Abstract
Combination antiretroviral therapy (ART) has improved outcomes for human immunodeficiency virus (HIV) associated non-Hodgkin lymphoma. This is an analysis of 127 patients with HIV with Burkitt lymphoma (HIV-BL) and diffuse large B-cell lymphoma (HIV-DLBCL) treated at the Zhongnan Hospital of Wuhan University over a 17-year period during the ART and rituximab era. The median CD4 count for the cohorts was 0.141 × 109/L (range, 0.001-0.861 × 109/L). DA-EPOCH ± R (54%) were most commonly used in HIV-BL. CHOP± R (42%) was most commonly used to treat HIV-DLBCL. The complete response rate after first-line curative therapy was 10/28 (36%) in HIV-BL and 25/57 (44%) in HIV-DLBCL. The 2-year progression-free survival (PFS) and overall survival (OS) for the HIV-BL cohort was 50% and 41% respectively. The 2-year PFS and OS for the HIV-DLBCL cohort was 55% and 47% respectively. Current China practice favours the treatment of HIV-BL and HIV-DLBCL similarly to the HIV-negative population with the use of concurrent ART. However, due to the extremely low percentage of patients receiving ART prior to the lymphoma diagnosis, the high percentage of patients with poor performance status, and the advanced stage at diagnosis, the treatment of HIV-related lymphoma remains the major challenge in China.
Similar content being viewed by others
Introduction
In China, 110,000 people were newly infected with HIV in 2020, reaching 1.04 million HIV-positive people1. People living with HIV (PLWH) have a greater risk of developing cancer than the general population. Cancers that develop in the setting of HIV have traditionally been categorized into two categories: cancers that, when present, provide an AIDS diagnosis (AIDS-defining malignancies, or ADMs) and cancers that do not necessarily signal AIDS (non-AIDS-defining malignancies, or NADMs)2. The most common subtypes of HIV-associated non-Hodgkin lymphoma (NHL) are diffuse large B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL), which are both ADMs3. Before the development of effective combination antiretroviral therapy (ART), the relative risk for NHL was estimated as 60- to 200-fold compared with the general population4. Since the introduction of ART in 1996, the incidence of various ADMs has decreased by 75–80%5. However, the risk remains significantly elevated for each AIDS-defining NHL subtype, specifically DLBCL standardized incidence ratio (SIR 10), and BL (SIR 20)6,7.
HIV-DLBCL, which accounts for 45% of all HIV-related NHL subtypes, is linked to higher-risk prognostic characteristics8. HIV-DLBCL patients had a median survival duration of only 5 to 8 months prior to the advent of ART. This is because opportunistic infections can quickly complicate patients, which raises mortality9. In the ART era, individuals with HIV-DLBCL may experience a 5-year overall survival (OS) of up to 55% when ART is combined with intense chemotherapy10. The preferred regimen varies by region and institution, but one retrospective series suggests that DA-EPOCH-R (etoposide, prednisolone, vincristine, cyclophosphamide, doxorubicin, rituximab) may be associated with superior OS in immunocompetent patients with HIV-DLBCL. Currently, the first-line regimens used are R-CHOP-based regimens (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisolone) and DA-EPOCH-R11,12.
HIV-BL, which accounts for 35% of NHL subtypes, is more prevalent in PLWH with a comparatively elevated CD4 cell count13. The incidence of BL has not decreased throughout the ART era, in contrast to other subtypes. One of the suggested theories is that elevated CD4 cell numbers could trigger more B cell activation, which would speed up the production of lymphomagenic molecular events like the c-myc immunoglobulin translocation event in BL14. As of right now, R-CODOX-M/IVAC (rituximab, cyclophosphamide, vincristine, doxorubicin, high-dose methotrexate, ifosfamide, etoposide, high-dose cytarabine), R-Hyper-CVAD (rituximab, cyclophosphamide, doxorubicin, vincristine, methotrexate, high-dose cytarabine), and DA-EPOCH-R are the preferred chemotherapy regimens currently used to treat BL in the general population15,16.
In the general population, rituximab is an essential part of B-cell NHL therapy; nevertheless, preliminary phase 2 studies raised concerns about safety in HIV17. A phase 3 trial revealed that rituximab enhanced toxicity in patients with CD4 counts < 50 cells/µL and was unable to show any additional benefits when added to CHOP18. Rituximab, however, seems to be safe in all other individuals according to a pooled analysis of AMC studies. Particularly, patients with a CD4 count < 50 cells/µL had a treatment-related mortality (TRM) of 37%, while the remaining patients had a TRM of only 6% (p < 0.01)11. Non-comparison trials have also contributed to the broad view that rituximab should be used while infection is being monitored, as well as preventive hematopoietic growth factors in all patients and antibiotic prophylaxis in those at greatest risk19.
Studies summarizing the Chinese experience treating NHL-associated HIV are currently lacking. In the present study, we report on 17 years of retrospective China data on HIV-BL and HIV-DLBCL, including diagnosis, therapy, and lymphoma- related outcomes.
Methods and materials
Study population
Consecutive patients with HIV-associated, biopsy confirmed, BL and DLBCL diagnosed between 1 January 2005 and 31 December 2022 at the Department of Infectious Diseases, Zhongnan Hospital of Wuhan University through electronic database were included for this single center retrospective analysis. Other histological subtypes such as Hodgkin lymphoma, T-cell lymphoma, primary effusion lymphoma, primary central nervous system (CNS) lymphoma and plasmablastic lymphoma were excluded. This study was approved by the Medical Ethics Committee of Zhongnan Hospital of Wuhan University (No. 2023266 K). It was performed in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent.
Data on patient demographics, HIV-related characteristics at the time of lymphoma diagnosis (e.g., CD4 count, ART regimen, concurrent hepatitis B/C co-infection), lymphoma-related characteristics (e.g., cell-of-origin subtype for DLBCL, presence of MYC proto-oncogene, bHLH transcription factor (MYC), BCL2 apoptosis regulator (BCL2) or BCL6 transcription repressor (BCL6) rearrangements, lactate dehydrogenase (LDH), Ann Arbor stage, extranodal sites, Eastern Cooperative Oncology Group Performance Status (ECOG PS) score, International Prognostic Index (IPI) score), and treatment-related information (e.g., first-line and subsequent therapy regimens including radiotherapy, the use of rituximab, CNS prophylaxis, the use of concurrent ART) were collected and analysed.
Treatment and supportive care
Before 2018, HIV patients received free anti HIV treatment provided by the Chinese government, which included two nucleoside/nucleotide reverse transcriptase inhibitors (zidovudine + lamivudine, or lamivudine + tenofovir disoproxil) plus one non-nucleoside reverse transcriptase inhibitor (efaviren, or nevirapine) or protease inhibitor (lopinavir, or ritonavir capsules), and after 2018, due to the availability of drugs, the ART regimen was adjusted to either bictegravar soudium, emtricitanine and tenofovir alafenamid fumarite tablets or dolutegravir sodium and lamivudine tablets. Most oncologists continue ART during chemotherapy. In early ART days concerns arouse regarding drug-drug interactions and increased toxicities. With new ART medications available, it is now possible to avoid specific ART components to minimize drug-drug interaction20. Cotrimoxazole was given to prevent pneumocystis jirovecii pneumonia. The chemotherapy cohort included patients who received any of the following regimens: CHOP; R-CHOP; EPOCH; R-EPOCH.
Outcome assessment
Treatment outcome assessments were performed either positron emission tomography (PET) ± computed tomography ± bone marrow (BM) biopsy. They were assessed according to the standard response criteria at the time of assessment; either response evaluation criteria in solid tumors (RECIST) 2000 or Lugano 201421,22. Response outcomes were defined as either complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD). Date of HIV-lymphoma diagnosis, death, progression/relapse, and last follow-up was collected for survival analysis. Additional information collected include the number of cycles of chemotherapy delivered, evidence of serious treatment-related complications, the HIV viral load and CD4 cell counts were tested at diagnosis.
Statistical analysis
The program used was GraphPad Prism version 10.0.0 (GraphPad Software Inc. www.graphpad.com). Baseline characteristics were presented using mean (standard deviation) or median (interquartile range (IQR)) for continuous variables and count (percentage) for categorical variables. Baseline demographic, clinical and pathological variables were compared between BL and DLBCL groups using Pearson’s chi-square test and the Mann-Whitney U-test. Progression-free survival (PFS) was defined as the time from lymphoma diagnosis to disease progression, relapse or death from any cause. OS was defined as the time from lymphoma diagnosis to last follow-up or death from any cause. Kaplan-Meier curves were used for survival analysis (OS and PFS) and comparisons between groups were analysed using the log-rank (Mantel-Cox) test and univariate Cox proportional hazards regression model. Changes over time in CD4 counts was presented using median and IQR. A p < 0.05 was considered statistically significant. Missing data was handled using the pairwise deletion statistical method.
Results
Participant characteristics
A total of 127 patients were included in the study. There were 86 (68%) patients with HIV-DLBCL and 41 (32%) with HIV-BL. The median (range) follow-up was 0.4 (0.1–14.0) years. Baseline characteristics for each cohort are summarised in Table 1. The median (range) age of the cohort was 47.1 (11–71) years and 114 (90%) were male. Of the 127 patients, 89 (70%) were concurrently diagnosed with NHL and HIV. The median CD4 count for the cohorts was 0.141 × 109/L (range, 0.001–0.861 × 109/L), of whom 79 (62%) had a CD4 cell count below 0.200 × 109/L at diagnosis. 11 patients had concurrent hepatitis B surface antigen positivity and 9 patients had active hepatitis C infection at diagnosis. Before 2018, there were limited HIV virus load testing institutions and equipment in China, mainly concentrated in provincial and above disease prevention and control centers for testing. Although there have been more HIV testing institutions since 2018, they have not yet become widespread, and only some patients have information on their virus load at the time of initial diagnosis. There were 25 patients (25/127, 13 with DLBCL, 12 with BL) with HIV viral loads available at first diagnosis, 52% of patients had a HIV viral load of < 50 copies/mL.
The majority of patients (n = 91 (72%), HIV-BL (98%) and HIV-DLBCL (59%)) were diagnosed with high-risk disease based on their disease-specific IPI (DLBCL R-IPI by Sehn et al. and BL-IPI by Olszewski et al.23,24). In the HIV-BL cohort, 32 (78%) patients had an ECOG PS of ≥ 2, 35 (85%) with stage III/IV disease, 32 (78%) with two or more extranodal sites, 36 (88%) with an elevated LDH, 24 (59%) with BM involvement, 12 (29%) with CNS/leptomeningeal involvement at diagnosis and 17 (41%) with B symptoms. In the HIV-DLBCL cohort, 50 (58%) patients had an ECOG PS of ≥ 2, 60 (70%) with stage III/IV disease, 31 (36%) with two or more extranodal sites, 50 (58%) with an elevated LDH, 33 (38%) with BM involvement, 20 (23%) with CNS/leptomeningeal involvement and 37 (43%) with B symptoms.
There were 82 (65%) patients had an ECOG PS of ≥ 2 with a higher proportion seen in the HIV-BL cohort (78% vs. 58%, p = 0.028). There were 63 (50%) patients with two or more extranodal sites with a higher proportion seen in the HIV-BL cohort (78% vs. 36%, p = 0.000). There were 86 (68%) patients with an elevated LDH with a higher proportion seen in the HIV-BL cohort (88% vs. 58%, p = 0.001). There were 57 (45%) patients with BM involvement with a higher proportion seen in the HIV-BL cohort (59% vs. 38%, p = 0.033). There were 75 (59%) patients with bulky disease with a higher proportion seen in the HIV-BL cohort (78% vs. 50%, p = 0.003).
Lymphoma treatment
A total of 85/127 (67%) patients received therapy with curative intent, where 23/85 (27%), 60/85 (71%), and 2/85 (2%) were in the 1–3, 4–6, and > 6 cycles chemotherapy cohort, respectively. The patients had less than four cycles of antilymphoma therapy due to poor PS and advanced stage at diagnosis, most of them died due to the rapid progression of the disease. 1/127 patients with HIV-BL and 6/127 with HIV-DLBCL receiving palliative therapy. 35/127 (28%) patients received no anti-lymphoma therapy because of fear of discrimination and poor financial situation. Patients with HIV-BL were most commonly treated with dose-intensive regimens such as R-DA-EPOCH or DA-EPOCH (54%), followed by R-CHOP (12%). CHOP-based chemotherapy was most commonly used to treat HIV-DLBCL, with 36 patients receiving this regimen (42%). There were 21 (24%) patients with HIV- DLBCL managed with more intensive regimens DA-EPOCH ± R. Of the patients receiving curative chemotherapy, 45 (35%) patients received rituximab (21 (51%) with HIV-BL and 24 (28%) with HIV-DLBCL). In all, 89 (70%) patients received ART with chemo-immunotherapy concurrently. Only nearly half of the patients (62/127 (49%)) completed their intended chemotherapy regimen. There were 6 (5%) patients who had treatment truncated due to infective complications (5 (4%) patients), pulmonary embolism (one (0.8%) patient).
The computed tomography or PET-defined CR rate after first-line curative therapy was 10/28 (36%) in HIV-BL and 25/57 (44%) in HIV-DLBCL (Fig. 1). In HIV-BL, best tumor responses included CR (6 R-DA-EPOCH, 2 DA-EPOCH, 2 R-CHOP, 10 patients), PR (2 R-DA-EPOCH, 2 DA-EPOCH, 1 R-CHOP, 5 patients), 0 patient for SD, and PD (8 R-DA-EPOCH, 2 DA-EPOCH, 2 R-CHOP, 1 CHOP, 13 patients). In HIV-DLBCL, best tumor responses included CR (5 R-DA-EPOCH, 3 DA-EPOCH, 6 R-CHOP, 11 CHOP, 25 patients), PR (2 R-DA-EPOCH, 2 DA-EPOCH, 3 R-CHOP, 1 CHOP, 8 patients), SD (1 R-CHOP, 1 patients), and PD (4 R-DA-EPOCH, 5 DA-EPOCH, 3 R-CHOP, 11 CHOP, 23 patients).
Febrile neutropenia (Common Terminology Criteria for Adverse Events Grade ≥ 3) was higher in the HIV-BL cohort compared to the HIV-DLBCL cohort (68% vs. 47% respectively, p = 0.075). It was also higher for DA-EPOCH ± R when compared to CHOP ± R (57% vs. 42%, p = 0.259). There were two treatment related deaths, one from pulmonary embolism, the other from tracheoesophageal fistula in the HIV-BL group. There were four treatment related deaths, three from infections (one intestinal infection, two pulmonary infection), one from gastrointestinal bleeding in the HIV-DLBCL group.
Survival outcomes
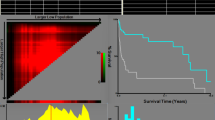
92 (72%) patients received anti-tumor therapy (85 patients received curative therapy, 7 patients received palliative therapy), and those 35 patients did not receive chemotherapy have been excluded from the survival analyses. After a median (range) follow-up of 0.4 (0.1–14.0) years, 53 (58%) patients had died; 45 (49%) from disease, two from severe pneumonias, one from pulmonary embolism, one from severe diarrhea leading to water electrolyte disorders, one from sepsis, one from infection caused by esophagotracheal fistula, one from gastric cancer, and one from valvular heart disease. There were no HIV-related deaths. The 2-year OS rate for the entire cohort was 45% (95% confidence interval (CI) 35-55%). The 2-year OS for the HIV-BL cohort was 41% (95% CI 24%-58%) and 47% (95% CI 34%-59%) for HIV-DLBCL cohort. The 2-year PFS for the HIV-BL cohort was 50% (95% CI 30%-66%) and for the HIV-DLBCL cohort was 55% (95% CI 41%-67%) (Fig. 2).
An exploratory univariate analysis was performed on selected lymphoma variables (histological subtype, IPI > 2, BM involvement, CNS involvement, elevated LDH, bulky disease, B symptoms, rituximab use) and CD4 count < 0.100 × 109/L with the recognition that this study was not powered to draw definitive conclusions (Table 2). In our analysis, no variables impacted on OS. CNS involvement negatively impacted PFS (HR 3.23, 95% CI 1.38–7.53, p = 0.007). In HIV-BL, B symptoms negatively impacted OS (HR 10.07, 95% CI 1.92–52.72, p = 0.006) and PFS (HR 8.73, 95% CI 1.43–53.35, p = 0.019), and CD4 count < 0.100 × 109/L negatively impacted OS (HR 12.49, 95% CI 2.44–63.80, p = 0.002) and PFS (HR 8.23, 95% CI 1.92–35.36, p = 0.005) (Table 3). In HIV-DLBCL, CNS involvement negatively impacted PFS (HR 4.59, 95% CI 1.20–17.52, p = 0.026) (Table 4).
Discussion
Understanding the clinical features and prognostic variables of HIV-associated lymphoma is limited since it is less common in China than HIV-negative lymphoma10,25. As the biggest cohort described in China to date, we performed a description of the clinical features and prognosis of patients with HIV-DLBCL and BL across a 17-year period at a single academic medical center. The initial symptoms of HIV-associated lymphoma are more diverse than those of HIV-negative lymphoma; more cases of this disease are diagnosed at an advanced stage, frequently with B symptoms present, and exhibit more extranodal involvement3. In the present study, the majority of patients presented with advanced stage (85% in HIV-BL and 70% in HIV-DLBCL) and high-risk disease based on disease-specific IPI scoring systems (HIV-BL 98%, HIV-DLBCL 59%). Patients had a high frequency of B symptoms (HIV-BL 41%, HIV-DLBCL 43%), extranodal involvement ≥ 2 (HIV-BL 78%, HIV-DLBCL 36%), and bulky disease (HIV-BL 78%, HIV-DLBCL 50%). According to these findings, HIV-associated lymphoma may be more aggressive. On the other hand, compared to their HIV-negative counterparts, HIV positivity has been demonstrated to have no effect on treatment deliverability, response, and patient survival in ART-treated patients15,26.
A German group of patients with HIV-lymphoma who were diagnosed between 2005 and 2012 had a median CD4 count of 0.200 × 109/L, and 37% of them were on ART at the time of diagnosis27. In a French study, 79% of patients with an HIV-DLBCL cohort had already started ART, with a median CD4 count of 0.233 × 109/L28. The bulk of patients in our study (70%) were on ART at the time of their lymphoma diagnosis, which probably played a role in the relatively low baseline mean and median CD4 counts (0.182 and 0.141 × 109/L) observed in our real-world cohort when compared to developed countries27,28. This suggests that HIV screening should be a priority for patients with newly diagnosed BL and DLBCL.
According to research by Lim et al., patients with HIV-DLBCL had a 2-year PFS of 77% and an OS of 81%, while those with HIV-BL had a 2-year PFS of 67% and an OS of 67%13, Coutinho et al. showed a 5-year OS of 78% versus 64% in HIV-positive and HIV-negative DLBCL respectively29, in patients with HIV-DLBCL, Besson et al. reported a 2-year PFS and OS of 75% and 75%, respectively28. Regardless of HIV status, a US retrospective research for HIV-BL reported a 3-year PFS and OS rate of 64% and 70%, respectively30. A follow-up collaborative study between the USA and the UK revealed that the 3-year PFS and OS for 249 HIV-BL patients treated between 2008 and 2019 were 61% and 66%, respectively15. Our study findings of a 2-year PFS of 55% and OS of 47% in patients with HIV-DLBCL, and a 2-year PFS of 50% and OS of 41% in patients with HIV-BL, were lower than the published international data. Even though the comparison is still in its preliminary stages, there are a few reasons why our study’s PFS and OS were lower and they merit additional research: (1) CD4 counts: The fact that 70% of the patients in our study started ART concurrently to the lymphoma diagnosis suggests that the baseline mean and median CD4 counts were not particularly high. These patients are easily complicated by opportunistic infections, resulting in an increase in mortality. (2) baseline clinicopathological characteristics: Due to poor PS and an advanced stage upon diagnosis, 27% of patients received less than four cycles of antilymphoma therapy; the majority of these patients passed away as a result of the disease’s quick progression. According to the CALL trial, patients with HIV- associated DLBCL who had 4–6 cycles of chemotherapy had considerably better outcomes; individuals who received fewer than 4 cycles of chemotherapy had an independent risk factor for a poor prognosis (HR 0.520, 95% CI 0.424–0.637; p < 0.001)9. (3) Rituximab: Rituximab usage is linked to improved PFS and OS in patients with a CD4 count ≥ 50 cells/µL and positive expression of CD20. However, because infections are more common in patients with a CD4 count < 50 cells/µL, the benefit of rituximab is less evident31. 47 patients in our study received rituximab, 11 of them had a CD4 count < 50 cells/µL, and 6 of the 11 patients (55%) died. Our results showed that treatment of HIV-related lymphoma remains the major challenge in China.
It is currently unknown if the prognostic risk of aggressive B-cell NHL associated with HIV infection may be evaluated using the same model as individuals without HIV infection. The AIDS-related lymphoma IPI (ARL-IPI), developed by Barta SK et al., is a new prognostic index that patients patients into low-, intermediate-, and high-risk groups32. The ARL-IPI based on the baseline characteristics of ECOG PS, LDH level, stage, number of involved extranodal sites and an HIV score that incorporates base-line CD4 count, HIV viral load and prior history of AIDS. Barta SK et al. found that the ARL-IPI performed significantly better in predicting OS than the age-adjusted IPI32. Our analysis showed that CNS involvement (HR 3.23, 95% CI 1.38–7.53, p = 0.007) was independent risk factors for adverse prognosis based on PFS for HIV-DLBCL and HIV-BL patients. In HIV-BL patients, B symptoms and CD4 count < 0.100 × 109/L were independent risk factors for adverse prognosis.
Numerous studies have shown that CODOX-M/IVAC chemotherapy, in addition to rituximab, is a feasible and efficient treatment for HIV-BL33. It has also been discovered that DA-EPOCH-R is a good substitute with similar survival rates31. When there are obvious brain metastases, this regimen cannot be administered since the cytotoxic drugs in R-EPOCH do not penetrate the blood-brain barrier; instead, regimens that include CNS therapy are better in this circumstance. None of the 22 patients in our cohort who received DA-EPOCH treatment experienced CNS relapse, despite a previous retrospective research indicating a greater risk of CNS recurrence when this treatment was used15. The most widely used front-line regimens in HIV-DLBCL were CHOP-based regimens (42%), while a sizable minority (25% DA-EPOCH ± R) received higher intensity regimens. This was probably caused by findings indicating that, in HIV-DLBCL, DA-EPOCH-R compared favorably to R-CHOP11,12. The objective response rate was 58% vs. 57% in our trial, which did not show any significant treatment response between CHOP ± R and DA-EPOCH ± R. However, DA-EPOCH ± R compared favorably to CHOP ± R in terms of survival rate (57% vs. 44%).
Limitations of the study
One of the study’s shortcomings is its retrospective design, which has biases by nature. Furthermore, this real-world study comprised low- and middle-income populations with lower popularization of rituximab, partly owing to the treatment resources, supportive care, and patient affordability in developing countries. Other nations and areas with inadequate or unequal resources face the same problem, which may be a reflection of differences in treatment philosophies and socioeconomic circumstances.
Conclusions
In conclusion, this study examining real-world Chinese data on HIV-BL and DLBCL showed the majority of patients were on ART concurrently to the lymphoma diagnosis. Due to the extremely low percentage of patients receiving ART prior to the lymphoma diagnosis, the high percentage of patients with poor PS, and the advanced stage at diagnosis, our study’s survival results were worse than those of industrialized nations. Furthermore, our research indicated that B symptoms and a low CD4 count predicted poor OS and PFS in HIV-BL patients, and CNS involvement predicted poor PFS in HIV-DLBCL and BL patients.
Data availability
Data are available upon request from the znact1936@126.com.
References
Cao, W., Hsieh, E. & Li, T. Optimizing treatment for adults with HIV/AIDS in China: Successes over two decades and remaining challenges. Curr. HIV/AIDS Rep. 17 (1), 26–34 (2020).
Yarchoan, R. & Uldrick, T. S. HIV-associated cancers and related diseases. N Engl. J. Med. 378 (11), 1029–1041 (2018).
Carbone, A., Vaccher, E. & Gloghini, A. Hematologic cancers in individuals infected by HIV. Blood 139 (7), 995–1012 (2022).
Aboulafia, D. M. Non-Hodgkin lymphoma in people with HIV. Lancet HIV. 6 (4), e209–e210 (2019).
Borges, Á. H. Combination antiretroviral therapy and cancer risk. Curr. Opin. HIV AIDS. 12 (1), 12–19 (2017).
Hernández-Ramírez, R. U., Shiels, M. S., Dubrow, R. & Engels, E. A. Cancer risk in HIV-infected people in the USA from 1996 to 2012: A population-based, registry-linkage study. Lancet HIV. 4 (11), e495–e504 (2017).
AIDS-defining Cancer Project Working Group of IeDEA, COHERE in EuroCoord. Non-hodgkin lymphoma risk in adults living with HIV across five continents. AIDS 32 (18), 2777–2786 (2018).
Wang, C., Liu, J. & Liu, Y. Progress in the treatment of HIV-associated lymphoma when combined with the antiretroviral therapies. Front. Oncol. 11, 798008 (2022).
Wang, C. et al. Impact of initial chemotherapy cycles and clinical characteristics on outcomes for HIV-associated diffuse large B cell lymphoma patients: The Central and Western China AIDS Lymphoma League 001 study (CALL-001 study). Front. Immunol. 14, 1153790 (2023).
Wang, C. et al. Clinical characteristics and outcomes of newly diagnosed patients with HIV-associated aggressive B-cell NHL in China. J. Cell. Mol. Med. 26 (19), 5067–5077 (2022).
Barta, S. K., Lee, J. Y., Kaplan, L. D., Noy, A. & Sparano, J. A. Pooled analysis of AIDS malignancy consortium trials evaluating rituximab plus CHOP or infusional EPOCH chemotherapy in HIV-associated non-Hodgkin lymphoma. Cancer 118 (16), 3977–3983 (2012).
Barta, S. K. et al. Treatment factors affecting outcomes in HIV-associated non-hodgkin lymphomas: A pooled analysis of 1546 patients. Blood 122 (19), 3251–3262 (2013).
Lim, K. J. C. et al. Outcomes of human immunodeficiency virus-associated Burkitt lymphoma and diffuse large B-cell lymphoma treated in Australia: A report from the Australasian Lymphoma Alliance. Br. J. Haematol. 201 (5), 865–873 (2023).
Opie, J., Antel, K., Koller, A. & Novitzky, N. In the South African setting, HIV-associated Burkitt lymphoma is associated with frequent leukaemic presentation, complex cytogenetic karyotypes, and adverse clinical outcomes. Ann. Hematol. 99 (3), 571–578 (2020).
Alderuccio, J. P. et al. HIV-associated Burkitt lymphoma: Outcomes from a US-UK collaborative analysis. Blood Adv. 5 (14), 2852–2862 (2021).
Roschewski, M. et al. Multicenter study of risk-adapted therapy with dose-adjusted EPOCH-R in adults with untreated Burkitt lymphoma. J. Clin. Oncol. 38 (22), 2519–2529 (2020).
Spina, M. et al. Rituximab plus infusional cyclophosphamide, doxorubicin, and etoposide in HIV-associated non-Hodgkin lymphoma: Pooled results from 3 phase 2 trials. Blood 105 (5), 1891–1897 (2005).
Kaplan, L. D. et al. Rituximab does not improve clinical outcome in a randomized phase 3 trial of CHOP with or without rituximab in patients with HIV-associated non-hodgkin lymphoma: AIDS-Malignancies Consortium Trial 010. Blood 106 (5), 1538–1543 (2005).
Wei, K. C. et al. Pneumocystis Jirovecii pneumonia in HIV-uninfected, rituximab treated non-Hodgkin lymphoma patients. Sci. Rep. 8 (1), 8321 (2018).
Noy, A. Optimizing treatment of HIV-associated lymphoma. Blood 134 (17), 1385–1394 (2019).
Therasse, P. et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J. Natl. Cancer Inst. 92 (3), 205–216 (2000).
Cheson, B. D. et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J. Clin. Oncol. 32 (27), 3059–3067 (2014) (European Mantle Cell Lymphoma Consortium; Italian Lymphoma Foundation; European Organisation for Research; Treatment of Cancer/Dutch Hemato-Oncology Group; Grupo Español de Médula Ósea; German High-Grade Lymphoma Study GroupNCIC Clinical Trials Group; Nordic Lymphoma Study Group).
Sehn, L. H. et al. The revised international prognostic index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood 109 (5), 1857–1861 (2007).
Olszewski, A. J. et al. Burkitt lymphoma international prognostic index. J. Clin. Oncol. 39 (10), 1129–1138 (2021).
Xiong, Y. et al. The safety and efficacy of PD-1 inhibitors in patients with advanced cancers and HIV/AIDS in China. Front. Oncol. 13, 1248790 (2023).
Magnusson, T. et al. Clinical features, treatments and outcomes of HIV associated diffuse large B-cell lymphoma: A single-center experience. Blood 136, 20 (2020).
Schommers, P. et al. Survival of AIDS-related diffuse large B-cell lymphoma, Burkitt lymphoma, and plasmablastic lymphoma in the German HIV lymphoma cohort. Br. J. Haematol. 168 (6), 806–810 (2015).
Besson, C. et al. ANRS-CO16 LYMPHOVIR Cohort. Outcomes for HIV-associated diffuse large B-cell lymphoma in the modern combined antiretroviral therapy era. AIDS 31 (18), 2493–2501 (2017).
Coutinho, R. et al. HIV status does not impair the outcome of patients diagnosed with diffuse large B-cell lymphoma treated with R-CHOP in the cART era. AIDS 28 (5), 689–697 (2014).
Evens, A. M. et al. Burkitt lymphoma in the modern era: real-world outcomes and prognostication across 30 US cancer centers. Blood 137 (3), 374–386 (2021).
Sparano, J. A. et al. Response-adapted therapy with infusional EPOCH chemotherapy plus rituximab in HIV-associated, B-cell non-Hodgkin’s lymphoma. Haematologica 106 (3), 730–735 (2021).
Barta, S. K. et al. A new prognostic score for AIDS-related lymphomas in the rituximab-era. Haematologica 99 (11), 1731–1737 (2014).
Atallah-Yunes, S. A., Murphy, D. J. & Noy, A. HIV-associated Burkitt lymphoma. Lancet Haematol. 7 (8), e594–e600 (2020).
Acknowledgements
The authors acknowledge the the patients, investigators, and staff at the Zhongnan Hospital of Wuhan University for their support.
Funding
This study was funded by the Center for AIDS Research, Wuhan University (PTPP2023002).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation were by Yu.X., W.L., X.C., data collection were by Yu.X., P.M., and analysis were performed by W.L., L.D., Yo.X. The first draft of the manuscript were written by L.D., Y.Z. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xiong, Y., Liu, W., Chen, X. et al. Survival of HIV associated diffuse large B-cell lymphoma and Burkitt lymphoma in China. Sci Rep 14, 30397 (2024). https://doi.org/10.1038/s41598-024-80749-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-80749-9