Abstract
The homeostasis of gastric mucosa is extremely delicate. Neutrophils, the most abundant immune cells in human circulation, are regarded crutial in the regulation of gastric mucosal immune response. Non-steroidal anti-inflammatory drugs (NSAIDs) induced gastric injury is the second major reason for gastric ulcers. The relations between neutrophils and Indomethacin-induced gastric injury are not fully understood. A mouse model of gastric injury was established using Indomethacin, followed by proteomic analysis (raw data are available via ProteomeXchange with identifier PXD058482). GO functional annotations and KEGG pathway enrichment analysis were conducted on significant differential proteins. The formation of neutrophil extracellular traps (NETs) was observed using ELISA and immunofluorescence. TEM, Western blot and Real-time PCR were applied to observe programmed death of gastric epithelial cells (GECs), and ELISA was conducted to measure levels of TNF-α and IL-1β in the gastric tissue. Deoxyribonuclease 1 (DNase 1), a NETs inhibitor, was administered intraperitoneally to inhibit NETs formation. In vitro, neutrophils were isolated from peripheral blood of mice and co-cultured with mouse GECs cell line, different dosage of Indomethacin were added to the culture dish, the levels of inflammatory factors, formation of NETs and GECs programmed death were assessed in vitro. Poly morphonuclear neutrophils (PMN) were extracted from mouse peripheral blood and single-cell RNA-sequencing (scRNA-seq) was further applied (raw data are available via Genome Sequence Archive with identifier CRA020950) to explore the intracellular mechanism of NETs formation. ELISA and immunofluorescence were performed to validate expression of IL-17 signaling pathway. After Indomethacin gavage, obvious gastric injury was observed. Proteomic analysis indicated that NETs formation played a crucial role in Indomethacin-induced gastric injury. Compared to control group, Indomethacin treatment resulted in NETs formation, elevated levels of TNF-α and IL-1β and GECs programmed death. Inhibition of NETs significantly reduced inflammatory factor levels and mitigated gastric injury caused by indomethacin. In vitro, 200 µL, 400 µL and 600 µL of Indomethacin caused excessive NETs formation in neutrophils. Besides, Indomethacin-induced NETs formation led to GECs programmed death in vitro. scRNA-seq revealed that neutrophils enrichment in the peripheral blood of Indomethacin-induced gastric injury and IL-17 signaling might be the key intracellular of NETs formation. Expressions of neutrophil IL-17R and concentration of IL-17 were significantly higher in model group. NETs formation is pivotal in Indomethacin-induced gastric injury, contributing to programmed cell death of GECs and inflammation; IL-17 signaling might be the key intracellular mechanism of NETs formation.
Similar content being viewed by others
Introduction
Neutrophils, the most abundant immune cells in human circulation1, play crucial roles in various biological processes, including inflammation, immune responses, and tissue injury. They are also the earliest immune cells recruited to sites of inflammation or injury2. Exaggerated inflammatory response is the main cause of gastrointestinal (GI) tract injury3. Tumor necrosis factor (TNF-α) and interleukin-1β (IL-1β) were highly involved in the damage of gastric mucosa, driving inflammatory responses and neutrophils adhesion and was regarded a recognized marker for gastric injury4. Importantly, neutrophils play an important role in gastric mucosal injury: when the gastric tissue is stimulated, the activation of neutrophils will lead to increased protease and ROS levels, amplifying the inflammatory responses and ultimately damaging the gastric mucosa5. Also, activated neutrophils were observed in the gastric tissue of animal models of gastric ulcers, with significantly increased levels of myeloperoxidase (MPO), leading to elevated levels of TNF-α, IL-1β, and other inflammatory factors6. Those evidence suggested a key role for neutrophils in gastric injury.
Historically, phagocytosis and degranulation were considered the primary mechanisms of neutrophil activation7. However, with advancements in research, the diversity and plasticity of neutrophils have gained recognition. Neutrophil extracellular traps (NETs), which are reticular structures composed of DNA, histones, neutrophil elastase (NE), and myeloperoxidase (MPO), represent a recently discovered form of neutrophil activation8. Initially, NETs were thought to play a purely positive role in regulating innate immunity9. Increasing evidence has indicated that NETs can act as double-edged swords: excessive NETs formation is a major mechanism contributing to inflammatory diseases10 and tissue injury11, especially in the GI tract: it is reported that NETs formation aggravated intestinal epithelial necroptosis, causing intestinal barrier damage12,13. Also, Histones of NETs were proved to directly disrupt the integrity of the intestinal barrier14. NETs-related signature was regarded as a robust model for predicting immunotherapy response in gastric cancer15. Regretfully, the number of studies focusing on gastric injury is limited.
Gastric epithelial cells (GECs), a primary component of the gastric mucosa, protect against harmful substances and noxious stimuli11. Programmed cell death, including apoptosis, pyroptosis, and necrosis, is vital for GECs renewal and the maintenance of gastric mucosal homeostasis16. Abnormal programmed cell death in GECs can lead to gastric mucosal damage17. Studies have shown that NETs formation is linked to tubular epithelial cell necrosis18 and inhibiting NETs formation can mitigate neuronal apoptosis in mice19. Additionally, increased NETs formation has been associated with apoptosis in autoimmune-mediated diffuse alveolar hemorrhage20. More importantly, NETs formation aggravated intestinal epithelial cell necroptosis in ischemia–reperfusion by regulating mitophagy21. These findings underscore the significance of NETs in epithelial cell death; however, limited evidence exists concerning the GI tract.
Interleukin-17 (IL-17), a pro-inflammatory cytokine, is essential for the immune defense of mammals against bacterial and fungal pathogens. Research has shown that the IL-17 signaling pathway is very important in the gastric injury process22, it is worth mentioning the strong connection between IL-17 and the formation of NETs: IL-17 increased neutrophil infiltration and was regarded as a potent promoter of NETs formation23,24,25. The underlying connections between IL-17 signaling pathway and NETs formation in Indomethacin-induced gastric injury still remains unknown.
To explore the role of NETs in gastric injury and the intracellular mechanism of NETs formation, we established a gastric ulcer model using Indomethacin, a widely used non-steroidal anti-inflammatory drugs (NSAIDs)26. Gastric injury is one of the most significant side effects of Indomethacin27, which functions by inhibiting cyclooxygenase-1 (COX-1), cyclooxygenase-2 (COX-2), and prostaglandin E2 (PGE2), compromising the protective function of the gastric mucosa and leading to injury28. Misuse of Indomethacin is the second leading cause of gastric ulcers after Helicobacter pylori infection29.
In this study, using an Indomethacin-induced gastric ulcer mouse model, cell culture and single-cell RNA-sequencing (scRNA-seq), we demonstrated that indomethacin triggers NETs formation, further drives programmed cell death of GECs, causing gastric injury, IL-17 signaling pathway might play a key role in this process. Our findings suggest that NETs are heavily involved in programmed cell death of GECs, contributing to Indomethacin induced gastric mucosal injury. This indicates that targeting NETs may offer a promising approach for adjunctive therapy in the future.
Results
Indomethacin caused gastric mucosal injury in mice
As shown in Fig. 1a and b, after Indomethacin gavage, compared to the control group, a significant damage, degeneration and necrosis of mucosa, lymphocyte and neutrophil were observed in the gastric mucosa of mice in the model group. Also, Fig. 1c and d displayed the levels of TNF-α (P < 0.01) and IL-1β (P < 0.01) were significantly increased. These data suggested that 30 mg/Kg of Indomethacin gavage caused significant gastric mucosal damage and inflammation.
Observation of IIndomethacin-induced gastric injury. (a): Gastric injury in each group; (b): TNF-α concentration in each group, bar: mean ± SE, n = 6, vs control group, **P < 0.01; (c): Pathology observation (× 400, scale bar = 50 µm),  : degeneration and necrosis of mucosa,
: degeneration and necrosis of mucosa,  : lymphocyte,
: lymphocyte,  : neutrophil; (d): IL-1β concentration in each group, bar: mean ± SE, n = 6, vs control group, **P < 0.01.
: neutrophil; (d): IL-1β concentration in each group, bar: mean ± SE, n = 6, vs control group, **P < 0.01.
Quality control and differential proteins screening of proteomics
Figure 2a and b displayed the results of quality control of proteomics. Proteomic analysis indicated that most peptides were 7–20 amino acids in length, which met the mass spectrum fragmentation standards. Figure 2c displayed fraction of peptides with zero, one and two missed cleavages. The more fraction of peptides with zero, the more favorable the identification. The percentage of fraction of peptides with zero was 76.06%, suggesting the results of quality control are satisfactory. As shown in Fig. 2d and e, heatmap and Volcano plot revealing differential proteins between two groups. We identified 346 upregulated (red colored dots) and 203 downregulated (green colored dots) proteins from control versus model comparisons.
Quality control and differential proteins screening. (a): Peptide number distribution; (b): Peptide length distribution; (c): Fraction of peptides with zero, one and two missed cleavages. (d): Heatmap of differential proteins between control group and model group; (e): Volcano Plot of differential proteins between two groups.
Enrichment analysis revealed the important role of NETs in Indomethacin induced gastric injury
Figure 3 exhibited the enrichment analysis results of proteomics. GO classification enrichment revealed that differential proteins were primarily upregulated in the item of immune system process (Fig. 3a). According to the analysis of GO enrichment, the proteins expressed differentially are mainly enriched in molecular functions such as inflammatory response and innate immune response. With regard to cell components, they are primarily enriched in the item of extracellular region (Fig. 3b). KEGG30,31,32 enrichment revealed that differential proteins are mainly enriched in the item of neutrophil extracellular trap formation (Fig. 3c). According to Subcellular localization annotation, a significant upregulation can be observed in the item of extracell (Fig. 3d). These enrichment analysis results indicated that immune response, especially NETs, might serve as an important role in this process. ELISA was further applied to confirm our findings: compared to control group, MPO-DNA concentration was significantly increased in the gastric tissues of model group (P < 0.05), suggesting increased NETs formation (Fig. 3e).
Observation of NETs using immunofluorescent double labeling
To better observe NETs, immunofluorescent double labeling was further performed. As shown in Fig. 4a, in the gastric mucosal layer, percentages of citrullinated histone H3 (H3Cit) and MPO positive area were significantly higher in model group compared to control group (P < 0.01) (Fig. 4b and c). Also, co-expression of H3Cit and MPO of model group was significantly increased (P < 0.05) (Fig. 4d). Figure 4e displayed expressions and locations of MPO and H3Cit in the submucosal layer. Compared to control group, percentages of H3Cit and MPO positive area were significantly higher in model group (P < 0.05) in the submucosal layer (Fig. 4f and g). However, co-expression of H3Cit and MPO showed no significant difference (P > 0.05) (Fig. 4h).
Observation of NETs in gastric mucosal and submucosal layers. )a): NETs marker expressions in the mucosal layer (× 40, scale bar = 20 µm), red indicates H3Cit, green indicates MPO, and blue indicates DAPI-stained nucleus; (b): Proportions with positive expression of H3Cit in the mucosal layer, bar: mean ± SE, n = 3; (c): Proportions with positive expression of MPO, bar: mean ± SE, n = 3; (d): Proportions with co-expression of MPO and H3Cit in the mucosal layer, bar: mean ± SE, n = 3. vs control group, **P < 0.01, *P < 0.05. (e): NETs marker expressions in the submucosal layer (× 40, scale bar = 20 µm), red indicates H3Cit, green indicates MPO, and blue indicates DAPI-stained nucleus; (f): Proportions with positive expression of H3Cit in the submucosal layer, bar: mean ± SE, n = 3; (g): Proportions with positive expression of MPO, bar: mean ± SE, n = 3; (h): Proportions with co-expression of MPO and H3Cit in the submucosal layer, bar: mean ± SE, n = 3. vs control group, *P < 0.05, **P < 0.01.
Indomethacin drove NETs formation in vitro
As Fig. 5a illustrated, the viability of neutrophils was checked by trypan blue staining, the isolated neutrophils were 94.74% viable. Figure 5b and c exhibited the expressions of CD11b and ly6G. Those results suggested that neutrophils were successfully extracted. As Fig. 5d shown, after added with 200µL, 400µL and 600µL Indomethacin, MPO-DNA concentration was significantly increased compared to NEU group. This further illustrated that Indomethacin caused excessive NETs. A dose of 400µL was also applied for further in vitro experiment. Figure 5e–h further showed NETs formation in each group: compared to NEU and NEU + GEC group, fluorescence intensity of MPO, H3Cit and co-expression of MPO and H3Cit were significantly higher in NEU + GEC + Indo group, these data further supported that Indomethacin drove NETs formation in vitro.
Observation of NETs formation in vitro. (a): Trypan blue staining of isolated neutrophils; (b) and (c): Expressions of CD11b and ly6G; (d): MPO-DNA concentration after adding different dosage of Indomethacin. bar: mean ± SE, n = 3; vs control group, **P < 0.01; (e): NETs marker expressions in vitro (× 60, scale bar = 20 µm), red indicates H3Cit, green indicates MPO, and blue indicates DAPI-stained nucleus; (f): Fluorescence intensity of H3Cit in vitro, bar: mean ± SE, n = 3; (g): Fluorescence intensity of MPO, bar: mean ± SE, n = 3; (h): Fluorescence intensity of co-expression of MPO and H3Cit, bar: mean ± SE, n = 3. vs control group, **P < 0.01, *P < 0.05, vs model group, ##P < 0.01.
Programed cell death of GECs was observed in mice with gastric injury
Figure 6a revealed that significant mitochondrial swelling and perforation of cell membranes were observed in model group whereas control group exhibited normal mitochondrion, suggesting programmed cell death of GECs was observed after Indomethacin gavage. The relative expressions of Apaf 1 (P < 0.01) and Caspase-1 (P < 0.05) mRNA (Fig. 6b), Gasdermin D and Cyto C proteins (P < 0.01) (Fig. 6c), Gasdermin D and Cyto C mRNA (P < 0.01 and P < 0.05) (Fig. 6d) were considerably elevated in the model group compared to the control group. These indexes indicated that after Indomethacin gavage, significant programmed cell death of GECs was observed.
Observation of programmed cell death of GECs. (a): Observation of ultrastructure of GECs (×30,000, scale bar = 500 nm), N: nucleus, Mi: mitochondrion, RER: rough endoplasmic reticulum;  : normal mitochondrion,
: normal mitochondrion,  : expanded rough endoplasmic reticulum,
: expanded rough endoplasmic reticulum,  : mitochondrial swelling,
: mitochondrial swelling,  : perforation of cell membranes; (b): Relative expressions of Apaf-1 and Caspase-1 mRNA. bar: mean ± SE, n = 4; (c): Relative expressions of Gasdermin D and Cyto C proteins. bar: mean ± SE, n = 4; (d): Relative expressions of Gasdermin D and Cyto C mRNA. bar: mean ± SE, n = 4; vs control group, **P < 0.01, *P < 0.05.
: perforation of cell membranes; (b): Relative expressions of Apaf-1 and Caspase-1 mRNA. bar: mean ± SE, n = 4; (c): Relative expressions of Gasdermin D and Cyto C proteins. bar: mean ± SE, n = 4; (d): Relative expressions of Gasdermin D and Cyto C mRNA. bar: mean ± SE, n = 4; vs control group, **P < 0.01, *P < 0.05.
Inhibition of NETs alleviated Indomethacin-induced gastric injury in mice
To further validate the role of NETs in Indomethacin-induced gastric injury, NETs inhibitor was utilized. DNase 1, which digests the DNA backbone of NETs, has been reported to significantly inhibit NETs formation and aid in tissue repair33. As shown in Fig. 7a and b, compared to the control group, model group showed significant damage in gastric mucosa whereas that of the model + Dnase1 group exhibited no significant change. Figure 7c displayed ultrastructure of GECs in each group: normal mitochondrion was observed in control group and model + DNase 1 group, model group exhibited expanded rough endoplasmic reticulum, mitochondrial swelling, fading of the cell membranes and loss of ribosomes, indicating the programmed cell death of GECs. Figure 7d–h illustrated that compared to control group, the levels of ROS, MPO-DNA, H3Cit, TNF-α and IL-1β significantly increased in model group, whereas ROS, MPO-DNA, H3Cit and TNF-α of the model + DNase1 group exhibited no significant change (P > 0.05). In contrast to the model group, there was a notable decrease in the levels of these indexes in model + DNase 1 group. In this part, the important role of NETs was further validated.
Observation of gastric injury after NETs inhibition. (a): Gastric injury in each group; (b): Pathology observation (× 400, scale bar = 50 µm, green arrow: shed epithelial cells,  : lymphocyte,
: lymphocyte,  : degeneration and necrosis of mucosa; (c): Observation of ultrastructure of GECs under TEM (× 30,000, scale bar = 500 nm), N: nucleus, Mi: mitochondrion, RER: rough endoplasmic reticulum, MV: microvilli;
: degeneration and necrosis of mucosa; (c): Observation of ultrastructure of GECs under TEM (× 30,000, scale bar = 500 nm), N: nucleus, Mi: mitochondrion, RER: rough endoplasmic reticulum, MV: microvilli;  : normal mitochondrion,
: normal mitochondrion,  : expanded rough endoplasmic reticulum,
: expanded rough endoplasmic reticulum,  : mitochondrial swelling,
: mitochondrial swelling,  : fading of the cell membranes,
: fading of the cell membranes,  : permeabilization of mitochondrial outer membrane,
: permeabilization of mitochondrial outer membrane,  : loss of ribosomes. (d): ROS contents in each group, bar: mean ± SE, n = 3; (e): MPO-DNA concentration in each group, bar: mean ± SE, n = 6; (f): H3Cit concentration in each group, bar: mean ± SE, n = 4; (g): TNF-α concentration in each group, bar: mean ± SE, n = 6; (h): IL-1β concentration in each group, bar: mean ± SE, n = 6; vs control group, **P < 0.01, *P < 0.05; vs model group, ##P < 0.01, #P < 0.05.
: loss of ribosomes. (d): ROS contents in each group, bar: mean ± SE, n = 3; (e): MPO-DNA concentration in each group, bar: mean ± SE, n = 6; (f): H3Cit concentration in each group, bar: mean ± SE, n = 4; (g): TNF-α concentration in each group, bar: mean ± SE, n = 6; (h): IL-1β concentration in each group, bar: mean ± SE, n = 6; vs control group, **P < 0.01, *P < 0.05; vs model group, ##P < 0.01, #P < 0.05.
NETs formation driven by Indomethacin caused programed cell death of GECs in vitro
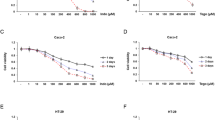
To demonstrate the relations between NETs formation and programmed cell death of GECs, we further validate our findings in vitro. As shown in Fig. 8, compared to NEU group, relative expressions of Apaf 1 and Cyto C proteins (P < 0.01) (Fig. 8a), MPO-DNA concentration (P < 0.01) (Fig. 8b), ROS level (P < 0.01) (Fig. 8c) and cell apoptosis level (P < 0.01) (Fig. 8d and e) were significantly increased in NEU + GEC group and NEU + GEC + Indo group. In contrast to Neu + GEC group, those indexes were significantly increased in Neu + GEC + Indo group (P < 0.01). At this stage, we further observed evidence for a key negative role of the NETs in the programmed cell death of GECs.
Observation of programmed cell death of GECs in vitro. (a): Relative expressions of Apaf-1 and Cyto C proteins. bar: mean ± SE, n = 3; (b): MPO-DNA concentration. bar: mean ± SE, n = 3; (c): ROS levels. bar: mean ± SE, n = 3; (d): Cell apoptosis level. bar: mean ± SE, n = 3; (e): Cell apoptosis observation; vs NEU group, **P < 0.01, vs NEU + GEC group, ##P < 0.01.
scRNA-Seq revealed neutrophils enrichment in the peripheral blood of Indomethacin-induced gastric injury
Figure 9a illustrated number of DEGs of different immune cells, a total of 356 upregulated and 736 downregulated DEGs were identified in neutrophils. Figure 9b displayed the heatmap of different immune cell types in each sample, notably, compared to control group, neutrophils activation was accompanied in model group. By combining the dataset from control and model groups, we were able to identify 24 distinct cell clusters including neutrophils, B cells, T cells, NK cells and Erythroblasts (Fig. 9c,d and e). Figure 9f and g showed expression levels of markers of different immune cell types. To further explore the immunological mechanism of Indomethacin-induced gastric injury, the particular gene expression pattern of immune cell populations was analyzed (Fig. 9h). The results suggested that well-recognized markers for neutrophils, including Csf3r, Cxcr2, S100a8 and G0s2, were primarily expressed. Those results indicated that neutrophils enrichment in the peripheral blood of Indomethacin-induced gastric injury.
Neutrophils were enriched in the peripheral blood of gastric injury mice. (a): Differential statistics of immune cell types; (b): Heat map of immune cell types in each sample; (c): tSNE identifies 24 cell clusters in the peripheral blood of control and mice; (d): tSNE visualization of the cell types identified in the peripheral blood of control (n = 3) and model (n = 3) groups; (e): tSNE visualization of the cell types identified in each sample. (f): Violin plots of the expression levels of different markers of immune cell types; (g): Stack violin plots of the expression levels of markers of different cell types; (h): Expressions of the top two key genes in different immune cell populations.
IL-17 signaling might be the key intracellular mechanism of NETs formation
Figure 10a–f displayed enrichment analysis of differentially expressed genes in neutrophils isolated from the peripheral blood of control and model groups. According to the Reactome enrichment, the genes that are expressed differentially are mainly enriched in neutrophil degranulation, innate immune system and immune system. (Fig. 10c and d, red square). KEGG enrichment analysis revealed that differential expressed genes are enriched in the item of IL-17 signaling pathway (Fig. 10e and f, red square). To observe the expression of neutrophil IL-17 signaling pathway in the gastric mucosa, immunofluorescence double labeling was applied. Compared to control group, percentages of mucosal MPO and IL-17R positive areas and co-expressions of mucosal MPO and IL-17R were significantly increased in model group (P < 0.01) (Fig. 10g,h,i and j). Besides, concentration of IL-17 in the gastric tissue was significant higher in the model groups (P < 0.05) (Fig. 10k). These data preliminarily support the over expression of neutrophil IL-17 signaling pathway in the Indomethacin-induced gastric injury and NETs formation.
Importance of IL-17 signaling in Indomethacin-induced gastric injury. (a): GO enrichment analysis on the differentially expressed genes of neutrophils in control group and model group; (b): Bubble plot of GO enrichment; (c): Bar plot of Reactome enrichment; (d): Bubble plot of Reactome enrichment; (e): Bar plot of KEGG enrichment; (f): Bubble plot of KEGG enrichment; (g): Neutrophil IL-17 signaling expressions in the mucosal layer (×40, scale bar = 20 µm), red indicates IL-17R, green indicates MPO, and blue indicates DAPI-stained nucleus; (h): Proportions with positive expression of MPO in the mucosal layer, bar: mean ± SE, n = 4; (i): Proportions with positive expression of IL-17R, bar: mean ± SE, n = 4; (j): Proportions with co-expression of MPO and IL-17R in the mucosal layer, bar: mean ± SE, n = 4; (k): IL-17 concentration, bar: mean ± SE, n = 4, vs control group, **P < 0.01, *P < 0.05.
Discussion
In this study, we confirmed that NETs formation played a crucial role in Indomethacin-induced gastric injury, demonstrated through both in vivo and in vitro experiments. NETs formation contributed to the programmed cell death of GECs, offering new insights into the role of NETs in gastrointestinal diseases. Additionally, IL-17 signaling pathway might be the key intracellular mechanism of NETs formation (Fig. 11).
Schematic illustration of the entire study. (a): Hypothesis of this study; (b): Flow diagram of the study procedure. GEC: gastric epithelial cell; ROS: reactive oxygen species; NETs: neutrophil extracellular traps; MPO: myeloperoxidase; H3Cit: citrullinated histone H3. This figure was drawn with Figdraw (www.figdraw.com).
Indomethacin is a widely used NSAIDs, but is also known for causing significant gastric injury34. NSAIDs are reported to interact chemically with cell membrane phospholipids, damage membrane permeability, and form membrane pores, inducing gastric cell death35. Also, it is reported that Indomethacin gavage increased concentrations of inflammatory factors including TNF-α and IL-1β, which are also regarded as well-recognized biomarkers of gastric injury36,37. Previous research has shown that a 30 mg/Kg dose of Indomethacin can cause marked gastric damage in mice38. Consistent with these findings, our study observed substantial gastric injury and elevated levels of TNF-α and IL-1β in the model group, confirming the successful establishment of a gastric injury model.
To further investigate the mechanisms behind Indomethacin-induced gastric injury, we conducted proteomic analysis. GO, KEGG, and subcellular enrichment analyses revealed that the differential proteins were significantly enriched in pathways related to immune system processes, inflammatory responses, innate immune responses, extracellular regions, and NETs formation. These findings strongly suggested that neutrophil activation, especially NETs formation is a key mechanism contributing to Indomethacin-induced gastric injury.
Neutrophils are primary responders in the innate immune system, playing an essential role in inflammatory responses and tissue injury39. Their infiltration is considered critical in the pathogenesis of NSAIDs-induced gastric ulcers40. NETs formation, another discovered form of neutrophil activation41, has been increasingly implicated in gastrointestinal tract injury42. NETs consist of DNA adorned with histones, its formation depended on ROS produced by NADPH oxidase43,44. Studies have reported that NETs-associated proteins are overexpressed in patients with ulcerative colitis, supporting the involvement of NETs in sustaining mucosal inflammation in the gastrointestinal tract45.
To assess NETs concentration, we measured MPO-DNA levels. Following Indomethacin administration, we observed increased gastric MPO-DNA concentrations, indicating excessive NETs formation.
It is reported that significant neutrophil accumulation was observed DSS-induced ulcerative colitis mice model, causing mucosal and submucosal inflammation46, this indicated that neutrophils could activated both in mucosal and submucosal layer in the gastrointestinal tract. Interestingly, neutrophil infiltration was also observed in the gastric tissue of patients with gastric cancer47 and Indomethacin-induced gastric ulcer mice48. To better observe expression and location of NETs, immunofluorescent double labeling was applied. MPO, a major component of neutrophils, is considered as a direct measure of the neutrophil presence49. H3Cit is regarded as a biomarker for NETs and was proved to cause endothelial barrier dysfunction and tissue injury50. In this study, mucosal co-expression of MPO and H3Cit was significantly higher after Indomethacin gavage, these findings consistent with previous studies and further suggested that mucosal activated neutrophils released extracellular trap structures and caused gastric tissue injury.
To better validate this in vitro, neutrophils were isolated from mice and treated with various concentrations of Indomethacin (100 µL, 200 µL, 400 µL, and 600 µL). Neutrophils added with Indomethacin (200 µL, 400 µL, and 600 µL) showed significantly elevated MPO-DNA levels. These results indicate that Indomethacin effectively induces NETs formation. To further support this, a co-culture system of isolated neutrophils and GECs was established. First, neutrophils were extracted from peripheral blood of mice and were cultured with GECs cell line, Indomethacin was further added. It is found that after addition of Indomethacin, NETs formation was significantly higher in neutrophils compared to neutrophils alone and co-culture of neutrophils and GECs. This further suggested that excessive NETs formation was driven by Indomethacin.
Using DNase 1 to break down the backbone of NETs is a well-known therapeutic intervention for NETs formation, previous studies have demonstrated that through the clearance of NETs, DNase 1 enhanced inflammation resolution, reduced the buildup of reactive oxygen species (ROS), restored the tissue integrity and improve symptoms in diabetic51, brain hemorrhage52, acute respiratory distress syndrome53 and aging54 mice. In our study, DNase 1 administration markedly alleviated gastric injury, reduced inflammatory factor levels, repaired gastric epithelial damage, reduced ROS and MPO-DNA levels, suggesting that inhibition of NETs resulted in significant reduction in gastric injury. These observations align with previous studies and further confirm the detrimental impact of NETs formation on gastric mucosal homeostasis.
With the deepening of research, increasing researches begin to focus on the relations between NETs formation and epithelial cells homeostasis55. Programmed cell death, including necrosis, apoptosis, and pyroptosis, is critical for maintaining gastrointestinal mucosal integrity56. However, excessive programmed cell death may exacerbate tissue damage57. Prior research has documented apoptosis58 and pyroptosis59 of gastric epithelial cells in various gastric injury conditions. More importantly, NSAIDs have been reported to induce apoptosis in gastric mucous cells60. In the present study, apoptosis-related proteins Cytochrome C (Cyto C) and Apoptotic Protease-Activating Factor 1 (Apaf-1)61, along with pyroptosis-related proteins Caspase-1 and Gasdermin D62, were examined. Our data revealed that the expression levels of Apaf-1, Cyto C, Caspase-1, and Gasdermin D were significantly elevated in the gastric tissue of the model group compared to the control group, suggesting Indomethacin caused excessive programmed cell death of GECs.
To explore the relationship between NETs formation and gastric injury, programmed cell death of GECs was further observed in vitro. Compared to the GEC group and the NEU + GEC group, the NEU + GEC + Indomethacin (Indo) group exhibited increased programmed cell death of GECs. This evidence supports the hypothesis that heightened NETs formation contributes to programmed cell death of GECs, which might be a key mechanism underlying Indomethacin-induced gastric injury. Previous research has highlighted the critical interaction between neutrophils and epithelial cells in gastrointestinal mucosal inflammation63. Studies have shown that inhibiting NETs ameliorates neuroinflammation and neuronal apoptosis in mice with traumatic brain injury19. Additionally, it is reported that histones, a main component of NETs, released by neutrophils killed endothelial cells and epithelial cells in a dose-dependent manner64. Those findings indicated that NETs might play as a negative role in the maintenance of epithelial homeostasis. Our results further underscore that NETs formation promoted programmed cell death of GECs, leading gastric injury.
To further explore the intracellular of NETs formation, neutrophils were extracted from peripheral blood of mice and scRNA-seq was applied. Compared to control group, neutrophils were significantly activated in model group, this consists with our expectations. Enrichment analysis revealed that IL-17 signaling might play a key role in the Indomethacin-induced NETs formation. Members of the IL-17 cytokine family perform a variety of biological roles including drive inflammatory pathology. It is reported that IL-17 has a tight relation with NETs formation: NETs formation directly enhanced Th17 cell differentiation and IL-17 production65, notably, IL-17 was regarded as a central driver of NETs formation induced tissue injury and prolongation of inflammation23,66. In our study, compared to control group, IL-17 concentration and neutrophil IL-17R expression in the gastric mucosa were significantly higher in the model group, highlighting the significant involvement of the IL-17 signaling pathway in the NETs formation.
Despite these significant insights, this study has some limitations. First, advanced technologies are needed to observe NETs more comprehensively. Moreover, peptidylarginine deiminase 4 (PAD4) is essential for NETs formation; therefore, employing PAD4 gene knockout mice could further strengthen our findings. Then, in vitro experimental design can be further improved: DNase 1 could be further applied in vitro experiment to better clarify the importance of NETs, western blot could be further conducted to measure protein level of Caspase-1 and Apaf-1 to match with their real-time PCR results. Finally, although scRNA-seq revealed the importance of IL-17 signaling and expression of IL-17R and IL-17 were observed in this study, more experiments including inhibition of IL-17R could be applied to validate this finding. These aspects will be addressed in future research.
In summary, excessive NETs formation in the gastric mucosa leads to programmed cell death of GECs, playing a crucial role in Indomethacin-induced gastric mucosal injury. IL-17 signaling pathway might be the key intracellular mechanism of NETs formation. This suggests that targeting NETs could be a promising strategy for future adjunctive therapy for gastric injury.
Methods and materials
Animals
Fifty male C57 mice (aged 8 weeks, weighing 22 ± 2 g) were obtained from Dashuo Biological Technology Company, Chengdu, China. A constant circadian rhythm, humidity, and temperature (18–25 °C) were provided to the mice, along with adequate food and water. The Ethics Committee of Chengdu University of Traditional Chinese Medicine (2024037) approved this study. All experiments were performed in accordance with relevant guidelines and regulations including ARRIVE guidelines.
Indomethacin-induced gastric injury
CMC-Na (Sigma-Aldrich, USA, 419273) was used to dissolve Indomethacin. Sonicated suspensions were administered to mice by gavage at a dose of 30 mg/Kg after sonication29. Mice in control group received the solvent at the same time as the model group.
Injection of DNase1
Deoxyribonuclease (DNase1) was used to inhibit NETs formation. DNase1 (Roche, China, 4716728001) was dissolved in 0.9% NaCl and administered intraperitoneally to mice in the Model + DNase1 group at a dose of 1000 units 30 min before Indomethacin treatment. Control group and model group received the solvent at the same time.
Sample collection
Twenty-four hours after Indomethacin treatment, the mice were euthanized by rapid decapitation. The stomachs were excised, opened along the greater curvature, and washed with cold PBS to remove gastric contents. The gastric tissues were pinned flat with the mucosal side up. After visual inspection and documentation, tissues were placed in ice-colded PBS, 4% paraformaldehyde, fixation liquid, or liquid nitrogen for further analysis.
H&E staining and immunofluorescence
Sample sections were dewaxed, rehydrated, and subjected to hematoxylin (Sigma-Aldrich, Germany, H9627) and eosin (BIOBIOMEI, China, YE2080) staining. The sections were dehydrated and observed under conventional microscopes. For immunofluorescence detection, sections were blocked with BSA (Servicebio, China, GC305010) to inhibit endogenous peroxidase. Primary antibodies (MPO: ZENBIO, China, R25062, 1:100; H3Cit: Proteintech, China, 68345-1-Ig, 1:200) and secondary antibodies (FITC goat anti-rabbit: Servicebio, China, GB22303, 1:100; CY3 goat anti-rabbit: Servicebio, China, GB21301, 1:200) were applied. Finally, sections were stained with DAPI and observed using a camera system (OLYMPUS, Japan, VS200).
Enzyme-linked immunosorbent assay (ELISA)
ELISA was used to measure the levels of MPO-DNA, TNF-α, and IL-1β. Tissue homogenates were prepared, and ELISA was performed using the respective kits (IL-1β ELISA KIT, ZC-37974; MPO-DNA ELISA KIT, ZC-56424; TNF-α ELISA KIT, ZC-39024; ZCIBIO, China).
Real-time polymerase chain reaction (Real-time PCR)
Real-time PCR was performed to measure the relative expressions of Cyto C, Apaf 1, Gasdermin D, and Caspase-1 mRNA. Total RNA was extracted and used to synthesize cDNA. Primer sequences are listed in Table 1 (Shanghai SANGON Biotech, China). PCR reactions were conducted using a real-time fluorescence quantitative instrument (QuantStudio™ Design & Analysis SE Software, Thermo Fisher, USA) over 45 cycles. Relative mRNA levels were calculated using the 2−ΔΔCT method.
Transmission electron microscopy (TEM)
TEM was used to observe the ultrastructure of GECs. Samples were fixed, dehydrated, embedded, and initially examined by light microscopy to locate the GECs area. They were then observed under an electron microscope (JEOL, Japan, JEM-1400FLASH) after staining with uranyl acetate and lead citrate.
Flow cytometry
Flow cytometry was performed to measure levels of ROS in the gastric tissue. After grinding, filtration, and centrifugation, the precipitated cells were collected. A 10 µmol/L solution of DCFH-DA was prepared and introduced into each well. Rosup dilution served as the positive control, and data analysis was conducted using CytExpert software. ROS levels were quantified by the mean fluorescent intensity of FITC.
Proteomics
Proteomic analysis was performed on gastric tissue from control and model groups (n = 8) to investigate key mechanisms underlying Indomethacin-induced gastric injury.
Sample processing
Extracted proteins were quantified using a BCA kit (Beyotime, China). Peptides were desalted before further analysis.
LC–MS/MS detection
Samples were separated using a NanoElute UHPLC system with nanoliter flow rates and analyzed using a timsTOF Pro mass spectrometer (Bruker, Germany) in PASEF mode for diaPASEF acquisition.
Mass spectrometry data analysis
Data were processed using DIA-NN software (v1.8.1) and the Uniprot-proteome_UP000000589_Mus_musculus.fasta database. A total of 55,319 high-quality reads were obtained and filtered for further analysis.
Protein quantification
Relative protein quantification was conducted using the MaxLFQ algorithm. T-tests were performed for each protein in the control and model groups, with corresponding P values calculated.
Bioinformatic analysis
Functional annotation of proteins was carried out using GO, KEGG, and subcellular localization databases.
In vitro experiment
Neutrophils and cultured GECs (iCell, MIC-iCell-d004) were co-cultured using a transwell system. Cells were divided into three groups: Neu, Neu + GEC, and Neu + GEC + Indo, with three replicates per group. Supernatants were collected after 12 h of incubation and stored.
Cell culture
Cells were resuscitated, passaged, and counted under a microscope. Cell suspensions were frozen and stored at − 80 °C.
Isolation and identification of neutrophils
Mouse peripheral blood was collected, and neutrophils were isolated using a magnetic separation system (MS MACS columns and MACS Separator) following the addition of Neutrophil Biotin-Antibody (Miltenyi Biotec, 130-097-658). Neutrophils were identified with CD11b (Biolegend, 101205) and Ly-6G (Biolegend, 101613) antibodies.
Detection of ROS
Extracted neutrophils and GECs were seeded in the lower chamber of Transwell plates. After the cells adhered to the wall, they were grouped as NEU, NEU + GEC and NEU + GEC + Indo groups. Indomethacin was added in the upper chamber. Neutrophils were collected. DCFH-DA and Rosup dilutions were added to cell suspensions. After discarding the supernatant, cells were resuspended in PBS, and ROS levels were measured.
Cell apoptosis assay
Extracted neutrophils and GECs were seeded in the lower chamber of Transwell plates. After the cells adhered to the wall, they were grouped as GEC, NEU + GEC and NEU + GEC + Indo groups. Indomethacin was added. GECs were collected 12 h later, the cells were resuspended with 500 µL binding buffer after centrifugation. 5 µL Annexin V and 5 µL PI were added separately, the cells for 15 min at room temperature avoiding the light until the analysis.
Detection of NETs
ELISA was used to quantify MPO-DNA as described previously.
Observation of the programmed cell death of GECs
TEM, western blot, and Real Time-PCR were performed to assess the expressions of Apaf 1, Cyto C, Gasdermin D, and Caspase-1, following established methods.
Single-cell RNA-sequencing (scRNA-Seq)
Single-cell RNA-sequencing (scRNA-Seq) was performed on neutrophils extracted from peripheral blood from control and model groups (n = 3) to investigate the intracellular mechanisms of NETs formation.
Sample processing
Poly morphonuclear neutrophils were extracted from peripheral blood of mice. Single-cell suspensions were obtained after density gradient centrifugation. Live cell rate was calculated twice and averaged.
10× library preparation and sequencing
Immediately following GEM generation, the cell was lysed, the RNA was extracted and cDNA was generated, each cDNA molecule was tagged on the 5′ end with UMI and cell label indicating its cell of origin. Briefly, 10× beads that were then subject to second-strand cDNA synthesis, adaptor ligation, and universal amplification. Sequencing libraries were prepared using randomly interrupted whole-transcriptome amplification products to enrich the 3’ end of the transcripts linked with the cell barcode and UMI. All the remaining procedures including the library construction were performed according to the standard manufacturer’s protocol (Chromium Single Cell 3ʹ v3.1). Sequencing libraries were quantified using a High Sensitivity DNA Chip (Agilent) on a Bioanalyzer 2100 and the Qubit High Sensitivity DNA Assay (Thermo Fisher Scientific). The sequencing and bioinformatic analysis were performed on platform of Majorbio Co., Ltd (Shanghai, China).
Single cell RNA-seq data processing
Reads were processed using the Cell Ranger (v7.1.0) pipeline with default and recommended parameters. FASTQs generated from Illumina sequencing output were aligned to the mouse genome, version GRCm38, using the STAR algorithm. Next, Gene-Barcode matrices were generated for each individual sample by counting UMIs and filtering non-cell associated barcodes. Finally, we generate a gene-barcode matrix containing the barcoded cells and gene expression counts. This output was then imported into the Seurat (v4.1.1) R toolkit for quality control and downstream analysis of our single cell RNAseq data. All functions were run with default parameters, unless specified otherwise. We first filtered the matrices to exclude low-quality cells using a standard panel of three quality criteria: number of detected transcripts (number of unique molecular identifiers); detected genes and percent of reads mapping to mitochondrial genes. The expression of mitochondria genes was calculated using Percentage Feature Set function of the seurat package. The normalized data (Normalize Data function in Seurat package) was performed for extracting a subset of variable genes. Variable genes were identified while controlling for the strong relationship between variability and average expression. Next, we integrated data from different samples after identifying ‘anchors’ between datasets using Find Integration Anchors and Integrate Data in the seurat package. We visualized the clusters on a 2D map produced with t-distributed stochastic neighbor embedding (t-SNE).
Identification of cell types and subtypes by nonlinear dimensional reduction (t-SNE)
Cells were clustered using graph-based clustering of the PCA reduced data with the Louvain Method after computing a shared nearest neighbor graph. For each cluster, we used the Wilcoxon Rank-Sum Test to find significant deferentially expressed genes comparing the remaining clusters. SingleR and known marker genes were used to identify cell type.
Differential expression analysis and functional enrichment
To identify DEGs (differential expression genes) between two different samples or clusters, was performed using the function FindMarkers in Seurat, using a likelihood ratio test. Essentially, DEGs with |log2FC|> 0.25 and Q value ≤ 0.05 were considered to be significantly different expressed genes. In addition, GO, KEGG and Reactome enrichment analysis were performed.
Statistical analysis
Data were analyzed using SPSS 26. Comparisons between groups were made using two-tailed t-tests or one-way ANOVA. A P value < 0.05 was considered statistically significant. Statistical graphs were generated using GraphPad Prism software (v8.0.2), and data are expressed as mean ± SE.
Data availability
The mass spectrometry proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE partner repository with the dataset identifier PXD058482. The raw Single cell RNA-seq data reported in this paper has been deposited in the Genome Sequence Archive in National Genomics Data Center, China National Center for Bioinformation/Beijing Institute of Genomics, Chinese Academy of Sciences (GSA: CRA020950) that are publicly accessible at https://ngdc.cncb.ac.cn/gsa.
References
Borregaard, N. Neutrophils, from marrow to microbes. Immunity 33, 657–670. https://doi.org/10.1016/j.immuni.2010.11.011 (2010).
Chen, J. et al. CREB1-driven CXCR4(hi) neutrophils promote skin inflammation in mouse models and human patients. Nat. Commun. 14, 5894. https://doi.org/10.1038/s41467-023-41484-3 (2023).
Zhang, P., Mao, R., Zhang, C., Qiu, Y. & Chen, M. Gastrointestinal injury induced by immunomodulators: A review article. Ther. Adv. Gastroenterol. 16, 17562848231158548. https://doi.org/10.1177/17562848231158549 (2023).
Zhang, X. et al. Gastroprotective effect of the Lachnum polysaccharide and polysaccharide-dipeptide conjugates against gastric ulcer. Food Chem. Toxicol.: Int. J. Publ. Br. Indust. Biol. Res. Assoc. 174, 113661. https://doi.org/10.1016/j.fct.2023.113661 (2023).
Yoshikawa, T. & Naito, Y. The role of neutrophils and inflammation in gastric mucosal injury. Free Radical Res. 33, 785–794. https://doi.org/10.1080/10715760000301301 (2000).
Boeing, T. et al. Antiulcer mechanisms of Vernonia condensata Baker: A medicinal plant used in the treatment of gastritis and gastric ulcer. J. Ethnopharmacol. 184, 196–207. https://doi.org/10.1016/j.jep.2016.02.049 (2016).
Zhang, M., Li, S., Ying, J. & Qu, Y. Neutrophils: a key component in ECMO-related acute organ injury. Front. Immunol. 15, 1432018. https://doi.org/10.3389/fimmu.2024.1432018 (2024).
Knackstedt, S. L. et al. Neutrophil extracellular traps drive inflammatory pathogenesis in malaria. Sci. Immunol. 4, eaaw0336. https://doi.org/10.1126/sciimmunol.aaw0336 (2019).
Kaplan, M. J. & Radic, M. Neutrophil extracellular traps: double-edged swords of innate immunity. J. Immunol. (Baltimore, Md.: 1950) 189, 2689–2695. https://doi.org/10.4049/jimmunol.1201719 (2012).
Castanheira, F. V. S. & Kubes, P. Neutrophils and NETs in modulating acute and chronic inflammation. Blood 133, 2178–2185. https://doi.org/10.1182/blood-2018-11-844530 (2019).
Dömer, D., Walther, T., Möller, S., Behnen, M. & Laskay, T. Neutrophil extracellular traps activate proinflammatory functions of human neutrophils. Front. Immunol. 12, 636954. https://doi.org/10.3389/fimmu.2021.636954 (2021).
Chaaban, H. et al. Neutrophil extracellular trap inhibition increases inflammation, bacteraemia and mortality in murine necrotizing enterocolitis. J. Cell Mol. Med. 25, 10814–10824. https://doi.org/10.1111/jcmm.15338 (2021).
Schroder, A. L. et al. Neutrophil extracellular trap density increases with increasing histopathological severity of Crohn’s disease. Inflamm. Bowel Dis. 28, 586–598. https://doi.org/10.1093/ibd/izab239 (2022).
Lai, H.-J. et al. Histones of neutrophil extracellular traps directly disrupt the permeability and integrity of the intestinal epithelial barrier. Inflamm. Bowel Dis. 29, 783–797. https://doi.org/10.1093/ibd/izac256 (2023).
Sun, N. et al. Neutrophil extracellular trap genes predict immunotherapy response in gastric cancer. Heliyon 10, e37357. https://doi.org/10.1016/j.heliyon.2024.e37357 (2024).
Lee, J., Lim, J. W. & Kim, H. Astaxanthin inhibits oxidative stress-induced Ku protein degradation and apoptosis in gastric epithelial cells. Nutrients 14, 3939. https://doi.org/10.3390/nu14193939 (2022).
Guo, Y. et al. Licorice flavonoid ameliorates ethanol-induced gastric ulcer in rats by suppressing apoptosis via PI3K/AKT signaling pathway. J. Ethnopharmacol. 325, 117739. https://doi.org/10.1016/j.jep.2024.117739 (2024).
Nakazawa, D. et al. Histones and neutrophil extracellular traps enhance tubular necrosis and remote organ injury in ischemic AKI. J. Am. Soc. Nephrol. 28, 1753–1768. https://doi.org/10.1681/asn.2016080925 (2017).
Shi, G. et al. Inhibition of neutrophil extracellular trap formation ameliorates neuroinflammation and neuronal apoptosis via STING-dependent IRE1α/ASK1/JNK signaling pathway in mice with traumatic brain injury. J. Neuroinflamm. 20, 222. https://doi.org/10.1186/s12974-023-02903-w (2023).
Hsieh, Y.-T. et al. Down-regulated miR-146a expression with increased neutrophil extracellular traps and apoptosis formation in autoimmune-mediated diffuse alveolar hemorrhage. J. Biomed. Sci. 29, 62. https://doi.org/10.1186/s12929-022-00849-4 (2022).
Chu, C. et al. Neutrophil extracellular traps aggravate intestinal epithelial necroptosis in ischaemia-reperfusion by regulating TLR4/RIPK3/FUNDC1-required mitophagy. Cell Prolif. 57, e13538. https://doi.org/10.1111/cpr.13538 (2024).
Feng, L. et al. An integrated network analysis, RNA-seq and in vivo validation approaches to explore the protective mechanism of Mongolian medicine formulae Ruda-6 against indomethacin-induced gastric ulcer in rats. Front. Pharmacol. 14, 1181133. https://doi.org/10.3389/fphar.2023.1181133 (2023).
Tohme, S. et al. Computational analysis supports IL-17A as a central driver of neutrophil extracellular trap-mediated injury in liver ischemia reperfusion. J. Immunol. (Baltimore, Md.: 1950) 202, 268–277. https://doi.org/10.4049/jimmunol.1800454 (2019).
Stark, M. A. et al. Phagocytosis of apoptotic neutrophils regulates granulopoiesis via IL-23 and IL-17. Immunity 22, 285–294. https://doi.org/10.1016/j.immuni.2005.01.011 (2005).
Lee, S. K. et al. Phospholipase D2 drives mortality in sepsis by inhibiting neutrophil extracellular trap formation and down-regulating CXCR2. J. Exp. Med. 212, 1381–1390. https://doi.org/10.1084/jem.20141813 (2015).
Villar-Martínez, M. D., Moreno-Ajona, D., Chan, C. & Goadsby, P. J. Indomethacin-responsive headaches-A narrative review. Headache 61, 700–714. https://doi.org/10.1111/head.14111 (2021).
Hamza, S. E., Wahdan, S. A. & El-Demerdash, E. Effect of phylloquinone on indomethacin-induced gastric ulceration in rats: Role of SIRT-1. Clin. Exp. Pharmacol. Physiol. 50, 369–379. https://doi.org/10.1111/1440-1681.13752 (2023).
Lucas, S. The pharmacology of indomethacin. Headache 56, 436–446. https://doi.org/10.1111/head.12769 (2016).
Cho, H.-S. et al. Gintonin alleviates HCl/ethanol- and indomethacin-induced gastric ulcers in mice. Int. J. Mol. Sci. 24, 16721. https://doi.org/10.3390/ijms242316721 (2023).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30. https://doi.org/10.1093/nar/28.1.27 (2000).
Kanehisa, M. Toward understanding the origin and evolution of cellular organisms. Protein Sci.: Publ. Protein Soc. 28, 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–D592. https://doi.org/10.1093/nar/gkac963 (2023).
Wong, S. L. et al. Diabetes primes neutrophils to undergo NETosis, which impairs wound healing. Nat. Med. 21, 815–819. https://doi.org/10.1038/nm.3887 (2015).
Naito, Y. et al. Prevention of indomethacin-induced gastric mucosal injury in Helicobacter pylori-Negative healthy volunteers: A comparison study rebamipide vs famotidine. J. Clin. Biochem. Nutr. 43, 34–40. https://doi.org/10.3164/jcbn.2008041 (2008).
Afroz, S. et al. Lysophosphatidic acid in medicinal herbs enhances prostaglandin E(2) and protects against indomethacin-induced gastric cell damage in vivo and in vitro. Prostaglandins Other Lipid Mediat. 135, 36–44. https://doi.org/10.1016/j.prostaglandins.2018.01.003 (2018).
Harsch, I. A. et al. Impaired gastric ulcer healing in diabetic rats: Role of heat shock protein, growth factors, prostaglandins and proinflammatory cytokines. Eur. J. Pharmacol. 481, 249–260. https://doi.org/10.1016/j.ejphar.2003.09.019 (2003).
Mehmet, N. et al. Serum and gastric fluid levels of cytokines and nitrates in gastric diseases infected with Helicobacter pylori. New Microbiol. 27, 139–148 (2004).
Marques, F. d. C. J. et al. Galactomannan from the seeds of Caesalpinia pulcherrima prevents indomethacin-induced gastrointestinal damage via neutrophil migration. Int. J. Biol. Macromol. 141, 68–75. https://doi.org/10.1016/j.ijbiomac.2019.08.193 (2019).
Mayadas, T. N., Cullere, X. & Lowell, C. A. The multifaceted functions of neutrophils. Annu. Rev. Pathol. 9, 181–218. https://doi.org/10.1146/annurev-pathol-020712-164023 (2014).
Jainu, M. & Devi, C. S. S. Attenuation of neutrophil infiltration and proinflammatory cytokines by Cissus quadrangularis: A possible prevention against gastric ulcerogenesis. J. Herb. Pharmacother. 5, 33–42 (2005).
Brinkmann, V. et al. Neutrophil extracellular traps kill bacteria. Science (New York, N.Y.) 303, 1532–1535. https://doi.org/10.1126/science.1092385 (2004).
Chu, C. et al. Neutrophil extracellular traps drive intestinal microvascular endothelial ferroptosis by impairing Fundc1-dependent mitophagy. Redox Biol. 67, 102906. https://doi.org/10.1016/j.redox.2023.102906 (2023).
Zhu, Y. et al. Zingerone inhibits the neutrophil extracellular trap formation and protects against sepsis via Nrf2-mediated ROS inhibition. Oxid. Med. Cell. Longev. 2022, 3990607. https://doi.org/10.1155/2022/3990607 (2022).
Ravindran, M., Khan, M. A. & Palaniyar, N. Neutrophil extracellular trap formation: Physiology, pathology, and pharmacology. Biomolecules 9, 365. https://doi.org/10.3390/biom9080365 (2019).
Dinallo, V. et al. Neutrophil extracellular traps sustain inflammatory signals in ulcerative colitis. J. Crohns Colitis 13, 772–784. https://doi.org/10.1093/ecco-jcc/jjy215 (2019).
Puppala, E. R. et al. Mesua assamica (King&Prain) kosterm. Bark ethanolic extract attenuates chronic restraint stress aggravated DSS-induced ulcerative colitis in mice via inhibition of NF-κB/STAT3 and activation of HO-1/Nrf2/SIRT1 signaling pathways. J. Ethnopharmacol. 301, 115765. https://doi.org/10.1016/j.jep.2022.115765 (2023).
Sugimoto, T. et al. Neutrophil infiltration and the distribution of intestinal metaplasia is associated with metachronous gastric cancer following endoscopic submucosal dissection. Can. J. Gastroenterol. Hepatol. 29, 321–325. https://doi.org/10.1155/2015/950734 (2015).
Nakajima, A. et al. Attenuation of indomethacin-induced gastric mucosal injury by prophylactic administration of sake yeast-derived thioredoxin. J. Gastroenterol. 47, 978–987. https://doi.org/10.1007/s00535-012-0564-5 (2012).
Rizo-Téllez, S. A., Sekheri, M. & Filep, J. G. Myeloperoxidase: regulation of neutrophil function and target for therapy. Antioxidants (Basel, Switzerland) 11, 2302. https://doi.org/10.3390/antiox11112302 (2022).
Meegan, J. E. et al. Citrullinated histone 3 causes endothelial barrier dysfunction. Biochem. Biophys. Res. Commun. 503, 1498–1502. https://doi.org/10.1016/j.bbrc.2018.07.069 (2018).
Zhang, J. et al. DNase I improves corneal epithelial and nerve regeneration in diabetic mice. J. Cell Mol. Med. 24, 4547–4556. https://doi.org/10.1111/jcmm.15112 (2020).
Wang, R. et al. Neutrophil extracellular traps promote tPA-induced brain hemorrhage via cGAS in mice with stroke. Blood 138, 91–103. https://doi.org/10.1182/blood.2020008913 (2021).
Jarrahi, A. et al. Recombinant human DNase-I improves acute respiratory distress syndrome via neutrophil extracellular trap degradation. J. Thrombosis Haemostasis: JTH 21, 2473–2484. https://doi.org/10.1016/j.jtha.2023.04.044 (2023).
Kumar, R. et al. DNase 1 protects from increased thrombin generation and venous thrombosis during aging: Cross-sectional study in mice and humans. J. Am. Heart Assoc. 11, e021188. https://doi.org/10.1161/jaha.121.021188 (2022).
Hudock, K. M. et al. Neutrophil extracellular traps activate IL-8 and IL-1 expression in human bronchial epithelia. Am. J. Physiol. Lung Cell. Mol. Physiol. 319, L137–L147. https://doi.org/10.1152/ajplung.00144.2019 (2020).
Bedoui, S., Herold, M. J. & Strasser, A. Emerging connectivity of programmed cell death pathways and its physiological implications. Nat. Rev. Mol. Cell Biol. 21, 678–695. https://doi.org/10.1038/s41580-020-0270-8 (2020).
Wang, H. et al. Complement induces podocyte pyroptosis in membranous nephropathy by mediating mitochondrial dysfunction. Cell Death Dis. 13, 281. https://doi.org/10.1038/s41419-022-04737-5 (2022).
Wu, H. et al. Role of MKP-5-p38/MAPK pathway in Clopidogrel-induced gastric mucosal epithelial cells apoptosis and tight junction dysfunction. Am. J. Transl. Res. 12, 1741–1753 (2020).
Zhang, X. et al. H. pylori CagA activates the NLRP3 inflammasome to promote gastric cancer cell migration and invasion. Inflamm. Res. 71, 141–155. https://doi.org/10.1007/s00011-021-01522-6 (2022).
Tomisato, W., Tsutsumi, S., Rokutan, K., Tsuchiya, T. & Mizushima, T. NSAIDs induce both necrosis and apoptosis in guinea pig gastric mucosal cells in primary culture. Am. J. Physiol. Gastrointest. Liver Physiol. 281, G1092–G1100. https://doi.org/10.1152/ajpgi.2001.281.4.G1092 (2001).
Ai, X. et al. Berberis dictyophylla F. inhibits angiogenesis and apoptosis of diabetic retinopathy via suppressing HIF-1α/VEGF/DLL-4/Notch-1 pathway. J. Ethnopharmacol. 296, 115453. https://doi.org/10.1016/j.jep.2022.115453 (2022).
Burdette, B. E., Esparza, A. N., Zhu, H. & Wang, S. Gasdermin D in pyroptosis. Acta pharmaceutica Sinica. B 11, 2768–2782. https://doi.org/10.1016/j.apsb.2021.02.006 (2021).
Lemme-Dumit, J. M., Doucet, M., Zachos, N. C. & Pasetti, M. F. Epithelial and neutrophil interactions and coordinated response to Shigella in a human intestinal enteroid-neutrophil coculture model. MBio 13, e0094422. https://doi.org/10.1128/mbio.00944-22 (2022).
Kumar, S. V. R. et al. Neutrophil extracellular trap-related extracellular histones cause vascular necrosis in severe GN. J. Am. Soc. Nephrol. 26, 2399–2413. https://doi.org/10.1681/asn.2014070673 (2015).
Wilson, A. S. et al. Neutrophil extracellular traps and their histones promote Th17 cell differentiation directly via TLR2. Nat. Commun. 13, 528. https://doi.org/10.1038/s41467-022-28172-4 (2022).
Papagoras, C., Chrysanthopoulou, A., Mitsios, A., Tsironidou, V. & Ritis, K. Neutrophil extracellular traps and interleukin 17 in ankylosing spondylitis. Mediterranean J. Rheumatol. 32, 182–185. https://doi.org/10.31138/mjr.32.2.182 (2021).
Perez-Riverol, Y. et al. The PRIDE database resources in 2022: A hub for mass spectrometry-based proteomics evidences. Nucleic Acids Res. 50, D543–D552. https://doi.org/10.1093/nar/gkab1038 (2022).
Chen, T. et al. The genome sequence archive family: Toward explosive data growth and diverse data types. Genom. Proteom. Bioinform. 19, 578–583. https://doi.org/10.1016/j.gpb.2021.08.001 (2021).
Partners, C.-N. Database resources of the National Genomics Data Center, China National Center for Bioinformation in 2022. Nucleic Acids Res. 50, D27–D38. https://doi.org/10.1093/nar/gkab951 (2022).
Acknowledgements
This research was funded by the National Key R&D Program of China (No. 2022YFC3500604).
Author information
Authors and Affiliations
Contributions
Y.J.H. and W.W. contributed equally in this study. Conceptualization, Y.J.H.; methodology, Y.C. and L.W.; software, Y.J.H. and X.Y.Y.; validation, R.H.W. and S.C.; data curation, Y.C. and J.N.Y.; writing—original draft preparation, Y.J.H. and W.W.; writing—review and editing, Y.J.H. and Y.L.; visualization, L.Q.S., S.Y.Z. and Q.H.Z.; supervision, Y.L. and Y.Z.S.; project administration, Y.J.H., J.P.Y. and Y.L. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hou, Y., Wang, W., Ye, J. et al. The crucial role of neutrophil extracellular traps and IL-17 signaling in indomethacin-induced gastric injury in mice. Sci Rep 15, 12109 (2025). https://doi.org/10.1038/s41598-025-95880-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-95880-4