Abstract
Whether and how the non-lesional sensorimotor cortex is activated and contributes to post-injury motor recovery is controversial. Here, we investigated the role of interhemispheric pathway from the contralesional to ipsilesional premotor cortex in activating the ipsilesional sensorimotor cortex and promoting recovery after lesioning the lateral corticospinal tract at the cervical cord, by unidirectional chemogenetic blockade in macaques. The blockade impaired dexterous hand movements during the early recovery stage. Electrocorticographical recording showed that the low frequency band activity of the ipsilesional premotor cortex around movement onset was decreased by the blockade during the early recovery stage, while it was increased by blockade during the intact state and late recovery stage. These results demonstrate that action of the interhemispheric pathway changed from inhibition to facilitation, to involve the ipsilesional sensorimotor cortex in hand movements during the early recovery stage. The present study offers insights into the stage-dependent role of the interhemispheric pathway and a therapeutic target in the early recovery stage after lesioning of the corticospinal tract.
Similar content being viewed by others
Introduction
The lateral corticospinal tract (l-CST) is crucial for dexterous hand movements in higher primates1,2. Lesions of the l-CST impair hand dexterity and the activities of daily living. It is widely known that damaged neurons regenerate rarely in adults3,4, but impaired motor function can be recovered considerably by rehabilitative training5,6. Thus, the mechanism of functional recovery is associated with the training-induced plasticity of residual neural circuits7,8. Identifying the pathways for functional recovery would reveal targets for future neuromodulation therapies. In the clinical setting, the unilateral lesions of CST are often observed in patients with stroke or spinal cord diseases, highlighting interest in the role of the non-lesional sensorimotor cortex; however, whether and how it contributes to the post-injury recovery remains controversial9,10,11,12,13.
We previously demonstrated that after l-CST lesioning of the middle cervical cord (C4–C5) in macaque monkeys, the ipsilesional sensorimotor cortex was activated during the early recovery stage by using positron emission tomography, and that inactivation of the ipsilesional primary motor cortex (M1) with muscimol affected the recovery of hand dexterity14. The study revealed the role of the ipsilesional sensorimotor cortex for the recovery, and it has also been reported that the ipsilesional sensorimotor cortex is involved in locomotion recovery in rodents15,16. However, which pathway activates the ipsilesional sensorimotor cortex remains elusive. Then, Chao et al. performed Granger causality (GC) analysis, which can provide a unidirectional causal dependence between two signals, and evaluated the connectivity between all pairs of multichannel (30 × 30 channels) electrocorticography (ECoG) records spanning the bilateral sensorimotor cortices that were obtained throughout the intact and recovery periods17. As a result, interhemispheric signal flow from the contralesional to ipsilesional premotor cortex (PM) at the α and low-β bands (10–15 Hz) during motor preparation was detected as one of the main components explaining the variance in the whole dataset by the data-driven generalization of principal component analysis for higher order arrays called Parallel Factor Analysis. The longitudinal profile of these network dynamics paralleled recovery, suggesting the contribution of the interhemispheric pathway to the increased activity of the ipsilesional sensorimotor cortex and functional recovery. However, this mathematical analysis-based hypothesis awaits biological validation.
The previous study suggested that inactivation of the contralesional or ipsilesional PM with muscimol affected the recovery of hand dexterity, but the effect was not consistent between the monkeys14. The inconsistency might be due to the muscimol injection that restricts the area that can be injected at one time. Another limitation of the muscimol inactivation is that it inactivates all the neurons at injection site so that it is difficult to evaluate the role of the specific pathway. Recently, pathway-specific manipulation using chemogenetic or optogenetic tools has been developed not only in model animals such as rodents but also in primates to analyze the causal role of target pathways18,19,20.
Here, we blocked the interhemispheric pathway from the contralesional to ipsilesional PM to demonstrate its contribution to dexterous hand movements during recovery in macaque monkeys following lesioning. We also recorded the activity of the sensorimotor cortices with ECoG to study the change in network dynamics caused by the manipulation of the interhemispheric pathway.
Results
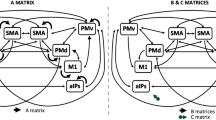
Blockade of the unidirectional interhemispheric pathway using DREADDs
We combined double viral vector intersectional technology18,21,22,23 with Designer Receptors Exclusively Activated by Designer Drugs (DREADDs)24,25 for the reversible and unidirectional blockade of the interhemispheric pathway. First, we trained two macaque monkeys to perform a reach and grasp task with their right forelimb (Fig. 1A, B). Before lesioning the right l-CST, we injected an anterograde vector (AAV1-EF1α-DIO-hM4D(Gi)-mCherry) into the left (contralesional) PM (mainly in its dorsal part, PMd) and a retrograde vector (AAV2retro-CAGGs-Cre) into the right (ipsilesional) PM so that commissural neurons from the contralesional to ipsilesional PM expressed hM4Di and mCherry (Figs. 1C, S1A) using the convection enhanced delivery technique which enabled the injection of large dose without leakage. Postmortem anti-RFP immunohistochemistry showed the labeling of the cell bodies of pyramidal neurons in the superficial layers of the contralesional PM, their axons in the corpus callosum, and their terminal axons and buttons in the superficial layer of the ipsilesional PM (Fig. 1D–H). The estimated averaged density of labeled neurons in the contralesional PM was 344 /mm3 in Monkey A and 548 /mm3 in Monkey H (Fig. S1B). At the center of the injection site in the contralesional PM (ex. Fig. 1D), 11.1 % and 9.9 % of the layer II/III neurons were labeled in Monkey A and H, respectively, although it is difficult to evaluate the total number of the neurons projecting to the ipsilesional PM in that location. Note that there were no labeled cell bodies in the ipsilesional PM, suggesting that unidirectional blockade had been achieved. Conversely, although a small number of collateral fibers were detected in the bilateral putamen (Fig. S1C)—intratelencephalic neurons, recognized as having collateral projections to the striatum in rodents26,27—the density of the labeled fibers was considerably lower compared to that in the ipsilesional PM. The total fiber length at the regions where projections were observed in contralesional and ipsilesional putamen was only 4.6 % and 4.4 % of that in the ipsilesional PM, respectively (Fig. S1D).
A Reach and grasp task. B Experimental schedule. C Schematic diagrams of vector injections and the mechanism of unidirectional blockade of the interhemispheric pathway. D Representative RFP-labeled cells in the contralesional (left) PM of Monkey A. Rectangle indicates the area shown in (E). Scale bar, 200 µm. E High magnification view of D. Scale bar, 100 µm. F RFP-labeled fibers in the corpus callosum of Monkey A. Scale bar, 100 µm. G RFP-labeled fibers in the ipsilesional (right) PM of Monkey A. Rectangle indicates the area shown in (H). Scale bar, 100 µm. H High magnification view of (G). Scale bar, 20 µm. I Extent of the l-CST lesions. Lesions are indicated by black areas. The percentage indicates the proportion of the unilateral ventral and lateral funiculus that are lesioned. Scale bar, 1 mm. Rehab., rehabilitation. Similar images were obtained from three independent brain sections. (D, F, G).
In addition, we chronically implanted a 28-channel subdural ECoG electrode array on each side of the PM, M1, and primary sensory cortex (S1) for longitudinal recording (Fig. S1A).
Unidirectional blockade of the interhemispheric pathway affects recovered hand movements
We made a surgical lesion involving the right dorsolateral funiculus at the middle cervical cord (C4–C5) (Fig. 1I). We evaluated performance in the reach and grasp task according to the success rate of precision grip and movement kinematics before lesioning and during recovery. In the prelesional state, the monkeys could retrieve the food pieces with a precise grip, using just the index finger and the pad of the thumb, with a 100% success rate. We injected a DREADD agonist, deschloroclozapine (DCZ)28, systemically to block the interhemispheric pathway; however, no significant effect was observed on the success rate of precision grip movements (Fig. 2A, P > 0.05, Pearson’s χ2 test) or movement velocity (Fig. S2A, P > 0.05, Wilcoxon rank-sum test) before lesioning.
A Success rate of precision grip before (open circles) and after (red circles) DCZ administration and after vehicle administration (blue circles). The dotted lines indicate the days when the results of the reaching and grasping times shown in (C) were obtained. *P < 0.05 (two-sided Pearson’s χ2 test; Monkey A: P = 3.0 × 10–7 [day 45], 0.0071 [day 49]; Monkey H: P = 1.2 × 10−4 [day 31], 6.4 × 10–7 [day 35], 0.028 [day 36], 0.017 [day 38]). B Examples of food retrieval behavior before (upper figures) and after (lower figures) DCZ injection; 45 days after lesioning in Monkey (A). C Grasping and reaching time before (white bars) and after (red bars) DCZ administration; 45 days after lesioning in Monkey A (Pre-DCZ: 70 trials, Post-DCZ: 56 trials), and 35 days after lesioning in Monkey H (Pre-DCZ: 70 trials, Post-DCZ: 69 trials). Data are presented as mean values ± SD. *P < 0.05 (two-sided Wilcoxon rank-sum test; Grasping time: P = 5.1 × 10–6 [Monkey A], 1.3 × 10−11 [Monkey H]; reaching time: P = 8.3 × 10−5 [Monkey A], 7.3 × 10−4 [Monkey H]).
Just after lesioning, the monkeys could barely move their shoulders but not muscles distal to the elbow at all; however, they gradually recovered with rehabilitative training. Initially, the monkeys lifted their shoulders significantly to compensate for elbow extension, but this behavior disappeared as recovery progressed. From day 42 in Monkey A and day 31 in Monkey H, the monkeys started to retrieve the food pieces with their fingertips, and the success rate of precision grip was improved. When we administered DCZ during the recovery (at day 45 and 49 in Monkey A, and day 31, 35 and 38 in Monkey H), the recovered dexterous hand movements were impaired and the success rate dropped in both monkeys (Fig. 2A, B, P < 0.05, Pearson’s χ2 test); grasping time was also significantly prolonged (Fig. 2C, P = 5.1 × 10−6 [Monkey A], 1.3 × 10−11 [Monkey H], Wilcoxon rank-sum test). In contrast, when we administered the vehicle at day 36 in Monkey H, the success rate and the grasping time was significantly improved. We also observed slight improvement of the grasping time at day 46 in Monkey A, although there was no significant difference (Figs. 2A, S2B). The results suggested that within-day recovery was seen in the early recovery stage and DCZ was effective enough to cancel out the within-day learning effect and further impair the hand movements. Additionally, we confirmed that no learning effect was observed during the sessions after DCZ administration (Fig. S2D).
A detailed video analysis for the type of motor impairment revealed that Monkey A failed to retrieve the food pieces and tried to grasp them repeatedly (wandering error; Fig. S2C and Supplementary movie 1) and Monkey H retrieved them by using the dorsum of the thumb, failing to use the pad of the thumb (precision error; Fig. S2C). Both of them suggested an impairment in opposing movement of the thumb and index finger. Furthermore, video images and machine-learning based analysis of finger trajectories revealed that the monkeys had difficulty in inserting their thumb into the slit (Fig. 2B, S3A–C). Conversely, the trajectory of the index finger was not different between before and after DCZ administration (Fig. S3A).
These results show that the interhemispheric pathway from the contralesional to ipsilesional PM contributes to motor function during recovery, especially the dexterity of the thumb such as opposability. Additionally, the shoulder position during grasping was not different between before and after DCZ administration, suggesting that the effects of DCZ on behavior were independent of compensatory movements of the proximal muscles (Figs S3D, S3E).
We found that the effect of DCZ diminished as the baseline success rate of the precision grip was increased. In Monkey H, since the increase in success rate was slower compared to Monkey A and we could administrate DCZ during the stages with lower success rate, the effects seemed to be longer and clearer than in Monkey A. Another possible explanation of the difference in effects across monkeys was a greater density of infected neurons in Monkey H compared to Monkey A (Fig. S1B).
Although DCZ is a high-affinity agonist for DREADDs, it could still have off-target effects on endogenous receptors. To exclude the possibility that our behavioral results were due to off-target effects, we examined another monkey without DREADD expression and found that DCZ did not affect its behavior during recovery after the lesioning (Fig. S3F, G).
In this monkey, instead of chemogenetic blockade with DREADDs, we performed a partial callosotomy between the PMs during recovery after the lesioning and obtained similar behavioral results (Fig. S3F–H). These results suggest that commissural fibers were the main contributors to our results, although the interhemispheric pathway projected a small number of collateral fibers to the putamen (Fig. S1C, D).
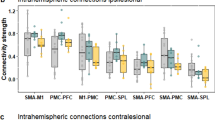
Interhemispheric connectivity is blocked unidirectionally by DREADDs
In this study, we recorded ECoG longitudinally and calculated GC between the electrodes during the reach and grasp task to evaluate the interhemispheric connectivity. We especially focused on GC in the low frequency band because many studies suggested that the low frequency band activity is related to long-range or interhemispheric cortico-cortical connectivity while the high frequency band is related to intracortical or local connectivity29,30. In addition, as described above, the previous study from our laboratory showed GC from the contralesional to ipsilesional PM (mainly the PMd) in the low frequency band (10–15 Hz) around movement onset was increased during early recovery after l-CST lesioning17. Therefore, we compared the GC at this timing and frequency band between before and after DCZ administration to confirm that our manipulation could block the interhemispheric connectivity. We divided the recovery stage into the ‘early’ and ‘late’ periods, and the border between ‘early’ and ‘late’ was termed the ‘full recovery day’, which was defined as the experimental day on which the success rate of precision grip first reached 100% after lesioning. During the early recovery stage, we found the high GC from the contralesional to ipsilesional PMd in the low frequency band (10–15 Hz) around movement onset (–0.2 to 0 s in Monkey A, –0.1 to 0.1 s in Monkey H; see Methods for how to define these intervals) and the GC was decreased after DCZ administration (Fig. 3A, B, D, E). We combined the data from both monkeys and found a significant difference in the GC value before and after using DCZ (Fig. 3G, P = 0.0039, Wilcoxon sign-rank test). In Monkey H, changes in GC were observed in other time windows (–0.6 to –0.4 s and –0.35 to –0.15 s; Fig. 3D, right). However, when using only the data from Monkey H, the effect of DCZ on GC in the selected window (–0.1 s to 0.1 s) remained significant (P = 0.031), while change in the other windows (–0.6 to –0.4 s and –0.35 to –0.15 s) was not significant (P = 0.22 and 0.16, respectively, Wilcoxon sign-rank test).
A, D Averaged time-frequencygram of GC from the contralesional to ipsilesional PMd before (left figure) and after (middle figure) DCZ administration and their difference (right) in the early recovery stage of Monkey A (A) and Monkey H (D). Time 0 (black line) indicates movement onset. Red rectangles indicate the time frequency ROI that was used for the calculations shown in (B, C, E–I). Black triangles at the bottom indicate the onset of grasping. B, E Anatomical dimension of GC from the contralesional to ipsilesional PMd (7 × 7 channels, encircled in red lines) in the low-frequency band around movement onset (ROI shown in A, D), before (left) and after (middle) DCZ administration and their difference (right). Each arrow indicates the directionality and strength of GC. C, F Anatomical dimension of GC from the ipsilesional to contralesional PMd. G–I Averaged value of GC in the ROI (shown in A, D) in the early recovery stage of both monkeys (A, H). Each line plot indicates the result of each experimental day in the early recovery stage (n = 9 days). Error bars indicate standard deviation. *P < 0.05 (two-sided Wilcoxon sign-rank test; P = 0.0039 [left], 0.07 [middle], 0.25 [right]).
In contrast, GC in the opposite direction (from the ipsilesional to contralesional PMd) was not significantly changed by DCZ administration (Fig. 3C, F, H, S4A, P = 0.07, Wilcoxon sign-rank test). These results suggest that our method successfully blocked the connectivity of the target pathways in a unidirectional manner.
When aligning the data to the reaching onset, we found that the time window of high GC in Monkey A was earlier compared to that in Monkey H (–0.2 to 0 s in Monkey A, –0.1 to 0.1 s in Monkey H). On the other hand, when aligning the data to the grasping onset, the time window in Monkey A was later than that in Monkey H (–0.4 to –0.25 s in Monkey A, –0.5 to –0.3 s in Monkey H, Fig. S4B). Taking into account the difference in reaching time between Monkey A and Monkey H in the early recovery stage (0.24 s in Monkey A vs 0.37 s in Monkey H), these results might suggest that the enhanced connectivity included both reaching and grasping elements, and the high GC period differed across the monkeys in both cases of alignment depending on each monkey’s speed of reaching.
As the enhanced connectivity included the both reaching and grasping elements, it could be possible that the prolongation of reaching time after DCZ administration influenced the change of GC. However, significant effects on GC could be seen both in the results aligned to the reaching onset (Fig. 3G) and grasping onset (Fig. S4D, P = 0.027, Wilcoxon sign-rank test), suggesting that the effects on GC were not caused by the change in reaching time.
In the late recovery stage, the high GC observed in the early recovery stage had diminished and the effect of DCZ on the GC was not observed (Fig. S4C, E). This suggests that interhemispheric connectivity was decreased after full recovery, consistent with the previous study17.
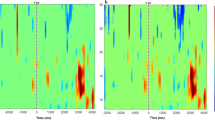
Interhemispheric facilitation during recovery
We investigated the longitudinal change in the activity of the ipsilesional PM during blockade of the interhemispheric pathway. We performed time-frequency analysis of ECoG activity during the task and compared the activity between before and after DCZ administration. Since we aimed at revealing the role of the interhemispheric pathway for activation of the ipsilesional sensorimotor cortex during the recovery, we focused on the brain area with high activity during the task in the early recovery stage (Ch 10 in PMd, black circle in Fig. S5). We found that in the early recovery stage, the activity in the low frequency band (7–9 Hz) was high during the movement onset (–0.2 to 0 s in Monkey A, –0.1 to 0.1 s in Monkey H) and the activity was decreased by DCZ administration (Figs. 4, S5B, P < 0.039, Wilcoxon sign-rank test). The effect was prominent particularly during the earlier experimental days in both monkeys (Fig. S5D, Day 45 in Monkey A (red) and Day 27 in Monkey H (violet)). However, in Monkey H, the effect became unclear during the later part of the early stage (Day 43 and 48 in Monkey H (light blue)). Contrary, in the intact state and the late recovery stage, the activity was increased by DCZ administration (Fig. 4, S5A, C, P = 7.8 × 10–4 [intact], 0.020 [late], Wilcoxon sign-rank test). Vehicle had no effect on the activity in any stage (Fig. S5E). Regarding the contralesional PM, no change was observed in the intact state and the late recovery stage. In the early recovery stage, there was a trend of decreased activity with DCZ administration, although this did not reach statistical significance (Fig. S6, P = 0.055, Wilcoxon sign-rank test).
A–F The average normalized time-frequencygram of brain activity at the ipsilesional PMd (Ch 10) before (left) and after (middle) DCZ administration in the intact state (A for Monkey A and D for Monkey H), early recovery stage (B for Monkey A and E for Monkey H), and the late recovery stage (C for Monkey A and F for Monkey H). Right figures show the difference in activity between before and after DCZ administration. Time 0 (black line) indicates movement onset. Red rectangles indicate the time frequency ROI that was used for the calculations shown in (G), H, I Black triangles indicate the onset of grasping. Averaged value of normalized brain activity (ECoG) at the ipsilesional PMd in the ROI in the intact state (G, n = 16 experiment days including 1074 trials [Pre-DCZ] and 1093 trials [Post-DCZ]), early recovery stage (H, n = 9 days, 591 trials [Pre-DCZ] and 525 trials [Post-DCZ]), and late recovery stage (I, n = 14 days, 970 trials [Pre-DCZ] and 972 trials [Post-DCZ]) of both monkeys (A, H). Error bars indicate standard deviation. *P < 0.05 (two-sided Wilcoxon sign-rank test, P = 7.8 × 10−4 [G], 0.039 [H], 0.020 [I]).
These results indicate that the interhemispheric pathway inhibits the activity of the opposite PM in the intact state, while this pathway facilitates the ipsilesional PM and contributes to recovery in the early recovery stage (Fig. 5). It is known that the commissural fibers are from excitatory neurons which mainly project to the inhibitory interneurons on the opposite side. Thus, the disinhibition observed in this study should be due to the change in the local inhibitory mechanisms at the ipsilesional PM (see Discussion).
In addition, we performed electrical stimulation with the subdural ECoG electrodes on the bilateral sensorimotor cortices and observed muscle twitches in the ipsilesional forelimb (Figs. S7A–D). Lesioning of l-CST at C4/C5 diminished twitches of the elbow or more distal muscle by stimulation of contralesional sensorimotor cortices. On the contrary, since the motor pathways to parts of shoulder muscles such as trapezius and levator scapulae could be spared in this lesion, shoulder twitches were still preserved postoperatively. This might be associated with the compensatory shoulder movements observed during the period when distal muscles were paralyzed. As twitches in the distal muscles began to recover, the compensatory movements diminished, suggesting a reduced relative contribution of the shoulders to limb movements. More interestingly, in the intact state, muscle twitches of the ipsilesional forelimb were barely observed when stimulation was given through the ipsilesional electrodes. However, during the early recovery stage, electrical stimulation on the ipsilesional side induced twitches in the ipsilesional forelimb muscles, suggesting the involvement of the ipsilesional sensorimotor cortex in the control of affected hand movements.
We also recorded cortico-cortical evoked potentials (CCEPs)31 at the ipsilesional PM by stimulating the contralesional PM. The amplitude of CCEPs was increased during the early recovery stage (Fig. S7E, F, F = 52.04, P < 0.05 for Monkey A; F = 18.33, P < 0.05 for Monkey H, one-way analysis of variance followed by Bonferroni’s post hoc test).
These results supported our conclusion that the interhemispheric pathway from the contralesional PM facilitates the activity of the ipsilesional sensorimotor cortex, and the pathway from the ipsilesional motor cortex to the ipsilesional hand muscles is upregulated and supports recovery during the early stage after lesioning (Fig. 5).
Discussion
The early recovery stage after lesioning is critical because a previous study showed that the lack of training during the first month after l-CST lesioning has a severe impact on recovery32. In the present study, we first demonstrated that DCZ-induced blockade of the interhemispheric pathway caused impairment of hand movements during the early recovery stage, but not in the intact state or late recovery stage, by using an intersectional pathway-specific blocking technique. Additionally, DCZ administration to the monkey without DREADD expression had no effect in the early recovery stage. All these results indicated that the behavioral impairment observed in this study was the result of interhemispheric pathway blockade and not of a non-specific effect of DCZ administration. Furthermore, electrophysiological recordings with ECoG demonstrated that the action of the interhemispheric pathway changed from inhibition to facilitation, leading to the involvement of the ipsilesional sensorimotor cortex in hand movements during the early recovery stage.
In the intact state, blockade of the interhemispheric pathway did not affect motor performance in the reach and grasp task, showing that neither the interhemispheric pathway nor ipsilateral motor cortex contributed to hand movements. Time-frequency analysis suggested that the interhemispheric pathway from the contralesional PM inhibited the activity of the ipsilesional PM in the intact state, which is consistent with previous reports33,34. Interestingly, the present results suggest that the effect of the interhemispheric pathway changes from inhibition to facilitation and the ipsilesional sensorimotor cortex becomes directly involved in the control of dexterous hand movements during the early recovery stage after lesioning. Commissural fibers originate from glutamatergic excitatory pyramidal neurons and exert excitatory and inhibitory effects on the pyramidal neurons in the opposite sensorimotor cortex35,36. Therefore, the disinhibition observed in the early recovery stage could be due to changes in the activity level of inhibitory interneurons at the ipsilesional PM or the postsynaptic effect of GABA from inhibitory to excitatory due to changes in Cl- transporters, as observed during the early developmental stage or in some pathological conditions37, but the detailed mechanisms still remain unclear. Additionally, it has been reported that disinhibition occurred not only in the intact side but also in the affected side especially in patients with stroke38,39. In the current study we focused on the disinhibiton of the ipsilesional cortex and not the contralesional cortex. However, the result that DCZ administration also decreased the activity of the contralesional PM, although without statistical significance, might suggest that disinhibition occurred bilaterally so that inactivation of the ipsilesional PM caused the inactivation of the contralesional PM by the secondary effect through the interhemispheric pathway.
Our electrophysiological data recorded with ECoG showed that the activity of the ipsilesional PM was increased around the movement onset in low frequency band but not in high frequency band during the movement that is known to be directly related to the process of motor execution in M140,41. In addition, the blockade of the interhemispheric pathway affected the activity of the ipsilesional PM around the movement onset. These results suggest that the interhemispheric pathway between PM may have a gating function that modulates the motor execution signals rather than directly conveying them. Some other studies supported this hypothesis by showing that the cortico-cortical oscillations in the low frequency band play a role for an inhibitory gating control42,43. Additionally, it has been reported that the activity in the ipsilateral PMd during movement preparation represents ipsilateral arm movements in an abstract manner in intact monkeys44. Also, ipsilateral M1 neurons represent the ipsilateral arm movements to some extent in monkeys and humans44,45, although the contribution of the ipsilateral M1 is much lower than that of contralateral M1. These findings suggest that the motor representation in the ipsilateral motor cortex exists to some extent but is suppressed in the intact state. The current study suggested that in early recovery stage, the gating control might change from inhibition to facilitation to enhance the motor execution signals in the ipsilesional motor cortex. Since it has been reported that the motor execution signals (i.e. the high frequency activity) in M1 are also modulated by other motor related areas like supplementary motor area and subcortical regions such as thalamus, cerebellum or basal ganglia46,47,48,49, it is possible that the cortico-cortical or cortico-subcortical pathways also contributed to the recovered dexterous hand movements. In this study, we could show the role of the interhemispheric pathway between premotor cortices for the motor recovery but further studies are needed to evaluate the contribution of other areas and the interaction between them.
More interestingly, DCZ administration had no effect on behavior in the late recovery stage, and time-frequency analysis showed the effects of DCZ in this period were similar to those in the intact state. These results suggest that the action of the interhemispheric pathway returned to inhibition after full recovery. These findings were consistent with previous studies also suggesting that the contribution of the interhemispheric pathway and ipsilesional motor cortex was more obvious in the early stage than in the chronic stage14,17. In addition, a recent study in patients with stroke also showed that the interhemispheric inhibition was increased in chronic stage while motor function was improved50. Although the mechanism and the role of interhemispheric inhibition after the recovery are still controversial, the current and relevant studies suggest that the increased interhemispheric inhibition in chronic stage might be the consequence of the recovery rather than preventing motor recovery. Furthermore, our recent neuroanatomical study demonstrated that late stage recovery is supported by reorganization of the CST including the sprouting of axons originating from the contralesional and ipsilesional motor cortices in the gray matter both caudal and rostral to the lesion, including a re-direction of the CST to hand motoneurons51. In addition, other descending motor pathways such as propriospinal and reticulospinal tracts remained intact in our lesion model. Since these pathways might also contribute to the recovery of hand movements, contribution of the ipsilesional motor cortex could be decreased by the increase of interhemispheric inhibition in the chronic stage.
In the clinical setting, many studies have focused on the role of the interhemispheric pathway in patients with a CST lesion such as stroke9,10,11. However, it is still controversial whether the interhemispheric pathway and motor cortex on the intact side support or disrupt recovery12,13. It is thought that the results depend on lesion size, recovery stage, comorbidities, etc., but these are difficult to control in clinical studies. One of the advantages of our research was that we could follow the whole process longitudinally before and after a particular lesion. In addition, pathway-specific manipulation using chemogenetic techniques is one of the best approaches to reveal the causal relationship between a target pathway and its functions. Furthermore, since it enabled us to block the pathway reversibly and repeatedly, we could investigate its role longitudinally in different phases with a minimum number of animals.
There are some technical concerns about our pathway-specific blockade method. First, since it is difficult to evaluate the total number of the commissural fibers between PM, we could not estimate the accurate target efficiency of the double viral injections. Although some portion of the target neurons might have been spared from the DREADD manipulation, the efficiency was high enough to show the significant effects on the behavior and electrophysiology. Second, in this study, we could not assess the time course of DREADD expression, and it is possible that changes in expression levels before and after lesioning contributed to differences in the effects. However, an earlier study, though not using the double viral vector technique, has reported that DREADD expression via AAV vectors stabilized six weeks post-injection and remained stable for over a year52. Additionally, before lesioning, we conducted the behavioral and electrophysiological experiments repeatedly from 8 weeks to 4 months after the viral injections. We confirmed that the effect of the chemogenetic blockade on the brain activity was stable and there was no behavioral effect before lesioning. Therefore, we consider it unlikely that changes in expression levels significantly contributed to differences in the effects before and after lesioning. Third, the current study could not completely rule out the possibility that collateral fibers to the putamen influenced the results. However, considering the results of callosotomy and the majority of labeled neurons projecting to the ipsilesional PM, we believe that the role of interhemispheric pathways was predominant. Fourth, in this study, it was not possible to assess how much other neural circuits, including distant ones, were affected by the blockade of the interhemispheric pathway, and whether such indirect effect led to behavioral changes. Further research is needed, such as using neuroimaging techniques to evaluate the global brain activity including subcortical nuclei after blockade. However, even if we take into account potential secondary effects, the behavioral effect can be safely inferred as a consequence of the interhemispheric blockade. Finally, the current study showed that the effect of the interhemispheric blockade on the behavior disappeared over recovery stage. As we mentioned above, the result suggest that the interhemispheric pathways returned to inhibitory as a result of involving alternative pathways. However, it was possible that repeated DCZ administration was involved in attenuating the effect. Recent studies have reported attenuation of the effect of chemogenetic blockade by repeating the task several hundred times in a session and between sessions on different days, suggesting compensation through other pathways53. On the other hand, our previous study showed that sustained blockade of the propriospinal pathway over several days attenuated the effect of motor deficit, but did not show attenuation between sessions. This suggests that the degree of compensation during blockade may depend on the target pathways, duration and frequency of the blockade, and the task intensity during blockade. Although we minimized the frequency of DCZ administration and the number of task trials to avoid learning effects and compensation during blockade, it was difficult to exclude that the tasks during the DCZ session promoted compensation by other pathways.
Our findings demonstrated that the contribution of the interhemispheric pathway was observed in the early recovery stage. In the clinical setting, the enhancement of functional recovery in the early stage with neurorehabilitation is important for patients to increase their activities of daily living and motivation. Otherwise, poor functional recovery in the early stage results in disuse and muscle atrophy in the late stage. Our results offer insights on a target pathway for neuromodulation therapy to enhance recovery during the early phase after lesioning of the CST.
Methods
Study design
We designed this study to test our hypothesis that the interhemispheric pathway from the contralesional to the ipsilesional PM contributed to the motor functional recovery after the unilateral l-CST lesioning. To achieve this aim, we used two Japanese macaque monkeys (Macaca fuscata; Monkey A [5 years old, 7 kg, male] and Monkey H [7 years old, 8 kg, female]) for the pathway-specific blockade experiments in which we blocked the interhemispheric pathway by using DREADD and evaluated the effect on motor function and the brain activity recorded with ECoG before lesioning and during recovery. We selected the number of monkeys, experimental days and trials on the basis of the previous studies17,18,21,28,54. No sex- and gender-based analyses have been performed due to the limitation of the number of animals. However, both male and female monkeys participated in this study and the results were consistent across sex. The two monkeys were not allocated and they underwent the same experimental procedures. In both monkeys, DCZ or vehicle were used in different days. The order of drug administration was not random. Instead, the administration days of DCZ and vehicle were alternated as much as possible to control the influence of the degree of recovery on the results. The behavioral analyses were performed in a blinded fashion and the electrophysiological analyses were performed automatically by using the same MATLAB code across experimental days. We used another two monkeys (Monkey I [6 years old, 7 kg, female] and Monkey K [6 years old, 6 kg, female]) for the callosotomy experiments (Fig. S2E–S2G). All the monkeys used in this study were provided by the National BioResource Project of the Ministry of Education, Culture, Sports, Science, and Technology of Japan (MEXT). All experimental procedures and animal care were performed in accordance with the ILAR’s Guide for the Care and Use of Laboratory Animals and were approved by the Committee for Animal Experiments at the Graduate School of Medicine in Kyoto University, Japan.
Surgery
We performed all surgical procedures described below under general anesthesia. First, we anesthetized the animals with ketamine hydrochloride (10 mg/kg, i.m.) and xylazine (1 mg/kg, i.m.) and then intubated them and maintained anesthesia with isoflurane (1 ~ 2 %) inhalation. We monitored heart rate, blood pressure, peripheral capillary oxygen saturation, body temperature, and end-expiratory carbon dioxide pressure during surgery. We administered dexamethasone (0.825 mg/kg, i.m.), analgesics (butorphanol [0.2 mg/kg, i.m.], ketoprofen [1 mg/kg, i.m.], or diclofenac [12.5 mg, anally]), and antibiotics (ampicillin sodium [200 mg, i.m.], ceftriaxone [50 mg, i.m.], or cefazolin [100 mg, i.m.]) during and after surgery.
Implantation of steel tubes for head fixation
First, we performed magnetic resonance imaging of the brain under anesthesia with ketamine hydrochloride (10 mg/kg, i.m.) and xylazine (1 mg/kg, i.m.) and then intubated the animals and maintained anesthesia with isoflurane (1–2 %) inhalation using a 3 T magnetic resonance imaging scanner (Verio; Siemens, Washington, DC, USA) to decide the location of plastic screws, steel tubes, and craniotomy.
We mounted two steel tubes on the monkey’s head for fixation during the behavioral task. First, we made a skin incision on the head. We peeled off the soft tissue and a part of the temporal muscles to expose the skull. We attached small plastic screws to the skull as anchors. We mounted two steel tubes in parallel over the frontal and occipital lobes. Finally, we covered the skull, screws, and steel tubes completely with acrylic resin.
Injection of viral vectors and implantation of ECoG electrodes
To block signal transmission through the interhemispheric pathway from the contralesional (left) to ipsilesional (right) PM, we injected AAV1-EF1α-DIO-hM4Di-mCherry (1.5 × 1012 vg/mL [Monkey A] and 2.2 × 1012 vg/mL [Monkey H]) into the contralesional PM and AAV2retro-CAGGS-Cre (6.0 × 1012 vg/mL [Monkey A] and 5.3 × 1012 vg/mL [Monkey H]) into the ipsilesional PM. We packaged the vectors using the AAV Helper Free Expression System (Cell Biolabs, Inc., San Diego, CA) following a previous study55. A transferred plasmid, pAAV-hSyn-hM4D(Gi)-mCherry was a gift from Bryan Roth (Addgene plasmid # 50475; http://n2t.net/addgene:50475; RRID:Addgene_50475). We transfected the packaging and transfer plasmids into HEK293 T cells by using calcium phosphate method. We obtained a crude cell extract containing AAV vector particles from the cells and subsequently purified the AAV vector particles by serial ultracentrifugation with cesium chloride. We dialyzed the purified particles, followed by concentration. We determined the titer by real-time quantitative PCR.
We exposed the PM, M1, and S1 by removing the acrylic resin, craniotomy, and incision of the dura mater. We injected six tracks in the PMd (the area between the spur of the arcuate sulcus and superior precentral sulcus) and two to three tracks in the ventral part of the PM (lateral to the spur of the arcuate sulcus). The distance between the tracks was 2.0 ~ 2.5 mm (Fig. S1A). To spread the vector solution to a large area of the cortex, we adopted a convection-enhanced delivery technique56,57, which enabled the injection of a large volume of solution at a controlled high rate. Specifically, we injected 6.05 μL vector at each track in two steps. We injected the first 1.25 μL at 0.25 μL/min, and injected the remaining 4.80 μL at 0.60 μL/min by using a 25-μL Hamilton syringe (1702SN, flat tip; Hamilton Company, Reno, NV, USA) with a 32-gauge injection needle. We fitted a fused silica capillary (450-μm outside diameter) to create a 1 mm ‘step’ away from the needle tip to reduce reflux. We inserted the needle 1.5 mm from the surface of the cortex. Before and after injection, we waited for 5 and 10 min, respectively.
After the injection, we implanted a platinum ECoG array comprised of 28 channels (7 × 4 grid) electrodes on a parallelogram-shaped silicon sheet (23 × 11.5 mm) covering the PM where the injections were made, M1 hand area, and S1. The diameter of each electrode was 2 mm and the inter-electrode distance was 3 mm (the distance between the electrodes on the M1 and S1 was 4 mm). There were four other electrodes on the opposite surface of the sheet for reference. We performed the surgeries one side at a time in two separate days.
Lesioning of the l-CST
We lesioned the l-CST at the right middle cervical cord (C4–C5)17,54. We exposed the dorsal surface of the spinal cord by laminectomy of the C3 and C4 vertebrae and incision of the dura mater. We transected the dorsal part of the lateral funiculus at the border between the C4 and C5 segments from the dorsal root entry zone ventrally to the level of the lateral ligaments by using a pair of fine forceps. We extended the lesion ventrally at the most lateral part of the lateral funiculus. We closed the opening of the dura mater by using artificial dura mater (Gore-Tex membrane; WL Gore & Associates, Flagstaff, AZ, USA), and we sutured the muscles and skin with absorbable sutures and silk, respectively.
Behavioral testing
First, we trained the monkeys to sit in a monkey chair with their heads fixed in a stereotaxic frame attached to the chair and with their left arm fixed gently in the arm holder (Fig. 1A). The monkeys were required to push a button on a board attached to the chair with their right hand for more than 2 s. Then, a cube of sweet potato (6 × 6 × 6 mm3) was presented between a vertical slit (8 mm width), and the monkeys could retrieve it with their thumb and index finger. Signals from the button allowed us to determine the timing of movement onset. We used two digital video cameras (120 frames/s) to record and analyze the reach and grasp task; one from the left and another from the upper side of the monkeys. Additionally, a third camera (60 frames/s) was placed in front and above the monkeys to capture supplementary footage.
Since the monkeys could not perform the reach and grasp task just after l-CST lesioning, we performed intensive rehabilitation for 5–6 days per week with manual assistance of movements and with larger pieces of sweet potatoes and apples to promote rehabilitation until they were able to perform the task.
ECoG recording during behavioral testing
While the monkeys performed the reach and grasp task, we recorded brain activity on the surface of the bilateral sensorimotor cortices using the ECoG electrodes. We recorded the signals at a sampling rate of 2000 Hz using PyCorder V1.0.9 (Brain Products GmbH, Gilching, Germany). We extracted ECoG signals using multichannel amplifiers with 0.3-Hz high-pass and 7500-Hz low-pass analog filters.
Administration of DCZ
We used DCZ (HY-42110; MedChemExpress, Monmouth Junction, NJ, USA), a high-affinity and selective agonist for DREADDs24, to block the interhemispheric pathway. We dissolved DCZ in 2% dimethyl sulfoxide in saline (vehicle) to a final concentration of 1 mg/mL. Before DCZ administration, the monkeys performed 70 trials of the reach and grasp task as the Pre-DCZ session. After the Pre-DCZ session, we administered DCZ (100 µg/kg) intramuscularly and the monkeys performed 70 trials of the task as the Post-DCZ session. The Post-DCZ session was started at 30 min after DCZ administration and was accomplished by 60 min after administration. We waited 8 weeks after injection of viral vectors before starting the sessions of DCZ administration. Previous studies suggested that this waiting time was sufficient for each viral vector and DREADD to be expressed28,52,58,59. We administered DCZ or vehicle once or twice per week during the prelesional period, for 2–3 months before lesioning, and for 4 months in the postlesional period.
We conducted all sessions and rehabilitation in the early afternoon. To control hunger during the sessions, we gave a fixed amount of food, fruit and candy after the experiments instead of allowing free access to food. We set the amount of food to be sufficient for the daily nutritional intake and confirmed that there was no weight loss throughout the recovery course.
Behavioral data analysis
We calculated the success rate of precision grip during the reach and grasp task18,21. We identified three types of error: ‘drop error’, ‘wandering error’, and ‘precision grip error’. For drop errors, the monkeys dropped the food and failed to eat it. We defined wandering errors as trials in which both fingers touched the food, but the monkeys released it and tried to pick it up again. If the monkeys could not pinch the food with their index finger and the pad of the thumb, we defined these trials as precision grip error trials, although they were able to eat the food. In this study, we evaluated success rates by removing these errors. We compared the success rates of the Pre- and Post-DCZ sessions on each day by using Pearson’s χ2 test (two-sided).
We calculated the reaching and grasping times in each trial. We defined reaching time as the time from movement onset to when the monkey’s finger first touched the slit, while grasping time was the time during which the monkey’s fingers were inside the slit. We removed drop error trials from the analysis. We tested the significance of the difference in the reaching and grasping times between the Pre- and Post-DCZ sessions by using the Wilcoxon rank-sum test (two-sided).
We tracked the position of the thumb and index finger recorded from the left side by using machine-learning software (DeepLabCut)60. Briefly, we selected 500 frames randomly from two videos that recorded the Pre- and Post-DCZ sessions on the same experimental day that we used to label the tips of the thumb and index finger, food, and upper and lower right edges of the slit. We trained the deep learning network over 500,000 iterations and fed it both videos to track the tips of the fingers during the task. We extracted the coordinates of all labels using MATLAB (MathWorks, Natick, MA, USA). We removed the drop error trials and plotted the trajectories of the thumb and index finger in each trial (Fig. S3A) at the timing just before the monkeys retrieved the food. We plotted the positions of the thumb and index finger (Fig. S3B) at the timing of retrieval, which we defined as the timing at which the x coordinate of the food first exceeded the baseline position by a threshold of 5 standard deviations. We calculated the distance of the thumb tip from the slit entrance at the timing when the monkeys retrieved the food as an index for the dexterity of the thumb, which indicates how well they could insert the thumb into the slit (Fig. S3C). Additionally, we tracked the position of the shoulder using the camera placed in front and above the monkeys and defined its position at the timing of retrieval. As an indicator of the shoulder movements during grasping, we calculated the distance of the shoulder from a fixed neck plate, which remained constant throughout the experiments, and compared this measurement before and after DCZ administration (Fig. S3D, E). We tested the significance of the difference in the distance between the Pre- and Post-DCZ sessions by using the Wilcoxon rank-sum test (two-sided).
Dynamics of corticocortical connectivity
We quantified the dynamics of corticocortical connectivity by spectral GC61, following a previous study17. We removed the 60-Hz line noise from the raw ECoG data using the MATLAB FieldTrip toolbox62. We downsampled the data eight times, resulting in a sampling rate of 250 Hz. We then aligned the ECoG signals from each channel using the timing of reaching onset, which we defined as the timing when the monkeys left the button (Time 0; see Fig. 3). In addition, we aligned the data to the grasping onset by measuring the time from reaching onset until the monkey’s finger entered the slit using video recordings. Basically, by the time monkeys started retrieving the food, they could press buttons. However, Monkey A was unable to press the button in 28 % of the trials during the session after DCZ administration on day 45 due to the weakness of the hand and the wrist. We excluded these trials from electrophysiological analysis. Also, the drop error and wandering error trials were removed from the analysis. Between the signals from two channels (56 × 56 channels), we calculated in-trial spectral GCs from each session, where each GC represents a unidirectional connectivity from one channel to another, during times between –1.5 and 1 s (50 time points), and across frequencies between 5 and 120 Hz.
We used three preparation steps for spectral GC calculation:
1) Preprocessing: we performed detrending, temporal normalization, and ensemble normalization to achieve local stationarity of the data63;
2) Window length selection: we set the length and step size of the sliding window for segmentation as 200 ms and 50 ms, respectively;
3) Model order selection: we set the model order, which is related to the length of the signal in the past that is relevant to the current observation, as 10 samples (equivalent to 10 × 4 = 40 ms of history) in both monkeys, following a previous study17.
After GC calculation, we averaged all combinations of GC from the contralesional PMd to ipsilesional PMd (7 × 7 channels, Fig. 3B) or the opposite direction. We set the time frequency region of interest (ROI) in the low frequency band (10 ~ 15 Hz) around movement onset (–0.2 to 0.2 s for Monkey A, –0.1 to 0.1 s for Monkey H) where GC in 0010–15 Hz exceeded three standard deviation above the averaged GC of baseline (–1.5 to –1 s) before DCZ administration, and calculated the mean GC of the ROI in each session of each experimental day. We divided the experimental period into three groups: ‘intact’ (pre-lesion), ‘early’ recovery stage, and ‘late’ recovery stage. We termed the border between early and late as the ‘full recovery day’, which we defined as the experimental day on which the success rate of precision grip first reached 100% (day 57, Monkey A; day 49, Monkey H). We tested the significance of the difference in the mean GC of the ROI between the Pre- and Post-DCZ sessions in each experimental day during the early recovery stage (n = 3 for Monkey A, n = 6 for Monkey H) or late recovery stage (n = 7 for Monkey A, n = 7 for Monkey H) by using the Wilcoxon sign-rank test (two-sided).
Dynamics of cortical activity
To evaluate the dynamics of cortical activity, we performed time-frequency analysis of the ECoG data17. We downsampled the data four times, resulting in a sampling rate of 500 Hz. We then aligned the ECoG signals from each channel at reaching onset. By using the MATLAB FieldTrip toolbox, we quantified the dynamics of cortical activation in each channel by the time-frequency representation generated by the Morlet wavelet transform method at 116 different center frequencies (5–120 Hz) with the half-length of the Morlet analyzing wavelet set at the coarsest scale of five samples. We normalized each time-frequency representation value by the baseline value (mean time-frequency representation value at the corresponding frequency during the resting period from –1.5 to –1 s).
To focus on a time window where activity was high in the ipsilesional PM in the early recovery stage, we set the time window around the movement onset (–0.2 to 0.2 s for Monkey A, –0.1 to 0.1 s for Monkey H), consistent with the Granger causality (GC) analysis. We chose a frequency range of 7–9 Hz for the region of interest (ROI), as the activity within the time window was at least 3 SD higher than the averaged activity of all frequency bands before DCZ administration in the early recovery stage (Fig. 4B, E). We calculated the mean normalized time-frequency representation of the ROI in each session of each experimental day. We tested the significance of the difference in the mean activity of the ROI between the Pre- and Post-DCZ sessions in each recovery stage (intact, n = 9 for Monkey A, n = 7 for Monkey H; early, n = 3 for Monkey A, n = 6 for Monkey H; late, n = 7 for Monkey A, n = 7 for Monkey H) by using the Wilcoxon sign-rank test (two-sided).
Electrical stimulation
We performed electrical stimulation experiments by using the ECoG electrodes several times before l-CST lesioning and once a week after lesioning. We trained the monkeys to sit on the monkey chair during stimulation under awake conditions. We delivered current pulses (monophasic, 3 pulses with 20 Hz, 3 ~ 4 mA, pulse duration: 0.5 ms) 20 ~ 30 times with a 2-s interval through a stimulator (Nihon Kohden, Tokyo, Japan). In response to stimulation, we recorded the muscle twitches in the ipsilesional forearm and CCEPs on the hemisphere opposite to the stimulated side. Throughout the entire experiment, the same two fixed experimenters together confirmed and recorded muscle contractions by observing and palpating the muscles. We evaluated the magnitude of muscle twitches in each body part by using the following criteria: (1) no response; (2) invisible muscle twitches (detected by palpation); (3) visible muscle twitches without joint movements; and (4) muscle twitches with joint movements (Fig. S7A–S7D). We calculated the baseline to first negative peak amplitude of the CCEPs and tested the significance of the difference in the amplitude between each recovery period by using one-way analysis of variance (ANOVA) and post hoc pairwise comparisons with Bonferroni’s correction (Fig. S7F).
We also evaluated the change in the amplitude of CCEPs recorded at the ipsilesional PM between before and after intramuscular DCZ administration (100 µg/kg). However, DCZ did not show any significant effect on CCEPs in any recovery stage (data not shown). Possible reasons we considered are as follows.
-
1.
DREADDs including hM4Di are expressed at the surface of cell bodies and axon terminals19. As electrical stimulation directly activates Na+ channels at the axon hillock and evokes action potentials, hM4Di expressed at the surface of the cell bodies does not affect CCEPs.
-
2.
hM4Di expression at the axon terminals might not be sufficiently high to change CCEPs, although it did affect spontaneous or physiological activity including the event-related activity shown in Fig. 3. One factor was that its expression with the double viral vector technique could be relatively low compared with single vector injection.
Histological assessment and anti-RFP immunohistochemistry
After the behavioral experiments were completed, we anaesthetized the monkeys deeply with thiopental sodium (25 mg/kg, i.v.) and perfused them transcardially with 0.1 M phosphate-buffered saline (PBS), followed by 4% paraformaldehyde in PBS.
We extracted and preserved the whole brain and cervical and upper thoracic spinal cord in 4% paraformaldehyde overnight for post-fixation. After saturation with 30% sucrose solution in PBS, we used a freezing microtome (Retoratome; Yamato Kohki Industrial, Saitama, Japan) to make serial sections (40-μm thick) of the brain (coronal) and spinal cord (axial).
We processed the brain sections for anti-RFP immunohistochemistry. Specifically, we incubated the sections with a rabbit anti-RFP antibody (1:2,000; Rockland Immunochemicals, Inc. Boyertown, PA, USA, 600-401-379, polyclonal, Lot: 42896) and then with a biotinylated goat anti-rabbit IgG antibody (1:200; Vector Laboratories, Burlingame, CA, USA, BA-1000, polyclonal, Lot: ZE0730). We visualized the immunoreactive signals with diaminobenzidine (1:10,000; Wako, Tokyo, Japan) containing 1% nickel sodium ammonium and 0.0003% H2O2 in Tris-buffered saline. We counterstained the sections with Neutral Red. We processed the spinal cord sections for Nissl staining with 0.1% cresyl violet to evaluate the size of the l-CST lesion.
To estimate the density of labeled neurons in the contralesional PM of each monkey, we manually counted the labeled neurons in every 12th section (every 480 µm), for a total of 15 sections per monkey using BZ-X Viewer v.1.03 (Keyence, Osaka, Japan) and the Cell Counter plugin in ImageJ 1.54 f (Wayne Rasband, US National Institutes of Health, rsb.info.nih.gov/ij/). The total number of labeled neurons in each section was shown (Fig. S1B left). To further investigate the distribution of the labeled neurons, we divided PM within each section into 1 mm2 regions and counted the number of cells within each ROI to estimate the cell density (Fig. S1B right).
Additionally, to estimate the density of the labeled fibers, we observed the ipsilesional PM and the bilateral putamen in every 12th section and photographed the regions where labeled fibers were most prominent in three different sections of each monkey using a 20x objective lens. We then manually traced the fibers with a consistent thickness and estimated the total fiber length by dividing the sum of the traced fiber pixels by the number of pixels for the thickness using ImageJ.
Experiments with callosotomy
We trained Monkey I to perform the reach and grasp task and then lesioned the l-CST at the right C4–C5. Before lesioning and during recovery, we administered DCZ (100 µg/kg) intramuscularly and measured the success rate of precision grip (Fig. S3F) to confirm that DCZ by itself did not affect task performance during recovery in a monkey without DREADD expression. We performed a partial callosotomy at the rostral part of the corpus callosum where the callosal fibers connect to the bilateral PMs during the early recovery stage (35 days after l-CST lesioning). Briefly, under the general anesthesia described above, we performed a craniotomy and incision of the dura mater at the vertex. We accessed the corpus callosum with gentle retraction of the right hemisphere and coagulated the corpus callosum between the bilateral PMs by using bipolar forceps. After callosotomy, we sutured the dura and skin.
We trained Monkey K to perform the task and it underwent the same partial callosotomy without l-CST lesioning to confirm that callosotomy in the intact state did not affect the success rate of the task (Fig. S3H).
Statistical analysis
We used MATLAB for statistical analyses. We used Wilcoxon rank-sum test, Wilcoxon sign-rank test, Pearson’s χ2 test or One-way ANOVA depending on the experimental design (see each section of “Methods”. We used post hoc pairwise comparisons with Bonferroni’s correction for One-way ANOVA. Values of P < 0.05 were considered significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The primary data described in the manuscript are available online at https://doi.org/10.6084/m9.figshare.26013223. Source data are provided with this paper.
Code availability
The codes for the main findings of this study are available online at https://doi.org/10.6084/m9.figshare.26013223.
References
Lawrence, D. G. & Kuypers, H. G. The functional organization of the motor system in the monkey. I. The effects of bilateral pyramidal lesions. Brain 91, 1–14 (1968).
Alstermark, B. et al. Motor command for precision grip in the macaque monkey can be mediated by spinal interneurons. J. Neurophysiol. 106, 122–126 (2011).
Blesch, A. & Tuszynski, M. H. Spinal cord injury: plasticity, regeneration and the challenge of translational drug development. Trends Neurosci. 32, 41–47 (2009).
Barker, R. A., Götz, M. & Parmar, M. New approaches for brain repair-from rescue to reprogramming. Nature 557, 329–334 (2018).
Fawcett, J. W. et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 45, 190–205 (2007).
Ward, N. S. Restoring brain function after stroke - bridging the gap between animals and humans. Nat. Rev. Neurol. 4, 244–255 (2017).
Nudo, R. J., Wise, B. M., SiFuentes, F. & Milliken, G. W. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science 272, 1791–1794 (1996).
Krajacic, A., Weishaupt, N., Girgis, J., Tetzlaff, W. & Fouad, K. Training-induced plasticity in rats with cervical spinal cord injury: effects and side effects. Behav. Brain. Res. 214, 323–331 (2010).
Grefkes, C. et al. Cortical connectivity after subcortical stroke assessed with functional magnetic resonance imaging. Ann. Neurol. 63, 236–246 (2008).
Yin, D. et al. Patterns in cortical connectivity for determining outcomes in hand function after subcortical stroke. PLoS One 7, e52727 (2012).
Liu, J., Qin, W., Zhang, J., Zhang, X. & Yu, C. Enhanced interhemispheric functional connectivity compensates for anatomical connection damages in subcortical stroke. Stroke 46, 1045–1051 (2015).
Dodd, K. C., Nair, V. A. & Prabhakaran, V. Role of the Contralesional vs. Ipsilesional Hemisphere in Stroke Recovery. Front. Hum. Neurosci. 11, 469 (2017).
Plow, E. B., Cunningham, D. A., Varnerin, N. & Machado, A. Rethinking stimulation of the brain in stroke rehabilitation: why higher motor areas might be better alternatives for patients with greater impairments. Neuroscientist 21, 225–240 (2015).
Nishimura, Y. et al. Time-dependent central compensatory mechanisms of finger dexterity after spinal cord injury. Science 318, 1150–1155 (2007).
Massai, E., Bonizzato, M., Jesus, I., Drainville, R. & Martinez, M. Cortical neuroprosthesis-mediated functional ipsilateral control of locomotion in rats with incomplete spinal cord injury. eLife 12, RP92940 (2023).
Brown, A. R. & Martinez, M. Ipsilesional motor cortex plasticity participates in spontaneous hindlimb recovery after lateral hemisection of the thoracic spinal cord in the rat. J. Neurosci. 38, 9977–9988 (2018).
Chao, Z. C., Sawada, M., Isa, T. & Nishimura, Y. Dynamic Reorganization of Motor Networks During Recovery from Partial Spinal Cord Injury in Monkeys. Cereb. Cortex 29, 3059–3073 (2019).
Kinoshita, M. et al. Genetic dissection of the circuit for hand dexterity in primates. Nature 487, 235–238 (2012).
Oyama, K. et al. Chemogenetic dissection of the primate prefronto-subcortical pathways for working memory and decision-making. Sci. Adv. 7, eabg4246 (2021).
Sasaki, R. et al. Balancing risk-return decisions by manipulating the mesofrontal circuits in primates. Science 583, 55–61 (2024).
Tohyama, T. et al. Contribution of propriospinal neurons to recovery of hand dexterity after corticospinal tract lesions in monkeys. Proc. Natl Acad. Sci. USA 114, 604–609 (2017).
Oguchi, M. et al. Double Virus Vector Infection to the Prefrontal Network of the Macaque Brain. PLoS One 10, e0132825 (2015).
Isa, T. Double viral vector intersectional approaches for pathway-selective manipulation of motor functions and compensatory mechanisms. Exp. Neurol. 349, 113959 (2022).
Armbruster, B. N., Li, X., Pausch, M. H., Herlitze, S. & Roth, B. L. Evolving the lock to fit the key to create a family of G protein-coupled receptors potently activated by an inert ligand. Proc. Natl Acad. Sci. USA 104, 5163–5168 (2007).
Alexander, G. M. et al. Remote control of neuronal activity in transgenic mice expressing evolved G protein-coupled receptors. Neuron 63, 27–39 (2009).
Wilson, C. J. Morphology and synaptic connections of crossed corticostriatal neurons in the rat. J. Comp. Neurol. 263, 567–580 (1987).
Ferino, F., Thierry, A. M., Saffroy, M. & Glowinski, J. Interhemispheric and subcortical collaterals of medial prefrontal cortical neurons in the rat. Brain Res 417, 257–266 (1987).
Nagai, Y. et al. Deschloroclozapine, a potent and selective chemogenetic actuator enables rapid neuronal and behavioral modulations in mice and monkeys. Nat. Neurosci. 23, 1157–1167 (2020).
von Stein, A. & Sarnthein, J. Different frequencies for different scales of cortical integration: from local gamma to long range alpha/theta synchronization. Int J. Psychophysiol. 38, 301–313 (2000).
Zazio, A., Miniussi, C. & Bortoletto, M. Alpha-band cortico-cortical phase synchronization is associated with effective connectivity in the motor network. Clin. Neurophysiol. 132, 2473–2480 (2021).
Matsumoto, R., et al Cortico-cortical evoked potentials. In: Deep brain stimulation and epilepsy. CRC Press, 105-111 (2020).
Sugiyama, Y. et al. Effects of early versus late rehabilitative training on manual dexterity after corticospinal tract lesion in macaque monkeys. J. Neurophysiol. 109, 2853–2865 (2013).
Kujirai, T. et al. Corticocortical inhibition in human motor cortex. J. Physiol. 471, 501–519 (1993).
Mochizuki, H., Huang, Y. Z. & Rothwell, J. C. Interhemispheric interaction between human dorsal premotor and contralateral primary motor cortex. J. Physiol. 561, 331–338 (2004).
Kawaguchi, Y. Receptor subtypes involved in callosally-induced postsynaptic potentials in rat frontal agranular cortex in vitro. Exp. Brain. Res. 88, 33–40 (1992).
Petreanu, L., Huber, D., Sobczyk, A. & Svoboda, K. Channelrhodopsin-2-assisted circuit mapping of long-range callosal projections. Nat. Neurosci. 10, 663–668 (2007).
Kitamura, A. et al. Sustained depolarizing shift of the GABA reversal potential by glutamate receptor activation in hippocampal neurons. Neurosci. Res. 62, 270–277 (2008).
Manganotti, P., Acler, M., Zanette, G. P., Smania, N. & Fiaschi, A. Motor cortical disinhibition during early and late recovery after stroke. Neurorehabil Neural Repair 22, 396–403 (2008).
Liepert, J., Storch, P., Fritsch, A. & Weiller, C. Motor cortex disinhibition in acute stroke. Clin. Neurophysiol. 111, 671–676 (2000).
Rickert, J. et al. Encoding of movement direction in different frequency ranges of motor cortical local field potentials. J. Neurosci. 25, 8815–8824 (2005).
Leuthardt, E. C., Schalk, G., Wolpaw, J. R., Ojemann, J. G. & Moran, D. W. A brain-computer interface using electrocorticographic signals in humans. J. Neural Eng. 1, 63–71 (2004).
Klimesch, W., Sauseng, P. & Hanslmayr, S. EEG alpha oscillations: the inhibition-timing hypothesis. Brain Res Rev. 53, 63–88 (2007).
Wildegger, T., van Ede, F., Woolrich, M., Gillebert, C. R. & Nobre, A. C. Preparatory α-band oscillations reflect spatial gating independently of predictions regarding target identity. J. Neurophysiol. 117, 1385–1394 (2017).
Cisek, P., Crammond, D. J. & Kalaska, J. F. Neural activity in primary motor and dorsal premotor cortex in reaching tasks with the contralateral versus ipsilateral arm. J. Neurophysiol. 89, 922–942 (2003). PMID: 12574469.
Ganguly, K. et al. Cortical representation of ipsilateral arm movements in monkey and man. J. Neurosci. 29, 12948–12956 (2009).
Ulloa, J. L. The Control of Movements via Motor Gamma Oscillations. Front Hum. Neurosci. 15, 787157 (2022).
Gross, J. et al. Task-dependent oscillations during unimanual and bimanual movements in the human primary motor cortex and SMA studied with magnetoencephalography. Neuroimage 26, 91–98 (2005).
Cheyne, D., and Ferrari, P. MEG studies of motor cortex gamma oscillations: evidence for a gamma “fingerprint” in the brain? Front Hum Neurosci. https://doi.org/10.3389/fnhum.2013.00575. 575, (2013)
Alhourani, A. et al. Subthalamic Nucleus Activity Influences Sensory and Motor Cortex during Force Transduction. Cereb. Cortex 30, 2615–2626 (2020).
Xu, J. et al. and SMARTS Study Group. Rethinking interhemispheric imbalance as a target for stroke neurorehabilitation. Ann. Neurol. 85, 502–513 (2019).
Sawada, M. et al. Reorganization of corticospinal projections after prominent recovery of finger dexterity from partial spinal cord injury in macaque monkeys. eNeuro 10, 0209–0223 (2023).
Nagai, Y. et al. PET imaging-guided chemogenetic silencing reveals a critical role of primate rostromedial caudate in reward evaluation. Nat. Commun. 6, 13605 (2016).
Jeurissen, D., Shushruth, S., El-Shamayleh, Y., Horwitz, G. D. & Shadlen, M. N. Deficits in decision-making induced by parietal cortex inactivation are compensated at two timescales. Neuron 110, 1924–1931 (2022).
Sawada, M. et al. Function of the nucleus accumbens in motor control during recovery after spinal cord injury. Science 350, 98–101 (2015).
Sano, H., Kobayashi, K., Yoshioka, N., Takebayashi, H. & Nambu, A. Retrograde gene transfer into neural pathways mediated by adeno-associated virus (AAV)-AAV receptor interaction. J. Neurosci. Methods 345, 108887 (2020).
Bobo, R. H. et al. Convection-enhanced delivery of macromolecules in the brain. Proc. Natl Acad. Sci. USA 91, 2076–2080 (1994).
Yu, Z., Nurmikko, A. & Ozden, I. Widespread functional opsin transduction in the rat cortex via convection-enhanced delivery optimized for horizontal spread. J. Neurosci. Methods 291, 69–82 (2017).
Weiss, A. R., Liguore, W. A., Domire, J. S., Button, D. & McBride, J. L. Intra-striatal AAV2.retro administration leads to extensive retrograde transport in the rhesus macaque brain: implications for disease modeling and therapeutic development. Sci. Rep. 24, 6970 (2020).
Cushnie, A. K. et al. Using rAAV2-retro in rhesus macaques: Promise and caveats for circuit manipulation. J. Neurosci. Methods 1, 108859 (2020).
Mathis, A. et al. DeepLabCut: markerless pose estimation of user-defined body parts with deep learning. Nat. Neurosci. 21, 1281–1289 (2018).
Kamiński, M., Ding, M., Truccolo, W. A. & Bressler, S. L. Evaluating causal relations in neural systems: Granger causality, directed transfer function and statistical assessment of significance. Biol. Cybern. 85, 145–157 (2001).
Oostenveld, R., Fries, P., Maris, E. & Schoffelen, J. M. FieldTrip: open source software for advanced analysis of MEG, EEG, and invasive electrophysiological data. Comput. Intell. Neurosci. 2011, 156869 (2011).
Ding, M., Bressler, S. L., Yang, W. & Liang, H. Short-window spectral analysis of cortical event-related potentials by adaptive multivariate autoregressive modelling: data preprocessing, model validation, and variability assessment. Biol. Cybern. 83, 35–45 (2000).
Acknowledgements
We thank Masashi Nakamura and Erika Omae for technical assistance. We thank Bryan Roth for providing the plasmid. The monkeys used in this study were provided by the National BioResource Project of the Ministry of Education, Culture, Sports, Science, and Technology of Japan (MEXT). This work was supported by a Grant-in-Aid for Scientific Research on Innovative Areas ‘Hyper-adaptability’ to T.I. (Project no. 19H05723), a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology (MEXT) to T.I. (KAKENHI (A) no. 19H01011 and (S) no. 22H04992), Japan Agency for Medical Research and Development (JP18dm0307005 to N.S. and T.I.), and a Grant-in-Aid for Scientific Research from MEXT to H.O. (KAKENHI (A) no. 20H00573) and to R.Y. (KAKENHI (B) no. 21H02798).
Author information
Authors and Affiliations
Contributions
M.M., R.Y., and T.I. designed the experiments with contributions from H.O. and R.T. as well. K.K. designed and produced the viral tools. M.M., R.Y., T.K., S.U., Y.S., and H.O. performed the surgeries. M.M., R.Y., T.K., S.U., and Y.S. conducted the behavioral and electrophysiological experiments. M.M., S.U., K.I., H.O., and J.T. conducted the histological and imaging experiments. M.M., R.Y., and S.U. analysed the experimental data. R.T. and T.I. supervised the study. M.M. and T.I. wrote the manuscript with input from all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mitsuhashi, M., Yamaguchi, R., Kawasaki, T. et al. Stage-dependent role of interhemispheric pathway for motor recovery in primates. Nat Commun 15, 6762 (2024). https://doi.org/10.1038/s41467-024-51070-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-024-51070-w
This article is cited by
-
Advances in chemogenetics: a review of DREADDs and its application in psychiatric disorders
Molecular Psychiatry (2025)