Abstract
Stroke remains a critical global health issue, significantly impacting India with substantial contributions to mortality and disability. This study comprehensively analyses stroke incidence, mortality, and disability-adjusted life years (DALYs) across India from 1990 to 2021, using the latest Global Burden of Disease (GBD) 2021 data. We evaluate how Universal Health Coverage (UHC), health expenditure, human development index (HDI), and gross national income (GNI) influence stroke outcomes. Our findings reveal significant regional disparities, with higher stroke rates in urban areas and states like Goa and Kerala. Higher health expenditure and HDI are linked to lower stroke rates, while higher GNI per capita correlates with increased stroke incidence, likely due to lifestyle changes. Risk factors include air pollution, tobacco use, dietary risks, and high blood pressure. Air pollution notably impacts stroke mortality in Bihar and Jharkhand, while tobacco use is a major risk factor in Mizoram and Manipur. Dietary risks and hypertension are prevalent in Maharashtra and Jammu & Kashmir. The study highlights the need for targeted public health strategies addressing regional disparities and socioeconomic factors. Policymakers should focus on lifestyle modification programs, public awareness campaigns, and enhanced access to quality stroke care to reduce stroke-related morbidity and mortality effectively.
Similar content being viewed by others
Introduction
Stroke is a leading cause of mortality and disability worldwide, significantly impacting global public health. The World Health Organization (WHO) identifies stroke as the second leading cause of death globally, responsible for approximately 11% of all deaths1. The Global Burden of Disease (GBD) study highlights that stroke was accountable for over 6.6 million deaths and 143 million disability-adjusted life years (DALYs) in 20192. The burden is particularly pronounced in low- and middle-income countries (LMICs), which bear nearly 75% of all stroke deaths and DALYs3.
In India, the burden of stroke is substantial and growing, with profound implications for the healthcare system and public health. Stroke ranks as the fourth leading cause of death and the fifth leading cause of disability in the country4. The incidence of stroke in India ranges from 119 to 145 per 100,000 population annually, with a higher prevalence observed in urban areas compared to rural regions5. This high burden can be attributed to multiple risk factors, including hypertension, diabetes, tobacco use, dyslipidemia, and lifestyle changes associated with rapid urbanization and socioeconomic transitions6. A notable characteristic of stroke in India is the younger average age of patients compared to Western countries. A significant proportion of strokes occur in individuals younger than 65 years, with approximately 20–30% of cases occurring in those under 507,8. The gender distribution shows a higher prevalence in males, although this disparity varies by region and age group9. Disparities between rural and urban populations are evident, with urban areas generally having better access to healthcare facilities, leading to more timely interventions and improved outcomes. In contrast, rural areas face challenges such as limited healthcare access, lower awareness, and delayed treatment10.
Regarding stroke subtypes, ischemic strokes are the most common, accounting for about 70–80% of all strokes, while hemorrhagic strokes make up the remaining 20–30%11. This distribution is consistent with global trends but shows slight regional variations across different Indian states12. Stroke mortality in India is notably high, contributing significantly to the overall burden of neurological disorders13. According to the Global Burden of Disease Study (1990–2019), stroke remains one of the leading causes of death and DALYs in India14. Mortality rates for stroke vary widely across states, influenced by factors such as healthcare access, public awareness, and socioeconomic conditions15. Hypertension, diabetes, smoking, and dyslipidemia are the most prevalent risk factors for stroke in India16. The rising burden of non-communicable diseases, coupled with lifestyle changes, has exacerbated the incidence of stroke17. Public health interventions targeting these risk factors are crucial for reducing the stroke burden.
Recent studies emphasize the strong association between hypertension, diabetes, and dyslipidemia with acute stroke incidence in India18. Effective management of diabetes mellitus through integrated care approaches is critical for stroke prevention19. Tobacco use significantly impacts stroke rates, highlighting the need for robust public health policies and smoking cessation programs20. Enhanced lipid screening and management are recommended to prevent stroke21. Additionally, promoting physical activity and dietary modifications are essential strategies for reducing stroke risk22,23. These studies collectively underscore the importance of a multifaceted approach to stroke prevention in India, encompassing lifestyle modifications, medical management, and comprehensive public health initiatives to effectively mitigate the stroke burden.
In this study, we analyze the incidence of stroke and its risk factors in India, focusing on data from different geographic regions and states from 1990 to 2021 using the latest Global Burden of Disease (GBD) 2021 data. This research goes beyond a descriptive analysis of GBD data by uniquely estimating the impact of Universal Health Coverage (UHC), per capita health expenditure, per capita income, and human development on the stroke burden in India over the period from 2000 to 2021.
Examining the association between stroke burden and UHC in India is both relevant and innovative. Stroke is a leading cause of mortality and disability in the country, underscoring the need to understand its burden in relation to UHC for effective public health planning and resource allocation24. India’s commitment to achieving UHC aims to ensure that all individuals receive the necessary health services without incurring financial hardship25. Thus, assessing stroke burden within the context of UHC is crucial for evaluating progress towards these health goals26.
Insights from this study can offer valuable guidance for policymakers in crafting effective health policies and interventions. Understanding the relationship between stroke burden and UHC can pinpoint areas needing improvement, such as expanding health service coverage and optimizing financing mechanisms27. For example, a scoping review of stroke management under UHC in South Africa illustrates how enhanced coverage can improve stroke outcomes28. Additionally, incorporating per capita income and human development indicators provides a comprehensive view of how socioeconomic factors affect health outcomes29. This is especially pertinent in a diverse and rapidly developing country like India, where economic disparities have a significant impact on health30.
The novel aspect of this study lies in its longitudinal analysis covering over two decades (2000 to 2021). This extensive timeframe allows for a thorough examination of trends and long-term effects, offering valuable insights into the evolving relationship between stroke burden and UHC31. The study presents a holistic view of how these factors impact stroke burden by considering both health service coverage and financing mechanisms as components of UHC. This approach is less common in existing literature, which often separates the analysis of service coverage and financing32. This study also aligns with research on the cost-effectiveness of stroke management under UHC, emphasizing the importance of comprehensive coverage33,34.
Including per capita income and the Human Development Index (HDI) enhances the depth of the analysis, providing a nuanced understanding of how economic and developmental factors interplay with health outcomes. For instance, research on HDI and stroke mortality in the Brazilian capital highlights the impact of development on stroke outcomes35. Similarly, understanding the global relationship between socioeconomic status and stroke mortality underscores the relevance of including HDI in the analysis31. Despite substantial global research on stroke and UHC, focused studies on India are relatively limited. Given India’s unique health system challenges and socioeconomic diversity, this study addresses a critical gap in the literature36,37.
The findings from this study can help identify specific areas where health service coverage or financing mechanisms may be insufficient, facilitating targeted interventions to reduce the stroke burden. Insights into the relationship between stroke burden and socioeconomic factors can guide resource allocation, ensuring that funds are directed toward the most effective and necessary areas38,39. Furthermore, this study can illuminate disparities in health service access and financial protection, informing strategies to promote health equity in India. The novel aspects of this study also pave the way for further research, encouraging similar analyses in other countries or regions and deepening the understanding of the global UHC-stroke burden nexus.
Results
Burden of stroke (incidence, deaths, and DALYs) in India by age and sexes
Figure 1 represents the stroke incidence rate in India. The stroke incidence rate for all ages has generally increased from 76 per 100,000 population in 1990 to 88 in 2021. The 15–49 age group maintained a relatively stable incidence rate, fluctuating slightly but remaining in the mid-30 s to mid-40 s range throughout the period. A notable decreasing trend is observed in the 50–69 age group, where the incidence rate dropped from 318 in 1990 to 241 in 2021. Similarly, the 70 + age group shows a significant decrease in stroke incidence, from 962 in 1990 to 719 in 2021. The overall increase in the incidence rate for all ages may be attributed to factors such as an aging population, improved detection methods, and other epidemiological changes.
Supplementary Figure S1 shows stroke death rates in India. The overall stroke death rate in India has increased from 44 per 100,000 population in 1990 to 55 in 2021. For the 15–49 age group, the death rate remained relatively stable, fluctuating slightly around 7–9 throughout the period. In contrast, the 50–69 age group showed a significant decrease in death rates, dropping from 207 in 1990 to 152 in 2021. Similarly, the 70+ age group experienced a decrease in death rates from 806 in 1990 to 674 in 2021. The overall increase in the death rate suggests a potential rise in risk factors or an aging population contributing to higher mortality.
Supplementary Figure S2 shows the stroke DALYs rate in India. The overall DALYs rate for all ages fluctuated but generally increased from 1259 per 100,000 population in 1990 to 1374 in 2021. For the 15–49 age group, the DALYs rate decreased from 499 in 1990 to 379 in 2021. The 50–69 age group also saw a decrease in DALYs rate from 6437 in 1990 to 4711 in 2021. The 70+ age group experienced a significant reduction in the DALYs rate, decreasing from 13,565 in 1990 to 10,909 in 2021. The overall DALYs rate for all ages showed both rise and fall over the years, but the general trend was increasing.
Table 1 offers a detailed look at the burden of stroke (incidence, deaths, and DALYs rates) in India by gender (male and female) and various age groups (i.e., all ages, 15–49 years, 50–69 years, and 70+ years) between the period 1990 and 2021. The burden of stroke in India has shown mixed trends over the years. Incidence rates have generally increased for all ages but decreased in the 50–69 and 70+ age groups. Both genders have shown improvements, with males having higher rates than females. Death rates have increased overall but decreased significantly in younger and middle-aged groups. Females have shown more substantial reductions in death rates. DALYs rates have increased for all ages combined but decreased significantly in younger and middle-aged groups. Males consistently have higher rates of incidence, deaths, and DALYs compared to females across all age groups.
Burden of stroke (incidence, deaths, and DALYs) in India by geographical region and states
Table 2 provides an overview of the stroke incidence rate, death rate, and DALYs rate across various Indian states by geographical region from 1990 to 2021. Many states have seen an increase in the incidence rate of stroke over this period. Notable increases are observed in Goa (from 90 to 145), Kerala (from 113 to 145), and West Bengal (from 105 to 148). These increases could be attributed to factors such as aging populations, lifestyle changes, and improved detection rates. Conversely, a few states showed stability or a decrease in incidence rates. For instance, Jharkhand witnessed a decrease from 70 to 56, and Arunachal Pradesh remained relatively stable with a slight decrease from 64 to 63. The trends in death rates parallel those of the incidence rates, with many states showing an upward trend. Goa’s death rate increased from 90 to 145, and Kerala’s from 113 to 145, indicating a persistent mortality burden despite advancements in healthcare. Jharkhand demonstrated a decrease in death rates from 70 to 56, possibly reflecting effective stroke management and healthcare interventions. The DALYs rate, which considers both morbidity and mortality, generally increased across most states. Between 1990 and 2021, Odisha and West Bengal recorded a substantial increase, rising from 1870 to 2516 and 2308 to 3028, respectively. This underscores a growing health burden due to stroke in these states. Conversely, Delhi and Jharkhand experienced a decrease in DALYs rate, from 765 to 720 in Delhi and from 1198 to 730 in Jharkhand, suggesting effective public health measures and healthcare improvements.
To provide a clearer regional perspective, this study analyzes the burden of stroke across different geographical regions. Northern India shows mixed trends. Haryana and Himachal Pradesh saw increases in both incidence and death rates, while Uttarakhand and Delhi showed increases in DALYs rate, indicating an overall rising burden of stroke. Southern states generally exhibit an increasing stroke burden. Kerala and Karnataka saw significant increases in both incidence and death rates. The Eastern region showed significant increases in stroke burden, especially in West Bengal and Odisha, although Jharkhand demonstrated improvements. In the Western region, Goa and Maharashtra observed substantial increases in stroke burden, while Rajasthan and Gujarat had moderate increases, suggesting varying healthcare development levels. North-eastern states showed mixed trends, with Tripura and Manipur seeing significant increases in stroke burden, while Arunachal Pradesh and Mizoram showed stability or slight increases, reflecting ongoing healthcare access challenges.
The varied trends across states indicate differing levels of healthcare access, quality, and effectiveness of public health interventions in managing stroke. Addressing the stroke burden in India necessitates tailored public health strategies that account for regional healthcare capabilities and challenges.
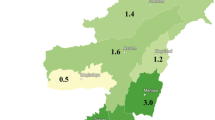
The data in Figs. 2, 3 and 4 and Supplementary Figs. S3–S5 shows a geographical map depicting the stroke burden in different Indian states between 1990 and 2021. We specifically highlight the top 10 states in India based on the incidence rate, death rate, and DALYs rate of stroke between 1990 and 2021. In 1990, the top 10 states with the highest incidence rates were Kerala, Tripura, West Bengal, Odisha, Goa, Assam, Manipur, Chhattisgarh, Karnataka, and Nagaland (Fig. S3). In 2021, the top 10 states with the highest incidence rates were West Bengal, Goa, Kerala, Tripura, Odisha, Andhra Pradesh, Assam, Chhattisgarh, Karnataka, and Manipur (Fig. 2). The top 10 states with the highest death rates in 1990 were West Bengal, Tripura, Chhattisgarh, Kerala, Assam, Odisha, Tamil Nadu, Manipur, Telangana, and Karnataka (Fig. S4). In 2021, the top 10 states with the highest death rates were West Bengal, Odisha, Chhattisgarh, Kerala, Tripura, Assam, Goa, Manipur, Maharashtra, and Telangana (Fig. 3). The top 10 states with the highest DALYs rates in 1990 were West Bengal, Tripura, Chhattisgarh, Assam, Odisha, Kerala, Tamil Nadu, Manipur, Karnataka, and Telangana (Fig. S5). In 2021, the top 10 states with the highest DALYs rates were West Bengal, Chhattisgarh, Odisha, Tripura, Kerala, Assam, Manipur, Goa, Maharashtra, and Karnataka (Fig. 4). All states have witnessed an increase in the incidence rate, death rate, and DALYs rate from 1990 to 2021. The most significant increases in death rates were observed in West Bengal (from 80 to 120) and Odisha (from 63 to 104). West Bengal (from 2308 to 3028) and Chhattisgarh (from 2131 to 2698) have shown significant increases in DALYs rates. States like West Bengal (from 105 to 148) and Kerala (from 113 to 145) have shown notable increases in incidence rates.
Risk factors of stroke and disease burden in India
Table 3 presents a list of various risk factors contributing to stroke-related death and DALYs in India in 2021, along with their respective percentages. The data shows three major risk categories: environmental/occupational, behavioral, and metabolic risks. Environmental risks include air pollution, non-optimal temperatures, and other environmental factors. Behavioral risks include tobacco use, high alcohol consumption, low physical activity, and dietary risks. Dietary risks include a low consumption of fruits and vegetables and a high consumption of red meat, fiber, and sodium. Finally, metabolic risks include high body-mass index, high cholesterol, high glucose, high blood pressure, and kidney dysfunction. Overall, the study has identified 20 risk factors associated with the burden of stroke in India.
Air pollution is a significant contributor to both death (41%) and Disability-Adjusted Life Years (DALYs) (41%) related to strokes in India. This category encompasses ambient particulate matter pollution (19%) and household air pollution from solid fuels (22%). Non-optimal temperatures also play a role, contributing 5% to both death and DALYs, with high temperatures accounting for 3% and low temperatures for 2%. Other environmental risks, primarily lead exposure, contribute 11% to death and 10% to DALYs.
Tobacco use is another major risk factor, contributing 12% to death and 14% to DALYs, with smoking (9%) and exposure to secondhand smoke (4%) contributing separately. High alcohol consumption, while a minor contributor at 3% to both death and DALYs, still plays a role. Dietary factors contribute significantly, accounting for 19% of deaths and 22% of DALYs. Diets low in fruits (12%) and high in sodium (6%) are particularly notable contributors.
Among metabolic risks, high systolic blood pressure stands out as the most significant, contributing 56% to death and 55% to DALYs associated with strokes. High fasting plasma glucose and high LDL cholesterol each contribute around 10–11% to both death and DALYs. Conversely, kidney dysfunction and high body-mass index contribute minimally to the burden of stroke-related death and DALYs in India.
In summary, air pollution, particularly from particulate matter and household fuels, non-optimal temperatures, and lead exposure, along with tobacco use (both active and passive), dietary habits (specifically low fruit intake and high sodium consumption), and high blood pressure are primary contributors to stroke-related mortality and disability in India. Addressing these risk factors through targeted public health interventions is crucial for reducing the burden of strokes and improving overall health outcomes in the population.
Figure 5 provides the percentage change in stroke deaths and DALYs number by risk factors between 1990 and 2021 in India. Overall, the analysis shows a general increase in most risk factors contributing to stroke deaths and DALYs in India between 1990 and 2021. Key contributors include lifestyle factors such as obesity, high alcohol use, high blood glucose, and high blood pressure, as well as environmental factors like air pollution.
State-wise stroke deaths by risk factors in India
Figures 6, 7, 8 and 9 presents the percentage of deaths attributed to major risk factors of stroke—air pollution (environmental risk), tobacco use, dietary risks (behavioral risks), and high systolic blood pressure (metabolic risk)—across Indian states in 2021. States like Bihar (49%), Jharkhand (40%), Odisha (40%), and Uttar Pradesh (39%) have the highest percentage of deaths attributed to air pollution, highlighting severe environmental challenges. Goa (12%), Kerala (17%), Tamil Nadu (19%), and Mizoram (21%) show lower percentages, indicating relatively better air quality or less impact from air pollution on mortality. Mizoram (24%), Manipur (21%), Meghalaya (21%), and J & K and Ladakh (19%) have the highest mortality rates due to tobacco use, pointing to significant public health issues related to smoking or tobacco consumption. Goa (5%), Jharkhand (6%), Punjab (6%), Maharashtra (7%), and Odisha (8%) have the lowest percentages, suggesting effective tobacco control measures or lower prevalence of tobacco use. Maharashtra (22%), J & K and Ladakh (21%), Uttar Pradesh (21%), and Madhya Pradesh (20%) show the highest mortality due to dietary risks, possibly due to unhealthy dietary habits or lack of access to nutritious food. Goa (12%), Kerala (14%), Telangana (15%), and Himachal Pradesh (15%) exhibit lower percentages, indicating better dietary practices or availability of healthier food options. Nagaland (68%), Sikkim (67%), Punjab (66%), and Kerala (64%) show very high percentages, indicating significant issues with hypertension and related health problems. Uttar Pradesh (50%), Madhya Pradesh (51%), Telangana (52%), and Chhattisgarh (52%) have the lowest percentages, which might be due to better management of hypertension or lower prevalence of high blood pressure. The data indicates substantial regional disparities in the health impacts of various risk factors. States with high percentages for each risk factor may need targeted interventions to address these specific issues.
The linkage between stroke burden and universal health coverage (UHC) in India
Figure 10 shows trends in Universal Health Coverage (UHC) and stroke burden in India from 2000 to 2021. The UHC (Universal Health Coverage) Service Coverage Index is a composite measure that reflects the coverage of essential health services across countries. It ranges from 0 to 100, where: Index Zero (0) means that there is no coverage of essential health services. Index One Hundred (100) represents full coverage of essential health services. It indicates a highly effective health system where all required services are available, accessible, and affordable, ensuring that the population can achieve the highest possible level of health. The UHC Service Coverage Index (SDG 3.8.1) and its sub-indices on service capacity/access and non-communicable diseases reflect gradual improvements in healthcare coverage. In 2000, the UHC Service Coverage Index was 29.66, which increased to 63.33 by 2021, indicating significant progress in healthcare access and services. Figure 4 suggests that while UHC coverage improved significantly, the stroke burden, in terms of incidence and DALYs, also rose. This indicates that increased healthcare access and services alone may not be sufficient to reduce stroke incidence and burden. Additional factors, such as lifestyle changes, preventive measures, and better management of risk factors, may be necessary to address the rising stroke burden effectively.
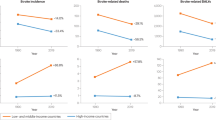
This study provides a unique estimation of the impact of universal health coverage (UHC), per capita income, and human development on the stroke burden in India from 2000 to 2021. Beyond a descriptive analysis using Global Burden of Disease (GBD) data, this study employs Ordinary Least Squares (OLS) regression to assess the effects of key predictor variables on stroke outcomes. Specifically, it examines the influence of the UHC index (focusing on service capacity and access, as well as non-communicable disease control), per capita current health expenditure, per capita gross national income, and the human development index on incidence rates, death rates, and DALYs rates associated with stroke. The detailed descriptions of the variables, along with summary statistics, correlation results, and regression results, are presented in Supplementary Tables S1 and S2. To enhance the comprehension for a broader audience across different research fields, we have illustrated our empirical findings in Fig. 11. This comprehensive approach provides valuable insights into how improvements in health coverage, economic development, and human development have contributed to mitigating the stroke burden in India over the past two decades.
Regression result graphs of stroke burden in India. Regression results can be found in Supplementary Table S1, where a color dot (.) represents the coefficient estimate, and an error bar shows the 95% confidence interval with lower and upper limits.
The regression results in Table S2 and Fig. 11 provide insights into the relationship between various factors and stroke burden in India. The regression analysis shows that the UHC index on service capacity and access has a coefficient of − 0.0864, indicating a slight negative relationship with stroke incidence, but it is not statistically significant. Similarly, the UHC index on non-communicable diseases has a coefficient of − 0.0310, which is also not significant, meaning it does not have a notable impact on stroke incidence rates. The coefficient for current health expenditure per capita is − 0.139, which is significant at the 10% level (p < 0.1). This implies that a 1% increase in health expenditure per capita is associated with a 0.139% decrease in the stroke incidence rate, indicating that higher health spending can help reduce the incidence of stroke. The Human Development Index (HDI) shows a highly significant coefficient of − 2.918 (p < 0.01), meaning that a unit increase in HDI is associated with a 2.918 unit decrease in stroke incidence rate, highlighting the crucial role of human development in reducing stroke incidence. Conversely, the gross national income (GNI) per capita has a positive coefficient of 0.808 (p < 0.01), suggesting that a 1% increase in GNI per capita is associated with a 0.808% increase in stroke incidence rate, indicating that higher income levels may be linked to higher stroke incidence.
The study shows that higher health expenditure and better human development significantly reduce stroke incidence rates. However, higher gross national income per capita is associated with increased stroke incidence and DALYs rates, indicating that rising income levels might correlate with a higher stroke burden. The UHC indices for service capacity, access, and non-communicable diseases do not show significant impacts on stroke burden indicators. This suggests that while financial and developmental improvements play crucial roles, other targeted health interventions may be needed to address the stroke burden effectively.
Discussion
This study offers a comprehensive analysis of stroke incidence, mortality, and disability-adjusted life years (DALYs) across India from 1990 to 2021, utilizing the latest Global Burden of Disease (GBD) 2021 data. Our findings reveal significant regional disparities in stroke burden, with varying trends in incidence, mortality, and DALYs across different states and geographic regions.
The observed increase in stroke incidence rates, particularly in states such as Goa, Kerala, and West Bengal, can be attributed to demographic changes, including an aging population, and improvements in stroke detection and reporting6,13. However, this increase is not uniform across the country. For example, states like Jharkhand and Arunachal Pradesh have exhibited relative stability or even slight decreases in incidence rates. The rise in stroke mortality rates in states such as Goa and Kerala, despite advancements in healthcare, highlights ongoing challenges in stroke management and underscores the need for improved stroke care and prevention strategies2,7.
The trends in DALYs across states further emphasize the necessity for region-specific public health interventions. States such as Odisha and West Bengal have shown substantial increases in DALYs, indicating a growing burden of stroke, while Delhi and Jharkhand have experienced reductions. These reductions suggest effective public health measures and improvements in healthcare services in these regions23,40.
Our analysis indicates that Universal Health Coverage (UHC) indices, including service capacity and access, do not have a significant impact on stroke incidence rates. This finding aligns with previous research suggesting that while UHC is crucial for overall health improvement, its impact on specific non-communicable diseases like stroke may be limited without targeted interventions19,20.
Socioeconomic factors play a critical role in stroke incidence rates. Higher per capita health expenditure and better Human Development Index (HDI) are significantly associated with reduced stroke incidence rates. This finding is consistent with broader literature linking increased health spending and improved development indicators with better health outcomes21,26. Interestingly, higher Gross National Income (GNI) per capita is associated with increased stroke incidence and DALYs rates. This suggests that rising income levels might correlate with lifestyle changes and increased risk factors, such as unhealthy diets and reduced physical activity27,31.
Our study identifies several key risk factors contributing to the stroke burden in India, including air pollution, tobacco use, dietary risks, and high blood pressure. Air pollution is a significant contributor to stroke mortality, particularly in states like Bihar and Jharkhand, underscoring the urgent need for environmental health interventions11. Tobacco use, although lower in some states, remains a major risk factor in others, such as Mizoram and Manipur, indicating regional variations in tobacco control efforts12,39. Additionally, dietary risks and hypertension are critical contributors to stroke burden, with states like Maharashtra and Jammu & Kashmir exhibiting high mortality rates due to these factors. This suggests that addressing dietary habits and improving hypertension management could have substantial benefits for stroke prevention28,37.
Strengths and limitations of the study
This study benefits from its use of comprehensive and up-to-date data from the Global Burden of Disease (GBD) 2021, which provides a robust and standardized assessment of stroke burden and risk factors across India41. Leveraging such a comprehensive dataset ensures that the analysis is grounded in the most current and widely accepted metrics available. Additionally, the longitudinal perspective of the study, spanning over two decades, allows for an in-depth examination of trends and changes in stroke incidence, mortality, and disability-adjusted life years (DALYs), offering valuable insights into how the stroke burden has evolved over time42. This extended timeframe enhances the study’s ability to identify long-term patterns and shifts in the burden of disease and associated risk factors. Furthermore, the study’s multifaceted approach, which includes variables related to Universal Health Coverage (UHC), health expenditure, Human Development Index (HDI), and Gross National Income (GNI), provides a holistic view of the factors influencing stroke burden. This comprehensive analysis distinguishes it from other studies that may focus on only one or two elements26.
Despite its strengths, the study has some limitations. While the Global Burden of Disease (GBD) data is extensive, it may have limitations related to the availability of other socioeconomic parameters in Indian states to estimate the regional level impact on the reduction of stroke burden. Recent studies highlight that regional socioeconomic disparities can significantly influence stroke outcomes, which may not be fully captured in national datasets43. Additionally, the impact of Universal Health Coverage (UHC) indices on specific non-communicable diseases like stroke might be more nuanced than the broad indices suggest. General UHC measures may not fully capture the complexities of how healthcare access and quality affect stroke outcomes44. Finally, the variability in stroke burden and risk factors across different states in India may not be entirely addressed by a national-level analysis. This approach could overlook significant local disparities and nuances, which might be critical for developing targeted interventions45.
Conclusion
The varying trends in stroke burden across India highlight the need for tailored public health strategies that address regional disparities in healthcare access and risk factors. While higher health expenditure and better human development are associated with reduced stroke incidence, other factors such as air pollution, tobacco use, and dietary habits require targeted interventions. Policymakers and healthcare providers must focus on improving stroke management and prevention strategies, particularly in high-burden states, to effectively reduce the overall stroke burden in India. This study underscores the importance of a multifaceted approach in tackling the complex issue of stroke and calls for continued efforts to address both the preventive and management aspects of stroke care.
Future research should explore the impact of localized interventions and policies on stroke burden at the state and district levels. Additionally, studies could investigate the effects of emerging health technologies and innovations in stroke prevention and treatment. Integrating qualitative data on healthcare access and patient experiences could further enhance understanding and inform more effective, region-specific strategies.
Methods
This study uses the latest Global Burden of Disease (GBD) study-2021 to analyze the burden of stroke and risk factors in India46. The Global Burden of Disease Study 2021 (GBD 2021), coordinated by the Institute for Health Metrics and Evaluation (IHME), estimated the burden of diseases, injuries, and risk factors for 204 countries and territories and selected subnational locations from 1990 to 202141. In this study, we extracted data related to stroke, also known as cardiovascular disease, under the non-communicable disease categories. First, we estimate the burden of stroke in India by measuring incidence, death/mortality, and Disability-Adjusted Life Years (DALYs) from 1990 to 2021. Incidence means the number of new cases of a given cause during a given period in a specified population. In other words, it is expressed as the number of new cases in a year divided by the mid-year population size. Mortality/deaths represent deaths occurring in a population during a certain time period. DALYs define the sum of years lost due to premature death (YLLs) and years lived with disability (YLD). In other words, DALYs mean years of healthy life lost. We have measured these three indicators—Incidence, Deaths, and DALYs as a rate that shows the distribution of disease burden per 100,000 population. Further, this study also examines the burden of stroke across age groups, including all ages, 15–49 ages, 50–69 Older, and 70+ aging, and across genders, i.e., male, female, and both. Second, we estimate the risk factors of stroke and associated disease burdens such as death and DALY percentage. Third, we explore stroke burden and risk factors across states in India by dividing them into four geographical regions (i.e., North, South, East, West, and North-Eastern).
Apart from conducting a descriptive analysis using Global Burden of Disease (GBD) data, this study uniquely estimates the impact of universal health coverage (UHC), current health expenditure (CHE) per capita, gross national income (GNI) per capita, and human development index (HDI) on the stroke burden in India from 2000 to 2021. The study uses the following Ordinary regression model (OLS).
Equation (1) presents a simple OLS regression equation where the outcome variable is stroke burden, which is measured in three indicators—incidence rate, death rate, and DALYs rate, whereas predicted variables are UHC services coverage index on Service Capacity and Access; and service coverage on Non-communicable diseases, and control variables are current health expenditure (CHE) per capita, human development Index (HDI), and gross national income (GNI) per capita. ‘t’ denotes time, β1-β4 presents coefficient estimates which shows the elasticity of stroke burden with respect to independent variables. ¨ln¨ presents the logarithmic transformation of variables; α0 denotes intercept; and µt denotes disturbances error term.
A description of variables and summary statistics of variables is reported in the Supplementary Table S1. The UHC index is typically scored on a scale from 0 (i.e., lowest level of service coverage) to 100 (i.e., highest level of service coverage). The UHC (Universal Health Coverage) index on service capacity and access is a comprehensive measure designed to evaluate the ability of a health system to provide essential health services to its population. It assesses various dimensions of healthcare, including service availability (i.e., hospitals, clinics, and specialty care centers), Service Quality (i.e., competency of healthcare professionals, the effectiveness of treatments, and patient satisfaction), service accessibility (i.e., access healthcare services, considering factors such as distance, transportation, and financial barriers), Health Workforce (i.e., doctors, nurses, and allied health professionals), Essential Medicines (i.e., availability of necessary medicines and medical supplies), and Health Information Systems (i.e., infrastructure for health data collection, management, and utilization, which is critical for informed decision-making and policy planning).
The UHC (Universal Health Coverage) index on non-communicable diseases (NCDs) specifically focuses on the capacity of a health system to prevent, manage, and treat chronic non-communicable diseases, such as cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes. This index evaluates several critical components that contribute to the effectiveness of a health system in addressing NCDs. These components include Prevention and Health Promotion, Access to Diagnosis and Treatment, Management of Risk Factors, Continuity of Care, and Health System Strengthening. The UHC (Universal Health Coverage) Service Coverage Index, also known as SDG 3.8.1. The index comprises of 16 tracer indicators grouped into four main categories: Reproductive, Maternal, Newborn, and Child Health; Infectious Diseases; Non-communicable Diseases; and Service Capacity and Access47. The Human Development Index (HDI) is a composite statistic that ranks countries based on human development levels. It provides a broad view of development by combining indicators of health (Life Expectancy at Birth), education (mean years and expected years of schooling), and income (Gross national income per capita). HDI index ranges from a scale of 0 to 1 using minimum and maximum values set by the UNDP. Data for this study has been collected from various sources. Stroke data was collected from the GBD study-2021 by IHME46; UHC index data was obtained from the Global Health Observatory database of the World Health Organization48. Health expenditure and gross national income data were collected from the World Health Organization’s Global Health Expenditure Database49. Human Development Index data was collected from the UNDP Human Development Report50.
Several key aspects are noteworthy to highlight the novelty of this study from a health system and policy perspective. Each dimension used in this study—Universal Health Coverage (UHC), Human Development Index (HDI), health expenditure, and gross national income (GNI)—contributes unique insights into understanding stroke burden in India. While most studies focus on individual aspects of UHC, this study integrates multiple dimensions of UHC, including service capacity and access and NCD-specific service coverage. This comprehensive approach provides a detailed understanding of how well the healthcare system manages stroke care and other chronic diseases51. This study uniquely incorporates HDI to examine stroke burden, linking broader socioeconomic conditions with health outcomes. Many studies only use economic or health-specific indicators, but this integration provides a holistic view of how development impacts stroke outcomes50. The study’s use of long-term data (2000–2021) to analyze the impact of CHE and GNI on stroke burden offers insights into how changes in health financing and economic conditions affect stroke outcomes over time. This temporal perspective is relatively rare in stroke burden research47. The study identifies regional disparities and variations in stroke outcomes by examining stroke burden across different states and geographical regions within India45. This granularity helps in understanding how local health system differences impact stroke burden.
This study’s novelty lies in its multifaceted approach to analyzing stroke burden using a combination of UHC dimensions, HDI, health expenditure, and GNI. This comprehensive perspective allows for a nuanced understanding of how different aspects of health systems and socioeconomic conditions impact stroke outcomes in India. By integrating these dimensions, the study provides valuable insights into the effectiveness of health policies and interventions.
Data availability
Data materials are available in the public domain for research purposes and not for commercial use. Data can be obtained from the open-access repository of the Institute of Health Metrics Evaluation (IHME).
Abbreviations
- DALYs:
-
Disability-adjusted life years
- GBD:
-
Global burden of disease
- CVA:
-
Cardiovascular accident
- IHME:
-
Institute of health metric evaluation
- YLLs:
-
Years lost due to premature death
- YLD:
-
Years lived with disability
- LDL:
-
Low-density lipoprotein
- NPCDCS:
-
National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke
- NHM:
-
National Health Mission
- UHC:
-
Universal health coverage
- HDI:
-
Human development index
- GNI:
-
Gross National Income
- NCDs:
-
Non-communicable diseases
- SCA:
-
Service capacity and access
- CHE:
-
Current health expenditure
References
World Health Organization. The Top 10 Causes of Death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (2020).
GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 20, 795–820 (2019).
Feigin, V. L., Norrving, B. & Mensah, G. A. Global burden of stroke. Circ. Res. 120, 439–448 (2017).
India State-Level Disease Burden Initiative Stroke Collaborators. The burden of stroke in India: A systematic review of population-based studies. Lancet Glob. Health 6, e662–e671 (2018).
Banerjee, T. K. & Das, S. K. Fifty years of stroke research in India. Ann. Indian Acad. Neurol. 19, 1–8 (2016).
Das, S. K. & Banerjee, T. K. Stroke: Indian scenario. Circulation 118, 2719–2724 (2008).
Gupta, R. & Xavier, D. Hypertension: The most important non-communicable disease risk factor in India. Indian Heart J. 70, 565–572 (2018).
International Diabetes Federation. IDF Diabetes Atlas 9th edn. (International Diabetes Federation, 2019).
Prabhakaran, D., Jeemon, P. & Roy, A. Cardiovascular diseases in India: Current epidemiology and future directions. Circulation 133, 1605–1620 (2016).
Ministry of Health and Family Welfare, Government of India. Ayushman Bharat for a New India—2022. https://www.pmjay.gov.in/about/ayushman-bharat-yojana (2018).
Rangamani, S. et al. Stroke incidence, mortality, subtypes in rural and urban populations in five geographic areas of India (2018–2019): Results from the National Stroke Registry Programme. Lancet Reg. Health Southeast Asia 23, 100308 (2023).
Singh, G. et al. The burden of neurological disorders across the states of India: The Global Burden of Disease Study 1990–2019. Lancet Glob. Health 9, e1129–e1144 (2021).
Katan, M. & Luft, A. Global burden of stroke. Semin. Neurol. 38, 208–211 (2018).
Mukherjee, D. & Patil, C. G. Epidemiology and the global burden of stroke. World Neurosurg. 76, S85–S90 (2011).
Khurana, S., Gourie-Devi, M., Sharma, S. & Kushwaha, S. Burden of stroke in India During 1960 to 2018: A systematic review and meta-analysis of community based surveys. Neurol. India 69, 547 (2021).
Kuriakose, D. & Xiao, Z. Pathophysiology and treatment of stroke: Present status and future perspectives. Int. J. Mol. Sci. 21, 20609 (2020).
Kaul, S., Bandaru, V. C. S. S., Suvarna, A. & Boddu, D. B. Stroke burden and risk factors in developing countries with special reference to India. J. Indian Med. Assoc. 107(358), 367–370 (2009).
Ram, C. V. S. et al. Risk factors predisposing to acute stroke in India: A prospective study. J. Hypertens. 39, 2183 (2021).
Marwaha, R. & Reddy, K. S. Management of diabetes mellitus and stroke risk reduction in India. J. Clin. Med. 11, 2432 (2022).
Mendis, S. & Puska, P. Tobacco use and stroke in India: The current status and future directions. Indian J. Public Health 66, 19 (2022).
Nair, S. S., Reddy, S. & Sahu, S. Lipid profiles in stroke patients: Insights from the Indian context. J. Cardiovasc. Dis. Res. 12, 105–110 (2021).
Babu, M. & Kurup, P. Promoting physical activity as a strategy for stroke prevention in India. Indian J. Sports Med. 35, 143–147 (2019).
Joshi, S. & Kaur, J. Dietary modifications and stroke prevention in Indian populations. J. Nutr. Health Food Eng. 7, 49–56 (2022).
WHO. Global Health Estimates: Leading Causes of Death. (World Health Organization).
Government of India. National Health Policy 2017 (Ministry of Health and Family Welfare, 2017).
Patel, V. et al. Assuring health coverage for all in India. Lancet 386, 2422–2435 (2015).
Reddy, K. S. et al. Responding to the threat of chronic diseases in India. Lancet 377, 541–548 (2011).
van Niekerk, S. M. et al. Towards universal health coverage for people with stroke in South Africa: A scoping review. BMJ Open 11, e049988 (2021).
Nandi, A. et al. Early life exposure to maternal health care and chronic disease risk in India. Soc. Sci. Med. 244, 112571 (2020).
Barik, D. & Thorat, A. Issues of unequal access to public health in India. Front. Public Health 3, 245 (2015).
Pandey, A. et al. Evidence from the India hypertension control initiative—A public health success story. J. Hum. Hypertens. 33, 576–586 (2019).
Chang, K. C. et al. Cost-effectiveness analysis of stroke management under a universal health insurance system. J. Neurol. Sci. 323, 205–215 (2012).
Gesesew, H. A. et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1250–1284 (2020).
E Melo Lucena, D. M. et al. Correlation between municipal human development index and stroke mortality: A study of Brazilian capitals. BMC Res. Notes 11, 1–6 (2018).
Wu, S. H. et al. Worldwide socioeconomic status and stroke mortality: An ecological study. Int. J. Equity Health 12, 1–11 (2013).
Das, M. et al. The gendered experience with respect to health-seeking behaviour in an urban slum context. PLoS ONE 15, e0227157 (2020).
Sposato, L. A. & Saposnik, G. Gross domestic product and health expenditure associated with incidence, 30-day fatality, and age at stroke onset: A systematic review. Stroke 43, 170–177 (2012).
Ramamoorthy, V. et al. Healthcare expenditure trends among adult stroke patients in the United States, 2011–2020. J. Stroke Cerebrovasc. Dis. 32, 107333 (2023).
Rajasulochana, S. R. & Kar, S. S. Economic burden associated with stroke in India: Insights from national sample survey 2017–18. Expert Rev. Pharmacoecon. Outcomes Res. 22, 455–463 (2022).
Kamalakannan, S. et al. Incidence & prevalence of stroke in India: A systematic review. Indian J. Med. Res. 146, 175–185 (2017).
IHME. Global Burden of Disease 2021: Findings from the GBD 2021 Study. https://vizhub.healthdata.org/gbd-results/ (Institute for Health Metrics and Evaluation, 2024).
Brauer, M. et al. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2162–2203 (2024).
Avan, A. et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 17, 1–30 (2019).
Ng, M. et al. Effective coverage: A metric for monitoring universal health coverage. PLoS Med. 11, e1001730 (2014).
Mohanty, R. K. & Behera, D. K. Heterogeneity in health funding and disparities in health outcome: A comparison between high focus and non-high focus states in India. Cost Eff. Resour. Alloc. 21, 44 (2023).
IHME. Global Burden of Disease Study 2021 (GBD 2021). Results. https://vizhub.healthdata.org/gbd-results/ (Global Burden of Disease Collaborative Network, 2022).
Behera, D. K. & Dash, U. Is health expenditure effective for achieving healthcare goals? Empirical evidence from South-East Asia Region. Asia-Pac. J. Reg. Sci. 4, 593–618 (2020).
WHO. Global Health Observatory Database. https://www.who.int/data/gho (2024).
WHO. Global Health Expenditure Database. https://apps.who.int/nha/database (2024).
UNDP. Human Development Report 2021–22: Uncertain Times, Unsettled Lives: Shaping our Future in a Transforming World. https://hdr.undp.org/content/human-development-report-2021-22 (United Nations Development Programme, 2022).
Marmot, M. & Allen, J. J. Social determinants of health equity. Am. J. Public Health 104, S517–S519 (2014).
Acknowledgements
We would like to thank the Institute of Health Metrics Evaluation (IHME) for providing data access support for this study. We would also like to thank the Asian Development Bank Institute (ADBI), Tokyo, Japan, for the support to this project. Views expressed in this paper do not reflect the view of the author’s institution, and the usual disclaimer applies. This map does not imply the expression of any opinions of the authors or the author’s institution concerning the boundaries.
Author information
Authors and Affiliations
Contributions
DKB: Conceptualization, data cleaning, analysis, write-up, editing, and structuring. DRB.: Conceptualization, write-up, editing and structuring, and supervision. SM: analysis and write-up.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
This paper utilizes secondary data available from the open-access repository of the Institute of Health Metrics Evaluation (IHME), which is in the public domain; therefore, no ethical clearance is required. The study did not involve any direct or indirect human participation.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Behera, D.K., Rahut, D.B. & Mishra, S. Analyzing stroke burden and risk factors in India using data from the Global Burden of Disease Study. Sci Rep 14, 22640 (2024). https://doi.org/10.1038/s41598-024-72551-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-72551-4
Keywords
This article is cited by
-
Analysis and comparison of the burden of male breast cancer: differences between the global, China, India, and the United States
BMC Public Health (2025)
-
Unveiling the neuroprotective power: the role of autophagy in remote ischemic conditioning
Metabolic Brain Disease (2025)
-
Exploring Hypoxia-Induced Neuroprotection Mechanisms in Post-Stroke Recovery
Translational Stroke Research (2025)
-
Evaluating the national burden of PM2.5 in India: a comprehensive study of spatiotemporal distribution at state and city levels, non-carcinogenic health hazards, and premature mortality
Environmental Monitoring and Assessment (2025)