Abstract
Nocturnal polyuria is a major cause of nocturia, which affects quality of life. Aging-related decreases in nitric oxide production have been reported to contribute to salt-induced nocturnal polyuria. We posited that enhanced nitric oxide production from exercise could mitigate salt-induced nocturnal polyuria. To validate, we assessed the impact of 4 weeks of moderate-intensity exercise on intrarenal renin-angiotensin system activity and salt-induced polyuria during inactive periods in 80-week-old mice. The moderate-intensity exercise group (Mod-Ex) had increased nitric oxide production and suppressed intrarenal renin-angiotensin system compared to the sedentary group (Sed) (renal angiotensinogen level: Sed vs. Mod-Ex, 1.101 ± 0.077 vs. 0.630 ± 0.048 arbitrary unit, P = 0.002). This exercise also alleviated salt-induced polyuria during inactive periods (diurnal polyuria index: Sed vs. Mod-Ex, 0.292 ± 0.027 vs. 0.193 ± 0.023, P = 0.018). These effects were neutralized by suppression of nitric oxide production by oral administration of Nω-Nitro-L-arginine methyl ester hydrochloride, an nitric oxide synthesis inhibitor. These findings indicate that exercise-induced improvements in salt-induced polyuria during inactive periods are caused by increases in nitric oxide production. In summary, increasing nitric oxide production may serve as a treatment method for salt-induced nocturnal polyuria in older adults.
Similar content being viewed by others
Introduction
Nocturia, defined as waking to pass urine during the main sleep period1, is a common health problem among middle-aged and older adults, affecting approximately 65% of adults over the age of 502. Nocturia is not only a troublesome symptom that affects quality of life3but is also a risk factor for death4. The pathologies of nocturia include decreased bladder capacity, sleep disturbances, nocturnal polyuria, or a combination of the three1. Among these, nocturnal polyuria is the most frequent. Nocturnal polyuria, which is defined as the passage of a large volume of urine during the main sleep period1, accounts for 50–80% of nocturia5. Excessive salt intake has been reported to cause nocturnal polyuria6,7. Although nocturnal urine volume increases with aging8, however, the amount of salt intake does not9. These findings suggest that some factors associated with aging are involved in nocturnal polyuria aside from excessive salt intake. Recently, we reported that decreased nitric oxide (NO) production is associated with salt-induced nocturnal polyuria in humans, and that high-salt diet causes nocturnal polyuria in aged mice with decreased NO production but not in young mice. We also reported that high-salt diet causes nocturnal polyuria in young mice when NO production is suppressed by L-NAME administration10. These results suggest that decreased NO production plays an important role in the pathogenesis of salt-induced nocturnal polyuria. Moreover, in animal experiments, we found that decreased NO production leads to the activation of the intrarenal renin-angiotensin system (RAS) and sodium chloride co-transporter (NCC), which results in decreased salt excretion and urine volume in the active period and increased salt excretion and urine volume in the inactive period10. This mechanism may be responsible for salt-induced nocturnal polyuria in older adult humans because decreased NO production is an age-related physiological change11. Therefore, increasing NO production may be a novel therapeutic strategy for salt-induced nocturnal polyuria in older adults.
Exercise training has remarkable positive effects on the body and benefits various diseases, such as cardiovascular disease, chronic kidney disease, mental health disorder, cancer, and dementia12. One of the positive effects of exercise is to improve endothelial function and increase the release of NO from the endothelium. Increased NO production with exercise decreases vascular resistance, lowers blood pressure in hypertension patients13, and improves renal function in patients with chronic kidney disease patients14. We posited that enhanced NO production from exercise could mitigate salt-induced nocturnal polyuria. To validate, we assessed the impact of exercise on intrarenal RAS activity and salt-induced polyuria during inactive periods in aged mice, finding that four weeks of moderate exercise curbed both by elevating NO levels. These findings indicate that increasing NO production may serve as a novel treatment for elderly patients with this condition.
Results
Exercise-induced changes in 24-hour urinary NOx amount
First, we evaluated the effect of exercise on NO production. We used 80-week-old C57/BL6 male mice. Mice were fed 1% high-salt diets (1% HSD) for 2 weeks and were randomized into sedentary (Sed), low-intensity exercise (Low-Ex), and moderate-intensity exercise (Mod-Ex) groups. After 4 weeks, the 24-hour urinary NOx levels were evaluated. The 24-hour urinary NOx amount of the Mod-Ex group was significantly higher than those of the Sed and Low-Ex group (Sed vs. Low-Ex vs. Med-Ex: 0.042 ± 0.005 vs. 0.018 ± 0.001 vs. 0.104 ± 0.015 µmol/Crmg, P = 0.017 and 0.006, respectively) (Fig. 1). There was no significant difference in the 24-hour urinary NOx levels between the Sed and Low-Ex groups (P = 0.122).
Increasing NO production-induced changes in intrarenal RAS and NCC activity in the active period
Next, we investigated exercise-induced changes in the intrarenal RAS activity in the active period. We performed a quantitative analysis of renal angiotensinogen (AGT) in the Sed and Mod-Ex groups. AGT/β-actin (ACTB) level in the Mod-Ex group was significantly lower than that of the Sed group (1.101 ± 0.077 vs. 0.630 ± 0.048 arbitrary unit, P = 0.002) (Fig. 2a). This indicates that moderate-intensity exercise decreases the intrarenal RAS activity in the active period. The intrarenal RAS regulates NCC activity in the distal tubule15. Thus, we quantitatively analyzed the phosphorylated NCC (pNCC) in the Sed and Mod-Ex groups to investigate exercise-induced changes in NCC activity. The pNCC/NCC level in the Mod-Ex group was significantly lower than that of the Sed group (0.812 ± 0.045 vs. 0.538 ± 0.030 arbitrary unit, P = 0.003) (Fig. 2b). This indicates that moderate-intensity exercise decreases NCC activity.
Increasing NO production-induced changes in intrarenal RAS and NCC activity in the active period. (a) AGT/ACTB levels were compared between Sed and Mod-Ex groups. Representative immunoblotting (above) and quantitative analysis (below) of renal AGT in the active period. Two-tailed Student’s t-test was performed (n = 6, each group), **P < 0.01. Error bars represent s.e.m. (b) pNCC/NCC levels were compared between Sed and Mod-Ex groups. Representative immunoblotting (above and middle) and quantitative analysis (below) of renal phosphorylated NCC (pT53), NCC, and ACTB in the active period. Two-tailed Student’s t-test was performed (n = 6, each group), **P < 0.01. Error bars represent s.e.m.
Increasing NO production-induced changes in sodium excretion kinetics and diurnal polyuria index
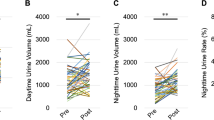
NCC activity in the distal tubule is known to control sodium reabsorption15,16; thus, we evaluated sodium excretion in the inactive and active periods of the Sed and Mod-Ex groups to investigate exercise-induced changes in sodium excretion kinetics. The urine collection test revealed that there was no significant difference in 24-hour sodium excretion between the two groups (0.219 ± 0.016 vs. 0.204 ± 0.010 mEq, P = 0.461). In contrast, the sodium excretion during the active period of the Mod-Ex group was significantly higher than that of the Sed group (0.114 ± 0.017 vs. 0.179 ± 0.012 mEq, P = 0.022). The sodium excretion during inactive periods of the Mod-Ex group was significantly lower than that of the Sed group (0.106 ± 0.021 vs. 0.024 ± 0.003 mEq, P = 0.006) (Fig. 3a–c). This indicates that moderate-intensity exercise shifts urinary sodium excretion from the inactive to the active period. Next, we evaluated the effect of exercise on the diurnal polyuria index (DPi), the ratio of the diurnal to daily urine volume. Because mice are nocturnal, the DPi in mice is an index corresponding to the nocturnal polyuria index in humans. We analyzed urine volume every 4-hour for 3.5 consecutive days before and after exercise (Fig. 3d and e). In the Mod-Ex group, exercise significantly decreased the DPi (from 0.292 ± 0.027 to 0.193 ± 0.023, P = 0.018), while in the Sed, there were no significant changes in the DPi (Sed: from 0.257 ± 0.008 to 0.306 ± 0.025, P = 0.236) (Fig. 3f). Notably, the extent of the decrease in DPi was significantly greater in the Mod-Ex group than in the Sed group (P = 0.003) (Fig. 3f). These findings suggest that moderate exercise-induced increase in NO production improves salt-induced polyuria during inactive periods in aged mice.
Increasing NO production-induced changes in urinary sodium excretion kinetics and diurnal polyuria index. 24-hour sodium excretion (a), sodium excretion during the active (b), and sodium excretion during inactive periods (c) were compared between the Sed and Mod-Ex groups. A two-tailed Student’s t-test was performed (n = 6 per group); *P < 0.05, **P < 0.01. Error bars represent s.e.m., n.s.: Not significant. The 4-hour urinary volume for 3.5 consecutive days in the Sed (d) and Mod-Ex (e) groups at week 2 (baseline) and week 6 was measured using the automated voiding staining on the paper method (aVSOP). Changes in the DPi were compared between Sed and Ex groups (f). Data were obtained from the same mice. Two-way repeated-measures analysis of variance (ANOVA) was performed (n = 6 per group); *P < 0.05 (time-by-group interaction). Error bars represent s.e.m.
The effect of NO suppression on exercise-induced changes in 24-hour urinary NOx amount, intrarenal RAS activity, and DPi
Moreover, we assessed NO suppression’s impact on exercise-induced alterations in 24-hour urinary NOx, intrarenal RAS activity, and DPi using Nω-Nitro-L-arginine methyl ester hydrochloride (L-NAME), an NO synthase inhibitor. We assigned eighty-week-old C57/BL6 male mice to three groups: Mod-Ex, Mod-Ex with L-NAME, and Sed with L-NAME. The 24-hour urinary NOx levels in the Mod-Ex with L-NAME and Sed with L-NAME groups were markedly lower than in the Mod-Ex group (0.131 ± 0.022 vs. 0.041 ± 0.018 vs. 0.015 ± 0.003 µmol/Crmg, P = 0.020 and 0.005, respectively) (Fig. 4a). Subsequently, we investigated the NO suppression’s effects on intrarenal RAS activity by quantifying renal AGT in the same groups. AGT/ACTB levels in the Mod-Ex with L-NAME and Sed with L-NAME groups significantly exceeded those in the Mod-Ex group (0.752 ± 0.026 vs. 0.979 ± 0.026 vs. 0.995 ± 0.027 µmol/Crmg, P = 0.001 and 0.001, respectively) (Fig. 4b).
The effect of NO suppression on exercise-induced changes in 24-hour urinary NOx amount, intrarenal RAS activity, and DPi. (a) 24-hour urinary NOx amounts were compared among Sed with L-NAME, Mod-Ex with L-NAME, and Mod-Ex group. Tukey’s honestly significant difference test was performed (n = 5, each group). *P < 0.05, **P < 0.01. Error bars represent s.e.m. (b) AGT/ACTB levels were compared among Sed with L-NAME, Mod-Ex with L-NAME, and Mod-Ex groups. Representative immunoblotting (above) and quantitative analysis (below) of renal AGT in the active period. Tukey’s honestly significant difference test was performed (n = 4, each group), *P < 0.05. Error bars represent s.e.m. The 4-hour urinary volume for 3.5 consecutive days in Sed with L-NAME (c), Mod-Ex with L-NAME (d), and Mod-Ex (e) groups at week 2 (baseline) and week 6 was measured using aVSOP. Changes in the DPi were compared between Sed with L-NAME, Mod-Ex with L-NAME, and Mod-Ex Groups (f). Data were obtained from the same mice. Two-way repeated-measures analysis of variance (ANOVA) was performed (n = 6, each group) *P < 0.05, **P < 0.01 (Time-by-group interaction). Error bars represent s.e.m.
Finally, we analyzed the every 4-hour urine volume for 3.5 consecutive days before and after exercise (Fig. 4c–e). The exercise-induced decrease in the DPi in the Mod-Ex group was abolished in the Mod-Ex with L-NAME group (P = 0.015) (Fig. 4f). There was no significant difference in the DPi between the Mod-Ex with L-NAME and the Sed with L-NAME group (Mod-Ex with L-NAME: from 0.252 ± 0.015 to 0.286 ± 0.014, P = 0.212; Sed with L-NAME: from 0.268 ± 0.010 to 0.305 ± 0.023, P = 0.181) (Fig. 4f). These results indicated that exercise-induced changes in salt-induced polyuria during inactive periods in aged mice were mediated by increased NO production and decreased intrarenal RAS activity.
Discussion
In this study, we provide experimental evidence that an increase in NO production by 4 weeks of moderate-intensity exercise can suppress intrarenal RAS and NCC activity, increase sodium excretion during active periods, decrease sodium excretion during inactive periods, and improve salt-induced polyuria during inactive periods in aged mice. Given that mice are nocturnal, polyuria during inactive periods is considered to correspond to nocturnal polyuria in humans. These findings suggest that increased NO production is a potential new treatment for salt-induced nocturnal polyuria in elderly individuals.
Excessive salt intake has been reported to cause nocturnal polyuria6,7. However, nocturnal urine volume increases with aging8, although the amount of salt intake does not increase with aging9. These findings suggest that age-related factors are involved in the association between salt intake and nocturnal polyuria. We previously reported that patients with decreased NO production exhibit salt-induced nocturnal polyuria10. We also found that decreased NO production leads to activation of the intrarenal RAS, which results in decreased salt excretion and urine volume in the active period and increased salt excretion and urine volume in the inactive period10. These findings indicated that decreased NO production is involved in the development of salt-induced nocturnal polyuria and could be a novel therapeutic target for salt-induced nocturnal polyuria. In this study, we hypothesized that exercise-induced increase in NO production would improve salt-induced nocturnal polyuria. To test this hypothesis, we evaluated the effects of exercise on NO production, intrarenal RAS activity, and salt-induced polyuria during inactive periods in aged mice. We found that 4 weeks of moderate-intensity exercise increased systemic NO production, suppressed intrarenal RAS and NCC activity, and improved salt-induced polyuria during inactive periods in aged mice. We also found that the effect of exercise on salt-induced polyuria during inactive periods in aged mice was inhibited by NO suppression. These findings indicate that exercise-induced improvement in salt-induced polyuria during inactive periods is mainly mediated by increased NO production. Therefore, increasing NO production could be a new treatment strategy for salt-induced nocturnal polyuria in older individuals.
Exercise has been reported to be effective in treating nocturnal polyuria17, but the mechanism by which exercise improves nocturnal polyuria is not well understood. Exercise has been speculated to improve nocturnal polyuria by pumping water from the interstitial space to the blood vessels and expelling it as sweat18or urine19. However, this mechanism has not been scientifically proven. In this study, we found that moderate-intensity exercise suppressed intrarenal RAS activity and improved salt-induced polyuria during inactive periods by increasing NO production in aged mice. Moderate-intensity exercise may improve salt-induced nocturnal polyuria through a similar mechanism in older adult humans because they have decreased NO production11. Exercise is distinguished by its intensity as low-, moderate-, or high-intensity. Low-intensity exercise includes walking and stretching, moderate-intensity exercise includes yoga and golfing, and high-intensity exercise includes marathon running and football20. It has been reported that NO production increases with exercise intensity21. First, we investigated the effects of high-intensity exercise on NO production in aged mice and found that the high-intensity exercise was too demanding for aged mice to complete the protocol. Therefore, we assessed the effects of low- and moderate-intensity exercises. Low-intensity exercise did not increase NO production, whereas moderate-intensity exercise increased NO production and improved salt-induced polyuria during inactive periods in aged mice. This finding suggests that moderate-intensity exercise is necessary to increase NO production and improve salt-induced nocturnal polyuria in older individuals. The urinary NOx excretion in the Low-Ex group tended to be lower than that in the Sed group, although the difference was not statistically significant. We believe this result may be because four weeks of low-intensity exercise does not increase NO production and the amount of NO production in old mice is highly variable. Several studies have reported that moderate-intensity exercise increases NO production, whereas low-intensity exercise does not22,23. These reports suggest that the reasons for the lack of increased NO production with low-intensity exercise may be because exercise-induced stimulus to vascular endothelium is too weak to elicit an increase in NO production during low-intensity exercise.
Exercise is known to improve hypertension. In this study, 4 weeks of moderate-intensity exercise lowered systolic and diastolic blood pressure during both the inactive and active periods (Supplementary Fig. 1a–d). Because non-dipping hypertension is associated with nocturnal polyuria24, the improvement in salt-induced polyuria during inactive periods by exercise may be related, in part, to the improvement in hypertension during inactive periods. However, lowering blood pressure with the antihypertensive drug hydralazine hydrochloride did not improve DPi (Supplementary Fig. 2a–e), indicating that exercise-induced improvement in polyuria during inactive periods was not due to an improvement in hypertension.
The intrarenal RAS is the pathway by which angiotensinogen produced in the kidney is converted to biologically active angiotensin II by renin and angiotensin-converting enzymes. The intrarenal RAS is distinct from the systemic RAS and plays a significant role in the pathogenesis of hypertension and renal disease25. The intrarenal RAS regulates the NCC activity in the distal tubule, which controls sodium reabsorption16. Previously, we reported that the suppression of NO production activates intrarenal RAS and NCC activity and increases sodium reabsorption during active periods, which leads to salt-induced polyuria during inactive periods in mice. In this study, we found that increased systemic NO production suppressed intrarenal RAS and NCC activity, decreased sodium reabsorption in active periods, and ameliorated salt-induced polyuria during inactive periods in aged mice. NO plays a crucial role in regulating physiological functions, such as vasodilation, neurotransmission, and immune response26. In the kidney, NO increases renal blood flow and glomerular filtration rate and promotes sodium excretion27. Moreover, NO suppresses intrarenal RAS activity13; however, the mechanism by which increased NO production suppresses intrarenal RAS is unclear. Therefore, it is possible that the increase in NO production associated with moderate-intensity exercise increased renal blood flow and promoted sodium excretion, thereby improving nocturnal polyuria. However, the mechanism by which increased NO production decreases intrarenal RAS activity was not elucidated in this study, and further research is required. Previously, we have reported that decreased renal function decreases daytime sodium excretion and increases nocturnal sodium excretion, resulting in increased nocturnal urine output28. We believe that sodium excretion kinetics have a crucial influence on salt-induced nocturnal polyuria. It is known that there are racial differences in sodium excretion kinetics29, and genetic factors related to sodium excretion kinetics may be involved in salt-induced nocturnal polyuria. It is also possible that NO production affects vasopressin secretion which, in turn, affects urine output. The association between NO production and vasopressin secretion has been reported in several studies. Ota et al. reported an increase in blood vasopressin concentration after intracerebroventricular administration of NO donors30. However, in the kidney, NO has been reported to reduce vasopressin responsiveness. Garcia et al. reported that increased NO in the cortical collecting ducts of the kidney inhibits vasopressin-stimulated water reabsorption31. Consequently, the impact of NO-induced changes in vasopressin on urine output remains poorly understood. While increased NO production is believed to enhance vasopressin secretion in the brain, it simultaneously appears to reduce vasopressin responsiveness in the kidneys, creating a complex and unresolved dynamic. However, the possibility that vasopressin is involved in the improvement of salt-induced nocturnal polyuria caused by increased NO production is undeniable.
This study had a limitation. We showed that moderate-intensity exercise is effective in the treatment of salt-induced polyuria during inactive periods in aged mice. Moderate-intensity exercise such as yoga or golfing is also thought to be necessary to improve nocturnal polyuria in humans; however, it may be challenging for some older individuals. Therefore, exercise may not be appropriate for all older adults with salt-induced nocturnal polyuria.
In summary, moderate-intensity exercise improved salt-induced polyuria during inactive periods in aged mice by increasing NO production. This suggests that increasing NO production may be a potential treatment for salt-induced nocturnal polyuria in some elderly individuals who have decreased NO production. Further studies are required to determine its efficacy in humans.
Methods
Experimental animals
All experiments involving animals were conducted in accordance with the Guidelines for the Care and Use of Laboratory Animals of Osaka University and approved by the Animal Care and Use Committee of Osaka University (No. J008231-002). All animal experiments in this study were done in accordance with ARRIVE guidelines. The study complied with all ethical regulations. Eighty-week-old C57BL/6J mice (aged mice were purchased from Charles River Laboratories [Tokyo, Japan]) were kept in a temperature-controlled room with a 12/12-hour light/dark cycle. The active period was from 8:00 p.m. to 8:00 a.m. and the inactive period was from 8:00 a.m. to 8:00 p.m. (both 12 h) and had ad libitum access to food and water.
Experimental protocol
We have adjusted the sodium content of the standard purified product for mouse and rat research published by the National Institute of Nutrition in 1993 to crease a 1% salt-containing diet. The mice were administered a 1% high sodium diet (HSD) for 2 weeks. All the diets were purchased from Oriental Yeast (Tokyo, Japan). We previously reported that a 1% HSD for mice aged 2 weeks increased urine volume during inactive periods without producing differences in daily urine output compared to a normal salt diet10. The mice were divided into the low-intensity exercise (Low-Ex), moderate-intensity exercise (Mod-Ex), moderate-intensity with Nω-Nitro-L-arginine methyl ester hydrochloride (L-NAME) (Mod-Ex with L-NAME), sedentary (Sed), and sedentary with L-NAME (Sed with L-NAME) groups. Mice in the Low-Ex, Mod-Ex, and Mod-Ex with L-NAME groups underwent forced treadmill exercise, while those in the Sed and Sed with L-NAME groups remained in their cages and listened to the sounds of treadmill running. Mice in the Mod-Ex with L-NAME and Sed with L-NAME groups were administered L-NAME (Sigma-Aldrich, St. Louis, MO, USA, 0.5 g per L in drinking water) for four weeks. After four weeks, urinary behavior was assessed using the automated Voided Stain on Paper (aVSOP) method, and urine samples were collected using metabolic cages. The mice were sacrificed by isoflurane inhalation during the active period, and their kidneys and blood were collected.
Exercise protocol
We conducted adaptive exercises prior to moderate- and low-intensity exercises. Mice were acclimated to the treadmill at 10 m/min and 0° incline for 15 min daily for 1 week. Mice in the Low-Ex, Mod-Ex, and Mod-Ex with L-NAME groups underwent forced treadmill exercises on TMS-6B units (MELQUEST, Toyama, Japan) in individual lanes. The Low-Ex group exercised for four weeks at 10 m/min, 60 min/day, 0° incline, and four days/week. The Mod-Ex group exercised similarly but at a progressive speed: starting at 10 m/min for 5 min, increasing to 12 m/min for 15 min, and reaching 14 m/min for 40 min, with an incline of 15°32,33. Mice in the Mod-Ex with L-NAME group were administered L-NAME and subjected to forced treadmill exercise at the same intensity as mice in the Mod-Ex group. All the mice performed the exercise without an electric stimulant.
Urine volume and time measurements
The urine volume was measured using the aVSOP method34,35. Briefly, a roll of laminated filter paper pretreated to turn the urine dark purple was rolled under a water-repellent wire grid at a speed of 10 cm/h. The mice were housed for four days in cages with dimensions of 110 mm × 160 mm × 75 mm (H × D × W). Urine samples were counted, tracked, and converted to volume using ImageJ software (ver. 1.53e, National Institutes of Health, Bethesda, MD, USA). The diurnal polyuria index (DPi) was calculated by dividing the volume of urine produced during inactive periods (8 a.m. to 8 p.m.) by the volume of urine produced per day. We measured urine volume every 4 h for 3.5 consecutive days to calculate DPi. In all experiments, changes in DPi were measured in the same mice to evaluate changes in DPi before and after the intervention.
Blood pressure measurement
Blood pressure was measured using the tail-cuff method (BP-98 A; Softron Corporation, Tokyo, Japan). All mice were first acclimated to the blood pressure measurements for 3 days. Three consecutive measurements were performed, and the average value was recorded.
Mouse urine analysis
Mice were placed individually in metabolic cages (3600M021; Techniplast, Tokyo, Japan), with unrestricted access to food and water for urine collection. Due to reduced urine volume during inactive period, diurnal urine and urinary electrolyte concentrations were calculated using the following formulae: (inactive period urine volume) = (24 − hour urine volume) − (active period urine volume); (inactive period urinary electrolyte concentration) = {(24 − hour urinary electrolyte amount) − (active period urinary electrolyte amount)} ÷ (inactive period urine volume). Urine electrolytes were assessed via Fujifilm Pet Systems Co. Furthermore, urinary NOx (NO2/NO3) levels were quantified using the NK05 NO2/NO3 Assay Kit-C II (Colorimetric, Japan), involving protein separation with a column, centrifugation at 7000 ×g for 20 min, and a subsequent centrifugation at 17,000 ×g for 10 min.
Immunoblotting
Proteins extracted from whole kidneys were homogenized in lysis buffer; the lysate and membrane fractions were then collected and prepared in sodium dodecyl sulfate sample buffer (Cosmo Bio Co., Ltd., Tokyo, Japan). Protein concentrations were determined using the Lowry method, and samples were stored at − 80 °C until immunoblotting. A total of 20 µg of protein underwent 8% non-SDS–PAGE or 10% SDS–PAGE, followed by immunoblotting. Membranes were blocked with Blocking One (Nacalai Tesque, Kyoto, Japan) and incubated overnight at 4 °C in Tris-buffered saline with primary antibodies. Detection used anti-rabbit IgG, horseradish peroxidase-conjugated antibody (Cell Signaling Technology, Danvers, MA, USA), and Chemi-Lumi One (Nacalai Tesque, Kyoto, Japan). A ChemiDoc XRS Plus system (Bio-Rad, Hercules, CA, USA) captured blot images, which were quantified using ImageJ software (National Institutes of Health, Bethesda, MD, USA). The primary antibodies were rabbit anti-NCC, anti-phosphorylated NCC (threonine 53), and anti-angiotensinogen, all at 1:1000; the secondary was anti-rabbit IgG HRP at 1:5000.
Statistical analysis
For the analysis of DPi, 24-hour urinary NOx, renal AGT and NCC activity, and sodium excretion kinetics, groups were compared by Student’s t-test, paired t-test, two-way repeated measures ANOVA, and Tukey’s test when applicable. Bonferroni correction was used for multiple comparison tests. All data are presented as means ± standard errors of the means, and values of P < 0.05 were considered statistically significant. All analyses were performed using the JMP version 17.1.0 software (SAS Institute, Cary, NC, USA).
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Hashim, H. et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol. Urodyn. 38, 499–508 (2019).
Mitsui, T. et al. Prevalence and impact on daily life of lower urinary tract symptoms in Japan: results of the 2023 Japan Community Health Survey (JaCS 2023). Int. J. Urol. 31, 747–754 (2024).
Andersson, F. et al. Assessing the impact of nocturia on health-related quality-of-life and utility: results of an observational survey in adults. J. Med. Econ. 19, 1200–1206 (2016).
Funada, S. et al. Impact of Nocturia on Mortality: the Nagahama Study. J. Urol. 204, 996–1002 (2020).
Van Doorn, B., Blanker, M. H., Kok, E. T., Westers, P. & Bosch, J. L. Prevalence, incidence, and resolution of nocturnal polyuria in a longitudinal community-based study in older men: the Krimpen study. Eur. Urol. 63, 542–547 (2013).
Matsuo, T., Miyata, Y. & Sakai, H. Daily salt intake is an independent risk factor for pollakiuria and nocturia. Int. J. Urol. 24, 384–389 (2017).
Matsuo, T., Miyata, Y. & Sakai, H. Effect of salt intake reduction on nocturia in patients with excessive salt intake. Neurourol. Urodyn. 38, 927–933 (2019).
Blanker, M. H. et al. Relation between nocturnal voiding frequency and nocturnal urine production in older men:a population-based study. Urology 60, 612–616 (2002).
Otsuka, R., Kato, Y., Imai, T., Ando, F. & Shimokata, H. Decreased salt intake in Japanese men aged 40 to 70 years and women aged 70 to 79 years: an 8-year longitudinal study. J. Am. Diet. Assoc. 111, 844–850 (2011).
Sekii, Y. et al. Dietary salt with nitric oxide deficiency induces nocturnal polyuria in mice via hyperactivation of intrarenal angiotensin II-SPAK-NCC pathway. Commun. Biol. 5, 175 (2022).
Torregrossa, A. C., Aranke, M. & Bryan, N. S. Nitric oxide and geriatrics: implications in diagnostics and treatment of the elderly. J. Geriatr. Cardiol. 8, 230–242 (2011).
Blair, S. N. et al. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 262, 2395–2341 (1989).
Carlström, M. Nitric oxide signalling in kidney regulation and cardiometabolic health. Nat. Rev. Nephrol. 17, 575–590 (2021).
Castaneda, C. et al. Resistance training to counteract the catabolism of a low-protein diet in patients with chronic renal insufficiency. A randomized, controlled trial. Ann. Intern. Med. 135, 965–976 (2001).
Nguyen, M. T., Lee, D. H., Delpire, E. & McDonough, A. A. Differential regulation of na + transporters along nephron during ANG II-dependent hypertension: distal stimulation counteracted by proximal inhibition. Am. J. Physiol. Ren. Physiol. 305, F510–F519 (2013).
Coffman, T. M. The inextricable role of the kidney in hypertension. J. Clin. Invest. 124, 2341–2347 (2014).
Cornu, J. N. et al. A contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management—a systematic review and meta-analysis. Eur. Urol. 62, 877–890 (2012).
Kowalik, C. G. et al. Nocturia: evaluation and current management strategies. Rev. Urol. 20, 1–6 (2018).
Torimoto, K. et al. The relationship between nocturnal polyuria and the distribution of body fluid: assessment by bioelectric impedance analysis. J. Urol. 181, 219–224 (2009).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462 (2020).
Goto, C. et al. Acute moderate-intensity exercise induces vasodilation through an increase in nitric oxide bioavailiability in humans. Am. J. Hypertens. 20, 825–830 (2007).
Goto, C. et al. Effect of different intensities of Exercise on Endothelium-Dependent Vasodilation in humans. Circulation 108, 530–535 (2003).
Mota, M. M. et al. Endothelium adjustments to acute resistance exercise are intensity-dependent in healthy animals. Life Sci. 142, 86–91 (2015).
Kato, Y. et al. Association between nocturnal polyuria and 24-h blood pressure fluctuations in males with lower urinary tract symptoms: a multicenter prospective study. Int. J. Urol. 31, 259–264 (2024).
Kobori, H., Nangaku, M., Navar, L. G. & Nishiyama, A. The intrarenal renin-angiotensin system: from physiology to the pathobiology of hypertension and kidney disease. Pharmacol. Rev. 59, 251–287 (2007).
Palmer, R. M., Ferrige, A. G. & Moncada, S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 327, 524–526 (1987).
Hsu, C. N. & Tain, Y. L. Regulation of nitric oxide production in the developmental programming of hypertension and kidney disease. Int. J. Mol. Sci. 20, 681 (2019).
Takezawa, K. et al. Decreased renal function increases the nighttime urine volume rate by carryover of salt excretion to the nighttime. Sci. Rep. 11, 10587 (2021).
Elijovich, F., Kirabo, A. & Laffer, C. L. Salt sensitivity of blood pressure in Black people: the need to Sort out Ancestry Versus Epigenetic Versus Social determinants of its causation. Hypertension 81, 456–467 (2024).
Ota, M., Crofton, J. T., Festavan, G. T. & Share, L. Evidence that nitric oxide can act centrally to stimulate vasopressin release. Neuroendocrinology 57, 955–959 (1993).
Garcia, N. H., Stoos, B. A., Carretero, O. A. & Garvin, J. L. Mechanism of the nitric oxide-induced blockade of collecting duct water permeability. Hypertension 27, 679–683 (1996).
Billat, V. L., Mouisel, E., Roblot, N. & Melki, J. Inter- and intrastrain variation in mouse critical running speed. J. Appl. Physiol. (1985). 98, 1258–1263 (2005).
Lawson, E. C. et al. Aerobic exercise protects retinal function and structure from light-induced retinal degeneration. J. Neurosci. 34, 2406–2412 (2014).
Negoro, H. et al. Involvement of urinary bladder Connexin43 and the circadian clock in coordination of diurnal micturition rhythm. Nat. Commun. 3, 809 (2012).
Takezawa, K. et al. Authentic role of ATP signaling in micturition reflex. Sci. Rep. 6, 19585 (2016).
Acknowledgements
We thank Yoshinori Koishi, Hikari Takeshita, and Koichi Yamamoto for their technical assistance with treadmill exercises and blood pressure measurements. We would also like to thank Editage for their English editing assistance.
Author information
Authors and Affiliations
Contributions
TI and KT contributed to conceptualization. TI, GT, and KT contributed to data curation. TI, KT , and NU contributed to the formal analysis. TI, KT, YK, HK, GT, SK, YS, NU, SF, HK, HN and NN contributed to the methodology. TI, KT, and NN contributed to project administration. KT and NN contributed to supervision. TI contributed to Writing – original draft. TI, KT, and NN contributed to Writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Imanaka, T., Takezawa, K., Kujime, Y. et al. Decreased nitric oxide production is a novel therapeutic target for salt-induced nocturnal polyuria in aging. Sci Rep 15, 3589 (2025). https://doi.org/10.1038/s41598-025-86526-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-86526-6