Abstract
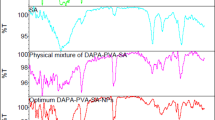
Tenofovir disoproxil fumarate is a widely prescribed component in antiretroviral therapy regimes frequently associated with nephrotoxicity. Dapagliflozin, an SGLT2 inhibitor, is primarily used as a hypoglycemic agent but is increasingly recognized for its pleiotropic protective effects. To investigate whether dapagliflozin could mitigate tenofovir-induced nephrotoxicity, Wistar rats were randomly assigned to four groups: Control- received a standard diet for 45 days, TDF- received a standard diet added with tenofovir (300 mg/kg food) for 45 days, DAPA- received a standard diet for 45 days added with dapagliflozin (20 mg/kg food) in the last 15 days, and TDF + DAPA- received a standard diet added with tenofovir for 45 days and dapagliflozin in the last 15 days. Dapagliflozin administration restored glomerular filtration rate, improved renal hemodynamic parameters and maintained the adequate balance of TBARS/GSH levels through the modulation of SIRT1/Nrf2/HO-1 signaling pathway and mitochondrial enzymatic antioxidant system-related markers. Furthermore, dapagliflozin treatment reduced inflammatory response and apoptotic cell death, marked by increased Bcl-2 expression and decreased levels of TLR4, NF-κB, pro-inflammatory cytokines, Bax, cytochrome c, and caspase-3. Dapagliflozin holds multifaceted renoprotective effects potentially offering a therapeutic strategy to slow the progression of kidney injury in tenofovir-induced nephrotoxicity.
Similar content being viewed by others
Introduction
Human immunodeficiency virus (HIV) infection remains a global public health challenge. As of the end of 2023, an estimated 40 million people were living with HIV, including approximately 1.4 million children and 38.6 million adults 1. Antiretroviral therapy (ART) regimen considerably changed the status of HIV, from a fatal disease into a manageable chronic condition, improving lifespan and enabling patients to lead productive lives2. Tenofovir disoproxil fumarate (TDF), a nucleotide reverse transcriptase inhibitor (NRTI), is considered a cornerstone drug in many treatment regimens for HIV infection3. Despite its efficacy, long-term use of tenofovir has been associated with the development of nephrotoxicity, which may progress to acute kidney injury (AKI) or chronic kidney disease (CKD)4. Clinical reports of tenofovir-associated nephropathy described partial or complete Fanconi syndrome, often accompanied by a reduced glomerular filtration rate (GFR)5,6. Other manifestations of proximal tubule dysfunction include osteomalacia and loss of bone mineral density, attributed to phosphate wasting and/or calcitriol deficiency7,8. Supporting these clinical findings, experimental evidence showed that tenofovir induces proximal tubular injury, marked by increased urinary phosphate excretion and decreased renal expression of the NaPiIIa cotransporter, resulting in hypophosphatemia and hyperphosphaturia9. Moreover, tenofovir-treated rats exhibited an imbalance in redox homeostasis and reduced renal expression of endothelial nitric oxide synthase (eNOS), indicating renovascular dysfunction that may contribute to hypertension10. Tenofovir-induced nephrotoxicity has been reported in approximately 15% of patients after 2–9 years of treatment11 and its side effects are mainly attributed to disruption of the nitric oxide (NO) cascade, activation of the renin-angiotensin-aldosterone system (RAAS), and interference with both mitochondrial enzymatic antioxidant system and the Nrf2/HO-1 signaling pathway9,10.
Dapagliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, is a hypoglycemic drug originally developed for the treatment of diabetes mellitus (DM). However, beyond its hypoglycemic properties, dapagliflozin has demonstrated robust cardio-renal protective effects in large-scale clinical trials such as EMPA-REG (Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients), CANVAS (Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes), CREDENCE (Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation), and DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease), including populations with and without DM 12. In addition, dapagliflozin has shown beneficial effects in nephrotoxicity models of colistin13, cyclosporine A 14, gentamicin15 and cisplatin16,17. Although the mechanisms underlying the pleiotropic actions of SGLT2 inhibitors are not fully understood, their renoprotective effects appear to be multifactorial and independent of glycemic control. The protection of kidney structure and function may result from the modulation of redox state, apoptotic signaling pathways, and inflammatory mediators12,18,19. Thus, SGLT2 inhibitors may represent a potential adjunct or alternative strategy for the management of CKD, regardless of diabetic status20. Considering the pleiotropic properties of dapagliflozin, the present study aimed to investigate whether its therapeutic actions could mitigate tenofovir-induced nephrotoxicity, thereby supporting kidney function and potentially improving the prognosis and quality of life in individuals living with HIV.
Results
Glomerular filtration rate and hemodynamics studies
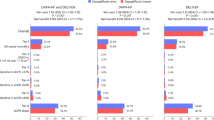
The animals did not show significant differences in body weight, since diet intake was similar among groups, ~ 25 g/day (Table 1). Tenofovir-treated rats showed impaired renal function compared to C and DAPA rats. TDF + DAPA group presented a full recovery in renal function compared to TDF group (Table 1), indicating that dapagliflozin was able to reestablish glomerular filtration rate (GFR) in tenofovir-induced nephrotoxicity. In addition to the restoration of renal function, TDF + DAPA group showed a remarkable improvement in the hemodynamic parameters. TDF group exhibited a higher MAP, a diminished RBF and an augmented RVR compared to C and DAPA groups. Treatment with dapagliflozin reduced MAP, increased RBF and decreased RVR in the TDF + DAPA rats compared to the TDF rats (Table 1). Hypertension was accompanied by renovascular alterations. Tenofovir-treated rats exhibited downregulated protein expression of eNOS compared to C and DAPA rats. TDF + DAPA group presented a reestablishment in the expression of this enzyme compared to C and DAPA groups (Fig. 1).
Semiquantitative immunoblotting for eNOS expression in rat kidney tissue. (a) eNOS densitometric analysis of samples from C, DAPA, TDF and TDF + DAPA rats. (b) Representative immunoblots which reacted with anti-eNOS revealing a band of 140 kDa. All Western Blot experiments were performed in biological replicates (n = 6–8 each group) across multiple gels, each with their respective loading controls. Original blots (uncropped images) are presented in the supplementary Fig. 1S in the supplementary files. Values are means ± SEM. ap<0.001 vs. C; dp<0.001 vs. DAPA; gp<0.001 vs. TDF. C, control; DAPA, dapagliflozin; TDF, tenofovir.
The effects of pro-oxidants and antioxidants signaling pathways on the modulation of redox state
TDF group exhibited higher plasma and renal tissue TBARS levels and lower GSH concentration compared to C and DAPA groups. Treatment with dapagliflozin led to a partial recovery of both plasma and renal TBARS levels, as well as, GSH concentration in the TDF + DAPA group compared to the TDF group (Table 1). Supporting this data, we found increased renal protein expression of NOX4 in the TDF group compared to the C and DAPA groups. Dapagliflozin administration notably reduced the renal expression of this enzyme in the TDF + DAPA rats compared to the TDF rats (Fig. 2). Furthermore, tenofovir-treated rats showed a decreased renal protein expression of SIRT1, Nrf2 and HO-1 compared to C and DAPA rats. TDF + DAPA group exhibited a significant increase in the expression of these Nrf2/HO-1 signaling pathway components (Fig. 2). Similarly, we observed a slight reduction in both renal expressions of MnSOD and CuZnSOD, main components of the mitochondrial enzymatic system, in the TDF group compared to C and DAPA groups. Treatment with dapagliflozin considerably enhanced the renal protein expression of these components (Fig. 2). Altogether, these findings suggest that dapagliflozin is associated with redox state maintenance probably through the modulation of NOX4 and the restoration of the constitutive antioxidant systems.
Semiquantitative immunoblotting for oxidative stress-related components expression in rat kidney tissue. Densitometric analysis of (a) NOX4, (b) SIRT1, (c) Nrf2, (d) HO-1, (e) MnSOD and (f) CuZnSOD of samples from C, DAPA, TDF and TDF + DAPA rats. (g) Representative immunoblots which reacted with anti- NOX4 (82 kDa), anti-SIRT1 (82 kDa), anti-Nrf2 (90 kDa), anti-HO-1 (32 kDa), anti-MnSOD (25 kDa) and anti-CuZnSOD (16 kDa). All Western Blot experiments were performed in biological replicates (n = 6–8 each group) across multiple gels, each with their respective loading controls. Original blots (uncropped images) are presented in the Supplementary Figs. 2 S(I), 2 S(II) and 2 S(III) in the supplementary files. Values are means ± SEM. ap<0.001, bp<0.01 and cp<0.05 vs. C; dp<0.001, ep<0.01 and fp<0.05 vs. DAPA; gp<0.001 vs. TDF. C, control; DAPA, dapagliflozin; TDF, tenofovir.
Activation of PARP-1 by oxidative stress and inflammation/cell death outcomes
Oxidative stress can lead to the activation of PARP-1, resulting in inflammation and cell death. TDF group showed a significant increase in PARP-1 renal protein expression compared to C and DAPA groups. Treatment with dapagliflozin restored this DNA repair enzyme in the TDF + DAPA rats compared to the C and DAPA rats (Fig. 3).
Semiquantitative immunoblotting for inflammation-related molecules expression in rat kidney tissue. Densitometric analysis of (a) PARP-1, (b) TLR4 and (c) pNFκB of samples from C, DAPA, TDF and TDF + DAPA rats. (d) Representative immunoblots which reacted with anti-PARP-1 (89 kDa), anti-TLR4 (90 ~ 120 kDa) and anti- pNFκB (65 kDa). All Western Blot experiments were performed in biological replicates (n = 6–8 each group) across multiple gels, each with their respective loading controls. Original blots (uncropped images) are presented in the supplementary Figs. 3 S(I) and 3 S(II) in the supplementary files. Values are means ± SEM. bp<0.01 and cp<0.05 vs. C; ep<0.01 and fp<0.05 vs. DAPA; gp<0.001 and hp<0.01 vs. TDF. C, control; DAPA, dapagliflozin; TDF, tenofovir.
PARP-1 interacts with TLR4 and NFκB signaling pathways, leading to the production of inflammatory mediators. Renal protein expression of TLR4 and NFκB were higher in the TDF rats than in the C and DAPA rats. Dapagliflozin treatment reduced the renal protein expression of both TLR4 and NFκB in the TDF + DAPA group compared to the TDF group (Fig. 3). Likewise, tenofovir-treated animals presented higher concentration of pro-inflammatory interleukins 1β, 6 and 12 and a decreased concentration of the anti-inflammatory interleukin 10 compared to the C and DAPA animals. TDF + DAPA group showed a reduction in the expression of pro-inflammatory interleukins and an increase in the expression of the anti-inflammatory interleukin (Table 1). Therefore, dapagliflozin treatment decreased the activation of the TLR4/NFκB signaling pathway, modulating the recruitment of inflammatory cells and molecules.
The pro-apoptotic component Bax exhibited higher renal protein expression in TDF group while the pro-survival component Bcl-2 displayed a diminished renal protein expression in the same group compared to C and DAPA groups. Dapagliflozin treatment reestablished renal protein abundance of Bax, whereas increased the renal expression of Bcl-2. In fact, there was almost a two-fold increase in Bax/Bcl-2 ratio in the TDF group compared to the C and DAPA groups. On the other hand, TDF + DAPA rats presented the Bax/Bcl-2 ratio reduced to control levels (Fig. 4). Moreover, tenofovir-treated animals showed increased renal protein expression of cytochrome c compared to C and DAPA animals. TDF + DAPA group exhibited a decrease in this pro-apoptotic component compared to TDF group. Similarly, TDF group presented a higher renal protein expression of caspase 3 compared to C and DAPA groups. Dapagliflozin administration restored this parameter in the TDF + DAPA group compared to the TDF group (Fig. 4). These results suggest a protective effect of dapagliflozin on renal apoptosis followed by tenofovir administration.
Semiquantitative immunoblotting for apoptosis-related components expression in rat kidney tissue. Densitometric analysis of (a) Bax, (b) Cytochrome C, (c) Bcl-2 and (d) caspase 3 of samples from C, DAPA, TDF and TDF + DAPA rats. (e) Alterations (fold change) in Bax/Bcl-2. (f) Representative immunoblots which reacted with anti-Bax (20 kDa), anti-Cytochrome C (15 kDa), anti- Blc-2 (23 kDa) and anti-caspase 3 (35 kDa). All Western Blot experiments were performed in biological replicates (n = 6–8 each group) across multiple gels, each with their respective loading controls. Original blots (uncropped images) are presented in the supplementary Fig. 4S in the supplementary files. Values are means ± SEM. ap<0.001, bp<0.01 and cp<0.05 vs. C; dp<0.001, ep<0.01 and fp<0.05 vs. DAPA; gp<0.001 and hp<0.01 vs. TDF. C, control; DAPA, dapagliflozin; TDF, tenofovir.
Kidney injury and renal fibrosis
TDF group showed mild morphological changes including tubular cell necrosis, areas of denuded basement membrane, flattening of proximal tubular cells with brush border loss and tubular atrophy or dilatation. TDF + DAPA rats presented a significant decrease in tubular injury score compared to TDF rats (Fig. 5). Corroborating this data, tenofovir-treated rats exhibited an increased renal expression of TGF-β1 compared to C rats. Dapagliflozin administration reduced this parameter in the TDF + DAPA group compared to the TDF group (Table 1). Moreover, TDF rats showed a higher renal concentration of collagen 3 (COL3) compared to C and DAPA rats. Treatment with dapagliflozin reduced COL3 renal concentration in the TDF + DAPA group compared to the TDF group (Table 1).
Tubular injury score in the renal cortex evaluated at the end of the protocol. (b) Bar graph of tubular injury score values. (a) Representative photomicrographs of renal histological changes from a C (n = 7), DAPA (n = 6), TDF (n = 7) and TDF + DAPA (n = 8) rat (x400). Values are means ± SEM. ap<0.001 vs. C; dp<0.001 vs. DAPA; hp<0.01 vs. TDF. C, control; DAPA, dapagliflozin; TDF, tenofovir.
Discussion
The number of individuals infected with HIV has been increasing over the years. However, the introduction of ART has significantly altered the progression of acquired immunodeficiency syndrome (AIDS) and improved the quality of life of patients2. Long-term use of tenofovir is associated with nephrotoxicity, leading to AKI or CKD4. The present study demonstrated that tenofovir administration led to impaired renal function, hypertension, endothelial dysfunction, oxidative stress, apoptosis and inflammation. Our results revealed that dapagliflozin treatment improved renal function, normalized MAP and RBF, and reduced RVR in the TDF + DAPA rats. Furthermore, dapagliflozin attenuated renal injury and oxidative imbalances by modulating key oxidant/antioxidant signaling pathways, thereby decreasing levels of inflammatory and apoptotic markers.
Clinical studies suggest that SGLT2 inhibitors improve cardiovascular and renal outcomes in patients with type 2 DM (T2DM)21. Although SGLT2 inhibition produces an initial decline in GFR, clinical trials demonstrated stabilization of renal function in the SGLT2 inhibitor-treated groups, whereas progression of renal disease was observed in the placebo group21. Post hoc analyses of phase III trials showed that dapagliflozin stabilized the decline in estimated GFR for up to 2 years and reduced the urinary albumin/creatinine ratio by 38%–48% in individuals with elevated albuminuria at baseline21. In murine models of nephrotoxicity, dapagliflozin also exhibits a biphasic renal response - an early eGFR decline followed by long-term renoprotection - driven by reductions in oxidative stress, inflammation, fibrosis, and cell death, along with improved mitochondrial function14,15,22. It is important to highlight that rodents, with their faster metabolism and shorter lifespan, respond to disease and treatment more rapidly, allowing effective studies within days to weeks using proportionally higher doses23,24. In the present study, dapagliflozin administration restored renal function and hemodynamic parameters, including the reestablishment of renal eNOS protein expression in the TDF + DAPA group. These findings align with those of Solini et al., who reported that individuals with T2DM treated with dapagliflozin exhibited improved systemic and renal vascular stiffness, as well as enhanced endothelial function - effects observed independently of changes in glucose levels, blood pressure, or natriuresis. The study further suggested that these vascular benefits may be attributed, at least in part, to a reduction in oxidative stress25.
Oxidant agents play an important role in the pathogenesis of tenofovir-induced nephrotoxicity9,10, with NOX emerging as a key cytosolic source of reactive oxygen species (ROS) generation26. Furthermore, an imbalance between ROS production and antioxidant defense systems leads to oxidative stress27. Our results showed that tenofovir administration resulted in increased lipid peroxidation and reduced intracellular antioxidant capacity, as evidenced by higher plasma and tissue TBARS concentrations and lower plasma GSH levels in the TDF group. In agreement with these findings, TDF-treated rats exhibited a significant increase in renal protein expression of NOX4, a NOX isoform highly expressed in the kidney. Treatment with dapagliflozin mitigated the increase in TBARS levels and the reduction in GSH concentration, along with the restoration of NOX4 renal expression in the TDF + DAPA group, indicating that dapagliflozin had a positive impact on redox imbalances by affecting oxidative stress-related signaling pathways. Additionally, tenofovir treatment led to downregulation of key redox-regulating proteins, including SIRT1, Nrf2 and HO-1. Nrf2 is known to play a central role in cellular defense against oxidative stress by regulating antioxidant gene expression28. However, experimental models of CKD have demonstrated that, despite increased oxidative stress and inflammation - conditions that would typically upregulate Nrf2 - renal injury can paradoxically impair its activation and reduce the expression of its target genes28,29,30. Treatment with dapagliflozin restored the redox state balance in the TDF + DAPA group, evidenced by the overactivation of SIRT1, Nrf2 and, consequently, HO-1. Moreover, TDF group presented a slight decrease in the renal protein expression of mitochondrial antioxidant enzymes, including CuZnSOD and MnSOD, likely in response to oxidative stress and renal damage. Dapagliflozin enhanced the expression of these enzymes, further supporting its role in mitigating renal injury through antioxidant mechanisms. Hence, these findings indicate that dapagliflozin effectively attenuates tenofovir-induced nephrotoxicity by reducing oxidative stress via modulation of the SIRT1/Nrf2/HO-1 signaling pathway and enhancing mitochondrial antioxidant defenses. Supporting these observations, Shihab et al. reported that dapagliflozin exhibited protective effects on cardiomyocytes by upregulating the expression of SIRT1 and increasing the expression of MnSOD and other antioxidants, such as catalase. The authors emphasized that SGLT2 inhibitors play a critical role in maintaining redox balance and protecting against mitochondrial dysfunction31.
Another important factor involved in maintaining cellular redox balance is NO 32,33. Our results indicate that the improvement in renal function and hemodynamics is possibly related to the reestablishment of the constitutive antioxidant systems and the restoration of eNOS renal protein expression. In support of our findings, Zhou et al. demonstrated that dapagliflozin restored eNOS Ser1177 phosphorylation and reduced eNOS acetylation through SIRT1 upregulation, thereby mitigating endothelial dysfunction in diabetic mice34. In addition, oxidative and nitrative stress and/or DNA damage are potent triggers for PARP-1 activation35. Our data revealed that tenofovir administration led to PARP-1 overactivation in the TDF group and treatment with dapagliflozin was able to reduce its renal expression in the TDF + DAPA group. PARP-1 plays a key role in upregulating the expression of pro-inflammatory genes, such as NFκB, and/or inducing cell death in injured tissues36. Furthermore, PARP-1 overactivation has also been implicated in renal tubular cell injury and death in models of cisplatin- and gentamicin-induced nephrotoxicity37,38.
Tenofovir induces mitochondrial dysfunction, resulting not only in mtDNA damage and depletion but also in its release. Circulating mtDNA stimulates toll-like receptors (TLRs), resulting in NFκB activation and interferon production39,40,41. Moreover, PARP-1 is known to act both upstream and downstream of TLR4 signaling, regulating the expression of innate immunity-related genes and mediating inflammatory responses42. Our study demonstrated that tenofovir long-term use led to an increase in TLR4 and pNFκB renal protein expression in TDF rats. TDF + DAPA rats showed a significant decrease in the expression of both components, indicating that treatment with dapagliflozin reduced TLR4 and NFκB levels, possibly due to its beneficial effect on redox state balance and PARP-1 modulation.
The balance between pro- and anti-inflammatory cytokines is fundamental to regulate the inflammatory response and may influence the progression of CKD43. Clinical studies have shown that HIV-infected adults treated with ART exhibited higher levels of IL-1β, indicating that its persistent production may be associated with chronic immune activation and inflammation44. Furthermore, the Chronic Renal Failure Cohort (CRIC) study demonstrated that elevated IL-6 concentration in patients with CKD was significantly associated with progression of kidney disease or a 50% reduction in estimated GFR from baseline45. Melchjorsen et al. reported that tenofovir selectively shifted the IL-10/IL-12 balance toward a pro-inflammatory state following stimulation with TLR ligands or bacterial infection in an in vitro experimental model of human primary cells, indicating that tenofovir primes cells for a heightened inflammatory response through increased IL-12 production and suppressed IL-10 secretion46. Our results showed that TDF rats presented an increase in the pro-inflammatory interleukins 1β, 6, and 12 and a decrease in the anti-inflammatory interleukin 10. Treatment with dapagliflozin restored the balance of pro- and anti-inflammatory cytokines in TDF + DAPA rats, suggesting that dapagliflozin exerts modulatory effects on the inflammatory response. Corroborating our data, Qiuxiao et al. reported that dapagliflozin attenuates kidney damage and improves renal function in an ischemia/reperfusion model by modulating the NFκB signaling pathway and suppressing the release of pro-inflammatory mediators47.
Oxidative stress and inflammation further contribute to cellular apoptosis, a process fundamentally involved in the pathogenesis of renal injury across various experimental models. Apoptotic cell death impairs renal function and promote fibrosis47,48. Our study demonstrated that tenofovir administration led to a two-fold increase in the Bax/Bcl-2 ratio, along with higher renal expression of cytochrome c and caspase 3, indicating the activation of both mitochondrial and caspase-mediated apoptotic pathways in tenofovir-induced nephrotoxicity. Treatment with dapagliflozin restored renal protein expression of these apoptotic markers in the TDF + DAPA group, suggesting a protective role against cell death. These findings are supported by both clinical and experimental evidence highlighting the anti-apoptotic and antioxidant properties of SGLT2 inhibitors. Cheng et al. revealed that SGLT2 inhibitors protect against oxidative stress by reducing streptozotocin-induced cell death and ROS in pancreatic β cells in diabetic patients49. Furthermore, Shibusawa et al. reported that dapagliflozin can reduce endoplasmic reticulum-mediated stress and apoptosis in renal tubular epithelial cells50. Another experimental study demonstrated that canagliflozin reduced cisplatin uptake by tubular cells in renal tissue and proximal renal cell culture in rats and protected against proximal tubular apoptosis17. Recently, Deger et al. demonstrated that dapagliflozin administration in a cyclosporine A-induced nephrotoxicity model effectively decreased Bax and caspase-3 levels, increased Bcl-2 expression, and reduced oxidative stress and histopathological damage14. Thus, it is reasonable to assume that dapagliflozin also has a beneficial influence on mitochondrial-mediated cell death pathways in tenofovir-induced renal toxicity.
A large body of evidence suggests that oxidative stress along with inflammation and apoptosis promote renal histopathological changes51. It is well established that long-term use of tenofovir impairs renal function and causes vascular endothelial damage, as well as increases morphological changes in the kidney tubules, resulting in renal disease progression9,10,52. Our study demonstrated that dapagliflozin treatment mitigated tubular injury score and restored renal COL3 expression. Additionally, TDF + DAPA rats presented reduced renal TGF-β1 concentration, indicating that dapagliflozin treatment ameliorated kidney injury probably due to its actions on profibrotic molecules. In agreement with our findings, Zeng et al. revealed that dapagliflozin effectively ameliorated renal fibrosis in a high-adenine diet-induced experimental model by inhibiting the TGF-β1/MAPK signaling pathway22.
In summary, dapagliflozin has a positive impact on renal function, hemodynamics and on the redox state balance through its modulatory effect on the NOX, SIRT1/Nrf2/HO-1 signaling pathway and the mitochondrial antioxidant enzyme system. This SGLT2 inhibitor also ameliorated inflammation by regulating NFκB activation and cytokine production, thereby attenuating renal injury. Finally, dapagliflozin regulated apoptosis by targeting the intrinsic mitochondrial pathway, chiefly through restoring the balance between pro-apoptotic and anti-apoptotic proteins of the Bcl-2 family. The interplay between oxidative stress, apoptosis, and inflammation forms a complex regulatory network. By improving redox balance, dapagliflozin reduces oxidative injury that would otherwise trigger apoptotic cascades and inflammatory responses. Likewise, its anti-inflammatory effects help to attenuate secondary oxidative stress and cell death, creating a positive feedback loop of cellular protection (Fig. 6). Importantly, these effects have been observed without changes in glycemic status, underscoring the pleiotropic and glucose-independent actions of SGLT2 inhibitors in nondiabetic settings (Table 1). Supporting our findings, SGLT2 inhibitors were favorable to kidney morphology and function, strikingly attenuating biomarkers of oxidative stress and inflammatory responses in various animal models of non-diabetic kidney diseases13,15,16,17. Given the limited availability of novel agents for the treatment of kidney disease and the favorable safety profile of SGLT2 inhibitors, our study suggests that dapagliflozin may represent a promising alternative therapeutic strategy to slow the progression of kidney injury and enhance the quality of life in patients receiving tenofovir therapy. However, whether these experimental findings can be effectively translated to patients with non-diabetic kidney disease remains to be determined and warrants further clinical investigation.
Signaling pathways involved in the pathogenesis of tenofovir-induced nephrotoxicity. Increased tenofovir concentration in the proximal tubular cell triggers multiple cellular processes that lead to increased ROS production. ROS generation influences the redox state balance, leads to mitochondrial dysfunction, and releases cytokines and chemokines, which recruit immune cells, triggering inflammatory processes. ROS also increases Bax/Bcl2 ratio in the mitochondrial membrane that activates caspase-3, resulting in apoptosis. In addition, higher ROS levels activate the TGFβ pathway, leading to extracellular matrix accumulation. Altogether, these effects can promote tubulointerstitial fibrosis and subsequent renal tissue damage, resulting in the clinical manifestations observed in the early stages of tenofovir-induced nephrotoxicity. Figure kindly elaborated by the Projeto Homem Virtual – FMUSP, Department of Telemedicine.
Methods
Experimental protocol
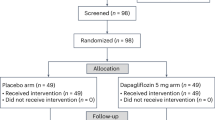
Male Wistar rats weighing 180–200 g were obtained from the animal facilities of the University of São Paulo - Institute of Biomedical Sciences. During the 45-day protocol, we kept our animals at controlled temperature (23 ± 1 °C) with a light/dark cycle of 12/12 hours. Rats received a standard diet (Nuvilab, PR, Brazil) added with tenofovir (300 mg/kg food equivalent to approximately 30 mg/kg BW) and/or dapagliflozin (20 mg/kg food equivalent to approximately 1,6 mg/kg BW) and had free access to tap water. Drug-infused food was freshly prepared and weighed to match the total calculated dose per cage based on average body weight, and animals were allowed to feed under supervision to confirm complete consumption. Rats were allocated to the following groups: Control (n = 7), received a standard diet for 45 days; DAPA (n = 6), received a standard diet for 45 days added with dapagliflozin in the last 15 days; TDF (n = 7), received a standard diet added with tenofovir for 45 days; and TDF + DAPA (n = 8), received a standard diet added with tenofovir for 45 days and dapagliflozin in the last 15 days. The chosen doses of tenofovir and dapagliflozin were based on previous experimental studies10,52,53,54. We conducted all the experimental procedures in accordance with the guidelines outlined and approved by the local Research Ethics Committee (CEUA-HCFMUSP, protocol number 1986/2023).
Inulin clearance and hemodynamic studies
On day 45, we anesthetized the animals with sodium thiopental (50 mg/Kg BW) and then we cannulated the trachea with a PE-240 catheter for spontaneous breathing. The jugular vein was cannulated with a PE-60 catheter for infusion of inulin and fluids. To monitor mean arterial pressure (MAP, mmHg) and collect blood samples, the right femoral artery was catheterized with a PE-50 catheter. We assessed MAP with a data acquisition system (MP100; Biopac Systems, CA, USA). To collect urine samples, we cannulated the bladder with a PE-240 catheter by suprapubic incision. After the surgical procedure, a loading dose of inulin (100 mg/Kg BW diluted in 1 mL of 0.9% saline) was administered through the jugular vein. A constant infusion of inulin (10 mg/Kg BW) was started and continued at 0.04 mL/min throughout the whole experiment. We collected three urine samples at 30-min intervals. Blood samples were obtained at the beginning and at the end of the experiment. Inulin clearance values represent the mean of three periods. Plasma and urinary inulin were determined by the anthrone method, and the glomerular filtration rate (GFR) data were expressed as mL/min/100 g BW 55,56. To measure renal blood flow (RBF, mL/min), we made a median incision and dissected the left renal pedicle for isolating the renal artery. An ultrasonic flow probe was placed around the exposed renal artery, and RBF was measured with an ultrasonic flow meter (T402; Transonic Systems, MD, USA). We divided blood pressure by RBF to calculate renal vascular resistance (RVR, mmHg/mL/min). At the end of the experiments, rats were euthanized via sodium thiopental overdose.
Plasma glucose dosage
We collected blood samples (no fasting) following the clearance studies to assess plasma glucose levels using a colorimetric assay kit (Labtest Diagnóstica, Minas Gerais, Brazil).
Tissue sample preparation
After blood samples collection, we perfused the kidneys with a phosphate-buffered solution (PBS, pH 7.4). We froze the right kidneys in liquid nitrogen and stored at -80 °C for western blotting, ELISA and luminex assay. The left kidneys were removed and a fragment of the renal tissue was fixed in methacarn solution (60% methanol, 30% chloroform, 10% glacial acetic acid) for 24 h and replaced by 70% alcohol thereafter. The kidney blocks were embedded in paraffin and cut into 4-µm sections for histological studies.
Total protein isolation
Kidney samples were homogenized in ice-cold isolation solution containing a protease inhibitor cocktail (Sigma Chemical Company, MO, USA) with a homogenizer (Polytron PT10-35). Homogenates were centrifuged at 4,000 rpm for 30 min at 4 °C to remove nuclei and cell debris. Supernatants were isolated and protein was quantified by Bradford assay (Bio-Rad Laboratories, CA, USA).
Western blot assay
For western blot analysis, 25 ~ 100 µg of total kidney protein were separated on SDS-polyacrylamide minigels by electrophoresis57. After transfer by electroelution to PVDF membranes (GE Healthcare Limited, Little Chalfont, UK), blots were blocked for 1 h with 5% nonfat milk in tris-buffered saline solution. Blots were then incubated with primary antibodies for anti-NOX4 (1:4,000; Elabscience E-AB-70215, TX, USA); anti-Sirt1 (1:10,000; Boster Biological Technology A00018-1, CA, USA); anti-Nrf2 (1:1,000; Cayman Chemicals 10214, MI, USA); anti-HO-1 (1:200; Enzo Life Science ADI-SPA-895, NY, USA); anti-CuZnSOD and anti-MnSOD (1:20,000; Cayman Chemicals 37087 / 10011389, MI, USA), anti-Bax, anti-Bcl-2 and anti-caspase 3 (1:1,000; Cell Signaling 2772-S / 3869-S / 9662, MA, USA), anti-cytochrome C (1:5,000; Abcam ab90529, MA, USA); anti-PARP-1 and anti-NFkB p65 (1:1,000; Santa Cruz Biotechnology sc-53643 / sc-33039 Ser311, CA, USA); anti-TLR4 (1:250; Santa Cruz Biotechnology sc-293072, CA, USA); anti-e-NOS (1:500; BD Bioscience 610296, CA, USA). The labeling was visualized with a horseradish peroxidase-conjugated secondary antibody (anti-mouse or anti-rabbit, Sigma Chemical A9044 / A9169, MO, USA) and enhanced chemiluminescence detection (Cytiva, Amersham, Buckingshire, UK). Kidney protein levels were further analyzed with a gel documentation system (ChemiDoc TM Imaging System, Biorad, Hercules, CA, USA) and the software Image J for Windows (Image J-NIH Image). We used densitometry to quantitatively analyze the protein levels, normalizing the bands to β-actin expression (anti-β-actin, Sigma Chemical A2228, MO, USA).
ELISA in renal tissue
We assessed Transforming Growth Factor Beta 1 (TGF-β1, ng/µg protein) and Collagen Type 3 (COL3, pg/µg protein) in renal tissue by ELISA using commercial kits (Elabscience®, TX, USA). The detection system and quantification followed the protocols described by the manufacturer. The absorbances were obtained using the Epoch/2 device (Biotek Instruments, VE, USA).
Luminex assay in renal tissue
To determine renal tissue levels of IL-1β, IL-6, IL-10, and IL-12, we used a Bio-Plex cytokine assay kit (Milliplex® Rat Cytokine/Chemokine Magnetic Bead Panel RECYTMAG-65k, Millipore, MA, USA). The assay was read on the Bio-Plex suspension array system, and the data were analyzed with Bio-Plex Manager software, version 4.0 58.
Light microscopy
Four-micrometer histological sections of kidney tissue were stained with Hematoxylin-eosin (HE) and examined under light microscopy. For the evaluation of renal damage, 40–60 grid fields (x400 magnification) measuring 0.245 mm2 were evaluated by graded scores according to the following criteria: (0), less than 5% of the field showing tubular epithelial swelling, vacuolar degeneration, necrosis, and desquamation; (I), 5–25% of the field presenting renal lesions; (II), involvement of 25–50% with renal damage; (III), 50–75% of damaged area; and (IV), more than 75% of the grid field presenting renal lesions. To minimize bias during the morphometric examination, the observer was blinded to the treatment groups. The mean score for each rat and the mean score for each group were calculated59,60. For histomorphometry, the images obtained by microscopy were captured on a computer screen via an image analyzer software (NIS-Elements D 5.42.03.64 bit, Nikon, Tokio, Japan).
Reactive oxygen metabolites assessment
Plasma (nmol/mL) and tissue (nmol/mg protein) levels of thiobarbituric acid reactive substances (TBARS) were assessed by ELISA using TBARS Assay Kit (Cayman Chemicals, MI, USA). The detection system and quantification followed the protocols provided by the manufacturer. The absorbances were obtained using the Epoch/2 device (Biotek Instruments, VE, USA). Glutathione (GSH) was determined in total blood by the method of Sedlak and Lindsay61. Whole blood was processed by addition of four volumes of ice-cold 5% (W/V) metaphosphoric acid (Sigma Chemical, St. Louis, MO, USA) and centrifuged at 14,000× g for 10 min. This assay consists of reacting the supernatants of the total blood with Ellman’s reagent to produce a yellow pigment measured spectrophotometrically at 412 nm. The GSH was quantified by mean of standard curve and reported as µmol/mL 62.
Statistical analysis
All quantitative data were expressed as mean ± SEM. Differences among groups were analyzed with GraphPad Prism 5.0 software (GraphPad Software, CA, USA) by one-way analysis of variance followed by the Student–Newman–Keuls test. Values of p < 0.05 were considered statistically significant.
Data availability
All data supporting the findings of this study are available within the article and the supplementary file. Further inquiries can be directed to the corresponding author.
References
WHO. (2024). https://unaids.org.br/estatisticas/.
Campos, P., Ortiz, A. & Soto, K. HIV and kidney diseases: 35 years of history and consequences. Clin. Kidney J. 9, 772–781. https://doi.org/10.1093/ckj/sfw104 (2016).
Milian, L. et al. Tenofovir-induced toxicity in renal proximal tubular epithelial cells: involvement of mitochondria. Aids 31, 1679–1684. https://doi.org/10.1097/QAD.0000000000001572 (2017).
Fernandez-Fernandez, B. et al. Tenofovir nephrotoxicity: 2011 update. AIDS Res Treat 354908, (2011). https://doi.org/10.1155/2011/354908 (2011).
Cooper, R. D. et al. Systematic review and meta-analysis: renal safety of Tenofovir disoproxil fumarate in HIV-infected patients. Clin. Infect. Diseases: Official Publication Infect. Dis. Soc. Am. 51, 496–505. https://doi.org/10.1086/655681 (2010).
Irizarry-Alvarado, J. M., Dwyer, J. P., Brumble, L. M., Alvarez, S. & Mendez, J. C. Proximal tubular dysfunction associated with Tenofovir and didanosine causing Fanconi syndrome and diabetes insipidus: a report of 3 cases. AIDS Read. 19, 114–121 (2009).
Parsonage, M. J., Wilkins, E. G., Snowden, N., Issa, B. G. & Savage, M. W. The development of hypophosphataemic osteomalacia with myopathy in two patients with HIV infection receiving Tenofovir therapy. HIV Med. 6, 341–346. https://doi.org/10.1111/j.1468-1293.2005.00318.x (2005).
Perrot, S., Aslangul, E., Szwebel, T., Caillat-Vigneron, N. & Le Jeunne, C. Bone pain due to fractures revealing osteomalacia related to tenofovir-induced proximal renal tubular dysfunction in a human immunodeficiency virus-infected patient. J. Clin. Rheumatology: Practical Rep. Rheumatic Musculoskelet. Dis. 15, 72–74. https://doi.org/10.1097/RHU.0b013e31819c20d8 (2009).
Canale, D. et al. Vitamin D deficiency aggravates nephrotoxicity, hypertension and dyslipidemia caused by tenofovir: role of oxidative stress and renin-angiotensin system. PloS One. 9, e103055. https://doi.org/10.1371/journal.pone.0103055 (2014).
Nascimento, M. M. et al. Treatment with beta-blocker nebivolol ameliorates oxidative stress and endothelial dysfunction in tenofovir-induced nephrotoxicity in rats. Front. Med. 9, 953749. https://doi.org/10.3389/fmed.2022.953749 (2022).
Jafari, A., Khalili, H. & Dashti-Khavidaki, S. Tenofovir-induced nephrotoxicity: incidence, mechanism, risk factors, prognosis and proposed agents for prevention. Eur. J. Clin. Pharmacol. 70, 1029–1040. https://doi.org/10.1007/s00228-014-1712-z (2014).
Heerspink, H. J. L. et al. Dapagliflozin in patients with chronic kidney disease. N Engl. J. Med. 383, 1436–1446. https://doi.org/10.1056/NEJMoa2024816 (2020).
Kabel, A. M. & Salama, S. A. Effect of taxifolin/dapagliflozin combination on colistin-induced nephrotoxicity in rats. Hum. Exp. Toxicol. 40, 1767–1780. https://doi.org/10.1177/09603271211010906 (2021).
Deger, M. et al. Protective effect of Dapagliflozin against cyclosporine A-induced nephrotoxicity. Drug Chem. Toxicol. 45, 2637–2643. https://doi.org/10.1080/01480545.2021.1979996 (2022).
Mohamed, D. I., Khairy, E., Saad, S. S. T., Habib, E. K. & Hamouda, M. A. Potential protective effects of Dapagliflozin in gentamicin induced nephrotoxicity rat model via modulation of apoptosis associated MiRNAs. Gene 707, 198–204. https://doi.org/10.1016/j.gene.2019.05.009 (2019).
Abdelrahman, A. M. et al. Effect of canagliflozin, a sodium glucose co-transporter 2 inhibitor, on cisplatin-induced nephrotoxicity in mice. Naunyn Schmiedebergs Arch. Pharmacol. 392, 45–53. https://doi.org/10.1007/s00210-018-1564-7 (2019).
Song, Z., Zhu, J., Wei, Q., Dong, G. & Dong, Z. Canagliflozin reduces cisplatin uptake and activates Akt to protect against cisplatin-induced nephrotoxicity. Am. J. Physiol. Renal. Physiol. 318, F1041–F1052. https://doi.org/10.1152/ajprenal.00512.2019 (2020).
Jaikumkao, K. et al. Dapagliflozin and Metformin in combination ameliorates diabetic nephropathy by suppressing oxidative stress, inflammation, and apoptosis and activating autophagy in diabetic rats. Biochim. Et Biophys. Acta Mol. Basis Disease. 1870, 166912. https://doi.org/10.1016/j.bbadis.2023.166912 (2024).
Luna-Marco, C. et al. Cardiovascular benefits of SGLT2 inhibitors and GLP-1 receptor agonists through effects on mitochondrial function and oxidative stress. Free Radic. Biol. Med. 213, 19–35. https://doi.org/10.1016/j.freeradbiomed.2024.01.015 (2024).
Isidto, R. et al. Emerging role of Sodium-Glucose Co-Transporter 2 inhibitors for the treatment of chronic kidney disease. Int. J. Nephrol. Renovasc Dis. 16, 43–57. https://doi.org/10.2147/IJNRD.S387262 (2023).
Hallow, K. M. et al. Renal effects of Dapagliflozin in people with and without diabetes with moderate or severe renal dysfunction: prospective modeling of an ongoing clinical trial. J. Pharmacol. Exp. Ther. 375, 76–91. https://doi.org/10.1124/jpet.120.000040 (2020).
Zeng, J. et al. Dapagliflozin alleviates renal fibrosis in a mouse model of adenine-induced renal injury by inhibiting TGF-beta1/MAPK mediated mitochondrial damage. Front. Pharmacol. 14, 1095487. https://doi.org/10.3389/fphar.2023.1095487 (2023).
Le Bras, A. Humanized mouse models of drug metabolism. Lab Anim. 53, 87. https://doi.org/10.1038/s41684-024-01357-8 (2024).
Perlman, R. L. Mouse models of human disease: An evolutionary perspective. Evolution, medicine, and public health 170–176, (2016). https://doi.org/10.1093/emph/eow014 (2016).
Solini, A. et al. The effects of Dapagliflozin on systemic and renal vascular function display an epigenetic signature. J. Clin. Endocrinol. Metab. 104, 4253–4263. https://doi.org/10.1210/jc.2019-00706 (2019).
Younis, N. N., Elsherbiny, N. M., Shaheen, M. A. & Elseweidy, M. M. Modulation of NADPH oxidase and Nrf2/HO-1 pathway by Vanillin in cisplatin-induced nephrotoxicity in rats. J. Pharm. Pharmacol. 72, 1546–1555. https://doi.org/10.1111/jphp.13340 (2020).
Coats, A. & Jain, S. Protective effects of nebivolol from oxidative stress to prevent hypertension-related target organ damage. J. Hum. Hypertens. 31, 376–381. https://doi.org/10.1038/jhh.2017.8 (2017).
Zoja, C., Benigni, A. & Remuzzi, G. The Nrf2 pathway in the progression of renal disease. Nephrol. Dialysis Transplantation: Official Publication Eur. Dialysis Transpl. Association - Eur. Ren. Association. 29 Suppl 1, i19–i24. https://doi.org/10.1093/ndt/gft224 (2014).
Kim, H. J., Sato, T., Rodriguez-Iturbe, B. & Vaziri, N. D. Role of intrarenal angiotensin system activation, oxidative stress, inflammation, and impaired nuclear factor-erythroid-2-related factor 2 activity in the progression of focal glomerulosclerosis. J. Pharmacol. Exp. Ther. 337, 583–590. https://doi.org/10.1124/jpet.110.175828 (2011).
Kim, H. J. & Vaziri, N. D. Contribution of impaired Nrf2-Keap1 pathway to oxidative stress and inflammation in chronic renal failure. Am. J. Physiol. Renal. Physiol. 298, F662–671. https://doi.org/10.1152/ajprenal.00421.2009 (2010).
Shihab, E. M., Kadhim, H. M. & Shahooth, S. S. Dapagliflozin mitigates oxidative stress, inflammatory, and histopathological markers of aging in mice. J. Med. Life. 17, 157–163. https://doi.org/10.25122/jml-2023-0343 (2024).
Joshi, S., Peck, A. B. & Khan, S. R. NADPH oxidase as a therapeutic target for oxalate induced injury in kidneys. Oxid Med Cell Longev 462361, (2013). https://doi.org/10.1155/2013/462361 (2013).
Ogura, Y., Kitada, M. & Koya, D. Sirtuins and renal oxidative stress. Antioxid. (Basel). 10 https://doi.org/10.3390/antiox10081198 (2021).
Zhou, Y., Tai, S., Zhang, N., Fu, L. & Wang, Y. Dapagliflozin prevents oxidative stress-induced endothelial dysfunction via Sirtuin 1 activation. Biomed. Pharmacother. 165, 115213. https://doi.org/10.1016/j.biopha.2023.115213 (2023).
Ramamoorthy, H., Abraham, P., Isaac, B. & Selvakumar, D. Mitochondrial pathway of apoptosis and necrosis contribute to Tenofovir disoproxil fumarate-induced renal damage in rats. Hum. Exp. Toxicol. 38, 288–302. https://doi.org/10.1177/0960327118802619 (2019).
Ba, X. & Garg, N. J. Signaling mechanism of poly(ADP-ribose) polymerase-1 (PARP-1) in inflammatory diseases. Am. J. Pathol. 178, 946–955. https://doi.org/10.1016/j.ajpath.2010.12.004 (2011).
Biro, A. et al. The effect of Poly (ADP-ribose) Polymerase Inhibition on aminoglycoside-induced acute tubular necrosis in rats. Clin. Nephrol. 85, 226–234. https://doi.org/10.5414/CN108697 (2016).
Kim, J. Poly(ADP-ribose) polymerase activation induces high mobility group box 1 release from proximal tubular cells during cisplatin nephrotoxicity. Physiol. Res. 65, 333–340. https://doi.org/10.33549/physiolres.932948 (2016).
Mitrofanova, A., Fontanella, A. M., Burke, G. W., Merscher, S. & Fornoni, A. Mitochondrial Contribution to Inflammation in Diabetic Kidney Disease. Cells 11, (2022). https://doi.org/10.3390/cells11223635
Vazi, S., van Zyl, S., -de Wet, V., Tiloke, C. & R. & Inflammatory properties of Tenofovir in human liver cells. Health Sci. Rev. 8, 100114. https://doi.org/10.1016/j.hsr.2023.100114 (2023).
Yao, Y. et al. Dexmedetomidine alleviates lipopolysaccharide-induced acute kidney injury by inhibiting the NLRP3 inflammasome activation via regulating the TLR4/NOX4/NF-kappaB pathway. J. Cell. Biochem. 120, 18509–18523. https://doi.org/10.1002/jcb.29173 (2019).
Kim, J., Long, K. E., Tang, K. & Padanilam, B. J. Poly(ADP-ribose) polymerase 1 activation is required for cisplatin nephrotoxicity. Kidney Int. 82, 193–203. https://doi.org/10.1038/ki.2012.64 (2012).
Okada, R. et al. Pro-/anti-inflammatory cytokine gene polymorphisms and chronic kidney disease: a cross-sectional study. BMC Nephrol. 13 https://doi.org/10.1186/1471-2369-13-2 (2012).
Nabatanzi, R., Ssekamatte, P., Castelnuovo, B., Kambugu, A. & Nakanjako, D. Increased levels of Caspase-1 and IL-1beta among adults with persistent immune activation after 12 years of suppressive antiretroviral therapy in the infectious diseases Institute HIV treatment cohort. Open. Forum Infect. Dis. 10, ofad539. https://doi.org/10.1093/ofid/ofad539 (2023).
Amdur, R. L. et al. Inflammation and progression of CKD: the CRIC study. Clin. J. Am. Soc. Nephrology: CJASN. 11, 1546–1556. https://doi.org/10.2215/CJN.13121215 (2016).
Melchjorsen, J. et al. Tenofovir selectively regulates production of inflammatory cytokines and shifts the IL-12/IL-10 balance in human primary cells. J. Acquir. Immune Defic. Syndr. 57, 265–275. https://doi.org/10.1097/QAI.0b013e3182185276 (2011).
Qiuxiao, Z. et al. Protective effects and mechanisms of Dapagliflozin on renal ischemia/reperfusion injury. Transpl. Immunol. 84, 102010. https://doi.org/10.1016/j.trim.2024.102010 (2024).
Benzer, F., Kandemir, F. M., Kucukler, S., Comakli, S. & Caglayan, C. Chemoprotective effects of Curcumin on doxorubicin-induced nephrotoxicity in Wistar rats: by modulating inflammatory cytokines, apoptosis, oxidative stress and oxidative DNA damage. Arch. Physiol. Biochem. 124, 448–457. https://doi.org/10.1080/13813455.2017.1422766 (2018).
Cheng, S. T., Chen, L., Li, S. Y., Mayoux, E. & Leung, P. S. The effects of Empagliflozin, an SGLT2 Inhibitor, on pancreatic beta-Cell mass and glucose homeostasis in type 1 diabetes. PloS One. 11, e0147391. https://doi.org/10.1371/journal.pone.0147391 (2016).
Shibusawa, R. et al. Dapagliflozin rescues Endoplasmic reticulum stress-mediated cell death. Sci. Rep. 9, 9887. https://doi.org/10.1038/s41598-019-46402-6 (2019).
Chen, X., Wei, W., Li, Y., Huang, J. & Ci, X. Hesperetin relieves cisplatin-induced acute kidney injury by mitigating oxidative stress, inflammation and apoptosis. Chemico-Biol. Interact. 308, 269–278. https://doi.org/10.1016/j.cbi.2019.05.040 (2019).
Liborio, A. B. et al. Rosiglitazone reverses tenofovir-induced nephrotoxicity. Kidney Int. 74, 910–918. https://doi.org/10.1038/ki.2008.252 (2008).
Juttla, P. K., Chege, B. M., Mwangi, P. W. & Bukachi, F. Dapagliflozin pretreatment prevents cardiac electrophysiological changes in a diet and streptozotocin induction of type 2 diabetes in rats: A potential new First-Line? J. Experimental Pharmacol. 16, 123–133. https://doi.org/10.2147/JEP.S443169 (2024).
Kingir, Z. B. et al. Effects of Dapagliflozin in experimental sepsis model in rats. Ulusal Travma Ve Acil Cerrahi dergisi = Turkish J. trauma. Emerg. Surgery: TJTES. 25, 213–221. https://doi.org/10.5505/tjtes.2018.82826 (2019).
Delanaye, P. et al. [Measurement of inulin: development]. Ann. Biol. Clin. 69, 273–284. https://doi.org/10.1684/abc.2011.0580 (2011).
White, R. P. & Samson, F. E. Jr. Determination of inulin in plasma and urine by use of anthrone. J. Lab. Clin. Med. 43, 475–478 (1954).
Burnette, W. N. Western blotting: electrophoretic transfer of proteins from sodium Dodecyl sulfate–polyacrylamide gels to unmodified nitrocellulose and radiographic detection with antibody and radioiodinated protein A. Anal. Biochem. 112, 195–203. https://doi.org/10.1016/0003-2697(81)90281-5 (1981).
Rodrigues, C. E. et al. Effects of continuous erythropoietin receptor activator in sepsis-induced acute kidney injury and multi-organ dysfunction. PloS One. 7, e29893. https://doi.org/10.1371/journal.pone.0029893 (2012).
de Braganca, A. C. et al. Vitamin D deficiency aggravates ischemic acute kidney injury in rats. Physiological Rep. 3 https://doi.org/10.14814/phy2.12331 (2015).
Miyaji, T., Kato, A., Yasuda, H., Fujigaki, Y. & Hishida, A. Role of the increase in p21 in cisplatin-induced acute renal failure in rats. J. Am. Soc. Nephrol. 12, 900–908. https://doi.org/10.1681/ASN.V125900 (2001).
Sedlak, J. & Lindsay, R. H. Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with ellman’s reagent. Anal. Biochem. 25, 192–205. https://doi.org/10.1016/0003-2697(68)90092-4 (1968).
Vogt, B. L. & Richie, J. P. Jr. Glutathione depletion and recovery after acute ethanol administration in the aging mouse. Biochem. Pharmacol. 73, 1613–1621. https://doi.org/10.1016/j.bcp.2007.01.033 (2007).
Acknowledgements
This study was supported by grants for Scientific Research (2024/09066-9 DC, 2022/07409-0 RV, 2022/05519-3 AB) by the São Paulo Research Foundation (FAPESP). We would like to thank Gustavo Zagatto, member of the Projeto Homem Virtual – FMUSP, for creating the figure presented in this study, and Dr. Chao Lung Wen, head of the Telemedicine Department at FMUSP, for his support. We also express our gratitude to Dr. Meire Ioshie Hiyane for assistance with the Luminex assay experiments, and to Prof. Dr. Niels Olsen Saraiva Câmara, professor in the Immunology Department at the Institute of Biomedical Sciences, University of São Paulo (ICB-USP), for his valuable contributions.
Author information
Authors and Affiliations
Contributions
Conceptualization: VS and DC. Data curation: VS, AV, MN, DB, MS, CS, AB and DC. Writing and reviewing the original drafting: VS, AB, RV and DC. Editing: AS and DC. All authors approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The animal study was reviewed and approved by Comissão de Ética no Uso de Animais (CEUA) do Hospital das Clínicas da Universidade de São Paulo – protocol n. 1986/2023. Experiments involving animals are described in accordance with ARRIVE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
dos Santos, V.A., Viotto, A.C.R., Nascimento, M.M. et al. Dapagliflozin treatment ameliorates oxidative stress, apoptosis and inflammation in tenofovir-induced nephrotoxicity in rats. Sci Rep 15, 43706 (2025). https://doi.org/10.1038/s41598-025-27555-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-27555-z