Abstract
In Africa, the intricate relationship between food security and health outcomes is increasingly challenged by the unpredictable forces of climate change. With this in mind, we utilized panel data spanning from 2010–2022 for 46 African nations, sub-grouped into regional panels to analyze the moderating role of climate change on food security- health outcome nexus, contributing to Sustainable Development Goals (SDGs) 2 (Zero Hunger), 3 (Good Health and Well-Being), and 13 (Climate Action). Considering issues of residual cross-sectional dependence and slope heterogeneity which are potential in panel data setting, the study utilized the Augmented Mean Group and the Common Correlated Mean Group techniques as the main methods in estimating the relationships amid the employed variables. Major outcomes from the study’s analysis revealed that, across all panels of African states, there is no doubt that climate change has a substantial, direct detrimental impact on health outcomes. Also, while the moderating effect of climate change is clearly negative in the case of Northern and Central regional panels, it is significantly positive in the aggregated, Eastern, Western, and Southern African regions with regard to the relationship between food security and health outcomes. In light of these findings, addressing the relationship between food security and health in Africa while taking the moderating impacts of climate change into account requires a region-specific approach.
Similar content being viewed by others
Introduction
At the 1996 World Food Summit, the Food and Agriculture Organization (FAO) defined food security as the state in which "all people, at all times have physical and economic access to sufficient, safe and nutritious food that meets their dietary needs and food preferences for an active and healthy life" (Food and Agriculture Organization, 1996). A person’s ability to regularly obtain sufficient and nourishing food is emphasized by food security, which goes beyond the ease and measurement of food production. Achieving and ending hunger is acknowledged by Sustainable Development Goal (SDG) 2 as a critical factor in fostering sustainable socioeconomic progress and emerging economies, of which Africa is not an exception1. High nutrition-related problems coexist with poor health in Africa. Increased life expectancy, improved nutrition and the prevention of malnutrition, reduced poverty and hunger, and increased productivity are all possible outcomes of improved food security on the continent2. International human rights conventions frequently include food security as one of the core rights, which includes food availability, accessibility, use, and stability. Nonetheless, it continues to be among the most commonly infringed human rights3. Recent researches indicate that global food insecurity has increased despite the progress made in enhancing food security, especially under the Millennium Development Goals (MDGs)4. This indicates that SDG2 has not been achieved in a world population that is growing3,5.
According to The State of Food Security and Nutrition in the World (2022), Africa’s food security is extremely unsatisfactory because the continent trails significantly behind Europe, America, and Asia. The terrible state of food security in Africa is caused by a number of issues. Africa’s agricultural practices are mostly subsistence with little mechanization, despite the continent having a major share of the world’s arable land. For example, while irrigation covers 14% of cultivated land in Latin America and 37% in Asia, only about 5% of Africa’s agricultural land benefits from irrigation system6. The huge proportion of impoverished people in Africa who work in agriculture makes it difficult for the sector to adopt innovation and mechanization to improve food security. Specifically, food security is important for health because it guarantees that everyone has consistent access to enough safe, nourishing food to sustain an active and healthy life. Pérez-Escamilla7 argued that insufficient food supply can cause serious health inequalities that impact a person’s physical, social, emotional, and cognitive development over the course of their lifetime. Furthermore, food security includes not only the accessibility and availability of food but also its nutritional value and safety, both of which are critical for avoiding foodborne infections and guaranteeing general health8. According to Robertson, Tirado9, addressing food security through integrated, multisectoral strategies has been shown to lower healthcare expenditures, lessen the burden of disease, and benefit society socially and economically. Thus, maintaining food security is essential to advancing sustainable development objectives and public health10.
Furthermore, it has been discovered that climate change significantly affects health outcomes through a number of mechanisms, including water availability, and the spread of infections11. According to the World Health Organization (WHO), between 2030 and 2050, climate change may cause an additional 250,000 fatalities every year from heat stress, diarrhea, malaria, and malnutrition12. For instance, it has been noted that climate change makes food and water insecurity worse, which worsens health outcomes, especially for disadvantaged groups. In places like South Asia and sub-Saharan Africa, where poverty, state fragility, and high disease loads exacerbate climate-driven health crises, this relationship is clear11. According to the Intergovernmental Panel on Climate Change (IPCC) report, the impact of climate change on people’s health in Africa has been extremely substantial, especially for vulnerable groups such as women, children, and impoverished communities13. Extreme weather events, temperature swings, and changes in rainfall patterns are the main causes of the health issues facing the African continent. Water, food, vector-borne infections, malnutrition, and mental health consequences are all caused by these conditions14. According to the U.C.L. Lancet Commission, 34% of disability-adjusted life years (DALYs) worldwide occur in Sub-Saharan Africa as a result of climate change. With only 11% of the world’s population living in Sub-Saharan Africa, climate change presents a twofold health risk to the entire population15.
Particularly, the production, distribution, and availability of food are all impacted by climate change, which in turn has an influence on the health of millions of people throughout the African continent. Climate change is a moderator that affects the health outcomes linked to poor nutrition and exacerbates food insecurity. Agriculture systems are under stress as a result of increasingly unpredictable climate conditions, which lowers food output, raises food prices, and makes it harder to obtain wholesome food. The most vulnerable and impoverished groups, who are least equipped to cope with climate shocks, are disproportionately affected by these effects. The problem of enhancing food security to improve health outcomes is still significant, even with the research on food security and health in Africa16,17,18. The regulatory effects of climate change exacerbate this difficulty and continue to impede efforts throughout the continent. Given this difficulty, the research question that arises is: "How does improving food security improve health outcomes while conditioning the moderating effect of climate change?" To develop focused interventions that can lessen the negative effects of climate change on the relationship between food security and climate change, it is essential to comprehend this acclimatizing effect. Numerous regions of Africa are already experiencing the consequences of climate change. In the Horn of Africa, for example, droughts have resulted in severe food shortages, malnutrition, and a rise in mortality, especially among children and displaced people19. According to WHO20, floods in West Africa have also caused agricultural destruction, supply chain disruptions, and water source contamination, which has resulted into an increase in food shortages and waterborne disease outbreaks. The shifting patterns of disease transmission also demonstrate the moderating effects of climate change. Vector-borne illnesses like dengue fever and malaria are spreading more easily due to changing precipitation patterns and rising temperatures (WHO, 2020). Malnutrition exacerbates these health issues by weakening the immune system and increasing susceptibility to disease. In light of these dynamics, research into how climate change affects the relationship between food security and health outcomes in Africa and its regions is desperately needed. In order to improve food security, safeguard public health, and increase climate change resilience, policies and initiatives must take this into consideration.
Focusing on the connection between food security and health outcomes, the FAO, Ifad21 defines food security as having four pillars: food availability, accessibility, utility, and stability while the Global Burden of Disease22, shows that health outcomes are defined by a number of dimensions, including life expectancy, infant mortality, maternal mortality, infectious disease, and burden disease. Studies have, however, replaced the dimensions of health outcome and food security with the general terms "health," as measured by life expectancy10,18, and "food security," as measured by the food production index16,17,23. This study therefore demonstrated uniqueness by using the various dimensions of health outcomes and the pillars of food security to build indexes in order to evaluate the nexus between the mentioned variables, in contrast to the previously mentioned studies that used single proxies to measure food security and health outcome, respectively. Furthermore, after a careful review of the literature, no study conducted in Africa to the best of our familiarity has quantitatively investigated the association between food security and health outcomes while taking into account any indirect pathways that climate change may have on the aforesaid relationship. Majority of these research conducted in Africa either examine how food security affects health10,18 or how food security is affected by climate change3,24. Therefore, by investigating how climate change impacts the nexus between food security and health outcomes, our study bridges this gap and represents a beginning step. Furthermore, the sample of African research does not give sub-panel classifications any consideration when it comes to the literature on the connection between food security-health-climate change nexus in Africa. Significantly, however, findings may not be applicable to all nations due to the anticipated outcomes from the perspective of an aggregated panel and the potential for glaring differences in economic structure, technical capability, and resource endowment. To solve the lump sum problem, we divide the 45 African countries in the panel into five geographical groups: Northern, Eastern, Western, Central, and Southern Africa. More specifically, these particular geographic panels of African economies are the first of their kind to be examined in the literature on the relationship between food security and health outcome in Africa while taking into account the moderating effect of climate change. Lastly, in terms of methodology, most panel studies on the relationship between food security and health10,18,25 use standard panel estimation techniques, which ignore heterogeneity and cross-section residual correlations, leading to inconsistent results in a panel data analysis. Consequently, our study employs second-generation estimating methodologies that are resistant to the methodological problems in panel data settings in order to bridge this knowledge gap.
This study advances a novel conceptual framework by integrating systems theory26 with nutritional adequacy and ecological perspectives to explore the food security-health-climate nexus. Departing from prior research that often isolates these factors or assumes uniform effects across Africa27,28, the study conceptualize them as interdependent within a dynamic system, where climate change acts as an external shock moderating the food security-health relationship. This systemic, region-specific approach, rare in African studies accounts for heterogeneity in environmental, economic, and social contexts across Northern, Eastern, Western, Central, and Southern regions. Complementing this, the study’s multidimensional health index shifts from single-proxy measures (e.g., life expectancy18; ) to a holistic outcome framework, incorporating life expectancy, infant mortality, maternal mortality, infectious disease burden, and overall disease burden. This provides a more comprehensive understanding of health outcomes in the context of climate change and food security. Furthermore, the study adopts the FAO’s four-pillar framework for food security—food availability, accessibility, utility, and stability to construct a composite food security index. This approach moves beyond traditional single-dimensional measures (e.g., calorie intake or food production) and captures the multidimensional nature of food security, which is critical for understanding its impact on health outcomes. By explicitly examining the moderating role of climate change, the study offers new insights into how climate variability exacerbates or mitigates the relationship between food security and health outcomes. Together, these innovations rooted in systems theory, the FAO framework, and a multidimensional health index provide a robust and deeper understanding of the food security- health- climate change nexus in Africa.
It is impossible to overstate the importance of researching the relationship between food security and health in Africa while taking climate change’s moderating influence into consideration. First off, as Fig. 1 shows, this study has important ramifications for reaching the Sustainable Development Goals (SDGs) of the UN, especially SDG 2 (Zero Hunger), SDG 3 (Good Health and Well-Being), and SDG 13 (Climate Action). Reducing hunger and enhancing health outcomes in Africa requires addressing food insecurity and its effects on health. However, without accounting for the moderating influence of climate change, these targets will not be achievable. As climate change continues to transform public health and food systems, it is critical that attempts to accomplish the SDGs are based on a thorough comprehension of the relationship between food security, health, and climate. Finally, this research addresses critical knowledge gap in the current literature by exploring how climate change interacts with food security to influence health outcomes. Understanding these interactions is essential for designing effective interventions that address the short and long-term challenges posed by climate change.
Methods
Theoretical underpinning and empirical model building
A combination of interdisciplinary theories that emphasize the multidimensional nature of sustainability challenges and opportunities forms the theoretical foundation for comprehending the connections among food security, health outcomes, and climate change. In particular, theories about how food security affects health outcomes are based on the idea that regular availability to enough nourishing food is necessary to sustain optimal physical and mental health. People’s bodies get the nutrients they need to sustain healthy growth, immunological response, and general metabolic processes when they regularly have access to balanced meals29. The nutritional adequacy theory is a well-known theory regarding the relationship between food security and health outcomes. It asserts that preventing malnutrition and diet-related diseases like diabetes, obesity, and cardiovascular disease requires consistent access to a variety of nutrient-rich foods. Another viewpoint is the psychological stress theory, which contends that lack of availability or uncertainty in food access can raise stress levels, which can then have a detrimental impact on mental health and aid in the emergence of stress-related illnesses like depression and hypertension23.
Regarding how climate change affects health outcomes, the ecological theory holds that shifting habitats for mosquitoes and other vectors cause ecosystems and biodiversity to change, which in turn affects the spread of diseases like dengue and malaria30. Furthermore, because vulnerable populations thus those with less access to clean water, healthcare, and nutrition have a harder time adapting to environmental changes, the social determinants theory emphasizes how climate change exacerbates social inequality31. Furthermore, systems theory provides a useful perspective for examining the moderating influence of climate change’s interacting nature. Food production, economic policy, and the healthcare system are all impacted by external causes like climate change, according to this theory, which suggests that the relationship between food security and health functions within a larger, dynamic system. Food security and health outcomes are linked to the system’s capacity to withstand shocks, and climate change has the potential to either exacerbate or ameliorate this relationship. Investing in resilient food systems, climate-smart technologies, and health infrastructure are examples of adaptive measures that help the system stay balanced under pressure. For example, in systems that have made investments in climate adaptation, such as better weather early-warning systems or innovations in food storage, the detrimental effects of climate variability on food security are mitigated, protecting the population’s general health from the more severe effects of food shortages and malnutrition.
Summarily, these theories collectively illustrate the multifaceted effect of food security and climate change together with the moderating effect of climate change on health outcome. Considering the avowals with respect to the theoretical rationale, this extant study proposed a function in a multivariate framework to estimate the effect of food security on health outcomes by conditioning the moderating effect of climate change across all the regions in Africa as
where \(HLTH\) indicates health outcome index, FDS is food security index, CLM represents climate change, FDS*CLM is the interaction between FDS and CLM. Notably, the interactive term is included to examine the moderating effect of CLM on the link between HLTH and FDS.
Crucially, for estimation purposes, the explanatory variables need to be expressed as a linear combination of their corresponding parameters. Thus far, all variables have been changed to natural logarithms in order to enhance residual normality, strengthen the model’s interpretability, lessen the effect of extreme values, and minimize heteroscedasticity by stabilizing the error variance. Thus, our proposed transformed log-linear model in a panel multivariate context is specified as;
where \(lHLTH\), \(lFDS\), and \(lCLM\) correspondingly represent the natural logarithms of health outcome index, food security index and climate change.
In particular, to control for socioeconomic conditions in nations and time-varying bias that may influence changes in the dependent variable, the study incorporated control variables such as income (economic growth) and government health spending (expenditure). Thus, the specified model in Eq. (2) is extended as;
where \({\delta }_{0}\) is a constant term for the individual cross-sections, \({\delta }_{1}\), and \({\delta }_{2}\), are the parameter estimates which captures the effect of FDS and CLM on HLTH correspondingly, \({\delta }_{3}\) gauges the moderating effect of CLM on the HLTH-FDS nexus, \({\varnothing }_{j}\) is \(k\times 1\) vector of parameters which accounts for the respective effect of the control variables whereas \({Z}_{it}\) is also a vector containing the control variables (government health expenditure and income) , where \(i\) and \(t\) represents individual countries within a panel at specific time correspondingly and \({\varepsilon }_{it}\) represents the error term.
Specifically, by adjusting for economic growth, the distinct effects of climate change and food security on health outcomes can be distinguished without confusing them with more general economic gains. Similarly, adjusting for differences in health spending is crucial because it has a direct impact on how people perceive and respond to health concerns related to climate change and food security. This ensures that the effects being measured are due these factors and not underlying healthcare capacity or funding disparities.
Estimation approach
In particular, panel framework estimation of variables requires the use of panel time series data techniques. Therefore, the study first employed the Pesaran32 (PCSD) test in conjunction with Juodis and Reese33 Power Enhanced CSD-test (PECSDw +) to investigate residual cross-sectional correlations in the panel data used (The PSCD test is use to examine the presence or absence of CSD issues within the panel data whereas the PECSDw+-test is used in examining the strength of the CSD issues within the panel data). Furthermore, it’s critical to comprehend the data’s stationarity characteristics with regard to the study variables. Thus, to investigate unit roots, the study used Pesaran34 cross-sectional Augmented Dickey-Fuller (CADF) test due to the latent existence of residual cross-sectional connection in a panel data context. Once the stationarity qualities of the variables have been examined, the cointegration flanked by variables specified in the study’s suggested models is examined using the Banerjee and Carrion‐i‐Silvestre35(BCS) and Westerlund and Edgerton36(W-E) cointegration tests. Importantly, slope heterogeneity affects the consistency and efficiency of the estimated coefficients by introducing variation in error terms37. Ignoring this difficulty could lead to autocorrelation issues that go against important regression presumptions. Thus to determine whether heterogeneity is a significant concern, the Pesaran and Yamagata38(PY) homogeneity test is used.
The Augmented Mean Group (AMG) and Common Correlated Effect Mean Group (CCEMG) estimator long-run elasticity estimation approach by Bond and Eberhardt39 and Pesaran40 are finally used in light of the potential existence of heterogeneous slopes and cross-sectional residual connectedness in panel time series data. The AMG considers that unobserved common components are part of a common dynamic process (CDP) that may be estimated, rather than being considered a nuisance. The AMG cointegration estimation procedure is theoretically divided into two steps. First, a pooled difference ordinary least square (PDOLS) model with time-based dummy variables is estimated in order to determine the CDP estimate. The CDP is represented by the calculated parameters of these time dummies. Second, the CDP is either included in each of the N regressions or subtracted from the dependent variable in order to include it to the pooled difference OLS model. In our case, the dependent variable is deducted from the CDP. After estimating each of the N individual regressions, the averages or individual estimated slopes are calculated. Relying on these theories concerning the AMG estimator, the proposed study models are re-specified as;
where Eq. (4a) represents the pooled difference OLS models with dummy times variables \({D}_{t}\) during the first stage of the AMG approach whereas Eq. (4b) is the pooled OLS difference model with the common dynamic process \({\eta }_{t}\left({d}_{t}\right)\), subtracted from the dependent variable concerning the second stage of the AMG method of estimation, also \(\Delta\) denotes the difference operator and \({\theta }_{t}\) is the parameter estimates of the time dummies (Concerning the second phase of the AMG estimation approach, the parameter estimates of the time dummies \({\theta }_{t}\)are reparametrized to \({\eta }_{t}\)in the common dynamic process).
The parameter estimates of each variable is thus determined correspondingly by using the following relations;
where, \({\delta }_{i,AMG}\) represents the AMG estimator for a specific parameter estimate \({\widehat{\delta }}_{i}\) respectively.
According to the CCEMG technique, the common factors are considered nuisance parameters. The CCEMG technique includes unobserved components since it is necessary to consider a multi-factorial error structure given individual interminable regressors. The basic idea is to use cross-sectional techniques to filter the individual-specific regressors in a way that, as the cross-section dimensions approach infinity, the various biases from the unobserved factors are asymptotically eliminated. The linear combinations of the unrealistic elements are approximated by the CCEMG technique using cross-section averages of the dependent and independent variables. Next, standard panel regressions are conducted using these cross-section averages as a supplement. The panel regressions based on which the CCEMG estimator is employed are thus specified using the study variables as follows;
where \(\overline{lHLTH }\), \(\overline{lFDS }\), \(\overline{lCLM }\), \(\overline{{Z }_{it}}\), represents the cross-sectional averages of variables of interest and control variables utilized in the study, whereas \(\lambda\) denotes the group or panel specific linear trend.
Comparably, the various parameter estimates of the explanatory variables specified in Eq. (6) can thus be computed using the following CCEMG estimator expressed as:
where, \({\delta }_{i,CCEMG}\), represents the CCEMG estimator for a specific parameter estimate \({\widehat{\delta }}_{i}\) respectively.
The analytical framework is thus summarized in the Fig. 2 as:
Data and variables description
This current analysis used balanced panel time series data covering the economies of Africa between 2010 and 2022. We have selected 45 African countries for our sample, which is sub-paneled according to regional classifications (Northern, Eastern, Western, Central, and Southern areas of Africa), based on data availability and the need to maintain a highly balanced panel data. Supplementary Table S1 lists the members of the regional panels and the Aggregated panel. In particular, the data pertaining to climate change (CLM), which was measured using total greenhouse gas emissions along with government health expenditure (GHEXP), and income (GDP) were directly extracted from the World Bank Development Indicators (WDI) whereas that of health outcome (HLTH) dimensions were sourced from Global health database. Meanwhile, the Principal Component Analysis (PCA) was used to construct indexes for HLTH, food security (FDS), and its pillars. In contrast to previous research that solely used life expectancy as a proxy for health outcomes, this study, based on the Global Burden Disease (GBD) framework, demonstrated uniqueness by utilizing five dimensions thus life expectancy, infant mortality, maternal mortality, infectious disease, and burden disease—to construct an index for HLTH. Furthermore, according to41, food security is a significant issue but is practically hard to quantify. Its interconnected character is mostly to blame for this. Therefore, the aforementioned author contended that in order to gain a better understanding of food security, there has been a paradigm shift and conceptual development in this area. This includes a move away from limited availability, a move away from objective and subjective measurements, and a final shift in emphasis from proxy and distal measures to fundamental measurements. According to the Food and Agriculture Organization (FAO), focusing on just one aspect might not adequately represent the actual state and character of food security. Therefore, this study uses the FAO paradigm to capture the four pillars of food security: food availability (FAV), accessibility (FACC), usefulness (FUT), and stability (FST) in order to advance our understanding of food security. Specifically, each FDS pillar is quantified using different sets of items in accordance with the research of Lefe, Asare-Nuamah3. Specifically, aside Food stability and utility that were measured using three times each, Food availability was measured with five items, whereas food accessibility used four measurement items (See Table S2 for specific items assessing each pillar and their respective sources of data). The research ensured that indexes were as well created for each of the aforementioned FDS pillars prior to developing the FDS index. Instead of utilizing a single variable to describe a demission, the study included various data categories that make up a food security dimension. Thus, using the PCA the indexes concerning HLTH and FDS together with its respective pillars are computed in line with the linear combinations of their respective variables of concern as follows;
where;
Markedly, HLTHIND and FDSIND indicates health outcome and food security indexes; LEXP, INFMR, MMR, IDDR and BDR represent life expectancy, infant mortality rate, maternal mortality ratio, infectious disease rate and burden disease rate utilized as primary health outcome dimensions; FAVIND, FACCIND, and FUTIND, FSTIND also stands for indexes for the primary pillars of food security which includes food availability, accessibility, utility and stability; \({\alpha }_{i}{\prime}s\), \({\beta }_{i}\)’s, \({\updelta }_{i}\)’s, \({\uptheta }_{i}\)’s, and \({\upphi }_{i}\)’s distinctly represent the weights or the scoring coefficients which is generated by the respective eigen vectors of the derived principal components when computing the respective indexes; all the other variables from Eqs. 10, 11, 12 are described in Table S2.
Preliminary analysis
Notably, prior to performing the PCA, we standardized the data pertaining to the five dimensions of HLTH together with items measuring each pillar of food security so that the set of data values falls between 1 and 100 using the Standardized Min–Max Normalization approach. To do this, we create a function that will standardize one variable, and then apply that function to every column (for a specific dimension and measurement item) in the data. The PCA outcomes are thus displayed or outlined from Supplementary Table S4 to Supplementary Table S9 (Table S4 to Table S9 are all presented in the supplementary file). The first three components in Supplementary Table S4 and Supplementary Table S5 accounted for roughly 90% and 87% of the variance in the estimated HLTHIND and FAVIND indexes, respectively, while the first two components extracted from Supplementary Table S6 to Supplementary Table S9 were responsible for roughly 85%, 89%, 72%, and 86% of the variations in the estimated FACCIND, FUTIND, FSTIND and FDSIND respectively. A popular strategy, according to Jolliffe42, is to keep enough components to explain a specific threshold of total variance, often 70%–90% in PCA, in addition to depending on the components with eigen values greater than one. According to this claim, every component that was extracted to create the different indexes, together explained a significant portion of the differences in the respective ways. Furthermore, according to the estimations shown in the Supplementary Tables pertaining to the PCA, all of the series of variables used had substantial loadings evenly across components extracted correspondingly. This implies that the set of variables used satisfied all requirement to be taken into account when calculating the various indexes.
Additionally, Table 1 provides a summary of descriptive statistics, including the mean, standard deviation, and Jarque Berra (JB) normality tests for each study variable across all panels under investigation. With average food security index of 3.960 and 3.311, respectively, African nations in the northern regional panel and those in the southern regional panel are unquestionably the most highly rated. However, in a sequential and comparative manner, the Western, Eastern, and Central areas of Africa had poor levels of food security on average. Recent regional reports on food security and nutrition from the FOA, AUC, ECA, and WFP reinforce this, showing that, in comparison to other regions, Northern and Southern Africa have better food security and more people can afford a nutritious diet. Additionally, these areas often have lower rates of severe food insecurity and higher overall food access. However, the lowest food security indices are found in Africa’s Central, Eastern, and Western regions, where two-thirds of the population faces moderate food insecurity. The worst conditions for food security are found in Central Africa, specifically, and are made worse by environmental issues, economic instability, and conflict43. Furthermore, countries in the Central region of Africa recorded the lowest value of health outcome on average, indicating that these countries face more challenges, such as higher disease burdens and poorer access to medical care. In contrast, the Southern and Northern regions of Africa averaged the highest level of health outcome, indicating that the population in these regions generally enjoys better overall health. Generally due to improved economic resources, health interventions, and health infrastructure. Southern Africa generally enjoys superior health results. Improved life expectancy and mortality rates are a result of nations like South Africa and Egypt having the best access to healthcare services and controlling both communicable and non-communicable diseases. Central African nations, on the other hand, have challenges related to high mortality rates, inadequate healthcare infrastructure, and restricted access to medical treatments. For instance, the Democratic Republic of Congo continues to struggle with non-communicable diseases and communicable diseases like malaria, which are made worse by prolonged conflict and poverty. In a similar vein, Africa’s northern and southern regions, on average, reported the highest levels of climate change, while the Eastern and Central regions, respectively, had the lowest levels. In particular, both Northern and Southern Africa are more industrialized and consume more energy, particularly in nations like Egypt in Northern Africa and South Africa in Southern Africa. Conversely, the Eastern and Central regions consume less energy and are less industrialized over time. Due to lower levels of fuel use and industrial activity, the economies of many of these regions’ more agrarian nations produce fewer greenhouse gas emissions. Taking into account the case of the control variables, a largest average estimate of GDP per capita was evidenced in Northern region followed by Southern and Eastern regions whereas the Western region recorded the least average value. On the side of government health expenditure, Eastern region in Africa is characterized by the largest mean value followed by Western African region whilst Central region obtained the smallest average value.
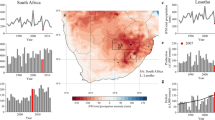
Additionally, the JB test findings for the study variables are statistically significant in all panels, indicating that the data concerning the variables employed do not follow a normal distribution. In addition, Fig. 3 displays the variables’ correlation analysis. Specifically, food security and climate change correspondingly showed negative and positive linear liaisons with health among the studied panels of African nations except for Southern African regional panel where both food security and climate are marked by negative correlation with health. Concerning the control variables, government health expenditure is negatively correlated with health across all the studied panel of African states whilst on the side of economic growth a mixture of both positive and negative correlations is witnessed across the whole and regional panels under study. In conclusion, as the correlation coefficient between the explanatory variables in the given model is less than 0.7, we do not consider the study to have any significant multicollinearity problems. Additionally, Fig. 4 displays or illustrates the average geographic distribution of the food security, and health outcome indexes together with climatic change, economic growth and government health expenditure from 2010 to 2022 (The various the data on food security, health outcome, climate change, gross domestic product and government health expenditure were expressed as values between 1 and 100 (using Standard Min-Max Normalization approach) to generate the generate geographical distribution diagrams. Hence the higher the value the better or worse a specific variable becomes. For instance, in the case of food security index, health outcome index, gross domestic product and government health expenditure, the higher the value the better the status quo and for climate change, the higher the value the worse the status quo becomes).
Empirical results
Test of cross-sectional dependences
In a panel data context, it is crucial to first investigate the problems of residual cross-sectional connection among cross-sections before estimating the study’s suggested model. Therefore, to address this objective, the PCSD and PECSDw+ tests are used. The null conjuncture, which contends that there is cross-section independence among cross-sections in a panel data, is the foundation of the PCSD test, as opposed to the alternative hypothesis, which makes the opposite claim. According to the PCSD test results, the null conjuncture is rejected for all study panels, proving that there are CSD problems in the data relating to every series from one regional panel to another. The depth of the aforementioned issue requires further investigation in light of the existence of CSD difficulties. To test the null hypothesis of weak cross-sectional residual reliance, the PECSDw+ technique is employed. The null hypothesis of weak residual cross-sectional correlations across all study panels is also rejected as a result of the PECSDw+ test results. This indicates that there are strong CSD issues with the panel data related to the series among the study panel. Table 2 thus summarizes the results related to the PCSD and the PECSDw+.
Panel stationarity and co-integration tests
As all variables in the research panels were impacted by significant CSD, the PCADF test of unit root, which is resilient in the presence of CSD, is used. Specifically, the stationarity qualities of the variables are analyzed based on constant via trend in order to exploit potential hidden features such as selecting appropriate methods, understanding relationships, and assuring the stability of variances and covariances. According to the PCADF results shown in Table 3, all variables in every panel have uniform unit roots in their levels (I(0)) and are stationary in their first differences (I(1)). This suggests that the same order of unit root integration characterizes all of the variable series employed in the study. Therefore, a long-term relationship between the series of variables taken together could be anticipated. Given that the variables in the series have the same order of integration, it is crucial to observe the long-term equilibrium (cointegration) among the variables under consideration. In order to achieve this goal, the BCS and W-E cointegration tests are used, with their respective results also outlined in Table 3. Notably, significant long-term equilibrium linkages between the used variables from the designated study model are evident from the aforementioned cointegration tests since the null conjecture of no cointegration is rejected in both cases across all the utilized panel. There is therefore the need to estimate the confirmed long-run relationships evidenced empirically in the subsequent section.
Panel slope-homogeneity test
The slope coefficients, which quantify the elasticities of the explanatory variables with respect to the response variables, must be examined to determine whether they are homogeneous or heterogeneous before estimating the confirmed long-run relationship among the variables listed in the study’s proposed empirical model. The choice of the best estimator to use to prevent spurious estimate is aided by determining if the slope coefficients are homogeneous or heterogeneous. Thus, the P-Y slope homogeneity test is executed. Slope homogeneity is the null hypothesis that the aforementioned tests rely on, as opposed to a different combination of slope heterogeneity. Table 4 makes it clear that the null postulate is rejected among the proposed empirical model across the study panels since the test values for the delta_tilde (∆ ̃) and adjusted delta_tilde (∆ ̃adj) statistics across all panels are statistically significant. The study’s postulated model is therefore clearly characterized by heterogeneous slope coefficients, which must be evaluated using heterogeneous panel estimators.
Augmented mean-group estimation
Bearing in mind the evidence of residual cross-sectional correlations and slope heterogeneity, this study as indicated utilized the AMG approach to estimate the nexus amid health and food security whiles taking into account the effect of climate change. Table 5 and summary illustration from Fig. 5 thus presents the results after estimating the study’s proposed panel data model using the AMG estimator. Comparatively, the outcomes evidenced from the aggregated panel and regional panels of African nations undoubtedly indicates that the effect of climate change on health outcome is significantly negative across all panels utilized. In the case of food security, significant positive impact is evidenced in the aggregated panel together with Northern, Central and Western regions of Africa whereas on the side of Eastern and Southern regions of Africa, palpable negative relations are evidenced with health outcome. Markedly, climate change is evident to positively moderate the food security-health outcome connection for the aggregated panel, Eastern, Western and Southern regions of Africa. Nonetheless, the picture took a different turn where, climate change negatively moderates the effect of food security on health outcome in the case of Northern and Central regions of Africa (The moderating effect climate change is captured by the interaction between food security and climate change). Taking into the account the results from the control variables, economic growth and health outcome are characterized by noteworthy negative connection in the aggregated panel of African nations, Northern, Central and Western regional panels whereas Eastern and Southern regions of Africa are pigeonholed by significant positive impact from income on health outcome. Finally, with the exception of Eastern regional panel, government health expenditure is noted to have significant positive influence on health outcome when it comes to the aggregated panel, Northern, Central, Western and Southern regions of Africa.
Interestingly, the Wald test and post estimation checks based on the Root Mean Square Error (RMSE) show that the estimated proposed health outcome model in each panel of African countries used is sufficiently credible and well-defined to produce innovative prediction results. This is because every value from the Wald test is statistically significant, and every estimate related to the RMSE is below the 0.7 threshold which is supported by44. In light of the possible significance of the interactions between cross-sectional residuals and heterogeneity, the current study investigated the robustness of the results from the AMG estimator using the CCEMG estimation method. Table S3 therefore summarizes the results of the CCEMG approaches. The estimated conclusions regarding the impacts of each explanatory variable and interaction term on health outcome are evidenced to be consistent with the AMG estimation results, despite the fact that parameter estimations differed in weight. Therefore, we can deduce that the outcomes of the AMG technique are accurate and dependable.
Discussions
The findings of this comprehensive study on the nexus between health, food security, and climate change across African regions reveals complex relationships that warrant careful examination. Our analysis, utilizing the Augmented Mean Group (AMG) approach, provides robust insights into the nexus amid these critical factors affecting human wellbeing across the African continent. The results not only highlight the significant impacts of climate change and food security on health outcomes but also underscore important regional variations that demand tailored policy responses. This discussion will delve into the key findings, exploring their implications for public health, food systems, and climate change adaptation strategies in Africa. By examining the direct effects and moderating influences observed in our study, we aim to contribute valuable insights to inform evidence-based policymaking and interventions aimed at improving health outcomes in the face of climate change and food security challenges.
Firstly, the findings highlight a pervasive and concerning trend, that is, climate change exerts a consistent and significant negative impact on health outcomes across all regions in Africa, albeit with varying magnitudes of effect that reflect regional disparities in exposure, vulnerability, and adaptive capacity. These results, with a robust body of evidence, highlight the intersection of climate change and public health, particularly in regions where socioeconomic fragility and environmental precarity converge. The analysis indicates that rising temperatures, erratic precipitation patterns, and extreme weather events, which are hallmarks of anthropogenic climate change, exacerbate health burdens through multiple pathways, including heat-related morbidity, waterborne and vector-borne diseases, malnutrition, and the disruption of healthcare systems. The universal negative relationship observed across regions corroborates the conclusion of the Lancet Countdown report 45, which identifies climate change as a critical amplifier of global health inequities, disproportionately affecting low- and middle-income countries with limited resources to mitigate or adapt to environmental shocks. This is particularly salient in Africa, where health systems already grapple with high burdens of infectious diseases, maternal and child mortality, and non-communicable diseases, all of which are further strained by climate-induced stressors. The pervasive negative impacts observed in Africa highlight the continent’s acute vulnerability to climate change, rooted in structural factors such as economic dependence on climate-sensitive sectors (such as rain-fed agriculture), inadequate healthcare infrastructure, and limited access to adaptive technologies. These findings align with Mekonnen and Hoekstra46, who demonstrate that climate change exacerbates water scarcity in Africa, directly affecting health through reduced access to safe drinking water and indirectly via conflicts over dwindling resources. For instance, in the Sahel, competition over water and arable land has intensified pastoralist-farmer conflicts, displaced populations, and increased trauma injuries, mental health disorders, and infectious disease transmission in overcrowded displacement camps. Furthermore, erosion of ecosystem services such as the loss of pollinator species due to habitat fragmentation, undermines nutrition security, exacerbating micronutrient deficiencies that compromise immune function and child development47.
Regional variations in the magnitude of climate-health linkages provide critical insights into the localized dynamics of vulnerability. Notably, Northern Africa emerges as the most severely affected region, with a pronounced decline in health outcomes linked to climate variable. This finding resonates with the projections by the Intergovernmental Panel on Climate Change48, which identifies North Africa and the Sahel as hotspots for extreme heat waves, prolonged droughts, and desertification factors that directly compromise health through heat stress, reduced agricultural productivity, and water scarcity49. For instance, rising temperatures in this region exacerbate cardiovascular and respiratory diseases, particularly among urban populations exposed to heat islands, while declining rainfall undermines food security, leading to malnutrition and stunted growth in children48. The Western region follows closely, with significant health declines also attributed to climate change. This aligns with studies documenting the dual burden of flooding and drought in West Africa, where erratic rainfall patterns disrupt crop cycles, heighten food insecurity, and propagate waterborne diseases such as cholera, particularly in densely populated urban areas with inadequate sanitation infrastructure48. The interplay of climatic extremes and pre-existing socio-economic vulnerabilities such as poverty, urbanization, and weak governance amplifies these effects, as noted by Haines and Ebi50, who emphasize that climatic changes act as a “risk multiplier” in settings where health systems lack resilience. In contrast, Eastern Africa exhibits a relatively lower, though still negative impact, a divergence that may reflect the region’s heterogeneous topography and microclimates, which could buffer certain populations from uniform climatic shocks. For example, highland areas in Ethiopia and Kenya may experience milder temperature increases compared to lowland regions, moderating heat-related risks. Similarly, the presence of large water bodies, such a Lake Victoria, might mitigate water scarcity in some areas, though this is counter balanced by risks of flooding and water contamination51. However, this apparent buffering effect should not obscure the region’s susceptibility to climate-driven health crises, such as the expansion of malaria transmission zone to higher altitudes due to warming trends, which threatens previously unexposed populations. The nuanced interplay of geographic and climatic diversity of Eastern Africa underscores the complexity of climate-health interactions, necessitating subnational analyses to capture intra-regional disparities. The study’s identification of climate change as a continent-wide health threat challenges narratives that frame its impacts as localized or incidental. Instead, the results affirm climate change is a systematic risk permeating all facets of public health, from infectious diseases dynamics to non-communicable disease burdens. This aligns with50, which argues that Africa’s unique geographical and socio-economic contexts —including high poverty rates, rapid urbanization, and governance challenges — render its populations disproportionately susceptible to climate-health synergisms. For example, urban slams in cities like Lagos in Nigeria and Nairobi in Kenya, characterized by poor ventilation and limited green spaces, amplify heat stress and air pollution exposures, compounding respiratory and cardiovascular conditions. Meanwhile, rural populations face dual threats of crop failure and zoonotic disease emergence, as habitat encroachment and shifting wildlife patterns increase human-animal interactions.
Additionally, the study’s finding underscore a statistically significant positive relationship between food security and health outcomes in the aggregated panel of Africa, as well as in the Northern, Central and Western African regions, illuminating the critical role of accessible, nutritious food in fostering population health. This relationship is particularly pronounced in regions where agriculture policies, food distribution systems, and nutrition programs have been strategically integrated into public health frameworks. The aggregated panel results suggest that, at a continental scale, improvement in food security —measured through indicators such as stability of food access —correlate significantly with enhanced health metrics including child stunting, lower maternal mortality, and decreased prevalence of communicable diseases linked to malnutrition. These findings align with the arguments of51, who posit that food security operates as a foundational determinant of health, shaping both physiological resilience and psychological well-being. In Northern Africa, for instance, nations such as Morocco and Tunisia have implemented large-scale agricultural modernization programs, including irrigation projects and subsidies for staple crops, which have stabilized food supplies and reduced-price volatility. These measures have not only bolstered caloric intake but also improved micronutrient availability, directly addressing deficiencies in iron, vitamin A, and zinc that contributes to anemia, impaired cognitive development, and susceptibility to infections. Similarly, in Western Africa, countries like Ghana and Senegal have prioritized the integration of nutrition-sensitive agriculture into development plans, ensuring that crops such as biofortified cassava and vitamin A-enriched maize are disseminated to vulnerable populations. This has been complemented by school feeding programs and community-based nutrition education, which synergistically enhance dietary practices and health literacy, as evidenced by declines in child wasting and acute malnutrition rates in these regions51.
The regional disparities observed —where Northern, Central and Western Africa exhibit positive food security-health linkages compared to Eastern and Southern Africa —can be attributed to differentials in policy coherence, infrastructure investment, and the scalability of interventions. In Northern Africa, relative political stability and higher GDP allocations to agriculture (averaging 10–15% of the national budget) have enabled sustained investments in climate-resilient farming techniques and food storage facilities, mitigating post-harvest losses that historically undermined food availability. For example, Egypt’s national silo network, developed through international partnerships, has reduced grain spoilage by 40%, helpng to maintain steady bread supplies, a vital staple for preventing hunger crises51. Also, Central Africa, while grappling with governance challenges, has seen localized successes in countries like Cameroon, where decentralized food distribution systems in partnership with non-governmental organizations have improved access to fortified foods in remote areas. These efforts are reinforced by regional trade agreements with the Economic Community of Central African States (ECCAS), which facilitate cross-border food flows during shortages, dampening price spikes and ensuring continuity of supply. In Western Africa, the positive food security- health nexus is further amplified by the proliferation of social safety nets, such cash transfer programs conditioned on health check-ups and prenatal care attendance. For instance, Nigeria’s National Social Safety Nets Program (NASSP) provides monthly stipends to low-income households, enabling them to purchase nutrient-dense foods while simultaneously incentivizing the utilization of primary healthcare52. This dual approach addresses both the immediate caloric needs and the structural barriers to healthcare access, creating a virtuous cycle where improved nutrition reduces disease burden, freeing household resources for further health investments. Such integrated models exemplify the findings of Sheahan and Barrett53, who emphasized that agricultural productivity gains alone are insufficient without parallel investments in healthcare infrastructure and social protection. The results also highlight the importance of temporal consistency in policy implementation. Regions exhibiting sustained positive outcomes, such as Northern Africa, have benefited from multi-decadal commitments to agricultural research and development. Morocco’s “Green Generation 2020–2030” strategy, which allocates $3billion to smallholder farmers for adopting drought-resistant crops and precision irrigation, has enhanced yield stability despite increasing climatic volatility54. These advancements have direct health implications, as stable food production curtails periods of hunger—conditions which are strongly associated with acute malnutrition and opportunistic infections in children under five. This aligns with the study of Dury, Bendjebbar55 who emphasizes that food security’s health dividends are contingent on equitable distribution mechanisms. Moreover, in Western Africa, the Senegalese government’s “National Food Security Stock” program maintains strategic reserves of rice, millet, and oil, releasing them during lean seasons to stabilize prices. This buffer has been instrumental in preventing the type of speculative price surges that, in other regions, render nutritious foods unaffordable for low-income households, forcing reliance on calorie-dense but nutrient-poor alternatives. By ensuring price stability, such polices indirectly reduce the incidence of diet-related non-communicable diseases like diabetes and hypertension, which are exacerbated by prolonged consumption of processed foods high in sugars and fats.
However, the study reveals a contrasting pattern in Eastern and Southern Africa, where food security shows a negative relationship with health outcomes. The study’s identification of a negative liaison amid food security and health outcomes in Eastern and Southern Africa presents a paradox that demands a nuanced exploration of the region’s socioecological and political complexities. While food security metrics often calibrated to caloric sufficiency or dietary energy availability suggest adequacy, the persistence of poor health outcomes accentuates limitations of conventional measurements in capturing the multidimensional nature of nutrition and systematic vulnerabilities. This divergence is particularly evident in contexts where political instability disrupts food systems. In countries like Sudan and Somalia in Southern Africa, protracted conflicts destabilize agricultural production, displace farming communities, and cripple infrastructure, severing access to markets and healthcare services. These disruptions create a façade of transient food availability through humanitarian aid, which may temporarily alleviate caloric deficit but fails to address the chronic deprivation of micronutrients essential of physiological resilience. For instance, in Somalia, despite international aid programs providing staple grains, 60% of children under five suffer from vitamin A deficiency, a condition linked to impaired immune function and heightened susceptibility to infections56. This phenomenon, termed “hidden hunger”, reveals a critical flaw in food security assessments that prioritize quantity over quality, making it insidious prevalence of iron, zinc, and folate deficiencies that erode health outcomes even in areas with ostensibly adequate food supply. The agroecological fragility of Eastern and Southern Africa further compounds these challenges. The Horn of Africa, as noted by Qu, Hao57, is ensnared in a vicious cycle of climate-induced droughts and soil degradation, with warming trends exceeding global averages. Recurrent droughts, such as the 2020–2023 catastrophe affecting Ethiopia, Kenya, and Somalia, decimate crop yields and livestock herds, the primary livelihoods for over 70% of the population. While food aid may buffer caloric intake, it often relies on energy-dense but nutrient-poor commodities like maize and wheat, exacerbating micronutrient gaps. Simultaneously, drought-driven migration to urban peripheries forces displaced populations into informal settlements with limited access to diverse diets, amplifying reliance on processed foods high in sugar and fats. This dietary transition, coupled with contaminated water sources in overcrowded camps, fuels a dual burden of malnutrition and waterborne diseases, as seen in the cholera outbreaks plaguing drought-stricken regions in Kenya. Such dynamics illustrate how environmental shocks interact with food systems to undermine both nutritional quality and health, even as caloric metrics suggest transient security.
Moreover, the structural underdevelopment of agricultural sectors in these regions (Southern and Eastern Africa) further entrenches this paradox. For instance, Southern Africa’s reliance on rain-fed subsistence farming, practiced by 95% of smallholders, leaves food production vulnerable to climatic volatility. In Zimbabwe, where maize yields have declined by 30% over two decades due to erratic rainfall, households increasingly depend on imported refined grains stripped of essential nutrients during processing. This shift has precipitated a rise in diet-related non-communicable diseases, with hypertension and diabetes rates climbing by 15% in urban areas in 2015, juxtaposed against persistent child stunting rate of 25%2,48. The lack of investment in irrigation infrastructure, diversification and post-harvest storage rooted in decades of economic austerity and governance failures perpetuates a cycle where food availability does not equate to nutritional adequacy. Besides, the interplay of HIV/AIDS and food uncertainty in Southern Africa reveals a syndemic dynamic, where disease and malnutrition mutually reinforce vulnerability. In Eswatini and Lesotho, HIV prevalence rates exceeding 25% have decimated agricultural labor forces, reducing household capacity to cultivate nutrient-rich crops like legumes and vegetables. Antiretroviral therapy (ART), while lifesaving, often heightens nutritional needs, creating a dire scenario where food-insecure households face increased exposure to opportunistic infections due to both immunodeficiency and micronutrient deficiencies. Drimie and Ruysenaar58 emphasize that Southern Africa’s health systems, already strained by HIV/AIDS and tuberculosis, lack the capacity to integrate nutrition-sensitive interventions, resulting in fragmented responses that fail to address the root causes of malnutrition. Governance failures further exacerbate these challenges. In Madagascar, political corruption and mismanagement have diverted funds from agriculture extension services, leaving farmers without access to drought-resistant seeds or training in sustainable practices. Consequently, even in years of adequate rainfall, post-harvest losses exceed 40%, undermining food availability59. Similarly, in Malawi, fertilizer subsidy programs, while boosting maize production, have neglected dietary diversity, leading to overdependence on a single crop and worsening deficiencies. These examples highlight that food security policies from nutritional and health objectives risk perpetuating cycles of hinder hunger.
Furthermore, the study’s exploration of climate change as a moderator in the relationship between food security and health outcomes across Africa reveals a complex interplay of regional vulnerabilities, adaptive capacities, and environmental dynamics, offering critical insights into how climatic shifts reconfigure the pathways through which food systems influence population health. At the continental level, the aggregated panel analysis demonstrates a positive moderating effect, indicating that climate change amplifies the health benefits from improved food security. This phenomenon is particularly pronounced in Western Africa, where innovations in climate-resilient agriculture, such as the adoption of drought-tolerant maize varieties in Ghana and Niger, have mitigated yield losses during erratic rainfall seasons. This stabilization ensures consistent access to calories and nutrients, directly reducing the incidence of acute malnutrition and related immune deficiencies in children, as documented by Wheeler and Von Braun27. Furthermore, the rising atmospheric CO2 levels, while a driver of global warming, have paradoxically enhanced the photosynthetic efficiency of certain C3 crops like sorghum and millet, prevalent in Western Africa. Studies by Edward R. Rhodes60 noted that CO2 fertilization has extended growing seasons in parts of Senegal and Burkina Faso, where farmers now harvest dual cropping cycles annually, increasing household food availability by 20–25%. This surplus not only averts seasonal hunger but also generates income through market sales, enabling investments in healthcare and sanitation factors that synergistically improve health outcomes. The positive moderation observed underlines the potential for climate adaptations to transform agricultural challenges into health opportunities, provided interventions are contextually grounded in scale. Eastern and Southern Africa present a paradoxical scenario where the direct relationship of food security and health outcome is negative, yet the climate change exerts a positive moderating effect. This contradiction stems from the region’s struggle with “hidden hunger” and governance failures. In Malawi, for instance, despite national maize surpluses from subsidy programs, 42% of children under five suffer from stunting due to diets dominated by maize, which lacks adequate protein and micronutrients. Climate change, however, is promoting shift toward diversified farming systems61. In Tanzania, agroforestry initiatives integrating drought-resistant tree like Faidherbia albida with staple crops have improved soil fertility and yield stability, increasing household access to nutrient-rich foods such as legumes and leafy greens62. This is attributed to the transition of NGO led climate adaptation projects that prioritize dietary diversity alongside productivity. Similarly, in Zambia’s adoption of conservation agriculture minimal tillage, crop rotation has reduced soil erosion and enhanced water retention, enabling farmers to cultivate vitamin A-rich orange sweet potatoes alongside maize. These practices, while not eliminating food insecurity, mitigate its health impacts by improving dietary quality. The positive moderation observed here suggests that climate adaptation, even in contexts of systemic food insecurity, can enhance the nutritional value of available food, thereby buffering health outcomes against climatic and economic shocks.
In contrast, Northern and Central Africa exhibit a negative moderation effect, where climate change undermines the historically robust link between food security and health. Northern Africa, particularly the Sahelian belt, faces intensifying desertification, with the Sahara advancing southward at 1.2 km annually, engulfing arable land and displacing pastoral communities. In Chad, the lake surface area of Lake Chad has shrunk by 90% since the 1960s, decimating fisheries and irrigation-dependent agriculture, which previously supplied 40% of the region’s dietary protein. As Niang, Ruppel28 emphasize, such environmental degradation disrupts traditional food systems, forcing reliance on imported refined grains that lack essential micronutrients. This shift has precipitated a dual burden: while caloric intake may appear stable, micro-nutrient deficiencies, particularly iron, zinc, and vitamin A, have surged, manifesting in elevated rates of anemia childhood stunting63. Health systems, already strained by malnutrition, are further overwhelmed by heat-related morbidity, illustrating how climate change erodes the capacity of food security gains to translate into health improvements64. Central Africa’s negative moderation is rooted in its unique hydrological and infrastructural challenges. For instance, the Congo Basin, despite its vast freshwater resources, experiences frequent flooding due to intensified rainfall variability, destroying crops and contaminating water supplies. In the Democratic Republic of Congo (DRC), annual floods displace 200,000 people annually, disrupting food distribution networks and spreading waterborne diseases like cholera, which claims 1,500 lives yearly65. Schmidhuber and Tubiello66 highlight that Central Africa’s limited adoption of climate-smart technologies such as flood-resistant rice varieties or elevated grain storage, leaves food systems vulnerable to these shocks. Even when food security initiatives succeed in boosting production, as seen in Cameroon’s maize belt, the lack of all-weather roads prevents surplus grains from reaching urban markets, leading to post-harvest spoilage67. This infrastructural deficit transforms potential health gains into losses, as communities remain trapped in cycles of scarcity and disease. The negative moderation here thus reflects a critical policy gap thus, investments of food production must be matched by climate-resilient infrastructure to ensure equitable distribution of health equity.
Considering the case of the control variables, the study’s findings reveal a paradoxical relationship between economic growth and health outcomes across Africa, challenging conventional narratives that equate economic prosperity with universal health improvements. Specifically, in the aggregated panel, as well as in Northern, Central, and Western Africa, economic growth exhibits a negative association with health outcomes, contradicting the widely held assumption that wealth generation inherently fosters better public health. This counterintuitive result highlights the complex interplay between economic expansion, socio-cultural inequities, and environmental externalities that mediate health trajectories. For instance, in Nigeria, Africa’s largest economy, GDP growth averaged 6% annually in early 2000s, yet maternal mortality rates remain among the highest globally, at 1,047 deaths per 100,000 live births68. This disparity reflects how growth-driven urbanization and oil-section industrialization have concentrated wealth in urban elites while rural populations, constituting 50% of Nigerians, face stagnant access to healthcare, clean water, and nutrition. Such inequities align with Pickett and Wilkinson69 income inequality hypothesis, which posits that unequal wealth distribution erodes social cohesion and exacerbates health disparities. In Lagos, Nigeria’s economic hub, the top 10% earners command 40% of the city’s income, while slum dwellers endure overcrowded living conditions, inadequate sanitation, and limited primary care access, fostering high rates of infectious diseases like tuberculosis and cholera68. Similarly, Ghana’s celebrated GDP growth (averaging 5% post-2010) has not alleviated stunting in Northern regions, where 33% of children under five suffer chronic malnutrition due to persistent poverty and agricultural neglect70. These examples illustrate that unmanaged growth can deepen spatial and socio-economic divides, leaving marginalized populations vulnerable to health crises despite macroeconomic progress.
Environmental degradation emerges as another critical mediator of the growth-health paradox. Rapid industrialization in Northern Africa, driven by sectors like cement production in Egypt, and petrochemicals in Algeria, has escalated air and water pollution, directly impairing respiratory and cardiovascular health. Also, Cairo’s annual PM2.5 concentrations average thirteen times above the WHO recommended limit, contributing to approximately 12.5% of all deaths related to lung cancer and chronic obstructive pulmonary disease (COPD)71. In Central Africa, deforestation for logging and mining key drivers of GDP in Cameroon and Gabon, has disrupted the ecosystem, increasing vector-borne disease risks. The Congo Basin, which absorbs 4% of global CO2 emissions, has lost 1.5 million hectares annually to illegal logging, fragmenting habitats and bringing humans into closer contact with zoonotic pathogens72. Fletcher, Hernández-Villena73 documented how such environmental exploitation correlates with malaria resurgence in deforested areas, where mosquito breeding sites multiply in stagnant water from abandoned mining pits. These dynamics highlight that growth strategies prioritizing resource extraction over ecological stewardship exert a heavy health toll, disproportionately affecting low-income communities reliant on natural ecosystems for sustenance and medicine.
Lifestyle changes accompanying economic modernization further erode health gains. Urbanization in Western Africa has spurred dietary transitions towards processed foods high in sugars, fats, and salt, driven by multinational corporate penetration and sedentary employment patterns. In Accra, Ghana, for instance, fast-food consumption has risen by 25% since 2015, paralleling a 15% increase in obesity rates and a doubling of diabetes prevalence74. A study by Modi, Panchani75 attributes these trends to the epidemiological transition, where societies shifting from agrarian to industrial economies face rising burdens of non-communicable diseases (NCDs) alongside persistent infectious threats. This dual burden strains underfunded health systems: in Senegal, NCDs account for 34% deaths, yet 70% of health budgets remain allocated to infectious diseases, reflecting institutional inertia ill-suited to evolving health demographics. In stark contrast, Eastern and Southern Africa exhibit a positive relationship between economic growth and health outcomes, aligning with traditional development paradigms. Kenya’s GDP growth (averaging 5.5% since 2010) has coincided with a 10-year increase in life expectancy, driven by expanded healthcare access. The rollout of universal health coverage (UHC) in 2018 subsidized insurance for 3.5 million low-income households, reducing maternal mortality by 35% through improved prenatal care access. Similarly, Rwanda’s post-genocide economic revival, with 7% annual growth, has seen under-five mortality drop by 75%, attributable to community-based health insurance76 and a network of 45,000 community health workers (CHWs). These successes underscore how pro-equity growth policies, redistributive taxation, social safety nets, and health infrastructure investment can channel economic gains into health improvements. Botswana exemplifies this synergy: diamond revenues fund Africa’s first public HIV/AIDS treatment program, achieving 95% antiretroviral therapy coverage and reducing AIDS-related deaths by 70% since 2005. Such models highlight that growth’s health dividends depend on governance quality and policy intentionality. The divergent outcomes between regions also reflect disparities in environmental governance. Eastern Africa’s renewable energy investments, such as Kenya’s geothermal projects and Ethiopia’s Grand Renaissance Dam, have decoupled growth from fossil fuel dependence, mitigating pollution-related health risks. Conversely, Nigeria’s oil-dependent economy exacerbates environmental health hazards: gas flaring in the Niger Delta emits carcinogens linked to leukemia rates five times the national average77. Southern Africa’s mining sector illustrates similar contrasts: Botswana’s stringent regulation of diamond mining minimizes ecological damage, whereas Zambia’s unregulated copper mines contaminate water supplies with heavy metals, causing kidney disease epidemics in the Copperbelt province.
Lastly, the study’s examination of government health expenditure and its relationship with health outcomes across Africa reveals a nuanced landscape where the efficacy of public health financing is deeply contingent on regional governance structures, spending efficiency, and the interplay of external stressors. In the aggregated panel analysis, as well as in Northern, Central, Western, and Southern Africa, government health expenditure demonstrates a positive association with health outcomes, reinforcing the pivotal role of state-led investments in healthcare infrastructure, workforce training, and perspective services. This aligns with Novignon, Olakojo78, whose analysis of Sub-Saharan Africa highlights that public health spending exerts a larger positive impact on health status compared to private expenditure, primarily by subsidizing care for low-income populations and scaling essential services like immunization and prenatal care. Similarly, Botswana’s decision to allocate 1% of its diamond revenues to health has enabled 95% antiretroviral therapy coverage for HIV patients, exemplifying the transformative potential of targeted fiscal policies. These successes highlight that when governments prioritize equitable resource distribution and institutional capacity building, health expenditures translate into measurable gains, such as reduced infant mortality, increased life expectancy, and containment of infectious disease outbreaks. In Western Africa, Ghana’s National Health Insurance Scheme (NHIS), established in 2003, illustrates how strategic public financing can bridge healthcare access gaps. By exempting premiums for the poorest 40% of households, NHIS has increased skilled birth attendance from 47 to 79%, directly lowering maternal mortality from 580 to 310 deaths per 100,000 live births79. This mirrors the findings of Akachi and Atun80, who attribute declines in child mortality across sub-Saharan Africa to scaled-up funding for malaria control, including bed net distribution and artemisinin-based therapies. The positive association in these regions thus reflects not only the volume of spending but also its alignment with evidence-based interventions. For example, Senegal’s decision to earmark 25% of its health budget for community health workers (CHWs) has enabled door-to-door malaria testing and treatment in remote areas, reducing under-five mortality by 40% since 2015. Such outcomes highlight that government health expenditure’s dividends depend on allocative efficiency directing funds toward high-impact, localized interventions rather than mere budgetary increases. Notably, the Central Africa’s positive government health expenditure-health relationship also offers lessons in adaptive governance.
However, the study’s identification of negative relationship between government health expenditure and health outcomes in Eastern Africa disrupts this narrative, exposing systemic inefficiencies and contextual vulnerabilities that undermine fiscal investment. In South Sudan for instance, despite health expenditures constituting 12% of the national budget, maternal mortality is the highest globally (1,150 deaths per 100,000 live births), with only 10% of births attended by skilled personnel. This paradox aligns with Anyanwu and Erhijakpor81, who found that health spending in Africa occasionally correlates with worsening outcomes due to leakages, corruption, and misallocation. In Eastern Africa, these inefficiencies are compounded with fragmented governance and conflict-driven disruption. For instance, Somalia’s healthcare system faces challenges due to limited government revenue generation, relying heavily on international and private sources for support82. Even in relatively stable Kenya, audits reveal that corrupt practices in Kenya’s county health systems negatively impact efficiency by leading to a direct loss of resources, increased operational costs, poor quality of care, reduced staff motivation and productivity, and reduced access to healthcare services83. These issues reflect broader failure to institutionalize accountability mechanisms, such as real-time expenditure tracking or community oversight, which are critical for optimizing government health expenditures.
Environmental degradation and demographic pressures further erode the effectiveness of health spending in Eastern Africa. Recurrent droughts in the Horn of Africa displace populations, strain health systems, and divert funds from preventive care to emergency relief84. Rapid population growth (3% annually in Uganda) outpaces healthcare capacity, with nurse-to-patient ratios worsening from 1:500 to 1:1,200 in rural areas over the past decade85. These challenges are aggravated by urbanization without infrastructure development in Nairobi’s informal settlement; majority of residents lack access to public clinics, forcing resilience on unregulated private providers who charge exorbitant fees for substandard care. This urban–rural disparity reflects the findings of Grigoli and Kapsoli86, who identify spatial inequities in health spending as a key driver of inefficiency in low-income countries, where urban-biased investments neglect peri-urban and rural populations. The interplay of epidemiological transitions and disease burdens further complicates government health expenditures in Eastern Africa. While infectious diseases like HIV and malaria remain prevalent, non-communicable diseases now account for about 35% of deaths in Kenya, yet less than 5% of health budgets address non-communicable disease prevention. This mismatch between funding priorities and disease profiles stems from rigid budgetary frameworks that prioritize vertical programs over integrated care models. In Tanzania, diabetes management receives only 2% of health expenditures, despite a 10% prevalence rate, leading to high rates of untreated complications such as renal failure and amputations. Such misallocations echoes Asante, Wasike87‘s critique of the African health system’s inability to adapt financing to evolving epidemiological realities, perpetuating cycles of inefficiency.
Specifically, the conceptual connection between climate change, food security, and health outcomes in this study are intricately tied to the proxy measures selected, which collectively operationalize to cascading impacts of environmental stressors on human well-being. Climate change, proxied by greenhouse gas (GHG) emissions, serves as a driver of ecological disruption that permeates food systems and health infrastructure. The FOA’s four-pillar framework for food availability, accessibility, utility, and stability provides a structural lens to dissect how climate variability destabilizes food security, thereby mediating health outcomes. For instance, GHG emissions, while directly contributing global warming, indirectly compromise food availability by altering precipitation patterns and increasing the frequency of extreme weather events, such as droughts and floods. These disruptions reduce agriculture yields, particularly in rain-fed systems predominant in Africa, which directly impacts metrics like crop production indices and irrigation coverage. Reduced availability then cascades into food accessibility, as supply shortages inflate prices, limiting economic access for vulnerable populations, a relationship captured through proxies like GDP. This economic strain forces households to prioritize calorie sufficiency over nutritional quality, undermining food utility, measured through dietary diversity. Concurrently, climate-induced volatility erodes food stability, which exacerbates episodic hunger and chronic malnutrition. These interconnected food security deficits manifest in health outcomes through pathways such as weakened immune systems (linked to infectious disease rates), maternal undernutrition (affecting maternal mortality ratios) and developmental stunting (impacting infant mortality rates). The health outcome index, integrating life expectancy, infant and mortality rates, together with infectious disease and disease burden, captures these multidimensional repercussions. For example, in regions like Northern Africa, high GHG emissions correlate with industrial activity and energy consumption, exacerbating aridity and heat stress. This not only reduces agricultural productivity (food availability) but also directly increases heat-related morbidity and vector-borne disease prevalence (for example, malaria expansion due to warmer temperatures). Here, the interaction between climate change and food security reveals a negative moderation: even when food is available, climate-driven instability in accessibility and utility such as reliance on imported, nutrient-poor staples during droughts fails to translate into health gains. Conversely, in regions like Western Africa, where agroecological practices may buffer climates shocks, the positive moderation suggests that food security improves under climate stress can mitigate health risks, such as child malnutrition.
The study’s nuanced use of proxies also explains paradoxical findings, such as the negative food security- health relationship in Eastern and Southern Africa. While aggregate food production indices might suggest adequacy, proxies for food utility such as dietary diversity, reveal hidden gaps. For instance, reliance on calorie-dense but nutrient-poor staples in these regions, compounded by climate-driven disruption to traditional food systems, leads to hidden hunger. This manifests in health metrics like high rates of anemia (affecting maternal mortality) and immunodeficiency (elevating infectious disease burden). Meanwhile, GHG emissions in these regions, often linked to deforestation and land degradation, further degrade ecosystems that traditionally support diverse diets, creating a feedback loop between environmental decline and poor health. The interaction term (food security * climate change) encapsulates these dynamics. In Central Africa, where climate change intensifies flooding and soil erosion, the negative moderation reflects how even modest improvements in food availability are nullified by instability in accessibility and utility such as post-harvest losses or contaminated water sources during flooding, which elevate diarrheal disease (a component of the health index). In Southern Africa, the positive moderation suggests that climate adaptation, such as drought-resistant crops or improved storage infrastructure, stabilize food access despite emissions-driven warming, thereby indirectly bolstering health by ensuring consistent nutrient intake. Grounding these relationships in multidimensional proxies, the study moves beyond simplistic cause-effect narratives. The GHG emissions proxy, captures the anthropogenic drivers of climate variability that strain food system, while the FOA pillars dissect how these strains propagate through economic, social, and biological pathways to affect health. This approach aligns with systems theory, where climate change is not merely an external shock but a dynamic modifier of the food-health nexus. For policymakers, this accentuates the need to pair emissions reduction with investments in food system resilience such as diversifying crops to enhance utility in order to disrupt the climate-food-health feedback loop. For researchers, the proxies demonstrate the value of granular, context-sensitive metrics in unpacking complex interdependencies, offering a blueprint for future studies to avoid oversimplification and embrace the multidimensionality of sustainable challenges.
Policy suggestions and research limitations
The results of this study highlight the critical need for region-specific policies to address the interconnected challenges of health, food security, and climate change across Africa. As emphasized by30, addressing climate change should be viewed as a significant public health opportunity. The consistent negative effect of climate change on health outcomes across all regions suggests an urgent need for stronger climate adaptation strategies. Policymakers should prioritize investments to mitigate the adverse impacts of climate-related stressors such as droughts, extreme temperatures, and water scarcity. Policymakers should prioritize the development and implementation of region-specific climate-resilience plans that address the unique vulnerabilities of each area. This could include investing in climate-resilient infrastructure, early warning systems for extreme weather events, improving water management infrastructure, and enhancing healthcare systems as well as agriculture to cope with climate-related health risks45,50. This is especially crucial in Northern and Western Africa, where the effects of climate change on health are most pronounced. Governments need to focus on enhancing the adaptive capacity of vulnerable populations by investing in early warning systems, water management, climate-smart agricultural practices, and training healthcare workers on climate-related health risks. Further, Eastern Africa’s relatively moderated risks though still significant demand adaptive strategies while preserving microclimates. Crucially, the climate-health impacts evidenced underlines the necessity of integrating climate adaptation into public health planning across all regions, prioritizing interventions such as early warning systems for extreme weather, climate-smart healthcare facilities, and community-based surveillance for climate-sensitive diseases. International cooperation, as emphasized in the Paris Agreement and Sustainable Development Goals, must prioritize financing for African nations to build adaptive capacity, ensuring that climate action and health equity go hand in tandem.
The positive relationship between food security and health outcomes in Northern, Central, and Western regions of Africa emphasizes the importance of improving food systems to boost health outcomes. Policies that promote agricultural productivity, food distribution, and nutrition-sensitive programs should be prioritized. For instance, integrating food security programs with healthcare services can help meet the nutritional needs of vulnerable groups, such as children and the elderly88. In contrast, Eastern and Southern Africa, where food security has a negative relationship with health outcomes, require targeted interventions focusing on food quality rather than quantity. Addressing micronutrient deficiencies through access to nutrient-rich foods and improving food production systems through sustainable agricultural practices can help ensure better health outcomes in these regions56.
The divergent moderating effect of across regions highlights the importance of localized climate-food-health nexuses. In Western Africa, the synergy between carbon dioxide fertilization, extended growing seasons, and adaptive agriculture creates a virtuous cycle where climate change inadvertently supports health through enhanced food security. Conversely, in the Northern and Central Africa, the interplay of desertification, infrastructural deficits, and reliance on nutrient-poor imports creates a vicious cycle, eroding health gains. Eastern and Southern Africa’s complex dynamics highlight the potential for climate adaptations to recalibrate food systems toward nutritional adequacy, even amid broader systemic failures. These findings necessitate a reevaluation of food security metrics to incorporate nutritional quality and distribution equity, ensuring that interventions address a full spectrum of climate-health instructions. Policymakers must therefore, prioritize integrated strategies that combine agricultural innovation, infrastructure development, and healthcare strengthening, tailored to regional ecological and socio-political contexts. Only through such holistic approaches can Africa navigate the dual challenges of climate change and health equity, transforming vulnerabilities into opportunities for sustainable development.
The negative relationship between economic growth and health outcomes in the aggregated panel, as well as in Northern, Central, and Western Africa, suggests that economic development alone does not automatically translate into better health outcomes. In these regions where rapid industrialization and urbanization may drive environmental degradation, occupational hazards, and lifestyle diseases may offset the benefits of economic expansion, policymakers must prioritize inclusive growth frameworks that couple economic development with environmental regulations, healthcare access, and social protections. For example, green industrial policies that incentivize clean energy production while creating jobs in the renewable energy sector could mitigate health risks linked to pollution and fossil fuel dependence. Further, policymakers should focus on addressing income inequality, improving access to healthcare for disadvantaged populations, and mitigating the negative health impacts of rapid urbanization and industrialization89. In Eastern and Southern Africa, where the relationship is positive, it highlights the potential of targeted investment such as rural healthcare infrastructure or sanitation projects to amplify the health dividends of economic progress. Also, sustaining this positive trend requires safeguarding gains against climate change and global economic shocks. For example, Kenya’s universal health coverage faces funding shortfalls as climate disasters increasingly redirect public resources toward emergency drought relief. Building long-term resilience therefore requires embedding health priorities within climate adaptation strategies, such as Ethiopia’s Productive Safety Net Programme (PSNP), which effectively integrates food security measures with access to essential healthcare services. These divergent outcomes emphasize that economic policies must be contextually calibrated, integrating health impact assessments to avoid unintended consequences.
The generally positive impact of government health expenditure on health outcomes highlights the importance of sustained and efficient public investment in healthcare. Policymakers should prioritize increasing health budgets and ensuring efficient allocation of resources. However, while most regions benefit from increased health spending, its inefficacy in Eastern Africa points to systemic issues like corruption, mismanagement, or fragmented service delivery. Here, simply boosting budgets without institutional reforms such as strengthening accountability mechanisms, training healthcare workers, or decentralizing decision-making will yield limited returns. This aligns with global evidence that spending efficiency often matter more than absolute amount. For international donors and governments, this underlines the importance of coupling financial support with capacity-building initiatives and governance reforms to maximize health outcomes in this region.
Finally, the study’s findings highlight the interconnected nature of climate change, food security, and health. This calls for integrated policy approaches that address these issues simultaneously. Policymakers should work towards developing comprehensive strategies that consider the complex interplay between environmental, agricultural, and health factors. This could involve cross-sectoral collaboration, integrated rural development programs, and holistic approaches to public health that consider both immediate health needs and long-term environmental and food security challenges. It is important to note that, despite the study’s contributions to the achievement of the Sustainable Development Goals (SDGs 2, 3, and 13), this existing study has certain limitations. First, an aggregated panel of 45 African countries—which were further separated into regional panels—was used in our study. Despite the benefit of employing an aggregated panel of African states as well as sub-regional panels for valid generalization and conclusions, the policy recommendations may not apply to all individual regions within the various panels used. Additional drawback is that while indexes for the study’s sub-dimensions (pillars) of food security were constructed, its main objective was to create an overall index for food security. The study did not examine the precise relationships between the sub-dimensions (pillars) of the food security index and health outcomes since it used the overall index or measure for food security. However, the issues with multicollinearity that arise when incorporating numerous sub-dimensions of the same construct in a regression model lead to biased results, which is why this decision was made. Another limitation of this study is its reliance on GHG emissions as a proxy for climate change, which effectively captures the driver of climate variability (e.g., temperature and precipitation shifts) linked to food security and health outcomes, but excludes broader perspectives such as climate impacts or vulnerability (e.g., ND-GAIN). While emissions robustly connect climate change to agricultural disruptions and health effects across African regions90, this focus on a driver rather than its consequences may overlook adaptation dynamics or regional exposure nuances. Lastly, the study did not consider the spatial dynamics of how climate change affects the relationship between food security and health outcomes over time; instead, it focused solely on the geographic distribution (spatial patterns) of variables among the African countries used for descriptive reasons. Despite these drawbacks, our research on regional variations in Africa nonetheless advances knowledge of contemporary circumstances and patterns pertaining to the interaction of food security, health, and climate change.
Conclusion and future research propositions
This study extensively examined the food security-health outcomes nexus while taking into account the moderating role of climate change across Africa. A plethora of time series and panel econometric techniques were employed to rigorously analyze a balanced panel data for 45 African countries grouped into five distinct regional panels from 2010 to 2022. Specifically, the augmented mean group and common correlated effects mean group estimators revealed heterogeneous relationships between the variables. Food security was found to significantly boost health outcomes for the aggregated African panel as well as the Northern, Central and Western regional groupings. However, perversely, food security access had a sizeably deleterious impact on population well-being amongst Eastern and Southern African nations. Additional findings indicated climate change exerted substantial direct harm towards overall populace health status across the continental spectrum. Yet, its moderating impacts diverged greatly according to geographical segmentation. Specifically, the climate moderator dampened the food security-health relationship severely within Northern and Central Africa. Contrarily, for the holistic African assemblage plus Eastern, Western and Southern territorial collectives, the moderator considerably accentuated the food security-health interplay positively. The disparate outcomes crystalize the necessity for diversified, region-focused strategies that cater to each area’s idiosyncratic food security-health-climate change interfaces. Only through tailor-made measures can the destabilizing consequences of global warming on Africa’s progress towards nourishment and wellness agendas be mitigated in a sustainable, equitable manner.
The findings of this study offer actionable insights for policymakers, development practitioners, and public health experts working to address the intertwined challenges of climate change, food security, and health outcomes in Africa. The regional heterogeneity in the moderating role of climate change on the food security- health nexus underscores the necessity of moving beyond continental or national generalizations to develop context-specific interventions. In Northern and Central Africa, where climate change exacerbates the negative relationship between food security and health, investments in climate-resilient agriculture practices must be prioritized. For instance, the adoption of drought-resistant crop varieties, improved irrigation infrastructure, and sustainable water management systems could mitigate the adverse effects of rising temperature and erratic rainfall on food production. Simultaneously, integrating climate adaptation into healthcare planning, such as strengthening disease surveillance systems for vector-borne illnesses linked to shifting climate change patterns, can buffer against health risks amplified by food security. Conversely, in Eastern, Western, and Southern Africa, where climate change positively moderates the food security- health relationship, scaling up existing successful strategies like agroforestry systems or community-based nutrition programs could leverage this synergy. Policymakers in these regions might focus on enhancing market access for smallholder farmers, promoting crop diversification to improve dietary diversity, and fortifying social safety nets to stabilize food access during climate shocks. These region-specific approaches must be underpinned by cross-sectoral collaboration, ensuring agricultural policies are aligned with public health goals and climate action frameworks.
A critical departure of this study from earlier research lies in its methodological and conceptual innovations. Unlike prior studies that often relied on single proxies for food security or health outcomes, this research employes multidimensional indices grounded in the FAO’s four pillars framework for food security and the Global Burden Disease’s health dimensions. This holistic approach captures the complexity of food security encompassing availability, accessibility, utility, and stability and health outcomes, including infant and maternal mortality, infectious disease, disease burdens, and life expectancy. For example, the negative association between food security and health in Eastern and Southern Africa, despite apparent food availability, likely reflects unmeasured factors like micronutrient deficiencies or food safety issues, which simplistic metrics overlook. By adopting comprehensive indices, the study reveals that food interventions must address not only quantity but also nutritional quality, safety, and equitable distribution to improve health. Similarly, the health outcome index’s inclusion of maternal and infant mortality, infectious diseases, and disability-adjusted life years (DALYs) provides a deeper understanding of how climate and food systems interact with health vulnerabilities. This multidimensionality challenges policymakers to design integrated programs, for instance, pairing agricultural extension services with nutrition education or maternal health clinics with food fortification initiatives to address interconnected risks. The study’s use of advanced econometric techniques, such as the AMG and the CCEMG estimators, further differentiates it from earlier works. These methods account for residual cross-sectional dependence and slope heterogeneity, common pitfalls in panel data analysis that previous studies often ignored. By rigorously addressing these issues, the findings offer more reliable estimates of climate change’s moderating effects, enabling precise policy targeting. For instance, the robust estimation of the Northern African’s heightened vulnerability to climate-driven health risks linked to its arid ecosystem and energy-intensive economies calls for tailored investments in renewable energy transitions and heatwave preparedness programs. Conversely, the positive moderation observed in Western Africa suggests that existing climate-smart practices, such as intercropping or soil conservation, are already yielding co-benefits for health, which could be replicated and scaled with targeted support. For researchers, this methodological rigor sets a precedent for analyzing complex, interdependent systems, encouraging future studies to adopt similar approaches when investigating multifaceted sustainability challenges. Another critical contribution is the explicit examination of climate change as a moderator rather than a standalone determinant. Most prior studies treated climate change, food security, and health as linear or isolated factors, neglecting their dynamic interactions. By modelling the interaction between food security and climate change, this study reveals that climate variability does not merely exacerbate food insecurity but alters the fundamental relationship between food systems and health. For example, in Southern Africa, food security alone is negatively associated with health—likely due to high rates of obesity and diet-related non-communicable diseases. However, the positive moderating effect of climate change suggests that climate-resilient food systems could paradoxically lead to better health outcomes by promoting agricultural shifts toward nutrient-dense crops and reducing dependence on processed food imports.
Furthermore, for researchers, concerning the aforesaid research limitations, this study opens several avenues for further exploration. First, future research could focus on heterogeneity in socio-economic conditions, institutional capacity, and climate exposure, offering more precise policy guidance than regional or aggregated panel approaches. Researchers could also disaggregate the food security index and examine the individual effects of its pillars —availability, access, utilization, and stability, on health outcomes, using statistical techniques that address multicollinearity, such as the partial least squares regression. Another involves investigating integrated intervention strategies that simultaneously tackle food insecurity, health vulnerabilities, and climate change adaptation or mitigation, potentially through interdisciplinary and mixed-method approaches. Moreover, expanding the proxy for climate change beyond GHG emissions to include vulnerability and impact indices like ND-GAIN or Climate Risk Index could provide a broader understanding of how climate dynamics influence food and health systems. Finally, incorporating spatial-temporal modelling would allow future studies to analyze how climate-related changes affect food security and health outcomes over time and across regions, using spatial econometric techniques to capture spillover effects and regional interdependencies.
In conclusion, this study advances the field by transcending simplistic, monolithic analyses of Africa’s climate-food-health challenges. Its regional lens, multidimensional indices, and sophisticated methodology provide a template for future research while yielding actionable insights to policymakers. By revealing how climate change differentially moderates the food security- health nexus across Africa, it compels a shift from uniform policies to tailored, integrated strategies that account for ecological, economic, and social contexts. For practitioners, the findings emphasize the urgency of cross-sectoral collaboration, equitable growth, and governance reforms to build resilient systems. For researchers, the study demonstrates the value of embracing complexity through advanced econometrics, systems thinking, and interdisciplinary frameworks to unravel the multifaceted dynamics of sustainable development. As climate change intensifies, such nuanced, evidenced-based approaches will be indispensable in safeguarding Africa’s health and food systems against an uncertain future.
Data availability
Publicly available dataset was analyzed in this study and can be extracted from the following outlined sources: Global Health-Our World in Data, https://ghdx.healthdata.org/ihme_data. World Bank Development Indicators (WDI) (https://databank.worldbank.org/source/2?country = IRN&l = en), Food and Agricultural Organization Corporate Statistical Database (FOASTAT) https://www.fao.org/faostat/en/#data. World Health Organization/Global Health Observatory https://aho.afro.who.int/ind/af?ind = 21&dim = 100&dom = Doen%C3%A7as%20cardiovasculares%20nas%20DNT&cc = af&ci = 1&cn = Afro%20Region.
References
Misselhorn, A. et al. A vision for attaining food security. Curr. Opin. Environ. Sustain. 4(1), 7–17 (2012).
Organization, W.H., The state of food security and nutrition in the world 2020: transforming food systems for affordable healthy diets. Vol. 2020.: Food & Agriculture Org. (2020)
Lefe, Y. D. H. et al. Does climate variability matter in achieving food security in Sub-Saharan Africa?. Environmen. Chall 15, 100870 (2024).
Hickel, J. The true extent of global poverty and hunger: Questioning the good news narrative of the Millennium Development Goals. Third World Q. 37(5), 749–767 (2016).
FAO, Africa Regional Overview of Food Security and Nutrition - In Brief. 2020: http://www.fao.org/3/ca7659en/CA7659EN.pdf. (2019)
Ringler, C., et al., Climate change impacts on food security in Sub-Saharan Africa: Insights from comprehensive climate change scenarios. (2010).
Pérez-Escamilla, R. Food security and the 2015–2030 sustainable development goals: From human to planetary health. Curr. Dev. Nutr. 1(7), e000513 (2017).
Walls, H. et al. Food security, food safety & healthy nutrition: Are they compatible?. Glob. Food Sec. 21, 69–71 (2019).
Robertson, A., et al., Food and health in Europe: A new basis for action (European series No 96), WHO Regional Office for Europe. (2004)
Subramaniam, Y., Loganathan, N. & Tang, C. F. Effect of food security on health in developing countries. Int. J. Soc. Determ. Health and Health Serv. 53(4), 414–423 (2023).
Gupta, V. et al. Adapting global health aid in the face of climate change. Lancet Glob. Health 5(2), e133–e134 (2017).
WHO, W.H.O. Climate Change. [cited 2024; Available from: https://www.who.int/health-topics/climate-change#tab=tab_1. (2024)
Campbell-Lendrum, D. et al. Climate change and vector-borne diseases: What are the implications for public health research and policy?. Philos. Trans. Royal Soc. B: Biol. Sci. 370(1665), 20130552 (2015).
Opoku, S. K. et al. Climate change and health preparedness in Africa: Analysing trends in six African countries. Int. J. Environ. Res. Public Health 18(9), 4672 (2021).
Byass, P. Climate change and population health in Africa: Where are the scientists?. Glob. Health Action 2(1), 2065 (2009).
Tackie, E. A. et al. Drivers of food security in West Africa: Insight from heterogeneous panel data analysis on income-level classification. Environ. Sci. Pollut. Res. 30(37), 87028–87048 (2023).
Brenya, R. et al. Food security in sub-Sahara Africa: Exploring the nexus between nutrition, innovation, circular economy, and climate change. J. Clean. Prod. 438, 140805 (2024).
Beyene, S. D. The impact of food insecurity on health outcomes: Empirical evidence from sub-Saharan African countries. BMC Public Health 23(1), 338 (2023).
Tadesse, T. et al. Improving national and regional drought early warning systems in the greater horn of Africa. Bull. Am. Meteorol. Soc. 99(8), ES135–ES138 (2018).
WHO. Devastating West and Central Africa floods affect over 4 million people, raise health risks. [cited 2024 September 2024]; Available from: https://www.afro.who.int/news/devastating-west-and-central-africa-floods-affect-over-4-million-people-raise-health-risks. (2024)
FAO, Ifad, and WFP, The State of Food Insecurity in the World 2015. Meeting the 2015 international hunger targets: taking stock of uneven progress. Food and Agriculture Organization of the United Nations, (2015).
Collaborators, G. & Ärnlöv, J. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1223–1249 (2020).
Gundersen, C. & Ziliak, J. P. Food insecurity and health outcomes. Health Aff. 34(11), 1830–1839 (2015).
Adesete, A. A., Olanubi, O. E. & Dauda, R. O. Climate change and food security in selected Sub-Saharan African Countries. Environ. Dev. Sustain. 25(12), 14623–14641 (2023).
Sultana, N. et al. Food insecurity and health outcome nexus: Empirical evidence from the informal sector enterprises in Bangladesh. BMC Public Health 23(1), 722 (2023).
Folke, C. et al. Our future in the Anthropocene biosphere. Ambio 50, 834–869 (2021).
Wheeler, T. & Von Braun, J. Climate change impacts on global food security. Science 341(6145), 508–513 (2013).
Niang, I., et al., Africa. Climate change 2014: impacts, adaptation, and vulnerability. Part B: regional aspects. Contribution of working Group II to the fifth assessment report of the intergovernmental panel on climate change. Climate Change 2014: Impacts, Adaptation and Vulnerability: Part B: Regional Aspects: Working Group II Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. p. 1199-1266. (2014)
Seligman, H. K. & Berkowitz, S. A. Aligning programs and policies to support food security and public health goals in the United States. Annu. Rev. Public Health 40(1), 319–337 (2019).
Patz, J.A. and H. Frumkin, Climate change and human health. Environmental health: From global to local. 275. (2016)
Bowen, K. J. & Friel, S. Climate change adaptation: Where does global health fit in the agenda?. Glob. Health 8, 1–7 (2012).
Pesaran, M. H. General diagnostic tests for cross-sectional dependence in panels. Empir. Econ. 60(1), 13–50 (2021).
Juodis, A. & Reese, S. The incidental parameters problem in testing for remaining cross-section correlation. J. Bus. Econ. Stat. 40(3), 1191–1203 (2022).
Pesaran, M. H. A simple panel unit root test in the presence of cross-section dependence. J. Appl. Economet. 22(2), 265–312 (2007).
Banerjee, A. & Carrion-i-Silvestre, J. L. Testing for panel cointegration using common correlated effects estimators. J. Time Ser. Anal. 38(4), 610–636 (2017).
Westerlund, J. & Edgerton, D. L. A panel bootstrap cointegration test. Econ. Lett. 97(3), 185–190 (2007).
Baltagi, B. H. & Rich, D. P. Skill-biased technical change in US manufacturing: A general index approach. J. Econom. 126(2), 549–570 (2005).
Pesaran, M. H. & Yamagata, T. Testing slope homogeneity in large panels. J. Econom. 142(1), 50–93 (2008).
Bond, S. and M. Eberhardt, Accounting for unobserved heterogeneity in panel time series models. University of Oxford. p. 1–11. (2013)
Pesaran, M. H. Estimation and inference in large heterogeneous panels with a multifactor error structure. Econometrica 74(4), 967–1012 (2006).
Webb, P. et al. Measuring household food insecurity: Why it’s so important and yet so difficult to do. J. Nutr. 136(5), 1404S-1408S (2006).
Jolliffe, I. T. Principal component analysis for special types of data (Springer, 2002).
FAO, A., ECA and WFP, Africa - Regional Overview of Food Security and Nutrition. Accra, Ghana: FAO ; AUC ; ECA ; WFP (2023)
Sarstedt, M., C.M. Ringle, and J.F. Hair, Treating unobserved heterogeneity in PLS-SEM: A multi-method approach. Partial least squares path modeling: Basic concepts, methodological issues and applications. p. 197–217. (2017)
Watts, N. et al. The 2020 report of The Lancet Countdown on health and climate change: Responding to converging crises. Lancet 397(10269), 129–170 (2021).
Mekonnen, M. M. & Hoekstra, A. Y. Four billion people facing severe water scarcity. Sci. Adv. 2(2), e1500323 (2016).
Potts, S.G., et al., The assessment report on pollinators, pollination and food production: summary for policymakers. Secretariat of the Intergovernmental Science-Policy Platform on Biodiversity (2016)
Trisos, C., et al., Africa. In: Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. (2022)
Pörtner, H. et al. Impacts, adaptation, and vulnerability. Contribution of Working Group II to the sixth assessment report of the intergovernmental panel on climate change (Cambridge University Press, 2022).
Haines, A. & Ebi, K. The imperative for climate action to protect health. N. Engl. J. Med. 380(3), 263–273 (2019).
Ryan, C. & Elsner, P. The potential for sand dams to increase the adaptive capacity of East African drylands to climate change. Reg. Environ. Change 16, 2087–2096 (2016).
Bank, W., A better future for all Nigerians: Nigeria poverty assessment 2022. (2022)
Sheahan, M. & Barrett, C. B. Ten striking facts about agricultural input use in Sub-Saharan Africa. Food Policy 67, 12–25 (2017).
Bank, T.W., international bank for reconstruction and development program appraisal document on a proposed loan in the amount of eur214.2 million (us$250 million equivalent) to the kingdom of morocco for a morocco green generation program-for-results (2020).
Dury, S., et al., Food systems at risk. New trends and challenges. CIRAD (Montpellier; France); FAO, CIRAD. (2019)
Harika, R. et al. Micronutrient status and dietary intake of iron, vitamin A, iodine, folate and zinc in women of reproductive age and pregnant women in Ethiopia, Kenya, Nigeria and South Africa: A systematic review of data from 2005 to 2015. Nutrients 9(10), 1096 (2017).
Qu, C., Hao, X. & Qu, J. J. Monitoring extreme agricultural drought over the Horn of Africa (HOA) using remote sensing measurements. Remote Sens. 11(8), 902 (2019).
Drimie, S. & Ruysenaar, S. The integrated food security strategy of South Africa: An institutional analysis. Agrekon 49(3), 316–337 (2010).
FAO, F.a.A.O.o.t.U.N., The future of food and agriculture Trends and challenges. (2017).
Edward R. Rhodes, E.N.T., Solomon Bangali State of Knowledge on CSA in Africa: Case Studies from Burkina Faso, Senegal and Sierra Leone. (2015).
Index, G.H. Malawi A Closer Look at Hunger and Undernutrition. Available from: https://www.globalhungerindex.org/case-studies/2018-malawi.html. (2019)
Saria, G., et al., Plant species composition, richness and diversity in different agroforestry practices of Moshi rural district, Northern Tanzania. (2025).
Egbuonye, N. C. et al. Examining the dietary diversity of children in Niger. Nutrients 13(9), 2961 (2021).
Onyeaka, H. et al. The ripple effects of climate change on agricultural sustainability and food security in Africa. Food Energy Sec. 13(5), e567 (2024).
Mbanzulu, K. M. et al. Mosquito-borne viral diseases in the Democratic Republic of the Congo: A review. Parasit. Vectors 13, 1–11 (2020).
Schmidhuber, J. & Tubiello, F. N. Global food security under climate change. Proc. Natl. Acad. Sci. 104(50), 19703–19708 (2007).
Forbanka, D. Post-harvest storage practices and insect pests of maize and beans in the North West Region of Cameroon. Afr. Entomol. 29(1), 133–141 (2021).
Ekwuazi, E. K., Chigbu, C. O. & Ngene, N. C. Reducing maternal mortality in low-and middle-income countries. Case Reports in Women’s Health 39, e00542 (2023).
Pickett, K. E. & Wilkinson, R. G. Income inequality and health: A causal review. Soc. Sci. Med. 128, 316–326 (2015).
Adjepong, M. et al. Association of whole blood n-6 fatty acids with stunting in 2-to-6-year-old Northern Ghanaian children: A cross-sectional study. PLoS ONE 13(3), e0193301 (2018).
Abera, A. et al. Air quality in Africa: Public health implications. Annu. Rev. Public Health 42(1), 193–210 (2021).
Tchiofo Lontsi, R. et al. Soil greenhouse gas fluxes following conventional selective and reduced-impact logging in a Congo Basin rainforest. Biogeochemistry 151(2), 153–170 (2020).
Fletcher, I. K. et al. The effect of environmental degradation and land use change on malaria re-emergence in south Venezuela: A spatiotemporal modelling study. Lancet Planet. Health 5, S13 (2021).
Adjei, A. P. et al. Availability of healthy and unhealthy foods in modern retail outlets located in selected districts of Greater Accra Region. Ghana. Frontiers in Public Health 10, 922447 (2022).
Modi, A. et al. The Phenomenon of Epidemiological Transition in Health and the Necessity to Update. NMO J. 17(2), 85–89 (2023).
Lu, C. et al. Towards universal health coverage: An evaluation of Rwanda Mutuelles in its first eight years. PLoS ONE 7(6), e39282 (2012).
Orisakwe, O. E. Crude oil and public health issues in Niger Delta, Nigeria: Much ado about the inevitable. Environ. Res. 194, 110725 (2021).
Novignon, J., Olakojo, S. A. & Nonvignon, J. The effects of public and private health care expenditure on health status in sub-Saharan Africa: New evidence from panel data analysis. Heal. Econ. Rev. 2, 1–8 (2012).
Sofo, S. & Thompson, E. Maternal mortality in Ghana: Impact of the fee-free delivery policy and the National Health Insurance Scheme. Int. J. Public Health Sci. 4(3), 232–237 (2015).
Akachi, Y. & Atun, R. Effect of investment in malaria control on child mortality in sub-Saharan Africa in 2002–2008. PLoS ONE 6(6), e21309 (2011).
Anyanwu, J. C. & Erhijakpor, A. E. Health expenditures and health outcomes in Africa. Afr. Dev. Rev. 21(2), 400–433 (2009).
Said, A. S. & Kicha, D. I. Implementing health system and the new federalism in Somalia: challenges and opportunities. Front. Public Health 12, 1205327 (2024).
Munywoki, J., et al., How does corruption influence health system efficiency? A case study of two counties in Kenya. MedRxiv p. 2023.06. 27.23291949. (2023)
Lindvall, K. et al. Health status and health care needs of drought-related migrants in the Horn of Africa—a qualitative investigation. Int. J. Environ. Res. Public Health 17(16), 5917 (2020).
Koutsoumpa, M. et al. Health workforce financing in Uganda: challenges and opportunities. Eur. J. Public Health https://doi.org/10.1093/eurpub/ckaa165.525 (2020).
Grigoli, F. & Kapsoli, J. Waste not, want not: the efficiency of health expenditure in emerging and developing economies. Rev. Dev. Econ. 22(1), 384–403 (2018).
Asante, A., Wasike, W. S. & Ataguba, J. E. Health financing in sub-Saharan Africa: from analytical frameworks to empirical evaluation. Appl. Health Econ. Health Policy https://doi.org/10.1007/s40258-020-00618-0 (2020).
Smith, L. C. & Haddad, L. Reducing child undernutrition: Past drivers and priorities for the post-MDG era. World Dev. 68, 180–204 (2015).
Lu, Z.-N. et al. The dynamic relationship between environmental pollution, economic development and public health: Evidence from China. J. Clean. Prod. 166, 134–147 (2017).
Romanello, M. et al. The 2023 report of the Lancet Countdown on health and climate change: The imperative for a health-centred response in a world facing irreversible harms. Lancet 402(10419), 2346–2394 (2023).
Funding
This work was funded by the National Natural Science Foundation of China (Grant No. 72274116), STU Scientific Research Initiation Grant (Grant No. STF20012) and Open Fund of Key Research Base of Philosophy and Social Science of Higher Education in Guangdong Province-Local Government Development Research Institute of Shantou University (Grant No. 07420005 and 07421005).
Author information
Authors and Affiliations
Contributions
The tasks and contribution to the work by each author are as follows I.A.M and S.A: Conceptualization. W.W: Supervision and Funding. I.A.M and S.A: Data curation and Formal analysis. I.A.M, and A.Y.O: Methodology and Software. I.A.M and S.A: Writing-Original Draft. W.W and A.Y.O: Reviewing, Editing and Validation-. All the authors have approved the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, W., Mensah, I.A., Atingabili, S. et al. Climate change as a game changer: Rethinking Africa’s food security- health outcome nexus through a multi-sectoral lens. Sci Rep 15, 16824 (2025). https://doi.org/10.1038/s41598-025-99276-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99276-2
Keywords
This article is cited by
-
The vulnerability of women and children in West Africa
Nature Climate Change (2025)