Abstract
Nontuberculous mycobacterial pulmonary disease (NTM-PD) is associated with functional decline and limited treatment options, highlighting the need for adjunctive exercise interventions. This study aimed to evaluate the feasibility, safety, and preliminary effects of a 4-week combined supervised and home-based exercise program for patients with NTM-PD. This single-arm feasibility study included 23 outpatients with NTM-PD. The intervention comprised weekly supervised sessions and daily home-based aerobic and resistance training over 4 weeks. The primary outcomes were feasibility parameters (retention, adherence, and safety). The exploratory outcomes included cardiorespiratory fitness (VO₂max), functional capacity (6MWD, 30-s STS), muscle strength, pulmonary function, body composition, and health-related quality of life (quality of life-bronchiectasis domains). Of the 23 enrolled participants, 19 (82.6%) completed the study. All predefined feasibility thresholds were achieved: retention 82.6% (≥ 80% threshold), supervised-session adherence 100% (≥ 80% threshold), and home-based adherence 73.5% (≥ 70% threshold). No serious adverse events occurred. Modest functional improvements were observed: 6MWD increased by 20 m (p = 0.008), and 30-s STS performance improved by 3.5 repetitions (p = 0.010). VO₂max showed minimal changes, although valid measurements were obtained in only 10/18 participants. Health-related quality of life showed mixed results, with only the vitality domain showing a statistically significant change in distribution pattern. Pulmonary function and body composition remained unchanged. A 4-week hybrid exercise program demonstrated feasibility, safety, and acceptability in patients with NTM-PD, with modest short-term functional gains. The brief duration of the intervention may have limited clinically meaningful improvements. These findings support the progression to long-duration randomized controlled trials with enhanced home-based exercise adherence strategies and alternative outcome measures appropriate for this population.
Similar content being viewed by others
Introduction
Nontuberculous mycobacterial pulmonary disease (NTM-PD) is a chronic lung disease caused by environmental mycobacteria other than Mycobacterium tuberculosis and Mycobacterium leprae. The global prevalence of NTM-PD has steadily increased, particularly in aging populations and individuals with preexisting lung conditions1,2,3. In South Korea, the incidence of NTM-PD has exceeded that of tuberculosis since 2021, reflecting a shift in the epidemiology of mycobacterial infections4. Treatment remains challenging because of prolonged use of multidrug regimens, often extending beyond a year, with significant toxicity, poor adherence, and low success rates. Recurrence is common even after microbiological treatment and requires long-term clinical monitoring5,6.
Symptoms such as chronic cough, sputum production, dyspnea, fatigue, and reduced exercise tolerance contribute to declining physical function and health-related quality of life (HRQOL)7. Patients with NTM-PD are often underweight and physically weak8. Decreased skeletal muscle mass has been associated with an increased mortality risk9,10, and recent findings have shown that patients with NTM-PD exhibit systemic weaknesses such as low body mass index (BMI), reduced physical fitness, and increased healthcare burden, which may lead to persistent infection and worse clinical outcomes11,12. Given these challenges, including progressive functional decline and limited treatment options, there is an urgent need for non-pharmacological interventions.
Exercise interventions and pulmonary rehabilitation have been found to ameliorate symptoms and improve exercise capacity and HRQOL in patients with bronchiectasis and chronic obstructive pulmonary disease13,14,15. However, exercise programs for patients with NTM-PD are rare. Previous physiotherapy studies have mainly focused on airway clearance rather than complete physical training9,16, and there are no feasibility studies evaluating structured exercise protocols in this population.
To address this gap, we conducted a feasibility study to inform the design of a future randomized controlled trial (RCT) to evaluate exercise interventions for NTM-PD. We selected a hybrid model combining supervised and home-based components. This hybrid design offers several advantages: first, it reduces the burden of frequent hospital visits for patients who often experience fatigue and reduced exercise tolerance; second, it promotes self-management skills essential for long-term adherence beyond the intervention period; and third, it enhances scalability and real-world applicability, particularly important given the rising prevalence of NTM-PD and limited healthcare resources. This approach aligns with emerging evidence supporting home-based pulmonary rehabilitation in other chronic respiratory conditions17,18. This study aimed to assess feasibility of implementing a 4-week hybrid (supervised plus home-based) exercise program with primary objectives focused on retention, adherence to supervised and home-based components, and safety. In line with methodological recommendations19, our focus was on addressing uncertainties relevant to a future definitive trial rather than testing intervention efficacy.
Methods
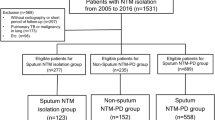
Study design and procedure
This was a prospective, single-center, single-arm feasibility study designed to assess the feasibility of a hybrid exercise intervention for patients with NTM-PD and to inform the design of a future RCT. Exploratory clinical outcomes were collected to estimate changes and variability for future trial planning. This study was conducted between July 2023 and January 2024 at Severance Hospital, a tertiary referral hospital in South Korea. Participants diagnosed with NTM-PD according to established guidelines were recruited20.
The hybrid exercise intervention program involved six visits over a 4-week period (Fig. 1). Center-based physical assessments were performed at baseline (1st visit) and post-intervention (final visit), with an exercise intervention conducted between the 2nd and 5th visits. The intervention comprised both supervised and home-based exercise components, with supervised sessions conducted once weekly for 60 min, while participants performed home-based exercises on the remaining 6 days.
The program comprised body-weight resistance movements selected to enhance core strength, trunk stability, and functional capacity. Representative exercises included: dynamic mobility (modified child’s pose, cobra), trunk and hip stabilization (bird-dog pointer, plank, hip external rotation, posterior pelvic tilt, shoulder bridge), upper body and scapular control (push-ups, wall-assisted scapular upward rotation), and global functional strength (full squat, calf raise, curl-up/crunch). Proper technique was taught during the supervised sessions, and participants were instructed to replicate the prescribed sets and repetitions at home on non-supervised days.
The program goals were as follows: (1) at least 150 min of moderate to vigorous aerobic exercise per week and (2) 1 − 3 sets of the body-weight calisthenics (10 repetitions of twelve exercises) at 40 − 80% of heart rate reserve, with no restriction on rest intervals21,22. One “set” was defined as completing all twelve exercises once through. No handheld weights or equipment were required, making the program suitable for home-based implementation. During each 60-min center-based session, an exercise specialist supervised groups of two to four participants. For the home component, participants were instructed to perform one to three sets of the prescribed body-weight routine, 10 repetitions per exercise, on at least two days per week. Exercise type, duration, and number of sets were logged in a diary that the exercise specialist reviewed at the next session to monitor adherence and provide feedback. This body-weight resistance exercise protocol has been previously validated, demonstrating high feasibility (81.3% completion rate, 83.1% adherence) and effectiveness in improving physical fitness and metabolic outcomes in cardiovascular disease and cancer populations23,24,25.
Participants accumulated aerobic minutes across 5–6 days and completed resistance sets on ≥ 2 days per week. The key components included weekly face-to-face exercise education sessions covering proper exercise techniques and diary use, weekly telephone follow-ups based on motivational interviewing principles to monitor adherence, identify barriers, assess adverse effects, and provide motivational support, and exercise diaries for self-monitoring. The detailed intervention protocol is presented in (Table 1).
Outcome measures
Following the feasibility study guidance, the outcomes were classified into primary feasibility outcomes and exploratory clinical outcomes19. For this feasibility study, thresholds for acceptability were set a priori as ≥ 80% for retention, ≥ 80% for supervised-session adherence, and ≥ 70% for home-based adherence. Outcomes meeting or exceeding these thresholds were considered supportive of feasibility, whereas lower values indicated areas requiring modification prior to a future trial. Where relevant, point estimates are presented with 95% confidence intervals to aid in planning a definitive trial.
Primary outcomes (feasibility)
The primary outcomes focused on feasibility parameters essential for planning a future definitive trial. The retention rate was defined as the proportion of enrolled participants who completed the 4-week post-intervention assessment. Adherence was assessed using two components: supervised session adherence, calculated as the number of supervised sessions attended divided by four; and home-based adherence, derived from exercise diaries and represented in different formats. For home-based adherence, daily participation patterns (Fig. 2) were coded as white for data unavailable (lost diary), hatched for no participation (0 sets), light gray for low to moderate participation (1 − 2 sets), and dark gray for high participation (≥ 3 sets), where one set represented completing all 12 calisthenic exercises once through. Weekly participation patterns (Fig. 3) displayed the proportion of participants meeting resistance exercise adherence targets across each intervention week. Safety was monitored throughout the intervention period, with particular attention to symptoms or events that could interfere with exercise participation. Any adverse events were documented and reviewed by study pulmonologists to determine causality and severity.
Daily exercise adherence patterns of study participants during the 4-week intervention period. Each cell represents daily participation status: White = data unavailable due to lost exercise diary, Diagonal lines (white with hatching) = no participation (0 set), Gray = low to moderate participation (1 − 2 sets), Dark gray = high participation (≥ 3 sets). Participant codes are shown on the left.
Weekly exercise adherence patterns of study participants during the 4-week intervention period. Each cell represents daily participation status: White = data unavailable due to lost exercise diary, Gray = performed ≥ 3 sets of exercise on 1 − 2 days per week, Dark gray = performed ≥ 3 sets of exercise on ≥ 3 days per week. Participant codes are shown on the left.
Additional feasibility indicators included data completeness, defined as the proportion of participants with valid measurements at both time points for each assessment, with diary completeness expressed as weeks with any diary data divided by 4 per participant and summarized at the cohort level. Intervention fidelity was assessed through delivery (the proportion of planned components delivered across four weekly supervised/education sessions) and receipt/enactment (diary completion rates and week-level adherence category distribution). Acceptability was evaluated through indirect indicators, including sustained diary completion and stated intention to continue exercise.
Exploratory clinical outcomes
Exploratory outcomes were collected to estimate changes and variability for future trial planning but not for hypothesis testing. Maximal oxygen consumption (VO₂max) was assessed using the Bruce protocol treadmill cardiopulmonary exercise test at baseline and within 1 week of completing the 4-week intervention26. The protocol began with walking at 2.7 km/h, with the speed and incline increasing every 3 min until exhaustion or clinical termination. The participants wore a non-rebreathing facemask (Rudolph series 7910, Hans Rudolph, USA), and breath-by-breath gas exchange was recorded using a computerized metabolic system (TrueOne 2400, Parvo Medics, USA).
As a subgroup analysis, we evaluated VO₂max data validity using the following three criteria: respiratory exchange ratio ≥ 1.15 or equal to/greater than baseline value, considering the older patient population, heart rate achieving ≥ 90% of age-predicted maximum calculated using the formula (220 - age), and rating of perceived exertion ≥ 17 on the Borg 6 − 20 scale27. A subgroup analysis was performed for participants meeting ≥ 2 of these three criteria to confirm the achievement of valid maximal effort.
The 6WMD was performed once according to standardized guidelines, measuring the distance covered in 6 min28,29. The 30-s STS was performed once, recording the number of full stands completed within 30 s30. The SPPB was administered once, providing a 0 − 12 composite score, including gait speed, balance, and chair rise performance31. Handgrip strength was measured twice on each hand using a Takei A5401 dynamometer (Takei Scientific Instruments, Niigata, Japan), with the highest value recorded32. HRQOL was assessed using the Quality of Life-Bronchiectasis (QOL-B) v3.1 domains standardized to 0 − 100 (higher scores indicating better quality) for physical functioning, role functioning, vitality, emotional functioning, social functioning, health perceptions, and respiratory symptoms; treatment burden was omitted due to incomplete responses33.
Statistical analysis
As this was a feasibility study, the primary analysis focused on descriptive statistics and estimations, rather than on hypothesis testing. Continuous data are reported as medians (IQR). For feasibility outcomes, the retention rate was calculated as participants attending the 4-week post-assessment divided by those enrolled. Supervised adherence was calculated as sessions attended divided by 4; home-based adherence was calculated as recorded divided by prescribed home sessions ×100 among those with ≥ 1 week of diary data. For detailed diary analysis, daily exercise participation in resistance exercise was categorized into three levels (≥ 3 sets, 1 − 2 sets, or 0 sets) based on the number of complete 12-exercise calisthenic routines performed and analyzed across the 4-week intervention period to assess adherence patterns (Fig. 2). Weekly diaries were classified using the World Health Organization 2020 guideline (≥ 150–300 min/week moderate or ≥ 75–150 min/week vigorous activity, or equivalent, plus strength ≥ 2 days/week), with proportions meeting aerobic, strength, and both components reported34. Predefined feasibility thresholds were applied to determine whether the intervention was feasible for progression to a definitive trial.
Exploratory clinical outcomes were analyzed to estimate changes in scores and variability. VO₂max analysis was restricted to participants achieving a valid maximal effort according to predefined criteria. Wilcoxon signed-rank tests were performed only for exploratory purposes, as hypothesis testing was not the primary objective of this feasibility study. All analyses were performed using SPSS version 28.0 (IBM Corp., Armonk, NY, USA).
Results
Participants’ characteristics (n = 19)
Of the 27 patients who received detailed study information, 23 participants were recruited, and 19 (82.6%) completed the program. Among the completers, 15 (78.9%) were female and four (21.1%) were male, with a median age of 66 years ([IQR], 60.0–72.0). The BMI was 19.0 (17.7–21.1) kg/m² (Table 2).
Regarding medical history, four participants (21.1%) had a history of pulmonary tuberculosis, four (21.1%) had a history of solid tumors (thyroid cancer, breast cancer, and colorectal cancer; no lung cancer), three (15.8%) had systemic hypertension, and one (5.3%) was a current smoker. The most common Mycobacterium species were M. avium in nine participants (47.4%), followed by M. abscessus in five participants (26.3%), and M. intracellulare in four participants (21.1%). Three participants (15.8%) had positive sputum acid-fast bacilli smear, and the median disease duration was 39.0 (21.0–74.0) months.
Feasibility outcomes (n = 19)
The exercise program showed high feasibility across the predefined primary outcomes. The retention rate was 82.6% (19/23), exceeding our threshold of ≥ 80%. Adherence to the supervised sessions was 100% (76/76 sessions attended), which was above the 80% threshold.
Home-based adherence, the key indicator of program sustainability, was 73.5%, meeting our predefined threshold of 70%. This was calculated for the 17 participants with available diary data. Across the 4-week intervention period (68 participant-weeks total), participants achieved the weekly target within 50 weeks (73.5%). The weekly adherence patterns are shown in Fig. 3, displaying the proportion of participants meeting full adherence (≥ 3 sets on ≥ 3 days/week) versus partial adherence (≥ 3 sets on 1 − 2 days/week) across each intervention week.
Daily adherence data (Fig. 2) provided detailed insights into exercise participation patterns. Analysis of 476 total exercise days (17 participants × 28 days) revealed that participants performed ≥ 3 sets on 302 days (63.4%), 1 − 2 sets on 140 days (29.4%), and no exercise on 34 days (7.1%). This resulted in 92.8% of the days with at least one set performed, indicating high engagement with the home-based program despite day-to-day variability in exercise volume.
No exercise-related adverse events requiring medical attention or program modification occurred during the 4-week intervention period. Four participants (17.4%) discontinued the study: one due to thoracic vertebral fracture, one due to adverse effects of osteoporosis medication, and two due to withdrawal of consent. The intervention fidelity was high, with all planned supervised sessions delivered (100% delivery), and sustained diary completion was observed among participants with available diaries. The program showed acceptable receipt and enactment, as shown by consistent weekly adherence rates and the participants’ stated intentions to continue exercising beyond the study period.
Changes in outcome variables (n = 18)
Eighteen participants were included in the exploratory outcome analysis (one participant was excluded because of physical limitations) (Table 3). VO₂max showed minimal change from 29.8 mL/kg/min (26.2 − 33.4) at baseline to 28.6 mL/kg/min (24.1 − 33.2) at 4 weeks (p = 0.777). The data of the 10 participants who met the validity criteria are presented in Additional files 1 & 2. The 6-min walk distance improved from 594 m (IQR, 553.4 − 634.6) at baseline to 614 m (554.9 − 673.1) at 4 weeks (p = 0.008). The 30-s STS improved from 13.0 repetitions (10.5 − 15.5) to 16.5 repetitions (14.3 − 18.8) (p = 0.010). SPPB scores remained at ceiling level for most participants (12.0 [12.0 − 12.0] at both time points; p = 0.157), suggesting limited sensitivity for detecting change in this high-functioning cohort. Handgrip strength slightly increased from 23.6 kg (18.7 − 28.6) to 23.7 kg (18.8 − 28.7) (p < 0.001).
HRQOL assessment using QOL-B v3.1 (scores 0 − 100, higher indicating better status) showed variable changes across domains. The vitality domain showed a statistically significant change from 66.6 (33.3–66.6) to 61.1 (52.7–77.7) (p = 0.040), with the median slightly decreasing but the distribution shifting toward higher values. Other QOL-B domains, including physical functioning, role functioning, emotional functioning, social functioning, health perceptions, and respiratory symptoms, showed no significant changes (all p > 0.05). Pulmonary function parameters (forced vital capacity [FVC], forced expiratory volume in 1 s [FEV₁], and FEV₁/FVC) and body composition measures (fat mass and skeletal muscle mass) remained unchanged (all p > 0.05, Table 3).
Discussion
This study demonstrates that a combined supervised and home-based exercise program is feasible, safe, and acceptable for patients with NTM-PD. Primary feasibility outcomes met our predefined thresholds—retention was 82.6% (≥ 80% threshold), supervised-session adherence was 100% (≥ 80% threshold), and home-based adherence reached 73.5% (≥ 70% threshold). These rates compare favorably with feasibility studies of home-based rehabilitation for other chronic respiratory conditions (81.3–83.1%)17,18. Detailed adherence monitoring showed 92.8% of days with at least one set performed and 73.5% of participant-weeks achieving the target of ≥ 3 sets on ≥ 3 days.
The weekly supervised education, telephone follow-up, and exercise diaries likely supported adherence and safety. The image-coded diary summaries enabled rapid feedback and simple monitoring. The diaries facilitated the monitoring and adjustment of training, aligning with the current recommendations for the non-pharmacological management of NTM-PD, where exercise training improves exercise capacity and HRQOL35,36.
Exploratory clinical outcomes showed functional gains in the 6MWD (+ 20 m) and 30-s STS (+ 3.5 repetitions). The minimal clinically important difference (MCID) for the 6-min walk test varies from 14 to 54 m across different populations, with chronic respiratory diseases specifically showing MCIDs of 25–33 m37,38. While the observed improvement of 20 m falls within the broader MCID range, it is below the threshold for chronic respiratory conditions. However, NTM-PD-specific MCID values have not yet been established, limiting interpretation of this change’s clinical significance. Handgrip strength increased by only 0.1 kg, which is unlikely to be clinically meaningful, but relevant given the association between reduced muscle mass and disease severity in patients with NTM-PD9,39. The minimal change in VO₂max (median decrease of 1.15 mL/kg/min in 18 participants) may reflect the short intervention duration or the submaximal nature of exercise training, as short-term interventions often show functional improvements before changes in maximal exercise capacity appear40. Only 10 of the 18 participants met the validity criteria for maximal effort at both time points, highlighting the difficulty of conducting maximal exercise testing in this population.
HRQOL outcomes showed mixed results after the 4-week intervention period. The vitality domain showed a statistically significant change (p = 0.040), with the median slightly decreasing; however, the distribution shifted toward higher values. No significant changes were observed in other QOL-B domains. The limited improvement contrasts with longer pulmonary rehabilitation studies in bronchiectasis that demonstrated more substantial reductions in fatigue after 8 weeks of intervention41. This likely reflects the brief intervention period, as previous studies showed that 8-week supervised programs achieved clinically meaningful HRQOL improvements immediately after the intervention, although these benefits were not sustained at 6 months41. Given the established MCID of 8 − 10 points for QOL-B domains33, longer intervention periods may be necessary to achieve clinically meaningful and sustained QoL improvements across all domains.
The enrollment rate was 85.2% (23/27) among patients who received detailed study information, and the dropout rate of 17.4% (4/23) reflects common challenges in exercise programs for chronic respiratory diseases. All discontinuations were due to medical events or withdrawal of consent unrelated to the exercise intervention—one withdrawal due to thoracic vertebral fracture, one due to side effects of medications for osteoporosis, and two consent withdrawals. These events highlight the need for risk stratification and flexible adaptation42,43. No serious adverse events occurred during the program, confirming the safety of the intervention. Based on our results, with retention and supervised adherence exceeding the thresholds and home-based adherence meeting the minimum threshold, we recommend proceeding with modifications to strengthen home-based exercise adherence strategies.
This study had several limitations. The 4-week duration was shorter than that of standard pulmonary rehabilitation (8–12 weeks)24,44,45, the sample size was small (n = 19 completers), this was a single-center study, and no control group was included. As a feasibility study, it was not sufficiently powered to detect clinical effects; therefore, the estimates should be interpreted as preliminary. The challenges in obtaining valid VO₂max measurements (only 10/18 had valid data) suggest that submaximal exercise tests may be more appropriate as primary outcomes in future trials. The outcomes were limited to short-term functional measures. Therefore, the duration may have been insufficient to capture meaningful changes in QOL.
Future research should include powered, multicenter, randomized trials of longer duration (8 − 12 weeks) with blinded outcome assessment and subgroup analyses (e.g., cavitary disease, baseline deconditioning, and comorbidity burden). Trials should include serial QOL-B assessments to identify the optimal intervention duration and should test enhanced adherence support (e.g., automated reminders, app-based diaries) to improve home exercise adherence beyond the 73.5% weekly target achievement observed. Future programs should also incorporate NTM-PD-specific education addressing disease management, symptom monitoring (hemoptysis, sputum production), airway clearance techniques, medication adherence, and infection control practices, integrated with the exercise intervention. Programs tailored to NTM-PD and integrated with medical management are needed, given its rising global prevalence and limited non-pharmacological options1,5,46.
Conclusions
This feasibility study demonstrates that a 4-week hybrid exercise program is feasible, safe, and acceptable for patients with NTM-PD. All primary feasibility thresholds for retention, supervised-session adherence, and home-based adherence were achieved, with no serious adverse events. Exploratory outcomes showed modest functional improvements, while challenges in obtaining valid maximal exercise testing data suggest that submaximal assessments may be more appropriate for this population. These findings support the progression to a longer-duration randomized controlled trial with enhanced home-based exercise adherence strategies, alternative outcome measures, and evaluation of clinical effectiveness and sustainability of benefits.
Data availability
All data used or analyzed in this study are available from the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- HRQOL:
-
Health-related quality of life
- NTM-PD:
-
Nontuberculous mycobacterial pulmonary disease
- QOL-B:
-
Quality of life-bronchiectasis
- SPPB:
-
Short physical performance battery
- VO2max :
-
Maximal oxygen uptake
- 6MWD:
-
6-minute walk distance
- 30-s STS:
-
30-second sit-to-stand test
References
Lee, H., Myung, W., Koh, W. J., Moon, S. M. & Jhun, B. W. Epidemiology of nontuberculous mycobacterial Infection, South Korea, 2007–2016. Emerg. Infect. Dis. 25 (3), 569–572 (2019).
Dahl, V. N. et al. Global trends of pulmonary infections with nontuberculous mycobacteria: a systematic review. Int. J. Infect. Dis. 125, 120–131 (2022).
Park, S. C. et al. Prevalence, incidence, and mortality of nontuberculous mycobacterial infection in korea: a nationwide population-based study. BMC Pulm Med. 19 (1), 140 (2019).
Kim, J. Y., Kwak, N. & Yim, J. J. The rise in prevalence and related costs of nontuberculous mycobacterial diseases in South Korea, 2010–2021. Open. Forum Infect. Dis. 9 (12), ofac649 (2022).
Daley, C. L. et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Eur. Respir J. 56 (1). (2020).
Pasipanodya, J. G., Ogbonna, D., Deshpande, D., Srivastava, S. & Gumbo, T. Meta-analyses and the evidence base for microbial outcomes in the treatment of pulmonary Mycobacterium avium-intracellulare complex disease. J. Antimicrob. Chemother. 72 (suppl_2), i3–i19 (2017).
Ono, K. et al. Decreased incremental shuttle walk test distance characterized by fibrocavitary lesions in non-tuberculous mycobacterial pulmonary disease. Expert Rev. Respir Med. 16 (4), 469–475 (2022).
Chung, E., Park, Y., Park, D. H., Jeon, J. Y. & Kang, Y. A. Association of physical inactivity and handgrip strength with non-tuberculous mycobacterial pulmonary disease. Int. J. Tuberc Lung Dis. 28 (8), 367–373 (2024).
Omatsu, S. et al. Clinical significance and safety of combined treatment with chemotherapy and pulmonary rehabilitation regarding health-related quality of life and physical function in nontuberculous mycobacterial pulmonary disease. Respir Investig. 60 (5), 674–683 (2022).
Asakura, T. et al. Quantitative assessment of erector spinae muscles in patients with Mycobacterium avium complex lung disease. Respir Med. 145, 66–72 (2018).
Lee, S. W. et al. Healthcare use and medical cost before and after diagnosis of nontuberculous mycobacterial infection in korea: the National health insurance Service-National sample cohort study. Ther. Adv. Respir Dis. 17, 17534666221148660 (2023).
Park, Y., Hong, J. W., Ahn, E., Gee, H. Y. & Kang, Y. A. PARK2 as a susceptibility factor for nontuberculous mycobacterial pulmonary disease. Respir Res. 25 (1), 310 (2024).
Lee, A. L. et al. The short and long term effects of exercise training in non-cystic fibrosis bronchiectasis–a randomised controlled trial. Respir Res. 15 (1), 44 (2014).
Mandal, P. et al. A pilot study of pulmonary rehabilitation and chest physiotherapy versus chest physiotherapy alone in bronchiectasis. Respir Med. 106 (12), 1647–1654 (2012).
McCarthy, B. et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015 (2), Cd003793 (2015).
Basavaraj, A. et al. Effects of chest physical therapy in patients with non-tuberculous mycobacteria. Int. J. Respir Pulm Med. 4 (1). (2017).
Deng, N. et al. A home-based pulmonary rehabilitation mHealth system to enhance the exercise capacity of patients with COPD: development and evaluation. BMC Med. Inf. Decis. Mak. 21 (1), 325 (2021).
José, A. et al. Home-based pulmonary rehabilitation in people with bronchiectasis: a randomised controlled trial. ERJ Open. Res. 7 (2). (2021).
Eldridge, S. M. et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Bmj 355, i5239 (2016).
Daley, C. L. et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Eur. Respir. J. 56 (1), 2000535 (2020).
Armstrong, T. & Bull, F. Development of the world health organization global physical activity questionnaire (GPAQ). J. Public Health. 14 (2), 66–70 (2006).
Lee, J. et al. Development of the Korean global physical activity questionnaire: reliability and validity study. Glob Health Promot. 27 (3), 44–55 (2020).
Lee, M. K. et al. Development and application of a home-based exercise program for patients with cardiovascular disease: a feasibility study. BMC Sports Sci. Med. Rehabil. 16 (1), 51 (2024).
Lee, M. K. et al. Effect of home-based exercise intervention on fasting insulin and adipocytokines in colorectal cancer survivors: a randomized controlled trial. Metabolism 76, 23–31 (2017).
Lee, M. K., Kim, N. K. & Jeon, J. Y. Effect of the 6-week home-based exercise program on physical activity level and physical fitness in colorectal cancer survivors: A randomized controlled pilot study. PLOS ONE. 13 (4), e0196220 (2018).
Bruce, R. A., Blackmon, J. R., Jones, J. W. & Strait, G. Exercising testing in adult normal subjects and cardiac patients. Pediatrics 32, 742 – 56 (1963).
Howley, E. T., Bassett, D. R. Jr. & Welch, H. G. Criteria for maximal oxygen uptake: review and commentary. Med. Sci. Sports Exerc. 27 (9), 1292–1301 (1995).
Rikli, R. E. & Jones, C. J. The reliability and validity of a 6-Minute walk test as a measure of physical endurance in older adults. J. Aging Phys. Act. 6 (4), 363–375 (1998).
Nathan, S. D. et al. Validation of test performance characteristics and minimal clinically important difference of the 6-minute walk test in patients with idiopathic pulmonary fibrosis. Respir Med. 109 (7), 914–922 (2015).
Jones, C. J., Rikli, R. E. & Beam, W. C. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res. Q. Exerc. Sport. 70 (2), 113–119 (1999).
Guralnik, J. M. et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 49 (2), M85–94 (1994).
Watanabe, T. et al. The short-term reliability of grip strength measurement and the effects of posture and grip span. J. Hand Surg. Am. 30 (3), 603–609 (2005).
Quittner, A. L. et al. Quality of life Questionnaire-Bronchiectasis: final psychometric analyses and determination of minimal important difference scores. Thorax 70 (1), 12–20 (2015).
Bull, F. C. et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54 (24), 1451–1462 (2020).
Kawahara, K., Tabusadani, M., Ohta, K. & Morimoto, K. Assessment of health-related quality of life in patients with nontuberculous mycobacterial pulmonary disease: A comprehensive review. Respir Investig. 62 (6), 1006–1014 (2024).
Lan, C-C., Lai, S-R. & Chien, J-Y. Nonpharmacological treatment for patients with nontuberculous mycobacterial lung disease. J. Formos. Med. Assoc. 119, S42–S50 (2020).
Bohannon, R. W. & Crouch, R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. J. Eval Clin. Pract. 23 (2), 377–381 (2017).
Schrover, R., Evans, K., Giugliani, R., Noble, I. & Bhattacharya, K. Minimal clinically important difference for the 6-min walk test: literature review and application to Morquio A syndrome. Orphanet J. Rare Dis. 12 (1), 78 (2017).
Chung, E., Park, Y., Lee, H. J. & Kang, Y. A. Usefulness of the mini nutritional assessment short-form for evaluating nutritional status in patients with nontuberculous mycobacterial pulmonary disease: a prospective cross-sectional study. BMC Infect. Dis. 24 (1), 604 (2024).
Frei, A. et al. Effectiveness of a Long-term Home-Based exercise training program in patients with COPD after pulmonary rehabilitation: A multicenter randomized controlled trial. Chest 162 (6), 1277–1286 (2022).
Lee, A. L., Gordon, C. S. & Osadnik, C. R. Exercise training for bronchiectasis. Cochrane Database Syst. Rev. 4 (4), Cd013110 (2021).
Keating, A., Lee, A. & Holland, A. E. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron. Respir Dis. 8 (2), 89–99 (2011).
Rochester, C. L. et al. Pulmonary rehabilitation for adults with chronic respiratory disease: an official American thoracic society clinical practice guideline. Am. J. Respir Crit. Care Med. 208 (4), e7–e26 (2023).
An, K. Y. In Yang H, Kang DW, Courneya KS, Jeon JY. Development process of an evidence-based exercise program for post-operative colorectal cancer patients. Support Care Cancer. 28 (2):755 – 65. (2020).
Lee, D. H. et al. Effects of a 12-week home-based exercise program on the level of physical activity, insulin, and cytokines in colorectal cancer survivors: a pilot study. Support Care Cancer. 21 (9), 2537–2545 (2013).
Chang, S. et al. Medical costs of nontuberculous mycobacterial pulmonary disease, South Korea, 2015–2019. Emerg. Infect. Dis. 30 (9), 1841–1849 (2024).
Acknowledgements
We thank all the participants in this study.
Funding
This research was supported by a grant from the Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health & Welfare, Republic of Korea (RS-2021-KH119793) and by a National Research Foundation of Korea(NRF) grant funded by the Korean Ministry of Science and ICT (MSIT) (RS-2024-00341299) and by a faculty research grant of Yonsei University College of Medicine for (6-2023-0102).
Author information
Authors and Affiliations
Contributions
Conceptualization: Kang YA, Park Y, Jeon J. Data curation: Kim EC, Kim C, Park DH, Park Y. Formal analysis: Kim EC, Park Y. Funding acquisition: Kang YA, Park Y. Investigation: Kim EC, Kim C, Park DH, Park Y, Kang YA, Jeon J. Supervision: Jeon J, Kang YA. Writing - original draft: Kim EC, Park Y, Kang YA, Jeon J. Writing—review & editing: Kim EC, Kim C, Park DH, Park Y, Jeon J, Kang YA. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (IRB #4-2023-0549), and was conducted according to the tenets of the Declaration of Helsinki. All the participants provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, E.C., Park, Y., Kim, C. et al. Feasibility of a 4-week combined supervised and home-based exercise program for patients with nontuberculous mycobacterial pulmonary disease: a single-center, single-arm feasibility study. Sci Rep 16, 138 (2026). https://doi.org/10.1038/s41598-025-28839-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-28839-0