Abstract
Occlusal stresses on the tooth and implant are critical in determining their prognosis. When the abutment and implant collar have different diameters, the occlusal stresses are transmitted to the implant’s central axis, reducing their impact on the tissue surrounding it.The objectives of this study was to use finite element analysis (FEA) to study the effect of occlusal pressures on the bone surrounding natural teeth and implants fitted with platform-matched and platform-switched abutments. Three models were developed: Model 1 representing a normal tooth, Model 2 represents an implant with a platform-matched abutment, and Model 3 represents an implant with a platform-switched abutment. Each model received a 100 N perpendicular concentrated load, and the resulting Von Mises stress distribution was evaluated. The results showed that occlusal stresses on implants were much higher than those on natural teeth, with platform-matched implants having the greatest stress values. Platform-switched implants transmitted less stress to the peri-implant bone than platform-matched implants, indicating that platform switching decreases occlusal pressures while preserving peri-implant bone levels. The study indicated that platform-switched abutments may extend the life of osseointegrated implants by reducing bone stress, while simultaneously emphasizing the protective role of the periodontal ligament in natural teeth.
Similar content being viewed by others
Introduction
During mastication, the periodontal ligament fibers transfer the occlusal stresses from the teeth to the alveolar bone beneath. These occlusal stresses are crucial for both the resorption and formation of alveolar bone. An increase in the occlusal stresses may accelerate the alveolar bone resorption around the teeth1,2,3,4.
It has been challenging to study the impact of occlusal stresses on the health of periodontal tissues. Several studies were conducted to study the effect of the occlusal stresses on the periodontal tissues during mastication. However, the observations of these studies are either contradictory or inconclusive5,6.
Dental implants are rapidly becoming the choice of treatment for replacement of missing teeth. The occlusal stresses acting on the implant are critical for preserving its integrity and the health of the surrounding tissues. The absence of the periodontal ligament in an osseointegrated implant subjects it, to increased occlusal stresses which are directly transmitted to the underlying alveolar bone. Increased occlusal forces have the potential to cause implant failure by causing fractures and peri-implant bone loss7.
The level of the peri-implant bone determines the success of an osseointegrated implant. A radiographic marginal bone loss of 1.5 mm in the first year and less than or equal to 0.2 mm in each subsequent year are traditionally considered to be significant parameters for evaluating implant success8. Among the elements influencing the peri-implant bone level are occlusal stresses, the position, size and shape of the implant—abutment microgap, the biologic width around the implant, and microbial contamination of the tissues surrounding the implant9. To reduce peri-implant bone loss, it is essential to comprehend the masticatory system and the biomechanical behavior of each implant rehabilitation component, as the occlusal loads imparted to the implant have an impact on the bone tissues. Abutment design, implant diameter and length, bone quality, and implant material are some of the variables that influence implant stability or result in marginal bone loss. Therefore, a patient’s long-term therapeutic outcome is positively impacted by selecting the appropriate abutment10. Maintaining the peri-implant bone levels has been suggested through the use of wider diameter implants with smaller abutments (platform switching concept), surface treatment of implants, and improvements to the implant abutment connection to reduce the microgap between the implant and the abutment11,12,13,14.
The long-term success of dental implants is dependent on structural and functional osseointegration between the implant and the surrounding intraoral tissues. It has been discovered that the proposed model is particularly beneficial for highlighting biomechanical phenomena in the bone-implant interface that play an important role in bone loss surrounding the dental implant. Furthermore, the observed results aim to provide enhanced understanding to designers in biomedical engineering and dentistry15.
Platform switching, which supports using a smaller diameter abutment on a larger diameter implant collar, causes the perimeter of the implant abutment junction (IAJ) to shift inward towards the implant’s central axis (i.e., the middle). This maintains biologic width, reduces microgaps on the crestal bone, and reduces occlusal pressures in the peri-implant bone, resulting in preserving its level16,17.
Mechanical testing methods namely: photoelasticity, strain gauge-based measurements, optic measurement as well as numerical / computational approaches have been used to study the effect of stresses18,19. Finite element analysis (FEA) is the commonly used computational technique for analysis of stresses acting on the hard tissue models like teeth including dental restorations, implants, etc20,21,22,23,24,25.
It delivers detailed quantitative data on stresses at every position in the mathematical model. Specific tools, like as ANSYS software, can visualize the distribution of such data across models26,27.
To our knowledge, no study has been done to compare the occlusal stresses on natural tooth and implants fitted with platform-matched and platform-switched abutments till date. As a result, the current study was conducted using Finite Element Analysis to compare the effects of occlusal stresses on bone around natural tooth and implants fitted with platform matched and platform switched abutments.
The current study’s objective include
To use FEA to assess and compare the occlusal stresses on the bone around a natural tooth, an implant with platform matched and platform switched abutment design (1 mm platform switching).
Materials and methods
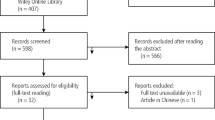
This in vitro study was carried out in accordance with Helsinki’s International Standards and Ethical Directives. The information and confirmation principles for research purposes were strictly adhered to; signed informed consent for study inclusion was obtained for tooth collection. The study procedure was approved by the Institutional Review Board and Ethical approval committee at King Khalid University, College of Dentistry, Abha, Saudi Arabia (IRB/KKUCOD/ETH/2021-22/036). Figure 1 shows the flow chart that outlines the study methodology and the steps involved in FEA.
A natural tooth (mandibular first molar Fig. 2) was used, to assess the occlusal stresses around natural tooth. An implant of size 5 mm (width) × 10 mm (length) with a surface screw structure, Implant abutment connection with diameter 5 mm (Platform matched) and 4 mm (Platform switched), Abutment screw and Hex Driver was used. The first model represented a simulated 5 mm diameter abutment connection (Platform matched model), while the second model represented a platform switched model configuration with a 4 mm diameter abutment connection (Fig. 3).
Geometric model development
The mandibular first molar, implant and abutments were scanned with a white light scanner (Hexagon WLS400M) which was the first step in construction of 3D geometric models. Then the point cloud data generated for individual parts was utilized to create 3D models with SOLIDWORKS 3D CAD solutions. Three such models were produced. Model 1 depicted the mandibular first molar, a natural tooth; Model 2 showed an implant with a platform-matched abutment with an appropriate crown; and Model 3 showed an implant with a platform-switched abutment with an appropriate crown. To create the appropriate FEA model, the models were subsequently processed by ANSYS R15.0 software (Swanson Analysis System, Houston, PA, USA).
Behaviour and properties of physical model
Table 1 presents the material properties for bone and implant that were designed based on a previous study28. These material properties were assigned by ANSYS R15.0 software (Swanson Analysis System, Houston, PA, USA).
Following that, 100 N of perpendicular concentrated load was given to the three models: mandibular first molar, implant with platform matched, and platform switched abutment. The data were acquired in the form of Von Mises stresses portrayed as colour coded contour maps, with each contour representing a specific magnitude of the stress applied individually to the various components investigated. The minimum, maximum and average equivalent Von Mises stress values were recorded for each model (Figs. 4, 5 and 6)
Results
The observation of equivalent Von Mises stress distribution in the three models: Model-1, Model-2 and Model-3 were recorded and tabulated. Table 2 depicts the equivalent Von Mises stress values in Model-1 natural tooth-mandibular first molar. Table 3 depicts the equivalent Von Mises stress values in Model-2 implant fitted with platform matched abutment. Table 4 depicts the equivalent Von Mises stress values in Model-3 implant fitted with platform switched abutment.
Table 5 depicts the comparison of average equivalent Von Mises Stress values around Natural Tooth, Implant with Platform Matched and Switched abutment.
It was seen that, the overall average stress values were higher in the Model-2 implant fitted with platform matched abutment (9.5E-01) as compared to the Model-1 natural tooth (2.98E-01) and Model-3 implant fitted with platform switched abutment (8.84E-01). The average stress values on the cancellous bone were similar in Model-1 (1.65E-01) and Modal-3 (1.65E-01) with slightly higher values for Model-2 (1.69E-01). The cortical bone stress values were higher in Model-2 (7.09E-01) and Model-3 (7.05E-01) as compared to Model-1 (4.08E-01).
When the average stresses values for Crown, Titanium implant, abutment and screw were compared, it was observed that the values were higher in the Model-2 indicating that the stresses induced in the implant fitted with platform matched abutment were considerably higher as compared to implant fitted with platform switched abutment. However, when compared to Model-1 natural tooth mandibular first molar, both Model-2 and Model-3 experienced higher stress values. These observations suggest the role of periodontal ligament as a shock absorber and thereby reducing the occlusal stresses acting on the underlying alveolar bone.
Discussion
The occlusal stresses acting on the tooth and implant are critical in determining the prognosis of both. Excessive occlusal forces can lead to resorption of the alveolar bone supporting the teeth and also the implant resulting in loss of tooth and implant failure29. Due to excessive occlusal stresses, there is loss of peri-implant bone on the facial as well as interproximal aspects of the implant supported crowns. This leads to loss of peri-implant soft tissue manifesting as root recession and loss of interdental papillae, thereby affecting the esthetic outcome of the implant therapy30.
Attempts have been made in the past for minimizing the effect of increased occlusal stresses on the peri-implant bone by the application of platform switch concept31,32,33,34.
When the abutment and implant collar have different diameters, the occlusal pressures are shifted to the implant’s central axis, lessening the effect on the tissue surrounding the implant11. However when compared to the natural tooth the occlusal forces acting on the alveolar bone surrounding an implant are higher due to the absence of the shock absorption effect of the periodontal ligament.
In the present study, natural tooth mandibular first molar was considered, as it is the tooth that bears the maximum occlusal forces and is the key to occlusion6. Occlusal stress was shown to have greater average stress levels in the cortical bone than in the cancellous bone in the current study. Reddy and Vandana35 used a finite element model (FEM) study to evaluate the stress generated on different periodontal tissues at different occlusal loads. They found that the stresses increased at hyperfunctional load because the bone levels were compromised and the stresses increased as the crest moved apically. Messias et al. in their study has stated that the use of Platform Switched components helps to maintain the peri-implant marginal bone level in patients who need implant-supported restorations in edentulous gaps of the mandible, even though this benefit may not be clinically apparent31.
Studies have been conducted assessing the occlusal stresses in implants with platform matched and platform switched abutments. To the best of our knowledge, no study has been done to compare the occlusal forces acting on natural tooth, implants with platform-matched and platform-switched abutments. Maeda et al.16 reported the beneficial effect of platform switching configuration in implants using 3D finite element analysis. Schrotenboer et al.36 investigated the effects of various abutment diameters and concluded that a smaller abutment diameter resulted in less stress transmitted to the crestal bone. The beneficial effects of platform switching were also reported by Cimen and Yengin37, Bouazza-Juanes et al.38, Sawarkar et al.39 and Khambatta et al.40 .These observations are similar to the present study.
Pessao et al.30 reported that a circumferential mismatch of 0.5 mm in implant diameter and abutment diameter does not significantly affect the biomechanical environment. This observation is in contrast to the present study. In the present study, we observed that mismatch in implant and abutment diameter reduced the average occlusal stresses in the platform switched model as compared to the platform matched model. However, the mismatch in diameter was 1 mm in the present study.
In comparison to standard implants, Markose et al. found that sloping shoulders and platform-switched implant designs resulted in a lower stress value and a more beneficial stress distribution. The results of the study suggested that increasing the implant’s diameter can improve contact between the implant and the bone, which will drastically lower the concentration of stress. This finding are similar to our study were the 1 mm mismatch in diameter was included in the model 341.
A similar finite element study comparing the strain generated in bone on platform-switched and standard implants under vertical and angulated load found that platform switching of dental implants (with an abutment-implant diameter difference of 1 mm) can exhibit the ideal values of microstrain (50–3000 microstrain) and can be considered a better alternative for preventing crestal bone loss when compared to non-platform-switched implants. This finding support the results of our study were platform switching with 1 mm diameter had less stress generated compared to platform matched abutment42.
Considering the constraints of this study, it can be said that the natural tooth can bear the maximum amount of occlusal stress without significantly damaging the alveolar bone underneath. The average occlusal stresses in the implant fitted with platform switched abutment were higher than natural tooth but lower than the implant fitted with platform matched abutments. Although implants are now the preferred method of replacing lost teeth, it is still more important to preserve natural teeth because there is no ideal replacement to natural teeth.
The findings of this study demonstrate that platform-switched abutments reduce occlusal stresses while maintaining peri-implant bone levels by transferring less occlusal forces to the peri-implant bone. This would assist clinicians in considering the use of platform switched abutments design in situations where bone loss surrounding implants is a concern, such as in patients with impaired bone quality or a high risk of peri-implant bone loss. This could be especially helpful for patients who are at a high risk of implant failure, bone loss, or cosmetic issues. Through careful application of the study’s findings, clinicians can give their patients more customized, evidence-based treatment.
Limitations and future research
While this study provides valuable insights into the impact of occlusal stresses, the use of finite element analysis is limited by the assumptions made in the material properties and the applied stress conditions. Even though FEA has many benefits, it also has drawbacks. Since FEA is a computerized approach, its accuracy is reliant on the quality of the input data. The FEA analysis will be inconsistent if the user enters erratic data. In certain situations, design snags will not be seen throughout the FEA process since FEA models are a simplified representation of the actual system. Because of the complexity of performing FEA analysis and interpretation of results, it takes a lot of computing knowledge and involvement to set up and operate.
Future studies could include more complex models that simulate dynamic chewing forces and consider variations in bone quality, implant designs, and patient-specific factors. The study highlights the significance of occlusal stresses in dental implantology, emphasizing the benefits of platform switching in reducing these forces and maintaining peri-implant bone integrity. Further research and clinical trials are necessary to validate these findings in real-world scenarios. For example, the distribution of stress surrounding implants is significantly influenced by differences in bone quality. Individual differences in bone quality that range from less mineralized trabecular bone to dense cortical bone may have an impact on how pressures are transmitted to the implant and surrounding tissues. Stress concentrations at the bone-implant interface may be greater in individuals with low bone quality, which could result in implant failure or bone resorption.
Additionally, the distribution of stress may become variable according to implant designs. The way occlusal stresses are communicated to the bone can be affected by the implant’s geometry and material composition, including characteristics like platform switching. The mechanical behavior of actual implants under dynamic loading circumstances may not be accurately replicated by FEA models, which frequently rely on idealized implant forms and consistent material properties. Differently designed implants, for instance, can change how forces are dispersed along the implant-bone contact, which could either lessen or increase localized stress concentrations. By adding patient-specific elements like unique implant designs, differences in bone quality, and more intricate, dynamic loading scenarios, future research could increase the accuracy of FEA models.
Conclusion
From the observations of this study, it can be concluded that the occlusal stresses acting on an implant are higher than that on a natural tooth. Further, the occlusal stresses on an implant fitted with platform matched abutment are considerably higher than those acting on implant fitted with platform switched abutment. The findings of this study emphasize the importance of selecting the correct abutment design for implant rehabilitation. As, platform switched abutment design has shown lower occlusal stresses, it may be crucial and used in minimizing the possibility of peri-implant bone loss, which would increase the stability and long-term success of osseointegrated implants. This knowledge can be used to design future implants and abutments, giving patients long-lasting results.
Data availability
All data generated or analysed during this study are included in this article.
References
Ispas, A., Craciun, A., Kui, A., Lascu, L. & Constantiniuc, M. Occlusal forces and their transmission to the periodontium. HVM Bioflux. 11(1), 18–21 (2019). http://www.hvm.bioflux.com.ro/docs/2019.18-21.pdf
Fan, J. & Caton, J. G. Occlusal trauma and excessive occlusal forces: Narrative review, case definitions, and diagnostic considerations. J. Periodontol. 89(Suppl. S1), S214–S222. https://doi.org/10.1002/JPER.16-0581 (2018).
Satpathy, M., Duan, Y., Betts, L., Priddy, M. & Griggs, J. A. Effect of bone remodeling on dental implant fatigue limit predicted using 3D finite element analysis. J. Dent. Oral Epidemiol. 2(1). https://doi.org/10.54289/JDOE2200102 (2022).
Sadowsky, S. J. Occlusal overload with dental implants: A review. Int. J. Implant Dent. 5, 29. https://doi.org/10.1186/s40729-019-0180-8 (2019).
Muneer, S. & Vandana, K. L. Effect of different occlusal loads on periodontium: A three-dimensional finite element analysis. CODS J. Dent. 8(2), 78–90. https://doi.org/10.5005/jp-journals-10063-0018 (2016).
Falcinelli, C., Valente, F., Vasta, M. & Traini, T. Finite element analysis in implant dentistry: State of the art and future directions. Dent. Mater. 39(6), 539–556. https://doi.org/10.1016/j.dental.2023.04.002 (2023).
Stilwell, C. Occlusal considerations in maintaining health of implants and their restorations. Br. Dent. J. 236, 773–779. https://doi.org/10.1038/s41415-024-7407-7 (2024).
Albrektsson, T. & Isidor, F. Consensus report of session IV. In (eds. Lang, N. P., Karring, T). Proceedings of the 1st European Workshop on Periodontology 365–369. (Quintessence Publishing, 1994).
Atieh, M. A., Ibrahim, H. M. & Atieh, A. H. Platform switching for marginal bone preservation around dental implants: A systematic review and meta-analysis. J. Periodontol. 81(10), 1350–1366. https://doi.org/10.1902/jop.2010.100232 (2010).
Abdelhak Ouldyerou, A. et al. Functionally graded ceramics (FGC) dental abutment with implant-supported cantilever crown: Finite element analysis. Compos. Commun. 38, 101514 (2023). https://doi.org/10.1016/j.coco.2023.101514
Lazzara, R. J. & Porter, S. S. Platform switching: A new concept in implant dentistry for controlling postoperative crestal bone levels. Int. J. Periodontics Restor. Dent. 26(1), 9–17 (2006).
Insua, A., Galindo-Moreno, P., Miron, R. J., Wang, H. L. & Monje, A. Emerging factors affecting peri-implant bone metabolism. Periodontol 2000 94(1), 27–78. https://doi.org/10.1111/prd.12532 (2024).
Kowalski, J., Lapinska, B., Nissan, J. & Lukomska-Szymanska, M. Factors influencing marginal bone loss around dental implants: A narrative review. Coatings 11, 865. https://doi.org/10.3390/coatings11070865 (2021).
Satpathy, M. Screening dental implant design parameters for effect on the fatigue limit of reduced-diameter implants. Dent. Mater. 41(Issue 4), 444–450. https://doi.org/10.1016/j.dental.2025.02.001 (April 2025).
Merdji, A. et al. Finite-element study of biomechanical explanations for bone loss around dental implants. J. Long-Term Effects Med. Implants. 30(1). https://doi.org/10.1615/JLongTermEffMedImplants.2020035028 (2020).
Maeda, Y., Miura, J., Taki, I. & Sogo, M. Biomechanical analysis on platform switching: Is there any biomechanical rationale. Clin. Oral Implant Res. 18, 581–584. https://doi.org/10.1111/j.1600-0501.2007.01398.x (2007).
Prasad, K. D., Shetty, M., Bansal, N. & Hegde, C. Platform switching: An answer to crestal bone loss. J. Dent. Implant 1, 13–17. https://doi.org/10.4103/0974-6781.76426 (2011).
Dogru, S. C., Cansiz, E. & Arslan, Y. Z. A review of finite element applications in oral and maxillofacial biomechanics. J. Mech. Med. Biol. 18(2), 18300028. https://doi.org/10.1142/S0219519418300028 (2018).
Khaleed, H. M. T. et al. Finite element analysis of nylon based 3D printed autonomous underwater vehicle propeller. Mat. Res. 23(5). https://doi.org/10.1590/1980-5373-mr-2020-0236 (2020).
Gultekin, B. A., Gultekin, P. & Yalcin, S. Application of finite element analysis in implant dentistry. finite element analysis: New trends and developments. Rijeka, Croatia: Tech Publishing 10, 21–54 https://doi.org/10.5772/48339 (2012).
Ibrahim, C. R., Sameh, A. & Askar, O. A finite element analysis study on different angle correction designs for inclined implants in All-On-Four protocol. BMC Oral Health 24, 331. https://doi.org/10.1186/s12903-024-04091-2 (2024).
Yudistiro, D. & Cheng, Y. C. Optimization and innovative design of dental implants under dynamic finite element analysis. J. Chin. Inst. Eng. 46(6), 615–627. https://doi.org/10.1080/02533839.2023.2227878 (2023).
Yang, F. et al. Three-dimensional finite element analysis of the biomechanical behaviour of different dental implants under immediate loading during three masticatory cycles. Heliyon 10(11), e32616 https://doi.org/10.1016/j.heliyon.2024.e32616 (2024).
Satpathy, M., Pham, H. & Shah, S. Material properties and finite element analysis of adhesive cements used for zirconia crowns on dental implants. Comput. Methods Biomech. Biomed. Eng. 17, 1–21. https://doi.org/10.1080/10255842.2024.2404152 (2024).
Kim, J. W., Vo, T. V., Satpathy, M. & Malyala, R. Improving fracture resistance of 5Y-PSZ-based three-unit bridge prostheses. Int. J. Prosthodont. 37(6), 650–658. https://doi.org/10.11607/ijp.8643 (2024).
Chopade, S. R., Madhav, V. V. & Palaskar, J. Finite element analysis: New dimension in prosthodontic research. J. Dent. Allied Sci. 3, 85–88. https://doi.org/10.4103/2277-4696.159089 (2014).
Panna, R., Podar, A., Miglani, A. & Dhingra Finite element analysis ̵ an insight. Indian J. Dent. Sci. 1, 151–154 (2014).
Satoh, T., Maeda, Y. & Komiyama, Y. Biomechanical rationale for intentionally inclined implants in the posterior mandible using 3D finite element analysis. Int. J. Oral Maxillofac. Implants. 20, 533–539 (2005).
Agrawal, R. et al. Influence of occlusal bite forces on teeth with altered periodontal support: A three-dimensional finite element stress analysis. J. Pharm. Bioall Sci. 13, S688–S691. https://doi.org/10.4103/jpbs.JPBS_785_20 (2021).
Pessoa, R. S. et al. Biomechanical evaluation of platform switching: Different mismatch sizes, connection types, and implant protocols. J. Periodontol. 85(9), 1–11. https://doi.org/10.1902/jop.2014.130633 (2014).
Messias, A. et al. Peri-implant marginal bone loss reduction with platform-switching components: 5-Year post-loading results of an equivalence randomized clinical trial. J. Clin. Periodontol. 46, 678–687. https://doi.org/10.1111/jcpe.13119 (2019).
Canullo, L., Fedele, G. R., Iannello, G. & Jepsen, S. Platform switching and marginal bone-level alterations: The results of a randomized-controlled trial. Clin. Oral Implant Res. 21, 115–121. https://doi.org/10.1111/j.1600-0501.2009.01867.x (2010).
Iezzi, G. et al. Histological and histomorphometrical analysis on a loaded implant with Platform-Switching and conical connection: A case report. J. Oral Implantol. 43, 180–186. https://doi.org/10.1563/aaid-joi-d-16-00182 (2017).
Rocha, S. et al. Effect of platform switching on crestal bone levels around implants in the posterior mandible: 3 years results from a multicentre randomized clinical trial. J. Clin. Periodontol. 43, 374–382 (2016).
Reddy, R. T. & Vandana, K. L. Effect of hyperfunctional occlusal loads on periodontium: A three-dimensional finite element analysis. J. Indian Soc. Periodontol. 22, 395–400. https://doi.org/10.4103/jisp.jisp_29_18 (2018).
Schrotenboer, J., Tsao, Y. P., Kinariwala, V. & Wang, H. L. Effects of microthreads and platform switching on crestal bone stress. J. Periodontol. 79, 2166–2172. https://doi.org/10.1902/jop.2008.080178 (2008).
Cimen, H. & Yengin, E. Analyzing the effects of the platform-switching procedure on stresses in the bone and implant-abutment complex by 3-dimensional Fem analysis. J. Oral Implantol. 38(1), 21–26. https://doi.org/10.1563/AAID-JOI-D-10-00033 (2012).
Bouazza-Juanes, K., Martínez-González, A., Peiro, G., Rodenas, J. J. & López-Molla, M. V. Effect of platform switching on the peri-implant bone: A finite element study. J. Clin. Exp. Dent. 7(4), e483–488. https://doi.org/10.4317/jced.52539 (2015).
Sawarkar, M. S. & Sanadi, R. M. Comparison of biomechanical effects of platform switching on peri-implant bone using finite element analysis: An in vitro study. Int. J. Rec Sci. Res. 12(08), 42699–42703. https://doi.org/10.24327/ijrsr.2021.1208.6135 (2021).
Khambatta, X., Sanadi, R. M., Pillai, M. & Sawarkar, M. Evaluation and comparison of crestal bone changes in patient with implant supported prostheses fitted with conventional abutments and platform switched abutments. Int. J. Recent. Sci. Res. 8(11), 21856–21860. https://doi.org/10.24327/ijrsr.2017.0811.1155 (2017).
Markose, J. et al. Comparison of platform switched and sloping shoulder implants on stress reduction in various bone densities: Finite element analysis. J. Contemp. Dent. Pract. 18(6), 510–515. https://doi.org/10.5005/jp-journals-10024-2075 (2017).
Paul, S., Padmanabhan, T., Swarup, S. & & Comparison of strain generated in bone by platform-switched and non-platform-switched implants with straight and angulated abutments under vertical and angulated load: A finite element analysis study. Indian J. Dent. Res. 24, 8–13. https://doi.org/10.4103/0970-9290.114913 (2013).
Acknowledgements
This study was financially supported by Research Grant from the Deanship of Scientific Research of King Khalid University, Abha, Saudi Arabia. The authors extend their appreciation to the Deanship of Research and Graduate Studies at King Khalid University, for funding this work through large research project under grant number (RGP2/491/46).
Funding
This study was financially funded by Research Grant (RGP2/491/46) from the Deanship of Scientific Research of King Khalid University, Abha, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
Concepts, design and literature review was done by Mukhatar Ahmed Javali , Rizwan M Sanadi, Irfan Anjum Badruddin, Saad M AlQahtani, Mohasin Abdul Khader, Weam Sharif Abdelrazaq Ibrahim, Imran Khalid. Author Mukhatar Ahmed Javali and Rizwan M Sanadi were involved in the data acquisition and analysis. Statistical analysis and manuscript preparation was done by author Mukhatar Ahmed Javali, Rizwan M Sanadi and Mohasin Abdul Khader. Manuscript editing, review was done Mukhatar Ahmed Javali , Rizwan M Sanadi, Irfan Anjum Badruddin, Saad M AlQahtani, Mohasin Abdul Khader, Weam Sharif Abdelrazaq Ibrahim, Imran Khalid.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocols were approved by the Institutional Review Board and Ethical approval committee at King Khalid University, College of Dentistry, Abha, Saudi Arabia (IRB/KKUCOD/ETH/2021-22/036) and informed consent was taken from the participants.
Consent for publication
All authors have read and approved the manuscript and agree with submission to Results in engineering.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Javali, M.A., Sanadi, R.M., Badruddin, I.A. et al. Comparative analysis of occlusal stresses on bone around natural teeth, platform matched and switched implants abutments: a finite element study. Sci Rep 15, 19541 (2025). https://doi.org/10.1038/s41598-025-02570-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02570-2
Keywords
This article is cited by
-
Comparative study by FEM of different liners of a transfemoral amputated lower limb
Scientific Reports (2025)