Abstract
Consumer-grade wearables provide an opportunity to understand public health trends, develop risk stratification tools and monitor interventions. This review introduces the most common wearable sensors and describes the health parameters that can be measured using them. We highlight research into the validity and accuracy of these measurements and practical considerations for the use of wearable data. Finally, we provide future perspectives on wearables in cardiovascular clinical practice and population health research.
Similar content being viewed by others
Introduction
Use of consumer-grade wearables has grown considerably in recent years1. These devices, most commonly in the form of smartwatches, wrist-bands or rings, enable users to access personalised healthcare data and physical activity parameters remotely, continuously and in real-time. In the context of healthcare and population research, wearable technology provides an opportunity to harness data at scale, understand public health trends, develop risk stratification tools and monitor interventions.
Some features of consumer-grade wearables have regulatory board (e.g. United States Food and Drug Administration; US FDA) approval, however, the majority of biometric parameters are derived from sensor signals such as photoplethysmography (PPG) and tri-axial accelerometery and proprietary algorithms which are not available for public scrutiny. Wearable device software and hardware are regularly improved in the form of software updates and new models with an increasing number of features on offer. The proprietary nature and iterative approach in this market makes product comparison and clinical utility difficult to quantify and track in real-time. Furthermore, these devices are engineered and marketed predominantly for individual use and therefore consideration for the practicalities surrounding data acquisition at scale and analysis pipelines is required.
This review aims to provide a non-expert guide to practitioners in clinical care and population health who are considering the use of consumer-grade wearables in cardiovascular healthcare or research settings, with a focus on the following: 1) a general introduction to wearable sensors; 2) the health parameters that can be measured using these sensors; 3) the validity and accuracy of these measurements; 4) practical considerations for the acquisition and use of wearable data at scale and 5) clinical cardiovascular and population health future perspectives.
What sensors are used in wearables?
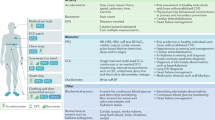
While a growing number of sensors can potentially be embedded into wearables, most of the physiological data in consumer-grade smartwatches and rings is captured by accelerometery, photoplethysmography (PPG) and electrocardiography (ECG) sensors (Fig. 1).
Photoplethysmography (PPG)
PPG is a non-invasive optical technique that uses an infrared light source and a detector at the surface of the skin to measure small variations in blood volume. The intensity of the light transmitted through, or reflected from, skin capillaries is proportional to the blood volume and its light absorption2. In reflectance PPG, the methodology commonly built into wearables, light is shone from a light emitting diode (LED) on to the skin, and the amount of light reflected back is measured using a photodetector positioned close to the emitting LED3. Wearable technology utilises the PPG signal, whose shape is analogous to an arterial pulse wave but its unitless (Fig. 1), to estimate heart rate (HR) and HR variability (HRV)4. Other physiological parameters derived from the PPG include respiratory rate5, peripheral oxygen saturation6 and, more recently, blood pressure (BP)7,8.
Accelerometery
Accelerometers are sensors that detect and measure acceleration forces (the rate of change in velocity). Tri-axial accelerometers can detect changes in movement and orientation in three planes (x; medial-lateral, y; cranial-caudal and Z; anterior-posterior axes) and are widely incorporated into wearables to estimate body position, and several measures of physical activity9.
Electrocardiography (ECG)
The ECG is the gold-standard non-invasive measure of the rhythm of the heart. A standard 12-lead ECG provides a visual representation of the propagation of the electrical impulse through the heart during each cardiac cycle. The variations in the amplitude of the ECG signal over time provide information relating to both HR (e.g., fast or slow) and rhythm (e.g., normal or abnormal). Traditionally, for clinical purposes this method of cardiac monitoring is performed for 10-seconds at rest or can be performed for 24-hours to several days using portable continuous Holter monitors. With advancements in wearable technology, the recording of short ( ~ 30-second) single-lead ECG recordings is now feasible in the most recent devices. These measurements tend to be taken between opposite arms via two electrodes in close proximity to one another, often a positive electrode on the back of a wrist-worn wearable and a negative electrode positioned on the digital screen, to create a bipolar ECG signal similar to lead I of the traditional 12-lead ECG10,11.
Additional Sensors
Wearables are now commonly equipped with many more sensors such as barometers (elevation/altitude), magnetometers (magnetic fields), global positioning systems (GPS; geolocation) and thermometers (temperature), to provide more comprehensive functionality.
Electrodermal activity (EDA)
Electrodermal activity (EDA) sensors, also known as galvanic skin response sensors use electrodes on the skin to measure subtle variations in electrical conductance. These changes occur as a result of sweat gland activity and are commonly associated with changes in emotional state. In the context of wearables, EDA sensors are often used to infer periods of perceived stress12,13.
Bioelectrical Impedance (BioZ)
Body composition (fat mass, fat free mass, body water content and body fat percentage) can be estimated through the use of bioelectrical impedance analysis (BioZ). BioZ measures the body’s resistance to a low-level electrical current. Traditionally, the integration of this metric with wearable-derived data has been achieved through the use of manufacturer specific compatible bioimpedance scales which can be synchronised to an individual’s wearable health dashboard14. More recently, this technology has been integrated into a consumer-grade smartwatch, enabling individuals to estimate body composition by taking a measurement at rest14. This is done by placing two fingers from the opposite hand to the watch on designated smartwatch button sensors to administer the microcurrent required for BioZ assessment15. Due to its association with tissue hydration status, BioZ has also been used in conjunction with the ECG sensor to predict heart failure decompensation16,17 and has been used as part of predictive algorithms in implantable devices18.
Gyroscopes
Gyroscopes are sensors that measure angular velocity (gyration) and can detect very small angular displacements caused by cardiac activity19. Gyroscopes are often used in combination with accelerometers in a technique called Gyrocardiography to record cardiac vibration signals in the chest. This technique has been developed to provide insights into the mechanical aspects of the cardiac cycle and detect cardiovascular diseases such as atrial fibrillation (AF) and heart failure using smartphone applications20.
What health parameters can be derived from these sensors and how accurate are they?
Table 1 provides details about commonly used smartwatch, wrist-band and ring (Apple, Fitbit, Garmin, Oura, Polar, Samsung, Withings and Whoop) devices and their biometric features. Table 2 highlights systematic reviews and meta-analyses that have been performed in each of the biometric parameters described in this section along with the wearable manufacturers that were reviewed in each. This table is detailed but not exhaustive.
A living umbrella review of systematic reviews evaluating the accuracy of consumer-grade technologies in health measurement can be found elsewhere21.
Resting heart rate (HR) and HR tracking
HR is modulated by the autonomic nervous system (ANS) and can be modified by several physiological and environmental factors. HR changes in response to many physiological and medical stimuli, such as exercise, anxiety, pregnancy, physical fitness, and cardiovascular and non-cardiovascular diseases. A chronically elevated resting HR is a strong independent risk factor for all-cause mortality and for adverse outcomes in individuals with cardiovascular disease22,23.
The accuracy of PPG estimation of HR has been widely documented with validation performed against reference ECG measurements. At rest, wearables are widely considered to measure HR accurately, with mean absolute errors (AE) in the region of 2 beats per minute (bpm), mean absolute percentage errors (MAPE) reported as less than 10% and correlations between the devices and reference methods consistently reported as moderate to excellent24,25,26,27,28,29,30,31,32.
A systematic review of the reliability and validity of commercially available wearables (Fitbit, Apple Watch, Samsung and Garmin) was performed for the measurement of HR (Table 2)33. A total of 29 studies examined wearable device HR measurements compared with reference measures including ECG, Polar chest straps and pulse oximetry. Of the 177 comparisons, 100 (56.5%) were within ±3% measurement error, 44 (24.9%) were below -3% measurement error and 33 (18.6%) were above 3% measurement error, with a slight tendency to underestimate HR33.
However, the accuracy of HR measurement in wearables is known to decline during physical activity. In addition to activity intensity, the activity type and specifically arm movement during the activity have been shown to influence the accuracy of HR measurements34,35,36. We recently observed excellent accuracy in measuring HR at rest, and during recovery (MAPE ≤3%), in both Garmin and Fitbit devices, but accuracy worsened during peak exercise37. MAPE was similar to rest and recovery during peak exercise, however, the limits of agreement widened due to an increase in the number of outliers ( ~ 7% for Garmin and ~ 12% for Fitbit)37. Contact pressure and sweat have also been shown to impact accuracy38.
Heart rate variability (HRV) and pulse rate variability (PRV)
HRV is a measure of the variation in the time interval between each successive heartbeat, specifically the variation in the duration of consecutive R-R intervals on an ECG. HRV is considered a non-invasive ANS marker representing the balance between the sympathetic and parasympathetic branches39. Low HRV is associated with cardiovascular disease, diabetes mellitus, hypertension, arrhythmia and all-cause mortality40 and conversely, optimal HRV is associated with health and resilience41. There are several HRV parameters that can be measured from an ECG which are grouped primarily into time domain and frequency domain markers42, but more complex markers have been proposed43. Time-domain measurements quantify HRV over a period of time (e.g., 2 min to 24 h) and include the root mean square of successive differences (RMSSD) and the standard deviation of normal-to-normal intervals (SDNN). In contrast, frequency domain metrics measure the signal in various bands of frequency and include high frequency power and low frequency power.
In the context of wearables, ‘HRV’ measurements may be obtained using an ECG sensor, PPG sensor or both. When measured using PPG, the most appropriate metric to use would be pulse rate variability44,45, which is derived from consecutive pulses recorded in the wrist or finger and not from consecutive R-R intervals on an ECG. Despite presenting some differences related to the pulse arrival time, i.e., the interval between the R-wave in the ECG and the onset of the PPG pulse, HRV from ECG and PPG have been shown to be similar, even in dynamic conditions45. Smartwatches measure the ECG for a short period of time, typically 30 s, from which only measures of ultra-short HRV can be derived22,46.
Pulse rate variability has been shown to correlate with HRV during rest and during autonomic challenges45. According to a recent review, mainly focusing on measurements derived at rest, the correlation between ECG and wearable derived HRV ranged from very good to excellent at rest and declined progressively as exercise intensity increased (Table 2)47.
In a recent validation study of PPG derived HRV (RMSSD and SDNN) using Garmin’s health snapshot, we observed a strong correlation (between 0.82 and 0.89) between Garmin and reference ECG HRV32.
Arrhythmia and AF detection
An arrhythmia refers to an abnormality of the heart’s rhythm in which the heart may beat too slowly, too quickly or irregularly. AF is the most common serious arrhythmia, and refers to an irregular heart rhythm in which uncoordinated electrical activation in the top chambers of the heart (the atria) can impair cardiac efficiency. Although many people with AF are not aware of it, AF can also cause disabling symptoms of an awareness of an unusual heartbeat, breathlessness, dizziness and fatigue. AF affects approximately 59 million individuals worldwide and is associated with an increased risk of blood clots and stroke48. Early detection of AF allows for the prompt implementation of patient management and treatment such as medication, or interventions (such as ablation or cardioversion) as well as risk reduction for the development of AF complications such as stroke and heart failure. Wearables can detect AF through both ECG and PPG sensors49,50,51. Currently, other arrhythmias (e.g., atrial or ventricular tachycardia) or premature contractions (called ectopic beats) are not usually detected by consumer-grade smartwatches or rings, despite this may potentially contribute to improving risk assessment52.
Wrist-worn devices have been shown to have excellent diagnostic accuracy in AF diagnosis based on a systematic review and meta-analysis of 28 studies (n = 13,463, area under the ROC curve of 0.97 (95% CI: 0.94,0.99); Table 2)53.
The BASEL wearable study reported that the sensitivity and specificity for AF detection were 85% and 75% for the Apple Watch 6, 85% and 75% for the Samsung Galaxy Watch 3, 58% and 75% for the Withings Scanwatch and 66% and 79% for the Fitbit Sense, respectively54. The author’s reported that in a clinical setting, manual review of tracings is required in about one-fourth of cases.
Wearable models from Apple, Fitbit, Samsung and Withings have been cleared by the US FDA for pre-diagnostic AF detection that are not intended for clinical decision-making.
Cardiac intervals
Cardiac intervals such as the QT interval, which measures the duration of ventricular repolarisation, or the PR interval, which measures the duration of atrial activation, carry important diagnostic and prognostic value (Fig. 1). Recent studies have shown that cardiac intervals derived from smartwatch ECGs show moderate to strong correlation with standard medical-grade ECGs55,56,57, however, these are not currently measured by consumer-grade wearables.
It was noted in a 2023 review that only two commercially available devices (Apple Watch and Withings ScanWatch) had been adequately compared to 12-lead ECG measurements with respect to QTc measurements56. In 177 patients (56%), the Withings ScanWatch automated algorithm was able to automatically measure QTc with a mean difference of 6.6 ms [Limits of Agreement; LoA: −59, 72 ms] compared to manual measurements. The authors concluded that the Withings ScanWatch tends to underestimate the QTc interval in line with others56,58.
In another study, adequate QT measurements were observed in 85% of patients when the smartwatch was worn in the standard wrist position55.
Respiratory rate
Respiratory rate refers to the number of breaths taken per minute, and like HR is affected by a wide range of physiological and medical conditions59,60. Respiratory rate can be estimated by wearables through the analysis of subtle changes in the ECG or PPG signal that occur due to respiratory modulation; including baseline wander of the signal, changes in the amplitude of the signal and the frequency of the signal5,61.
The accuracy of the respiratory rate estimation during sleep using the Samsung Galaxy Watch compared to polysomnography has been investigated in 195 individuals with varying degrees of obstructive sleep apnoea (OSA)62. OSA is a sleep disorder characterised by periods of partial or complete closure of the airway resulting in reduced and irregular respiratory rate during sleep. The root mean squared error (RMSE) of the average overnight and continuous respiratory rate measurements were 1.13 bpm and 1.62 bpm, respectively, showing a small bias of 0.39 bpm and 0.37 bpm, respectively62. In participants with normal-to-moderate OSA, average overnight and continuous respiratory rate measurements were at least 90% accurate62. For patients with severe OSA, accuracy decreased to 79.5% and 75.8%, respectively62. Recently, Samsung and Apple watches offer the possibility to detect increased risk for OSA, however little validation data is currently available.
Pulse oximetry (SpO2)
Oxygen saturation is a measure of the amount of haemoglobin that is bound to oxygen compared to how much haemoglobin remains unbound in the blood. SpO2 refers to the saturation of peripheral oxygen reported as the percentage of oxygen in the blood. SpO2 values can be observed in individuals with heart and lung conditions, OSA and at high altitude63. Previously mostly used only in high-intensity hospital settings, COVID-19 led to much wider use of oximetry in the community, including monitors bought directly by citizens and patients. SpO2 can be measured using reflectance PPG in wearables4. For the majority of individuals, a normal SpO2 is between 95% and 99%.
In a 2023 review, five publications (n = 973) using Apple Watch Series 6 to measure SpO2 were evaluated (Table 2)64. When compared to medical-grade pulse oximeters, the 95% limits of agreement were reported to be −2.7% to 5.9% SpO2, however, outliers of up to 15% were reported. Whether wearables are suited for remote monitoring in patients with established conditions that affect their oxygen saturation is yet to be addressed and further validation in both patients and healthy controls is necessary before smartwatches are recommended for clinical use65. In a recent study using Garmin’s health snapshot, we observed frequent underestimation of SpO232.
Step count and distance travelled
Step count is a measure of physical activity which can objectively be measured by counting the number of steps an individual takes in a given period of time. The number of steps taken per day have strong associations with risk of chronic disease and mental health66 and are inversely related to obesity, OSA, gastroesophageal reflux disease and major depressive disorder67. The length of a walking step correlates to an individual’s height68, however, can be impacted by age, fitness level and health status.
Step count using wearables is derived as a composite of walking motion detected by the accelerometer and stride length (determined by pre-programmed height) and has been used as an outcome in clinical trials69. Distance travelled is commonly calculated from step count or measured through the activation of the GPS during outdoor activities and is the primary outcome of established sub-maximal tests of exercise capacity such as the 6 min walk test70.
32 studies of Garmin smartwatches were assessed for step count validity in a 2019 review71. 16 studies were found to have good (0.75–0.89) to excellent ( ≥ 0.90) correlation coefficients with acceptable APE ( < 5% in laboratory or controlled conditions and <10% in free-living conditions)71. Distance validity, which was tested in three studies, had lower correlation coefficients of <0.60 with acceptable APE and both over and underestimation was reported71.
In the context of established sub-maximal tests of exercise capacity, we recently observed that distance measured by Garmin and Fitbit through the activation of GPS was accurate, with as little as 6–8% error during a 6 min walk test if participants walked around a park37. However, error increased to 18–20% when a standard 30 m lap protocol was used. Step count was a more accurate measure of distance compared to GPS distance (MAPE: 0.9% [0.4, 2.2%] and 6.8% [3.2, 12.9%] for Garmin and Fitbit, respectively)37.
A 2020 systematic review of wearables (Fitbit, Apple Watch, Samsung and Garmin) also evaluated the reliability and validity of the measurement of step count33. From 158 studies, 805 comparisons between wearable derived step count and reference measures (manual counting or accelerometery) were made. Of these, 364 (45.2%) were within ±3% measurement error, 344 (42.7%) were below −3% measurement error and 97 (12.1%) were above 3% measurement error with an overall tendency to underestimate step count33.
Physical Activity Recognition
Physical activity recognition can refer to the classification process of physiological motion measurements that may occur in a laboratory or free-living conditions72. Wearables often include a feature whereby the type and duration of a physical activity is automatically recognised and recorded without input from the user.
In 2019, a validation study assessed the automatic identification of physical activity type and duration using three Fitbit models (Flex 2, Alta HR and Charge 2) and one Garmin model (Vivosmart HR)73. The activities were a treadmill walk, treadmill run, embedded run, outdoor walk, outdoor run, elliptical, bike and swim, each for a duration of 15 min. The proportion of trials in which the activity type was correctly identified was 93% to 97% for treadmill walking, 93% to 100% for treadmill running, 36% to 62% for treadmill running when preceded and followed by a walk, 97% to 100% for outdoor walking, 100% for outdoor running, 3% to 97% for using an elliptical, 44% to 97% for biking, and 87.5% for swimming73.
Cardiorespiratory Fitness (CRF) and VO2max Estimation
During exercise, an integrated and coordinated response from the heart, lungs, cardiovascular system and skeletal muscles is required to meet the metabolic demands of contracting muscles74. Maximal oxygen consumption (VO2max) is dependent on the ability of the oxygen transport system to deliver blood and the ability of cells to take up and utilise oxygen in energy production75. While maximal cardiopulmonary exercise testing (CPET) is the gold standard for assessing VO2max76, it requires clinical staff, space, expensive equipment and time and is rarely performed even in medical assessments.
CRF has been linked to several health-related outcomes, with low fitness being associated with increased risk of cardiovascular disease77,78, metabolic syndrome79, cognitive function80 and severe COVID-1981. Concurrently, increased levels of CRF are widely promoted as cardioprotective measures in the primary and secondary prevention of cardiovascular and coronary heart disease82,83 and a useful marker of training effectiveness in athletic individuals.
Smartwatch estimates of CRF can be estimated using anthropometric parameters (age, sex, height and weight), PPG-measured HR and HRV at rest, the relationship between changes in PPG-measured HR and HRV in relation to estimated workload during physical activity, exercise type or a combination of these factors using proprietary algorithms84,85.
A systematic review with meta-analysis of 14 studies that assessed the validity of smartwatch estimation of VO2max using either resting measurements (seated or supine resting HR) or exercise test-based measurements (outdoor running for at least 10 min) was performed in 2022 (Table 2)86. In the context of using resting measurements, an overestimation of VO2max was observed (mean difference [LoA]= 2.17 [−13.07, 17.41] ml/kg/min, p = 0.020) compared to the reference measurement. In contrast, a bias close to nil compared to the reference measurement (mean difference [LoA]= −0.09 [−16.79, 16.61] ml/kg/min, p = 0.910) was observed when outdoor running exercise measurements were used. However, the studies included in the meta-analysis were small (mean sample per study of 29) and based on young (pooled age 24.6 ± 5.7 years) healthy adults, who were active, recreational runners or soccer players86.
Absolute values and changes over time in VO2max as measured by Apple or Garmin wearables and CPET have been shown to correlate well (Pearson’s >0.80) in 48 adults with complex congenital heart disease87. However, in line with the findings of the Apple smartwatch validation study49 and prior work of ours utilising free-living activity88, despite observing moderate correlations, a large positive bias in smartwatch estimated VO2max has been observed, indicating that wearables often overestimate VO2max87.
Wearable estimates of CRF are currently limited to VO2max as an outcome parameter. In contrast, clinical CPET provides many other valuable metrics such as anaerobic threshold and oxygen uptake efficiency slope that contribute to a more comprehensive assessment of CRF and the utilisation of oxygen throughout exercise.
Energy expenditure
Energy expenditure is defined as the energy expended, above resting levels, during purposeful exercise89. Doubly labelled water, is considered the gold-standard indirect calorimetry assessment of free-living energy expenditure90, however, is associated with high costs and limited by the requirement for structured activities in laboratory settings91. Wearables estimate energy expenditure, often referred to as ‘Calories burned’ or similar, using anthropomorphic data such as body mass, PPG-measured HR, physical activity derived from accelerometery, GPS or both and exercise intensity using proprietary algorithms.
Two systematic reviews established that commercially available wearables estimated energy expenditure with insufficient validity33,92. Consistent with a separate review of Fitbit accuracy93, it was reported that wearables tend to underestimate energy expenditure compared to criterion laboratory measures (Oxycon Mobile, CosMed K4b2, or MetaMax 3B), however, at higher intensities of activity energy expenditure is overestimated92.
In 2020, it was also reported that no brand of wearable was within ±3% of measurement error more than 13% of the time33. Underestimation of energy expenditure was observed in Garmin wearables 69% of the time, and in Withings wearables 74% of the time, respectively. Apple wearables overestimated energy expenditure 58% of the time and Polar wearables overestimated energy expenditure 69% of the time, respectively. Despite showing reasonable median value for accuracy, Fitbit devices underestimated energy expenditure 48% of the time and overestimated energy expenditure 40% of the time33.
Blood Pressure (BP)
BP is the outward force by which blood pushes against the artery walls as it moves around the body. BP is described as the systolic over the diastolic BP (maximum over minimum) measured in millimetres of mercury (mmHg). Hypertension (elevated BP levels) affect more than 1 billion people globally and is the leading modifiable risk factor for preventable death94. The most commonly used method of BP assessment incorporates a cuff sphygmomanometer to assess brachial arterial BP level which can be incorporated into automatic oscillometric devices with a brachial cuff95.
Some wrist-worn devices (e.g., Omron HeartGuide) incorporate a cuff to measure BP at the wrist, but limited data on their accuracy is publicly available.
Cuffless wearables are emerging but often require user calibration prior to use8. BP measurements can then be derived from the time it takes for an arterial pulse wave to reach the periphery (pulse transit time) using ECG or pulse wave analysis using PPG in which the change in blood volume with each heart beat is assessed96. The amplitude of the PPG signal can provide information about the strength of the pulse, with consistently elevated amplitude in signal being an indication of hypertension7. The devices reviewed in Table 1 do not measure BP, but information about cuffless wearables for blood pressure monitoring can be found elsewhere95,97.
A systematic review and meta-analysis of 16 studies (n = 974) was performed in 202298. 81% of devices in the analyses used PPG to estimate BP against a reference device. The authors defined devices with a mean bias of <5 mmHg as valid as a consensus. Eight devices showed a mean bias of <5 mmHg for SBP and DBP compared with a reference device, three of which were commercially available (B-Pro, Somnotouch-NIBP and T2-Mart). Differences were not observed between the wearables and reference devices for SBP (pooled mean difference = 3.42 mmHg, 95% CI: −2.17, 9.01) and DBP (pooled mean difference = 1.16 mmHg, 95% CI: −1.26, 3.58), however, confidence intervals around the estimates was wide. Recent data have cast doubt about the accuracy of some these devices99,100 and cuffless-based technology101, and our own data have shown limited agreement between cuffless and cuff-based ambulatory BP monitoring102.
Sleep Duration and Stages
Sleep is an essential biological function with major roles in recovery, energy conservation and survival103. There is marked individual variation in the amount of sleep that an individual will need throughout the life span to ensure good health104. Objectively measured short and long sleep duration have been both associated with adverse health outcomes105,106,107.
The gold-standard assessment of sleep is laboratory-based polysomnography in which several parameters including brain waves, HR, respiratory rate, eye movement and muscle activity are monitored to classify sleep and wake cycles108. Wearables use a combination of PPG sensors and accelerometers to detect changes in HR and movement to calculate total sleep duration and classify sleep stages.
In 2023, a validation study was performed to assess the accuracy of 11 commercially available devices including five wearables (Google Pixel Watch, Galaxy Watch 5, Fitbit Sense 2, Apple Watch 8 and Oura Ring 3) compared to laboratory polysomnography in 75 participants109. Three wearables (Google Pixel Watch, Galaxy Watch 5 and Fitbit Sense 2) demonstrated moderate agreement with sleep stage classification (k = 0.4,0.6) and two wearables (Apple Watch 8 and Oura Ring 3) showed fair agreement (k = 0.2,0.4). The authors reported that wearables generally overestimate sleep by misclassifying periods of awake stillness as sleep. The Oura ring showed negligible proportional bias, potentially owing to its use of additional features beyond actigraphy such as body temperature and circadian rhythm for sleep staging110.
Fitbit devices were reported to be comparable to polysomnography in accuracy of detecting sleep phases, with 95% to 96% sensitivity and 58% to 69% specificity in detecting sleep epochs in a 2019 review111. A recent systematic review of eight studies investigated the accuracy of Fitbit, Garmin and Whoop in measuring sleep duration and sleep stages versus polysomnography108. Whoop was reported to have the least disagreement compared to polysomnography for total sleep time (−1.4 min), light sleep (−9.6 min) and deep sleep (−9.3 min) but the largest disagreement for rapid eye movement (REM) sleep (21.0 min). The Fitbit and Garmin devices both showed moderate accuracy in assessing sleep stages and total sleep time compared to polysomnography108.
Psychological stress
Stress can be defined as a state of worry or mental tension caused by a challenging situation in life or the environment. Stress activates the sympathetic nervous system resulting in an increase in HR and a decrease in HRV112. Conversely, during periods of relaxation and sleep, a decrease in HR and increase in HRV can be observed113. Chronic stress, the repeated occurrence of the stress response over a period of time, is associated with increased risk of cardiovascular disease and type 2 diabetes mellitus114,115. The integration of stress management features in wearables is based on HR and HRV analysis and in some, EDA sensors. HRV analysis in wearables may be accompanied by real-time prompts to perform breathing activities or relaxation techniques in periods of detected stress.
Smartwatches were found to more accurately detect periods of psychological stress when utilising HRV and other physiological parameters such as EDA, respiratory rate and temperature instead of HR alone116. However, concerns surrounding the reliability of EDA measurement due to motion artifact have been raised117. Similarly, the accuracy of stress detection has been noted to decline during periods of vigorous movement, also likely owing to motion artifact116.
Women’s Health
The monitoring of fertile windows and menstrual cycles have long been utilised for achieving planned pregnancy, preventing unplanned pregnancy, and the identification of irregular or abnormal cycles. Some wearables measure changes in HRV, body temperature and respiratory rate to detect and predict menstrual cycle stages including menstruation, the luteal phase and ovulation118,119.
A recent review of 13 studies found that most devices had high accuracy for detecting fertility and were able to differentiate between the luteal phase, fertile window and menstruation by changes in HR, HRV, temperature and respiratory rate (Table 2)120. In 2019, a study of the Oura ring reported a sensitivity for ovulation detection of 83.3% (−3 to +2 days) and menstruation detection of 71.9% to 86.5% (SD 2–4 days) using nocturnal finger skin temperature119. Compared to menstruation, a rise in HR (p = 0.001) and temperature (p < 0.001) during the luteal phases and lower HR (p = 0.02) and temperature (p = 0.05) during ovulation has been reported using the Oura ring more recently118.
Data acquisition and analysis pipelines
When selecting a wearable device for clinical or research purposes, data accessibility is a crucial consideration. Prior to wearable device selection, we would recommend reviewing device specifications to ensure that the measurement parameters of interest (Table 1) are available (at the sampling frequency required), accessible and exportable in a usable format.
Access to raw data varies by manufacturer and model. While some devices display several measurement parameters to users, export options may be limited. No manufacturer currently allows for the export of continuously recorded raw signals (i.e., PPG, 3D accelerometer, temperature etc.), except for the ECG, which can often be exported as a series of 30-second long recordings. Most of the data that can be exported for off-line analysis consist in aggregate time-series summarising the trend of a physiological parameter with a temporal resolution that typically goes from one second (e.g., HR) to 15 min (e.g., number of steps or respiratory rate for some brands) to 1 day (e.g., sleep duration). Of note, no smartwatch or smart ring currently allows for the export of beat-to-beat HR time-series. Instead, instantaneous HR is usually averaged using undetermined filters, resulting in relatively smooth trends. Physiological parameters from physical activities recorded by the user (e.g. running, walking, cardio etc.) may include ad-hoc information (e.g., distance, speed, altitude etc.) with sometimes a better temporal resolution (e.g., HR provided every second instead of every minute), or they may be only exportable as summary statistics (e.g., total number of steps and average HR). As an example, Supplementary Table 1 provides a comprehensive list of parameters that can be exported from a Garmin smartwatch (VivoActive 4), along with their temporal resolution and whether they are passively recorded or may need user’s input. Additionally, some manufacturers have introduced premium or subscription-based models that may restrict data access.
The format of exported raw data files is another important consideration. Many manufacturers, including Fitbit, Oura and Withings, use standard file formats such as CSV or TXT, which are relatively easy to process. However, others, including Garmin, use more complex formats such as .FIT files for some of their data export, which require more advanced data processing skills to access.
To support data retrieval and management, open source platforms such as RADAR-base121, offer infrastructure to facilitate data storage and processing, and third-party services are becoming available122,123.
Data security and privacy should be considered owing to the sensitive nature of the personalised health information that these devices collect, particularly when activating GPS tracking systems for location information. To mitigate data security and privacy risks, manufacturer privacy settings and security policies should be reviewed ahead of device selection.
Clinical Perspective for Cardiovascular Health
Cardiovascular diseases are the leading cause of death worldwide124. To reduce the enormous burden of cardiovascular diseases and disability125, progress is required in prevention, diagnosis, treatment and monitoring, and wearable data may play a useful role in all of these situations. The ability to collect data over months or years allows approaches that are not currently possible, however, may also present challenges in terms of the volume of data collected.
Evidence of the value of wearable data comes from the ability to detect abnormal heart rhythms, particularly AF, in people who would otherwise be unaware of this condition (and so at higher risk of stroke and other complications)49,126. Although questions remain about how to manage AF detected by such approaches, the ability to detect such a common and potentially devastating condition shows the potential for improved healthcare.
The addition of the ability to record a short ECG with sufficient accuracy to be approved as a medical device is now replacing more conventional ways to attempt to detect intermittent abnormal heart rhythms (such as issuing patients with such devices or recording the ECG for 72 h hoping to capture an event). Unlike PPG, ECG can only be recorded for short periods and often triggered by the user and so do not replace other methods to continually monitor ECG (such as Holter or implanted ECG recorders).
Arrhythmia can be diagnosed accurately using a single type of wearable data (ECG or HR characteristics from PPG). In contrast, other important cardiovascular diseases (such as heart failure, valvular heart disease, coronary artery disease, stroke) require specialist tests (such as cardiac ultrasound, coronary angiogram) to make an accurate diagnosis. However, the data wearables currently collect may still be useful. Heart failure and valvular heart disease are associated with increasing breathlessness on exertion and a reduced ability to be active127. It is highly likely that patterns of activity, respiratory rate, oximetry, and HR detected by wearables will change as a person develops these diseases and recent studies are encouraging16,128. Research is urgently required to test this potential, which may allow new approaches to community-based screening or diagnostic programmes.
Most patients who are diagnosed with cardiovascular disease typically have very limited interaction with healthcare services except when a crisis occurs (such as cardiac arrest, heart attack or urgent admission with heart failure). Such crises are often preventable if the signs of potential deterioration can be detected early enough for a change in management. Wearables hold great potential for such monitoring. For example, patients discharged after a heart attack are directed to adhere to a structured programme of physical activity129, and wearables have the potential to allow the healthcare system to know if patients are following such advice and target support to those who need this. People with heart failure suffer frequent worsening that can lead to life-threatening complications that are often preceded by weeks or months of increasing weight, reducing physical activity. These incipient signs of deterioration are likely also to be recognisable in changes in HR, respiratory rate, oximetry and BP. Wearables may therefore allow heart failure services to monitor patients and institute treatment (such as increasing diuretic therapy) to prevent admissions.
There remain several barriers to achieving the potential of wearables in healthcare. There is a pressing need for high-quality clinical studies that demonstrate the clinical scenarios in which providing wearable data improves outcomes. Data for its own sake is not helpful unless it can lead to an action that improves the patient’s health and clinicians already suffer “information overload”. Furthermore, in the health economic context, interventions need to meet a cost-benefit criteria.
Although consumer wearables are very attractive for introduction in healthcare due to their low cost and already high ownership levels, regulatory safeguards make this challenging. If data from wearables is used to make a clinical decision, then under current regulatory frameworks the wearable requires approval as a medical device. Most devices do not have such approvals and so using them in direct healthcare may pose legal risk.
Population Health Perspective
The large-scale collection of health data using consumer-grade wearables has the potential to address pressing population health challenges, including the obesity epidemic, mental health epidemic, and the growing burden of chronic illnesses and multimorbidity. Wearables provide an objective continuous stream of data, offering a more comprehensive and possibly more reliable alternative to traditional population health approaches like self-reported questionnaires, which are limited by recall bias and infrequent administration. The widespread uptake of wearables and thus the availability of vast amounts of remote data may play a pivotal role in advancing population-based research, answering key health questions and developing risk stratification tools to better target interventions.
Many cardiovascular diseases are preventable by increasing physical activity, changing diet, maintaining a healthy weight and lowering BP130. Wearables are already used by millions of people to monitor their levels of physical activity. Although total amount of daily activity is known to be protective, recent evidence shows that even very short bursts of vigorous activity can provide a substantial reduction in risk131. There is evidence that tracking physical activity using wearable devices can provide a modest increase in total amount performed132. However, using such tools as a way to evaluate and refine the effect of more general public health measures (such as education, improved public transport, or work-place interventions) may improve the evidence base of how to facilitate healthier behaviours in the population.
During the COVID-19 pandemic, it was demonstrated via the ZOE COVID symptom app and Covid Collab Fitbit study that large-scale collection of digital health data was feasible and valuable133,134.
Limitations and risks associated with population level monitoring using wearables should also be considered. For example, it’s conceivable that being monitored continuously might alter clinical relationships which are based on trust or compromise mental health. Personalised approaches should be implemented with caution, ensuring that the responsibility or burden of blame for certain health behaviours is not unfairly positioned from society to the individual. Furthermore, consideration must be made for the cost associated with the provision of wearables and similarly, selection bias if study participants have been recruited based on prior device ownership or high level of digital literacy as there is a risk of exacerbating health gradients along the digital divide, and excluding from interventions those strata that may receive the greatest benefit.
Data Availability
No datasets were generated or analysed during the current study.
References
Dhingra, L. S. et al. Use of wearable devices in individuals with or at risk for cardiovascular disease in the US, 2019 to 2020. JAMA Netw. Open 6, e2316634–e2316634 (2023).
Kumar, S. et al. Wearables in cardiovascular disease. J. Cardiovascular Transl. Res. 16, 557–568 (2023).
Charlton, P. H. & Marozas, V. Wearable photoplethysmography devices, in Photoplethysmography. 2022, Elsevier. p. 401–439.
Charlton, P. H. et al. Wearable photoplethysmography for cardiovascular monitoring. Proc. IEEE 110, 355–381 (2022).
Charlton, P. H. et al. Breathing rate estimation from the electrocardiogram and photoplethysmogram: A review. IEEE Rev. Biomed. Eng. 11, 2–20 (2017).
Nitzan, M., Nitzan, I. & Arieli, Y. The various oximetric techniques used for the evaluation of blood oxygenation. Sensors 20, 4844 (2020).
Elgendi, M. et al. The use of photoplethysmography for assessing hypertension. NPJ digital Med. 2, 60 (2019).
Stergiou, G. S. et al. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J. hypertension 40, 1449–1460 (2022).
Doherty, A. et al. Large scale population assessment of physical activity using wrist worn accelerometers: the UK biobank study. PloS one 12, e0169649 (2017).
Bouzid, Z., Al-Zaiti, S. S., Bond, R. & Sejdić, E. Remote and wearable ECG devices with diagnostic abilities in adults: A state-of-the-science scoping review. Heart Rhythm 19, 1192–1201 (2022).
Amir, H. M. et al. Comparison of Simultaneous Recordings from Medical-Grade and Smartwatch ECGs. Computing Cardiology (CinC) (IEEE, 2024).
Klimek, A., I. Mannheim, G. Schouten, E., Wouters, J. & Peeters, M.W. Wearables measuring electrodermal activity to assess perceived stress in care: a scoping review. Acta Neuropsychiatrica. 24, 1–11 (2023).
Posada-Quintero, H. F. & Chon, K. H. Innovations in electrodermal activity data collection and signal processing: A systematic review. Sensors 20, 479 (2020).
Mehra, A., Starkoff, B. E. & Nickerson, B. S. The evolution of bioimpedance analysis: From traditional methods to wearable technology. Nutrition. 129, 112601 (2024).
Samsung. How to measure your body composition or BMI with Galaxy Watch. 2025 [cited 2025 27/05/2025]; Available from: https://www.samsung.com/uk/support/mobile-devices/measure-your-body-composition-with-the-galaxy-watch-series/
Stehlik, J. et al. Continuous wearable monitoring analytics predict heart failure hospitalization: the LINK-HF multicenter study. Circulation: Heart Fail. 13, e006513 (2020).
Giménez-Miranda, L. et al. Wearable Devices Based on Bioimpedance Test in Heart Failure: Clinical Relevance: Systematic Review. Rev. Cardiovascular Med. 25, 315 (2024).
Boehmer, J. P. et al. A multisensor algorithm predicts heart failure events in patients with implanted devices: results from the MultiSENSE study. JACC: Heart Fail. 5, 216–225 (2017).
Sieciński, S., Kostka, P. S. & Tkacz, E. J. Gyrocardiography: a review of the definition, history, waveform description, and applications. Sensors 20, 6675 (2020).
Jaakkola, J. et al. Mobile phone detection of atrial fibrillation with mechanocardiography: the MODE-AF Study (Mobile Phone Detection of Atrial Fibrillation). Circulation 137, 1524–1527 (2018).
Doherty, C., M. Baldwin, A. Keogh, B. Caulfield, and R. Argent, Keeping Pace with Wearables: A Living Umbrella Review of Systematic Reviews Evaluating the Accuracy of Consumer Wearable Technologies in Health Measurement. Sports Medicine, 2024: p. 1–20.
Orini, M. et al. Long-term association of ultra-short heart rate variability with cardiovascular events. Sci. Rep. 13, 18966 (2023).
Vazir, A. et al. Association of resting heart rate and temporal changes in heart rate with outcomes in participants of the atherosclerosis risk in communities study. JAMA Cardiol. 3, 200–206 (2018).
Zhang, Y. et al. Validity of Wrist-Worn photoplethysmography devices to measure heart rate: a systematic review and meta-analysis. J. Sports Sci. 38, 2021–2034 (2020).
Parak, J. & Korhonen, I. Evaluation of wearable consumer heart rate monitors based on photopletysmography. in 2014 36th annual international conference of the IEEE engineering in medicine and biology society. IEEE (2014).
Nelson, B. W. & Allen, N. B. Accuracy of consumer wearable heart rate measurement during an ecologically valid 24-hour period: intraindividual validation study. JMIR mHealth uHealth 7, e10828 (2019).
Wallen, M. P., Gomersall, S. R., Keating, S. E., Wisløff, U. & Coombes, J. S. Accuracy of heart rate watches: implications for weight management. PloS one 11, e0154420 (2016).
Gillinov, S. et al. Variable accuracy of wearable heart rate monitors during aerobic exercise. Med. Sci. Sports Exerc. 49, 1697–1703 (2017).
Shcherbina, A. et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J. personalized Med. 7, 3 (2017).
Thiebaud, R. S. et al. Validity of wrist-worn consumer products to measure heart rate and energy expenditure. Digital health 4, 2055207618770322 (2018).
Dooley, E. E., Golaszewski, N. M. & Bartholomew, J. B. Estimating accuracy at exercise intensities: a comparative study of self-monitoring heart rate and physical activity wearable devices. JMIR mHealth uHealth 5, e7043 (2017).
Williams, K., A. Jamieson, N. Chaturvedi, A. Hughes, and M. Orini. Validation of Wearable Derived Heart Rate Variability and Oxygen Saturation from the Garmin’s Health Snapshot. in 2023 Computing in Cardiology (CinC). 2023. IEEE.
Fuller, D. et al. Reliability and Validity of Commercially Available Wearable Devices for Measuring Steps, Energy Expenditure, and Heart Rate: Systematic Review. JMIR Mhealth Uhealth 8, e18694 (2020).
Sartor, F., Papini, G., Cox, L. G. E. & Cleland, J. Methodological shortcomings of wrist-worn heart rate monitors validations. J. Med. Internet Res. 20, e10108 (2018).
Lang, M. Beyond Fitbit: a critical appraisal of optical heart rate monitoring wearables and apps, their current limitations and legal implications. Alb. LJ Sci. Tech. 28, 39 (2017).
Falter, M., Budts, W., Goetschalckx, K., Cornelissen, V. & Buys, R. Accuracy of Apple Watch Measurements for heart rate and energy expenditure in patients with cardiovascular disease: Cross-Sectional Study. JMIR mHealth uHealth 7, e11889 (2019).
Jamieson, A., Jones, S., Chaturvedi, N., Hughes, A. D. & Orini, M. Accuracy of smartwatches for the remote assessment of exercise capacity. Sci. Rep. 14, 22994 (2024).
Orini, M., G. Guvensen, A. Jamieson, N. Chaturvedi, and A. D. Hughes. Movement, Sweating, and Contact Pressure as Sources of Heart Rate Inaccuracy in Wearable Devices. in 2022 Computing in Cardiology (CinC). 2022. IEEE.
Malik, M. et al. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Eur. heart J. 17, 354–381 (1996).
Dekker, J. M. et al. Low heart rate variability in a 2-minute rhythm strip predicts risk of coronary heart disease and mortality from several causes: the ARIC Study. Circulation 102, 1239–1244 (2000).
Shaffer, F. & Ginsberg, J. P. An overview of heart rate variability metrics and norms. Front. Pub. Health. 5, 258 (2017).
Electrophysiology, T.F.o.t.E.S.o.C.t.N.A.S.o.P. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation 93, 1043–1065 (1996).
Sassi, R. et al. Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Ep. Europace 17, 1341–1353 (2015).
Schäfer, A. & Vagedes, J. How accurate is pulse rate variability as an estimate of heart rate variability?: A review on studies comparing photoplethysmographic technology with an electrocardiogram. Int. J. Cardiol. 166, 15–29 (2013).
Gil, E. et al. Photoplethysmography pulse rate variability as a surrogate measurement of heart rate variability during non-stationary conditions. Physiological Meas. 31, 1271 (2010).
Shaffer, F., Meehan, Z. M. & Zerr, C. L. A critical review of ultra-short-term heart rate variability norms research. Front. Neurosci. 14, 594880 (2020).
Georgiou, K. et al. Can wearable devices accurately measure heart rate variability? A systematic review. Folia Med. 60, 7–20 (2018).
Linz, D. et al. Atrial fibrillation: epidemiology, screening and digital health. Lancet Regional Health–Europe. 1, 37 (2024).
Perez, M. V. et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N. Engl. J. Med. 381, 1909–1917 (2019).
Tison, G. H. et al. Passive detection of atrial fibrillation using a commercially available smartwatch. JAMA Cardiol. 3, 409–416 (2018).
Bumgarner, J. M. et al. Smartwatch algorithm for automated detection of atrial fibrillation. J. Am. Coll. Cardiol. 71, 2381–2388 (2018).
Orini, M. et al. Premature atrial and ventricular contractions detected on wearable-format electrocardiograms and prediction of cardiovascular events. Eur. Heart J.-Digital Health 4, 112–118 (2023).
Prasitlumkum, N. et al. Diagnostic accuracy of smart gadgets/wearable devices in detecting atrial fibrillation: a systematic review and meta-analysis. Arch. Cardiovascular Dis. 114, 4–16 (2021).
Mannhart, D. et al. Clinical validation of 5 direct-to-consumer wearable smart devices to detect atrial fibrillation. BASEL wearable study Clin. Electrophysiol. 9, 232–242 (2023).
Strik, M. et al. Validating QT-interval measurement using the Apple Watch ECG to enable remote monitoring during the COVID-19 pandemic. Circulation 142, 416–418 (2020).
Hoek, L. J., Brouwer, J. L. P., Voors, A. A. & Maass, A. H. Smart devices to measure and monitor QT intervals. Front. cardiovascular Med. 10, 1172666 (2023).
Saghir, N. et al. A comparison of manual electrocardiographic interval and waveform analysis in lead 1 of 12-lead ECG and Apple Watch ECG: a validation study. Cardiovascular Digital Health J. 1, 30–36 (2020).
Pengel, L. K. et al. A comparison of ECG-based home monitoring devices in adults with CHD. Cardiol. Young-. 33, 1129–1135 (2023).
Nicolò, A., Massaroni, C., Schena, E. & Sacchetti, M. The importance of respiratory rate monitoring: From healthcare to sport and exercise. Sensors 20, 6396 (2020).
Baumert, M. et al. Mean nocturnal respiratory rate predicts cardiovascular and all-cause mortality in community-dwelling older men and women. Eur. Resp. J. 54, 1 (2019).
Varon, C. et al. A Comparative Study of ECG-derived Respiration in Ambulatory Monitoring using the Single-lead ECG. Sci. Rep. 10, 5704 (2020).
Jung, H., Kim, D., Choi, J. & Joo, E. Y. Validating a consumer smartwatch for nocturnal respiratory rate measurements in sleep monitoring. Sensors 23, 7976 (2023).
Shapiro, I., Stein, J., MacRae, C. & O’Reilly, M. Pulse oximetry values from 33,080 participants in the Apple Heart & Movement Study. NPJ Digital Med. 6, 134 (2023). p.
Windisch, P., Schröder, C., Förster, R., Cihoric, N. & Zwahlen, D. R. Accuracy of the apple watch oxygen saturation measurement in adults: a systematic review. Cureus. 15, e35355 (2023).
Zhang, Z. & Khatami, R. Can we trust the oxygen saturation measured by consumer smartwatches?. Lancet Respiratory Med. 10, e47–e48 (2022).
Tryon, W. W., Activity measurement in psychology and medicine. 2013: Springer Science & Business Media.
Master, H. et al. Association of step counts over time with the risk of chronic disease in the All of Us Research Program. Nat. Med. 28, 2301–2308 (2022).
Bassett, D. R., Toth, L. P., LaMunion, S. R. & Crouter, S. E. Step counting: a review of measurement considerations and health-related applications. Sports Med. 47, 1303–1315 (2017).
Buendia, R. et al. Wearable Sensors to Monitor Physical Activity in Heart Failure Clinical Trials: State-of-the-Art Review. J. Cardiac Fail. 30, 703–716 (IEEE, 2024).
Bohannon, R. W. & Crouch, R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. J. evaluation Clin. Pract. 23, 377–381 (2017).
Evenson, K. R. & Spade, C. L. Review of validity and reliability of Garmin activity trackers. J. Meas. Phys. Behav. 3, 170–185 (2020).
Straczkiewicz, M., James, P. & Onnela, J.-P. A systematic review of smartphone-based human activity recognition methods for health research. NPJ Digital Med. 4, 148 (2021).
Dorn, D. et al. Automatic identification of physical activity type and duration by wearable activity trackers: a validation study. JMIR mHealth uHealth 7, e13547 (2019).
Bassett, D. R. Jr. and E.T. Howley, Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci. Sports Exerc 32, 70–84 (2000).
Hartung, G. H., Blancq, R. J., Lally, D. A. & Krock, L. P. Estimation of aerobic capacity from submaximal cycle ergometry in women. Med. Sci. sports Exerc. 27, 452–457 (1995).
Walker, H. K., Hall, W.D., Hurst, J. W. Clinical methods: the history, physical, and laboratory examinations. (1990).
Blair, S. N. et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. Jama 276, 205–210 (1996).
Kodama, S. et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. Jama 301, 2024–2035 (2009).
Zaccardi, F. et al. Cardiorespiratory fitness and risk of type 2 diabetes mellitus: A 23-year cohort study and a meta-analysis of prospective studies. Atherosclerosis 243, 131–137 (2015).
Themanson, J. & Hillman, C. Cardiorespiratory fitness and acute aerobic exercise effects on neuroelectric and behavioral measures of action monitoring. Neuroscience 141, 757–767 (2006).
Ekblom-Bak, E. et al. Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279,455 adults: a case control study. Int. J. Behav. Nutr. Phys. Act. 18, 1–16 (2021).
Nocon, M. et al. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur. J. Preventive Cardiol. 15, 239–246 (2008).
Ross, R. et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation 134, e653–e699 (2016).
Ltd., F. T. Automated Fitness Level (VO2max) Estimation with Heart Rate and Speed Data. (2014).
Apple. Using Apple Watch to Estimate Cardio Fitness with VO2 max. 2021 cited 2024; Available from: https://www.apple.com/healthcare/docs/site/Using_Apple_Watch_to_Estimate_Cardio_Fitness_with_VO2_max.pdf.
Molina-Garcia, P. et al. Validity of estimating the maximal oxygen consumption by consumer wearables: a systematic review with meta-analysis and expert statement of the INTERLIVE network. Sports Med. 52, 1577–1597 (2022).
Tran, T., Steiner, J. M., Venkateswaran, A. & Buber, J. Peak oxygen consumption by smartwatches compared with cardiopulmonary exercise test in complex congenital heart disease. Heart. 110, 353–358 (2023).
Jamieson, A. et al. Comparison between Smartwatch-Derived and CPET-Measured VO2Max. Computing in Cardiology (CinC) (IEEE, 2024).
Loucks, A. B., B. Kiens, and H. H. Wright, Energy availability in athletes. Food, Nutrition and Sports Performance III, 2013: p. 7-15.
Seale, J. L., Conway, J. M. & Canary, J. J. Seven-day validation of doubly labeled water method using indirect room calorimetry. J. Appl. Physiol. 74, 402–409 (1993).
Hills, A. P., Mokhtar, N. & Byrne, N. M. Assessment of physical activity and energy expenditure: an overview of objective measures. Front. Nutr. 1, 5 (2014).
Bunn, J. A., Navalta, J. W., Fountaine, C. J. & Reece, J. D. Current state of commercial wearable technology in physical activity monitoring 2015–2017. Int. J. Exerc. Sci. 11, 503 (2018).
Moher, D. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4, 1–9 (2015).
Feigin, V. L. et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 20, 795–820 (2021).
Schutte, A. E., Kollias, A. & Stergiou, G. S. Blood pressure and its variability: classic and novel measurement techniques. Nat. Rev. Cardiol. 19, 643–654 (2022).
Welykholowa, K. et al. Multimodal photoplethysmography-based approaches for improved detection of hypertension. J. Clin. Med. 9, 1203 (2020).
Mukkamala, R. et al. Evaluation of the accuracy of cuffless blood pressure measurement devices: challenges and proposals. Hypertension 78, 1161–1167 (2021).
Islam, S. M. S. et al. Wearable cuffless blood pressure monitoring devices: a systematic review and meta-analysis. Eur. Heart J.-Digital Health 3, 323–337 (2022).
Tan, I. et al. Evaluation of the ability of a commercially available cuffless wearable device to track blood pressure changes. J. hypertension 41, 1003–1010 (2023).
Mukkamala, R., Shroff, S. G., Kyriakoulis, K. G., Avolio, A. P. & Stergiou, G. S. Cuffless Blood Pressure Measurement: Where Do We Actually Stand?. Hypertension 82, 957–970 (2025).
Mukkamala, R. et al. The Microsoft Research Aurora Project: important findings on cuffless blood pressure measurement. Hypertension 80, 534–540 (2023).
Bhatt, B. J. et al. Validation of a popular consumer-grade cuffless blood pressure device for continuous 24-hour monitoring. Eur. Heart J.-Digit. Health. 6, 704–712 (2025).
Rechtschaffen, A., Bergmann, B. M., Everson, C. A., Kushida, C. A. & Gilliland, M. A. Sleep deprivation in the rat: X. Integration and discussion of the findings. Sleep 12, 68–87 (1989).
Allebrandt, K. V. et al. Chronotype and sleep duration: the influence of season of assessment. Chronobiol. Int. 31, 731–740 (2014).
Cappuccio, F. P., D’Elia, L., Strazzullo, P. & Miller, M. A. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33, 585–592 (2010).
Jike, M., Itani, O., Watanabe, N., Buysse, D. J. & Kaneita, Y. Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep. Med. Rev. 39, 25–36 (2018).
Itani, O., Jike, M., Watanabe, N. & Kaneita, Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep. Med. 32, 246–256 (2017).
Schyvens, A.-M. et al. Accuracy of Fitbit Charge 4, Garmin Vivosmart 4, and WHOOP Versus Polysomnography: Systematic Review. JMIR mHealth uHealth 12, e52192 (2024).
Lee, T. et al. Accuracy of 11 wearable, nearable, and airable consumer sleep trackers: Prospective multicenter validation study. JMIR mHealth uHealth 11, e50983 (2023).
Altini, M. & Kinnunen, H. The promise of sleep: A multi-sensor approach for accurate sleep stage detection using the oura ring. Sensors 21, 4302 (2021).
Haghayegh, S., Khoshnevis, S., Smolensky, M. H., Diller, K. R. & Castriotta, R. J. Accuracy of wristband Fitbit models in assessing sleep: systematic review and meta-analysis. J. Med. Internet Res. 21, e16273 (2019).
Jerath, R., Syam, M. & Ahmed, S. The future of stress management: integration of smartwatches and HRV technology. Sensors 23, 7314 (2023).
Kim, H.-G., Cheon, E.-J., Bai, D.-S., Lee, Y. H. & Koo, B.-H. Stress and heart rate variability: a meta-analysis and review of the literature. Psychiatry Investig. 15, 235 (2018).
Hackett, R. A. & Steptoe, A. Type 2 diabetes mellitus and psychological stress—a modifiable risk factor. Nat. Rev. Endocrinol. 13, 547–560 (2017).
Steptoe, A. & Kivimäki, M. Stress and cardiovascular disease. Nat. Rev. Cardiol. 9, 360–370 (2012).
Hickey, B. A. et al. Smart devices and wearable technologies to detect and monitor mental health conditions and stress: A systematic review. Sensors 21, 3461 (2021).
Chen, J., Abbod, M. & Shieh, J.-S. Pain and stress detection using wearable sensors and devices—A review. Sensors 21, 1030 (2021).
Alzueta, E. et al. Tracking sleep, temperature, heart rate, and daily symptoms across the menstrual cycle with the Oura ring in healthy women. Int. J. Women’s Health 8, 491–503 (2022).
Maijala, A., Kinnunen, H., Koskimäki, H., Jämsä, T. & Kangas, M. Nocturnal finger skin temperature in menstrual cycle tracking: ambulatory pilot study using a wearable Oura ring. BMC Women’s. Health 19, 1–10 (2019).
Lyzwinski, L., Elgendi, M. & Menon, C. Innovative approaches to menstruation and fertility tracking using wearable reproductive health technology: systematic review. J. Med. Internet Res. 15, 26 (2024).
Ranjan, Y. et al. RADAR-base: open source mobile health platform for collecting, monitoring, and analyzing data using sensors, wearables, and mobile devices. JMIR mHealth uHealth 7, e11734 (2019).
Gill, S. K. et al. Consumer wearable devices for evaluation of heart rate control using digoxin versus beta-blockers: the RATE-AF randomized trial. Nat. Med. 30, 2030–2036 (2024).
Wetherell, M. A., Williams, G. & Doran, J. Assessing the psychobiological demands of high-fidelity training in pre-hospital emergency medicine. Scand. J. Trauma, Resuscitation Emerg. Med. 32, 101 (2024).
Naghavi, M. et al. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2100–2132 (2024).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
Lubitz, S. A. et al. Detection of atrial fibrillation in a large population using wearable devices: the Fitbit Heart Study. Circulation 146, 1415–1424 (2022).
Caraballo, C. et al. Clinical implications of the New York heart association classification. J. Am. Heart Assoc. 8, e014240 (2019).
Singhal, A. & Cowie, M. R. Digital health: implications for heart failure management. Cardiac Fail. Rev. 7, 8 (2021).
Oldridge, N. B., Guyatt, G. H., Fischer, M. E. & Rimm, A. A. Cardiac rehabilitation after myocardial infarction: combined experience of randomized clinical trials. Jama 260, 945–950 (1988).
Lee, I.-M. et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. lancet 380, 219–229 (2012).
Stamatakis, E. et al. Association of wearable device-measured vigorous intermittent lifestyle physical activity with mortality. Nat. Med. 28, 2521–2529 (2022).
Ringeval, M., Wagner, G., Denford, J., Paré, G. & Kitsiou, S. Fitbit-based interventions for healthy lifestyle outcomes: systematic review and meta-analysis. J. Med. Internet Res. 22, e23954 (2020).
Menni, C. et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study. Lancet 399, 1618–1624 (2022).
Stewart, C. et al. Physiological presentation and risk factors of long COVID in the UK using smartphones and wearable devices: a longitudinal, citizen science, case–control study. Lancet Digital Health 6, e640–e650 (2024).
Chan, P., Ryan, N., Chen, D., McNeil, J. & Hopper, I. Novel wearable and contactless heart rate, respiratory rate, and oxygen saturation monitoring devices: a systematic review and meta-analysis. Anaesthesia 77, 1268–1280 (2022).
Chevance, G. et al. Accuracy and precision of energy expenditure, heart rate, and steps measured by combined-sensing Fitbits against reference measures: systematic review and meta-analysis. JMIR mHealth uHealth 10, e35626 (2022).
Germini, F. et al. Accuracy and acceptability of wrist-wearable activity-tracking devices: systematic review of the literature. J. Med. Internet Res. 24, e30791 (2022).
Irwin, C. & Gary, R. Systematic review of Fitbit charge 2 validation studies for exercise tracking. Transl. J. Am. Coll. Sports Med. 7, 1–7 (2022).
Koerber, D., Khan, S., Shamsheri, T., Kirubarajan, A. & Mehta, S. Accuracy of heart rate measurement with wrist-worn wearable devices in various skin tones: a systematic review. J. Racial Ethn. Health Disparities 10, 2676–2684 (2023).
Board, L., Ispoglou, T. & Ingle, L. Validity of telemetric-derived measures of heart rate variability: a systematic review. J. Exerc. Physiol. online 19, 64–84 (2016).
Dobbs, W. C. et al. The accuracy of acquiring heart rate variability from portable devices: a systematic review and meta-analysis. Sports Med. 49, 417–435 (2019).
Belani, S., Wahood, W., Hardigan, P., Placzek, A. N. & Ely, S. Accuracy of detecting atrial fibrillation: a systematic review and meta-analysis of wrist-worn wearable technology. Cureus. 13, 12 (2021).
Giebel, G. D. & Gissel, C. Accuracy of mHealth devices for atrial fibrillation screening: systematic review. JMIR mHealth uHealth 7, e13641 (2019).
Hermans, A. N. et al. Mobile health solutions for atrial fibrillation detection and management: a systematic review. Clin. Res. Cardiol. 111, 479–491 (2022).
Lopez Perales, C. R. et al. Mobile health applications for the detection of atrial fibrillation: a systematic review. EP Europace 23, 11–28 (2021).
Nazarian, S., Lam, K., Darzi, A. & Ashrafian, H. Diagnostic accuracy of smartwatches for the detection of cardiac arrhythmia: systematic review and meta-analysis. J. Med. Internet Res. 23, e28974 (2021).
Evenson, K. R., Goto, M. M. & Furberg, R. D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 12, 1–22 (2015).
Feehan, L. M. et al. Accuracy of Fitbit devices: systematic review and narrative syntheses of quantitative data. JMIR mHealth uHealth 6, e10527 (2018).
Henriksen, A., Johansson, J., Hartvigsen, G., Grimsgaard, S. & Hopstock, L. Measuring physical activity using triaxial wrist worn polar activity trackers: a systematic review. Int. J. Exerc. Sci. 13, 438 (2020).
Leung, W., Case, L., Sung, M.-C. & Jung, J. A meta-analysis of Fitbit devices: same company, different models, different validity evidence. J. Med. Eng. Technol. 46, 102–115 (2022).
O’Driscoll, R. et al. How well do activity monitors estimate energy expenditure? A systematic review and meta-analysis of the validity of current technologies. Br. J. sports Med. 54, 332–340 (2020).
Kenyon, A., McEvoy, M., Sprod, J. & Maher, C. Validity of pedometers in people with physical disabilities: A systematic review. Arch. Phys. Med. Rehab 94, 1161–1170 (2013).
Birrer, V., Elgendi, M., Lambercy, O. & Menon, C. Evaluating reliability in wearable devices for sleep staging. npj Digital Med. 7, 74 (2024).
Imtiaz, S. A. A systematic review of sensing technologies for wearable sleep staging. Sensors 21, 1562 (2021).
Rentz, L. E., Ulman, H. K. & Galster, S. M. Deconstructing commercial wearable technology: contributions toward accurate and free-living monitoring of sleep. Sensors 21, 5071 (2021).
Scott, H., Lack, L. & Lovato, N. A systematic review of the accuracy of sleep wearable devices for estimating sleep onset. Sleep. Med. Rev. 49, 101227 (2020).
Acknowledgements
M.O. was supported by British Heart Foundation Accelerator Award AA/18/6/34223. A.J. was supported by a British Heart Foundation 4-year PhD studentship (FS/19/63/34902) awarded to UCL. S.J. is supported by BHF grant SP/F/21/150020. A.D.H. receives support from the BHF, the Horizon 2020 Framework Programme of the European Union, the National Institute for Health Research University College London Hospitals Biomedical Research Centre, the UK Medical Research Council and the Wellcome Trust. N.C. and A.D.H. work in a unit that receives support from the UK Medical Research Council (MC_UU_12019/1).
Author information
Authors and Affiliations
Contributions
A.J., T.C., and M.O. drafted the manuscript. All authors (A.J., T.C., S.J., N.C., A.D.H. & M.O.) reviewed and contributed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jamieson, A., Chico, T.J.A., Jones, S. et al. A guide to consumer-grade wearables in cardiovascular clinical care and population health for non-experts. npj Cardiovasc Health 2, 44 (2025). https://doi.org/10.1038/s44325-025-00082-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44325-025-00082-6