Abstract
Atrial fibrillation (AF) is prevalent in aging populations; however not all individuals age at the same rate. Instead, individuals of the same chronological age can vary in health status from fit to frail. Our objective was to determine the impacts of age and frailty on atrial function and arrhythmogenesis in mice using a frailty index (FI). Aged mice were more frail and demonstrated longer lasting AF compared to young mice. Consistent with this, aged mice showed longer P wave duration and PR intervals; however, both parameters showed substantial variability suggesting differences in health status among mice of similar chronological age. In agreement with this, P wave duration and PR interval were highly correlated with FI score. High resolution optical mapping of the atria demonstrated reduced conduction velocity and action potential duration in aged hearts that were also graded by FI score. Furthermore, aged mice had increased interstitial fibrosis along with changes in regulators of extracellular matrix remodelling, which also correlated with frailty. These experiments demonstrate that aging results in changes in atrial structure and function that create a substrate for atrial arrhythmias. Importantly, these changes were heterogeneous due to differences in health status, which could be identified using an FI.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common sustained arrhythmia1. It is an enormous clinical problem that is projected to affect up to 30 million people in North American and Europe by the year 20502. AF is associated with substantial morbidity and mortality, is prevalent in heart failure (which is worsened when coexisting with AF)3 and is a major risk factor for ischemic stroke4,5. It is well known that the prevalence of AF increases with age4,6. Furthermore, epidemiological studies demonstrate that the progression of AF from persistent or paroxysmal forms to permanent AF is also associated with increasing age7.
Although it is well appreciated that the frequency of AF development increases with age it is critical to recognize that not all individuals age at the same rate and an individual’s health status can vary from fit to frail regardless of chronological age8,9,10. This is because people accumulate health deficits, which manifest as frailty, at different rates and for different reasons11. People that age rapidly are described as frail, while those that age more successfully are fitter. As individuals become clinically frail the risk of adverse health outcomes increases12,13. Frailty is very common in patients with cardiovascular disease14.
A well-established clinical method to quantify frailty is to measure deficit accumulation using a frailty index (FI)8,11. In this approach, deficits in health status may include signs, symptoms, diseases, disabilities and/or laboratory abnormalities. The FI score for an individual is represented by the proportion of deficits present in that individual, whereby the number of health deficits present in each individual is counted and divided by the total number of items measured. Accordingly, FI scores can range from 0 (no deficits present; least frail) to 1 (all deficits present; most frail). We have developed a non-invasive 31 item FI based on deficit accumulation for use in animal models (i.e. mice)15,16,17. Using this FI we have demonstrated that the relationships between FI score and age are very similar in mice and humans. Furthermore, we have recently used our FI approach to study the impacts of age and frailty on ventricular myocyte18 and sinoatrial node19,20 function in mice. Collectively, our prior work demonstrates that our FI approach is a powerful new tool to study aging-related changes in the heart.
While the clinical links between age and AF are well established, very few studies have investigated the cellular and molecular mechanisms that create a substrate for AF in aged individuals and no studies have evaluated how atrial function is related to frailty. Our development of a method for quantifying frailty in mice enables detailed studies, including at the cellular and molecular levels, of age-related cellular dysfunction. Indeed, it has been proposed that alterations at the cellular and subcellular levels may scale up and give rise to deficits that can be detected clinically21. This represents an essential area of investigation that will provide much needed insight into the biology of frailty, which is not well understood. Accordingly, the purpose of this study was to determine how atrial structure and function are affected by age and frailty in mice using our deficit accumulation approach. Our experiments demonstrate that atrial arrhythmogenesis and changes in atrial function are present in aged mice and that these occur in association with electrical and structural remodelling in the atria. We also show that alterations in atrial structure and function, including at the molecular level, are strongly predicted by individual health status as assessed using a frailty index.
Methods
An expanded Methods section is available in the Supplementary data.
Mice and frailty assessment
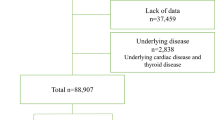
This study utilized young (13.1 ± 3.0 weeks; n = 80) and aged (101.8 ± 10.1 weeks; n = 110) male C57BL/6 mice, which were purchased at the age of 3–4 weeks and housed in our animal care facility until used experimentally. All experimental procedures were approved by the Dalhousie University Committee for Laboratory Animals and followed the guidelines of the Canadian Council on Animal Care.
Frailty was assessed in all mice immediately prior to experimental use using our non-invasive 31 item frailty index, which is based on established clinical signs of health deterioration in mice15,22 as we have done previously19. Specific clinical assessments of the integument, musculoskeletal, vestibulocochlear/auditory, ocular, nasal, digestive, urogenital and respiratory systems were made. We also assessed mice for signs of discomfort and measured both body surface temperature and body mass. Each of the 31 items that were assessed is listed in our published frailty assessment form (Supplemental Table 1)15. To score deficit accumulation, each trait was given a score of 0 (no sign of deficit), 0.5 (mild deficit) or 1 (severe deficit). Deficits in body mass and body temperature were scored based on deviation from the mean of young or aged mice15,19. For each animal the scores for each trait were summed and the total was divided by the number of items measured (i.e. 31) to provide a frailty index score between 0 (least frail) and 1 (most frail). Individuals performing functional measurements did not know the FI score of the mice until after data were analyzed.
In vivo electrophysiology and programmed stimulation
Electrophysiology and arrhythmia studies were performed in anesthetized mice (2% isoflurane) using 30 gauge subdermal needle electrodes (Grass Technologies) to record body surface (lead II) ECGs. In addition, a 1.2 French octapolar electrophysiology catheter was inserted in the heart via the right jugular vein, as we have described previously23,24. P wave duration and PR interval were measured from surface ECGs. Atrial (AERP) and atrioventricular node (AVERP) effective refractory periods were measured using S1/S2 stimulation protocols in which the heart was paced at a cycle length of 100 ms (S1) followed by an extra stimulus (S2) at progressively shorter cycle lengths. Inducibility of AF was measured using burst pacing in the right atrium. AF was defined as a rapid and irregular atrial rhythm lasting a minimum of 1s on the surface ECG. AF was categorized into three groups: <5s (brief); 5–30s (non-sustained); >30s (sustained). Further details are provided in the Data Supplement.
High resolution optical mapping
To investigate patterns of electrical conduction in the atria we used high resolution optical mapping in atrial preparations as we have described previously23,24,25. Optical mapping was performed using the voltage sensitive dye di-4-ANEPPS (10 μM). Contractile activity was suppressed using blebbistatin (10 μM)26. All analyses were performed using custom software. Details are provided in the Data Supplement.
Collagen staining and collagen assay
Interstitial collagen was assessed using picrosirius red (collagen) and fast green (myocardium) staining of paraffin embedded sections (3 μm) through the right and left atria. The level of fibrosis was quantified using ImageJ software as previously described23,24. Total collagen content was measured using a hydroxyproline assay (Sigma-Aldrich) according to kit instructions. These assays were performed using the right and left atrial appendages.
Quantitative PCR
Quantitative gene expression was measured in the right and left atria as we have done previously23,27,28. Intron spanning primers (Supplemental Table 2) were designed for collagen I (col1a), collagen III (col3a), matrix metalloproteinase 2 (MMP2), MMP9, tissue inhibitor of metalloproteinase 1 (TIMP1), TIMP2, TIMP3, TIMP4, transforming growth factor β (TGFβ) and connective tissue growth factor (CTGF). β-actin (Actb) and GAPDH were used as reference genes. Experimental protocols are described in the Data Supplement.
Statistical analysis
All data are presented as box and whisker plots (including median, upper and lower quartiles, upper and lower maximums) or means ± SD. Data were analyzed using Student’s t-test, two-way ANOVA with Tukey’s posthoc test or Fisher’s exact test, as indicated in each figure legend, to detect differences in young vs. aged mice. To assess differences as a function of frailty we performed linear regression analysis and used Pearson’s correlation to obtain correlation coefficients. P < 0.05 was considered significant.
Results
Assessment and quantification of frailty in mice
All mice utilized in this study underwent frailty assessment using our non-invasive FI15,16 resulting in the generation of an FI score for each individual. Young mice had an average FI score of 0.11 ± 0.01 while aged mice had an average FI score of 0.25 ± 0.01 (P < 0.001; Fig. 1). It is apparent from the data in Fig. 1 that mice of similar chronological age can have a range of FI scores. This is especially true in the aged mice and is indicative of differences in health status regardless of chronological age. Furthermore, it is important to note that while aged mice had a higher average FI score, there is overlap in these FI scores between young and aged mice even though they differ substantially in chronological age. Thus, by assessing frailty, we are able to identify differences in health status among different age groups as well as within a given age group, which is consistent with our previous work in this area19.
Occurrence of atrial fibrillation and atrioventricular node block in vivo
As AF is a common and serious problem in the aged population we began by assessing the occurrence and duration of AF during burst pacing in anesthetized mice (Fig. 2A). Although we did not observe a difference in overall susceptibility to AF in young vs. aged mice (Fig. 2B) we found that the duration of AF, when induced, was longer (P = 0.03) in aged mice compared to young mice (Fig. 2C). In fact, all AF in young mice was non-sustained, lasting less than 5s before spontaneously reverting back to sinus rhythm (Fig. 2C; Supplemental Table 3). In contrast, when AF was induced in aged mice it was long lasting. Specifically, one mouse had AF that lasted 21.3s, while the remainder all demonstrated sustained AF lasting longer than 30s and up to several minutes (Fig. 2C, Supplemental Table 3). The average FI score in young mice demonstrating AF was 0.08 ± 0.02 while the aged mice demonstrating AF had a higher (P < 0.05) average FI score of 0.25 ± 0.03 (Fig. 2D) indicating that mice with higher FI scores were more likely to experience sustained AF.
(A) Representative body surface (top) and intracardiac atrial (bottom) ECGs illustrating the induction of AF following burst pacing (P) in young and aged mice. Note that the young mouse spontaneously returned to sinus rhythm after 1.1s of AF while the aged mouse remained in AF over the same time period. In this example, the aged mouse was in AF for a total of 21.3s. (B) Summary of inducibility of AF in young and aged mice. Numbers in parentheses indicate the number of mice that were induced into AF following burst pacing. Data analyzed by Fischer’s exact test. (C) Summary data illustrating the duration of AF in young (n = 4) and aged (n = 4) mice that were induced into AF. Data analyzed by Student’s t-test. (D) Frailty index scores in young and aged mice that were induced into AF. *P < 0.05 vs. young by Student’s t-test.
Further evidence of a substrate for AF and abnormal conduction in aged mice was obtained by measuring the occurrence of AV node block (Fig. 3A). No AV node block was observed in young mice (0/20 mice). In contrast, 27% of aged mice (7/26 mice) displayed spontaneous AV node block (either 2:1 or complete AV node block; Fig. 3C). Average FI score in the aged mice used to assess incidence of AV node block was 0.23 ± 0.04, which was higher (P < 0.05) than the average FI score of 0.09 ± 0.04 (Fig. 3D) in the young mice used in this experiment, further suggesting that mice with higher FI scores are more susceptible to arrhythmias.
(A) Representative surface ECG illustrating an example of 2:1 AV node block in an aged mouse. (B) Representative surface ECG illustrating an example of complete AV node block in an aged mouse. (C) Summary data illustrating the frequency of occurrence of AV node block in young vs. aged mice. Numbers in parentheses indicate the number of mice that demonstrated AV node block. Data analyzed by Fischer’s exact test. (D) Frailty index scores in young and aged mice used in assessment of AV node block. *P < 0.05 vs. young by Student’s t-test.
Effects of age and frailty on conduction in the atria and through the atrioventricular node in vivo
Based on the evidence of increased predisposition to sustained AF and increased incidence of AV node block in aged mice we next measured P wave duration (a measure of atrial conduction time) and PR interval (a measure of conduction through the AV node) from ECG recordings in anesthetized young and aged mice (Fig. 4, Supplemental Table 4). P wave duration was increased (P < 0.001) in aged mice (Fig. 4B). Notably, there was substantial variability in both age groups so that mice of similar chronological age could have very different P wave durations, indicating that factors other than chronological age may impact atrial conduction time. To determine how P wave duration was impacted by frailty, P wave duration in each individual from both age groups was plotted as a function of each animal’s FI score (Fig. 4C). These data demonstrate that P wave duration is strongly correlated (P < 0.0001) with frailty.
(A) Representative surface ECG recordings in young and aged mice. (B) Summary of differences in P wave duration in young and aged mice. Data analyzed using Student’s t-test. (C) Linear regression analysis of P wave duration as a function of FI score for the same mice as used in panel B. (D) Summary of differences in PR interval in young and aged mice. Data analyzed using Student’s t-test. (E) Linear regression analysis of PR interval as a function of FI score for the same mice as used in panel D. For panels B and D n = 22 young mice and 24 aged mice. For panels C and E n = 46 mice.
PR interval was also increased (P < 0.001) in aged mice (Fig. 4D). Once again, there was substantial variability within age groups, particularly in the aged mice. Frailty analysis (Fig. 4E) illustrates that, similar to P wave duration, PR interval is correlated with FI score (P = 0.002). Thus, it becomes evident from these plots that young and aged mice with similar FI scores have similar measures of P wave duration and PR interval despite their differences in chronological age. Together, these analyses demonstrate that P wave duration and PR interval were graded with FI score such that these measures of atrial and AV node conduction fall along a continuum when measured as a function of frailty (i.e. health status).
We also assessed P wave duration and PR interval in young and aged mice after the application of atropine and propranolol to block muscarinic and β-adrenergic receptors respectively (Supplemental Fig. S1). This enables an assessment of atrial and AV node conduction independently of the autonomic nervous system23,24,29. P wave duration was increased (P < 0.05) following autonomic blockade in both young and aged mice. Furthermore, following blockade, P wave duration remained prolonged (P < 0.05) in aged mice vs. young mice (Supplemental Fig. S1B). Consistent with the data in Fig. 4, linear regression analysis demonstrates that P wave duration is correlated with FI score at baseline (P = 0.0001; Supplemental Fig. S1C) and after autonomic blockade (P = 0.02; Supplemental Fig. S1D). Similarly, following autonomic blockade, PR interval remained prolonged (P < 0.05) in aged mice vs. young mice (Supplemental Fig. S1E). Once again, scatter plots of PR interval as a function of FI score demonstrate PR interval is graded as a function of frailty at baseline (P = 0.001; Supplemental Fig. S1F) and after autonomic blockade (P = 0.002; Supplemental Fig. S1G). These data demonstrate that, independent of the autonomic nervous system, conduction across the atria and through the AV node becomes progressively slower as frailty increases.
Changes in P wave duration and PR interval are thought to be indicators of susceptibility to AF30,31. Furthermore, our data illustrate that AF severity is greater in older, more frail mice and that P wave duration and PR interval are graded by FI score. Accordingly, we examined whether AF duration demonstrated any relationships with P wave duration or PR interval in the mice that were induced into AF in our study (Supplemental Fig. S2). These measurements illustrate that AF duration was highly correlated with both P wave duration (P = 0.04) and PR interval (P = 0.003).
Impacts of age and frailty on atrial conduction patterns and action potential morphology
To study how age and frailty affect patterns of electrical conduction in the atria we used high resolution optical mapping in isolated atrial preparations (Fig. 5) as we have done previously23,25,26. Representative activation maps (Fig. 5A) demonstrate that conduction initiates in the right atrial posterior wall (which corresponds to the location of the sinoatrial node23,24) and then spreads throughout the right and left atria. Note that in these examples conduction time across the atrial preparation is longer in the aged heart (34 ms) compared to the young heart (23 ms).
(A) Representative activation maps in atrial preparations from a young mouse and an aged mouse. The right atrium is on the right side of the image. Red colour indicates the earliest activation time in the right atrial posterior wall. Time interval between isochrones is 1.25 ms. (B and C), Summary of the effects of age on right atrial (B) and left atrial (C) conduction velocity. Data analyzed using Student’s t-test; n = 10 young and 40 aged mice. (D and E), Linear regression analysis of right atrial (D) and left atrial (E) conduction velocity as a function of FI score; n = 50 mice for panels D and E.
We measured local conduction velocity (CV) in the right and left atria from these optical mapping studies. These measurements, performed in atrial preparations in sinus rhythm, demonstrate that CV was reduced in the right (P < 0.001; Fig. 5B) and left (P < 0.05; Fig. 5C) atria of aged mice. Similar to our in vivo findings, local CV in the atria showed substantial variability within age groups, especially in the aged mice. Accordingly, we next plotted local right and left atrial CV as a function of frailty. These data show that CV was highly correlated with FI score in the right (P < 0.0001; Fig. 5D) and left (P = 0.0004; Fig. 5E) atria. We also performed optical mapping studies in atrial preparations that were paced at a fixed cycle length (125 ms) in order to account for the possibility of rate dependent effects on atrial conduction (Fig. 6). The results from these experiments were very similar to the findings obtained from atrial preparations in sinus rhythm and further support the conclusion that right and left atrial conduction decreases with increasing FI score, including within an age group.
(A) Representative activation maps in atrial preparations from a young mouse and an aged mouse paced at a fixed cycle length of 125 ms. (B and C) Summary of the effects of age on right atrial (B) and left atrial (C) conduction velocity. Data analyzed using Student’s t-test; n = 10 young and 40 aged mice. (D and E), linear regression analysis of right atrial (D) and left atrial (E) conduction velocity as a function of FI score; n = 50 mice.
Next, we measured the effects of age and frailty on optical action potential (AP) morphology in the right and left atria (Fig. 7). AP duration at 50% repolarization (APD50) was not different (P = 0.50; Fig. 7B) while APD90 was reduced (P = 0.03; Fig. 7C) in the right atrium of aged mice. We did not detect a difference in left atrial APD50 between age groups (P = 0.99; Fig. 7D), but left atrial APD90 was also reduced in aged mice (P = 0.003; Fig. 7E). Aged mice, in particular, demonstrated substantial variability in APD in the right and left atria. When analyzed by FI score, we found that right atrial APD50 (Fig. 7F), right atrial APD90 (Fig. 7G) and left atrial APD90 (Fig. 7I) were all correlated with (P = 0.03) and graded by frailty. These findings demonstrate that frailty analysis enabled us to identify differences in atrial CV and APD as a function of differences in health status separately from chronological age.
(A) Representative optical APs from the right atrium (top) and left atrium (bottom) in young (left) and aged (right) mice. Right atrial APs were measured in the right atrial appendage while left atrial APs were measured in the left atrial appendage. (B–E), Summary data illustrating the effects of age on right atrial APD50 (B), right atrial APD90 (C), left atrial APD50 (D) and left atrial APD90 (E); data analyzed by Mann Whitney rank sum test; n = 10 young and 40 aged mice. (F–I), Linear regression analysis illustrating correlations between right atrial APD50 (F), right atrial APD90 (G), left atrial APD50 (H) or left atrial APD90 (I) and FI score; n = 50 mice.
Effects of age and frailty on atrial fibrosis
Slow conduction and increased susceptibility to AF can be caused in part by structural remodelling in the atria due to the accumulation of collagen4,32. Accordingly, we assessed patterns of interstitial fibrosis in the right and left atria using picrosirius red staining23,24. Representative histological images (Fig. 8A) as well as summary data (Fig. 8B) demonstrate that interstitial fibrosis was increased in the right (P < 0.001) and left (P < 0.001) atria in aged mice. Furthermore, interstitial fibrosis was highly correlated with FI score in the right (P = 0.002) and left (P = 0.0008) atria such that atrial fibrosis was graded with frailty (Fig. 8C). Collagen content in the atria was also quantified using hydroxyproline assays. These measurements demonstrated that total collagen content was increased in the right (P < 0.001) and left (P < 0.001) atria of aged mice (Fig. 8D). Furthermore, frailty analysis illustrates that total collagen content in the right (P = 0.0002) and left (P < 0.001) atria was highly correlated with FI score (Fig. 8E). From these analyses it is clear that young and aged mice with similar FI scores have similar levels of atrial collagen content regardless of their substantial differences in chronological age.
(A) Representative images demonstrating patterns of interstitial collagen deposition (red colour) in the right atrium (RA) and left atrium (LA) of young and aged mice. (B) Summary data quantifying right and left atrial fibrosis (measured from histological images as in panel A); data analyzed using Student’s t-test; n = 5 young and 5 aged hearts. (C) Linear regression analysis of interstitial fibrosis in the right and left atria as a function of FI score; n = 10 mice. (D) Effects of age on total collagen content in the right and left atria by hydroxyproline assay. Data analyzed using Student’s t-test; n = 14 young and 15 aged mice. (E) Linear regression analysis of total collagen content in the right and left atria as function of FI score, n = 29 mice.
We next investigated the mRNA expression patterns of genes involved in the regulation of fibrosis in the atria of aged mice and determined how they correlate with frailty. To determine if active collagen production was enhanced we measured the mRNA expression of collagen type I and collagen type III, which are major interstitial collagens in the myocardium33, in the right and left atria (Supplemental Fig. S3). These data demonstrate that there were no differences in expression of collagen I or collagen III in the right or left atria between young and aged mice. Furthermore, there were no significant correlations between collagen I or collagen III and FI score in the right or left atria. We also measured the expression of TGFβ and CTGF, which are both importantly involved in the production of collagens in the heart34,35, in the atria of young and aged mice (Supplemental Fig. S3). These data show that there were no differences in atrial TFGβ expression whether analyzed by age or by FI score. There were also no differences in atrial CTGF expression in young vs. aged mice or when measured as a function of frailty. Thus, our data show that atrial fibrosis is enhanced in the atria of aged and frail mice, but suggest that this is not due to actively increased collagen production via increased gene transcription.
We next evaluated whether fibrosis in the atria was associated with changes in regulation of the extracellular matrix by matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs). MMPs are involved in the processing and degradation of collagen (and other extracellular matrix proteins) while TIMPs function to inhibit the activity of MMPs33,36,37,38,39.
We initially focused on MMP2 and MMP9 as these are key gelatinases in the heart that play an important role in the degradation of collagens38. When measured as a function of age, MMP2 expression was not changed in the right atrium (P = 0.38), but was reduced (P < 0.001) in the left atrium of aged mice (Supplemental Fig. S4A). MMP2 expression was also negatively correlated (P = 0.0001) with FI score in the left atrium (Supplemental Fig. S4B). MMP9 expression was increased (P = 0.005) in the right atrium of aged mice, but not changed (P = 0.103) in the left atrium (Supplemental Fig. S4C). Interestingly, when analyzed as a function of frailty, MMP9 was positively correlated (P = 0.03) with FI score in the right atrium, but negatively correlated (P = 0.05) with FI score in the left atrium (Supplemental Fig. S4D).
We also measured the expression of TIMP1–4 (Supplemental Fig. S5) in the right and left atria as a function of age and FI score. When measured according to age we found that TIMP1 was increased (P = 0.001) in the left atrium of aged mice, TIMP2 was decreased (P = 0.04) in the left atrium of aged mice, TIMP3 was decreased in the right (P = 0.05) and left (P = 0.01) atria of aged mice and TIMP4 was increased (P = 0.002) in the right atrium of aged mice. When measured as a function of frailty, TIMP1 was positively correlated (P = 0.0003) with FI score in the left atrium, TIMP3 was negatively correlated with FI score in the right (P = 0.03) and left (P = 0.001) atria and TIMP4 was positively correlated (P = 0.01) with FI score in the right atrium.
Remodelling of the extracellular matrix is importantly determined by the balance between MMP and TIMP activities; therefore, we quantified the ratios between expression of TIMPs and MMPs as a function of age and frailty. The mRNA expression rations of TIMPs1-4 to MMP2 are presented in Fig. 9. Key differences include: TIMP1/MMP2 expression was increased (P < 0.001) in the left atrium of aged mice and positively correlated (P = 0.0002) with FI score in the left atrium, TIMP2/MMP2 expression was increased (P = 0.007) in the left atrium of aged mice and positively correlated (P = 0.002) with FI score in the left atrium, TIMP3/MMP2 was increased (P = 0.05) in the left atrium of aged mice, and TIMP4/MMP2 was increased in the right (P = 0.002) and left (P = 0.003) atria of aged mice as well as positively correlated with FI score in the right (P = 0.0006) and left atria (P = 0.002). There was also a trend towards an increase in TIMP2/MMP2 in the right atrium both as a function of age (P = 0.07) and FI score (P = 0.09).
(A) Effects of age on the TIMP1/MMP2 mRNA expression ratio in the right (RA) and left (LA) atria. Data analyzed by Student’s t-test for the RA and Mann Whitney rank sum test for the LA; n = 8 young and 8 aged hearts. (B) Linear regression analysis illustrating correlations between the TIMP1/MMP2 expression ratio and FI score in the right and left atria; n = 16 hearts. (C) Effects of age on the TIMP2/MMP2 expression ratio in the right (RA) and left (LA) atria. Data analyzed by Student’s t-test for the RA and Mann Whitney rank sum test for the LA; n = 8 young and 8 aged hearts. (D) Linear regression analysis illustrating correlations between the TIMP2/MMP2 expression and FI score in the right and left atria; n = 16 hearts. (E) Effects of age on the TIMP3/MMP2 expression ratio in the right (RA) and left (LA) atria. Data analyzed by Student’s t-test; n = 8 young and 8 aged hearts. (F) Linear regression analysis illustrating correlations between the TIMP3/MMP2 expression ratio and FI score in the right and left atria; n = 16 hearts. (G) Effects of age on the TIMP4/MMP2 expression ratio in the right (RA) and left (LA) atria. Data analyzed by Mann Whitney rank sum test; n = 8 young and 8 aged hearts. (H) Linear regression analysis illustrating correlations between the TIMP4/MMP2 expression ratio and FI score in the right and left atria; n = 16 hearts.
The mRNA expression ratios of TIMPs1-4 to MMP9 are presented in Fig. 10. Key differences include: TIMP1/MMP9 expression was increased (P = 0.005) in the left atrium of aged mice and positively correlated (P = 0.002) with FI score in the left atrium while TIMP3/MMP9 expression was reduced (P = 0.007) in the right atrium of aged mice and negatively correlated (P = 0.02) with FI score in the right atrium. There was a trend towards a positive correlation (P = 0.06) between TIMP4/MMP9 expression and FI score in the left atrium. Collectively, these data demonstrate a number of examples of increases in TIMP expression relative to MMP expression, which could explain, at least in part, the increase in interstitial fibrosis in the atria of aged and frail hearts (see Discussion).
(A) Effects of age on the TIMP1/MMP9 mRNA expression ratio in the right (RA) and left (LA) atria. Data analyzed by Student’s t-test for the RA and Mann Whitney rank sum test for the LA; n = 8 young and 8 aged hearts. (B) Linear regression analysis illustrating correlations between the TIMP1/MMP9 expression ratio and FI score in the right and left atria; n = 16 hearts. (C) Effects of age on the TIMP2/MMP9 expression ratio in the right (RA) and left (LA) atria. Data analyzed by Mann Whitney rank sum test for the RA and Student’s t-test for the LA; n = 8 young and 8 aged hearts. (D) Linear regression analysis illustrating correlations between the TIMP2/MMP9 expression and FI score in the right and left atria; n = 16 hearts. (E) Effects of age on the TIMP3/MMP9 expression ratio in the right (RA) and left (LA) atria. Data analyzed by Mann Whitney rank sum test for the RA and Student’s t-test for the LA; n = 8 young and 8 aged hearts. (F) Linear regression analysis illustrating correlations between the TIMP3/MMP9 expression ratio and FI score in the right and left atria; n = 16 hearts. (G) Effects of age on the TIMP4/MMP9 expression ratio in the right (RA) and left (LA) atria. Data analyzed by Mann Whitney rank sum test; n = 8 young and 8 aged hearts. (H) Linear regression analysis illustrating correlations between the TIMP4/MMP9 expression ratio and FI score in the right and left atria; n = 16 hearts.
Discussion
We have investigated the impacts of age and frailty on atrial arrhythmogenesis as well as atrial structure and function. Our novel experiments demonstrate that aging is associated with electrophysiological alterations (i.e. changes in AP morphology) in the atria as well as enhanced atrial fibrosis. We further demonstrate that these changes are strongly correlated with and graded by FI score. These findings show that aging results in the creation of a substrate for atrial arrhythmias and that these changes are highly correlated with frailty. This indicates that the age-dependent development of a substrate for atrial arrhythmias is highly dependent on how successfully individuals age. Individuals that accumulated more health deficits, and that were therefore more frail, had more pronounced changes in atrial structure and function.
AF is well known to increase in incidence and severity (i.e. progression from paroxysmal to permanent AF) in the aged population7,40. Consistent with these clinical data we found that, although AF could be induced at similar rates in young vs. aged mice, the AF we observed in aged mice was substantially longer in duration compared to young mice. In fact, all AF observed in young mice was very brief, lasting much less than 5s before spontaneous reversion back to sinus rhythm. In contrast, when AF was induced in aged mice it was sustained (i.e. longer than 30s and up to minutes) in the majority of cases. Furthermore, we observed substantial rates of AV node block in aged mice, while young mice did not demonstrate any AV node block. These data clearly demonstrate that aged mice show a susceptibility to more sustained, longer lasting AF compared to young mice. Using our novel FI tool we also observed a clear difference in frailty (i.e. health status) in mice that were induced into AF, whereby the aged mice that demonstrated sustained AF had higher FI scores than the young mice that only exhibited brief episodes of AF. This indicates that sustained AF was associated with an increase in frailty.
Consistent with the increased duration of AF and occurrence of AV node block, we found that P wave duration (a measure of atrial conduction time) and PR interval (a measure of conduction through the AV node) were prolonged in aged mice in baseline conditions as well as after autonomic nervous system blockade. Interestingly, both measures showed substantial variability within age groups, particularly in the aged mice. This heteroscedasticity (i.e. increasing variability in the aged mice) in measures of atrial and AV node conduction is in agreement with the concept that not all individuals age at the same rate. In support of this, we assessed frailty in our young and aged mice and found that animals of the same chronological age can have very different FI scores. Strikingly, P wave duration and PR interval were highly correlated with FI score, regardless of chronological age. In fact, scrutiny of our data reveals that young and aged mice could have very similar P wave and PR interval durations when they had similar FI scores. Thus, these measures of atrial and AV node conduction fall along a continuum according to FI score, regardless of their similarities or differences in chronological age. This is consistent with the observation that FI scores in young and aged mice could overlap in some cases. Collectively, these analyses demonstrate that we were able to detect differences in health status (based on FI score) in young and aged mice and frailty is a strong predictor of these measures of atrial and AV node conduction. The results of these experiments are important because P wave duration and PR interval are strong predictors of susceptibility and severity of AF, including in aging populations30,31,41,42. Consistent with this idea, we found that when AF was induced in our study, the duration of AF was highly correlated with P wave duration and PR interval. This suggests that quantifying frailty could be a powerful approach to predicting alterations in atrial electrophysiology and the severity of AF. It should be noted that our measurements of atrial electrophysiology were made in anesthetized mice. Our data demonstrate that atrial electrophysiology (P wave duration, PR interval) was correlated with FI score at baseline and in the presence of autonomic blockade indicating that these changes are intrinsic to the atria. Nevertheless, future studies in conscious, freely moving mice, where heart rate would be expected to be higher in the absence of anesthetics, will be important.
A major advantage of our frailty approach in mice is that it enabled us to investigate the cellular and molecular mechanisms for frailty-related changes in atrial function. We used high resolution optical mapping to study the effects of age and frailty on atrial conduction patterns. These experiments clearly demonstrate that conduction is slowed throughout the atria in aged and frail hearts. Specifically, we found that local CV in the right and left atria was reduced in aged mice; however, as was the case in our in vivo studies, we observed substantial variability in atrial CV, especially in the aged mice, further suggesting that factors other than chronological age affect atrial CV. Indeed, we found that CV in the right and left atria was strongly negatively correlated with FI score whereby atrial CV was graded with frailty regardless of chronological age. We also measured optical APs in the right and left atria. As expected, APs in the right atrium were longer, on average, than the left atrium43. When measured as a function of age, we were able to detect reductions in APD90, but not APD50 in aged mice. Once again, there was a high degree of variability in these measurements, particularly in the aged mice. Interestingly, right atrial APD50, right atrial APD90 and left atrial APD90 were all negatively correlated with FI score. Thus, frailty was a strong predictor of changes in APD and, in some cases, was better able to identify changes than chronological age.
Reductions in atrial CV and APD can both increase the susceptibility to AF by shortening the wavelength of re-entry and creating a substrate for arrhythmia4,44. Our findings that atrial CVs and APDs are correlated with frailty is consistent with the observation that the AF we observed in aged, frail mice was longer (i.e. sustained) than younger, less frail mice. The effects of age on APD have been measured in prior studies with mixed results45. For example, prior investigations in aged dogs have reported that in the right atrium the AP is shorter in early repolarization but that APD90 is prolonged46,47. Studies in aged rabbits reported no change in APD10, but a prolongation of APD9048. In aged rats it has been reported that the right atrial AP is prolonged while the left atrial AP is shortened49 indicating that there may be regional differences in atrial electrophysiology during aging. Our studies in mice support the conclusion that APs are shortened in the right and left atria during aging, which is in agreement with studies showing that AP duration is shortened in persistent AF in humans50,51. Consistent with this idea prior studies have also reported that L-type Ca2+ currents are decreased while transient outward K+ currents are increased in aged atrial myocytes45,52. We have not investigated the specific ionic currents responsible for the changes APD we have observed in the present study. It will be important to consider this, as well as whether any changes in ion channel function correlate with FI score, in future studies. It will also be important to investigate whether aging and frailty are associated with changes in expression or function of connexins in the atria since gap junctions are important determinants of CV53 and mutations that impair gap junction function have previously been linked to AF54,55. Collectively, our data demonstrate that aging results in electrical remodelling in the atria that creates a substrate for AF to occur and that frailty is powerful predictor of these changes regardless of chronological age.
We also investigated whether differences in atrial arrhythmogenesis and electrophysiology were associated with changes in fibrosis. We observed an increase in right and left atrial fibrosis (based on histological assessments as well as measures of total collagen content) in aged mice, an observation that is consistent with prior studies47,56 and clinical data from human patients57. Importantly, we found that enhanced fibrosis in the right and left atria was highly correlated with FI score indicating that health status is a strong predictor of structural remodeling in the atria during the aging process. Structural remodeling is an important contributor to the slowing of conduction in the heart because enhanced collagen deposition can interfere with electrical conduction58,59. This is now thought to be a major contributor to the substrate for AF4,57. Our finding that structural remodeling is enhanced in frail hearts is consistent with our observations that atrial conduction velocities and duration of AF are also correlated with FI score.
The mechanisms leading to atrial structural remodeling during aging are not well understood. Initially, we investigated whether active collagen production, in association with increased gene expression, was altered as a function of age or frailty. We observed no differences in expression of collagens or profibrotic proteins such as TGFβ or CTGF34, whether analyzed by chronological age or by frailty. This suggests that enhanced atrial fibrosis in aged and frail hearts is not due to actively enhanced collagen production, which is consistent with prior investigations60. We also studied whether atrial fibrosis was associated with changes in atrial gene expression of MMPs and TIMPs, which play critical roles in maintenance and remodelling of the extracellular matrix33,37,38,39. Prior studies have shown that circulating levels of MMPs and TIMPs are altered in aging61, but few studies have assessed cardiac specific expression. Accordingly, we measured the mRNA expression of MMPs and TIMPs in the right and left atria and analyzed these data as a function of age and frailty. We observed differences in atrial expression of MMP2 and MMP9, which both play a role in the degradation of interstitial collagen33, as a function of age and frailty. Similarly, TIMPs 1, 3 and 4, but not TIMP2, showed expression changes in aged and/or frail hearts. These findings strongly support the hypothesis that atrial fibrosis in aged and frail hearts is at least partially due to changes in extracellular matrix remodelling by MMPs and TIMPs.
Remodeling of the extracellular matrix is dependent on the balance between MMP and TIMP activity33; therefore, we quantified the ratios of TIMPs1-4 to MMP2 and MMP9 in the atria as a function of chronological age and frailty. This approach revealed several important differences. Specifically, TIMP1/MMP2 and TIMP2/MMP2 were both increased in the left atrium (but not the right atrium) of aged and frail hearts. There was also a trend towards an increase in the TIMP2/MMP2 ratio in the right atrium of aged and frail hearts. TIMP4/MMP2 was clearly increased in the right and left atria as a function of age and frailty. We also observed increases in the TIMP1/MMP9 ratio in the left atrium of aged and frail hearts while TIMP3/MMP9 was reduced in the right atrium as a function of age and frailty. Collectively, these findings strongly support the emerging hypothesis that fibrosis in the aging heart is associated with changes in extracellular matrix remodelling by MMPs and TIMPs rather than increases in active collagen deposition60. Our observation that atrial fibrosis in aged and frail hearts is associated with changes in the balance between TIMP and MMP expression is consistent with prior studies of aging in the sinoatrial node19 and ventricular myocardium22,60,62,63. Increases in the expression ratio of TIMP to MMP, of which we observed several examples, would be expected to reduce MMP activity and could at least partially explain the increases in fibrosis and collagen content that we observed.
Our studies of regulators of the extracellular matrix focused on patterns of gene expression. It is important to note that gene expression is only one aspect of how these proteins may regulate the extracellular matrix, including during the aging process. These proteins, including TGFβ, CTGF, MMPs and TIMPs are regulated in complex ways35,38 and it is conceivable that the function of a number of these proteins may be altered as a function of age and/or frailty independently of changes (or lack thereof) in gene expression. Similarly, while we have identified changes in expression patterns for several MMPs and TIMPs that are consistent with the enhanced fibrosis we have observed in the atria of aged and frail mice, it will be important to follow up on these studies with measurements of collagenase and gelatinase activity to further investigate the roles of MMPs and TIMPs in aging related remodelling of the extracellular matrix and fibrosis. While changes in expression ratios between TIMPs and MMPs are indicative of a change in extracellular matrix degradation19,22 it must be recognized that all TIMPs can inhibit a large number of MMPs and that a number of MMPs are expressed in the heart38. Thus, in summary, our findings demonstrate that aged and frail hearts are characterized by enhanced atrial fibrosis and that MMPs and TIMPs are importantly involved in this process; however, this is a complex area of study and additional experiments will be required to better understand how MMPs and TIMPs regulate the extracellular matrix in the atria as a function of age and frailty as well as the links between atrial fibrosis and AF.
Our finding that frailty is powerful predictor of atrial structure, function and arrhythmogenesis has important clinical implications. For example, the patients that are enrolled in clinical trials are typically highly selected and are at a lower risk for adverse outcomes than patients from routine practice, potentially impacting the conclusions of trials7. In agreement with this, trials of oral anticoagulants for the prevention of stroke in elderly patients with AF have been criticised for not properly representing frail patients64. Our work demonstrates conclusively that frailty enables us to detect differences in health status regardless of chronological age and that structural and electrical changes in the atria that create a substrate for AF are strongly correlated with FI score.
Many common forms of cardiovascular disease (i.e. hypertension, hypertrophy, heart failure) occur preferentially in aged populations and many of these diseases also create a substrate for AF. Thus it is likely that both aging and concurrent cardiovascular disease can both contribute to the creation of a substrate for AF; however, as we have shown, the effects of aging on atrial structure and function are heterogeneous and highly related to an individual’s health status. This suggests that quantifying frailty, as can be done using an FI, can provide powerful insight into the degree of atrial remodelling in individual patients, which will have important implications for understanding a patient’s likelihood of developing AF. Accordingly, frailty should be an important consideration when treating elderly patients with AF and/or common forms of cardiovascular disease and when designing and interpreting therapeutic interventions for AF in aged populations.
In conclusion, the incidence and severity of AF increases with age and this represents a major clinical challenge. We have studied the effects of age on atrial structure, function and arrhythmogenesis and utilized a FI to determine how health status of individuals impacts atrial function. We demonstrate that aged mice exhibit electrical and structural remodelling in the atria, both of which could contribute to the creation a substrate for AF to occur. Furthermore, our novel approach to quantifying frailty enabled us to demonstrate that frailty is highly associated with changes in atrial function, including at the cellular and molecular levels. Specifically, we found that all changes in atrial electrophysiology and fibrosis were graded by FI score indicating that mice of the same chronological age have measureable differences in health status that have profound impacts on atrial physiology. Our studies further demonstrate that frailty manifests at the molecular level and that these changes correlate with alterations in atrial electrophysiology and arrhythmogenesis in the intact organism. Given that many common cardiovascular diseases, including AF, occur in aged populations, our findings have important implications for understanding the mechanisms of diseases in the elderly and suggest that frailty can be used to better understand the health status of similarly aged populations, which may have important implications for treatments strategies.
Additional Information
How to cite this article: Jansen, H. J. et al. Atrial structure, function and arrhythmogenesis in aged and frail mice. Sci. Rep. 7, 44336; doi: 10.1038/srep44336 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
McManus, D. D., Rienstra, M. & Benjamin, E. J. An update on the prognosis of patients with atrial fibrillation. Circulation 126, e143–6 (2012).
Lloyd-Jones, D. M. et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation 110, 1042–6 (2004).
Caldeira, D., David, C. & Sampaio, C. Rate versus rhythm control in atrial fibrillation and clinical outcomes: updated systematic review and meta-analysis of randomized controlled trials. Arch Cardiovasc Dis 105, 226–38 (2012).
Heijman, J., Voigt, N., Nattel, S. & Dobrev, D. Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circ Res 114, 1483–99 (2014).
Benjamin, E. J. et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 98, 946–52 (1998).
Mirza, M., Strunets, A., Shen, W. K. & Jahangir, A. Mechanisms of arrhythmias and conduction disorders in older adults. Clin Geriatr Med 28, 555–73 (2012).
Chiang, C. E. et al. Distribution and risk profile of paroxysmal, persistent, and permanent atrial fibrillation in routine clinical practice: insight from the real-life global survey evaluating patients with atrial fibrillation international registry. Circ Arrhythm Electrophysiol 5, 632–9 (2012).
Rockwood, K. & Mitnitski, A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 62, 722–7 (2007).
Mitnitski, A. B., Mogilner, A. J. & Rockwood, K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 1, 323–36 (2001).
Clegg, A., Young, J., Iliffe, S., Rikkert, M. O. & Rockwood, K. Frailty in elderly people. Lancet 381, 752–62 (2013).
Searle, S. D., Mitnitski, A., Gahbauer, E. A., Gill, T. M. & Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr 8, 24 (2008).
McNallan, S. M. et al. Measuring frailty in heart failure: a community perspective. Am Heart J 166, 768–74 (2013).
Singh, M., Stewart, R. & White, H. Importance of frailty in patients with cardiovascular disease. Eur Heart J 35, 1726–31 (2014).
Forman, D. E. & Alexander, K. P. Frailty: A Vital Sign for Older Adults With Cardiovascular Disease. Can J Cardiol 32, 1082–7 (2016).
Whitehead, J. C. et al. A Clinical Frailty Index in Aging Mice: Comparisons With Frailty Index Data in Humans. J Gerontol A Biol Sci Med Sci (2013).
Feridooni, H. A., Sun, M. H., Rockwood, K. & Howlett, S. E. Reliability of a Frailty Index Based on the Clinical Assessment of Health Deficits in Male C57BL/6J Mice. J Gerontol A Biol Sci Med Sci 70, 686–93 (2015).
Howlett, S. E. Assessment of Frailty in Animal Models. Interdiscip Top Gerontol Geriatr 41, 15–25 (2015).
Parks, R. J. et al. A procedure for creating a frailty index based on deficit accumulation in aging mice. J Gerontol A Biol Sci Med Sci 67, 217–27 (2012).
Moghtadaei, M. et al. The impacts of age and frailty on heart rate and sinoatrial node function. J Physiol 594, 7105–26 (2016).
Cho, H. C. Age is just a number: frailty better evaluates age-dependent heart rhythm defects. J Physiol 594, 6805 (2016).
Rockwood, K. & Mitnitski, A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med 27, 17–26 (2011).
Sangaralingham, S. J. et al. Cardiorenal fibrosis and dysfunction in aging: Imbalance in mediators and regulators of collagen. Peptides 76, 108–14 (2016).
Egom, E. E. et al. Impaired sinoatrial node function and increased susceptibility to atrial fibrillation in mice lacking natriuretic peptide receptor C. J Physiol 593, 1127–46 (2015).
Krishnaswamy, P. S. et al. Altered parasympathetic nervous system regulation of the sinoatrial node in Akita diabetic mice. J Mol Cell Cardiol 82, 125–35 (2015).
Hua, R. et al. Effects of Wild-Type and Mutant Forms of Atrial Natriuretic Peptide on Atrial Electrophysiology and Arrhythmogenesis. Circ Arrhythm Electrophysiol 8, 1240–54 (2015).
Azer, J., Hua, R., Krishnaswamy, P. S. & Rose, R. A. Effects of natriuretic peptides on electrical conduction in the sinoatrial node and atrial myocardium of the heart. J Physiol 592, 1025–45 (2014).
Springer, J. et al. The natriuretic peptides BNP and CNP increase heart rate and electrical conduction by stimulating ionic currents in the sinoatrial node and atrial myocardium following activation of guanylyl cyclase-linked natriuretic peptide receptors. J Mol Cell Cardiol 52, 1122–34 (2012).
Hua, R., Adamczyk, A., Robbins, C., Ray, G. & Rose, R. A. Distinct patterns of constitutive phosphodiesterase activity in mouse sinoatrial node and atrial myocardium. PLoS One 7, e47652 (2012).
Rose, R. A., Kabir, M. G. & Backx, P. H. Altered heart rate and sinoatrial node function in mice lacking the cAMP regulator phosphoinositide 3-kinase-gamma. Circ Res 101, 1274–82 (2007).
Censi, F. et al. P-wave Variability and Atrial Fibrillation. Sci Rep 6, 26799 (2016).
Magnani, J. W. et al. Electrocardiographic PR interval and adverse outcomes in older adults: the Health, Aging, and Body Composition study. Circ Arrhythm Electrophysiol 6, 84–90 (2013).
Miragoli, M. & Glukhov, A. V. Atrial Fibrillation and Fibrosis: Beyond the Cardiomyocyte Centric View. Biomed Res Int 2015, 798768 (2015).
Kassiri, Z. & Khokha, R. Myocardial extra-cellular matrix and its regulation by metalloproteinases and their inhibitors. Thromb Haemost 93, 212–9 (2005).
Thannickal, V. J., Zhou, Y., Gaggar, A. & Duncan, S. R. Fibrosis: ultimate and proximate causes. J Clin Invest 124, 4673–7 (2014).
Leask, A. Getting to the heart of the matter: new insights into cardiac fibrosis. Circ Res 116, 1269–76 (2015).
Spinale, F. G. Matrix metalloproteinases: regulation and dysregulation in the failing heart. Circ Res 90, 520–30 (2002).
Spinale, F. G. Myocardial matrix remodeling and the matrix metalloproteinases: influence on cardiac form and function. Physiol Rev 87, 1285–342 (2007).
Takawale, A., Sakamuri, S. S. & Kassiri, Z. Extracellular matrix communication and turnover in cardiac physiology and pathology. Compr Physiol 5, 687–719 (2015).
Fan, D. et al. Differential role of TIMP2 and TIMP3 in cardiac hypertrophy, fibrosis, and diastolic dysfunction. Cardiovasc Res 103, 268–80 (2014).
Monfredi, O. & Boyett, M. R. Sick sinus syndrome and atrial fibrillation in older persons - A view from the sinoatrial nodal myocyte. J Mol Cell Cardiol 83, 88–100 (2015).
Guidera, S. A. & Steinberg, J. S. The signal-averaged P wave duration: a rapid and noninvasive marker of risk of atrial fibrillation. J Am Coll Cardiol 21, 1645–51 (1993).
Park, J. et al. Prolonged PR interval predicts clinical recurrence of atrial fibrillation after catheter ablation. J Am Heart Assoc 3, e001277 (2014).
Lomax, A. E., Kondo, C. S. & Giles, W. R. Comparison of time- and voltage-dependent K+ currents in myocytes from left and right atria of adult mice. Am J Physiol Heart Circ Physiol 285, H1837–48 (2003).
Nattel, S. New ideas about atrial fibrillation 50 years on. Nature 415, 219–26 (2002).
Dun, W. & Boyden, P. A. Aged atria: electrical remodeling conducive to atrial fibrillation. J Interv Card Electrophysiol 25, 9–18 (2009).
Anyukhovsky, E. P. et al. Age-associated changes in electrophysiologic remodeling: a potential contributor to initiation of atrial fibrillation. Cardiovasc Res 66, 353–63 (2005).
Anyukhovsky, E. P. et al. Cellular electrophysiologic properties of old canine atria provide a substrate for arrhythmogenesis. Cardiovasc Res 54, 462–9 (2002).
Toda, N. Age-related changes in the transmembrane potential of isolated rabbit sino-atrial nodes and atria. Cardiovasc Res 14, 58–63 (1980).
Huang, C., Ding, W., Li, L. & Zhao, D. Differences in the aging-associated trends of the monophasic action potential duration and effective refractory period of the right and left atria of the rat. Circ J 70, 352–7 (2006).
Van Wagoner, D. R. et al. Atrial L-type Ca2+ currents and human atrial fibrillation. Circ Res 85, 428–36 (1999).
Van Wagoner, D. R. & Nerbonne, J. M. Molecular basis of electrical remodeling in atrial fibrillation. J Mol Cell Cardiol 32, 1101–17 (2000).
Dun, W., Yagi, T., Rosen, M. R. & Boyden, P. A. Calcium and potassium currents in cells from adult and aged canine right atria. Cardiovasc Res 58, 526–34 (2003).
Jansen, J. A., van Veen, T. A., de Bakker, J. M. & van Rijen, H. V. Cardiac connexins and impulse propagation. J Mol Cell Cardiol 48, 76–82 (2010).
Gollob, M. H. et al. Somatic mutations in the connexin 40 gene (GJA5) in atrial fibrillation. N Engl J Med 354, 2677–88 (2006).
Thibodeau, I. L. et al. Paradigm of genetic mosaicism and lone atrial fibrillation: physiological characterization of a connexin 43-deletion mutant identified from atrial tissue. Circulation 122, 236–44 (2010).
Kumar, S. et al. Atrial remodeling in varying clinical substrates within beating human hearts: relevance to atrial fibrillation. Prog Biophys Mol Biol 110, 278–94 (2012).
Dzeshka, M. S., Lip, G. Y., Snezhitskiy, V. & Shantsila, E. Cardiac Fibrosis in Patients With Atrial Fibrillation: Mechanisms and Clinical Implications. J Am Coll Cardiol 66, 943–59 (2015).
Wolf, R. M. et al. Atrial fibrillation and sinus node dysfunction in human ankyrin-B syndrome: a computational analysis. Am J Physiol Heart Circ Physiol 304, H1253–66 (2013).
Rohr, S. Myofibroblasts in diseased hearts: new players in cardiac arrhythmias? Heart Rhythm 6, 848–56 (2009).
Horn, M. A. & Trafford, A. W. Aging and the cardiac collagen matrix: Novel mediators of fibrotic remodelling. J Mol Cell Cardiol 93, 175–85 (2016).
Bonnema, D. D. et al. Effects of age on plasma matrix metalloproteinases (MMPs) and tissue inhibitor of metalloproteinases (TIMPs). J Card Fail 13, 530–40 (2007).
Sangaralingham, S. J. et al. The aging heart, myocardial fibrosis, and its relationship to circulating C-type natriuretic Peptide. Hypertension 57, 201–7 (2011).
Horn, M. A. et al. Age-related divergent remodeling of the cardiac extracellular matrix in heart failure: collagen accumulation in the young and loss in the aged. J Mol Cell Cardiol 53, 82–90 (2012).
Stollberger, C. & Finsterer, J. Concerns about the use of new oral anticoagulants for stroke prevention in elderly patients with atrial fibrillation. Drugs Aging 30, 949–58 (2013).
Acknowledgements
This work was supported by operating grants from the Canadian Institutes of Health Research to R.A.R (MOP 93718, 142486) and S.E.H (MOP 126018). R.A.R. holds a New Investigator Award from the Heart and Stroke Foundation of Canada. H.J.J. is the recipient of a Nova Scotia Graduate Scholarship and a Dalhousie Medical Research Foundation MacDonald Graduate Scholarship.
Author information
Authors and Affiliations
Contributions
The conception of the research was by S.E.H and R.A.R. The design of the experiments was by M.M., H.J.J., S.E.H. and R.A.R. The collection, analysis and interpretation of the data was by M.M., H.J.J., M.M., S.A.R. O.B. J.L.S., S.E.H. and R.A.R. Drafting the article or revising it critically for important intellectual content was done by M.M., H.J.J., M.M., S.A.R. J.L.S., S.E.H. and R.A.R. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Jansen, H., Moghtadaei, M., Mackasey, M. et al. Atrial structure, function and arrhythmogenesis in aged and frail mice. Sci Rep 7, 44336 (2017). https://doi.org/10.1038/srep44336
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep44336
This article is cited by
-
The interplay of senescence and MMPs in myocardial infarction: implications for cardiac aging and therapeutics
Biogerontology (2025)
-
Comprehensive longitudinal non-invasive quantification of healthspan and frailty in a large cohort (n = 546) of geriatric C57BL/6 J mice
GeroScience (2023)
-
Epigenetic age is associated with baseline and 3-year change in frailty in the Canadian Longitudinal Study on Aging
Clinical Epigenetics (2021)
-
The degree of frailty as a translational measure of health in aging
Nature Aging (2021)
-
Age, Sex and Overall Health, Measured As Frailty, Modify Myofilament Proteins in Hearts From Naturally Aging Mice
Scientific Reports (2020)