Abstract
Objectives
New tools aid in the diagnosis of diseases and thus help in advancing patient care. “Fractal Analysis” is a versatile method of applying nontraditional mathematics to patterns that are beyond understanding with traditional Euclidean concepts. This analysis can be used on radiographic and non-radiographic images in dentistry. In this review we aim to identify the usefulness of fractal analysis in dentistry in radiographic images, its applications and future scope.
Materials and Methods
Articles published between 1992 and 2024 were retrieved through an electronic search of Medline via PubMed, Scopus, and Google Scholar databases. The search, which was limited to articles published in English, aimed to identify relevant studies by employing the following keywords: “fractal analysis,” “dental radiographs,” “mandibular,” “panoramic radiographs,” and “radiography.” Ultimately, 76 articles that addressed the application of fractal analysis in dental radiographs were selected.
Results
Fractal analysis can reveal alterations in bone and in images of morphologically altered tissue, however no set values exist which could be used as a standard for diagnosing various conditions.
Conclusion
Fractal Analysis can potentially be used as an adjunct to diagnostic tests as it is shown to identify alterations in bony and trabeculae patterns.
Similar content being viewed by others
Introduction
The world is rapidly progressing towards a period of almost complete digitalization, marked by significant transformations across various domains. Technological advancements persist at an accelerated rate, signifying a transformative phase in healthcare developments. Robotics, artificial intelligence, and progress in machinery have significantly enhanced the quality of care available to patients. One such advancement is “Fractal Analysis,” a concept that has existed for over 30 years but is being gradually and steadily implemented in the domains of medicine and dentistry [1]. Fractal analysis (FA) represents an innovative and adaptable approach to employing non-traditional mathematical concepts to patterns that are challenging to comprehend using conventional Euclidean frameworks. This domain was established to characterize computer-generated fractals; however, fractals are not exclusively limited to computer-generated imagery. Instead, Euclidean geometry is evident in commonplace objects such as oranges and watermelons, while fractal geometry is discernible in familiar forms including undulating coastlines, expanding crystals, and spiral galaxies [2, 3]. Within the human body, the most prominent fractal structures are observed in coronary vessels, Purkinje fibers in the heart, the lungs, neurons, trabeculae in bone, and blood vessels in the eye [3]. Benoit Mandelbrot is regarded as the father of contemporary fractal analysis; he disseminated the notion of fractals in his publication, “How Long Is the Coast of Britain? Statistical Self-Similarity and Fractional Dimension” [4], which appeared in 1967. This analysis has been utilized in various applications, including heart rate assessment, diagnostic imaging, cancer research [5], fractal analysis of complex networks, categorization of histopathology slides in medical contexts, evaluation of fractal landscapes or coastline complexity [1], electrical engineering, enzyme/enzymology (particularly in relation to Michaelis-Menten kinetics), the creation of novel music, the production of diverse art forms, signal and image compression, urban development, neuroscience, pathology, geology, geography, archaeology, seismology, soil studies [6], as well as the design of computer and video games, especially in the context of computer graphics for organic environments and as an element of procedural generation [7, 8].
In dental diagnosis, radiographs are an essential adjuvant. To help with precise clinical evaluation, a variety of imaging techniques are frequently used, including intraoral periapical radiographs (IOPA), orthopantomograms (OPG), and cone-beam computed tomography (CBCT). Tools that can objectively identify changes in bone density and trabecular patterns are becoming more and more important as a result of the quick development of dental technology. Particularly in situations involving bone pathology, periodontal disease and systemic diseases affecting the bone. These tools provide invaluable assistance in early diagnosis and treatment planning thereby reducing the load on the radiologist. In this review, we seek to examine the diverse applications of fractal analysis in dentistry using radiographic images and the results of these applications.
Materials and Methods
This review was based on the question: How common is the application of fractal analysis in dental radiographs and how useful is it? A literature search was performed in PubMed/MEDLINE, Ovid, LILACS, Web of Science and Google Scholar for all the published articles related to fractal analysis and its applications in dentistry. The last search was performed on March 10th, 2024.
The following search terms were used: “radiology” “fractal analysis” “dentistry” “periodontitis” “dental materials” “osteomyelitis” “implants” “dental caries” “root canals” “tmj dysfunction” “bruxism” “oral cancer” “salivary gland disorders”. Publications in English were included. Publications in other languages were excluded. Randomized and nonrandomized trials, cross-sectional studies, cohort, case-control studies, and systematic and literature reviews were included for data collection. The Grey Matters & Google scholar was also searched for relevant articles. The cross-reference of all studies was searched to include anything relevant to the topic. All studies that did not refer to the application of fractal analysis in dentistry were excluded. The total of all the results (3023 articles) was compiled in the Mendeley reference manager (v 2.85.0), and duplicates were removed. After removing the duplicates, 209 articles were included, and 76 articles were included for full-text screening. The data collected were reviewed by all the authors. Any disagreements were mutually discussed between the two reviewers (YC & LC), and a consensus was reached. A 3rd reviewer further reviewed the articles selected for analysis -Fig. 1. All the data related to the applications of fractal analysis in dental radiology were analyzed and reported
Results and Discussion
The capacity of fractal geometry to quantify and analyze the irregular, fragmented forms of natural objects that are not amenable to measurement by conventional mathematical methods has resulted in the widespread adoption of fractal analysis across various disciplines, particularly in the medical domain, where fractal structures are prevalent [2, 3, 9]. The mandibular bone, characterized by its branching trabeculae, demonstrates statistical self-similarity. Consequently, the utilization of fractal geometry and the quantification of fractal dimensions (FD) can facilitate the assessment of the complexity inherent in the trabecular pattern and bone architecture [10]. Several prevalent applications where FA has demonstrated its utility include quantifying trabecular alterations following surgical and orthodontic interventions, assessing the surface roughness of implants, and evaluating the healing of periapical lesions subsequent to root canal therapy. Pictorial fractal analysis is likewise employed to assess histopathological specimens of premalignant and malignant tissue [9, 11]. Nevertheless, a more prevalent utilization of FA in dentistry involves the assessment of radiographic images to track alterations in the morphological configurations of the jawbones. Numerous investigations have been conducted primarily to examine the trabecular architecture of the mandible through the utilization of intraoral periapical radiographs, panoramic radiographs, and CBCT images. The most prevalent technique in fractal analysis is the box counting method developed by White and Rudolph for the processing of dental images [12]. Figure 2 depicts the applications of fractal analysis in various areas of dentistry.
Osteoporosis detection
Osteoporosis is a global health issue marked by low bone mass and weakened bone structure, leading to a higher risk of fractures. Dental radiographs, commonly used in dental checkups, help in assessing bone conditions due to their accessibility, affordability, and low radiation exposure, making them an effective screening tool for osteoporosis risk. Research by Southard et al., focused on fractal analysis in osteoporotic subjects [13,14,15,16]. They first examined the link between fractal dimensions (FD) in the jawbone and bone density in rabbits with induced osteoporosis, findings showed reduced FD with higher steroid doses but no correlation with spine and mandible density [16]. In healthy women, FD in the jawbone was positively linked to local bone density but not to other areas like the spine [14]. Other studies, including those by Bollen et al. [17], and Park et al. [18], found higher FD values in panoramic and periapical radiographs of osteoporotic patients. Yasar & Akgunlu [19,20,21] carried out a series of studies, first on digital periapical images and then on panoramic images, they meticulously evaluated if fractal dimensions could be considered to detect osteoporosis and could differentiate the lacunarity and trabecular pattern of the mandible. They found a mean value of FD in osteoporotic subjects as 1.40 and 1.39 in non-osteoporotic subjects. Thereby confirming the usefulness of FD in detection of osteoporotic bone. Sindeaux et al. [22], evaluated 133 panoramic radiographs of 84 females and 49 males and they considered bone mineral density (BMD) values determined by dual-energy X-ray absorptiometry (DXA) as the gold standard. They found lower FD values in mandibular bone among postmenopausal women (normal = 1.420 ± 0.079, osteoporotic= 1.354 ± 0.090) and older men with osteoporosis (normal=1.373 ± 0.069, osteoporotic=1.371 ± 0.059). Their results suggested that cortical bone measurements could help identify patients need for further testing for bone density, however the results showed that FD values were not consistent over various regions. Table 1 summarizes all the studies done using fractal analysis to detect osteoporosis.
Periodontitis detection
Periodontitis is a chronic inflammatory disease that damages the tissues supporting teeth such as gingiva and bone. Detecting periodontitis involves clinical examination, gingival recession, through probing and radiographic assessment. Traditional radiographs often fail to depict radiographic changes until 30 to 50 percent of the bone is lost [23]. To effectively identify chronic periodontitis in its early stages, thorough examinations and evaluations are necessary. Many studies evaluating fractal dimensions of bone in periodontitis patients show lower FD values compared to healthy subjects or those with gingivitis [23,24,25,26,27,28,29,30,31]. Although various methodologies were used, these studies suggest that FD might help in diagnosing periodontitis, yet it is not applicable for clinical use and requires further validation. Efforts have also been made to model periodontal disease using various quantitative parameters like plaque levels or hormonal factors, but predicting bone loss remains challenging due to multiple influencing factors [23, 27, 32]. One study by Shrout et al., found that FD values were significantly lower in patients with periodontitis(mean fractal value = 2.049) compared to healthy individuals(mean fractal value = 2.061), confirming its potential as an objective detection method [33]. Other research indicated that FD effectively discriminates between healthy gingiva (1.74 ± 0.083), moderate periodontitis(1.66 ± 0.104) and severe periodontitis(1.64 ± 0.095), supporting its use for monitoring changes in bone structure [24]. Moreover, another study illustrated that FD values decrease as periodontitis stages increase, showing a strong negative correlation between FD and bone loss [30]. These studies showed that FD can serve as a quantitative tool for assessing changes in cancellous bone associated with periodontitis. Table 2 summarizes all the studies done using fractal analysis to detect periodontitis.
Root Canal Treatment (RCT) -healing and monitoring
Fractal analysis, particularly fractal dimension (FD), is important in root canal treatment to assess bone healing and treatment success. It provides a numerical value that describes the complexity of trabecular bone architecture, allowing for the quantification of bone regeneration and inflammation. Yu YY et al. [34], studied FD changes in periapical lesions after root canal treatment using digitized images from intraoral radiographs before and after treatment at different time points. They found a significant increase in FD after three months of successful treatment ranging from 1.720 to 1.580. Aydin et al. [35], compared FD changes in healthy individuals and type 2 diabetes mellitus patients after root canal treatment. They found increased FD values one-year post-treatment in both groups, with a more significant increase in the healthy group (0.274 ± 0.082) than in the group with diabetes mellitus (0.180 ± 0.114). Both these studies evaluated periapical radiographs. However,Yen YY et al carried out mathematical morphology analysis that increased the specificity of the fractal values. Tosun et al. [36], examined the changes in FD in patients undergoing nonsurgical endodontic retreatment. Increased FD was noted in healed cases (baseline=1.191 ± 0.022; postop=1.308 ± 0.094), while it decreased in unhealed cases (baseline=1.201 ± 0.023; postop=1.148 ± 0.078). These studies showed that changes in the FD values can depict pre and post treatment bony changes. Table 3 summarizes various studies done using fractal analysis for healing and treatment monitoring of bone after a root canal.
Implant evaluation
Bone quality is crucial for achieving osseointegration, which determines the stability and success of a dental implant. Proper bone regeneration around the implant ensures long-term load-bearing capacity and functional integration. Wilding et al. [37], studied fractal analysis to track bone healing after dental implants in 18 patients. They found that the bone structure changed significantly around the implant. Traini et al. [38], used fractal analysis to examine how the distance between implants affected blood vessel organization in bone, concluding that a 3 mm distance was better for vascular density than a 2 mm distance. Grizon et al. [39], utilized FD to assess the surface characteristics of titanium implants, suggesting that fractal analysis can evaluate mechanical compatibility. Yi et al. [40], introduced a method to assess bone mechanical properties using FD values from radiographs taken at different angles to create a map of the trabecular structure’s anisotropy. Mundim et al. [41], used periapical radiographs to analyze the bone texture in dental implant planning. They stated that fractal analysis could reliably predict implant stability. Lang et al. [42], researched whether fractal analysis could differentiate between healthy and diseased peri-implant bone and found contrasting results where he stated FD was not a valid distinguishing method. Cansu Kis et al. [43], evaluated microstructural changes around short implants using fractal analysis, concluding it could help predict implant survival based on the trabecular bone’s structure. Mishra et al. [44], also conducted a scoping review on FD in dental radiographs, they noted that most of the studies were done using periapical radiographs, followed by panoramic radiographs. They mentioned that while cone beam computed tomography (CBCT) provides a more accurate 3D view of the bone structure, fewer studies have utilized it compared to traditional methods. Table 4 summarizes all the studies done using fractal analysis to evaluate implants and implant stability.
Treatment and healing monitoring after surgery
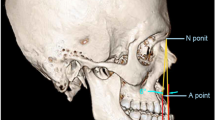
Monitoring trabecular pattern of the jawbones after any surgery is crucial to assess bone healing, detect early signs of infection or complications, and ensure proper integration of grafts, miniplates or implants. Heo et al. [45], and Park et al. [46], studied the fractal dimension (FD) of binary images from panoramic radiographs taken before and after orthognathic surgery for mandibular prognathism. They found their method of FD analysis to be more effective than visual inspection in assessing bone healing. Trabecular changes in the bone post cyst enucleation surgeries in the jaw, transient osteopenia from rapid orthodontic movement, genioplasty surgeries and post osteotomy surgery, could also be evaluated using FD analysis [47,48,49,50]. Akbulut et al. [51], evaluated the effectiveness of fractal analysis from hand-wrist radiographs in deciding between conventional or surgery-assisted rapid palatal expansion, suggesting it could be a useful predictor. Table 4 summarizes all the studies done using fractal analysis for healing and treatment monitoring of bone after surgery.
Fractal analysis of bone pattern in thyroid disorders
S Ergun et al. [52], discussed a 65-year-old patient diagnosed with primary hyperparathyroidism (HPT) due to dental issues. The study reviewed the patient’s medical records and panoramic films from 1997 to 2008, using fractal analysis to assess bone metabolism. The patient showed osteoporotic bone characteristics until a parathyroidectomy, after which biochemical levels normalized, and bone quality improved. The study suggests that fractal dimension (FD) analysis can effectively examine alveolar bone quality in HPT. Ozturk et al. [53], investigated bone changes in the mandible caused by hyperthyroidism and hypothyroidism using fractal analysis on panoramic radiographs. Their findings indicated that hyperthyroid patients had lower FD values than hypothyroid patients, confirming that fractal analysis is useful for early detection of bone density changes related to thyroid disorders, although trabecular regions were affected despite intact mandibular cortical bone.
Fractal analysis of bone in Rheumatoid arthritis and bruxism
Turkmenoglu et al. [54], compared the FD of mandibular condyles in rheumatoid arthritis (RA) patients to those without RA. They found no significant correlations between FD and bone density in the femoral neck or lumbar spine. However, the fractal analysis was effective in distinguishing RA patients from healthy individuals, even with normal bone density readings. Balkan et al. [55], examined the impact of bruxism on the mandibular bone structure after botulinum toxin-A (BTX-A) injections in patients’ masseter muscles, using fractal analysis. They found that hyperactivity in the masseter muscle increased bone density, whereas BTX-A injections reduced muscle activity and changed bone structure, reflected in decreased FD values.
Fractal analysis in diagnosing temporomandibular joint disorders
Early identification of degenerative changes in the temporomandibular joint is a challenging task. Role of FA in this aspect has been evaluated by various researchers [50, 56,57,58]. Canger et al. [56], retrospectively analyzed mandibular condyle in patients with ankylosing spondylitis on panoramic radiographs, they found FD values to be lower in the case group compared to healthy controls ranging from 1.31 ± 0.08 vs. 1.35 ± 0.06 in the first region of interest (ROI1) and ROI2 = 1.37 vs. 1.41. Hence they concluded that lower FD values in patients could indicate sub clinical erosive changes in the condyle, demonstrating the diagnostic value of fractal analysis. Further this was supported by Ozturk et al. [59], who through their CBCT based retrospective study proposed that fractal analysis might serve as a guide in identifying early pathological changes related to TMJ and by Cosgunarslan et al. [60], with their study on edentulous patients on CBCT. Similarly Gulec et al. [60], retrospectively analyzed panoramic radiographs of ankylosing spondylitis patients and reported lower FD values in affected individuals (1.38 ± 0.06) compared to controls (1.41 ± 0.07). Arsan et al. [60], conducted a prospective study comparing FD values between 100 TMD patients and 100 healthy controls using panoramic radiographs. Although the mean FD values were slightly lower in the TMD group (1.22 ± 0.06) compared to the control group (1.25 ± 0.06), the difference was not statistically significant (P > 0.05, ANOVA). However, the authors observed a general trend of decreasing FD with increased joint degeneration and suggested that fractal analysis may still be useful in improving diagnostic efficiency when combined with clinical examination parameters, such as mouth-opening measurements and joint sounds. Koprucu et al. [61], carried out a prospective MRI-based study assessed FD values in patients with unilateral disc perforation of the TMJ Table 5. The mean FD value in the affected joints was 1.07 ± 0.12, significantly lower than the healthy contralateral joints used as controls (1.20 ± 0.11; P = 0.001, independent t-test). The authors concluded that fractal analysis could serve as a predictive tool for TMJ disease by identifying internal disc derangement, effusion, and early degenerative changes, even in the absence of MRI findings.
Fractal analysis of bone in MRONJ
Sahin et al. [62], compared panoramic radiographs of patients with early and advanced stages of medication-related osteonecrosis of the jaw (MRONJ). They found more significant bone structure alterations at advanced stages, though FD values did not vary significantly among the groups. Table 6 summarizes all the studies done using fractal analysis detection in bony changes in patients having systemic diseases.
Limitations of fractal analysis
Fractal analysis, although extensively researched, is not yet clinically applicable due to the following drawbacks,
-
1.
Limited Reproducibility: The box-counting method remains the most widely applied FD algorithm, but inconsistencies across ROI selection, imaging modalities, and FD computation software tools and fractal algorithms (e.g., box-counting, power spectrum) may produce inconsistent results, thereby complicating comparisons.
-
2.
Image Quality Dependence: Fractal analysis exhibits a significant sensitivity to image resolution, noise, and contrast. Variations in the quality of radiographs can markedly impact the precision of the findings [63, 64].
-
3.
Standardization Challenges: The absence of uniform imaging protocols (e.g., exposure parameters, positioning) among various dental radiographs may result in variable fractal dimension measurements [10, 65].
-
4.
Two-Dimensional Constraint: The majority of dental radiographs are two-dimensional, thereby restricting the evaluation of intricate three-dimensional bone structures, which may result in incomplete or deceptive interpretations [66].
-
5.
ROI Selection Bias: The deliberate selection of the Region of Interest (ROI) introduces subjectivity and variability, which may compromise reproducibility and reliability [65].
-
6.
Restricted Clinical Correlation & Applicability: Fractal dimensions may not consistently exhibit a direct relationship with clinical variables including bone density, disease severity, or therapeutic outcomes. Although FD is significantly able to describe diseased bone, the biological significance of alterations in fractal dimension is often ambiguous, which complicates clinical interpretation [67].
-
7.
Impact of Anatomical Overlap: The presence of overlapping anatomical structures, such as trabeculae, roots, and sinus walls, may confound the accurate interpretation of trabecular patterns, thereby diminishing the precision of analyses [10, 65].
Clinical Applications and Integration of Fractal Analysis with Artificial Intelligence & Future Scope
-
Artificial intelligence (AI)—particularly deep learning—has excelled in segmentation, detection, and classification of dental radiographic features which can be combined with the numerical bone texture metrics determined by fractal analysis. A recent overview of systematic reviews of studies by Turosz N et al. [68], using AI on panoramic radiographs found that there was a human-level (or better) performance in detecting periapical radiolucencies, missing teeth, caries, and other findings—processing thousands of images swiftly and accurately. Meanwhile, these reviews also highlighted the growing use of convolutional neural networks for tasks like segmentation and pathology detection in dental imaging, laying the groundwork for combining FD metrics with AI feature extraction to enhance diagnostic precision. Future research directions could be carried out:
-
Hybrid Intraoral Scanning Systems: AI algorithms could automatically extract FD values from precisely identified regions of interest (ROIs), enabling real-time assessment of bone health, periodontal risk, and implant integration.
-
Multimodal Imaging: Integration of FD analysis with CBCT or higher-resolution modalities could yield more robust bone-quality biomarkers across diverse patient populations.
-
Predictive Analytics: Longitudinal and large-scale AI models incorporating FD trends could potentially forecast progression of early degenerative changes in TMJ, post extraction healing, post-surgical healing, and bone-related diseases, response to treatment, or implant outcomes.
Conclusion
The integration of radiographic imaging with mathematic based pattern recognition in Fractal Analysis (FA) presents a new avenue for analyzing dental images. By measuring intricate bone patterns with dental X-rays, it provides an objective means of studying bone structure that traditional methods cannot capture. FA is non-invasive and cost-effective, helping diagnose conditions like osteoporosis and periodontitis by detecting early changes in bone structure that are not visible with standard imaging. It has shown sensitivity to changes after dental treatments. FA can also assess dental implants and monitor bony changes in various systemic diseases. Its applications are highly promising but require more standardized studies before it can be validated for use in everyday dental practice.
Data availability
Not applicable.
References
Pentland AP. Fractal-Based Description of Natural Scenes. IEEE Trans Pattern Anal Mach Intell. 1984;PAMI-6:661–74.
Lopes R, Betrouni N. Fractal and multifractal analysis: A review. Med Image Anal. 2009;13:634–49.
Leszczyński P, Sokalski J. The use of fractal analysis in medicine: A literature review | Zastosowanie analizy fraktalnej w medycynie przegląd piśmiennictwa. Dent Med Probl. 2017;54:79–83.
Mandelbrot B How Long Is the Coast of Britain? Statistical Self-Similarity and Fractional Dimension. 156, New Series. 1967.
Landini G, Rippin JW. An “asymptotic fractal” approach to the morphology of malignant cell nuclei. Fractals. 1993;01:326–35.
Goodchild MF. Fractals and the accuracy of geographical measures. J Int Assoc Math Geol. 1980;12:85–98.
Schmidt PW. Small-angle scattering studies of disordered, porous and fractal systems. J Appl Crystallogr. 1991;24:414–35.
Chatterjee B, Sahoo P. Finite Element Based Contact Analysis of Fractal Surfaces – Effect of Varying Elastic Modulus. Procedia Eng. 2014;90:116–22.
Sánchez I, Uzcátegui G Fractals in dentistry. 39, Journal of Dentistry. 2011. 273–92.
de Nazaré Alves C, de Oliveira Kato A, Barra SG, Abreu LG, Machado VC, Pinheiro J, et al. Fractal analysis of fibrous dysplasia and ossifying fibroma in 2D and 3D CBCT images. J Oral Maxillofac Surg Med Pathol. 2022;34:791–9.
Pandey P, Kandakurti S, Saxena V, Tripathi P, Pamula R, Yadav M. Fractal analysis in oral leukoplakia. J Indian Acad Oral Med Radiol. 2015;27:354.
White SC, Rudolph DJ. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontology. 1999;88:628–35.
Verheij J, Geraets W, van der Stelt P, Horner K, Lindh C, Nicopoulou-Karayianni K, et al. Prediction of osteoporosis with dental radiographs and age. Dentomaxillofacial Radiol. 2009;38:431–7.
Southard TE, Southard KA, Lee A. Alveolar process fractal dimension and postcranial bone density. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontology. 2001;91:486–91.
Southard KA, Southard TE, Schlechte JA, Meis PA. The Relationship Between the Density of the Alveolar Processes and that of Post-cranial Bone. J Dent Res. 2000;79:964–9.
Southard TE, Southard KA, Krizan KE, Hillis SL, Haller JW, Keller J, et al. Mandibular bone density and fractal dimension in rabbits with induced osteoporosis. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontology. 2000;89:244–9.
Bollen AM, Taguchi A, Hujoel PP, Hollender LG. Fractal dimension on dental radiographs. Dentomaxillofacial Radiol. 2001;30:270–5.
Park GM, Jung YH, Nah KS. Prediction of osteoporosis using fractal analysis on periapical radiographs. Korean J Oral Maxillofac Radiol. 2005;35:41–6.
Yaşar F, Akgünlü F. The differences in panoramic mandibular indices and fractal dimension between patients with and without spinal osteoporosis. Dentomaxillofacial Radiol. 2006;35:1–9.
Yasar F, Akgunlu F. Evaluating mandibular cortical index quantitatively. Eur J Dent. 2008;2:283–90.
Yaşar F, Akgünlü F. Fractal dimension and lacunarity analysis of dental radiographs. Dentomaxillofacial Radiol. 2005;34:261–7.
Apolinário AC, Sindeaux R, de Souza Figueiredo PT, Guimarães AT, Acevedo AC, Castro LC, et al. Fractal dimension and mandibular cortical width in normal and osteoporotic men and women. Maturitas. 2014;77:142–8.
Landini G. A fractal model for periodontal breakdown in periodontal disease. J Periodontal Res. 1991;26:176–9.
Updike SX, Nowzari H. Fractal analysis of dental radiographs to detect periodontitis-induced trabecular changes. J Periodontal Res. 2008;43:658–64.
Sang-Yun Cha, Won-Jeong Han, Eun-Kyung Kim. Usefulness of fractal analysis for the diagnosis of periodontitis. Korean Acad Oral Maxillofac Radiol. 2001;31:35–42.
Korkmaz MZ, Altin A, Günaçar DN, Köse TE. Comparison of trabecular bone structure in individuals with healthy periodontium and stage III/IV, grade C periodontitis by fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radio. 2023;135:427–32.
Landini G. Is periodontal breakdown a fractal process? Simulations using the Weierstrass-Mandelbrot function. J Periodontal Res. 1997;32:300–7.
Aktuna Belgin C, Serindere G. Evaluation of trabecular bone changes in patients with periodontitis using fractal analysis: A periapical radiography study. J Periodontol. 2020;91:933–7.
Pârvu AE, Ţǎlu S, Crǎciun C, Alb SF. Evaluation of scaling and root planing effect in generalized chronic periodontitis by fractal and multifractal analysis. J Periodontal Res. 2014;49:186–96.
Sener E, Cinarcik S, Baksi BG. Use of Fractal Analysis for the Discrimination of Trabecular Changes Between Individuals With Healthy Gingiva or Moderate Periodontitis. J Periodontol. 2015;86:1364–9.
Soltani P, Sami S, Yaghini J, Golkar E, Riccitiello F, Spagnuolo G Application of Fractal Analysis in Detecting Trabecular Bone Changes in Periapical Radiograph of Patients with Periodontitis. Int J Dent. 2021;2021.
Madan MS, Liu ZJ, Gu GM, King GJ. Effects of human relaxin on orthodontic tooth movement and periodontal ligaments in rats. Am J Orthod Dentofac Orthopedics. 2007;131:8.e1–8.e10.
Shrout MK, Roberson B, Potter BJ, Mailhot JM, Hildebolt CF. A Comparison of 2 Patient Populations Using Fractal Analysis. J Periodontol. 1998;69:9–13.
Yu YY, Chen H, Lin CH, Chen CM, Oviir T, Chen SK, et al. Fractal dimension analysis of periapical reactive bone in response to root canal treatment. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontology. 2009;107:283–8.
Uğur Aydın Z, Ocak MG, Bayrak S, Göller Bulut D, Orhan K. The effect of type 2 diabetes mellitus on changes in the fractal dimension of periapical lesion in teeth after root canal treatment: a fractal analysis study. Int Endod J. 2021;54:181–9.
Tosun S, Karataslioglu E, Tulgar MM, Derindag G. Fractal analysis and periapical index evaluation of multivisit nonsurgical endodontic retreatment: A retrospective study. Oral Surg Oral Med Oral Pathol Oral Radio. 2022;133:245–51.
Wilding RJC, Slabbert JCG, Kathree H, Owen CP, Crombie K, Delport P. The use of fractal analysis to reveal remodelling in human alveolar bone following the placement of dental implants. Arch Oral Biol. 1995;40:61–72.
Traini T, Novaes AB, Piattelli A, Papalexiou V, Muglia VA. The relationship between interimplant distances and vascularization of the interimplant bone. Clin Oral Implants Res. 2010;21:822–9.
Grizon F, Aguado E, Huré G, Baslé MF, Chappard D. Enhanced bone integration of implants with increased surface roughness: a long term study in the sheep. J Dent. 2002;30:195–203.
Yi WJ, Heo MS, Lee SS, Choi SC, Huh KH. Comparison of trabecular bone anisotropies based on fractal dimensions and mean intercept length determined by principal axes of inertia. Med Biol Eng Comput. 2007;45:357–64.
Mundim MBV, Dias DR, Costa RM, Leles CR, Azevedo-Marques PM, Ribeiro-Rotta RF. Intraoral radiographs texture analysis for dental implant planning. Comput Methods Prog Biomed. 2016;136:89–96.
Lang MS, Miyamoto T, Nunn ME. Validity of fractal analysis of implants in individuals with healthy and diseased peri-implant mucosa. Clin Oral Implants Res. 2020;31:1039–46.
Kış HC, Güleryüz Gürbulak A. Evaluation of the peri-implant bone trabecular microstructure changes in short implants with fractal analysis. Int J Implant Dent. 2020;6:13.
Mishra S, Kumar M, Mishra L, Mohanty R, Nayak R, Das AC, et al. Fractal Dimension as a Tool for Assessment of Dental Implant Stability—A Scoping Review. J Clin Med. 2022;11:4051.
Heo MS, Park KS, Lee SS, Choi SC, Koak JY, Heo SJ, et al. Fractal analysis of mandibular bony healing after orthognathic surgery. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontology. 2002;94:763–7.
Park H, Jung Y, Cho B. Bone changes after bilateral sagittal split osteotomy for mandibular prognathism. Korean J Oral Maxillofac Radiol. 2006;36:183–8.
Koca H, Ergün S, Güneri P, Boyacıoglu H. Evaluation of trabecular bone healing by fractal analysis and digital subtraction radiography on digitized panoramic radiographs: a preliminary study. Oral Radio. 2010;26:1–8.
Kang HJ, Jeong SW, Jo BH, Kim YD, Kim SS. Observation of trabecular changes of the mandible after orthognathic surgery using fractal analysis. J Korean Assoc Oral Maxillofac Surg. 2012;38:96.
Çolak S, Altan A, Bayrak S, Akbulut N. Evaluation of bony changes observed in mandibular osteotomy lines and mandibular condyles following bilateral sagittal ramus osteotomy by fractal analysis. Oral Maxillofac Surg. 2022;27:519–26.
Çoban G, Öztürk T, Bilge S, Canger EM, Demirbaş AE. Evaluation of trabecular changes following advancement genioplasty combined with or without bilateral sagittal split osteotomy by fractal analysis: a retrospective cohort study. BMC Oral Health. 2023;23:160.
Akbulut S, Bayrak S, Korkmaz YN. Prediction of rapid palatal expansion success via fractal analysis in hand-wrist radiographs. Am J Orthod Dentofac Orthopedics. 2020;158:192–8.
Ergün S, Saraçoğlu A, Güneri P, Özpınar B. Application of fractal analysis in hyperparathyroidism. Dentomaxillofacial Radiol. 2009;38:281–9.
Ozturk EMA, Artas A. Evaluation of Bone Mineral Changes in Panoramic Radiographs of Hypothyroid and Hyperthyroid Patients Using Fractal Dimension Analysis. J Clin Densitom. 2024;27:101443.
Türkmenoğlu A, Yüksel HT, Karahan AY. Evaluation of mandibular condyle trabecular structure in patients with rheumatoid arthritis using fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radio. 2022;133:229–37.
Polat Balkan E, Paksoy CS, Bağış N. Fractal analysis of the effects on mandibular bone of botulinum toxin therapy of the masseter muscle in patients with bruxism. Oral Surg Oral Med Oral Pathol Oral Radio. 2024;137:83–8.
Canger EM, Coşgunarslan A, Dilek F, Talay Çalış H. Evaluation of temporomandibular joint components and mandibular bone structure in ankylosing spondylitis patients. Oral Surg Oral Med Oral Pathol Oral Radio. 2023;135:136–46.
Coşgunarslan A, Canger EM, Soydan Çabuk D, Kış HC. The evaluation of the mandibular bone structure changes related to lactation with fractal analysis. Oral Radio. 2020;36:238–47.
Gulec M, Tassoker M, Ozcan S, Orhan K. Evaluation of the mandibular trabecular bone in patients with bruxism using fractal analysis. Oral Radio. 2021;37:36–45.
Öztürk Kocak AT, Göller Bulut D. Measurement of the trabecular bone structure of the TMJ region in patients with transverse maxillary deficiency: a CBCT fractal analysis study. Oral Surg Oral Med Oral Pathol Oral Radio. 2021;132:352–60.
Kumar SS, Nagi R, Chacko R, Khan J. The effectiveness of fractal analysis in diagnosing temporomandibular joint disorders: a systematic review of clinical studies. Oral Radio. 2025;41:153–68.
Akçay Köprücü S, Uzun T. Magnetic resonance imaging and fractal analysis findings in temporomandibular joints with disk perforation. Oral Surg Oral Med Oral Pathol Oral Radio. 2023;135:914–27.
Şahin O, Odabaşı O, Demiralp KÖ. Kurşun-Çakmak EŞ, Aliyev T. Comparison of findings of radiographic and fractal dimension analyses on panoramic radiographs of patients with early-stage and advanced-stage medication-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol. Oral Radio. 2019;128:78–86.
Mishra S, Kumar M, Mishra L, Panda S, Panda S, Lewkowicz N, et al. Estimation of Cancellous Changes Using Fractal Analysis in Patients with Periodontitis. Biomedicines. 2023;11:2547.
Amuk M, Sarıbal G, Ersu N, Yılmaz S. The effects of technical factors on the fractal dimension in different dental radiographic images. Eur Oral Res. 2023;57:60–6.
Pekince A, Azlağ Pekince K, Yasa Y. How does the direction of region of interest selection affect the fractal dimension?. Oral Radio. 2025;41:180–9.
Soler-Alcaraz S, Guerrero-Sánchez Y, Pérez-Sayáns M, Bernabeu-Mira JC, Peñarrocha-Oltra D, Camacho-Alonso F. Evaluation of Change in Radiographic Fractal Dimension around Dental Implants Placed with Low-Speed Drilling and Standard Drilling Protocols. J Clin Med. 2023;12:2244.
Franciotti R, Moharrami M, Quaranta A, Bizzoca ME, Piattelli A, Aprile G, et al. Use of fractal analysis in dental images for osteoporosis detection: a systematic review and meta-analysis. Available from: https://doi.org/10.1007/s00198-021-05852-3
Turosz N, Chęcińska K, Chęciński M, Brzozowska A, Nowak Z, Sikora M. Applications of artificial intelligence in the analysis of dental panoramic radiographs: an overview of systematic reviews. Dentomaxillofac Radio. 2023;52:20230284.
Ruttimann UE, Webber RL, Hazelrig JB. Fractal dimension from radiographs of peridental alveolar bone. Oral Surg, Oral Med, Oral Pathol. 1992;74:98–110.
Law AN, Bollen AM, Chen SK. Detecting Osteoporosis Using Dental Radiographs: A Comparison of Four Methods. J Am Dent Assoc. 1996;127:1734–42.
Kim JY, Jung YH, Nah KS. Prediction of osteoporosis using fractal analysis on periapical and panoramic radiographs. Korean J Oral Maxillofac Radiol. 2008;37:147–51.
Wagle N, Do NN, Yu J, Borke JL. Fractal analysis of the PDL-bone interface and implications for orthodontic tooth movement. Am J Orthod Dentofac Orthopedics. 2005;127:655–61.
Serindere G, Belgin C. Evaluation of the effects of hemoglobinopathies on the mandible with fractal dimension analysis. Niger J Clin Pr. 2019;22:1435.
Lee JM, Park H, Jeong HG, Kim KD, Park CS. Bony change of apical lesion healing process using fractal analysis. Korean J Oral Maxillofac Radio. 2005;35:91–6.
Jung YH. Evaluation of peri-implant bone using fractal analysis. Korean J Oral Maxillofac Radio. 2005;35:121–5.
Veltri M, Balleri P, Ferrari M. Damping factor for monitoring the bone interface at dental implants. Clin Oral Implants Res. 2007;18:738–42.
Yi WJ, Heo MS, Lee SS, Choi SC, Huh KH, Lee SP. Direct measurement of trabecular bone anisotropy using directional fractal dimension and principal axes of inertia. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontology. 2007;104:110–6.
Lee DH, Ku Y, Rhyu IC, Hong JU, Lee CW, Heo MS, et al. A clinical study of alveolar bone quality using the fractal dimension and the implant stability quotient. J Periodontal Implant Sci. 2010;40:19.
Zeytinoğlu M, İlhan B, Dündar N, Boyacioğlu H. Fractal analysis for the assessment of trabecular peri-implant alveolar bone using panoramic radiographs. Clin Oral Investig. 2015;19:519–24.
Jodha KS, Salazar Marocho SM, Scherrer SS, Griggs JA. Fractal analysis at varying locations of clinically failed zirconia dental implants. Dent Mater. 2020;36:1052–8.
Arsan B, Köse TE, Çene E, Özcan İ. Assessment of the trabecular structure of mandibular condyles in patients with temporomandibular disorders using fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radio. 2017;123:382–91.
Gunacar DN, Goller Bulut D, Ustaoglu G, Yildirim EA. In vivo evaluation of mandibular trabecular and cortical bone quality in psoriasis vulgaris. Oral Surg Oral Med Oral Pathol Oral Radio. 2022;133:604–11.
Temur K, Magat G, Cosgunarslan A, Ozcan S. Evaluation of Jaw Bone Change in Children and Adolescents with Rheumatic Heart Disease by Fractal Analysis. Niger J Clin Pr. 2024;27:260–7.
Funding
The authors did not receive any external funds to support this research. The open-access APC was funded through the Manipal Academy of Higher Education, Manipal Karnataka. Open access funding provided by Manipal Academy of Higher Education, Manipal.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to this article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. This review analyses only existing, publicly available data and does not include new data collection or the processing of identifiable personal information. Therefore, ethical approval and consent is not required according to Indian research ethics guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Colaco, L.S.L., Chhaparwal, Y., Patil, V. et al. Decoding dental images: a comprehensive review of fractal analysis. BDJ Open 11, 74 (2025). https://doi.org/10.1038/s41405-025-00365-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41405-025-00365-1