Abstract
Modern life and rising stress have contributed to increased sleep disorders and metabolic and cardiovascular diseases. While exercise is known to be an important health intervention, the optimal timing for its effectiveness remains uncertain. This study aims to investigate the effects of a 12-week timed exercise program on sleep, lipid profiles, and vascular function. Fifty-eight sedentary males were divided into three groups: morning exercise (ME) at 6–8 a.m., evening exercise (EE) at 6–8 p.m., and control group (CON) without exercise. The 12-week intervention involved moderate-intensity aerobic exercise (≥ 150 min/week). Sleep was assessed using the Munich ChronoType Questionnaire (MCTQ) and Dim Light Melatonin Onset (DLMO). Metabolic indicators were assessed through body composition and blood biochemical tests. Ultrasound imaging was performed to evaluate hemodynamics at the common carotid artery. Both exercise groups reduced body fat after 12-week exercises, with ME showing significant reductions as early as week 4. Total cholesterol and triglycerides in ME also decreased. Shortened sleep latency was observed in both exercise groups, with DLMO and sleep advanced in ME. Although both exercise groups showed decreased stiffness and increased wall shear stress, EE demonstrated greater enhancements in blood flow rate, center-line velocity, carotid artery dilation and lowering systolic blood pressure. A 12-week aerobic exercise significantly improves physical health in sedentary adults. Morning exercise (6–8 a.m.) is particularly effective for rapid body fat reduction, lowering plasma cholesterol and triglycerides, and advancing sleep-wake cycle. Evening exercise (6–8 p.m.) is more effective for enhancing vascular function.
Trial registration: Chinese Clinical Trial Registry, ChiCTR2400094208, 18/12/2024.
Similar content being viewed by others
Introduction
Sleep, metabolic and cardiovascular health play pivotal roles in sustaining comprehensive physiological well-being1,2. However, in contemporary society, heightened stress levels, irregular lifestyles have exacerbated prolonged sedentary habits, which adversely affect physical health3. The escalating prevalence of sleep disorders, metabolic and cardiovascular diseases (CVDs) pose a substantial and pressing public health challenge, with CVDs ranking as the leading cause of death worldwide2,3,4.
The circadian clock is a crucial internal biological mechanism within the human body, regulating numerous physiological processes and behavioral activities. Among these, the sleep-wake cycle, metabolic regulation and vascular health undergo robust modulation by the circadian clock. For instance, the melatonin secretion starts before sleep onset, reaching its peak in the early hours of the morning5. Most cardiovascular parameters exhibit circadian rhythms, with blood pressure experiencing two peaks during the day, typically from 7 to 10 a.m. and from 6 to 9 p.m.. Platelet aggregability is also higher in the morning, which may contribute to the higher incidence of cardiovascular events during this time6,7,8. The relationship between sleep, metabolic disorders, and vascular dysfunction is deeply interconnected, and timing may be a key factor in prevention or treatment strategies9,10.
Sedentary is the risk factor for CVDs, while regular exercise can improve CVD risk factors, such as hypertension and lipid metabolism disorder11,12,13. Properly timed physical activity helps regulate the circadian rhythm after disruptions, supporting cardiovascular health6,14,15. In the midday-afternoon (11:00–17:00) and mixed moderate-to-vigorous intensity physical activity (MVPA) timing group, the risk of all-cause and CVD mortality is lower than in the morning group (05:00–11:00)15. However, another study suggests that morning exercise is associated with a reduced risk of CVDs and stroke16. Research also suggests that MVPA performed between 7 and 9 AM is most effective for weight loss17. The above investigated the impact of activity time on CV risk based on daily physical activity, while the comprehensive effects of additional long-term timed exercise on vascular and metabolic health in sedentary adults, particularly regarding hemodynamics, remain unclear.
Hemodynamics refers to the fluid dynamics of blood flow within the circulatory system. Assessing the hemodynamics of the carotid artery can provide important insights for the prevention and early diagnosis of cardiovascular and cerebrovascular diseases, as the blood supply to the cerebral circulatory system primarily relies on the carotid artery18. By collecting information such as arterial center-line velocity (FV) and diameter (D) waveforms, dynamic and kinematic parameters of arteries can be calculated, including blood flow rate (FR), dynamic resistance (DR), oscillatory shear index (OSI), wall shear stress (WSS), and others19,20,21,22.
Sleep disorders have a profound impact on quality of life, metabolic function, and cardiovascular health23,24. Adults are recommended to o get more than 7 h of sleep per night25. The prevalence of insufficient sleep is higher among males, reaching 37%, compared to females26. Sleep-wake cycles and melatonin rhythms are influenced by the timing of exercise27. Youngstedt et al. found that 3 days of exercise at 7 a.m. and 4 p.m. led to an advance in the aMT6s(6-sulphatoxymelatonin, the urinary metabolite of melatonin) acrophase, while delay was observed between 7 p.m. and 10 p.m.28. This result exhibits similarities to the phase response curve of light29. An experiment revealed that both morning and evening exercise prompted an advance in the sleep-wake cycle and Dim Light Melatonin Onset (DLMO), with the 5 days of exercise was performed in the laboratory30. While other studies have observed that exercise at 3–10 h after waking leads to a delay in melatonin rhythm31,32. Due to variations in exercise protocols, external environments and population characteristics, it is difficult to generalize the long-term effects of timed exercise on sleep in sedentary populations, including related hormonal regulation (melatonin)33,34. Therefore, further research is necessary.
Exercise acts as an input signal for regulating the circadian rhythm, making its timing a key factor in the effectiveness of health interventions. However, the lack of hemodynamic evidence and the diversity of experimental designs present challenges in establishing consistent findings on the long-term effects of timed exercise in sedentary adults. Investigating the effects of 12-week morning and evening aerobic exercise on sleep and cardiometabolic health can provide essential insights for making appropriate exercise regimens in the prevention and treatment of related diseases.
Methods
Experimental subjects
Participants included in this study were adult males who met the following criteria: non-smokers; no history of alcohol abuse; no history of cardiovascular or metabolic diseases; systolic blood pressure (SBP) ≤ 130 mmHg; diastolic blood pressure (DBP) ≤ 80 mmHg; body mass index (BMI) between 18.5 and 24.9 kg/m2; The amount of physical activity determined using the International Physical Activity Questionnaire Short Form (IPAQ-SF) was insufficient to meet the recommended standards (at least 150 min a week of moderate-to-vigorous intensity physical activity) and more than 8 h of sedentary behavior per day35,36; Participants had no apparent sleep disorders, with Pittsburgh Sleep Quality Index (PSQI) scores not exceeding 737,38. The participants were divided into three groups: the morning exercise group (ME, exercise between 6 and 8 a.m.), the evening exercise group (EE, exercise between 6 and 8 p.m.), and a control group (CON, no exercise).
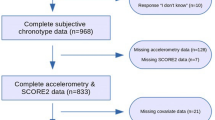
Experimental recruitment information was disseminated online, and questionnaires were used for participant screening. Initially, 65 individuals were recruited and randomly assigned to three groups using a simple randomization method with a random number table. (ME: 25, EE: 25, CON: 15). During the experiment, seven participants dropped out: five from the ME group and two from the EE group. Ultimately, complete data were collected from 58 participants (ME group: 20, EE group: 23, CON group: 15), aged between 18 and 28 years. No group differences were observed in the baseline values of the basic physical condition of the subjects (Table 1).
Exercise protocol
The ME group exercised between 6 and 8 a.m., while the EE group exercised between 6 and 8 p.m. (Fig. 1). The exercise intervention spanned 12 weeks, with a minimum of three sessions per week, totaling over 150 min of exercise weekly. Assessments of body composition, sleep, blood metabolic markers, and carotid arterial ultrasound were conducted before and after the 12-week intervention. Body composition was measured using a body analyzer (MC-980MA, Tanita, Japan) between 8 and 9 a.m. Participants engaged in aerobic activities involving large muscle groups, such as running, jumping rope, using an elliptical trainer, and cycling. They wore fitness bands with photoplethysmography sensors to monitor heart rate (HR) and adjust exercise intensity in real-time, recording each session39. The target HR for exercise was 60–70% of heart rate reserve (HRR)40,41. The Bruce protocol test was performed every four weeks to adjust the target HR based on participants’ cardiorespiratory fitness, using a high-resolution metabolic analyzer (MetaLyzer 3B-R2, Cortex, England).
Exercise intervention protocol. The exercise intervention spanned 12 weeks (≥ 3 sessions/week, ≥ 150 min/week). Body composition, sleep patterns, metabolic markers, and carotid arterial ultrasound information were assessed before and after the 12-week exercise. CON, the control group that did not exercise; ME, the morning exercise group that exercised between 6 and 8 a.m.; EE, the evening exercise group that exercised between 6 and 8 p.m.
There was no difference in the completion rate of the exercise protocol (Table 2). Participants exercised approximately three days per week and 36 exercise sessions in total, with running being the most frequently selected exercise followed by jumping rope. To control for potential confounding effects of nutritional supplementation on outcome measures, participants were strictly prohibited from consuming any dietary supplements or sports performance aids throughout the trial duration. According to the IPAQ survey, moderate-to-vigorous intensity physical activity (MVPA) was 32.75 ± 7.09 min in the ME group, 34.13 ± 7.42 min in the EE group, and 29.67 ± 9.52 min in the CON group before exercise. After 12 weeks of timed exercise, the self-reported total time of MVPA significantly increased for both the ME and EE groups, reaching 180.00 ± 7.15 and 183.70 ± 7.02 min, respectively, with no significant difference between the two groups.
Sleep and dim light melatonin onset (DLMO)
DLMO is a common circadian rhythm marker, detectable in blood, saliva, and urine samples42. Melatonin levels were assessed using the Melatonin Direct Saliva ELISA kit (IBL International). Participants collected saliva samples every hour, from 5 h before to 1 h after their habitual bedtime, totaling seven collections. Each collection consisted of 3–5 ml of saliva. To minimize light influence, participants wore dark glasses and avoided electronic devices during collection. Samples were stored in a cooler box or refrigerator and retrieved the following morning for analysis. DLMO was calculated using the absolute threshold method, with linear interpolation of time points before and after the melatonin concentration reached 3 pg/ml43. The Munich ChronoType Questionnaire (MCTQ) was used to record sleep patterns, including bedtime, sleep onset, and wake-up times on both workdays and work-free days. Sleep latency was defined as the time between bedtime and sleep onset. Mid-sleep time was calculated based on established references44.
Blood biochemical index
After fasting for more than 8 h, antecubital venous blood was drawn to assess lipid parameters (triglycerides and total cholesterol) between 8 and 9 a.m. The analysis was conducted using an automatic biochemical analyzer (CS-600B, DIRUI, China). The fingertip blood glucose monitoring (Contour TS, Ascensia, Malaysia) was used to measure the fasting blood glucose.
Hemodynamics
The waveforms of the right carotid arterial center-line velocity (FV) and diameter (D) were measured using a color Doppler ultrasound (Prosound Alpha 7, Aloka, Japan) between 8 and 9 a.m.. Simultaneously, blood pressure measurements were taken from the upper left arm brachial artery using an automatic sphygmomanometer (HEM-7136, Omron, Japan). Matlab R2023a was used to calculate the hemodynamic parameters based on the Womersley flow model, following methods previously described in the literature45,46,47 (Supplementary Methods and Fig. S1).
Statistics
The determination of sample size was guided by a previous study14. A medium effect size (0.30) for clinic SBP, with 0.80 power and an α of 0.05, required a minimum of 30 subjects (10 per group) for repeated measures ANOVA with within-between interactions. Calculations were performed in G*Power 3.1.9.7 (Universität Kiel, Germany). Statistical analyses were performed using GraphPad Prism 9.0.0 (GraphPad Software, USA). The data were analyzed using repeated measures of two-way ANOVA, considering group (ME, EE, and CON) as the between-subject factor and study phase (baseline vs. after 12 weeks) as the within-subject factor. Post hoc comparisons were made using the Bonferroni test. The results were presented as mean ± standard error (SE), and significant differences were indicated by an asterisk (*p < 0.05). Figures were generated with GraphPad Prism 9.0.0 and Origin 2024.
Results
The effects of 12-week timed exercise on sleep pattern
Sleep time and Dim Light Melatonin Onset (DLMO) reflect the changes of sleep-wake cycle at behavioral and hormonal levels, respectively. Both on the workday (WD) and work-free day (WFD) after 12-week exercise, the ME group exhibited advanced sleep onset (WD: 23.50 ± 7.41 min; WFD: 24.84 ± 9.13 min), mid-sleep (WD: 29.70 ± 6.67 min; WFD: 30.54 ± 9.27 min), and sleep end (WD: 35.85 ± 8.27 min; WFD: 43.11 ± 13.15 min) times compared to pre-exercise (Fig. 2A). After 12-week exercise, sleep onset (WD: 23:36 ± 00:08 vs. 00:05 ± 00:08; WFD: 23:43 ± 00:09 vs. 00:16 ± 00:08), mid-sleep (WD: 03:15 ± 00:09 vs. 03:56 ± 00:07; WFD: 03:36 ± 00:11 vs. 04:19 ± 00:08), and sleep end (WD: 06:54 ± 00:12 vs. 07:48 ± 0:07; WFD: 07:38 ± 00:17 vs. 08:31 ± 00:09) in the ME group were earlier than those in the EE group. Additionally, the MSFsc (the adjusted mid-point of sleep on free days) (26.19 ± 7.85 min) and DLMO (16.90 ± 4.68 min) were advanced in the ME group (Fig. 2B; Fig. S2; Fig. S3). In contrast, no significant changes were observed in DLMO and sleep times after 12 weeks of exercise in the EE group (Fig. 2A,B; Fig. S2; Fig. S3).
Effect of 12-week timed exercise on sleep-wake cycle. In the polar plot, the circumferential coordinate represents time, with the entire circumference of the circle divided into 24 segments, each corresponding to 1 h of the day, and the radial coordinate represents the number of people at each time point. DLMO, Dim light melatonin onset; MFSsc, the adjusted mid-point of sleep on free days. “*”indicates the statistical difference compared to pre-exercise values (P < 0.05).
Both exercise groups showed reduced sleep latency on workdays (ME:6.70 ± 2.40 min; EE:4.57 ± 1.21 min) and work-free days (ME:6.75 ± 1.65 min; EE:4.09 ± 1.15 min) after 12 weeks of exercise, with no significant changes in sleep duration (Fig. 3A,B), indicating that individuals fall asleep more quickly after going to bed. The PSQI results indicated that the scores of the ME and EE groups (ME: 3.20 ± 0.30; EE: 3.17 ± 0.37) were significantly lower than pre-exercise (ME: 4.20 ± 0.35; EE: 4.26 ± 0.36).
Effect of 12-week timed exercise on sleep latency and duration. Starting from 0°, clockwise represents sleep duration, while counterclockwise represents sleep latency. The units of the coordinates are in minutes. The solid-fill bands represent the mean values, while the dashed-fill sections indicate the standard error. “*” indicates the statistical difference compared to pre-exercise values (P < 0.05).
The effects of 12-week timed exercise on metabolic health
After 12 weeks of exercise, both the ME and EE groups showed significant decreases in body fat mass (BFM), including visceral fat (VFM) and subcutaneous fat (SFM), as well as waist-hip ratio (WHR), with no significant changes observed in the weight (Fig. 4A–D). At the 4th, 8th, and 12th weeks after ME, BFM, body fat rate (BFR), and WHR were significantly lower than pre-exercise levels (Fig. 4E–G), with reductions observed in both VFM and SFM (Fig. 4H–I). However, no statistical changes were found in muscle mass (Fig. S4). In the EE group, significant reductions in BFM, BFR, and SFM were observed after 8 and 12 weeks of exercise (Fig. 4E,F,I).
Effect of 12-week timed exercise on body composition and lipid metabolism. BFM, Body fat mass; VFM, Visceral fat mass; SFM, Subcutaneous fat mass; WHR, Waist-hip ratio; BFR, Body fat rate; TC, total cholesterol; TG, triglycerid; FBG, fasting blood glucose. (A) Weight includes BFM, and the data for both are displayed superimposed with weight at the bottom and BFM at the top; (B) VFM and SFM are displayed stacked with VFM on top and SFM below. “*” indicates the statistical difference compared to pre-exercise values (P < 0.05) in (A)–(I). “*” denotes statistical differences (P < 0.05) in (J)–(L).
Following ME, there was a reduction in total cholesterol (TC) and triglycerides (TG) after 12 weeks of exercise, with significant differences compared to the CON group (Fig. 4J,K). Fasting blood glucose (FBG) showed no significant changes after ME (Fig. 4L). After 12 weeks of EE, there were no changes in TC, TG, and FBG.
The effects of 12-week timed exercise on hemodynamics
Both the ME (63.34 ± 1.35 vs. 70.85 ± 1.89) and EE (64.85 ± 2.32 vs. 73.37 ± 2.85) groups showed a decrease in resting heart rate (HR) after 12 weeks of exercise, with the ME group showing a lower HR than the CON group (63.34 ± 1.35 vs. 71.53 ± 1.56). The EE group showed increases in both maximum and mean arterial diameters (Dmax and Dmean) (Fig. 5A; Fig. S5). Maximum flow velocity (FVmax) and flow rate (FRmax) also increased after 12 weeks of exercise in the EE group (Fig. 5B,C; Fig. S6), indicating a more sufficient cerebral blood flow supply.
The stiffness index (Fig. 6A) and pressure-strain elastic modulus (Fig. 6B) of the ME and EE groups were both reduced, indicating an improvement in vascular elasticity, with no significant differences observed between the two groups. A decrease in systolic blood pressure (SBP) compared to pre-exercise levels was observed in the EE group (Fig. 6C), with no significant differences in mean blood pressure (MBP) (Fig. 6D). Wall shear stress (WSS) is the frictional force exerted by blood flow on the endothelial surface and oscillatory shear index (OSI) is a quantification of the amount of shear stress oscillation. The maximum WSS (WSSmax) increased after ME and EE (Fig. 6E), with the OSI decreased (Fig. 6F). After EE, dynamic resistance (DR) (Fig. 6G) and peripheral resistance (PR) decreased (Fig. 6H), and pulsatility index (PI) increased (Fig. 6I), suggesting an enhancement in vascular regulatory capacity.
Effect of 12-week timed exercise on the hemodynamics of the common carotid artery. SBP, systolic blood pressure; MBP, mean blood pressure; WSSmax, the maximum wall shear stress; OSI, oscillatory shear index; DR, dynamic resistance; PR, peripheral resistance; PI, pulsatility index. “*” denotes statistical differences (P < 0.05).
Discussions
Adults can achieve health benefits from at least 150 min of moderate-intensity exercise per week12. While the impact of exercise is influenced by factors such as intensity, frequency, and volume, the timing of exercise also plays a crucial role48. This study focused on the effects of a long-term (12 weeks) morning (ME) vs. evening (EE) moderate-intensity aerobic exercise regimen on sleep, metabolic health and vascular hemodynamics in sedentary adults. The findings, summarized in the graphical abstract (Fig. 7), highlight the differential benefits of exercise timing.
Both ME and EE interventions significantly shortened sleep latency, indicating that exercise facilitates quicker onset of sleep. This finding aligns with existing evidence showing a mild reduction in sleep latency following regular exercise interventions33. However, it should be noted that acute moderate to vigorous exercise did not promote sleep need nor alter other sleep parameters, except for light sleep49. Moreover, a cross-sectional study among middle-aged adults showed that only morning MVPA was associated with fewer sleep disturbances50. This highlights the importance of exercise regularity and timing in eliciting meaningful sleep improvements. Sleep regulation follows the two-process model: the homeostatic sleep drive and the circadian rhythm51. Our study found that ME advanced sleep time and Dim Light Melatonin Onset (DLMO), suggesting a shift toward an earlier sleep-wake cycle. This effect may stem from the combined influence of morning daylight and physical activity, which can act as potent zeitgebers52. Morning exercise likely enhances circadian alignment by advancing the DLMO and increasing sleep homeostatic pressure earlier in the day, leading to an advanced sleep-wake cycle53. These findings underscore the potential of morning exercise to regulate sleep timing and improve overall sleep quality, particularly for individuals with delayed sleep phases or disrupted circadian rhythms.
Body composition is closely linked to CVD risk. For example, each 0.1 increase in waist-hip ratio (WHR) correlates with a 41% increase in all-cause mortality and a 59% increase in CVD mortality54. Both exercise groups in this study experienced significant improvements in body composition, with fat loss observed as early as week 4 in the ME group and week 8 in the EE group. This finding aligns with previous research by Willis et al. that the early-exercise group (7–12 a.m.) lost more weight than the late-exercise group (3–7 p.m.)55. These results suggest that the timing of exercise may influence fat loss, with early exercise being particularly effective. Interestingly, this pattern contrasts with findings in metabolically compromised populations, where afternoon exercise produced greater fat loss, suggesting that exercise timing effects may vary according to baseline metabolic status56. The differential effects of morning versus evening exercise observed in our study may be partially explained by the circadian regulation of hormones such as cortisol and melatonin, as well as diurnal fluctuations in metabolites57. Animal studies support the idea that early exercise boosts lipolysis (fat breakdown) and amino acid breakdown58. Moreover, early exercise has been shown to upregulate markers related to thermogenesis and mitochondrial proliferation, contributing to enhanced metabolic function59. The reduction in total cholesterol and triglycerides observed in the ME group may also be attributed to a decrease in body fat, which is consistent with findings that pre-breakfast exercise enhances lipid metabolism and insulin sensitivity60. However, there are also some studies suggesting that afternoon exercise might offer greater benefits for individuals with impaired metabolism, such as those with obesity or metabolic syndrome56,61,62,63. These conflicting results highlight the complex relationship between exercise timing and metabolism, varying by exercise protocol, population characteristics, and specific outcomes. Nevertheless, this variability underscores the importance of tailoring exercise timing to an individual’s needs and health status to optimize benefits for body composition and metabolic health.
Regular long-term exercise has been shown to improve arterial stiffness and enhance arterial elasticity, benefiting cardiovascular health64,65. Our study also demonstrated that 12 weeks of exercise improved arterial elasticity, suggesting that exercise positively affects vascular function. The impact of exercise on vascular elasticity function can be mediated through various signals, with wall shear stress (WSS) being a crucial mechanical signal66. Endothelial cells exposed to high levels of WSS for an extended period have a protective effect against atherosclerosis67,68. Exercise-induced changes in WSS lead to increased expression of endothelial nitric oxide (NO) synthase (eNOS) and production of NO, which are typical markers of a healthy endothelial phenotype with anti-atherosclerotic properties69. This suggests that both morning and evening exercise may help improve endothelial function and potentially help prevent atherosclerosis by increasing WSS and decreasing oscillatory shear index. Additionally, dynamic resistance, peripheral resistance and pulsatility index are important indicators reflecting vascular regulatory function. The changes of these indicators and flow rate in the EE group suggest that evening exercise helps improve cerebral blood supply and enhance vascular compliance. Furthermore, previous studies have shown that aerobic exercise in the evening is beneficial to lowering blood pressure in hypertensive patients by improving vasomotor sympathetic modulation and systemic vascular resistance6,14. Therefore, the improvement in vascular elasticity and regulatory capacity observed in this study may be factors contributing to the reduction in systolic blood pressure following evening exercise. Taken together, these findings highlight the potential of exercise timing to optimize cardiovascular health, particularly in enhancing vascular function and regulating blood pressure.
Overall, the current study focused on young, healthy, sedentary adults, and provided valuable insights into the effects of long-term timed exercise on sleep, metabolic health, and vascular function. Unlike observational studies linking habitual activity timing to health outcomes, our research provides interventional evidence through structured morning and evening exercise protocols in sedentary adults. Notably, our analysis of carotid artery hemodynamics—a critical yet underexplored predictor of cerebrovascular risk—illustrates how exercise timing modulates vascular adaptations. By integrating sleep, metabolic, and vascular endpoints under controlled conditions, our study addresses inconsistencies in previous heterogeneous methodologies and underscores the importance of exercise timing in optimizing health interventions. To build on these findings, future research should expand the scope to include populations with cardiovascular diseases and/or metabolic disorders. Such studies could offer deeper insight into how tailored interventions might improve health outcomes for individuals with existing health conditions. In addition, to gain a more comprehensive understanding of how timed exercise can regulate sleep disorders, it is necessary to conduct studies in populations with circadian rhythm disruptions, such as shift workers or individuals with insomnia. Another limitation is that due to potential menstrual cycle effects on exercise adherence, only men were recruited in the current study. Although literatures had shown no significant sex differences in cardiovascular variables like blood pressure, heart rate, and stroke volume when standardized for body composition70,71,72, future studies should include both male and female participants to assess any potential sex-specific responses to timed exercise.
Conclusions
In summary, a 12-week aerobic exercise program significantly improves sleep quality, with morning exercise promoting an earlier sleep-wake cycle and melatonin rhythm, contributing to better sleep quality. For cardiometabolic health, long-term aerobic exercise in both the morning and evening effectively reduces body fat, while morning exercise achieving faster reductions in subcutaneous and visceral fat, as well as significantly lowering triglycerides and total cholesterol. Additionally, 12 weeks of aerobic exercise may enhance cardiovascular health by reducing resting heart rate, improving arterial elasticity and optimizing wall shear stress patterns. Notably, evening exercise provides greater benefits in improving cerebral blood supply. These findings underscore the importance of exercise timing in tailoring health interventions for sleep and cardiometabolic health.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- BFM:
-
Body fat mass
- BFR:
-
Body fat rate
- BMI:
-
Body mass index
- CON:
-
Control
- CVDs:
-
Cardiovascular diseases
- D:
-
Arterial diameter
- DBP:
-
Diastolic blood pressure
- DLMO:
-
Dim light melatonin onset
- DR:
-
Dynamic resistance
- EE:
-
Evening exercise
- FBG:
-
Fasting blood glucose
- FR:
-
Blood flow rate
- FV:
-
Arterial center-line velocity
- IPAQ-SF:
-
International Physical Activity Questionnaire Brief Form
- MCTQ:
-
Munich ChronoType Questionnaire
- ME:
-
Morning exercise
- MSFsc:
-
The adjusted mid-point of sleep on free days
- MVPA:
-
Moderate-to-vigorous intensity physical activity
- OSI:
-
Oscillatory shear index
- PI:
-
Pulsatility index
- PR:
-
Peripheral resistance
- PSQI:
-
Pittsburgh Sleep Quality Index
- SBP:
-
Systolic blood pressure
- SFM:
-
Subcutaneous fat
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- VFM:
-
Visceral fat
- WD:
-
Workday
- WFD:
-
Work-free day
- WHR:
-
Waist-hip ratio
- WSS:
-
Wall shear stress
References
Drăgoi, C. M. et al. Circadian rhythms, chrononutrition, physical training, and redox Homeostasis—Molecular mechanisms in human health. Cells. 13(2). (2024).
Martin, S. S. et al. 2024 heart disease and stroke statistics: A report of US and global data from the American heart association. Circulation 149 (8), e347–e913 (2024).
Zagaria, A. et al. Poor sleep hygiene practices are associated with a higher increase in sleep problems during the COVID-19 pandemic: A latent change score model. J. Sleep. Res. 33 (3), e14057 (2024).
Tsao, C. W. et al. Heart disease and stroke Statistics-2023 update: A report from the American heart association. Circulation 147 (8), e93–e621 (2023).
Meyer, N., Harvey, A. G., Lockley, S. W. & Dijk, D. J. Circadian rhythms and disorders of the timing of sleep. Lancet 400 (10357), 1061–1078 (2022).
Brito, L. C. et al. Chronobiology of exercise: evaluating the best time to exercise for greater cardiovascular and metabolic benefits. Compr. Physiol. 12 (3), 3621–3639 (2022).
Gumz, M. L. et al. Toward precision medicine: circadian rhythm of blood pressure and chronotherapy for hypertension—2021 NHLBI Workshop Report. Hypertension (Dallas, Tex:1979). 80(3), 503–522 (2023).
Millar-Craig, M. W., Bishop, C. N. & Raftery, E. B. Circadian variation of blood-pressure. Lancet 1 (8068), 795–797 (1978).
Lane, J. M. et al. Genetics of circadian rhythms and sleep in human health and disease. Nat. Rev. Genet. 24 (1), 4–20 (2023).
Martino, T. A. & Delisle, B. P. Cardiovascular research and the arrival of circadian medicine. Chronobiol. Int. 40 (1), 1–3 (2023).
Teixeira, A. L., Padilla, J. & Vianna, L. C. Impaired popliteal artery flow-mediated dilation caused by reduced daily physical activity is prevented by increased shear stress. J. Appl. Physiol. 123 (1), 49–54 (2017).
Bull, F. C. et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54 (24), 1451–1462 (2020).
Blodgett, J. M. et al. Device-measured physical activity and cardiometabolic health: the prospective physical activity, sitting, and sleep (ProPASS) consortium. Eur. Heart J. 45 (6), 458–471 (2024).
Brito, L. C. et al. Morning versus evening aerobic training effects on blood pressure in treated hypertension. Med. Sci. Sports Exerc. 51 (4), 653–662 (2019).
Feng, H. et al. Associations of timing of physical activity with all-cause and cause-specific mortality in a prospective cohort study. Nat. Commun. 14 (1), 930 (2023).
Albalak, G. et al. Setting your clock: associations between timing of objective physical activity and cardiovascular disease risk in the general population. Eur. J. Prev. Cardiol. 30 (3), 232–240 (2023).
Ma, T., Bennett, T., Lee, C. D. & Wicklow, M. The diurnal pattern of moderate-to‐vigorous physical activity and obesity: a cross‐sectional analysis. Obesity 31 (10), 2638–2647 (2023).
Liu, Y-T., Zhang Z-M-Y, Li, M-L., Gao, S., Feng, F. & Xu, W-H. Association of carotid artery geometries with middle cerebral artery atherosclerosis. Atherosclerosis 352, 27–34 (2022).
Daniela, L., Carlo, P., Mara, M. & Massimo, P. Relationship between carotid artery mechanics and the spontaneous baroreflex: a noninvasive investigation in normal humans. J. Hypertens. 30 (9), 1809–1816 (2012).
Hirai, T., Sasayama, S., Kawasaki, T. & Yagi, S. Stiffness of systemic arteries in patients with myocardial infarction. A noninvasive method to predict severity of coronary atherosclerosis. Circulation 80 (1), 78–86 (1989).
Ranadive, S. et al. Comparison of the acute impact of maximal arm and leg aerobic exercise on arterial stiffness. Eur. J. Appl. Physiol. 112 (7), 2631–2635 (2012).
Qin, K. R., Xu, Z., Wu, H., Jiang, Z. L. & Liu, Z. R. Synergy of wall shear stress and circumferential stress in straight arteries. J. Hydrodyn. 17 (6), 752–757 (2005).
Alibhai, F. J., Tsimakouridze, E. V., Reitz, C. J., Pyle, W. G. & Martino, T. A. Consequences of circadian and sleep disturbances for the cardiovascular system. Can. J. Cardiol. 31 (7), 860–872 (2015).
Mahalakshmi, A. M. et al. Sleep, brain vascular health and ageing. Geroscience. 42 (5), 1257–1283 (2020).
Watson, N. F. et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American academy of sleep medicine and sleep research society. J. Clin. Sleep Med. 11 (06), 591–592 (2015).
CDC. Insufficient sleep among adults. : Centers for Disease Control and Prevention; 2024 (2022). https://www.cdc.gov/sleep/data-research/facts-stats/adults-sleep-facts-and-stats.html.
Shen, B. et al. Effects of exercise on circadian rhythms in humans. Front. Pharmacol. 14, 1282357 (2023).
Youngstedt, S. D., Elliott, J. A. & Kripke, D. F. Human circadian phase-response curves for exercise. J. Physiol. 597 (8), 2253–2268 (2019).
Kripke, D. F., Elliott, J. A., Youngstedt, S. D. & Rex, K. M. Circadian phase response curves to light in older and young women and men. J. Circ. Rhythms. 5, 4 (2007).
Thomas, J. M. et al. Circadian rhythm phase shifts caused by timed exercise vary with chronotype. JCI Insight ;5(3). (2020).
Buxton, O. M. et al. Roles of intensity and duration of nocturnal exercise in causing phase delays of human circadian rhythms. Am. J. Physiol. 273 (3 Pt 1), E536–E542 (1997).
Yamanaka, Y. et al. Morning and evening physical exercise differentially regulate the autonomic nervous system during nocturnal sleep in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 309 (9), R1112–R1121 (2015).
Xie, Y. et al. Effects of exercise on sleep quality and insomnia in adults: A systematic review and Meta-Analysis of randomized controlled trials. Front. Psychiatry. 12, 664499 (2021).
Wang, F. & Boros, S. The effect of physical activity on sleep quality: a systematic review. Eur. J. Physiotherapy. 23 (1), 11–18 (2019).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35 (8), 1381–1395 (2003).
Dempsey, P. C. et al. New global guidelines on sedentary behaviour and health for adults: broadening the behavioural targets. Int. J. Behav. Nutr. Phys. Act. 17 (1), 151 (2020).
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28 (2), 193–213 (1989).
Mollayeva, T. et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep. Med. Rev. 25, 52–73 (2016).
Xie, J. et al. Evaluating the validity of current mainstream wearable devices in fitness tracking under various physical activities: comparative study. JMIR mHealth uHealth. 6 (4), e94 (2018).
Hannan, A. L. et al. High-intensity interval training versus moderate-intensity continuous training within cardiac rehabilitation: a systematic review and meta-analysis. Open. Access. J. Sports Med. 9, 1–17 (2018).
Cunha, F. A., Midgley, A. W., Monteiro, W. D. & Farinatti, P. T. Influence of cardiopulmonary exercise testing protocol and resting VO(2) assessment on %HR(max), %HRR, %VO(2max) and %VO(2)R relationships. Int. J. Sports Med. 31 (5), 319–326 (2010).
Reiter, A. M., Sargent, C. & Roach, G. D. Concordance of chronotype categorisations based on dim light melatonin onset, the Morningness-Eveningness questionnaire, and the Munich chronotype questionnaire. Clocks Sleep. 3 (2), 342–350 (2021).
St. Hilaire, M. A. & Lockley, S. W. Measuring dim light melatonin onset in humans. In Melatonin: Methods and Protocols (eds Jockers, R. & Cecon, E.) 13–20 (Springer US, 2022).
Cheung, F. T. W. et al. Validation of the Chinese version of the Munich chronotype questionnaire (MCTQ(HK)) in Hong Kong Chinese youths. Chronobiol. Int. 39 (5), 678–689 (2022).
Shen, B. Y., Liu, H. B., Cao, L. & Qin, K. R. Acute effects of different intensities of cycling acute exercise on carotid arterial apparent elasticity and hemodynamic variables. Biomed. Res. Int. 2020, 9027560 (2020).
Womersley, J. R. Oscillatory flow in arteries: effect of radial variation in viscosity on rate of flow. J. Physiol. 127 (2), 38–9P (1955).
Liu, H. et al. Effects of accumulated exercise on the stiffness and hemodynamics of the common carotid artery. Front. Physiol. 15, 1348811 (2024).
Lewis, P., Korf, H. W., Kuffer, L., Gross, J. V. & Erren, T. C. Exercise time cues (zeitgebers) for human circadian systems can foster health and improve performance: a systematic review. BMJ Open. Sport Exerc. Med. 4 (1), e000443 (2018).
Wong, S. N., Halaki, M. & Chow, C. M. The effects of moderate to vigorous aerobic exercise on the sleep need of sedentary young adults. J. Sports Sci. 31 (4), 381–386 (2013).
Andriessen, C. et al. Amount and timing of physical activity in relation to sleep quality in the general middle-aged Dutch population: A cross-sectional analysis. Prev. Med. Rep. 53, 103035 (2025).
Deboer, T. Sleep homeostasis and the circadian clock: do the circadian pacemaker and the sleep homeostat influence each other’s functioning? Neurobiol. Sleep. Circ. Rhythms. 5, 68–77 (2018).
Yamanaka, Y. et al. Differential regulation of circadian melatonin rhythm and sleep-wake cycle by bright lights and nonphotic time cues in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 307 (5), R546–R557 (2014).
Escames, G. et al. Exercise and melatonin in humans: reciprocal benefits. J. Pineal Res. 52 (1), 1–11 (2011).
Khan, I. et al. Surrogate adiposity markers and mortality. JAMA Netw. Open. 6(9). (2023).
Willis, E. A., Creasy, S. A., Honas, J. J., Melanson, E. L. & Donnelly, J. E. The effects of exercise session timing on weight loss and components of energy balance: Midwest exercise trial 2. Int. J. Obes. (Lond). 44 (1), 114–124 (2020).
Mancilla, R. et al. Exercise training elicits superior metabolic effects when performed in the afternoon compared to morning in metabolically compromised humans. Physiol. Rep. 8 (24), e14669 (2021).
Bennett, S. & Sato, S. Enhancing the metabolic benefits of exercise: is timing the key? Front. Endocrinol. (Lausanne). 14, 987208 (2023).
Sato, S. et al. Atlas of exercise metabolism reveals time-dependent signatures of metabolic homeostasis. Cell. Metab. 34 (2), 329–345 (2022).
Pendergrast, L. A. et al. Time of day determines postexercise metabolism in mouse adipose tissue. Proc. Natl. Acad. Sci. U. S. A. 120 (8), e2218510120 (2023).
Edinburgh, R. M. et al. Lipid metabolism links Nutrient-Exercise timing to insulin sensitivity in men classified as overweight or obese. J. Clin. Endocrinol. Metab. 105(3). (2020).
Toghi-Eshghi, S. R. & Yardley, J. E. Morning (Fasting) vs afternoon resistance exercise in individuals with type 1 diabetes: A randomized crossover study. J. Clin. Endocrinol. Metab. 104 (11), 5217–5224 (2019).
Savikj, M. et al. Exercise timing influences multi-tissue metabolome and skeletal muscle proteome profiles in type 2 diabetic patients—A randomized crossover trial. Metabolism. 135 (2022).
Moholdt, T. et al. The effect of morning vs evening exercise training on glycaemic control and serum metabolites in overweight/obese men: a randomised trial. Diabetologia. 64 (9), 2061–2076 (2021).
Chacon, D. & Fiani, B. A review of mechanisms on the beneficial effect of exercise on atherosclerosis. Cureus. (2020).
Ornish, D. et al. Can lifestyle changes reverse coronary heart disease? The lifestyle heart trial. Lancet 336 (8708), 129–133 (1990).
Jenkins, N. T., Martin, J. S., Laughlin, M. H. & Padilla, J. Exercise-Induced signals for vascular endothelial adaptations: implications for cardiovascular disease. Curr. Cardiovasc. Risk Rep. 6 (4), 331–346 (2012).
Stephan, J. L. & Bakker, R. O. B. G. About the role of shear stress in atherogenesis. Cardiovasc. Res. 45 (2), 270–272 (2000).
Zarins, C. K. et al. Carotid bifurcation atherosclerosis. Quantitative correlation of plaque localization with flow velocity profiles and wall shear stress. Circ. Res. 53 (4), 502–514 (1983).
Garcia, V. & Sessa, W. C. Endothelial NOS: perspective and recent developments. Br. J. Pharmacol. 176 (2), 189–196 (2019).
Bassareo, P. P. & Crisafulli, A. Gender differences in hemodynamic regulation and cardiovascular adaptations to dynamic exercise. Curr. Cardiol. Rev. 16 (1), 65–72 (2020).
Maruf, F. A., Ogochukwu, U. N., Dim, P. A. & Alada, A. R. Absence of sex differences in systolic blood pressure and heart rate responses to exercise in healthy young adults. Niger. J. Physiol. Sci. 27 (1), 95–100 (2012).
Farinatti, P., Monteiro, W., Oliveira, R. & Crisafulli, A. Cardiorespiratory responses and myocardial function within incremental exercise in healthy unmedicated older vs. young men and women. Aging Clin. Exp. Res. 30 (4), 341–349 (2018).
Acknowledgements
The author expresses gratitude to all participants. Special thanks to Professor Kairong Qin and Associate Professor Rong Liu from the Faculty of Medicine, Dalian University of Technology, for providing the experimental equipment and guidance.
Funding
This work received financial support from the National Natural Science Foundation of China (32171165 to GY; 32071157 to LC).
Author information
Authors and Affiliations
Contributions
B.S. and G.Y. designed the study; B.S., H.Z., and H.L. conducted experiments and analyzed the data; B.S. and H.Z. drafted and revised the manuscript; G.Y. and L.C. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Participants received detailed information about the experimental procedures and potential risks, and each provided written informed consent. This research was approved by the Bioethics Committees of the Dalian University of Technology (DUTSKHP230224-01), with all procedures following the principles of the Declaration of Helsinki for research involving human subjects.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shen, B., Zheng, H., Liu, H. et al. Differential benefits of 12-week morning vs. evening aerobic exercise on sleep and cardiometabolic health: a randomized controlled trial. Sci Rep 15, 18298 (2025). https://doi.org/10.1038/s41598-025-02659-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02659-8