Abstract
Glaucoma, a leading cause of blindness due to elevated intraocular pressure (IOP), is managed with medications like latanoprost (LAT), a prostaglandin analogue, to enhance aqueous outflow. Despite the challenge posed by eye anatomy and tear dynamics, effective ocular bioavailability via topical administration remains elusive. This study aims to optimize self-assembled nanomicelles incorporating LAT, an anti-glaucoma drug, belonging to BCS Class II (low solubility and high permeability) via a two-level, two-factor full factorial design, the nanomicelles were formulated via direct dissolution method and validated using design of expert. The optimized nanomicelles exhibited a spherical morphology, with a size of 69 nm and encapsulation efficiency of 77.5%, demonstrating a sustained LAT release over 12 h. In normotensive rabbits, the nanomicelles elicited a substantial reduction in intraocular pressure (IOP) by up to 40% for a duration of three days, that was significantly longer than the IOP-lowering efficacy of XALATAN eye drops (24 h). These findings indicated that self-assembled nanomicelles hold promise for enhancing the ocular bioavailability and extending the therapeutic duration of LAT, while providing the physical stability.
Similar content being viewed by others
Introduction
Glaucoma, a common eye disorder and one the leading causes of blindness worldwide1; is predominantly linked to elevated intraocular pressure (IOP), which serves as the principal risk factor for the condition. Glaucoma medications lower IOP and are categorized by their mechanisms of action; prostaglandin (PG) analogues, alpha agonists, beta blockers and carbonic anhydrase inhibitors2. Currently, PG analogues are approved as a first line therapy for ocular hypertension in open angle glaucoma. Commercially available PG analogues are LAT, latanoprostene bunod, unoprostone, bimatoprost, tafluprost and travoprost3,4,5.
LAT is a prodrug of prostaglandin F-2 alpha, converted to active latanoprost acid (active form) by corneal esterases. The IOP reduction starts 3–4 h post-administration, peaks at 8–12 h, and lasts 24 h6,7. LAT is a colorless or slightly yellow oily viscous liquid and practically insoluble in water. Its chemical name is isopropyl-(Z)-7[(1R, 2R, 3R, 5 S) 3, 5-dihydroxy-2-[(3R)-3-hydroxy-5- phenylpentyl] cyclopentyl]-5-heptenoate (Fig. 1) and its molecular weight is 432.58 g/mol8.
LAT is fairly hydrophobic, as it has a water solubility of about 0.125 mg/mL9 and a logP (octanol/water) partition coefficient of 4.410 It is susceptible to thermal and solar instability and should be stored below room temperature and away from light11.
Ocular drug delivery systems offer targeted treatment, prolonged drug retention, enhanced bioavailability, protection of therapeutic agents, reduced systemic exposure, and improved patient comfort compared to conventional drug delivery systems12. The ocular drug delivery remains a challenge due to the unique anatomy and physiology of the eye as well as the presence of several static and dynamic barriers13.
Ocular drugs can be administered through different routes, namely; topical, systemic, subconjunctival, intracameral, and intravitreal14,15. The topical route is most preferred for ophthalmic drugs over other routes as it offers easy application and minimal risk of infection16. Topical ocular formulations with high drug concentration can be effective, but protective mechanisms limit drug absorption due to barriers like tear turnover, nasolacrimal drainage, and the ability of cul-de-sac to maintain a minimum of 7 µl volume in the eye, other shown in Fig. 213.
Nanomicelles are self-assembling colloidal dispersions within a size range of 10 to 100 nm17, featuring a hydrophobic core and a hydrophilic shell18, which makes them novel approaches for delivering medication with maximum efficacy, safety, and ease19. Alongside liposomes, dendrimers, and nanoparticles, nanomicelle formulations revolutionize drug delivery, offering sustained, controlled, and targeted release of therapeutic agents owing to their simple preparation, biocompatibility, effectiveness, and capacity to encapsulate poorly water-soluble drugs20. Nanomicelles enhance ocular bioavailability by minimizing or preventing degradation and enhancing drug permeation through ocular epithelia with minimal or no irritation21. Their high drug entrapment capacity, smaller size, and easy method of preparation make them an ideal drug delivery system for ocular applications22.
Soluplus (Sp), a grafted copolymer of polyvinyl caprolactam-polyvinyl acetate-polyethylene glycol (PVCap-PVAc-PEG), is frequently employed in drug delivery systems to enhance the solubility and bioavailability of poorly soluble drugs. It forms nanomicelles above a critical micelle concentration (CMC)of 7.6 mg/L23, enhancing solubility, stability, and drug bioavailability. Sp is a promising polymer for ocular delivery due to better tolerance, stability, and lower CMC compared to Pluronic F-12724, and has undergone safety evaluations, making it feasible for ocular drug delivery25. Its unique properties make it ideal for delivering poorly water-soluble drugs to the eye26.
Commercial LAT formulations (0.005% solution) are typically applied as a single daily drop27 and contain the preservative benzalkonium chloride (BAK), which also solubilizes LAT .Persistent use of benzalkonium chloride-containing solutions has been shown to be cytotoxic and damaging to the cornea28, as it can resorb (disrupting the corneal epithelial barrier)29 latanoprost acid from the cornea into tears, leading to decreased LAT concentration in ocular tissues. This can increase the risk of unwanted side effects and poor patient adherence to glaucoma treatment, potentially resulting in treatment failure30.
Prior research has primarily focused on extending the release of LAT via the development of subconjunctival liposomal injections31 and gels32. However, these approaches involve invasive procedures and the use of harsh chemicals such as spans and pluronic F-127 in niosomal gels, prompting the need for a topical delivery system33. To minimize risks and address BAK limitations, novel drug delivery systems like Sp -loaded nanomicelles containing LAT have been introduced.
Quality by Design (QbD) is a systematic approach in pharmaceutical development focusing on product quality throughout its lifecycle34. It involves understanding formulation and manufacturing processes early to mitigate risks and ensure consistency. Different methods and tools to implement QbD in practice are outlined by International Council for Harmonization (ICH) guideline Q8(R2), including “multivariate experiments”, “statistical process control methods”, also known as design of experiments, and a “risk-based control strategy”35. Ultimately, QbD facilitates the development of robust pharmaceuticals meeting regulatory standards and patient needs36.
The current study highlights the novel approach of formulating LAT nanomicelles using Sp as the graft polymer and optimizing it via QbD (design of experiment). The resultant clear aqueous solution is anticipated to offer high bioavailability and prolonged efficacy of LAT. Unlike gel formulations, the nanomicelles are optically clear, user-friendly, and manufactured without the need for harsh chemicals, rendering it a cost-effective preparation. Furthermore, the nanomicelles are expected to provide superior ocular tolerance to patients and deliver therapeutic levels of LAT to the eye.
Materials and methods
Materials and instruments
LAT with 98% purity was procured from Merck while Soluplus was supplied by the BASF. Sodium chloride, sodium dihydrogen phosphate, disodium hydrogen phosphate (Scharlau Chemie, Spain), sucrose, mannitol, glucose, phosphoric acid, potassium dihydrogen phosphate (Merck, Germany), Dialysis Tubing-Visking, (MWCO; 12–14 kDa); (Dia = 27/3200–21.5 mm); (Size 6 Inf. 30 M, Sigma-Aldrich; Darmstadt, Germany). Healthy Male rabbits (2.5 ± 0.2 kg) (albino) were supplied by Department of Pharmacy, University of Peshawar.
Analytical balance (Shimadzu, Kyoto, Japan); vacuum filtration assembly (Sigma-Aldrich, Darmstadt, Germany); distilled water (Millipore ultrapure water system (Milford, CT, USA)). pH meter (Jenway, Essex, UK), magnetic stirrer (DLAB, Fontana, CA, USA), peristaltic pump (Longer Precision Pump Co., Ltd., Baoding, China), centrifuge (DLAB, CA, USA), scanning electron microscope (JSM-5910, JEOL Ltd., Tokyo, Japan), zeta sizer (Malvern Zetasizer ZS-90, Malvern Instruments Ltd., Malvern, UK), FTIR spectrophotometer (Shimadzu, Kyoto, Japan, IRTracer-100), Franz diffusion cell (Perme Gear, Hellertown, PA, USA). The HPLC grade acetonitrile, ethanol and methanol were purchased from the Sigma–Aldrich (Oslo, Norway).
Methodology
Design of experiment (DOE)
Several process variables were screened and evaluated that affect the preparation of nanomicelles prior to experimental design. Drug, polymers and encapsulation methods were found to be the potential factors that affect the nanomicelle preparation. A two-level two factors full factorial design (FFD) was constructed which allowed investigation of main and interaction effects of selected variables or inputs on process outputs (responses). Direct dissolution method was selected for the encapsulation of LAT in self-assembled Sp nanomicelle. The independent factors were amount of LAT and SP at low (-1) and high (1) level, with three center points, the Design Expert software suggested seven (07) runs (Table 1) and the responses measured were particle size and percent drug entrapment efficiency (%EE).
Preparation of nanomicelle
The LAT self-assembled nanomicelles were prepared by dissolving the polymer in 10 ml of distilled water with continuous magnetic stirring (DLAB, Fontana, CA, USA), with ≈650 rpm, at 25 °C for 72 h. The nanomicelles formed were washed thrice via centrifugation, followed by removal of supernatant and resuspended with distilled water and ultimately freeze dried with 5% sucrose.
Optimization of nanomicelles
The concentrations of drug and polymer were optimized using design of experiments (DOE) with the Design Expert v.13.0 software. S.
There two independent factors (amount of drug and polymer) that play an important role in the optimization of nanomicelles. The design expert v.13.0 software (Stat-Ease, Minneapolis, MN, USA) proposed seven experimental runs for optimization of Sp based nanomicelles as shown in Table 1.
Evaluation of nanomicelle formulations
Particle size, poly dispersibility index (PDI) and zeta potential
Nanomicelles were assessed for particle size, polydispersity index (PDI) and zeta potential using dynamic light scattering (DLS) with a Zeta-Sizer Nano ZS-90. Measurements were conducted at a 90° scattering angle, at 25 °C, with 90-second cycles in triplicate, using disposable cuvettes and water as the dispersant. Mean standard deviation (± SD) values were determined from triplicate readings.
HPLC assay of LAT
A reported HPLC method was used for quantification of LAT with slight modification7. A C18 column (250 × 4.6 mm, 5 μm) was used for the analysis. The mobile phase comprised of acetonitrile and potassium dihydrogen phosphate 0.05 M, pH 3.0 adjusted with 10% orthophosphoric acid. The mobile phase was pumped at flow rate of 1.5 ml/min. The sample injection volume was 20 µl with the column oven temperature of 25 °C and detection was carried out at 210 nm.
Estimation of LAT content
The contents of LAT in the prepared samples were determined using HPLC method. In short, standard solutions of samples and drug were prepared and analyzed in triplicates by reported HPLC method outlined in “HPLC assay of LAT” section. The percent drug content was calculated by below Eq. (1);
Encapsulation efficiency (EE) and drug loading (DL)
The encapsulation efficiency (EE) of LAT within optimized nanomicelles was assessed through centrifugation at 15,000 rpm at 4℃ for 20 min using a Centurion Scientific centrifuge (UK)37, . This process facilitated the separation of drug-loaded nanomicelles from the aqueous medium. Subsequently, dilutions were prepared in acetonitrile, and the concentration of free drug present in the supernatant was determined. This involved quantifying the unencapsulated drug in the supernatant, alongside analyzing the precipitate directly via HPLC, as detailed in “HPLC assay of LAT” section. for precise analysis. The percentage of encapsulation efficiency (%EE) was calculated as mentioned by Eq. (2), while the percentage of drug loading (%DL) was determined using Eq. (3)7 respectively.
Characterization of nanomicelles
Scanning electron microscope (SEM)
The characterization of shape and surface morphology of drug loaded nanomicelles was measured by SEM (JSM-5910, Jeol Japan) analysis. The lyophilized nanomicelles were spread on the adhesive carbon tape attached to the stub. The nanomicelles surface were coated by gold (Au) through a coater (Argon Sputtering, SPI Module Control) for about 90 s under vacuum. The prepared sample was analyzed under SEM at different magnifications and then their images were captured.
Fourier-transform infrared (FTIR) spectroscopy
The FTIR spectra of LAT, Sp, physical mixture and optimized formulation were attained with potassium bromide disc technique on a Perkin Elmer Spectrum BX FTIR (PerkinElmer, Waltham, MA, USA). The percent absorbance was documented keeping spectrum within range (4000–400 cm−1) at a resolution of 4 cm−1.
Thermo-gravimetric analysis (TGA)
The TGA analysis was performed to assess phase transition, thermal decomposition and solid gas reactions (oxidation, reduction) at controlled temperatures in a controlled environment. The prepared sample was placed in a pan lying in a furnace and buoyed using precision balance. The experiment mass was examined throughout the experiment. Purge gas (inert, reactive) was used to control the sample environment.
In-vitro drug release
The optimized LAT-loaded NMs were analyzed in triplicate to assess their in-vitro drug release profile. A dialysis membrane (Dialysis Tubing-Visking MWCO: 12–14 kDa), previously soaked in PBS overnight, was mounted on the Franz diffusion cell. The acceptor compartment was filled with the dissolution media (Simulated Tear Fluid (STF) pH 7.4) and stirred at 100 rpm throughout the study. The acceptor compartment was covered with a jacketed vessel, with a peristaltic pump attached to circulate hot water and maintain the temperature at 37 °C ± 0.2. A 1 mL volume of LAT-loaded NMs suspension was placed in the donor compartment and covered using parafilm to prevent evaporation. Drug release was monitored over predetermined time intervals (0.25, 0.5, 1.0, 2.0, 3.0, 6.0, and 12.0 h), 0.5 mL sample of the release medium was collected and immediately replaced with fresh prewarmed STF. The samples were suitably diluted and analyzed using HPLC (outlined in “HPLC assay of LAT” section) to determine percent drug release data, which was then fitted to various mathematical models. Figure 3 depicts the schematic illustration of in-vitro release setup for LAT nanomicelles.
In-vivo studies
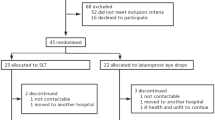
Normotensive male albino rabbits (2.5 ± 0.2 kg weight) were evaluated for in-vivo studies and study design is illustrated in Fig. 4. They were kept at temperature (20–25 °C) and relative humidity (40–70%) as well as fed with balanced diet. Animal based experiments were performed in compliance with committee for ethics in research, Department of Pharmacy, University of Peshawar, approval number 423/EC/F.LIFE/UOP-2021.
Ocular irritation evaluation
The in-vivo ocular irritation was assessed in a total of three groups, each comprising 3 male albino rabbits. Group I served as the control (undosed), despite one eye serving as an internal control, it was imperative to validate treatment effects, enabling baseline comparison, and reducing bias38. Group II received LAT-loaded NMs, administered in suspension form at a concentration of 0.005%, corresponding the concentration of LAT present in the marketed formulation XALATAN, which was administered to Group III as illustrated in Fig. 4. The ocular irritation assessment was conducted following the Draize test protocol39 endorsed by the OECD40. An aliquot of 50 µl of the tested preparation was administered to the lower cul-de-sac of the right eye of each rabbit, while the left eye served as the control. Signs of irritation, discharge, and conjunctival redness were evaluated at various intervals within 24 h post-administration. Each criterion was graded on a scale from zero to four, with zero indicating no irritation and four indicating severe irritation41. The cumulative scores determined the ocular irritation index (\({\text{I}}_{{{\text{irr}}}}\)). A score of two or three in any category or an (\({\text{I}}_{{{\text{irr}}}}\)) exceeding four indicated clinically significant irritation39.
IOP reduction evaluation
To conduct studies on IOP reduction, a total of three groups, each composed of 3 male albino rabbits, were employed. Group I was the control, Group II received LAT-loaded NMs (0.005%) and Group III received commercially available LAT eye drops (XALATAN, Pfizer, Belgium) as illustrated in Fig. 4. Prior to measurement a local anesthetic eye drops (proparacaine 0.5%) was administered to lessen eye discomfort. A test formulation of 50 µl was administered to the lower cul-de-sac of the right eye of each rabbit, with the left eye serving as the control. Tonopen Avia (Reichert Inc., Depew, NY, USA), a portable and handheld device that takes an average of ten IOP readings using a sterile ocu-film coated tonometer, was used to obtain all IOP measurements42. IOP measurements were taken immediately before administration and then hourly for 6.0, 12.0, 24.0, 48.0, and 72 h. The reduction in intraocular pressure (IOP) was assessed by comparing the control and treated eyes, while the further reduction in IOP (∆IOP) was determined by comparing the treated eye with the contralateral eye of the same rabbit, as reported previously39,43.
Stability studies
Stability studies were conducted on optimized LAT-loaded nanomicelles employed as a suspension at 4 °C ± 2 °C and 25 °C ± 2 °C for two months to assess storage impact. The nanomicelles were assessed for their particle size, PDI, zeta potential, drug content and % EE. The percentage of entrapped drug (% EE) was evaluated by separating nanomicelles from unentrapped drug via centrifugation. The entrapped drug was quantified using HPLC, following the methodology outlined in “HPLC assay of LAT” section.
Results and discussion
Prior to commencing a Quality by Design (QbD) experimental setup, it is imperative to define a product specification. This specification, derived from the intended application of nanomicelles drug carrier systems, sets forth specific criteria. These criteria are integral to the selection of variables and subsequent optimization of process parameters.
Preparation of nanomicelles
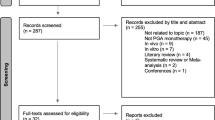
Design of experiment
A design of experiment (DOE) approach utilizing Sp polymer was employed to optimize LAT-loaded Sp NMs through the direct dissolution method. Design Expert v.13.0 software suggested seven runs, incorporating three center points, employing a two-level two-factor full factorial design for optimization. The concentration of both the drug and polymer were varied to evaluate their influence on particle size and % encapsulation efficiency. The procedures were executed in triplicates, with resulting data presented in Table 2.
Statistical significance was determined at α = 0.05, where a p-value less than 0.05 indicates statistical significance of the term in the model equation or property. Compatibility analysis between the drug and Sp combination was conducted via Fourier-transform infrared spectroscopy (FTIR) and drug content assays. Optimized formulations were assessed for in-vitro drug release and in-vivo effects on intraocular pressure (IOP). Nanomicelles were characterized for size, shape, PDI, % encapsulation efficiency (%EE), and stability.
Particle size of LAT loaded nanomicelles
The experimental data obtained from experiments showed that concentration of factor A (Drug) and factor B (polymer) individually had a significant effect on the particle size as confirmed by statistical analysis of the data.
Statistical analysis of particle size
Data obtained from experiments were analyzed using a half normal plot Fig. 5a to determine factors that had a significant effect on particle size. Results showed that the drug and polymer individually had a % contribution of 52.47 and 36.96 respectively, with the drug concentration having the highest contribution to varying particle size. There was no two-factor interaction observed, as suggested by the half normal plot.
ANOVA of particle size
The ANOVA data showed a highly significant linear regression model with a Model F value of 157.07 and a low p-value of 0.0009. The lack of curvature and lack of Fit F-value indicated the model’s fitness, while the excellent R2 value of 0.9905 showed goodness of fit (suggesting that responses are reasonably well described by the model equation). The predicted R2 value of 0.9481 was in good agreement with the adjusted R² of 0.9842, with a difference of less than 0.2 (Table 3). Additionally, the signal-to-noise ratio of 33.03 (greater than 4) indicated an adequate signal.
Final equation in terms of coded and actual factors
After evaluating the experimental data, multiple regression models were applied and the linear regression model was found to have the best descriptive statistics, with a higher R2 value and a low p-value. As a result, the linear regression model was used to fit the experimental data and establish a final model equation to demonstrate the correlation between formulation variables and particle size. The final model equation in terms of coded and actual term is given in the below equations;
The model equation showed that the amount of drug and polymer are significant factors in determining the particle size. The first equation is representing coded values (A = drug and B = Sp) assigned by the software while the second equation describes the actual values of the independent factors i.e., drug (LAT) and polymer (Sp).
Model graphs
The 3D response surface plot (Fig. 5b) was used to visualize the effect of the factors on particle size. The perturbation plot showed that high levels of factor A (drug) increased particle size while factor B (polymer) decreased it. The interactive plot displayed the interaction between factor A and B, showing that particle size increased with increasing drug concentration. The 3D response surface plot confirmed these results.
Encapsulation efficiency of LAT-loaded NMs
The results of % encapsulation efficiency of LAT- NMs revealed that concentration of drug individually has a high effect on the % EE as indicated by the low P-value of 0.0001 while the factor B (polymer) has no significant effect.
Statistical analysis of EE%
The half normal plot was analyzed to determine effects of selected factors on the encapsulation efficiency (Fig. 6a). It was apparent from the results that factor A have high contribution in varying encapsulation of the drug.
ANOVA of EE
ANOVA for the selected effects was performed to test the significance of the model. The suggested model (linear regression model) was highly significant with the model F-value of 19,116 and a low P-value of 0.0001. The model has no curvature with a non-significant Lack of Fit F-value of 4.90. The descriptive statistics (Table 4) showed an excellent R2 value of 0.999 confirmed the adequacy of the model. The Predicted R2 of 0.9992 is in reasonable agreement with the adjusted R2 of 0.9997; i.e. the difference is less than 0.2. Adeq Precision ratio of 207 indicated an adequate signal showing model can be used to navigate design space.
The final equation in terms of coded and actual factors
The linear regression model was identified as a significant model as it demonstrated.
highly reliable descriptive statistics. The linear regression model was the best fit for experimental data as confirmed from high R2 value by the P-value. Therefore, a model equation was developed to show correlation between the formulation variables and % encapsulation efficiency. The final model equation obtained in the coded of actual variables is given equation;
The model equation showed that only one factor (drug) was having significant influence on the % EE. The first equation is representing coded value (A = drug) assigned by the software while the second equation describes the actual value of the independent factor i.e., drug (LAT).
Model graphs
The response surface plot of % EE (Fig. 6b) shows that drug concentration is responsible for change in % EE. High concentration of the drug is responsible for increase in the % EE of LAT loaded nanomicelles whereas polymer concentration has no significant effect on EE%.
Optimization and validation of optimized conditions
The optimized formulation factors were assessed based on their levels and experimental values of nanomicelles. Factor A, LAT (drug) corresponded to an actual value of 2 mg, while Factor B, Sp (polymer), equated to 15 mg in actuality. Predictions indicated a particle size of 70 nm and an encapsulation efficiency (EE) of 77.5%. However, experimental results demonstrated a slightly smaller particle size of 69 nm and an EE of 77.4% ± 0.5. The variation in size is minimal but the variation in encapsulation efficiency was the other response to optimized the factors. The percent drug loading (% DL) value is 7% ±1. These findings highlight the close alignment between predicted and experimental outcomes, indicating the robustness of the formulation process, as illustrated in Table 5.
Particle size, PDI and zeta potential of optimized nanomicelles
The resultant LAT-loaded NMs were of small size (69 ± 2.76 nm) and bearing sufficiently high zeta potential (−12 ± 0.24 mV mV) preventing coalescence of individual particles, that will result in stable formulation. The addition of Sp to LAT at concentrations above the critical micelle concentration (CMC) significantly improved aqueous solubility. The particle size of nanomicelles (69 ± 2.76 nm) correlated well with the predicted value, falling within the required range of 10 to 100 nm44. The polydispersity index (PDI) indicates the level of non-uniformity in size distribution of nanomicelles, with values ranging from 0.0 to 1.0. A PDI value below 0.12 ± 0.04 is considered acceptable for polymeric nano formulations11. The optimized formulation exhibited a PDI of 0.12 ± 0.04, confirming its homogeneous and monodisperse nature (Fig. 7a). Zeta potential predicts the stability of colloidal carrier systems. The zeta potential value of LAT-loaded nanomicelles was determined to be approximately −12 mV (Fig. 7b), indicating limited electrostatic repulsion between nanomicelles resulting in monodisperse nanomicelles, as suggested by the PDI value, i.e., 0.12 ± 0.04 11.
LAT engages in interactions with Sp through hydrogen bonding, van der Waals forces, and other non-electrostatic forces, influencing the overall net charge of LAT-loaded NMs.The negative net charge of the nanomicelles suggests that the SP shell possesses a greater negative charge compared to the drug molecules. The polar functional groups (PVCap-PVAc-PEG) in Sp interact with water molecules to form a hydrated shell, contributing to the negative zeta potential46. This facilitates the encapsulation of LAT molecules, shielding the negatively charged groups (OH), thereby reducing the negative potential of the nanomicelles.
FTIR spectroscopy
FTIR spectroscopy was conducted to find interactions, if any, among the drug and.
polymer in the physical mixture and optimized nanomicelle formulations. The FTIR spectrum of LAT showed absorption peaks at 3374 cm−1 (aliphatic O-H stretching), 2933 cm−1 (aliphatic C-H stretching), 1729 cm−1 (stretching of ester carbonyl), 1455 cm−1(O-H bending), 1248 cm−1 (ester C-O stretching) and 747.89 cm−1 (C-H bending) as shown in the Fig. 8. The LAT spectrum showed intermolecular hydrogen bonding in the range of 3400–3468 cm−1, ester carbonyl stretching 1740–1640 cm−1 and C = O stretching for tertiary amides at 1740 cm−1. The absence of a spectral shift in the physical mixture suggested no chemical interaction between the drug and polymer.
As evident form the spectra of physical mixture and optimized nanomicelles, both the latanoprost and Sp retain their major peaks and bands, indicating the absence of any interaction.
Thermogravimetric analysis
TGA analysis was performed for LAT, Sp, their physical mixture and optimized nanomicelles to analyze their thermal behavior and decomposition.
The TGA analysis (Fig. 9) revealed that pure LAT began to degrade at 210 °C, while Sp started to degrade at 330 °C.
The physical mixture of Sp and LAT began degradation at 310 °C. The optimized nanomicelle formulation improved the thermal stability of LAT, with its thermal stability increasing from 210 °C to 300 °C. This suggested that the thermal stability of LAT was enhanced by the inclusion of the excipient, thereby shifting the degradation temperature to higher values. The enhanced thermal stability of LAT when combined with Sp might be physical in nature, as evident from FTIR spectra. Sp might create a protective environment, interact with LAT at a molecular level, and alter thermodynamic conditions, collectively increasing the drug’s thermal stability, especially since LAT is known to degrade at high temperatures during storage11. As the optimized formulation contains 15 mg of the soluplus and in comparison the drug is only 2 mg which is only 13.33%. hence the soluplus provided stability by encapsulating the latanoprost, the same property of the soluplus is reported in prervious literature47,48,49.
Scanning electron microscopy (SEM)
The SEM micrograph distinctly illustrates the discrete and finely spherical shape of self-assembled micelles, characterized by a smooth surface. Their average sizes ranged approximately from 70 to 75 nm in diameter, closely aligning with the average diameter of 69 nm measured by dynamic light scattering. These results demonstrate the effective dispersion of Sp in the aqueous solution, leading to the formation of stable spherical nanosized micellar structures, as depicted in Fig. 10.
In-vitro drug release profile of LAT loaded nanomicelles
LAT loaded nanomicelles were tested for drug release in STF (pH 7.4) using a Franz cell. Results revealed sustained release of the drug, with close to 100% being released from the nanomicelles over a 12-hour period. These findings are presented in Fig. 11. The slow release can be attributed to hydrogen bonds formation between drug molecule and polymer11.
In-vitro release kinetics
Drug release kinetics is the application of mathematical models to drug release process.
Several kinetic models such as zero order, first order, Higuchi, Hixon Crowell and Korsemeyer Peppas were applied to predict the mechanism of drug release from LAT loaded nanomicelles (Table 6).
The results of the fitting of the various drug release models to the data are presented in Table 1. With the exception of the Zero-Order model, there is a similar ability of the remaining models to describe the data with some accuracy, based on R-squared. Especially under these circumstances, it can be difficult to determine with confidence which model describes the data set best. Indeed, there are those who believe that a greater number of estimated parameters in the model should provide a better estimate of the true data. The AIC was calculated so that the number of data points and the number of estimated parameters is taken into consideration when comparing results from model fitting. The best-fit model according to the AIC is the one that explains the greatest amount of variation in the data using the fewest possible estimated independent parameters. The latter is evidenced by the term 2k that diminishes the rank of a model due to a greater number of estimated parameters.
The fitting of the Zero-Order release model equation to the release data resulted in the poorest fit to the data, as evidenced by both the low R2 and the least negative AIC value. This suggests that the drug is not released at a consistent rate from the nanomicelles. Further investigation should consider Fickian diffusion of drug from the nanomicelles. This was first investigated by fitting the First-Order release model equation to the data. The results from fitting the First-Order release model to the complete set of data provided a much-improved R2 in comparison to the Zero-Order R2. The AIC is more negative for the First-Order model than for the Zero-Order model because the SSR was lower and the number of estimated parameters was reduced to 1. These results suggest that first-order drug release is evident, supporting the supposition that Fickian diffusion is the drug release mechanism. This can be tested further using the remaining release model equations.
In the Korsmeyer-Peppas model equation, n is expected to equal 0.43 or less if Fickian diffusion is the sole release mechanism from a spherical drug delivery device that remains essentially intact during drug delivery. For an n value greater than 0.43, non-Fickian diffusion is also a contributing release mechanism (3,6). Data analysis provided an estimate of n equal to 0.335, a value lower than 0.43 for these spherical nanomicelles. This confirms the conclusion from the application of the First-Order model to the release data that Fickian diffusion is the likely drug release mechanism. An improved R2 and a reduced SSR indicate that the Korsmeyer-Peppas model describes the release data better than the First-Order model, but there is an additional estimated parameter with the Korsmeyer-Peppas model in its AIC calculation that makes the two models comparable in their ability to describe the release data.
Initial application of the Higuchi model to the drug release data was based only on data less than or equal to 70% drug released, limiting that data to 2 h which still provided 4 experimental data points for estimation of k and m. Increasing that to data up to 73% drug release by including the 3 h timepoint did not substantially reduce the model’s ability to describe the release data and therefore results for the Higuchi model in Table 1 are based on data up to 73% drug released. The y-intercept estimated using the Higuchi model and only 4 data points was 0.017, which represents the fraction of drug released at t = 0, amounting to only 1.7% of the drug. Therefore there is essentially no “burst effect” for drug release in this study of latanoprost-containing nanomicelles. When adding the t = 3 h data point (making n = 5), the burst effect has increased slightly, calculated to be 0.0265, where 2.65% is still a negligible amount for a burst effect.
The Higuchi model describes the data well, based on the excellent R2 and the dramatically reduced SSR. The use of only five instead of all 7 data points reduced the value of the AIC-n, which diminishes the magnitude of the negative AIC associated with the fit of the Higuchi model to the release data. Nevertheless, the AIC for the Higuchi model is the most negative value thus far, indicating the superiority of this model to describe the data. Since the Higuchi model equation is based on Fickian diffusion as the drug release mechanism, the excellent fit of this model to the drug release data is confirmation that Fickian diffusion is the dominant or the sole drug release mechanism.
Ocular irritation evaluation
The ocular irritation evaluation of LAT -loaded nanomicelles was pivotal for gauging their safety and clinical potential, commonly conducted on rabbits due to their large eyes and heightened sensitivity to irritation compared to humans50. Through macroscopic observation of signs such as redness and swelling following nanomicelle application revealed formulations with an irritation index (Iirr) of zero, indicating excellent ocular tolerance. These findings laid the groundwork for further investigations into the efficacy and safety of the nanomicelles in treating ocular conditions like glaucoma, underscoring their potential as a safe therapeutic option.
IOP reduction evaluation
The impact of LAT nanomicelles on IOP was evaluated in normotensive rabbits and compared to XALATAN eye drops. Results showed that a single dose of nanomicelles produced a sustained reduction in IOP (72 h) with a maximum reduction of 40% at 6–12 h post-administration, while XALATAN showed a maximum reduction of 26% at 4–5 h post-administration prolonged decrease in IOP is due to the mucoadhesive property of Sp that enhances ocular residence time. Statistical analysis indicates a significant difference (P value 0.002) in IOP reduction between XALATAN and the optimized nanomicelle group. These findings are presented in Fig. 12.
Stability studies
Stability studies were conducted on optimized LAT-loaded NMs at 4 °C ± 2 °C and 25 °C ± 2 °C to assess their particle size, PDI, charge, % EE, and drug content over a two-month period, evaluating the impact of storage conditions on nanomicelle stability. Statistical analysis revealed significant differences between storage at 4 °C and room temperature for particle size (p = 0.013), PDI (p = 0.03), and % EE (p = 0.04). The observed increase in particle size during storage can be attributed to nanomicelle aggregation over time. These findings underscore the importance of storing nanomicelles at 4 °C and shielding them from light for optimal physicochemical stability. Table 7 summarizes the results of the study.
Conclusion
Two level two factors full factorial design was designed for optimization. A total of seven runs were suggested for optimization of self-assembled LAT loaded nanomicelles using design expert. The nanomicelles were formulated by direct dissolution method, optimized and validated by optimized parameter in the software. The observed particle size and %EE well matched with the predicted values. The nanomicelles were of a small size 69 nm with a uniform spherical shape. The % EE of the optimized nanomicelles was 77.5%. The optimized nanomicelles released LAT up to 12 h when subjected to in-vitro release studies and showed prolonged drug release with no irritation to rabbit eyes. Furthermore, the self-assembled nanomicelles reduced the IOP in normotensive rabbits up to 40% and IOP lowering effect remained for three days which was significantly longer than that observed for XALATAN eye drops, that was capable of reducing IOP only for 24 h, requiring repeated application every 24 h. The results from this study confirmed the potential of LAT loaded nanomicelles to increase bioavailability of drug and prolong drug release which in turn reduces its frequency of administration and possibly enhance patient compliance. LAT loaded nanomicelles will decrease cost of glaucoma treatment as less frequent dosing will be required in comparison with conventional formulations.
Data availability
The data are included in the manuscript.
References
Schuster, A. K., Erb, C., Hoffmann, E. M., Dietlein, T. & Pfeiffer, N. The diagnosis and treatment of glaucoma. Dtsch. Arztebl Int. 117, 225 (2020).
Natarajan, J. V. et al. Sustained release of an anti-glaucoma drug: Demonstration of efficacy of a liposomal formulation in the rabbit eye. PloS One 6, e24513 (2011).
Klimko, P. G. & Sharif, N. A. Discovery, characterization and clinical utility of prostaglandin agonists for the treatment of glaucoma. Br. J. Pharmacol. 176, 1051–1058 (2019).
Cheema, A., Chang, R. T., Shrivastava, A. & Singh, K. Update on the medical treatment of primary open-angle glaucoma. Asia Pac. J. Ophthalmol. 5, 51–58 (2016).
Alm, A. Latanoprost in the treatment of glaucoma. Clin Ophthalmol. 1967–1985 (2014).
Russo, A., Riva, I., Pizzolante, T., Noto, F. & Quaranta, L. Latanoprost ophthalmic solution in the treatment of open angle glaucoma or raised intraocular pressure: A review. Clin. Ophthalmol. 2, 897–905 (2008).
Ashfaq, M., Khan, I. U. & Asghar, M. N. High-performance liquid chromatography determination of latanoprost in pharmaceutical formulations using UV detection. Anal. Lett. 39, 2235–2242 (2006).
Sawatdee, S., Phetmung, H. & Srichana, T. Development of a stable latanoprost solution for use as eye drops. Chiang Mai J. Sci. 40, 656–668 (2013).
Rodriguez-Aller, M. et al. New prostaglandin analog formulation for glaucoma treatment containing cyclodextrins for improved stability, solubility and ocular tolerance. Eur. J. Pharm. Biopharm. 95, 203–214 (2015).
Horne, R. R., Judd, K. E. & Pitt, W. G. Rapid loading and prolonged release of latanoprost from a silicone hydrogel contact lens. J. Drug Deliv. Sci. Technol. 41, 410–418 (2017).
Morgan, P. V., Proniuk, S., Blanchard, J. & Noecker, R. J. Effect of temperature and light on the stability of latanoprost and its clinical relevance. J. Glaucoma 10, 401–405 (2001).
Barar, J., Aghanejad, A., Fathi, M. & Omidi, Y. Advanced drug delivery and targeting technologies for the ocular diseases. BioImpacts BI. 6, 49 (2016).
Patel, H. A., Patel, J. K., Patel, K. N. & Patel, R. R. Ophthalmic drug delivery system—A review. Der Pharmacia Lettre 2, 100–115 (2010).
Janagam, D. R., Wu, L. & Lowe, T. L. Nanoparticles for drug delivery to the anterior segment of the eye. Adv. Drug Deliv. Rev. 122, 31–64 (2017).
Gaudana, R., Ananthula, H. K., Parenky, A. & Mitra, A. K. Ocular drug delivery. AAPS J. 12, 348–360 (2010).
Agarwal, R. et al. Liposomes in topical ophthalmic drug delivery: An update. Drug Deliv. 23, 1075–1091 (2016).
Vadlapudi, A. D. & Mitra, A. K. Nanomicelles: An emerging platform for drug delivery to the eye. Ther. Deliv. 4, 1–3 (2013).
Trivedi, R. & Kompella, U. B. Nanomicellar formulations for sustained drug delivery: Strategies and underlying principles. Nanomed 5, 485–505 (2010).
Velagaleti, P., Anglade, E., Khan, I., Gilger, B. & Mitra, A. Topical delivery of hydrophobic drugs using a novel mixed nanomicellar technology to treat diseases of the anterior and posterior segments of the eye. Drug Deliv Technol. 10, 42–47 (2010).
Amirmahani, N., Mahmoodi, N. O., Galangash, M. M. & Ghavidast A. advances in nanomicelles for sustained drug delivery. J. Industrial Eng. Chem. 55, 21–34 (2017).
Cholkar, K., Patel, A., Dutt Vadlapudi, A. & Mitra, K. Novel nanomicellar formulation approaches for anterior and posterior segment ocular drug delivery. Recent. Pat. Nanotechnol. 2, 82–95 (2012).
Wang, X., Wang, S. & Zhang, Y. Advance of the application of nano-controlled release system in ophthalmic drug delivery. Drug Deliv. 23, 2897–2901 (2016).
Dian, L. et al. Enhancing oral bioavailability of quercetin using novel soluplus polymeric micelles. Nanoscale Res. Lett. 9, 1–11 (2014).
Li, M., Xin, M., Guo, C., Lin, G. & Wu, X. New Nanomicelle curcumin formulation for ocular delivery: Improved stability, solubility, and ocular anti-inflammatory treatment. Drug Dev. Ind. Pharm. 43, 1846–1857 (2017).
Guo, C. et al. Nanomicelle formulation for topical delivery of cyclosporine A into the cornea: In vitro mechanism and in vivo permeation evaluation. Sci. Rep. 5, 1–14 (2015).
Noh, G. et al. Development and evaluation of a water soluble fluorometholone eye drop formulation employing polymeric micelle. Pharm 10, 208 (2018).
Ghate, D. & Edelhauser, H. F. Barriers to glaucoma drug delivery. J. Glaucoma 17, 147–156 (2008).
Hedengran, A., Steensberg, A. T., Virgili, G., Azuara-Blanco, A. & Kolko, M. Efficacy and safety evaluation of benzalkonium chloride preserved eye-drops compared with alternatively preserved and preservative-free eye-drops in the treatment of glaucoma: A systematic review and meta-analysis. Br. J. Ophthalmol. 104, 1512–1518 (2020).
Cha, S. H., Lee, J. S., Oum, B. S. & Kim, C. D. Corneal epithelial cellular dysfunction from benzalkonium chloride (BAC) in vitro. Clin. Experimental Ophthalmol. 32, 180–184 (2004).
Halder, A. & Khopade, A. J. Physiochemical properties and cytotoxicity of a benzalkonium chloride-free, micellar emulsion ophthalmic formulation of latanoprost. Clin. Ophthalmol. 3057–3064 (2020).
Kompella, U. B., Hartman, R. R. & Patil, M. A. Extraocular, periocular, and intraocular routes for sustained drug delivery for glaucoma. Progress Retinal eye Res. 82, 100901 (2021).
Fathalla, D., Fouad, E. A. & Soliman, G. M. Latanoprost niosomes as a sustained release ocular delivery system for the management of glaucoma. Drug Dev. Industrial Pharm. 46, 806–813 (2020).
Fathalla, D., Fouad, E. A. & Soliman, G. M. Latanoprost niosomes as a sustained release ocular delivery system for the management of glaucoma. Drug Dev. Ind. Pharm. 46, 806–813 (2020).
Nadpara, N. P., Thumar, R. V., Kalola, V. N. & Patel, P. B. Quality by design (QBD): A complete review. Int. J. Pharm. Sci. Rev. Res. 17, 20–28 (2012).
Mishra, V., Thakur, S., Patil, A. & Shukla, A. Quality by design (QbD) approaches in current pharmaceutical set-up. Expert Opin. Drug Deliv. 15, 737–758 (2018).
Schwartz, J. B., O’Connor, R. E. & Schnaare, R. L. In Modern Pharmaceutics 921–950 (CRC, 2002).
Salimi, A., Zadeh, B. S. M. & Kazemi, M. Preparation and optimization of polymeric micelles as an oral drug delivery system for deferoxamine mesylate: In vitro: and: Ex vivo: Studies. Res. Pharm. Sci. 14, 293–307 (2019).
Giarmoukakis, A. et al. Biodegradable nanoparticles for controlled subconjunctival delivery of latanoprost acid: In vitro and in vivo evaluation. Preliminary Results 112, 29–36 (2013).
Liu, Z., Nie, S., Guo, H., Pan, W. & Li, J. Effects of Transcutol P on the corneal permeability of drugs and evaluation of its ocular irritation of rabbit eyes. J. Pharm. Pharmacol. 58, 45–50 (2006).
Wilson, S. L., Ahearne, M. & Hopkinson, A. An overview of current techniques for ocular toxicity testing. Toxicology 327, 32–46 (2015).
Baeyens, V. et al. Clinical evaluation of bioadhesive ophthalmic drug inserts (BODI®) for the treatment of external ocular infections in dogs. J. Control Release 85, 163–168 (2002).
Bhartiya, S., Bali, S. J., James, M., Panda, A. & Dada, T. Test retest variability of TonoPen AVIA. Indian J. Ophthalmol. 61, 129–131 (2013).
Mehra, N., Aqil, M. & Sultana, Y. A grafted copolymer-based nanomicelles for topical ocular delivery of everolimus: Formulation, characterization, ex-vivo permeation, in-vitro ocular toxicity, and stability study. Eur. J. Pharm. Sci. 159, 105735 (2021).
Bhuptani, R. S. et al. Soluplus based polymeric micelles and mixed micelles of lornoxicam: design, characterization and in vivo efficacy studies in rats. Indian J. Pharm. Educ. Res. 50 (2016).
Nemati, M., Fathi-Azarbayjani, A., Al‐Salami, H., Roshani Asl, E. & Rasmi, Y. Bile acid‐based advanced drug delivery systems, bilosomes and micelles as novel carriers for therapeutics. Cell. Biochem. 40, 623–635 (2022).
Pervez, S. et al. Transdermal delivery of glimepiride: A novel approach using nanomicelle-embedded microneedles. Pharmaceutics 15, 2019 (2023).
Jia, S. et al. Stabilizing effect of Soluplus on Erlotinib metastable crystal form in microparticles and amorphous solid dispersions. Polymers 14, 1241 (2022).
Hidayatullah, T. et al. Hybrid dissolving microneedle-mediated delivery of ibuprofen: Solubilization, fabrication, and characterization. Pharmaceuticals 16, 677 (2023).
Guo, C. et al. Nanomicelle formulation for topical delivery of cyclosporine A into the cornea: In vitro mechanism and in vivo permeation evaluation. Sci. Rep. 5, 12968 (2015).
Abraham, M. H. et al. Draize rabbit eye test compatibility with eye irritation thresholds in humans: A quantitative structure-activity relationship analysis. Toxicol. Sci. 76, 384–391 (2003).
Acknowledgements
The authors would like to express their gratitude to the Centralized Resource Laboratory and NCE Geology at the University of Peshawar for their technical assistance.
Funding
The research was supported by the researchers supporting project number (RSP2024R235) King Saud University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, software, writing—review and editing along with visualization, S.G., F.N and Z.I.; writing—original draft preparation, investigation, S.G.; supervision, resources, Z.I, F.N. and S.N; validation, A.R and M.A.K., formal analysis, G.e.M.; AT , and S.R.Z.; data curation, S.G. and S.P.; project administration, F.N. and F.A.; funding acquisition, F.N. and F.A. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional Review Board Statement
The study was conducted in accordance with ARRIVE guidelines and approved by the ethical committee of the Department of Pharmacy, university of Peshawar (approval number 423/EC/F.LIFE/UOP-2021).
Informed consent
All subjects participating in the study provided informed consent along with written consent to publish the data in paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gohar, S., Iqbal, Z., Nasir, F. et al. Self-assembled latanoprost loaded soluplus nanomicelles as an ophthalmic drug delivery system for the management of glaucoma. Sci Rep 14, 27051 (2024). https://doi.org/10.1038/s41598-024-78244-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-78244-2
Keywords
This article is cited by
-
Quality by Design (QbD)-Improved Polymeric Micelles of Posaconazole with Increased Solubility, Oral Bioavailability, and Antifungal Activity against Invasive Fungal Infections
Journal of Pharmaceutical Innovation (2026)
-
Eyes on the Future: Nano-medicine Innovations in Enhancing Ocular Bioavailability
BioNanoScience (2026)