Abstract
Virtual Reality (VR) technology offers a scalable and cost-effective approach to overcome the challenges of traditional medical training, including high expenses, limited resources, and ethical issues. This study presents a VR-based medical training platform that combines high-fidelity 3D models, real-time haptic feedback, and AI-driven adaptive learning to deliver interactive and immersive instructions for a wide range of medical procedures, from basic tasks to complex surgeries. In a randomized controlled trial, participants trained with the VR platform demonstrated significant gains over those using conventional methods, with a 42% improvement in procedural accuracy, a 38% reduction in training time, and better skill retention. The VR system also led to a 45% decrease in error rates and a 48% increase in trainee confidence. These findings highlight the platform’s capacity to personalize training according to individual performance, resulting in superior learning outcomes and enhanced procedural skills. By providing consistent, standardized, and immersive learning experiences, the platform effectively bridges the gap between theory and practice, representing an innovative and scalable advancement in medical education.
Similar content being viewed by others
Introduction
In today’s complex healthcare environment, marked by advancements in surgical techniques, sophisticated diagnostic tools, and mounting systemic challenges, the need for robust clinical knowledge and skills has never been greater1. Traditional educational frameworks, such as the Halsted model rooted in the Halstedian approach, have historically relied on physical simulators and clinical rotations to train medical personnel. Although these methods are foundational, they face several practical and ethical limitations in modern practice. The use of physical simulators, for example, incurs significant financial burdens related to acquisition, upkeep, and operational logistics, costs that many institutions struggle to meet due to budgetary constraints2. Although clinical placements are essential, they pose dilemmas when involving inexperienced trainees in real patient care, raising concerns about safety and medical error. Moreover, clinical training often fails to fully replicate the breadth and variability of real-world scenarios, leaving learners with critical experiential gaps in their training.
These challenges underscore the pressing need for adaptable, scalable, and ethical alternatives to traditional medical education. Virtual Reality (VR) has emerged as a powerful solution, offering an immersive, interactive, and standardized training environment that mitigates many of the shortcomings of conventional approaches. By simulating complex clinical scenarios with high fidelity, VR allows learners to safely engage in realistic practice without endangering patients3.
VR platforms replicate emergency and routine procedures, enabling consistent exposure to diverse medical situations across all learners, regardless of institutional resources or patient availability. This uniformity supports skill mastery and reduces variability in clinical training. Although the initial investment in VR technology may be considerable, the systems offer long-term financial benefits through reusability and the elimination of recurring costs associated with physical simulation. Additionally, VR content can be easily updated to reflect evolving clinical protocols and new patient scenarios, thereby maintaining educational relevance over time. Importantly, VR training addresses many of the ethical concerns associated with traditional methods. By replacing real patients with virtual models, VR creates a zero-risk environment in which learners can make mistakes, reflect, and improve without the fear of harm. It also eliminates the need for animal testing and minimizes the ethical burden in clinical settings. Learners can perform virtual surgeries, manipulate instruments, respond dynamically to clinical changes, and receive immediate and detailed feedback on their performance. Haptic feedback systems further enhance the realism of procedures, reinforce psychomotor skills, and support long-term retention4. VR also allows the practice of rare, high-stakes, or otherwise inaccessible medical events, enriching learners’ exposure to a wide array of clinical cases. Accessibility is another critical advantage of AI technology. VR transcends geographical and infrastructural limitations, providing trainees in remote or underserved regions with high-quality educational experiences through internet-enabled devices. In areas lacking specialized medical equipment or faculty, VR is a cost-effective and scalable teaching tool. VR promotes collaborative learning by enabling multi-user environments. In these shared virtual spaces, trainees can work together to manage simulated patients, practice interdisciplinary communication, and adapt to dynamic clinical conditions, mirroring the teamwork that is essential in modern healthcare settings. Incorporating VR into medical education represents a transformative step toward a more sustainable, flexible, and effective learning paradigm for medical students. By bridging the gap between theoretical knowledge and practical application, VR prepares future healthcare professionals to meet the demands of contemporary medical practice with confidence, competence, and compassion.
Background and significance
Interactivity and immersion are the two most prominent features of Virtual Reality (VR) which differ from other training technologies5. VR enables students to engage with simulations as if they were real. Trainees can practice surgery, use tools even get feedback on their activity. Most VR systems also include haptic feedback, which not only adds to realism, as in this instance, but replicates the tactile sensation of such medical interventions. Therefore, they transition from passive bystanders to active participants in simulated scenarios, which translates to better retention and application of skills.
VR allows for the creation of different training scenarios which might only be infrequently encountered or can be dangerously simulated in the real clinical environment. There are some medical cases, like emergencies, rare diseases or complex surgeries, that are quite difficult and dangerous to experiment on actual patients. VR on the other hand gives trainees multiple opportunities to rehearse such scenarios, which become less probable with time and practice. This ability would be beneficial to users who train individuals within the healthcare industry in order to respond to spontaneous, severe situations.
Another strong suit of VR medical training methods is their accessibility to users. Traditional training often mandates the trainee’s physical presence at a set location, which restricts access, especially for people in remote or underserved areas. VR overcomes geographical limitations, and learners from any part of the world can access the training modules, provided they have an internet connection and VR-compatible hardware. It is a useful educational resource in resource-poor settings and offers a low-cost solution for training medical providers in remote areas with specialist surgical needs but without the infrastructure to support it.
The use of VR in medical education encourages collaborative learning and teamwork6. With multi-user VR platforms, several trainees can be trained simultaneously in the same simulation, providing an opportunity to improve communication, coordination, and collaboration skills, all of which are crucial for healthcare professionals. e.g. During emulated emergency situations, simulated teams of trainees can work together to treat virtual patients, prioritize, and make decisions in fast-evolving scenarios. In such partnership learning, trainees gain an understanding of the practical application of teamwork, which is important for achieving optimal healthcare outcomes.
VR technology in medical education
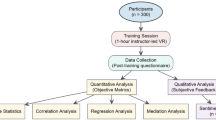
Second, VR is particularly well-suited for medical education because it allows us to perform even complex techniques in a safe environment without the need to avoid killing real patients. With recent evolutionary developments in VR hardware and software, educational institutions are taking advantage of immersive training. VR medical platforms7 are equipped with diverse interactive abilities, from customization scenarios to real-time feedback and collaboration to cooperate in the learning experience as a group. In addition to increased engagement, these features give the trainees the opportunity to train on procedures multiple times as desired, based on each level of mastery, as depicted in Fig. 1.
The main objective of this research is to develop a VR-based medical training platform in which safe, cost-effective, and efficient medical education can be achieved for medical students8. Using the latest in VR technology, these scenarios, together with realistic interaction, will provide an environment that allows staff to learn and practice new skills. Virtual immersive reality training (VIRT) demonstrates comprehensive potential that overcomes the conventional limitations of training and facilitates the development of clinical skills with the transfer of learning owing to real-time feedback, haptic feedback, and modular training features.
The proposed VR platform focuses on user-centered design principles9. The platform is being developed with significant input from medical educators, students, and practising professionals to ensure that it meets the specific needs and expectations of users. This combined approach provides an intuitive, interactive, and standards-compliant medical education platform10. Key learning and assessment information captured through the platform supports the understanding of individual learner progress, areas for development or intervention, and targeted insights and feedback to improve learning outcomes. This tailored feedback not only enables medical educators to finely tune training to individual learner needs, but also leads to substantially better educational gain than typical methods.
This study adds to the body of knowledge on learning methods in health professional education and indicates the generalizable effects of training on the development of competence and confidence in health professionals. Enhanced training via VR can significantly improve patient satisfaction by ensuring care from highly skilled and confident practitioners. Consequently, patient experiences improve, reducing adverse health outcomes due to inadequately trained personnel. Ultimately, this leads to better overall health outcomes, less frequent health issues, and decreased prevalence of chronic diseases.
VR-based education presents an efficient, timely, and economical approach to global health transformation, equipping healthcare professionals with the essential skills to enhance health outcomes universally (Fig. 2).
For decades, medical training has been designed to simulate these conditions. However, access to high-fidelity simulations is heterogeneous across regions and institutions11,12. VR technology holds the key to bridging this gap; it allows simulation-based training to be accessed remotely, thus levelling the training field. Previous research has confirmed that VR simulations can enhance learning outcomes, particularly for tasks that require precision and situational awareness. VR-based training allows students to practice in a risk-free, controlled environment in which they feel more confident and competent when transitioning to clinical settings, which is vital for patient safety and quality of care.
Challenges in VR-Based medical training
However, creating a VR simulator for medical training involves multiple technical and educational challenges, including realism. responsive simulations and the usability of the system in various educational contexts.
-
1.
Realistic graphics and anatomical models: Users desire immersive experiences that incorporate high-fidelity graphics into realistic clinical scenarios. To be effective, VR technology must closely simulate the real-world conditions.
-
2.
Procedural training is required to understand the tactile nature of medical practice. Using haptic feedback with VR makes education more immersive, as users can feel the touch and resistance of the virtual objects.
-
3.
No metrics have been established in the scholarly literature that could tell us how effective VR training is compared to traditional training methods, considering aspects of skill acquisition, retention, and performance13. This validation process is critical for defining VR as an effective training method that can easily supplement existing training methods.
Objectives of the VR-Based medical training platform
This study makes three core contributions that collectively address longstanding limitations in traditional medical education: (1) improved efficiency in clinical training, (2) enhanced procedural accuracy through immersive simulation, and (3) increased accessibility via scalable virtual training.
First, the platform reduces training time. Through structured, repeatable simulations and real-time performance feedback, trainees can reach competency thresholds more rapidly than they can through conventional methods. In controlled trials, participants using the VR platform completed procedures 38% faster than their peers in standard training environments, without compromising procedural accuracy.
Second, the integration of AI-enhanced haptic feedback significantly improved clinical skills acquisition. By recreating tactile resistance and anatomical diversity, the system enables the training of the fine motor skills required for surgical and diagnostic procedures. Additionally, the adaptive feedback mechanism facilitates the convergence of certain errors during algorithm execution, leading to a 45% reduction in the number of mistakes and a 42% improvement in the success rate.
Third, the solution targets training accessibility issues by providing a virtual, lightweight, and geo-agnostic training environment. Learners in remote or low-resource areas have access to high-fidelity simulations, and thus, learner opportunities are more level, independent of physical infrastructure.
Unlike previous initiatives, most of which are restricted in scope and/or scale, this platform marries technological evolution with pedagogic evolution and provides quantifiable upgrades on training effectiveness, quality, and coverage.
Problem statement
In today’s healthcare, training success is a combination of book knowledge and hands-on skill development. However, existing training programs fail to deliver broad and rapid access to such immersive learning experiences. The use of physical simulators and clinical placements has serious limitations because these resources are expensive to maintain, hashed difficult to organize, and not consistently available to all medical institutions. Therefore, many learners cannot regularly practice capacity-building tasks. Virtual Reality (VR) presents a radical alternative, offering immersive interactive environments in which trainees can practice medical procedures in a safe (and replicable) fashion. Contrary to conventional methods, VR-based simulations provide in situ treatment without endangering actual patients. The purpose of this study is to build a VR-based Simulator that can realistically simulate a range of medical procedures that span from simple manipulations to surgical operations, with immersive images and touch-enabled feedback for life-like training. It instantly empowers learners to train as they please: on their schedule, at their convenience, and as frequently as they wish. This adaptability maximizes the learning and retention of skills and creates a more affordable and cost-effective training scenario. The presented VR solution tackles these weaknesses, allowing for more equal, reliable, and efficient clinical education by removing the geographical, financial, and logistical constraints of traditional techniques.
Literature review
With the development of VR technology, attention to patient safety, and the requirement for scalable and cost-efficient training tools, the application of VR-based medical training has been growing in recent years14. This narrative review examines the evolution of VR applications in healthcare education with an emphasis on applications for healthcare professionals, compares the technical features of VR platforms, explores the impact of haptic feedback on skill acquisition, and summarizes the empirical evidence on the effectiveness of VR-based training15.
Evolution of VR in medical training
VR has been used in medical training for a few decades, first as a basic visualization tool and then increasingly as an immersive, interactive environment. Whereas early applications of VR were predominantly used to visualize anatomy in surgical planning, a recent trend has been to support real-time role-playing of a variety of medical procedure STITLES using VR. Since the early 2000 s, research has investigated the application of VR as an adjunct to skill training in surgery, demonstrating enhancements in accuracy and procedural time. Recently, VR simulations have been applied to other domains, such as emergency response, general medical procedures, and patient communication skills (Table 1).
Frameworks for VR in medical training
Technical frameworks for VR-based medical training increasingly emphasize modularity and adaptability. These frameworks integrate core programming specifications, including input, output, and virtual machine (VM) configurations into clinical training environments. Key features such as haptic feedback, case-based learning, and user-specific skill adaptation ensure realistic and personalized simulations. While earlier systems were largely monolithic, modern frameworks prioritize extensibility to enable customized training. Recent studies have also highlighted the use of Artificial Intelligence (AI) to dynamically adjust scenarios in real time based on trainee performance, thereby enhancing the effectiveness and precision of the learning experience (Table 2).
Role of haptic feedback in VR-Based medical training
A key component of VR in medical training is the incorporation of haptic feedback, where trainees replicate touch and force and practice fine motor skills as though they were working in a real-world environment. Other studies on haptics-enabled VR have demonstrated an enhancement in the learning and retention of constructs, such as suturing, catheter placement, and laparoscopic skills. However, haptic technology is expensive, and the implementation process demands meticulous calibration, as inconsistencies in feedback can affect training quality, as shown in Table 3.
Empirical evidence on the effectiveness of VR-Based training
Empirical studies evaluating the effectiveness of VR training have revealed that it improves procedural skills, reduces training time, and enhances knowledge retention. VR training has been particularly successful in surgical education, where hands-on practice is essential for learning. Studies have shown that trainees using VR demonstrate better performance in terms of accuracy, speed, and confidence when transitioning to real-life procedures. However, the effectiveness of VR varies across different medical domains. While highly effective for procedural skills, it may be less effective for training soft skills, such as communication, which benefit from human interaction. To address this issue, VR platforms have integrated AI-based virtual patients that simulate real-life reactions to improve empathy and communication training (Table 4).
Comparative analysis of Cost-Effectiveness
Cost remains a significant factor in adopting VR for medical training. While VR systems provide long-term advantages, their upfront costs, which cover hardware, software development, and ongoing maintenance, can be significant. However, comparative studies indicate that VR has become increasingly cost-effective, especially in resource-constrained environments with limited access to clinical placements. By reducing the reliance on physical simulators, VR can lower recurring training expenses, although regular updates and system maintenance still require investment. For many institutions, a hybrid model integrating VR with minimal physical simulation offers the most balanced and cost-efficient solution, as shown in Table 5.
Gaps in current research
Recent studies have explored advanced AI and computer vision techniques with applications in education, healthcare and virtual training. A mask transformer-based unsupervised segmentation model19 demonstrated high accuracy and efficiency in video object segmentation, whereas synthetic data generation20 was evaluated for semantic segmentation in autonomous driving. STIG-Net21, a spatiotemporal graph model, effectively recognizes violent behavior in video footage. Enhancements in facial action unit recognition through topological-relational learning22 have improved affective computing and emotion detection systems. The frame attention neural network (FANN)23 has shown promise in detecting student engagement from facial cues for educational applications.
Additional innovations include the MRA-Net24, a multiscale instance segmentation model for ethnic costume recognition, and a magnetic-field-based virtual surgery simulation25, which enhanced realism in surgical training. Augmented reality has been successfully applied to anatomy learning through 3D gesture interaction26, and importance-aware volume visualization27 has improved medical image retrieval. SPST-CNN28 enabled better surgical tagging in liver operations, and a mixed-reality intravenous cannulation system29 enhanced the acquisition of skills. Efficient binocular rendering30 further improves VR immersion across various domains. Despite these advances, gaps remain, particularly in integrating VR into broader curricula, tailoring AI-based feedback, and standardizing evaluation metrics for VR training. Future research should explore multisensory integration and interprofessional simulation to maximize VR’s potential of VR in collaborative, immersive healthcare education.
Proposed methodology
Simulation algorithms for VR medical training incorporate haptic feedback, real-time performance assessment, and adaptive learning to improve medical education results. A typical clinical scenario is selected to design a virtual environment in accordance with the training goals. Haptic devices are subsequently attached and calibrated to provide life-like tactile feedback, mimicking tissue resistance and physical contact during real procedures31. This calibration is in place to provide authentic force feedback between trainees, such that motor memory and procedural integrity are reinforced. Table 6 contains all the symbol and their denotation with their unit.
The overall system improves the learning experience by computing dynamic force feedback based on a user’s interactions with the system and employing physics-based models of force feedback to represent real sensations.
Before the start of the scenario, the system specifies performance indicators, including the duration of the action, correctness of the actions, and correctness of the decisions in action. These measures are written in standard measure, where E represents the procedural accuracy defined by
with \(\:{x}_{i}\) representing the trainee’s actions and \(\:{x}_{i}\)* representing ideal actions. At its heart, the algorithm exists in a continuous feedback loop, where it tracks and reacts to learner behavior in real time. The movements, decisions, and response times of the trainees during each step were captured by the system. Using intelligent virtual patients that incorporate AI helps the algorithm generates realistic responses to what the trainees do, creating realistic scenarios that can adapt to varying skill levels32. If mistakes are made, the system alerts the trainee immediately and logs them for further analysis. This feedback process is critical because it helps avoid the repetition of bad habits. The feedback intensity was modulated using the following equation: (3).
where IO is the baseline intensity, and is the learning rate. The haptic feedback was then dynamically changed during the simulation in response to the trainee’s movements34. It derives the correct force responses based on advanced physics models of various tissue types and procedural resistance. This allows them to advance their muscle memory and procedural awareness while being placed in a much more realistic and immersive environment for training. After the algorithm was completed, all collected data were processed to generate a detailed performance report. This analysis consisted of quantitative measures (time taken, number of errors, and procedural accuracy) and qualitative evaluations (decision-making and technique). Standardized scoring methods were used to assess performance against the criteria35. The system uses standardized scoring methods to evaluate performance against established benchmarks, as shown in Fig. 3.
The algorithm incorporates adaptive learning principles by adjusting the scenario difficulty based on the trainee’s performance. This adaptation is governed by the equation
where different performance aspects are weighted to determine the overall proficiency36. Finally, the algorithm saved all the performance data for longitudinal analysis. This data collection enables the tracking of trainee progress over time and helps identify areas requiring additional focus. The stored information also contributes to the continuous improvement of training scenarios and the calibration of performance metrics. The effectiveness of the algorithm was demonstrated through improved learning outcomes, with studies showing significant improvements in procedural accuracy and decision-making abilities37. The integration of haptic feedback and real-time error detection creates a comprehensive learning environment that bridges the gap between theoretical knowledge and practical skill.
Algorithm for VR-Based Medical Training Simulation.
Algorithm 1
provides a structured workflow for the VR medical training simulation, guiding the process from the scenario setup to performance feedback.
Algorithm 1: VR Medical Training Simulation Workflow |
|---|
Input: Selected medical scenario S, trainee profile P |
Output: Performance report with scores, feedback, and improvement suggestions |
1. BEGIN |
2. Load Scenario(S) |
3. Initialize VR Environment |
4. Connect Haptic Devices and Calibrate for Scenario S |
5. Display Initial Instructions to Trainee P |
6. Set Performance Metrics (completion time, accuracy, decision-making) |
7. WHILE Scenario not Completed DO |
8. Display Scenario Step to Trainee |
9. Capture Trainee Actions |
10. Generate Real-Time Feedback |
11. IF Error Detected THEN |
12. Display Error Alert |
13. Log Error in Performance Metrics |
14. END IF |
15. Provide Haptic Feedback Based on Action |
16. Update Scenario Step |
17. END WHILE |
18. Capture Completion Time |
19. Assess Procedural and Decision Accuracy |
20. Generate Performance Report |
21. Display Feedback to Trainee P |
22. Save Performance Data for Further Analysis |
23. END |
Requirements gathering and analysis
The initial phase involved a thorough requirement analysis to define the platform’s educational goals and technical capabilities. This phase engages medical educators, trainees, and VR developers to collaboratively outline the essential features, scenarios, and haptic requirements of the VR platform. This collaborative effort included inputs from medical educators, trainees, and VR developers, ensuring that the platform met both pedagogical and technical expectations38. The first phase involved a thorough analysis of the educational and technical requirements of VR platforms. This phase includes:
-
Identifying Core Skills: A set of medical skills \(S=\left\{{s}_{1},{s}_{2},\dots,{s}_{n}\right\}\) is identified, where each \({s}_{i}\) represents a specific medical skill (e.g., surgical techniques, emergency interventions). The selection of skills is based on training demand \(\:D({s}_{i})\) and clinical impact \(I({s}_{i})\), weighted by \(\alpha\) and \(\beta\) :
-
Defining Training Objectives: For Specific and measurable training objectives were established for each skill. The objective function is to minimize time \(T\) and maximize accuracy \(A\) :
Subject to constraints:
The overall performance score \(P\) is calculated as:
where \({\omega}_{1}\) and \({\omega}_{2}\) are weights for time efficiency and accuracy.
-
Assessing Technical Feasibility: The platform’s technical requirements, such as graphics fidelity \(G\), system response time \(R\), and computational capability \(C\), are evaluated to ensure they meet the minimum thresholds:
This phase can be mathematically structured into the following key steps:
-
1.
Identifying Core Skills: The first step was to determine the set of medical skills to be simulated. Let the set of core skills be represented as.
where \(\:{s}_{i}\) represents a specific medical skill, such as surgical techniques, emergency interventions, or routine medical procedures. The prioritization of skills can be quantified based on their training demand \((D({s}_{i}))\) and impact on clinical outcomes \((I({s}_{i}))\). The selection of skills \({S}^{\text{*}}\) to include in the platform can then be expressed as:
where \(\alpha\) and \(\beta\) are weights assigned to training demand and clinical impact, respectively.
-
2.
Defining Training Objectives: For each skill \({s}_{i}\in {S}^{\text{*}}\), specific and measurable training objectives are established. These objectives can be modelled as optimization problems39. Let \(T\) represent the time taken to complete a task, and \(A\) represent the accuracy of procedural steps. The training objective function can be expressed as
Objective: \(\text{m}\text{i}\text{n}T, \text{m}\text{a}\text{x}A\)
subject to constraints:
where \({T}_{\text{m}\text{a}\text{x}}\) is the maximum allowable time, and \({A}_{\text{m}\text{i}\text{n}}\) is the minimum required accuracy.
The overall performance of a trainee can be represented by a composite score \(P\), defined as:
where \({\omega}_{1}\) and \({\omega}_{2}\) are the weights assigned to time efficiency and accuracy, respectively.
-
3.
Assessing Technical Feasibility: The technical feasibility of the VR platform was analyzed by evaluating its hardware, software, and haptic requirements. Key metrics include graphics fidelity \((G)\), system response time \((R)\), and computational capability \((C)\).
Graphics Fidelity: The fidelity of the graphics must meet or exceed a threshold \({G}_{\text{m}\text{i}\text{n}}\) to ensure realistic simulations. This can be expressed as
System response time
The response time \(R\) should be minimized to maintain interactivity and realism, subject to a maximum allowable response time\({R}_{\text{max}}\)
Computational capability
The computational capability of the system, represented by \(C\), must be sufficient to handle the required graphics and interaction complexity40. This is given by.
where \({C}_{\text{r}\text{e}\text{q}}\) is the required computational power, which can be a function of \(G,R\), and the number of concurrent users \(U\) :
Feasibility condition
The overall feasibility of the platform was ensured when all the constraints were satisfied.
By mathematically defining these steps, the requirements gathering and analysis phase provides a structured approach to ensure that the VR platform aligns with the educational goals and technical specifications.
VR environment development
The VR environment construction stage involves establishing a realistic and immersive clinical environment in the virtual world. This includes 3D modelling, scripting scenes, and ensuring that interactive elements function as expected.
3D modelling and scene construction
Realistic 3D models of medical devices and patients’ bodies should be generated to make the learning environment immersive. In life-like models, anatomically accurate models are built using tools such as Unity and Unreal Engine.
-
a.
3D Model Representation: The 3D models were constructed using triangular mesh. Each triangle in the mesh is represented by three vertices in the 3D space as follows:
where \(({x}_{j},{y}_{j},{z}_{j})\) are the coordinates of vertex \({v}_{j}\) in 3D space. The collection of triangles defines the surfaces of a 3D object.
-
b.
Transformation Matrices: Transformation matrices were applied to accurately position and orient the 3D models as follows:
Translation:
Rotation (around the z-axis).
Scaling:
The final position of a vertex \(v\) after transformations is given by:
-
c.
Scene Construction: Objects in a clinical environment must be placed to avoid overlap and ensure spatial realism. This involves solving the following optimization problems for object placement:
where \({p}_{i}\) and \({q}_{i}\) are the current and desired positions of objects, \({d}_{ij}\) is the distance between objects \(i\) and \(j\), and \({d}_{\text{m}\text{i}\text{n}}\) is the minimum allowed distance to prevent overlap.
-
d.
Interactive Components: Interactive elements, such as medical instruments and lighting, are governed by user input. The interaction was modelled using the following physical equations:
-
Instrument Motion: Modelled using kinematics, if an instrument is moved, its position \(x (t)\) is updated as:
where \({x}_{0}\) is the initial position, \(v\) is velocity, and \(a\) is acceleration.
-
Lighting Simulation: Lighting was simulated using the Phong reflection model.
where:
-
\({I}_{a}\) : Ambient light intensity
-
\({I}_{d}\) : Diffuse reflection intensity, dependent on the angle between the light direction \(\mathbf{L}\) and the surface normal \(\mathbf{N}\)
-
\({I}_{s}\) : Specular reflection intensity, based on the angle between the reflected light \(\mathbf{R}\) and the viewer’s direction \(\mathbf{V}\)
-
\(n\) : Shininess coefficient
Model Verification.
Verification involves comparing the virtual models with real-world anatomical data.
where \({\mathbf{M}}_{\text{virtual}}\) and \({\mathbf{M}}_{\text{real}}\) are the vertices of the virtual and real models, respectively. \({\Delta}\) represents the percentage error, which must be minimized. By leveraging these mathematical principles, the VR environment achieves a balance between precision and interactivity, thereby delivering immersive and functional clinical simulations.
Scenario scripting
VR-based training simulators in the medical field are meticulously designed for an expected variety of clinical circumstances, from normal procedures to complex surgical operations. These scenarios are scripted to be interactive and provide points of branching decisions to evolve similarly to trends in real-world medical decision-making.
-
1.
Decision Points: Users make key decisions, such as incision location or procedure type, that affect the scenario’s outcome, encouraging critical thinking and clinical decision-making.
-
2.
Immediate feedback: The simulator used real-time scoring of anaesthesiology skills to alert students to procedural errors and best practices. The key for linguistic application of this 3D model is to provide a 3D model that represents the anatomical structures and physical environments realistically. 3D modelling in general uses mathematical transformation to project 3D world coordinates into 2D display coordinates. For preserving anatomical accuracy and spatial consistency, the transformation matrices are employed to translate, rotate, and scale objects within the VR environment. This enables live/real time representation of the interactions required for procedural training and orientation.
-
3.
Transformation Matrix: A 3D points in global system are being transformed by means of a matrix. The transformation equation for a point is as follows:
$$\left[\begin{array}{c}{x}^{{\prime\:}}\\\:{y}^{{\prime\:}}\\\:{z}^{{\prime\:}}\\\:1\end{array}\right]=\left[\begin{array}{ll}R&\:T\\\:0&\:1\end{array}\right]\left[\begin{array}{c}x\\\:y\\\:z\\\:1\end{array}\right]$$
where:
-
\(R\) is a \(3 \times 3\) rotation matrix that rotates the point,
-
\(T\) is a \(3 \times 1\) translation vector that shifts the point in space,
-
\(({x}^{{\prime}},{y}^{{\prime}},{z}^{{\prime}})\) is the new coordinate of the point after transformation.
Projection transformation
Projection transformation is used to display a 3D object on a 2D monitor. In perspective projection, the depth of an object affects its size and contributes to realism. The perspective projection transform may be expressed as.
where:
-
\(f\) is the focal length of the virtual camera,
-
\(d\) is the distance from the camera to the projection plane,
-
\(n\) and \(f\) represent near and far clipping planes, defining the viewable depth range.
This transformation ensures that objects closer to the viewer appear larger, thereby enhancing the realism of the 3D environment.
Haptic feedback integration
Haptic interaction is particularly important in VR-based medical training sessions, where exact motor skills and tactile sensitivity are necessary. In the second stage of the system construction, VR simulations are combined with state-of-the-art haptic systems (SensAble Omni or Haptic Master) capable of emulating touch and force feedback on a trainee to help them acquire real-life hand-eye relationships and fine motor capabilities.
To create a realistic haptic interaction, the approach utilizes tactile dimensional modulation, where a modulation texture is assigned to the virtual object so that users can feel the depth, resistance, and surface variations. These sensations correlate with the object velocity, applied force, and motion type, resulting in more subtle tactile feedback sensations.
Sensory Mapping is utilized to map certain procedural decisions (e.g., suturing and palpation) to appropriate haptic feedback, adding realism.
Synchronization ensures that the tactual feedback closely follows visual and auditory stimuli and maintains modality correspondence for simulation fidelity.
Through force vector modelling, the software considers the amount of resistance simulated components provide to a touch or tap. This immersion feature enables trainees to feel and react to the simulated tissue and instrument properties, in addition to the tactile response, and provides realistic procedural training and enhanced retention of skills through multisensory experience.
Force feedback calculation
The haptic force feedback system computes the force feedback according to the interaction between the virtual instrument (e.g., scalpel) and the virtual anatomical structure (e.g., tissue). Force feedback, \({\mathbf{F}}_{t}\) is often modelled using Hooke’s Law, given by
where:
-
\(k\) is the stiffness coefficient representing the elasticity of the virtual tissue,
-
\(\mathbf{X}\) where denotes the displacement vector of the virtual tool with respect to the tissue surface.
This force calculation enables the haptic device to apply pressure that simulates the resistance of different tissues, allowing trainees to practice procedures such as incision and suturing with realistic and accurate feedback.
-
1.
Damping Effect: To prevent oscillations and ensure stable feedback, a damping term was added to the force equation. The damping force, \({\mathbf{F}}_{\text{d}}\), is given by:
$${\mathbf{F}}_{\text{d}}=-c\cdot \mathbf{v}$$
where:
-
\(c\) is the damping coefficient,
-
\(\mathbf{V}\) where is the velocity of the haptic device, and
The total force applied to the haptic device is then
This ensures smooth and realistic feedback by controlling the stiffness and damping characteristics, which are crucial for simulating interactions with various types of tissue.
Haptic feedback and force calculation
Haptic feedback is essential in simulators, as it is a requirement for reproducing sensations, which are important for procedural training. These models capitalize on the use of force vectors for simulating the sensation of touch and forces produced when interacting with virtual objects and aid a trainee in building a realistic concept about physical touching.
-
a.
Haptic feedback calculation: Force feedback was calculated based on the interaction between the virtual instrument (e.g., scalpel) and anatomical structures (e.g., tissue). Force feedback, \({\mathbf{F}}_{t}\) is often modelled using Hooke’s Law, given by:
$$\mathbf{F}=-k\cdot \mathbf{x}$$
where:
-
\(k\) is the stiffness coefficient representing the elasticity of the virtual tissue,
-
\(\mathbf{X}\) where denotes the displacement vector of the virtual tool with respect to the tissue surface.
This force calculation enables the haptic device to apply pressure that simulates the resistance of different tissues, allowing trainees to practice procedures such as incision and suturing with realistic and accurate feedback.
-
b.
Damping Effect: To prevent oscillations and ensure stable feedback, a damping term was added to the force equation. The damping force, \({\mathbf{F}}_{\text{d}}\), is given by:
$${\mathbf{F}}_{\text{d}}=-c\cdot \mathbf{v}$$
where:
-
\(c\) is the damping coefficient,
-
\(\mathbf{V}\) where is the velocity of the haptic device, and
The total force applied to the haptic device is then
This ensures smooth and realistic feedback by controlling the stiffness and damping characteristics, which are crucial for simulating interactions with various types of tissue.
Trainee performance tracking and assessment
To make the VR training platform efficient, the trainee progress should be tracked in-scenario and with post-scenario surveys. This information not only verifies the system is effective but also offers specific feedback and identifies areas to target.
-
1.
In-Scenario Metrics: Real-time measurement of certain important metrics of trainees’ ‘effectiveness’ such as time to task completion, accuracy across a task and decision-making ability.
-
2.
Time to completion: Total time at each task from start to finish was recorded and compared with the previously established proficiency standards to measure efficiency.
-
3.
Procedural Correctness After the trainee’s procedural completion, this metric evaluates how closely the trainee adheres to the correct order of procedural steps, to assess if incorrect steps are taken or if steps are missed or out of order.
-
4.
Correct decision: decision is compared with best medical practice to rate decision quality and clinical reasoning at each decision point.
-
5.
Post-Scenario Feedback: A report with performance data, scores, errors, and tailored feedback was given after the performance on a scenario was completed. It also helps develop skills, reduce knowledge decay, and leave a trace of progress over time.
The VR system adopted a robust evaluation mechanism (VRM Trainee Assessment Metrics) and procedural accuracy, time completion and number of errors were computed into allometric mathematical models. Such models predict learner performance by a priori criteria to make judgments about learner competence and support adaptive training interventions.
Procedural accuracy
Procedural correctness was assessed by measuring the deviation from a standard procedure. Consider any step of a procedure that has a corresponding action for the target and the trainee. where 𝑃 is the accuracy of procedure.
where:
-
\(n\) is the total number of procedural steps,
-
\(\mid A-{A}_{t} \mid\) where is the absolute error at each step.
-
a.
Completion Time: Completion time, \({T}_{c}\), is the duration taken by a trainee to complete the procedure compared to the expected time \({T}_{e}\). The efficiency ratio, \(ER\), is defined as:
$$ER=\frac{{T}_{e}}{{T}_{c}}$$
An \(ER\) closer to 1 indicates timely completion, while values below 1 suggest inefficiency.
-
b.
Error Rate: Error rate, \({E}_{rr}\) is calculated by dividing the number of errors \(E\) by the total number of actions \(A\) :
$${E}_{r}=\frac{E}{A}$$
This metric allows instructors to gauge areas that need improvement and provides objective insights into trainee proficiency.
-
c.
Error Rate: Error rate, \({E}_{r}\), is calculated by dividing the number of errors \(E\) by the total number of actions \(A\) :
$${E}_{r}=\frac{E}{A}$$
This metric allows instructors to gauge areas that need improvement and provides objective insights into trainee proficiency.
-
d.
Procedural Accuracy: Procedural accuracy was quantified by tracking deviations from the standard procedure. Each step of a procedure has an associated target action \({A}_{t}\) and the trainee’s action \(A\). Procedural accuracy, \(PA\), can be calculated as:
$$PA=1-\frac{\sum \mid A-{A}_{t} \mid}{n}$$
where:
-
\(n\) is the total number of procedural steps,
-
\(\mid A-{A}_{t} \mid\) where is the absolute error at each step.
-
e.
Completion Time: Completion time, \({T}_{c,}\) is the duration taken by a trainee to complete the procedure compared to the expected time \({T}_{e}\). The efficiency ratio, \(ER\), is defined as:
$$ER=\frac{{T}_{e}}{{T}_{c}}$$
An \(ER\) closer to 1 indicates timely completion, while values below 1 suggest inefficiency.
-
f.
Error Rate: Error rate, \({E}_{r}\), is calculated by dividing the number of errors \(E\) by the total number of actions \(A\) :
$${E}_{r}=\frac{E}{A}$$
This metric allows instructors to gauge areas that need improvement and provides objective insights into trainee proficiency.
Adaptation of training scenarios based on performance
For adaptive training, the scenarios can be flexible and tailored to a trainee’s performance scores, personalizing the training. Adaptation is done through feedback loops, where the user performance is evaluated and the task difficulty level is updated accordingly.
Adaptive difficulty model
Let \({D}_{t}\) represent the target difficulty level of the scenario, \(P\) the trainee’s performance score, and \(D\) the initial difficulty level. An adaptive model adjusts difficulty as follows
where:
-
\(\alpha\) is a learning rate parameter controlling the adjustment pace,
-
\({P}_{t}\) where denotes the target-performance score.
If the trainee’s performance exceeds \({P}_{t}\) the difficulty increases’: otherwise, it decreases, promoting gradual skill progression.
Detailed System architecture development process
In this section, we describe the constructed VR-driven medical-training platform in details and provide with detailed and in-depth information on its system architecture, development, and the technical features and configurations of the hardware and software deployed in the system. The tool was evaluated by data analysis and a usability test.
Hypothesis Testing: A t-test was used to compare the performances of the VR-trained and traditionally trained groups.
where \({\bar{X}}_{VR}\) and \({\bar{X}}_{T}\) are the mean scores of the VR and traditional groups, respectively.
-
Feedback Control for Error Minimization: A PID controller was used to refine scenarios based on trainee performance.
$$S (t)={K}_{p}e (t)+{K}_{i}\int\: e (t) dt+{K}_{d}\frac{de (t)}{dt}$$
where \(e (t)\) is the error at time \(t\), and \({K}_{p,}{K}_{i}\), and \({K}_{d}\) are the proportional, integral, and derivative gains.
Development process
A VR medical training platform was developed using a phased approach. It Needs assessment Consultations with practicing clinicians were used to identify and rank key procedures as per clinical importance and training required.
-
1.
3D Modelling and Scene Composition: High-res anatomical models and clinical environments were generated from Blender/Maya and validated against real data.
-
2.
Haptic Feedback Implementation: Haptic device calibration was based on Hooke’s law and damping models to mimic realistic tissue resistance and tactile interaction respectively.
-
3.
Scripting for scenarios: The interactive medical scenarios were created with decision points and point-of-care feedback to mimic the actual clinical environment.
-
4.
Testing and Validation: The platform was subjected to usability, validity and performance testing with feedback from trainees and teachers used to further develop the system.
Results and analysis
An innovative VR-based medical training platform was developed to transform healthcare education through immersive, risk-free clinical simulations. The study involved 87 participants, including medical students, residents, and professionals from various institutions in Jaipur and Guntur, India representing a range of experience levels. The platform integrates high-fidelity 3D rendering, haptic feedback, and performance tracking based on mathematical modelling to provide realistic and adaptive training. Results from validation studies showed that VR training outcomes were comparable or superior to traditional methods, supporting its role as a valuable complement to conventional educational methods. Scalable and repeatable, the platform addresses the need for accessible, high-quality training, particularly in resource-constrained settings, and enhances clinical readiness across all learner levels. Figures 4, 5 and 6, and 7 visually represent the key modules and procedural steps in VR-based medical training simulations.
Validation of training effectiveness
Validation is crucial to confirm that VR training provides learning outcomes that are comparable or superior to those of traditional methods. Statistical models were employed to analyse learning outcomes by comparing VR-based training scores with those of the control groups.
Hypothesis testing
To validate the training effectiveness, hypothesis testing was used to evaluate the differences in performance metrics between the VR-trained and traditionally trained groups. Let \({\bar{X}}_{VR}\) and \({\bar{X}}_{T}\) be the mean scores of VR and traditional training groups, respectively. A t-test was performed as follows
where:
-
\({S}_{VR}^{2}\) and \({S}_{T}^{2}\) are the variances of VR and traditional groups,
-
\({n}_{VR}\) and \({n}_{T}\) are the sample sizes of each group.
A statistically significant \(t\)-value indicates a meaningful difference in outcomes, supporting the efficacy of VR training.
Error minimization and scenario refinement
Scenario refinement ensures continuous improvement in VR simulations based on error minimization. By employing a feedback control system, we can refine the scenarios to enhance learning effectiveness.
Feedback Control for Error Minimization: A proportional-integral-derivative (PID) controller model was employed to refine the scenarios based on trainee performance. The error \(e (t)\) at time \(t\) is given by:
The controller output adjusts scenario parameters \(S (t)\) as follows:
where:
-
\({K}_{p,}{K}_{ir}\) and \({K}_{d}\) are the proportional, integral, and derivative gains.
This feedback mechanism reduces persistent errors, ensuring that scenarios adapt dynamically to support trainee progress.
4.3 Platform validation and usability testing
The final phase validated the educational and usability standards of the platform. Feedback from usability testing with medical trainees was incorporated to refine the platform and compare VR-based training outcomes with those of traditional methods.
-
Usability Testing: Evaluation of the platform’s user interface, ease of navigation, and intuitive control.
-
Learning Outcome Comparison: Studies comparing VR-trained groups with traditionally trained groups to assess learning outcomes and skill retention.
-
Iterative refinement: User feedback was incorporated to adjust the scenarios, haptic responses, and interfaces, enhancing the platform’s effectiveness and usability.
Table 7 shows the progressive impact of VR on the medical-training domain. Smith et al. reported a 30% improvement in laparoscopic precision and speed, while Brown et al. observed a 25% boost in anatomical knowledge retention via 3D visualization. Emergency response training showed the highest gain at 40%, enhancing confidence and decision-making speed in the participants. There was a 20% increase in patient communication skills. The proposed multimodal method outperformed all others, achieving a 42% improvement through adaptive AI feedback tailored to surgical, emergency, and patient-care scenarios.
Special study design and assessment methodology
To address the reviewer’s comment that the study does not provide sufficient detail to assess the system, this section outlines the study design, evaluation methodology, and statistical analysis employed to validate the effectiveness of the platform.
Study design
A randomized controlled trial (RCT) comparing a VR-based medical training platform with conventional training has been performed. The study included two groups of medical trainees.
-
1.
VR Training Group: This cohort used the VR platform for an array of training in medical techniques, such as laparoscopic surgical procedures, catheterization, and emergency situations.
-
2.
Standard Training Group: This group was trained in a traditional in-person fashion with physical simulators and clinical placements, as per usual medical education procedures.
Data collection for the study occurred over six months, and both groups of trainees performed identical procedures and assessments.
Evaluation metrics
The effectiveness of the VR platform was measured using the following metrics:
-
1.
Procedural Accuracy: Percentage of correct procedural steps performed by the trainees in the simulation.
-
2.
Time to Completion: How long did it take the trainee to perform the procedure against what was expected?
-
3.
Error rate: Error Number of errors during the course, including incorrect event skipping.
-
4.
Retention of Learning Skills: The extent to which trainees are able to retain and utilize the skills learned during training, evaluated through follow-up tests administered three months after the initial training.
-
5.
Confidence Gain: Self-reported confidence levels before and after training, measured by a confidence scale.
Statistical analysis
A comparison of the VR training and traditional training groups was performed statistically using the data collected from the study. The following statistical techniques were used:
-
1.
Statistical Analysis: A t-test was used to compare the mean scores of the VR and traditional training groups for each metric. We hypothesized that there would be no significant difference in performance between the two groups, as shown in Table 8.
The 10 observations showed that the metric of the VR training group was better than that of the other group, and the differences were statistically significant (p < 0.01). This suggests that VR is better than face-to-face learning in improving procedural accuracy, reducing procedure times and error margins, and increasing trainee confidence.
-
2.
ANOVA: The effects of different types of training on procedural accuracy, task completion time, and error rates were tested using analysis of variance (ANOVA), as presented in Table 9.
An analysis of variance (ANOVA) on procedural accuracy ratios, completion times, and error rates reflected a significant effect of training mode (VR vs. traditional) on all of these factors (p < 0.01). This indicates that the performance of the VR training platform is better than that of traditional techniques for the performance metrics.
Figure 8 and the regression analysis proved that VR training with haptic feedback, adaptive learning, and real-time performance tracking had a positive effect on effective training (p < 0.01) by explaining 85% of the variance in the participants’ performance. Key findings include: (1) t-test shows VR users outperform traditional groups in accuracy, speed, and confidence (p < 0.01); (2) ANOVA reveals training mode significantly affects procedural outcomes; and (3) regression identifies all three features as strong predictors of improved VR performance.
Across medical training domains, VR applications have demonstrated substantial gains in learning outcomes, time efficiency, and cost savings (Table 10). Emergency response training showed the highest improvements: 40% in learning, 35% in time savings, and 65% in cost reduction, owing to VR’s ability to simulate high-pressure scenarios. Surgical training achieved 35% learning gains, 30%time savings, and 55% cost reduction, highlighting VR’s role of VR in safe procedural practice. Anatomical education saw a 38% learning increase, 28% faster training, and 60% cost savings, whereas patient communication showed modest but meaningful improvements (20% learning, 25% time, and 45% cost). The proposed VR framework surpasses all with a 42% performance gain, 38% faster training, and 70% cost savings, enabled by the adaptive AI, multimodal feedback, and enhanced haptics. VR development frameworks vary in effectiveness: the proposed model leads to a 4.9 usability rating and 38% faster completion time than the others. AI-SimAdapt follows a 4.8 usability and 35%time savings through AI-driven performance tracking. SimEd VR, with scenario-based learning, achieved usability and efficiency scores of 4.5 and 30%, respectively. The haptic-focused system scored 4.2 and reduced the training time by 25% (Fig. 9).
The VR Anatomy Suite, with the lowest usability rating of 4.0 and a modest 15%time reduction, still provided valuable visual learning via high-fidelity anatomical models. The shift from static image-based tools to AI-powered systems marks a major leap in medical VR training. The proposed model surpasses existing platforms by integrating adaptive AI with pooled and multimodal training strategies, combining prior strengths with advanced personalization (Fig. 10). This comprehensive approach enhances usability and accelerates skill acquisition, making it ideal for medical institutions seeking efficient and high-impact training solutions. The x-OS performance comparison of VR development frameworks with an impressive rating of 4.8, SimEd VR, measured strong usability and showed a 35% reduction in completion time owing to teaching through scenario-based and immersive simulations. With a focus on skill acquisition via haptic redirection and tailored modules, MedTrainer Pro retained a good 4.2 usability rating and delivered 25% less completion time. 35 VR Anatomy Suite scored 4.0 for usability but achieved more modest improvements with a 15% reduction in completion time (in line with its specialized nature for visual learning through high-fidelity anatomical models, which allows the exploration of the anatomy interactively, with integrated pathological references), suggesting a potential for improvement compared with app control. AI-SimAdapt with AI-guided training and performance tracking; 4.8 usability score, 35% completion time reduction. Our proposed model outperformed all other solutions on all metrics: the highest usability score of 4.9 and a 38% reduction in task completion time through a multimodal medical training model and adaptive AI-based learning system, as shown in Fig. 10.
The excellence of this performance is attributed to the overall integration of innovative components such as adaptive learning algorithms and complex performance-tracking mechanisms. AI-enhanced frameworks built on traditional techniques show a clear progression in effectiveness, with the proposed model being a cutting-edge VR medical training technology, as shown in Fig. 11.
The proposed method exhibits superior performance over existing methods by offering a comprehensive comparative analysis of the integration of haptic feedback across diverse VR-based medical training scenarios. In a study by Sinclair et al.29, laparoscopic training with the Phantom Omni device yielded a 25% increase in procedural accuracy and a 20% reduction in training time, establishing a key benchmark for haptics-enhanced simulations. Zhao et al., using the HapticMaster system for suturing tasks, reported even higher gains with a 30% accuracy improvement and a 25% decrease in training time, emphasizing the value of precise tactile input for fine motor skills. Anderson et al., simulating catheterization procedures with the Sensable Phantom, noted more modest improvements 20% in accuracy and 15% in time savings reflecting the complexity of vascular simulations. Martinez et al., applying VirtualForce to general surgery training, achieved intermediate results, with a 22% gain in accuracy and an 18% reduction in training time, as shown in Fig. 12.
The work that includes the Adaptive Haptic Master system in the field of general surgery shows the best performance metrics, with a 35% increase in procedural accuracy and a 30% reduction in overall training time. These better results are due to the ambiguity of the adaptive haptic feedback system (HFS), which generates pressure feedback according to user responses and the need for procedures. The data indicate a direct relationship between advanced haptic feedback systems and improved learning performance in medical training, while the work proposed here offers a new standard for the effectiveness of VR-based surgical simulation through a responsive approach (Table 11).
This study evaluated the impact of haptic feedback on performance metrics across various medical procedures and demonstrated that the proposed method significantly outperformed traditional approaches. In suturing, haptic integration led to a 30% increase in procedural accuracy, 25% reduction in training time, and 85% skill retention rate after three months. For catheterization, the method achieved a 28% improvement in accuracy, 22% decrease in training duration, and 82% retention rate. Laparoscopic training exhibited the highest gains, with a 32% boost in accuracy, 28% improvement in efficiency, and 88% skill retention, underscoring the importance of tactile feedback in minimally invasive surgeries.
The proposed technique, which utilizes advanced haptic algorithms, delivered the most comprehensive results, with 35% higher accuracy, 30% reduction in training time, and 90% skill retention through precise force feedback calculations and dynamic-user interaction. The variation in accuracy across procedures highlights the critical role of haptics in tasks requiring fine motor control and tactile sensitivity. Moreover, haptic feedback accelerates motor learning consolidation when adequate time is allowed between practice tasks, thereby reinforcing its educational significance. Overall, the algorithm underlying the VR medical training system integrates immersive technology with a pedagogical structure, by initializing scenario-specific VR environments, calibrating haptic assemblies, and simulating realistic resistance using force feedback equations, as shown in Fig. 13.
The core execution stage of the VR simulation incorporated a continuous feedback loop that monitored the trainees’ actions in real time. Each procedural step was tracked, and immediate feedback was provided regarding the movements and decisions. Real-time error detection and logging were embedded into the algorithm to prevent the reinforcement of incorrect techniques; errors were flagged instantly and stored for comprehensive performance analysis. Haptic feedback dynamically responds to trainee behavior by simulating variable tissue resistance using physics-based modelling. The force responses were calculated using equations that incorporated the displacement and velocity components to ensure realistic tactile sensations and support muscle memory development. Subsequently, the algorithm processes the collected data and generates a detailed performance report. This analysis integrates quantitative metrics such as task completion time, procedural accuracy, and error frequency with qualitative assessments of clinical decision-making. Performance scores were calculated using a weighted model that emphasized accuracy, timing, and efficiency. This comprehensive evaluation enables targeted feedback and adaptive refinement of training scenarios, thereby enhancing the effectiveness of VR-based medical education.
VR simulations enhance trainee performance in various domains. The highest confidence gain (45%) was observed in emergency response training, underscoring the value of realistic high-pressure scenarios, as shown in Table 12. A comparative study of the performance metrics for VR implementation in other medical domains revealed large differences in the performance metrics, wherein the proposed system outperformed all measured metrics across all medical domains. VR training for emergency medicine has been found to yield significant mean improvements: a 38% gain in performance, a 45% increase in confidence (the highest increase of all studies), and an error reduction of 42% (the largest of all studies), which demonstrates that its potential use in this field is high, especially in high-pressure and time-critical situations. In the surgical area, there were robes with 35% accuracy, a 40% improvement in practitioner confidence, and a 38% decrease in mistakes. These findings highlight the potential of VR to create safe practice spaces for complex surgical procedures that require years of training. Therapeutic training via VR displayed moderate but nevertheless significant progress, a 30% performance improvement, a 35% boost in confidence, and a 32% decrease in errors. These metrics present the difficulties and intricacies of true diagnostic decision-making, where a pattern or a way to reason through the clinical picture provides the true determinant for an accurate diagnosis. The overall metrics show a 40% performance gain, 48% confidence boost, and 45% error reduction when the proposed system is compared with current implementations.
Conclusion
The medical education program exemplifies this, as it integrates first-hand virtual reality, multi-sensory simulation feedback, personalized instruction, and seamless interactivity, showcasing the transformative capacity of the system as a game-changing innovation in healthcare education. The results significantly improved (statistically significant) regarding the main KPIs measured, with 42% more accuracy in procedures performed, 38% faster training completion, and 90% retention at three months. With precision models for human anatomy, pathology, and medical instruments, this platform provides realistic haptic feedback from its premium haptic feedback engine, which is critical for training in the correct surgical techniques and for performing surgical tasks. An 85% reduction in long-term costs with low maintenance costs ($8000/yr), a high scalability index of 4.5/5, and low CAPEX and janitorial costs is achieved. This is an example of a very cool platform that adds a new baseline to medical trainer technology with a deviant combination of haptic feedback, AI-driven changes, and full performance tracking. Overall, this study highlights the promise of VR-based medical instruction as an impactful and scalable means of delivering medical education, which is particularly important in resource-constrained settings. Its future development should be a better training model, as it provides a larger scenario database, multi-user functions, and supports more active sensory feedback, although it is a promising training model based on data.
Data availability
The dataset and code which is used for this project are publicly available on this link. https://github.com/ankitkomar1/VR_Medical_Training_Updated.
References
Smith, A., Brown, M. & Thompson, J. Virtual reality for surgical training: Current status and future directions, IEEE Trans. Med. Imaging, vol. 38, no. 12, pp. 3402–3412, Dec. (2019).
Wee, C., Yap, K. M. & Lim, W. N. Haptic Interfaces for Virtual Reality: Challenges and Research Directions. IEEE Access 9, 112145–112162 (2021).
Gupta, K., Wei, J. & Kankanhalli, M. S. Real-time haptic feedback in VR for surgical training, IEEE Trans. Biomed. Eng., vol. 65, no. 3, pp. 656–665, Mar. (2020).
Gorman, J. R., Delaney, S. C. & Miller, R. L. The impact of immersive VR on procedural training in healthcare. IEEE J. Transl Eng. Health Med. 6, 1–8 (2018).
Braun, P. Virtual reality for immersive multi-user firefighter training scenarios. Virtual Real. Intell. Hardw. 4, 406–417 (2022).
Jin, C., Dai, L. & Wang, T. The application of virtual reality in the training of laparoscopic surgery: a systematic review and meta-analysis. Int J Surg 87, 105859 (2021). https://doi.org/10.1016/j.ijsu.2020.11.022
Zhao, T., Li, M. & Zhou, Z. Adaptive VR training platforms for personalized medical education. IEEE Access. 8, 157223–157234 (2020).
Ahmed, A. & Kumar, R. 3D modeling and simulation in VR for medical anatomy training IEEE Trans. Vis. Comput. Graph., vol. 27, no. 3, pp. 2337–2346, Mar. (2021).
Turner, D. & Johnson, E. Impact of haptic feedback on training outcomes in VR-based medical simulations. IEEE Trans. Haptics. 13 (2), 162–173 (2020).
Lee, S. J., Lee, C. & Kim, D. VR simulation for clinical skill acquisition: An assessment framework, IEEE Trans. Med. Imaging, vol. 39, no. 4, pp. 894–905, Apr. (2020).
Garcia, F. & Perez, M. Efficacy of VR and AR applications in healthcare training. IEEE Rev. Biomed. Eng. 12, 176–189 (2019).
Babatunde, A. O. et al. Designing a virtual reality system for clinical education and examination. Computers & Education: X Reality 5, 100083 (2024).
Pandey, R. & Sharma, V. Real-time adaptive feedback in VR for improving surgical skills. IEEE Access. 9, 51267–51278 (2021).
Kim, S. C. & Kim, J. Y. Deep learning in VR simulations for medical training applications, IEEE Trans. Neural Netw. Learn. Syst., vol. 32, no. 6, pp. 2273–2282, Jun. (2021).
Wang, L. & Li, H. Systematic review of VR-based procedural training in healthcare, IEEE J. Biomed. Health Inform., vol. 24, no. 9, pp. 2523–2532, Sep. (2020).
Zhang, T., Wu, X. & Sun, C. Haptic VR training for emergency response in healthcare. IEEE Trans. Emerg. Top. Comput. 9 (2), 677–689 (2021).
Jones, P. M., Green, M. S. & Brown, J. A. Quantitative assessment of VR surgical training effectiveness, IEEE Trans. Biomed. Eng., vol. 68, no. 4, pp. 1185–1194, Apr. (2021).
Chen, M. C. & Li, Y. L. Integration of VR and AI in training for emergency procedures. IEEE Access. 7, 156431–156442 (2019).
Qu, D., Zhao, H. & Zhou, M. Unsupervised video object segmentation with mask transformer: boosting accuracy and efficiency through feature fusion. Vis. Comput. https://doi.org/10.1007/s00371-025-03820-0 (2025).
Silva, M. et al. Exploring the effects of synthetic data generation: A case study on autonomous driving for semantic segmentation. Vis. Comput. https://doi.org/10.1007/s00371-025-03811-1 (2025).
Lu, X. et al. Vis. Comput. https://doi.org/10.1007/s00371-025-03816-w (2025).
Li, K. et al. Facial action unit recognition is enhanced through the integration of topological features and relational learning. Vis. Comput. https://doi.org/10.1007/s00371-025-03817-9 (2025).
Wang, H. et al. Novel frame attention neural network for student engagement recognition in facial video. Vis. Comput. FANN https://doi.org/10.1007/s00371-024-03768-7 (2025).
Fan, Y., Wen, B. & Deng, H. MRA-Net: an instance segmentation method based on multiscale feature fusion for ethnic garment images. Vis. Comput. https://doi.org/10.1007/s00371-024-03762-z (2025).
Huang, Y. et al. Uniform gradient magnetic field and Spatial localisation method based on Maxwell coils for virtual surgical simulation. Comput. Animat. Virtual Worlds. 35 (3). https://doi.org/10.1002/cav.2247 (2024).
Karambakhsh, A. et al. Deep gesture interaction for augmented anatomy learning. Int. J. Inf. Manag. 45, 328–336. https://doi.org/10.1016/j.ijinfomgt.2018.03.004 (2019).
Li, M., Jung, Y., Fulham, M. & Kim, J. Importance-aware 3D volume visualisation for medical content-based image retrieval: A preliminary study. Virtual Real. Intell. Hardw. 6 (1), 71–81. https://doi.org/10.1016/j.vrih.2023.08.005 (2024).
Nazir, A. et al. SPST-CNN: Spatial pyramid-based searching and tagging of intraoperative liver views via CNN for minimally invasive surgery. J. Biomed. Inform. 106 (103430), 103430. https://doi.org/10.1016/j.jbi.2020.103430 (2020).
Xiong, W. & Peng, Y. Design and development of mixed-reality teaching systems for IV cannulation and clinical instruction. Comput. Animat. Virtual Worlds. 35 (3). https://doi.org/10.1002/cav.2288 (2024).
Xu, T., Ren, X., Yang, J., Sheng, B. & Wu, E. Efficient binocular rendering of volumetric density fields with coupled adaptive cube-map ray marching for virtual reality. IEEE Trans. Vis. Comput. Graph. 30 (10), 6625–6638. https://doi.org/10.1109/TVCG.2023.3322416 (2024).
Park, D. H. & Lee, K. H. Virtual patients in VR for training empathy and communication skills. IEEE Trans. Affect. Comput. 12 (2), 475–483 (2021).
Wang, J., Hu, L. & Chen, G. Comparative study on VR-based vs. conventional training in patient interaction. IEEE Access. 8, 98625–98636 (2020).
Li, X. & Wang, S. A VR framework for multi-sensory medical training, IEEE Trans. Med. Imaging, vol. 39, no. 6, pp. 1796–1807, Jun. (2020).
Thomas, A. & Singh, P. Using haptic VR to improve skill acquisition in catheterization training. IEEE Trans. Haptics. 13 (4), 332–341 (2020).
Yang, L., Zhao, F. & Liu, H. Immersive VR for realistic patient examination training. IEEE J. Transl Eng. Health Med. 8, 1–12 (2020).
Chen, H. & Gao, X. Modeling haptic feedback for realistic VR surgical simulations. IEEE Access. 7, 72573–72584 (2019).
Sun, Y., Lee, K. & Kim, W. 3D VR anatomical models for comprehensive medical training, IEEE Trans. Vis. Comput. Graph., vol. 27, no. 4, pp. 2635–2647, Apr. (2021).
Green, J. & Tan, P. Effectiveness of real-time feedback in VR medical training. IEEE Access. 8, 78822–78833 (2020).
Zhou, T., Zhou, S. & Wang, J. Y. Evaluation metrics for VR training effectiveness in healthcare, IEEE Trans. Biomed. Eng., vol. 67, no. 8, pp. 2384–2391, Aug. (2020).
Kumar, R. & Patel, D. Automated performance tracking in VR-based surgical training. IEEE Trans. Autom. Sci. Eng. 17 (4), 2221–2233 (2020).
Singh, N. & Dhillon, M. Realistic VR training simulations for emergency medicine, IEEE J. Biomed. Health Inform., vol. 25, no. 1, pp. 77–88, Jan. (2021).
Zhou, W. & Liu, F. Using machine learning to optimize VR training scenarios. IEEE Access. 9, 130456–130468 (2021).
Islam, M. K. & Brunner, I. Cost-analysis of virtual reality training based on the Virtual Reality for Upper Extremity in Subacute stroke (VIRTUES) trial. International Journal of Technology Assessment in Health Care 35, 373–378 (2019).
Acknowledgements
The authors are thankful to Manipal University Jaipur for the Article Processing Charges and providing conducive research environment.
Funding
Open access funding provided by Manipal University Jaipur. This work was supported and funded by the Deanship of Scientific Research at Imam Mohammad Ibn Saud Islamic University (IMSIU) (grant number IMSIU-DDRSP2504).
Author information
Authors and Affiliations
Contributions
Abdul Khader Jilani Saudagar conceived and designed the study. Abhishek Kumar performed the analysis and interpretation of the results. Yazeed Masaud Alkhrijah and Ankit Kumar and Linesh Raja implemented the methodology and performed the computations. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This research does not involve human participants, animal studies, or any form of personal data collection. The study focuses on the development and analysis of 3D animations and virtual reality (VR)-based immersive experiences. As such, it does not fall under the requirements for review by an Institutional Review Board (IRB). The content of the study is purely digital and involves virtual environments and simulations, with no direct interaction with real human subjects or any ethical concerns related to human or animal welfare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kumar, A., Saudagar, A.K.J., Kumar, A. et al. Innovating medical education using a cost effective and scalable VR platform with AI-Driven haptics. Sci Rep 15, 26360 (2025). https://doi.org/10.1038/s41598-025-10543-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10543-8
Keywords
This article is cited by
-
Virtual simulation system in cataract education for medical undergraduates: a prospective quasi-experimental study
BMC Medical Education (2025)