Abstract
Public health guidelines recommend exercise as a key lifestyle intervention for promoting and maintaining healthy sleep function and reducing disease risk. However, strenuous evening exercise may disrupt sleep due to heightened sympathetic arousal. This study examines the association between strenuous evening exercise and objective sleep, using data from 14,689 physically active individuals who wore a biometric device during a one-year study interval (4,084,354 person-nights). Here we show later exercise timing and higher exercise strain are associated with delayed sleep onset, shorter sleep duration, lower sleep quality, higher nocturnal resting heart rate, and lower nocturnal heart rate variability. Regardless of strain, exercise bouts ending ≥4 hours before sleep onset are not associated with changes in sleep. Our results suggest evening exercise—particularly involving high exercise strain—may disrupt subsequent sleep and nocturnal autonomic function. Individuals aiming to improve sleep health may benefit from concluding exercise at least 4 hours before sleep onset or electing lighter strain exercises within this window.
Similar content being viewed by others
Introduction
The relationship between exercise and sleep is symbiotic and complex. Theoretical models of healthy sleep function point to a number of physiological and psychological processes implicated in the sleep-promoting benefits of exercise, including the regulation of core body temperature1, mood2, metabolic expenditure3, and the circadian system4. However, acute strenuous exercise performed close to bedtime may induce prolonged sympathetic activation, e.g., increased heart and respiration rate, and therefore disrupt sleep5,6. As a result, traditional and contemporary sleep guidelines have discouraged strenuous exercise in the hours before bedtime7,8,9.
Recent meta-analytical evidence contradicts the view that evening exercise disrupts sleep. Engaging in evening exercise generally10 and high-intensity evening exercise specifically11 was not associated with decreases in sleep duration or quality. Although studies have examined the effects of evening exercise intensity or duration in isolation12, no studies to our knowledge have examined the combination of exercise intensity and duration (i.e., exercise strain). High intensity, long duration (i.e., strenuous) evening exercise is metabolically demanding and may result in an inadequate recovery window before bedtime, limiting the brain and body’s ability to return to the psychophysiological conditions compatible with sleep13. Indeed, researchers who have systematically reviewed the evening exercise literature have recommended future studies focus on the intensity by duration interaction2,14, particularly given most past studies included only lower levels of exercise strain10.
High exercise strain (i.e., cardiometabolic demand) is characterized by increased sympathetic activity15, e.g., increased excess post-exercise oxygen consumption16, core body temperature17, heart rate18, and cognitive arousal19. Following exercise, the autonomic nervous system (ANS) facilitates sympathetic withdrawal and parasympathetic re-activation20. Importantly, high strain exercise significantly slows this autonomic process towards resting homeostasis15,21. Swift parasympathetic re-activation at night is important as sleep is characterized by increasing parasympathetic (and declining sympathetic) activity22. This raises the question whether strenuous exercise near sleep onset results in heightened sympathetic activity and delayed parasympathetic re-activation, which could delay or impair sleep23.
Here, in a large multi-national sample of physically active adults, we examined the influence of exercise strain on the association between exercise timing and objectively measured sleep and nocturnal autonomic activity using a validated24 wrist-worn biometric device in free-living conditions. We hypothesised the combination of later exercise timing and higher exercise strain would be dose-dependently associated with disruptions to sleep (e.g., delayed sleep onset, shorter sleep duration, lower sleep quality) and nocturnal autonomic activity (e.g., increased resting heart rate [RHR] and decreased heart rate variability [HRV]).
Results
Demographics
The study population included 14,689 participants logging an average of 122.98 exercises (SD = 53.74) across the 1-year study. Baseline characteristics (Table S1) included age (M = 37.89, SD = 10.81), gender (10,845 [73.83%] men), weight (M = 80.39 kilograms, SD = 15.10), and height (1.76 meters, SD = 0.94).
Exercise timing relative to habitual sleep onset
Tables S2–6 present estimated marginal means (EMMs) and Tables S7-11 present strain vs. no-exercise contrasts for all analyses.
Sleep onset
When exercise concluded ≥6-h before social jet lag- and seasonality-adjusted habitual sleep onset (i.e., the average sleep onset corresponding to weekdays or weekends, as appropriate, across the calendar month), maximal exercise was associated with earlier sleep onset compared to lower levels of strain and non-exercise days. When exercise concluded 4- to 6-h before habitual sleep onset, sleep onset following light or moderate exercise was similar to non-exercise days. When exercise concluded 4-h before to 2-h after habitual sleep onset, sleep onset became progressively later for all levels of strain and was more pronounced when strain was higher. Engaging in maximal exercise instead of light exercise is associated with a 36.0-minute later sleep onset if the exercise ended 2-h before habitual sleep onset, and an 80.0-minute later sleep onset if the exercise ended 2-h after habitual sleep onset (Fig. 1A; Table 1).
GAMMs demonstrating the relationship between exercise timing relative to habitual sleep onset and A sleep onset, B sleep duration (in hours), C sleep quality, D nocturnal RHR, and E nocturnal HRV at different levels of exercise strain. Exercise group lines (measure of centre) represent GAMM estimates. Shaded area surrounding each exercise strain group line represents 95% confidence intervals. Horizontal grey dashed line indicates the mean outcome variable on no exercise days. Vertical black dotted line indicates habitual sleep onset. Source data are provided as a Source Data file.
Sleep duration
When exercise concluded ≥6-h before habitual sleep onset, exercise strain was positively correlated with sleep duration. In contrast, when exercise concluded 6-h before to 2-h after habitual sleep onset, sleep duration progressively reduced for all levels of strain and was more pronounced when strain was higher. Engaging in maximal exercise instead of light exercise is associated with a 5.4% (22.2 minute) shorter sleep duration if the exercise ended 2-h before habitual sleep onset, and a 13.9% (42.6 minute) shorter sleep duration if the exercise ended 2-h after habitual sleep onset (Fig. 1B; Table 2).
Sleep quality
When exercise concluded ≤8-h before habitual sleep onset, increased strain was associated with decreased sleep quality. When exercise concluded 2-h before to 2-h after habitual sleep onset, sleep quality became progressively worse for all levels of strain and was more pronounced when strain was higher. Engaging in maximal exercise instead of light exercise is associated with a 0.87 percentage point decrease in sleep quality if the exercise ended 2-h before habitual sleep onset, and a 5.6 percentage point decrease in sleep quality if the exercise ended 2-h after habitual sleep onset (Fig. 1C; Table 3).
Nocturnal RHR
Regardless of when exercise concluded, higher strain was associated with higher RHR. All levels of exercise strain were associated with higher RHR compared to non-exercise days. When exercise concluded 4-h before to 2-h after habitual sleep onset, RHR became progressively higher for all levels of strain and was more pronounced when strain was higher. Engaging in maximal exercise instead of light exercise is associated with a 6.8% (3.9 beats/min) increase in RHR if the exercise ended 2-h before habitual sleep onset, and a 15.0% (9.4 beats/min) increase in RHR if the exercise ended 2-h after habitual sleep onset (Fig. 1D; Table 4).
Nocturnal HRV
Regardless of when exercise concluded, higher strain was associated with lower HRV. All levels of exercise strain were associated with lower HRV compared to non-exercise days. When moderate, high, and maximal exercise concluded 4-h before to 2-h after habitual sleep onset, HRV became progressively lower and was more pronounced when strain was higher. When light exercise concluded 2-h before to 2-h after habitual sleep onset, HRV became progressively lower. Engaging in maximal exercise instead of light exercise is associated with a 14.1% (8.3 unit) decrease in HRV if the exercise ended 2-h before habitual sleep onset, and an 32.6% (14.6 unit) decrease in HRV if the exercise ended 2-h after habitual sleep onset (Fig. 1E; Table 5).
Exercise timing relative to actual sleep onset
Secondary analyses examining exercise timing to actual sleep onset were consistent with the primary analyses above. Specifically, the combination of higher exercise strain and later exercise timing relative to actual sleep onset that night was dose-dependently associated with shorter sleep duration, lower sleep quality, higher nocturnal RHR, and lower nocturnal HRV (Fig. 2A-D).
GAMMs demonstrating the relationship between exercise timing relative to actual sleep onset and A sleep duration (in hours), B sleep quality, C nocturnal RHR, and D nocturnal HRV at different levels of exercise strain. Exercise group lines (measure of centre) represent GAMM estimates. Shaded area surrounding each exercise strain group line represents 95% confidence intervals. Horizontal grey dashed line indicates the mean outcome variable on no exercise days. Source data are provided as a Source Data file.
Exploratory analyses: gender, age, and BMI status
The associations of interest between exercise timing and strain, and sleep and nocturnal autonomic activity did not differ across gender (Figs. S1 and S2), age (Figs. S3 and S4), or BMI status (Figs. S5 and S6).
Discussion
This large-cohort, multi-national study examined whether exercise strain and exercise timing would demonstrate dose-response relationships with objective sleep and nocturnal autonomic activity in free-living conditions. Results showed the combination of higher exercise strain and later exercise timing was dose-dependently associated with delayed sleep onset, shorter sleep duration, lower sleep quality, higher RHR, and lower HRV. Evening exercise—particularly involving high levels of cardiovascular strain—may disrupt subsequent sleep and nocturnal autonomic function, thereby impairing a critical stage of the recovery process25.
Our findings are consistent with research on physiological recovery after exercise. The dynamic recovery duration (i.e., time-course of parasympathetic re-activation) is proportionate to the level of homeostatic stress of the exercise session15. We found higher levels of exercise strain were associated with increased nocturnal RHR and decreased nocturnal HRV several hours after exercise cessation. The initiation and maintenance of healthy sleep function is characterized by parasympathetic activity (e.g., declines in RHR and core body temperature, increases in HRV)22,26. Therefore, when parasympathetic re-activation is disrupted due to increased exercise strain or later exercise timing, sleep may be both delayed in timing and impaired in quality. To minimise disruptions to sleep, individuals should allow for adequate recovery time proportionate to the level of strain achieved in an evening exercise session.
When exercise concluded 6–10 hours before habitual sleep onset, nocturnal HRV was slightly lower compared to non-exercise days. These differences were strain-dependent and minimal (e.g., a 1.56–4.52 unit decrease in HRV), suggesting healthy nocturnal autonomic functioning under these conditions. Nonetheless, this finding aligns with prior research demonstrating that the time required for complete autonomic recovery from a single exercise session can exceed 24 hours, especially following strenuous exercise27. Future research should examine how continuous measures of HRV recovery following exercise relate to subsequent sleep, and whether this relationship is moderated by successive days of high strain exercise. Strenuous evening exercise may also be associated with behavioural consequences that can impair sleep. Pre- and post-exercise dietary intake, including caffeine-containing beverages, carbohydrate-rich foods, and alcohol can negatively impact sleep28,29,30. Evening exercise may also occur in environments that expose individuals to bright light (e.g., 24-h gyms, elite sport competitions), which delays the timing of the circadian clock and suppresses release of the sleep-promoting hormone melatonin.
When light or moderate strain exercise ended more than ~2-h before habitual sleep onset, sleep onset and sleep quality were similar to non-exercise nights. These findings are consistent with recent meta-analyses that reported null effects of evening exercise on sleep10,11. Importantly, 82% of the studies meta-analysed would be categorized as light or moderate strain. We extend on this prior work by demonstrating higher strain evening exercise may be detrimental to sleep and autonomic functioning.
This study has important implications for exercise timing and sleep health recommendations. Our findings suggest that to optimize sleep timing, duration, and quality, when possible, individuals should stop exercising four or more hours before their habitual—or actual—sleep onset. When evening exercise is unavoidable, individuals could select lighter stain exercises to mitigate sleep disruption. Based on our data, opting for light strain exercise instead of maximal strain exercise ending 2-h before habitual sleep onset is associated with a 36.0-minute earlier sleep onset, 5.4% increase in sleep duration, 6.8% decrease in nocturnal RHR, and 14.1% increase in nocturnal HRV. Interestingly, prior research has demonstrated high intensity exercise can mitigate some of the adverse effects of sleep loss, such as impaired glucose tolerance31 and insulin resistance32. These findings highlight the complex relationship between sleep, exercise, and health and suggest future investigations require nuanced interpretation.
Contrary to previous sleep health guidelines that discourage exercise at night, recent guidelines are less conservative, suggesting, for example, that moderate-intensity exercise ending at least 90-minutes before bedtime will not delay or disrupt sleep33. However, these guidelines do not mention the duration of permissible moderate-intensity evening exercise; a critical consideration when quantifying exercise strain. Although short duration, moderate-intensity (i.e., light strain) evening exercise may not affect sleep34, our findings suggest that longer duration, moderate-intensity evening exercise that achieves sufficiently high levels of strain may be detrimental to sleep. Importantly, exercise of any strain, but particularly higher strain, occurring after habitual sleep onset was associated with stark disruptions to sleep and autonomic activity. This finding has important implications for elite and professional athletes, as many competitions that require high and maximal levels of strain are scheduled in the evening due to broadcasting rights. These evening competitions may be jeopardizing athlete sleep and recovery on nights it is needed most.
The present study had limitations that should be considered. The biometric device did not detect when sleep was first attempted; therefore, we were unable to estimate the time participants began to attempt sleep or calculate sleep onset latency. Future research could collect self-reported timing of attempted sleep or use behavioural devices that record conscious responses to stimuli to investigate whether heightened sympathetic arousal associated with strenuous evening exercise increases sleep onset latency. The summated-heart-rate-zones score (SHRZS) method for quantifying exercise strain may underestimate the relative metabolic strain of strength training that involves very brief durations of high-effort movements. Future research could examine the effects of different types of evening strength training (e.g., Olympic lifting). We were unable to control for potential confounds known to impact sleep, such as bright light exposure. Although we can take some confidence in our results given we observed a consistent dose-response relationship in the evening and bright light exposure likely does not covary with exercise strain, future research could measure and control for light exposure. Finally, election of only physically active adults created a sample that is not representative across the spectrum of physical activity levels. Future research could explore the extent to which our findings apply to the lower end of the physical activity spectrum. We predict the relationship between strenuous evening exercise and sleep to be even stronger in this group, as post-exercise autonomic recovery typically occurs less rapidly in individuals who train less frequently21, have lower levels of cardiovascular fitness27, and have lower resting vagal control35.
This study had several strengths. Previous studies on evening exercise and sleep have relied on small sample sizes (M = 12 participants/study)10 for brief periods, often in laboratory settings. This study examined data from a large sample (14,689 physically active participants) across one year (4,084,354 person-nights) in a real-world setting. These free-living conditions allowed participants to engage in exercises that varied widely in exercise strain. The analyses controlled for important individual differences in sleep and exercise strain. For example, instead of using clock time, exercise timing was calculated relative to each individual’s habitual sleep onset on a given day (thus considering individual, seasonal, and weekday changes in sleep timing) as well as each individual’s actual sleep onset on that night (Fig. 2). Similarly, exercise strain was quantified from real (as opposed to planned) exercise relative to each individual’s cardiovascular fitness level.
This large cohort study of ~4-million-person-nights demonstrates that exercise strain and exercise timing have dose-response relationships with sleep and autonomic activity. To optimize sleep, individuals should aim to complete bouts of exercise four or more hours before their sleep onset to minimise potential adverse consequences to their sleep. If exercising within a 4-h window of sleep onset, individuals could elect to engage in light strain exercises to mitigate sleep and ANS disruption. This study has significant implications for public health messaging around timing, duration, and intensity of exercise and presents a critical step towards improving population sleep health.
Methods
This large retrospective cohort study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines and was approved by Monash University Human Research Ethics Committee (#32928).
Study design, population, and data collection
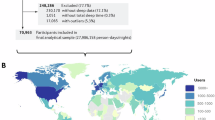
Data from 14,689 subscribers to the biometric device platform WHOOP, Inc. (Boston, MA) were collected across a 1-year study (Sep 1, 2021 to Aug 31, 2022). During registration with WHOOP, participants reported their age and gender and provided written informed consent to allow the use of their deidentified data for research. Due to confidentiality considerations, we did not have access to location data. Participant characteristics are presented in Table S1. Eligibility criteria required participants be ≥18 years of age, wear the biometric device for a minimum of 350 days (95.6% of total possible wear-time), and register ≥50 exercise activities within the analysis window of 10-h before to 2-h after habitual sleep onset to construct a sample of physically active individuals (i.e., with an exercise frequency of approximately one or more activities weekly) and to allow for within-person comparisons of different exercise timings and levels of exercise strain. Exercises outside this window were excluded. The final dataset included 4,084,354 person-nights of data (Fig. 3 presents CONSORT flow diagram). Table S12 includes demographic information for the included and excluded participants.
A multi-sensor wrist-worn biometric device (WHOOP versions 3.0 or 4.0; Boston, MA) that captures continuous heart rate, accelerometer, and three-axis gyroscope data was used to derive exercise, cardiovascular, and sleep/wake metrics. This biometric device has been validated against electrocardiography and polysomnography for the assessment of heart rate (99% agreement) and 2-stage sleep categorisation (86–89% agreement), respectively24,36.
Exercise timing
Exercise timing was operationalised using two reference points. In the primary analysis, exercise timing represented the conclusion of exercise relative to the participant’s habitual sleep onset. Individuals display a high degree of heterogeneity in sleep/wake timing37. What constitutes an evening exercise will depend on the typical sleep/wake patterns of the individual. Further, an individual’s sleep/wake timing can vary by season38 and by weekday/weekend37. Therefore, habitual sleep onset was quantified as the participant’s mean sleep onset of the corresponding calendar month and whether it was a weekday or weekend to account for seasonal variation and social jet lag. In the secondary analysis, exercise timing represented the conclusion of exercise relative to the participant’s sleep onset on that night. This method provides important context for how long it can take to recover from varying levels of exercise strain before sleep.
Exercise strain
Exercise activities were logged manually on the WHOOP smartphone app or detected automatically by the WHOOP analytics platform and then confirmed by the participant. Multiple exercise activities logged within 60-minutes of each other were treated as one activity. Activities less than 1-minute in duration and relaxation exercises, including yoga, stretching, meditation, and massage therapy were excluded from the analysis. Continuous heart rate data during each exercise activity were used to calculate durations spent in six heart rate zones (zones 0-5). Heart rate zones were determined as a percentage of the participant’s maximal heart rate (HRmax), where zone 0 = < 50% of HRmax, zone 1 = 50–60%, zone 2 = 60–70%, zone 3 = 70–80%, zone 4 = 80–90%, and zone 5 = 90–100%. HRmax was determined using the non-linear formula, 192–0.007 × age[239, or manually set by the participant, or automatically set to the maximal recorded heart rate.
Exercise strain was quantified using summated-heart-rate-zones scores (SHRZS)40. The duration (minutes) spent in each heart rate zone was multiplied by a corresponding factor for each zone (i.e., zone 1 = 1; zone 2 = 2; etc.) and then summated. This method has an open-source formula that can be replicated in future studies using any device that accurately records heart rate. SHRZS were then categorized into four groups designed to reflect common groups of exercises that vary in cardiometabolic load and that based on our hypothesis would be expected to impact subsequent sleep differently: <116=light; 116 to <214=moderate; 214 to 461=high; >461=maximal (Table 6).
Nocturnal autonomic activity markers and sleep metrics
Nocturnal RHR and HRV were calculated using a weighted average over the sleep period (i.e., from sleep onset to sleep offset), giving more weight to periods of slow wave sleep, as slow wave sleep is typically characterized by parasympathetic dominance22. Slow wave sleep was automatically detected using WHOOP’s analytics platform. PPG-derived RHR was quantified as the mean number of heart beats/minute. PPG-derived HRV was quantified as the resting root mean square of successive beat to beat interval differences (RMSSD). Sleep metrics were derived from biometric device data and automatically detected using WHOOP’s analytics platform and included sleep timing (sleep onset), duration (total sleep time), and quality (sleep percentage; [Sleep Period – wake after sleep onset]/Sleep Period).
Statistical analysis
Analyses were performed in R (v4.2.0)41. We fit generalized additive mixed models (GAMMs) which use nonparametric smoothing functions to examine the nonlinear (e.g., dose-response) relationship between exercise timing and sleep at different levels of exercise strain42.
Smoothing terms for exercise timing at each level of exercise strain were included in the model. Exercise strain was included as an ordered fixed factor with five levels (no exercise; low; moderate; high; maximal). Covariates included weekday vs. weekend, prior night’s outcome variable, participant general fitness (mean daily exercise strain), gender, and a smoothing term for age as there are nonlinear changes in sleep by age43. Results were averaged across all covariates. A random intercept by participant identifier was included to account for non-independence.
Smoothing functions were plotted and used for interpretation of the GAMMs. Estimated marginal means (EMMs) at 2-h intervals were compared using two contrast techniques. First, we used a consecutive contrast method that allows for testing the dose-response relationship between exercise strain and sleep/autonomic activity. This contrast method compares 1.) no exercise to light strain; 2.) light strain to moderate strain; 3.) moderate strain to high strain; and 4.) high strain to maximal strain, at each 2-h interval of exercise timing. Second, a treatment vs. control contrast method was used to compare exercise strain levels to the no exercise reference mean. Contrast estimates reflect estimated absolute differences, providing information about real-world importance and effect size beyond statistical significance. Multivariate t-distribution adjustment method was used to adjust for multiple comparisons. Given the large sample size, a p-value of 0.005 was used to determine statistical significance44.
Exploratory analyses were also conducted to examine whether the findings vary across demographic groups. The primary analyses were repeated stratified across gender (Figs. S1 and S2), age (Figs. S3 and S4), and BMI status (Figs. S5 and S6). Finally, we conducted a sensitivity analysis excluding the week following the start and the week following the end of daylight saving time, as prior research suggests catch-up sleep occurs after clock transitions45. The results did not change.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The dataset associated with this study comprises regularly collected physiological and healthcare data as well as demographic information and is stored in a proprietary repository. Given its sensitive nature and the potential for reidentification, access to the dataset is enforced through an application process. For inquiries regarding data access, please contact support@whoop.com. All data requests will be assessed and addressed in accordance with policies designed to safeguard participant and user confidentiality, as outlined in the terms and conditions and informed consent documentation. The timeframe for response to requests will be four weeks. Source data are provided with this paper.
Code availability
Data organization and analysis was performed in R (v4.2.0). The analysis code is available at https://doi.org/10.5281/zenodo.14933997.
Change history
27 October 2025
The wrong Peer Review File was originally published with this article; it has now been replaced with the correct. The original article has been corrected.
References
Siegel, J. M. Sleep function: an evolutionary perspective. Lancet Neurol. 21, 937–946 (2022).
Youngstedt, S. D., Passos, G. S. & Santana, M. G. Nighttime vigorous exercise: Is lack of sleep disruption good enough? Sleep. Med. Rev. 60, 101560 (2021).
Berger, R. & Phillips, N. Comparative aspects of energy metabolism, body temperature and sleep. Acta Physiol. Scand. Suppl. 574, 21–27 (1988).
Wolff, C. A. & Esser, K. A. Exercise timing and circadian rhythms. Curr. Opin. Physiol. 10, 64–69 (2019).
Oda, S. & Shirakawa, K. Sleep onset is disrupted following pre-sleep exercise that causes large physiological excitement at bedtime. Eur. J. Appl Physiol. 114, 1789–1799 (2014).
Roberts, S. S. H., Teo, W.-P. & Warmington, S. A. Effects of training and competition on the sleep of elite athletes: a systematic review and meta-analysis. Br. J. Sports Med. 53, 513–522 (2019).
European Academy of Sleep Medicine. The international classification of sleep disorders: diagnostic and coding manual. (American Academy of sleep medicine, 2005).
Association, A. S. American Sleep Association (ASA) Sleep hygiene tips - research & treatments American sleep assoc https://www.sleepassociation.org/about-sleep/sleep-hygiene-tips/ (2023).
Zarcone, V. Sleep hygiene. I.: Kryger M. H., Roth T., Dement W. C., red. Principles and Practice of Sleep Medicine. (Philadelphia: WB Saunders Company, 1994).
Stutz, J., Eiholzer, R. & Spengler, C. M. Effects of evening exercise on sleep in healthy participants: a systematic review and meta-analysis. Sports Med 49, 269–287 (2019).
Frimpong, E., Mograss, M., Zvionow, T. & Dang-Vu, T. T. The effects of evening high-intensity exercise on sleep in healthy adults: A systematic review and meta-analysis. Sleep. Med. Rev. 60, 101535 (2021).
Kredlow, M. A., Capozzoli, M. C., Hearon, B. A., Calkins, A. W. & Otto, M. W. The effects of physical activity on sleep: a meta-analytic review. J. Behav. Med. 38, 427–449 (2015).
Driver, H. S. & Taylor, S. R. Exercise and sleep. Sleep. Med. Rev. 4, 387–402 (2000).
Yue, T., Liu, X., Gao, Q. & Wang, Y. Different intensities of evening exercise on sleep in healthy adults: a systematic review and network meta-analysis. Nat. Sci. Sleep. 14, 2157–2177 (2022).
Mann, T. N., Webster, C., Lamberts, R. P. & Lambert, M. I. Effect of exercise intensity on post-exercise oxygen consumption and heart rate recovery. Eur. J. Appl. Physiol. 114, 1809–1820 (2014).
Gore, C. & Withers, R. Effect of exercise intensity and duration on postexercise metabolism. J. Appl. Physiol. 68, 2362–2368 (1990).
Sawka, M. N., Wenger, C. B. & Pandolf, K. B. Thermoregulatory responses to acute exercise‐heat stress and heat acclimation. Compr. Physiol. 14(Suppl.), 157–185 (2011).
Presby, D. M., Jasinski, S. R. & Capodilupo, E. R. Wearable derived cardiovascular responses to stressors in free-living conditions. PLoS One 18, e0285332 (2023).
Gupta, L., Morgan, K. & Gilchrist, S. Does elite sport degrade sleep quality? A systematic review. Sports Med. 47, 1317–1333 (2017).
Borresen, J. & Lambert, M. I. Autonomic control of heart rate during and after exercise: measurements and implications for monitoring training status. Sports Med. 38, 633–646 (2008).
Seiler, S., Haugen, O. & Kuffel, E. Autonomic recovery after exercise in trained athletes: intensity and duration effects. Med. Sci. Sports Exerc. 39, 1366 (2007).
Zoccoli, G. & Amici, R. Sleep and autonomic nervous system. Curr. Opin. Physiol. 15, 128–133 (2020).
Hynynen, E., Vesterinen, V., Rusko, H. & Nummela, A. Effects of moderate and heavy endurance exercise on nocturnal HRV. Int. J. Sports Med. 31, 428–432 (2010).
Miller, D. J., Sargent, C. & Roach, G. D. A validation of six wearable devices for estimating sleep, heart rate and heart rate variability in healthy adults. Sensors 22, 6317 (2022).
Walsh, N. P. et al. Sleep and the athlete: narrative review and 2021 expert consensus recommendations. Br. J. Sports Med. 55, 356–368 (2021).
Okamoto-Mizuno, K. et al. Heart rate variability and body temperature during the sleep onset period. Sleep. Biol. Rhythms 6, 42–49 (2008).
Stanley, J., Peake, J. M. & Buchheit, M. Cardiac parasympathetic reactivation following exercise: implications for training prescription. Sports Med. 43, 1259–1277 (2013).
Afaghi, A., O’Connor, H. & Chow, C. M. High-glycemic-index carbohydrate meals shorten sleep onset. Am. J. Clin. Nutr. 85, 426–430 (2007).
Gardiner, C. et al. The effect of caffeine on subsequent sleep: A systematic review and meta-analysis. Sleep. Med. Rev. 69, 101764 (2023).
Halson, S. L. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. 44, 13–23 (2014).
Saner, N. J. et al. Exercise mitigates sleep-loss-induced changes in glucose tolerance, mitochondrial function, sarcoplasmic protein synthesis, and diurnal rhythms. Mol. Metab. 43, 101110 (2021).
de Souza, J. F., Dáttilo, M., de Mello, M. T., Tufik, S. & Antunes, H. K. High-intensity interval training attenuates insulin resistance induced by sleep deprivation in healthy males. Front. Physiol. 8, 992 (2017).
Pacheco, D. The best time of day to exercise for sleep. https://www.sleepfoundation.org/physical-activity/best-time-of-day-to-exercise-for-sleep (2021).
Miller, D. et al. Moderate-intensity exercise performed in the evening does not impair sleep in healthy males. Eur. J. Sport Sci. 20, 80–89 (2020).
Cunha, F. A., Midgley, A. W., Gonçalves, T., Soares, P. P. & Farinatti, P. Parasympathetic reactivation after maximal CPET depends on exercise modality and resting vagal activity in healthy men. SpringerPlus 4, 1–9 (2015).
Miller, D. J. et al. A validation study of the WHOOP strap against polysomnography to assess sleep. J. Sports Sci. 38, 2631–2636 (2020).
Roenneberg, T., Wirz-Justice, A. & Merrow, M. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythms 18, 80–90 (2003).
Yetish, G. et al. Natural sleep and its seasonal variations in three pre-industrial societies. Curr. Biol. 25, 2862–2868 (2015).
Gellish, R. L. et al. Longitudinal modeling of the relationship between age and maximal heart rate. Med. Sci. Sports Exerc. 39, 822–829 (2007).
Borresen, J. & Lambert, M. I. The quantification of training load, the training response and the effect on performance. Sports Med. 39, 779–795 (2009).
Team, R. Developement Core. R: A language and environment for statistical computing. (2010).
Hastie, T. J. Generalized additive models in Statistical models in S 249-307 (Routledge, 2017).
Carrier, J. et al. Sex differences in age-related changes in the sleep-wake cycle. Front. Neuroendocrinol. 47, 66–85 (2017).
Benjamin, D. J. et al. Redefine statistical significance. Nat. Hum. Behav. 2, 6–10 (2018).
de Lange, M. A. et al. The effects of daylight saving time clock changes on accelerometer-measured sleep duration in the UK Biobank. J. Sleep Res. e14335, https://doi.org/10.1111/jsr.14335 (2024).
Acknowledgements
The authors did not receive specific funding for this work. J.L. and E.R.F-C received support from the Wu Tsai Human Performance Alliance and the Joe and Clara Tsai Foundation. J.L. and L.M. receive financial support from the Australian Government through Research Training Program scholarships. F.L. receives financial support from the Monash Graduate Scholarship and the Monash International Tuition Scholarship. E.R.F-C is financially supported by an Australian Research Council Industry Fellowship (IE240100162) and has received research support or consultancy fees from the Science Industry Endowment Fund, Monash Lung and Sleep Institute, Tempur Australia, Team Focus Ltd, British Athletics, Australian National Football League, Australian National Rugby League, Collingwood Football Club, Melbourne Storm Rugby Club, and Henley Business School, which are not related to this paper. S.M.W.R. has served as a Programme Leader for the Cooperative Research Centre (CRC) for Alertness, Safety and Productivity, Australia; is a Director and Chair of the Sleep Health Foundation; has received grants from Vanda Pharmaceuticals, Philips Respironics, Cephalon, Rio Tinto, BHP Billiton and Shell; and has received equipment support and consultancy fees through his institution from Optalert, Compumedics, Teva Pharmaceuticals, Roche and Circadian Therapeutics, which are not related to this paper. S.P.A.D. has received funding from the National Health and Medical Research Council (NHMRC) and the United States Department of Defence, received consultancy fees from Avecho Biotechnology Ltd, and participated on an advisory board for Zelda Therapeutics, which are not related to this paper.
Author information
Authors and Affiliations
Contributions
J.L. conceptualised the study. D.M.P. and E.R.C. acquired the data. J.L., F.L., and J.F.W. analysed and interpreted the data. J.L. and F.L. contributed to data visualisation. J.L. wrote the manuscript and all authors (J.L., D.M.P., F.L., M.É.C., L.M., E.R.C., J.F.W., S.P.A.D., S.M.W.R., and E.R.F-C.) edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare the following competing interests. E.R.C. and D.M.P. are affiliated with the commercial company WHOOP, Inc. which provided support in the form of salaries but did not otherwise play a role in the study design, data collection or analysis, decision to publish, or preparation of the manuscript. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Michael D. Schmidt and Christian Benedict for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Leota, J., Presby, D.M., Le, F. et al. Dose-response relationship between evening exercise and sleep. Nat Commun 16, 3297 (2025). https://doi.org/10.1038/s41467-025-58271-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-58271-x