Abstract
Sarcopenia causes muscle loss and functional decline in older adults, yet the lower limb muscle activation patterns of sarcopenic patients during functional activities remain unclear. This study aims to investigate the differences in muscle activation between sarcopenic and healthy older adults during functional activities and to explore task-specific compensatory neuromuscular strategies. Eight sarcopenic patients and eight age-matched healthy older adults performed the standardized six-meter walk test (6MWT) and five times sit-to-stand test (5STS) with surface electromyography (EMG) used to record activity from eight muscles of the dominant leg. Sarcopenic individuals exhibited lower walking speed (p = 0.005) and shorter stride length (p < 0.001) in 6MWT, as well as longer completion time (p < 0.001) in 5STS. Significant differences in muscle activation (p < 0.05) included: increased proximal muscle activation with decreased distal activation in both tasks; elevated antagonist co-activation during critical movement transitions; and task-specific EMG variability patterns with increased EMG variability during walking but decreased variability during sit-to-stand activities. Sarcopenic individuals demonstrate distinct muscle activation patterns compared to normally aging individuals. Rehabilitation for sarcopenia may benefit from incorporating ankle-strengthening exercises, functional coordination training, and task-specific neuromuscular control strategies with traditional strength-focused approaches.
Similar content being viewed by others

Introduction
Sarcopenia is a critical health concern for aging populations, characterized by age-related loss of skeletal muscle mass accompanied by reduced muscle strength or physical performance1. This condition affects approximately 10–27% of older adults worldwide2 and is associated with adverse outcomes including increased risks of falls, fractures, hospitalizations, and mortality3. Lower extremity function is particularly vital for maintaining independence and quality of life in older adults, and has also proven to be a predictor of disability and survival4,5. Physical performance assessment has become an integral part of sarcopenia diagnosis, severity evaluation, and adverse outcomes prediction. Compared to isolated muscle strength measurements, functional tasks provide more relevant information as they require coordinated activation of multiple muscle groups in movement patterns that directly relate to activities of daily living. The Asian Working Group for Sarcopenia (AWGS) recommends several standardized tests for evaluating physical function in sarcopenic individuals, including the six-meter walk test (6MWT), five times sit-to-stand test (5STS), and Short Physical Performance Battery (SPPB)1. These assessments have been widely adopted by clinicians and researchers in the field.
The understanding of sarcopenia has evolved considerably over the past decade. While initially understood primarily as age-related muscle mass loss, recent consensus definitions have expanded to incorporate muscle strength and physical performance measures1,6. Current evidence indicates that complex neuromuscular changes play a critical role in sarcopenia pathogenesis, including spinal motor neuron apoptosis, distal axon retraction, modified innervation patterns, and motor unit property changes7,8. Such neurological changes contribute to progressive decline of muscle strength and subsequent loss of muscle mass that characterizes sarcopenia. Notably, these neuromuscular changes appear to occur before clinical diagnosis of sarcopenia, as they can be detected in older non-sarcopenic individuals9. Surface electromyography (EMG) offers a non-invasive approach to examine neural activation of muscles during functional movements10. Comparative studies between older and younger adults demonstrate several age-related differences of muscle activation: greater involvement of the gluteus and thigh muscles of older adults during gait11,12, increased muscle co-activation at ankle and knee joints during both walking and sit-to-stand movements13,14, and higher variability in rectus femoris EMG amplitude during walking15.
Despite these advances in understanding sarcopenia and age-related changes in neuromuscular structure and function, limited research exists on differences of muscle activation patterns in age-matched sarcopenic individuals and healthy older adults. Besides, most studies focus solely on comparing spatiotemporal parameters or analysing muscle activation in single tasks, but task-specific compensatory strategies remain unexplored. Therefore, the primary objective of this study is to investigate the differences in muscle activation patterns between sarcopenic patients and healthy older adults during functional activities. The secondary objective is to explore the task-specific compensatory neuromuscular strategies employed across different physical performance tests. We hypothesize that sarcopenic patients and age-matched healthy controls will demonstrate significant differences in muscle activation amplitude, coactivation patterns, and variability.
Methods
Participants
Sixteen older adults (8 with sarcopenia and 8 healthy controls) were recruited through university and community posters for this cross-sectional study. Inclusion criteria specified participants aged ≥ 65 years who could walk and stand up from a chair independently. Exclusion criteria comprised conditions affecting functional performance (stroke, Parkinson’s disease, lower limb deformity, osteoarthritis, severe back pain, recent surgery) and comorbidities that could introduce risks or confounding factors (uncontrolled cardiovascular or renal disease, visible edema, implanted pacemaker, cognitive impairment, severe visual or hearing impairment). The study was approved by the Human Subjects Ethics Sub-committee of the Hong Kong Polytechnic University (Ref. No. HSEARS20240625002). All participants provided written informed consent prior to participation. Anthropometric data of the participants are presented in Table S1.
Sarcopenia assessment and classification
Participants were classified according to the AWGS 2019 consensus criteria1. Three components were evaluated:
-
1)
Muscle mass: measured using a multifrequency bioelectrical impedance device (InBody 970, Inbody Co. Ltd., Seoul, Korea). Low muscle mass was defined as skeletal muscle mass index (SMI) < 7.0 kg/m2 in men and < 5.7 kg/m2 in women.
-
2)
Muscle strength: assessed using a calibrated Smedley-type dynamometer (CAMRY EH101, Zhongshan Camry Electronic Co. Ltd., Zhongshan, China). Low muscle strength was defined as maximal handgrip strength < 28.0 kg for men and < 18.0 kg for women.
-
3)
Physical performance: evaluated using the 6MWT and 5STS. Low physical performance was defined as gait speed < 1 m/s or 5STS time > 12 s.
Sarcopenia was diagnosed when both low muscle mass and low muscle strength were present. Severe sarcopenia was diagnosed when all three components were below threshold values.
Experiment protocol
All measurements were carried out by the same examiner in an indoor laboratory. Participants were fully introduced to the procedures and safety precautions before testing. To standardize conditions, participants were provided with uniform attire, including appropriately sized shoes, socks, short-sleeved shirts, and shorts. Prior to data collection, participants received standardized demonstrations and completed 1–2 familiarization trials for each test to ensure proper technique and understanding.
Two physical performance tests were implemented in this study: the 6MWT and the 5STS. For the 6MWT, participants were instructed to walk along a flat laboratory walkway marked with red tape at 0 and 6 m at their self-selected usual pace. Timing began from a moving start and continued until the participant crossed the 6-meter mark, with no deceleration permitted. A valid trial was considered when the participant’s entire right foot contacted the force plate during the walk. The 5STS used a dual force plate setup, with a standard chair (height: 43 cm)16 mounted on one force plate and a separate force plate for foot placement. Participants maintained a neutral spine sitting position with arms crossed over the chest and approximately 90-degree knee flexion. Upon verbal command, participants performed five consecutive sit-to-stand cycles as quickly as possible. Timing began from the initial seated position and ended upon return to the seated position after the fifth repetition. Valid trials required participants to achieve full standing and make buttock contact with the chair between repetitions. Each participant performed five successful 6MWT trials and three 5STS trials, with adequate rest periods provided as needed. All tests were completed within a single day for each participant.
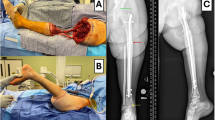
Biomechanical data were collected using an optical-based motion capture system with eight cameras (Vicon Motion System, Oxford Metrics Ltd, Oxford, UK) and a force platform system (OR6, AMTI, Watertown, USA). A total of 43 reflective markers were attached to the anatomical landmarks of each participant as shown in Fig. 1. The force platform recorded ground reaction forces during the right foot stance phase in gait, as well as forces from both feet and chair-ground contact during sit-to-stand tests, with the latter used to detect seat contact events.
Muscle activity was measured using wireless surface EMG sensors (Trigno Avanti, Delsys Inc., Massachusetts, USA) following SENIAM guidelines17. EMG signals were recorded from eight muscles of the right dominant leg: gluteus maximus (GMax), gluteus medius (GMed), rectus femoris (RF), vastus medialis (VM), vastus lateralis (VL), biceps femoris (BF), gastrocnemius medialis (GA), and tibialis anterior (TA). Prior to electrode placement, standardized skin preparation procedures were implemented, including local hair removal and alcohol cleansing to ensure good conduction. The maximal voluntary contraction (MVC) tests were performed following the guideline18 before physical performance tests to establish reference values for EMG signal normalization. Participants were instructed to perform maximal isometric contractions against manual resistance in standardized positions for each muscle, holding each contraction for 5 s with verbal encouragement to ensure maximal effort. Two trials were conducted per muscle, with 60 s of rest between trials, and the highest EMG amplitude was recorded for normalization. The motion capture, force platform, and EMG system were synchronized at sampling rates of 250 Hz, 2000 Hz and 2000 Hz, respectively.
Data processing and outcome variables
Temporal phase definition
A gait cycle studied in the 6MWT trial was defined from initial right heel strike, which was identified when the vertical ground reaction force on Force Plate 1 (FP1) exceeded 20 N19 to subsequent ipsilateral heel strike, when the right heel marker reached its minimum vertical displacement along the z-axis. Following Perry et al.‘s (1992) model20, each gait cycle was subdivided into seven phases: loading response (0–10% of the gait cycle), mid-stance (10–30%), terminal stance (30–50%), pre-swing (50–60%), initial swing (60–73%), mid-swing (73–87%) and terminal swing (87–100%). To eliminate the influence of leg length on walking speed measurements, nondimensional walking speed was calculated21:
where \(V~\)represents the actual walking speed, g is gravitational acceleration, L represents leg length, and \(Vmax\) is defined as \({\sqrt {g \cdot L} }\), representing the theoretical maximum walking speed based on leg length.
The 5STS test was analyzed as five consecutive cycles, with each cycle comprising four distinct phases (forward, upward, downward, backward)22. The “forward” phase initiated with body movement onset (defined as right shoulder marker velocity > 50 mm/s along the anterior direction) and ended at seat-off (vertical reaction force on Force Plate 2 (FP2) < 40 N). The “upward” phase extended from seat-off to full standing position, marked by peak vertical displacement of the right shoulder marker. The “downward” phase spanned from full standing to seat contact (vertical force on FP2 > 40 N). The “backward” phase encompassed the period from seat contact to the balanced sitting position. For the first four repetitions, this phase terminated at the initiation of the subsequent repetition’s forward phase (when anterior velocity exceeded 50 mm/s). For the final repetition, the backward phase concluded when the posterior velocity decreased below 50 mm/s, indicating completion of the entire 5STS task.
EMG signal processing
Raw surface EMG signals were first filtered using a zero-lag second-order Butterworth band-pass filter (20–450 Hz) to minimize baseline noise and movement artifact. The filtered signals were subsequently full-wave rectified and smoothed using a zero-lag fourth-order Butterworth low-pass filter with a 6 Hz cutoff frequency. EMG amplitudes were then normalized to their respective MVC values. For standardization purposes, both gait cycle and 5STS data were time-interpolated to a normalized 101-point time base. The mean values of five gait cycles and three 5STS trials were computed for each participant within their respective groups.
Outcome measures
Primary outcome variables included spatiotemporal parameters and multiple EMG-derived parameters: muscle activation amplitudes, maximum and mean values, coactivation index, and variability of activation.
Muscle activation envelope parameters:
For each of the eight muscles recorded, means and standard deviations of EMG envelopes were calculated at each percentage of the gait cycle and 5STS trial. Maximum and mean values of each EMG envelope were calculated through the gait cycle and 5STS trial.
Coactivation index (CI):
CI is the measure of simultaneous agonist-antagonist muscle activation, an index for movement stability23. To facilitate better interpretation and consistency, we adopted the normalization-based CI calculation method that scales the CI values to a range of 0–1. The value of 1 corresponds to the maximal coactivation and the value of 0 corresponds to no activation. The coactivation levels of the RF/BF, VM/BF, VL/BF, and TA/GA of the dominant leg were calculated for each trial using the following equation24:
where \({I_{antagonist}}\) is the area of the total antagonistic activity and \({I_{total}}\) is the integral of the sum of agonist and antagonist.
Variability of activation:
To quantify EMG variability across multiple trials for each participant, MeanSD was determined25:
where \(SD\left( i \right)\) represents the standard deviation of EMG activation at the ith % of the normalized gait cycle or 5STS trial, calculated across all trials performed by each participant, and \({\left\langle \cdot \right\rangle _i}\) indicates the average over all i.
Statistical analysis
Statistical analyses were performed using SPSS software (version. 27.0; IBM Corp., Armonk, NY, USA). Descriptive statistics were expressed as means ± standard deviations (SD) for continuous variables. Data normality was assessed using the Shapiro-Wilk test. For between-group comparisons, independent samples t-tests were conducted for normally distributed variables after verifying the homogeneity of variances using Levene’s test. When the assumption of equal variances was violated, Welch’s t-test was applied. For non-normally distributed data, the Mann-Whitney U tests were performed. Results included p-values, test statistics, and effect sizes (t statistic and Cohen’s d for t-tests; Z statistic and effect size r (calculated as\(\:\left|Z\right|/\sqrt{N}\) ) for Mann-Whitney U tests). Effect sizes were interpreted following Cohen’s guidelines26: for d values, small (0.2 ≤ d < 0.5), medium (0.5 ≤ d < 0.8), and large (d ≥ 0.8) effects; for r values, small (0.1 ≤ r < 0.3), medium (0.3 ≤ r < 0.5), and large (r ≥ 0.5) effects. Statistical significance was set at p < 0.05 (two-tailed) for all analyses.
Results
Spatiotemporal parameters
Results from the 6MWT showed significantly slower walking speeds (t = 3.315, p = 0.005, d = 1.658, large effect), lower nondimensional walking speeds (t = 2.944, p = 0.011, d = 1.472, large effect), shorter stride lengths (t = 4.402, p < 0.001, d = 2.201, large effect), and reduced normalized stride lengths (t = 3.857, p = 0.002, d = 1.929, large effect) in sarcopenic patients compared to healthy controls (Table 1). However, no significant differences were observed between groups in cadence (t = 0.682, p = 0.506), stride time (t = -0.742, p = 0.471), or stance phase percentage (t = -0.431, p = 0.673).
In the 5STS, the sarcopenic group showed significantly longer total completion time (Z = -5.856, p < 0.001, d = 0.845, large effect) and average repetition time (Z = -5.856, p < 0.001, d = 0.845, large effect) compared to healthy older adults (Table 2). Phase analysis revealed significant between-group differences in average forward (Z = -4.186, p < 0.001, d = 0.604, large effect), upward (Z = -5.485, p < 0.001, d = 0.792, large effect), downward (Z = -5.505, p < 0.001, d = 0.795, large effect), and backward phases (Z = -4.763, p < 0.001, d = 0.687, large effect). Among these phases, the downward phase demonstrated the longest duration in both groups.
Muscle activation amplitudes
EMG analysis of the gait cycle revealed distinct muscle activation patterns between sarcopenic patients and healthy older adults (Table 3). The sarcopenic group demonstrated increased activation of proximal muscles and decreased activation of distal muscles. During the stance phase, proximal muscles showed elevated activation patterns in sarcopenic patients. Loading response (0–10%) showed significantly higher activation in gluteal and thigh muscles (p < 0.005, medium to large effects). This elevated proximal muscle activation continued through mid-stance (10–30%) and terminal stance (30–50%), while the distal muscles (GA and TA) showed significantly lower activation (p < 0.05, small to medium effects). Pre-swing (50–60%) was characterized by sustained elevated thigh muscle activation (VM, VL, BF; all p < 0.001, small to large effects) and decreased distal muscle activity. The swing phase displayed phase-specific patterns: initial swing (60–73%) showed higher knee extensor activation (RF, VM, VL; all p < 0.001, small to large effects) and decreased GMed activation (p = 0.026, r = 0.154, small effect); mid-swing (73–87%) demonstrated increased proximal muscle activity in GMax (p < 0.001, r = 0.229, small effect), knee extensors (VM and VL, p < 0.001, small to medium effect), and BF (p = 0.002, r = 0.219, small effect); terminal swing (87–100%) displayed increased BF activation (p < 0.001, r = 0.424, medium effect), and decreased RF and TA activity (RF: p = 0.002, r = 0.261, small effect; TA: p < 0.001, r = 0.346, medium effect).
Temporal EMG patterns demonstrated these changes throughout the gait cycle (Fig. 2a). The quadriceps group (VM, VL, RF) demonstrated consistently higher activation throughout stance phase in sarcopenic patients. The hip muscles (GMax, GMed) showed selective increases during weight acceptance phases. Distal muscles exhibited contrasting patterns: GA showed consistently lower activation in sarcopenic patients during stance phase, while TA demonstrated phase-specific differences, particularly during pre-swing and terminal swing.
Ensemble electromyographic activities during walking and sit-to-stand tasks. (a) Normalized EMG activities during the gait cycle. Light shaded areas indicate ± 1 standard deviation. Horizontal lines with asterisks denote significant between-group differences (p < 0.05). (b) Normalized EMG activities during the five times sit-to-stand test.
Analysis of the 5STS revealed distinct activation patterns across movement phases and repetitions (Table 4). Overall performance showed high activation levels in quadriceps muscles (RF: 9–10% MVC, VM and VL: 6–9% MVC), moderate TA activation (4–6% MVC), and low activation in GMax, GMed, BF, and GA (1–2% MVC). Temporal EMG patterns throughout the task duration demonstrated clear between-group differences in muscle activation strategies (Fig. 2b). Throughout the task, the sarcopenic group exhibited significantly higher activation in proximal muscles (GMax, VM, BF; p < 0.001, small effect), while healthy controls demonstrated greater distal muscle activation (GA, TA; p < 0.001, small effect). No significant difference was observed among the five repetitions within the test. Phase-specific analysis revealed that during the forward phase, healthy participants demonstrated better preparatory muscle activation in RF (p < 0.001, r = 0.175, small effect) and TA (p = 0.001, r = 0.110, small effect). The upward phase exhibited peak activation in anti-gravity muscles, with sarcopenic participants showing significantly higher VM (p < 0.001, r = 0.272, small effect) and BF activation (p < 0.001, r = 0.195, small effect). The quadriceps muscles showed a unique activation pattern in sarcopenic patients: RF and VM maintained consistently higher activation throughout the task, while VL demonstrated significantly higher activation only during the downward phase (p < 0.001, r = 0.135, small effect) and remained lower during other phases. The backward phase demonstrated the lowest overall activation levels across all muscles, with differences in postural control strategies characterized by higher proximal muscle activation in the sarcopenic group (GMax and GMed) and higher distal muscle activation (GA and TA) in healthy controls.
Maximum and mean value in envelopes
The maximum and mean EMG values during both functional tasks were quantified (Table 5) and compared between groups (Fig. 3). In the 6MWT, the sarcopenic group showed significantly higher maximum activation in three thigh muscles: VM (p = 0.017, r = 0.267, small effect), VL (p < 0.001, r = 0.466, medium effect), and BF (p < 0.001, r = 0.566, large effect). Conversely, the GA exhibited significantly lower activation (p = 0.002, r = 0.341, medium effect). Mean EMG analysis revealed significantly higher VM (p = 0.001, r = 0.356, medium effect), VL (p < 0.001, r = 0.454, medium effect), BF (p < 0.001, r = 0.502, large effect), and GMax (p = 0.010, r = 0.289, small effect) activity in the sarcopenic group, while GA maintained significantly lower mean activity (p = 0.001, r = 0.364, medium effect). The GMed, RF, and TA showed no significant between-group differences in either maximum or mean EMG values (all p > 0.05).
During the 5STS, the quadriceps muscle group demonstrated the highest activation levels (maximum: 22–34% MVC; mean: 5–10% MVC), followed by moderate TA activation (maximum: 17–19% MVC; mean: 4–6% MVC). Other muscles displayed relatively lower activation levels (maximum: 4–9% MVC; mean: 0.9–2% MVC). Between-group analysis identified significantly higher mean VM activation in the sarcopenic group (p = 0.039, r = 0.298, small effect).
Box plots of maximum and mean normalized electromyographic activity during (a) 6-meter walking test and (b) five times sit-to-stand test in sarcopenic patients and healthy older adults. Box plots indicate the median (black dot), interquartile range (box edges: 25th-75th percentiles), mean values (black cross), and outliers (circles). Asterisks (*) denote statistically significant differences between groups.
Co-activation index
Analysis of muscle co-activation during gait revealed that the RF/BF co-activation index during the pre-swing phase was significantly higher in the sarcopenia group compared to the healthy group (p = 0.016, r = 0.760, large effect) (Table S2). No significant differences were observed in other muscle pairs (TA/GA, VM/BF, and VL/BF) across all gait phases, or for RF/BF during other phases of the gait cycle (p > 0.05).
During the 5STS (Table 6), the sarcopenia group demonstrated significantly higher RF/BF co-activation throughout the entire test and among repetitions (both p = 0.019, r = 0.390, medium effect), particularly during the forward phase (p < 0.001, r = 0.559, large effect) and downward phase (p = 0.006, r = 0.448, medium effect). Other muscle pairs showed phase-specific differences: VM/BF during the downward phase (p = 0.034, r = 0.315, medium effect), VL/BF during the forward phase (p = 0.018, r = 0.353, medium effect), and TA/GA during the backward phase (p = 0.035, r = 0.304, medium effect). The temporal pattern of thigh muscle co-activation also varied: RF/BF pair showed peak co-activation during the upward phase, while VM/BF and VL/BF pairs peaked during the backward phase.
Variability of activation
During 6MWT (Table S3), sarcopenic participants demonstrated significantly higher variability in BF (p = 0.021, r = 0.598, large effect) throughout the entire gait cycle compared to healthy controls. Phase-specific increases in variability were observed in VL during loading response (p = 0.027, r = 0.551, large effect), VM during mid-stance (p = 0.021, r = 0.578, large effect) and initial swing (p = 0.021, r = 0.578, large effect), and BF during terminal swing (p = 0.021, r = 0.598, large effect). This suggests increased neuromuscular control variability primarily in proximal muscles during walking.
In contrast, during the 5STS (Table S4), sarcopenic participants exhibited significantly decreased between-repetition variability in VL (p = 0.002, r = 0.455, medium effect) compared to healthy controls. Phase-specific analysis revealed substantially lower variability in sarcopenic participants during the forward phase for VL (p = 0.002, r = 0.443, medium effect), RF (p = 0.021 r = 0.370, medium effect), GA (p = 0.016, r = 0.348, medium effect), and TA (p = 0.011, r = 0.366, medium effect), as well as during the downward phase for VL (p = 0.003, r = 0.432, medium effect). However, VM showed higher variability in sarcopenic participants during the upward phase (p = 0.026, r = 0.321, medium effect). The gluteal muscles showed no significant between-group differences.
Discussion
This study aimed to investigate the differences in muscle activation patterns between sarcopenic patients and healthy older adults during functional activities and to explore the task-specific compensatory neuromuscular strategies employed across different physical performance tests. Our findings suggest that sarcopenic older adults exhibit a proximalization pattern of muscle activation during functional activities, characterized by significantly higher activation in proximal muscles (GMax, VM, VL, RF, BF) and lower activation in distal muscle (GA, TA); elevated antagonist co-activation index; task-specific EMG variability differences with increased variability during walking but decreased variability during sit-to-stand; impaired functional performance with slower walking speed, shorter stride length, and prolonged sit-to-stand times.
The observed proximalization pattern of muscle activation aligns with previous research on age-related changes. Aging is associated with the atrophy of motor cortical regions and degeneration of neurotransmitter systems, resulting in increased recruitment thresholds for motor units, which requires higher muscle activation to perform identical movements8,27. Previous research has documented a distal-to-proximal shift in joint torques and power during walking when comparing young and healthy older adults28. This shift similarly appears when comparing stronger and weaker older adults, with weaker individuals showing greater hip reliance and less ankle dependence29. This decreased distal muscle dependence is likely caused by plantarflexor weakness, which limits propulsive capacity30as well as diminished afferent feedback to ankle muscles with aging31. Both strength deficits and sensory impairments in distal muscles may necessitate greater compensatory reliance on proximal hip muscles. Our age-matched comparison between sarcopenic patients and healthy older adults revealed similar changes consistent with patterns observed during aging. This suggests that sarcopenia may represent an accelerated muscular aging phenotype, though future physiological studies are needed to confirm this finding. From a physiological perspective, increased thigh muscle activation may be explained by the susceptibility of quadriceps to age-related atrophy compared to distal and pelvic muscles32,33coupled with compensatory motor unit reinnervation processes that potentially lead to enlarged motor unit territories requiring heightened neural drive to achieve functional movement34. This proximalization pattern potentially limits walking speed35 and contributes to decreased walking economy through increased energy expenditure36. Targeted ankle muscle strengthening may improve walking performance and reduce proximal compensation strategies in sarcopenia.
Our study revealed higher coactivation in the RF/BF muscle pair compared to other muscle pairs, particularly during the pre-swing phase of gait cycle and the forward/downward phases of 5STS. Functionally, RF and BF precisely control the transition from stance to swing during pre-swing phase, regulate center of mass movement with hip and knee joint stability in the forward phase, and manage complex eccentric contraction during the downward phase. As biarticular muscles, their regional activation patterns require more sophisticated neural regulation37especially during these critical movement transitions. Beyond the motor unit remodelling effects on fine motor control, previous research suggests that age-related decreases in cortical and spinal reciprocal inhibition potentially facilitate increased antagonistic muscle coactivity38but whether similar neural mechanisms exist between age-matched sarcopenic individuals and healthy older adults remains unexplored. This increased coactivation appears to function as a compensatory strategy that enhances joint stability23while simultaneously limiting movement speed and increasing metabolic cost39. These findings suggest that comprehensive rehabilitation strategies, which include functional coordination training and sensorimotor integration exercises, are more likely to provide better outcomes compared to traditional approaches that only focus on strength training.
Sarcopenic individuals show task-specific patterns in muscle activation variability: increased EMG variability during walking (particularly in proximal muscles) but decreased variability during the 5STS test. The distinct directional changes in variability may be explained by two factors: neural control mechanisms and task execution strategies. While both walking and 5STS appear rhythmic, they involve different neural control mechanisms. Walking is inherently rhythmic and regulated primarily by the spinal-level central pattern generators (CPGs)40, while the 5STS task is goal-directed and requires precise cortical and subcortical coordination41. Therefore, sarcopenic individuals experiencing neuromuscular deterioration likely face decreased ability to maintain stable gait while walking, but may adopt compensatory, rigid movement strategies during rapid and effortful tasks like 5STS to preserve efficiency and minimize fall risks. Moreover, variability may be influenced by the task execution strategy in walking at a preferred speed compared to the maximal speed during the 5STS. Preferred-speed strategy allows greater flexibility and adaptive adjustments. But the maximal-speed tasks like 5STS encourage participants to select the most economical and stereotyped motor patterns, which constrains variability. Although it was suggested that gait variability in older adults is mainly due to deficits in strength and flexibility rather than speed25, further research is needed to clarify the independent role of execution speed on EMG variability. Functionally, increased variability during walking may lead to gait instability and fall risk, while decreased variability during 5STS may reflect a rigid control strategy that sacrifices adaptability for stability. Rehabilitation approaches might benefit from promoting optimal variability through integration of diverse neuromuscular control strategies, rather than focusing solely on strength or endurance42.
This study facilitates a deeper understanding of neuromuscular adaptation patterns in sarcopenia. First, by comparing age-matched sarcopenic and healthy older adults, it identifies adaptations specific to sarcopenia rather than general aging effects, including a previously undocumented compensatory pattern of expanded proximal muscle activation in both hip and thigh muscles. Second, the assessment across functional tasks reveals task-specific compensatory strategies, providing insight into sarcopenic adaptations during real-world activities. Third, the integration of variability analysis with EMG measures reveals functional differences from a motor control perspective, highlighting sarcopenia as a complex neuromuscular disorder rather than simply a muscle mass deficit.
From a clinical perspective, these findings suggest that rehabilitation strategies may benefit from addressing the specific neuromuscular adaptations observed in sarcopenic individuals through three evidence-based approaches. First, targeted ankle muscle strengthening should be emphasized, with evidence supporting interventions such as high-velocity/low-load ankle power training43, multi-directional ankle strengthening44, intrinsic foot muscle exercises45, and ankle power biofeedback training46, to restore distal muscle function and reduce proximal compensations. Second, functional coordination and sensorimotor integration exercises should be incorporated, with effective approaches encompassing balance and proprioceptive training47 and cognitive-motor dual-task training48, to address elevated antagonist coactivation and refine reciprocal inhibition mechanisms beyond traditional strength training approaches. Third, task-specific neuromuscular variability training should be implemented to address the distinct neural control mechanisms underlying different functional activities: progressive gait perturbation or variable speed protocols for walking tasks that utilize spinal-level central pattern generators, and variable initial position or movement speed training with environmental constraint modifications for sit-to-stand and other goal-directed tasks that require cortical-subcortical coordination, to optimize movement adaptability while maintaining stability49,50. However, future randomized controlled trials are needed to validate the efficacy of these specific training protocols in sarcopenic populations and determine optimal intervention parameters for clinical implementation.
Several methodological considerations should be acknowledged when interpreting our findings. First, given the pilot and exploratory nature of this investigation, the sample size was relatively small, and there was a gender imbalance among participants, which could potentially limit the generalizability of our findings. Due to the limited sample size, we did not perform a formal covariate analysis of potential sex differences. Future studies with balanced and larger cohorts are recommended to assess potential sex-specific effects on neuromuscular activation. Second, our participants were Asian older adults diagnosed with severe sarcopenia. Thus, findings should be cautiously generalized to other populations or ethnic groups. Third, surface EMG primarily captures superficial muscle activity and may be affected by subcutaneous fat thickness, possibly missing contributions from deeper muscles involved in compensatory strategies. Future research may use more advanced techniques to further elucidate these findings. For instance, high-density EMG could provide more detailed recruitment pattern changes, while ultrasound elastography might help assess intrinsic muscle properties related to compensatory strategies. Additionally, wearable sensors would enable monitoring of neuromuscular function during daily activities in natural settings. Clinically, it may be useful to investigate the efficacy of interventions integrating neuromuscular control and coordination training alongside traditional strength exercises. Exploring the use of neuromuscular electrical stimulation with functional training may also lead to better interventions for the compensatory patterns observed in our participants.
Conclusion
This study revealed distinct neuromuscular adaptations in sarcopenic older adults during functional activities, characterized by a proximalization pattern of muscle activation, increased antagonist co-activation, and task-specific EMG variability. Sarcopenic individuals demonstrated greater reliance on proximal muscles (hip and thigh) with decreased activation of distal muscles during functional tasks. Sarcopenic older adults also exhibited elevated antagonist co-activation index, particularly in the RF/BF muscle pair during critical movement transitions. Task-specific variability patterns were observed, with increased EMG variability during walking but decreased variability during sit-to-stand activities. These compensatory mechanisms extended beyond typical age-related changes and broadened our understanding of sarcopenia as a complex neuromuscular disorder rather than merely a muscle mass deficit. Future research with larger, diverse populations and advanced techniques is needed to validate these findings and develop more targeted rehabilitation strategies for sarcopenic patients.
Data availability
The data are provided within the manuscript and supplementary information files. The original data that support the findings of this study are available upon request to the corresponding author. The original data are not publicly available due to privacy or ethical restrictions.
References
Chen, L. K. et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 21, 300–307e2 (2020).
Petermann-Rocha, F. et al. Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle. 13, 86–99 (2022).
Beaudart, C., Zaaria, M., Pasleau, F., Reginster, J. Y. & Bruyère, O. Health outcomes of sarcopenia: a systematic review and Meta-Analysis. PLOS ONE. 12, e0169548 (2017).
Guralnik, J. M., Ferrucci, L., Simonsick, E. M., Salive, M. E. & Wallace, R. B. Lower-Extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl. J. Med. 332, 556–562 (1995).
Studenski, S. et al. Gait speed and survival in older adults. JAMA 305, 50–58 (2011).
Cruz-Jentoft, A. J. et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 48, 601 (2019).
Moreira-Pais, A., Ferreira, R., Oliveira, P. A. & Duarte, J. A. A neuromuscular perspective of sarcopenia pathogenesis: deciphering the signaling pathways involved. GeroScience 44, 1199–1213 (2022).
Hunter, S. K., Pereira, H. M. & Keenan, K. G. The aging neuromuscular system and motor performance. J. Appl. Physiol. 121, 982–995 (2016).
Sarto, F. et al. Neuromuscular impairment at different stages of human sarcopenia. J. Cachexia Sarcopenia Muscle. 15, 1797–1810 (2024).
Farina, D., Merletti, R. & Enoka, R. M. The extraction of neural strategies from the surface EMG: an update. J. Appl. Physiol. 117, 1215–1230 (2014).
Schloemer, S. A., Thompson, J. A., Silder, A., Thelen, D. G. & Siston, R. A. Age-Related differences in gait kinematics, kinetics, and muscle function: a principal component analysis. Ann. Biomed. Eng. 45, 695–710 (2017).
Hallal, C. Z., Marques, N. R., Spinoso, D. H., Vieira, E. R. & Gonçalves, M. Electromyographic patterns of lower limb muscles during apprehensive gait in younger and older female adults. J. Electromyogr. Kinesiol. 23, 1145–1149 (2013).
Kim, H. K. & Chou, L. S. Lower limb muscle activation in response to balance-perturbed tasks during walking in older adults: a systematic review. Gait Posture 93, 166–176 (2022).
Sadeh, S., Gobert, D., Shen, K. H., Foroughi, F. & Hsiao, H. Y. Biomechanical and neuromuscular control characteristics of sit-to-stand transfer in young and older adults: a systematic review with implications for balance regulation mechanisms. Clin. Biomech. 109, 106068 (2023).
Bailey, C. A. et al. Sex-independent and dependent effects of older age on cycle-to-cycle variability of muscle activation during gait. Exp. Gerontol. 124, 110656 (2019).
Kuo, Y. L. The influence of chair seat height on the performance of community-dwelling older adults’ 30-second chair stand test. Aging Clin. Exp. Res. 25, 305–309 (2013).
Stegeman, D. & Hermens, H. Standards for surface electromyography: the European project surface EMG for non-invasive assessment of muscles (SENIAM). Enschede Roessingh Res. Dev. 10, 8–12 (2007).
Konrad, P. The ABC of EMG: A Practical Introduction to Kinesiological Electromyography (Wiley, 2005).
Altman, A. R. & Davis, I. S. A kinematic method for footstrike pattern detection in barefoot and shod runners. Gait Posture. 35, 298–300 (2012).
Perry, J. Gait Analysis: Normal and Pathological Function (SLACK, 2010).
Uchida, T. K. Biomechanics of Movement: the Science of Sports, Robotics, and Rehabilitation (The MIT Press, 2020).
Ippersiel, P., Robbins, S. & Preuss, R. Movement variability in adults with low back pain during sit-to-stand-to-sit. Clin. Biomech. 58, 90–95 (2018).
Latash, M. L. Muscle coactivation: definitions, mechanisms, and functions. J. Neurophysiol. 120, 88–104 (2018).
Keloth, S. M., Arjunan, S. P., Raghav, S. & Kumar, D. K. Muscle activation strategies of people with early-stage parkinson’s during walking. J. Neuroeng. Rehabil. 18, 133 (2021).
Kang, H. G. & Dingwell, J. B. Dynamics and stability of muscle activations during walking in healthy young and older adults. J. Biomech. 42, 2231–2237 (2009).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences (Routledge, 2013). https://doi.org/10.4324/9780203771587.
Seidler, R. D. et al. Motor control and aging: links to age-related brain structural, functional, and biochemical effects. Neurosci. Biobehav Rev. 34, 721–733 (2010).
DeVita, P. & Hortobagyi, T. Age causes a redistribution of joint torques and powers during gait. J. Appl. Physiol. 88, 1804–1811 (2000).
Hortobágyi, T., Rider, P., Gruber, A. H. & DeVita, P. Age and muscle strength mediate the age-related Biomechanical plasticity of gait. Eur. J. Appl. Physiol. 116, 805–814 (2016).
Tijs, C., Bernabei, M., van Dieën, J. H. & Maas, H. Myofascial loads can occur without fascicle length changes. Integr. Comp. Biol. 58, 251–260 (2018).
Franz, J. R. & Kram, R. How does age affect leg muscle activity/coactivity during uphill and downhill walking? Gait Posture. 37, 378–384 (2013).
Abe, T., Loenneke, J. P., Thiebaud, R. S. & Fukunaga, T. Age-related site-specific muscle wasting of upper and lower extremities and trunk in Japanese men and women. Age 36, 813 (2013).
Fuchs, C. J. et al. Thigh muscles are more susceptible to age-related muscle loss when compared to lower leg and pelvic muscle. Exp. Gerontol. 175, 112159 (2023).
Clark, D. J. & Fielding, R. A. Neuromuscular contributions to Age-Related weakness. J. Gerontol. Biol. Sci. Med. Sci. 67A, 41–47 (2012).
Conway, K. A. & Franz, J. R. Increasing the propulsive demands of walking to their maximum elucidates functionally limiting impairments in older adult gait. J. Aging Phys. Act. 28, 1–8 (2020).
Delabastita, T. et al. Distal-to-proximal joint mechanics redistribution is a main contributor to reduced walking economy in older adults. Scand. J. Med. Sci. Sports. 31, 1036–1047 (2021).
Watanabe, K., Vieira, T. M., Gallina, A., Kouzaki, M. & Moritani, T. Novel insights into biarticular muscle actions gained from High-Density electromyogram. Exerc. Sport Sci. Rev. 49, 179 (2021).
Hortobágyi, T., del Olmo, M. F. & Rothwell, J. C. Age reduces cortical reciprocal Inhibition in humans. Exp. Brain Res. 171, 322–329 (2006).
Piche, E. et al. Metabolic cost and co-contraction during walking at different speeds in young and old adults. Gait Posture. 91, 111–116 (2022).
Takakusaki, K. Neurophysiology of gait: from the spinal cord to the frontal lobe. Mov. Disord Off J. Mov. Disord Soc. 28, 1483–1491 (2013).
Lee, S. H. et al. Cortical activities during a stand to sit movement using fNIRS. In 14th International Conference on Control, Automation and Systems (ICCAS 2014) 279–281 (2014). https://doi.org/10.1109/ICCAS.2014.6988002.
Nørgaard, J. E. et al. Effects of gait adaptability training on falls and fall-related fractures in older adults: a systematic review and meta-analysis. Age Ageing. 50, 1914–1924 (2021).
Webber, S. C. & Porter, M. M. Effects of ankle power training on movement time in mobility-impaired older women. Med. Sci. Sports Exerc. 42, 1233–1240 (2010).
Xu, H. & Liu, H. Effects of ankle isokinetic training on muscle strength and balance amongst older women with mild parkinson’s disease: a randomised trial. J. Back Musculoskelet. Rehabil. 37, 1007–1014 (2024).
Futrell, E. E., Roberts, D. & Toole, E. The effects of intrinsic foot muscle strengthening on functional mobility in older adults: A systematic review. J. Am. Geriatr. Soc. 70, 531–540 (2022).
Browne, M. G. & Franz, J. R. Ankle power biofeedback attenuates the distal-to-proximal redistribution in older adults. Gait Posture. 71, 44–49 (2019).
Varjan, M., Žiška Böhmerová, Ľ., Oreská, Ľ., Schickhofer, P. & Hamar, D. In elderly individuals, the effectiveness of sensorimotor training on postural control and muscular strength is comparable to resistance-endurance training. Front. Physiol. 15, 1386537 (2024).
Ghai, S., Ghai, I. & Effenberg, A. O. Effects of dual tasks and dual-task training on postural stability: a systematic review and meta-analysis. Clin. Interv Aging. 12, 557–577 (2017).
McCrum, C., Gerards, M. H. G., Karamanidis, K., Zijlstra, W. & Meijer, K. A systematic review of gait perturbation paradigms for improving reactive stepping responses and falls risk among healthy older adults. Eur. Rev. Aging Phys. Act. Off J. Eur. Group. Res. Elder. Phys. Act. 14, 3 (2017).
Stergiou, N. & Decker, L. M. Human movement variability, nonlinear dynamics, and pathology: is there a connection? Hum. Mov. Sci. 30, 869–888 (2011).
Acknowledgements
Data collection was performed in the Human Locomotion Laboratory of Department of Biomedical Engineering, Faculty of Engineering, The Hong Kong Polytechnic University. The authors are grateful to the participants in the experiment.
Funding
This work was supported by the research studentship from the Hong Kong Polytechnic University, Research Grants Council, University Grants Committee (PolyU 15211322), and Chongqing Wanzhou District PhD Direct-Access Research Project (wzstc-20220132).
Author information
Authors and Affiliations
Contributions
H.C. participated in the research design, data collection, data analysis, results interpretation, initial manuscript draft, manuscript revision, and submission preparation. G.Z. conducted data collection, result interpretation, and manuscript revision. L.W. conducted data collection and manuscript revision. J.X. conducted data collection and designed schematic diagrams. F.Y. conducted research design and manuscript revision. M.Z. conceived this study and contributed to the final version of this paper. All authors have read and approved the final version of the manuscript and agree with the order of the presentation of the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Human Subjects Ethics Sub-committee of the Hong Kong Polytechnic University (Ref. No. HSEARS20240625002). The study was performed in accordance with the 1964 Declaration of Helsinki and later amendments.
Informed consent
All participants provided written informed consent prior to participation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cai, H., Zhang, G., Wei, L. et al. Lower extremity muscle activation patterns in sarcopenic older adults during physical performance tests: implications for rehabilitation approaches. Sci Rep 15, 26932 (2025). https://doi.org/10.1038/s41598-025-10429-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10429-9