Patients with Atrial Fibrillation. N. Engl. J. Med. (2020) https://doi.org/10.1056/NEJMoa2019422.
Acknowledgements
The Swiss-AF study is supported by grants of the Swiss National Science Foundation (grant numbers 33CS30_148474, 33CS30_177520, 32473B_176178, 32003B_197524, and 324730_192394), the Swiss Heart Foundation (FF22036), the Foundation for Cardiovascular Research Basel (FCVR), and the University of Basel.
Author information
Authors and Affiliations
Consortia
Contributions
PK Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft. SA Methodology, Formal analysis, Writing – original draft. MC Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft. NR Methodology, Formal analysis, Data acquisition, Writing – original draft. TR Investigation, Data acquisition, Writing – review & editing. ASM Investigation, Data acquisition, Writing – review & editing. JHB Investigation, Data acquisition, Writing – review & editing. PA Investigation, Data acquisition, Writing – review & editing. AA Investigation, Data acquisition, Writing – review & editing. GM Investigation, Data acquisition, Writing – review & editing. RK Investigation, Data acquisition, Writing – review & editing. DS Investigation, Data acquisition, Writing – review & editing. MDV Investigation, Data acquisition, Writing – review & editing. GC Investigation, Data acquisition, Writing – review & editing. G.E. Investigation, Data acquisition, Writing – review & editing. E.H. Investigation, Data acquisition, Writing – review & editing. A.M. Investigation, Data acquisition, Writing – review & editing. R.E.P. Methodology, Data curation, Formal analysis, Writing – original draft. N.R. Investigation, Data acquisition, Writing – review & editing. L.R. Investigation, Data acquisition, Writing – review & editing. M.S. Methodology, Data curation, Formal analysis, Writing – review & editing. C.S. Investigation, Writing – review & editing. P.B. Investigation, Writing – review & editing. C.S.Z. Investigation, Data curation, Writing – review & editing. T.S. Investigation, Data curation, Writing – review & editing. M.D. Investigation, Writing – review & editing. F.M. Investigation, Writing – review & editing. L.H.B. Investigation, Data curation, Writing – review & editing. D.C. Investigation, Funding acquisition, Formal analysis, Writing – review & editing. S.O. Conceptualization, Methodology, Supervision, Project administration, Funding acquisition, Writing – original draft. M.K. Conceptualization, Methodology, Supervision, Project administration, Funding acquisition, Writing – original draft.
Corresponding author
Ethics declarations
Competing interests
Philipp Krisai (PK) reports speaker fees from BMS/Pfizer and Biosense Webster, and research grants from the Swiss National Science Foundation, Swiss Heart Foundation, Foundation for Cardiovascular Research Basel, Machaon Foundation. Michael Kühne (MK) reports grants from Bayer, grants from BMS, grants from Boston Scientific, grants from Daiichi Sankyo, grants from Pfizer, personal fees from Abbott, personal fees from Boston Scientific, personal fees from Daiichi Sankyo, and royalties from Springer (ECG book). Stefan Osswald (SO) reports grants from Swiss National Science Foundation, Swiss Heart Foundation, Foundation for Cardiovascular Research Basel. Felix Mahfoud (FM) has been supported by Deutsche Gesellschaft für Kardiologie (DGK), Deutsche Forschungsgemeinschaft (SFB TRR219, Project-ID 322900939), and Deutsche Herzstiftung. In the past 24 months, Saarland University has received scientific support from Ablative Solutions, Medtronic and ReCor Medical. Until May 2024, FM has received speaker honoraria/consulting fees from Ablative Solutions, Amgen, Astra-Zeneca, Bayer, Boehringer Ingelheim, Inari, Medtronic, Merck, ReCor Medical, Servier, and Terumo. Matthias Schwenkglenks (MS) reports grants from Swiss National Science Foundation, for the conduct of the study; grants from Amgen, grants from MSD, grants from Novartis, grants from Pfizer, grants from Roche, grants and personal fees from BMS and personal fees from Sandoz, all outside the submitted work. David Conen (DC) reports speaker fees from Servier, consulting fees from Trimedics. Giorgio Moschovitis (GM) has received advisory board or speaker’s fees from Astra Zeneca, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Gebro Pharma, Novartis and Vifor, all outside of the submitted work. All other authors declare no competing interest.
Peer review
Peer review information
Communications Medicine thanks Rajiv Mahajan, Rakesh Agarwal and Zuolin Lu for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Krisai, P., Aeschbacher, S., Coslovsky, M. et al. Ischemic brain infarcts, white matter hyperintensities, and cognitive impairment are increased in patients with Atrial Fibrillation. Commun Med (2026). https://doi.org/10.1038/s43856-026-01389-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-026-01389-w