Abstract
The physical and chemical properties of implanted materials play a key role in their interaction with synthetic peptides that exert antimicrobial activity. In this study, we explored the diffusion properties and efficacy of the SET-M33 antimicrobial peptide in combination with artificial substrates, comprising cardiac implantable electronic devices (CIEDs) or porous protective envelopes. We found that porous materials, such as biosynthesized cellulose, polymeric meshes, and electrospun membranes, were conducive to SET-M33 diffusion. The diffusion dynamics was controlled by the intrinsic fibrous architecture of the materials. Biosynthesized cellulose supported the peptide’s antimicrobial activity against E. coli and S. aureus. The efficacy of SET-M33 was instead reduced when combined with the other tested porous membranes and non-porous CIED interfaces, such as titanium and silicone. On the other hand, the low porosity of biosynthesized cellulose membranes, while effective in retaining the drug, diminished diffusion and thus peptide availability. In light of these findings, the implications for the use of antimicrobial peptides in the prevention of CIED surgical pocket infections are discussed.
Similar content being viewed by others
Introduction
Implant infections have specific characteristics that make them different from, and more insidious than, local or systemic infections driven by the same agents in the absence of a foreign interface1. Contamination of an implant site by opportunistic pathogens, entering the pocket during the deployment of synthetic biomaterials, can lead to the colonization of the implant surface. Despite careful perioperative antiseptic protocols, bacterial infections are relatively frequent and typically more serious when associated with permanent prosthetics, such as cardiovascular devices (e.g. cardiac implantable electronic devices; CIEDs)2. Here, surgical pocket contamination requires systemic antibiotic treatment and immediate device extraction. Even when treated promptly, CIED infections tend to recur and become chronic, increasing mortality and healthcare costs3. For this reason, electrophysiology has been at the forefront of prevention and treatment of surgical pocket infections connected to permanent implants4.
The chemical and physical surface properties of implant materials govern their interaction with the surrounding cells and tissues5. Micro- and nano-scale geometries have been exploited to modulate the binding of biological molecules, and the ensuing adhesion of eukaryotic and prokaryotic cells6. Surface roughness has an impact on hydrophilicity, which is measured as the water static contact angle, and defines the ability of one surface to interact with soluble molecules7. Depending on the arrangement, symmetry, and size of the topographic features the hydrophilicity of a material can be increased or decreased, without interfering with other parameters such as the mechanical properties or the surface charge8. This principle can be used to tailor the interaction between an implant material and the biological fluids that will be in contact with it upon deployment in the body9. Topographies that modify surface properties to demote interaction with biological molecules, such as proteins and sugars, have the intrinsic effect of reducing biological coating (i.e. fouling)10. Anti-fouling surfaces have long been studied as a possible solution to dampen the inflammatory response to biomaterials11 and to reduce biofilm formation12.
CIED implantation currently represents one of the few indications for which protective devices are available to reduce post-operative risks13. Antibiotic envelopes comprise porous materials and deliver rifampin and minocycline to reach and maintain minimum inhibitory concentration (MIC90) in the pocket space for several days after implantation4. A large scale randomized clinical study demonstrated that the local and sustained delivery of these classic antibiotics from a resorbable mesh significantly reduces the rate of surgical pocket infections14. Whilst successful, these solutions are not equipped to address the surge of antibiotic tolerant or resistant bacterial strains, which are deemed to increase the rate of non-treatable infections15. Of particular relevance, in this scenario, are Staphylococci (e.g. S. aureus, S. epidermidis, etc.) and gram-negative bacteria such as E. coli16. Natural antimicrobial peptides (AMPs) are present across all types of living organisms and play a crucial role in their innate immune systems. These peptides are known for their broad-spectrum antimicrobial activity, effectively targeting bacteria, viruses, and fungi. Notably, they are less likely to contribute to the development of antimicrobial resistance (AMR) in bacteria and they are emerging as a solution to address this problem9,10.
Antimicrobial peptides kill microbes through various mechanisms, primarily by disrupting bacterial membranes. They form pores in the membrane, with models such as the barrel-stave, carpet, and toroidal-pore models explaining the different ways in which AMPs insert and destabilize the membrane. The lipid composition of the bacterial membrane, rich in anionic phospholipids, facilitates the insertion of cationic AMPs, whereas mammalian membranes, containing cholesterol, reduce AMP activity, providing selective toxicity17. AMPs’ physicochemical properties, such as hydrophobicity and amphipathicity, influence their membrane interaction, and specific amino acids like proline increase peptide flexibility and activity. In addition to membrane disruption, AMPs can also penetrate bacterial cells to inhibit vital cellular processes, including cell-wall synthesis and protein production. The overall effectiveness of AMPs is shaped by peptide characteristics, environmental factors, and the properties of the target cell membrane18.
The SET-M33 peptide, a synthetic non-natural peptide with an amphipathic amino acid sequence closely resembling natural antimicrobial peptides, was developed in preclinical settings19. SET-M33 has a tetrabranched structure, obtained using a scaffold of three lysine to support four identical sequence copies attached to their amino groups. This compact dendrimer displays improved stability against proteases, likely due to its larger size, which prevents it from fitting into protease cleavage sites20. This increased stability makes it stand out when compared to commonly used antimicrobial peptides (e.g. LL-37) which are susceptible to protease degradation21. Furthermore, the multivalent structure of SET-M33 enables stronger interactions with bacterial outer membrane components such as lipopolysaccharide (LPS) and lipoteichoic acid (LTA), leading to faster bacterial killing and beneficial immunomodulatory effects. SET-M33 demonstrated notable MIC90 values and effective biofilm eradication against a broad range of bacterial species22. SET-M33 exhibits a flexible conformation in aqueous solution but transitions into an amphipathic helical structure upon interacting with SDS micelles, mimicking bacterial membranes, as shown by circular dichroism analysis23. This structural change facilitates partial membrane insertion24. Investigation of its enantiomers, M33-D and M33-L, using vesicles mimicking S. aureus (CL/PG, 4:6) and E. coli (PE/PG, 7:3) membranes, revealed a dose-dependent increase in permeability, with M33-D showing slightly higher activity against CL/PG vesicles at higher concentrations25. Kinetic studies indicated a biphasic release profile, suggesting a shared membrane-disrupting mechanism independent of lipid composition25. Furthermore, scanning electron microscopy of P. aeruginosa and K. pneumoniae treated with SET-M33 displayed superficial blisters and large membrane disruptions within 60 min, supporting its membrane-targeting activity26. Additionally, SET-M33 showed in vivo efficacy in treating bacterial sepsis, pneumonia, and skin infections in mice26.
With the same principle of anti-fouling modifications, the surface geometry of biomaterials can be employed, together with the chemical-physical composition of the surface, to regulate the interaction with anti-microbial molecules27. The biomaterial surface therefore represents a potent parameter to enhance the effect of these drugs both in space and time. At the same time, the porosity of materials employed in protective envelopes controls the diffusion of soluble molecules and represents a key element to support the controlled elution of active chemicals28.
Here, we aim at evaluating the efficacy of the SET-M33 antimicrobial peptide in combination with the different implant materials that enter the CIED surgical pocket. The tests presented include the in vitro evaluation of (i) the ability of molecules to permeate porous materials and diffuse in aqueous solution and (ii) to efficiently eradicate bacterial contamination. Altogether, our work identifies viable biomaterials/antimicrobial combinations and indicates the optimal strategy for their deployment in surgical settings.
Results
Implantable materials selection
To evaluate the efficacy of the SET-M33 antimicrobial peptide in the prevention of post-operative infections associated with cardiac implantable electronic devices (CIEDs), two groups of materials were included in this study. First, materials that constitute the target implant, including Titanium alloy (Ti) for the battery case and silicone rubber (Si) for the battery head and lead velour. Polytetrafluoroethylene (PTFE) was added to this list as control, representing the standard for anti-adhesive and hydrophobic interfaces8.
All the experimental samples were obtained in the form of sterile coupons. The second group included materials used in the production of protective envelopes, such as a non-resorbable membrane made of biosynthesized biocellulose29 (BC), a resorbable PLGA electrospun membrane30 (Espn), and a resorbable PGA mesh31 (Mesh).
The selection included in this study is representative of the CIEDs and protective envelope materials in contact with the surgical pocket tissues. They represent the interface at which bacterial contamination develops in clinical settings. Their specific physical parameters, including porosity, fiber diameter, and/or surface topography and roughness, were similarly defined to reproduce the clinical conditions generated by medical devices currently marketed or in an advanced phase of development for this indication29,32,33,34.
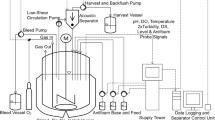
The methodologies employed in this study are presented in Fig. 1.
Testing set-ups and protocols are illustrated as follows: (a) costum-made side-by-side cell diffusion set up, (b) diffusion testing protocol, (c) antimicrobial efficiency testing: (1) sample treatment, (2) sample preconditioning, (3) bacteria inoculation, (4) bacteria recovery, (5) enumeration, (d) example of image processing for water static contact angle analysis.
Since unspecific affinity of antimicrobial peptides to implant materials is governed by physical and chemical properties31, including surface roughness, hydrophilicity, porosity, and fiber diameter (for the membrane-based materials) we first analyzed the surface morphology of the implant materials, using scanning electron (SEM) or light microscopy (Fig. 2). The envelope materials, BC and Espn, exhibited a similar interwoven fiber structure (Fig. 2a, b), though they differed significantly in porosity, expressed as a percentage of the total surface area (Table 1). Specifically, the porosity of the Espn (31.03%) was more than double that of the BC (11.98%). The macro-scale surface features of Mesh yielded a 63% porosity (Fig. 2c). The values concerning fiber diameter followed the same trend as those related to porosity. Specifically, BC displayed the smallest fibers (45 ± 0.013 nm) compared to Espn (790 ± 0.17 nm) and Mesh (232 × 103 ± 47 × 103 nm), which represented the material featuring the largest fibers. In contrast, target implant materials did not display regular surface patterns (Fig. 2d-f). Here, the surface geometry was characterized as nano-roughness35. PTFE and Ti exhibited comparable Ra (see Materials and Methods) values (1.86 ± 0.5 μm and 1.36 ± 0.28 μm, respectively), both significantly higher than Si, whose surface was closer to an ideal smooth form (0.14 ± 0.03 μm, Table 1).
Next, the water static contact angle (ca., see Materials and Methods) values were measured for each material to evaluate their wettability. The results are presented in Table 1. Among the tested surfaces, PTFE, as expected, proved the most hydrophobic (ca. = 108.48 ± 1.69°) followed by Espn (ca. = 101.14 ± 0.42°), Si (ca. = 79.66 ± 0.12°) and Ti (ca. = 76.65 ± 0.51°). Due to its known hygroscopic properties36, BC exhibited very low ca. Finally, the macroscopic architecture of the Mesh, did not allow performing ca. measurements.
Diffusion properties
Current standard-of-care for the use of protective envelopes in CIED implants requires the homogeneous elution of antibiotic molecules in the surgical pocket to achieve the minimum inhibitory concentration4 (MIC90). It is therefore critical to analyze the ability of antimicrobial peptides to diffuse across porous envelope materials (BC, Espn, and Mesh).
To study diffusion of the tetra-branched peptide SET-M33, a TAMRA-rhodamine labelled equivalent was obtained (TAMRA- SET-M33). The diffusion profile for TAMRA SET-M33 across each of the tested porous membranes was measured using a custom designed diffusion system (Figs. 1a and b and 3). From the absorption curves three independent parameters were obtained (Table 2). First, the diffusion rate, which indicates the speed at which particles spread or move from an area of higher concentration to an area of lower concentration, i.e. how fast the distribution occurs in the medium37. Second, the effective diffusion coefficient (Defy), which is defined as the rate of transfer of the diffusing substance across unit area considering the complexities and inhomogeneities of the system barriers, porosity, tortuosity, or the presence of multiple phases38. Finally, the drug retention, which accounts for drug that is retained in the separating membrane and is consequently not released in the acceptor compartment.
Diffusion trend of TAMRA-SET-M33 across BC (a), Espn (b), Mesh (c). (d) The graphs present the mean values of three measurements (n = 3) taken from the same sample at each time point, with error bars representing the standard deviation (SD). The dashed lines represent non-linear regression curves indicating the ideal trend of the time points. The continuous line shows half of the initial concentration of the molecule solution added in the Donor compartment. Panel (d) shows the calibration curve of TAMRA-SET-M33. These measurements were consistently replicated across three independent experiments, with one representative experiment depicted in the figure.
When moving across a BC membrane, TAMRA-SET-M33 concentration in the donor compartment decreased exponentially in the first 2 days, from 0.080 mg/ml to 0.036 mg/ml. An equilibrium between the two compartments was reached after 12 days, yielding values of diffusion rate and Deff of 0.7 × 10− 3 ± 0.59 × 10− 4 mg/h, and 0.0083 ± 0.0005 cm2/h; respectively. Importantly, the displacement of the peptide from the donor compartment did not match a corresponding increase in peptide concentration in the acceptor compartment. Equilibrium between the two compartments was reached at 0.02 mg/ml, indicating that a significant portion of the peptide (56.3% ± 1.7%) was retained within the membrane, as reported in Table 2.
Similarly, the equilibrium between the donor and acceptor compartments was reached after 12 days with the Espn membrane (Fig. 3b), yielding values of diffusion rate and Deff = 1.4 × 10− 3 ± 0.5 × 10− 4 mg/h and 0.003 ± 0.001 cm2/h; respectively. The concentration at equilibrium was reached below the expected value (indicated by the line in Fig. 3b) representing the ideal case at 0.034 mg/ml, indicating that a drug loss of 14.3% ± 1.7 occurred in this case. A different time scale was observed when evaluating Mesh samples, due to their macroscopic porosity (Table 2), with donor and acceptor compartments reaching equilibrium after 90 min (Figure 3c). In addition, Mesh allowed for the almost complete release of the antimicrobial peptide in the acceptor compartment leading to a concentration at equilibrium (0.046 mg/ml) close to the expected value (0.040 mg/ml). Altogether, these data indicate that, for the tested materials, the diffusion rate positively correlates with the membrane porosity whereas the overall drug retain has the opposite trend. A large proportion of the drug was retained by BC membranes.
Antimicrobial efficacy
Next, the antimicrobial performance of the SET-M33 peptide in combination with the selected implant materials was evaluated through in vitro bacterial challenge tests against S. aureus and E. coli. These bacteria were selected as representing the most frequent gram-positive and gram-negative pathogens in CIED pocket infections16. Two versions of SET-M33 were used. SET-M33L, prepared will all-L configuration aminoacids and SET-M33D obtained using D-aminoacids39. Primarily, the treatment with antimicrobial peptide SET-M33 caused an increased surface hydrophilicity in all the materials employed in the study (Supplementary Table S1).
To test whether the combination of the selected materials with the SET-M33 introduces additional safety concerns, a cytotoxicity test was performed using the THP-1 human monocytic cell line (Supplementary Figure S1I). These cells were selected as representing an established model for in vitro cytotoxicity tests40. All tested materials demonstrated optimal compatibility yielding cell viability above 90%.
The combination with SET-M33 did not introduce additional cytotoxicity and the viability remained comparable in all tested conditions (Supplementary Figure S1 II). These results indicate that the selected materials alone and in combination with SET-M33 demonstrate good biocompatibility.
Figure 4 displays the growth of E. coli on untreated and SET-M33L-treated samples after 24 h incubation. The growth of E. coli on non-treated samples was comparable on all tested surfaces indicating that no substrate-based effect could be measured (average growth on non-treated samples was 8.33 Log10 CFU/ml for PTFE, 8.15 Log10 CFU/ml for Ti, 8.23 Log10 CFU/ml for Si, 7.93 Log10 CFU/ml for Espn, 7.73 Log10 CFU/ml for Mesh, and 8.36 Log10 CFU/ml for BC; Fig. 4a-f). For the target implant materials, interaction of SET-M33L at all tested concentrations (3µM, 5µM, 10µM, 15µM) with PTFE and Ti substrates did not show any significant effect in reducing E. coli growth (Fig. 4a-b). On the other hand, bacterial growth on Si was reduced at 10 µM (5.06 Log10 CFU/ml) and 15 µM (5.03 Log10 CFU/ml), corresponding to 3x and 5x previously established MIC (Fig. 4c). The antimicrobial activity of SET-M33 on the implant materials was compared to the positive outcome of Rifampin treatment that inhibited the bacteria growth in all the surfaces and was indicated as the positive control in the experiment.
Growth of E. coli on PTFE (a), Ti (b), Si (c), Espn (d), Mesh (e) and BC (f) treated with increasing concentrations of SET-M33L, compared to untreated, Rifampin and H2O2 treated controls. Bars indicate mean and standard deviation (SD) among three replicates for each sample. Each graph represents one of three independent experiments that produced consistent results. **** Represents significant difference (p < 0.0001) between the treated sample and the untreated control.
For the envelope materials (Fig. 4d-f), a different trend was observed. With the increasing concentration of SET-M33, the growth of E. coli on Espn decreased linearly, leading to a significant reduction at 15 µM peptide (4.23 Log10 CFU/ml vs. 7.93 Log10 CFU/ml. Figure 4d). On the other hand, the treatment with SET-M33L did not have any measurable effect on bacterial growth on Mesh samples at any of the tested concentrations (Fig. 4e). Remarkably, a complete growth inhibition was obtained on BC membranes at all tested concentrations (Fig. 4f).
Comparable results were obtained when SET-M33D was challenged in combination with all the tested materials against S. aureus (Fig. 5a-f). No antimicrobial effect was detected on PTFE, Ti or Si (Log10 CFU/ml recovered were 7.05 Log10 CFU/ml for PTFE, 6.75 Log10 CFU/ml for Ti, and 7.34 Log10 CFU/ml for Si; respectively. Figure 5a-c). Similarly, Espn and Mesh substrates treated with SET-M33 had no significant effect on bacterial growth at any of the tested concentrations (Fig. 5d-e). On the contrary, when combined with BC, SET-M33 could fully eradicate bacteria at all tested concentration (Fig. 5f). Colony growth on agar plates for all the tested conditions is shown in the Supplementary Information (Supplementary Figure S3).
Growth of S. aureus on PTFE (a), Ti (b), Si (c), Espn (d), Mesh (e) and BC (f) treated with increasing concentrations of SET-M33L, compared to untreated, Rifampin and H2O2 treated controls. Bars indicate mean and standard deviation (SD) among three replicates for each sample. Each graph represents one of three independent experiments that produced consistent results. **** Represents significant difference (p < 0.0001) between the treated sample and the untreated control.
In light of the limited diffusion rate and high drug retention demonstrated by the SET-M33 across BC membranes (Fig. 3a), the efficacy of this combination was further evaluated. Specifically, an alternative configuration for the bacterial challenge was tested. While in the experiments reported in Figs. 4 and 5, the antimicrobial peptide and the challenging bacteria were applied to the same side of the BC substrates (cis configuration), in these furthers tests, the antimicrobial peptide and the challenging bacteria were applied to opposite sides (trans configuration) of the BC membrane. We previously demonstrated that bacteria cannot cross BC membranes29, however the efficacy of SET-M33 in these settings remains to be addressed and is bound to its ability to cross the BC membrane.
In the trans configuration, a marked reduction of antimicrobial efficacy against E. coli, was observed (Fig. 6a). At the lowest peptide concentrations, specifically 3 µM, 5 µM, and 10 µM, the AMP treatment exhibited limited effectiveness, with average colony counts of 7.19 Log10 CFU/ml, 6.8 Log10 CFU/ml, and 4.12 Log10 CFU/ml; respectively (vs. 8.09 Log10 CFU/ml in untreated). Complete inhibition of bacterial growth was only achieved at the highest tested concentration (15 µM). A similar trend was observed against S. aureus, as shown in Fig. 6b. These results demonstrate that the limited diffusion and high retention of the SET-M33 peptide across BC membranes hinders its efficacy against bacteria growing at the non-treated interface.
Growth of E. coli (a) and S. aureus (b) on BC when bacteria inoculation is performed on the opposite side of the sample with respect to the antimicrobial treatment. Antimicrobial peptide treatment is compared to untreated controls, Rifampin and H2O2 treated samples. Bars indicate the mean and standard deviation (SD) among three replicates for each sample. The results presented refer to one of two independent experiments performed that showed consistent results.
As control, the materials were treated with hydrogen peroxide (H₂O₂). H₂O₂ is routinely used for washing the CIED surgical pocket and the implant upon CIEDs implantation41. All tested materials were treated with a 3% H₂O₂ solution. The treatment was effective in erasing bacterial growth on all tested materials, when challenged with E. coli or S. aureus (Figure 4, 5). Interestingly, full efficacy was also observed when BC substrates were challenged in the trans configuration (Figure 6). To extend these conclusions to experimental conditions allowing the formation of biofilm, anti-biofilm assays were conducted using a genetically modified, bioluminescent E. coli strain. This strain enables the visualization and quantification of high- and low-density biofilm regions on biomaterial surfaces42.
The results (Supplementary Figure S3) confirm that the SET-M33L treatment exerted no detectable antibiofilm effect on the tested substrates, with the exception of BC. Here, a significant inhibition of both bacterial adhesion and biofilm formation was observed at all tested concentrations when the SET-M33 was combined in the cis configuration. On the other hand, a significant inhibitory effect on biofilm formation was only observed at the highest tested concentration (15 µM) when SET-M33 was combined to BC substrates in the trans configuration. These results confirm the findings obtained on planktonic bacteria (Fig. 6).
Discussion
The study investigates the interaction of the synthetic antimicrobial peptide SET-M33 with various implant materials used in cardiac implantable electronic devices (CIEDs) and protective envelopes. It highlights that porous biomaterials like BC and electrospun membranes facilitate peptide diffusion, enabling effective antimicrobial activity against pathogens such as E. coli and S. aureus. However, non-porous materials like titanium and silicone limit peptide efficacy. Notably, while BC retains a significant portion of the peptide, hindering its availability at distant sites, its ability to eradicate bacterial growth on contact demonstrates promise for targeted infection prevention.
The findings underline the critical role of material properties—such as porosity and surface morphology—in modulating peptide performance, emphasizing the need for tailored approaches in implant care. While current antibiotic-eluting envelopes offer infection control, the study advocates for optimized antimicrobial peptide delivery systems. These innovations could address growing antibiotic resistance by providing prolonged, localized infection prevention, potentially transforming postoperative care for CIED recipients. The current standard of care for the prevention of pocket infections in high risk CIED and neurostimulator patients recommends the use of antibiotic envelopes. These protective devices comprise a polymeric mesh which enforces the release of two antibiotic molecules in the surgical pocket for several days after implant31. To attain optimal protection, the antibiotics shall diffuse rapidly and homogeneously reaching a minimum inhibitory concentration in the pocket space, including the surrounding soft tissues and the implant interface. This aspect is key, as simple washes of the surgical pocket with antibiotic or antimicrobial solutions, performed during the surgical procedure, do not provide the same preventive benefit43,44. Looking at the future of infection prevention in implant recipients, the local and continued release of antimicrobial molecules shall therefore provide equivalent protection without eliciting antibiotic resistance. In this frame, the use of antimicrobial peptides opens the possibility to ensure long-term coverage extended to several weeks post implant, addressing the rise of late surgical pocket infections14. Sustained and homogeneous availability of an effective peptide concentration over space and time will necessarily depend on the complex interaction between the implant materials and the selected molecules. Two alternative solutions can be envisaged. First, the inclusion of antimicrobial peptides in protective envelopes similar to those currently available3132,that are assembled around the target implant before deployment. Second, the direct coating of the implant surface, including the battery case and leads. Both options carry intrinsic technical challenges.
Materials comprising the interface of electronic implants, including Titanium and Silicone, do not support the antimicrobial activity of the SET-M33 against S. aureus and E. coli in our experimental settings. These substrates are selected with a functional intent. By design, they are non-porous and relatively smooth with the intention to limit fouling. It is therefore to be expected that the simple coating of titanium and silicone is not sufficient to support the activity of the SET-M33 peptide. Variations in surface roughness, chemistry and/or wettability of these materials, which may facilitate coating, are not simply implemented. Any such modification would bring into question the overall device functionality. Furthermore, the stochastic nature of SET-M33 peptide surface adhesion influences its structural conformation and affects the material surface nature. As antimicrobial activity is intrinsically dependent on peptide structure, uncontrolled interactions with material surfaces may attenuate its efficacy. Along this line, the only viable development shall envision the chemical engineering of the peptide itself, to include functional groups allowing controlled interaction with the target surface, without compromising the antimicrobial effect.
Fibrous protective envelopes display high porosity, which depends on the fiber size and architecture, rendering them conducive to SET-M33 adsorption and diffusion. The combination of these two processes supports the antimicrobial activity of the peptide in bacterial challenge tests. Altogether, more flexibility is possible in the selection of excipients and architectures for the protective envelopes. The structure of these devices is porous, however with variations which are dependent on the fabrication method. Porosity and chemical composition define the ability of soluble molecules to cross the intervening layer formed by the envelopes between the target implant and the surgical pocket tissues. For optimal distribution, large molecules such as peptides should diffuse rapidly, typically in the first hours after implants. This is granted by structures with macroscopic pores, such as meshes. Envisioning a simple loading of an antimicrobial solutions into the matrix of an envelope material, shall leverage the loading capacity of the matrix itself. This is very high in hydrogels such as biosynthesized cellulose and can lead to more effective antimicrobial protection.
On the other hand, drug retention must be considered as a factor influencing the antimicrobial efficacy of biomaterial-peptide combination. Drug retention in the selected porous materials has different implications towards the clinical use in protective envelopes. BC is non-resorbable29 and protective BC envelopes are conceived to enforce a durable intervening layer6. The average pore size of the BC layer impedes the penetration of bacteria, which are confined to its surface29. Antimicrobial peptides which are stably retained in the BC matrix may therefore not contribute to the antibacterial effect (Fig. 6). In this scenario, high drug retention hinders the potential efficacy of AMPs in combination with BC. On the other hand, smaller antimicrobial molecules, which have a diffusion coefficient similar to water, are able to exert full activity across BC membranes. Diffusion and retention are therefore important parameters determining the effective availability of antimicrobials in combination with BC. Resorbable materials (Mesh and Electrospun) still display a small fraction of peptide retention (Table 2). Upon implantation, the fibers (e.g. PLGA, PGA, PEG, and similar) undergo degradation by hydrolysis45,46. This process induces additional pore formation, followed by fragmentation47,48. The drug initially retained in the matrix shall therefore be released over time, as demonstrated by marketed products featuring in vivo elution over several days4. This mechanism opens therefore to the sustained release of AMPs loaded in resorbable porous materials.
In summary, it appears that the current state of development for antimicrobial peptides, which are optimized for the protection of surfaces from biofilm formation25, will not be immediately translated into off-the-shelf solutions for the postoperative protection of surgical pockets hosting permanent implants. Dedicated peptide configurations will be required, with modifications ensuring optimal efficacy and prolonged and homogeneous coverage in the complex environment of the surgical pocket. To effectively address the critical challenge of antibiotic-induced microbial resistance in surgical pocket care, this paper’s findings lay the groundwork for the development of next-generation antimicrobial drugs. Antimicrobial peptides may offer a promising alternative to antibiotics for surgical environments, if tailored to match—and ultimately surpass—the efficacy of current antibiotic envelopes, offering a more sustainable and resistant-free solution for infection prevention in implant care.
Methods
For the presented experiment the tested implant materials were divided into two groups: Permeable materials: Materials with porosity allowing for percolation of soluble molecules. Biocellulose membrane (BC), Electrospun PGA/PLGA membrane (Espn) and PGA Mesh in the form of rectangular samples of 4 × 3 cm. Non-permeable materials: Titanium (Ti), Silicon (Si) and Polytetrafluoroethylene (PTFE) in the form of implantable standardized sterile coupons of 12.7 mm diameter x 3.8 mm height (RD128-Ti6AL, RD128-Si, RD128-PTFE, BioSurface Technologies).
Scanning electron microscopy
Samples were sputter coated with 4 nm Pt/Pd and images were acquired with TFS Magellan 400 (Thermo-Fisher Scientific) with field emission 200 kV via secondary electron detection. To image BC membranes samples were previously dried via critical point drying.
Light microscopy analysis
Bright field image was taken with Leica DMi8 microscope with integrated camera, using 5X objective.
Image analysis
SEM images were analyzed to extract physical parameters relative to envelope materials. The porosity and fiber diameter were extrapolated via imaging analysis using ImageJ (National Institute of Health, US), as follows.
Porosity measurement. To assess porosity, the images were first converted to 8-bit format. The “Threshold” function was the applied. Specifically, the pixel intensity distribution varied until all pores were captured. Subsequently, using the “Analyze” menu, the “Measure” function was selected, and porosity was calculated as a percentage of the total image area.
Fiber Diameter Measurement. Fiber diameter was quantified importing SEM images. The scale was set via the “Set Scale” function. For each fiber (n > 15), a line was drawn across its diameter, ensuring the endpoints were aligned with the fiber edges. The “Measure” function was then employed to determine the fiber diameter based on the traced line.
Surface roughness
Surface roughness measurements were conducted at RT using a calibrated MAHR PS-1 Surface Roughness Measuring Instrument (SFS, Switzerland). The measurements were performed in accordance with ISO 4288 and ASME B46.1 standards, with a cutoff length of 1.75 mm. In regions where sanding grain was detectable, measurements were taken perpendicular to the grain direction to ensure accuracy. Surface roughness is quantified by the deviations in the direction of the normal vector of a real surface from its ideal form and measured by the parameter Ra: the average of how far each point on the surface deviates in height from the mean height.
Water static contact angle
Hydrophilicity of material surfaces was measured via water static contact angle analysis. Specifically, a controlled volume (20 µl) of DI water was carefully placed on the surface of each material. Firstly, the samples were washed by immersion and sonication for 5 min in DI water, followed by isopropanol and again DI water and dried under nitrogen flow. Each sample was placed on a flat surface, against a dark background to enhance the visibility of the object’s contours in the image. Pictures were taken with ƒ/1.6 aperture camera equipped with macro lens and saved as RGB color. Each image was analyzed with the software ImageJ. The RGB image was split in the blue, red and green channel and the red color channel was selected for the analysis. The image was further processed using the function “invert’ to provide a better visualization of the drop against the background. The water static contact angle (c.a.) was measured using the drop analysis plug in of ImageJ defining the drop contours and allowing the software for the fitting and calculation of the internal angles that define the hydrophilicity/hydrophobicity of the surface. Figure 1d provides an example of processing. A c.a. below 90° indicates hydrophilicity, while values above this threshold denote hydrophobicity.
Peptide synthesis
The peptides SET-M33D (kkirvrlsa)4K2KβA-OH and SET-M33L (KKIRVRLSA)4K2KβA-OH were solid-phase synthesized by standard Fmoc chemistry using D-amino acids with a Syro multiple-peptide synthesizer (MultiSynTech, Witten, Germany), as previously described22. TentaGel-PHB 4 branch βAla Wang-type resin (Rapp Polymere, Germany) was used, which carries the branching core in L-form, Fmoc4-Lys2-Lys-β-Ala.TAMRA-SET-M33 was synthesized using FmocLys(TAMRA)OH as first aminoacid, FmocPEG4-OH as second coupling step and FmocLys(Fmoc)OH as third and fourth coupling steps. Sidechain-protecting groups were 2,2,4,6,7- pentamethyldihydrobenzofuran-5-sulfonyl for R, t-butoxycarbonyl for K, and t-butyl for S. The final product was cleaved from solid support, deprotected by treatment with TFA containing triisopropylsilane and water (95/2.5/2.5), and precipitated with diethyl ether. Crude peptide was purified by reversed-phase chromatography on a Phenomenex Jupiter C18 column (300 Å, 10 mm, 250, 610 mm), using 0.1% TFA/water as eluent A and methanol as eluent B, in a linear gradient from 80% A to 20% A in 30 min. Final peptide purity and identity were confirmed by reversed-phase chromatography on a Phenomenex Jupiter C18 analytical column (300 Å, 5 mm), and by mass spectrometry with a Bruker Daltonics Ultraflex MALDI TOF/TOF).
Diffusion testing
For the diffusion tests a costum-made side-by-side cell diffusion set-up (Fig. 1a) was built assembling two 50 ml LDPE bottles provided with a 1.2 cm2 aperture on the screw cap face and a 0.2 cm2 aperture on the side. The bottles were aligned horizontally with the two openings facing each other, creating two separate chambers. The system was sealed using a 3D printed PLA support together with a screwing system.
For each test, a 3 × 3 cm membrane sample was cut and placed between the two apertures. An O-ring was used to ensure a complete seal, preventing leakage. One of the two chambers was designated as Donor compartment and filled with 12 ml TAMRA-SET-M33 PBS solution (0.08 mg/ml), while the second chamber, identified as the Recipient was filled with a blank solution of PBS. Magnetic bars were included in both chambers and the system was incubated at 37 °C on a stirring plate. To measure diffusion, a calibration curve for TAMRA- SET-M33 dissolved in PBS was initially determined using a Nanodrop One Microvolume UV-Vis spectrophotometer (Thermo-Fisher Scientific) to measure absorbance at ʎ = 555 nm. The Lambert-Beer law was then used to convert absorbance of each sample in a concentration value (mg/ml). The corresponding protocol is shown in Fig. 3b. Based on the calibration curve (Fig. 3d), the time to equilibrium was measured and the diffusion rate and effective diffusion coefficient (Deff) were obtained for each diffusion experiment. Specifically, to evaluate the diffusion dynamics, the chambers were sampled every 2 days. Individual samples of 100 µl were collected and absorbance at ʎ=555 nm was immediately measured.
Bacterial culture
Reference strains of E. coli ATCC25922 and S. aureus ATCC29213 were grown o/n on nutrient Luria Bertani (LB) agar. Due to 20 min doubling time of E. coli in favorable conditions48 and 20 min doubling time for S. aureus49 o/n incubation is sufficient to assess bacterial growth. Isolated colonies were harvested and resuspended in LB broth adjusting the volume to reach OD600 of 0.1, corresponding to 1.5 × 108 CFU/ml. Stock solution was diluted to produce a final concentration of 1.5 × 105 CFU/ml and a working concentration of 1.5 × 104 CFU/ml.
Antimicrobial efficacy of AMPs in combination with implant materials
The antimicrobial efficacy of SET-M33 in combination with implantable materials was assessed adapting the AATCC TM100:2019 protocol (Fig. 1c). Two isomeric forms of the SET-M33 peptide, SET-M33L and SET-M33D, are available. Whilst their molecular weight and steric hindrance are identical (MW: 5857 g/mol), their specific efficacy is strain-dependent25. Both isomers exhibited comparable efficacy against E. coli with a minimum inhibitory concentration (MIC) of 3 µM. However, the D isomer demonstrated superior efficacy against S. aureus, with lower MIC to 1.5 µM25. Therefore, the L-isomer was used in the tests against E. coli, whereas the D-isomer was adopted against S. aureus.
For efficacy experiments, implant materials and membranes materials samples were first immersed for 1 h at RT (for BC overnight) in a SET-M33 solution in PBS at concentration of 3 µM, 5 µM, 10 µM, 15 µM. They were then collected from the solution, rinsed in PBS and placed in a Petri dish where 2 ml of PBS were added around the sample to ensure a moist environment. Bacterial suspensions (E. coli or S. aureus) were added on top of the samples, dropwise in a five dice arrangement. The inoculation volume (i.e. 100 µl for permeable materials and 50 µl for non-permeable materials with 1,5 × 105 CFU/ml) was chosen to ensure a uniform distribution of the bacteria given the difference in surface area. A negative control (equivalent sample immersed in PBS) and a positive control (equivalent sample immersed for 1 h in a 60 µg/ml rifampin solution) were tested together with AMP treated samples. Samples were incubated at 37 °C in a humidified environment o/n. Controls and test samples, along with the residual preconditioning fluid, were then harvested, moved into a 15 mL tube containing 10 mL PBS and vortexed for 5 min. The bacteria in the solution were enumerated via serial dilution and plating on nutrient LB agar.
Bacterial colony data quantification and statistical analysis
For quantification of bacteria, the average Log10 CFU/ml were reported as mean ± standard deviation (SD) from three independent experiments. In Figs. 4 and 5 the histogram bin represents the mean across the replicates of the experiment, while the error bars refer to standard deviation across the same replicates. Statistical analyses were performed using Prism 9.0 (GraphPad Software Inc., San Diego, CA, USA) and one-way ANOVA test was used to assess statistical differences between the Log10 CFU/ml recovery data from negative control and test items. Difference was considered statistically significant at p < 0.0001. The test outcome was considered significant if the reduction factor between non-treated and treated samples was ≥ Log4.
Data availability
All data generated and analyzed during the current study are available from the corresponding author on a reasonable request.
References
Arciola, C. R., Campoccia, D. & Montanaro, L. Implant infections: Adhesion, biofilm formation and immune evasion. Nature Reviews Microbiology vol. 16 397–409 Preprint at (2018). https://doi.org/10.1038/s41579-018-0019-y
Gutiérrez-Carretero, E. et al. Mortality and Costs of Cardiac Implantable Electronic Device (CIED) Infections According to the Therapeutic Approach: A Single-Center Cohort Study. Microorganisms 12, (2024).
Boriani, G. et al. Economic evaluation Cost-Effectiveness analyses of an absorbable antibacterial envelope for use in patients at increased risk of cardiac implantable electronic device infection in Germany, Italy, and England. https://doi.org/10.1016/j.jval.202
Callahan, T. D., Tarakji, K. G. & Wilkoff, B. L. Antibiotic eluting envelopes: Evidence, technology, and defining high-risk populations. Europace 23, IV28–IV32 (2021).
Bottan, S. et al. Surface-structured bacterial cellulose with guided assembly-based biolithography (GAB). ACS Nano. 9, 206–219 (2015).
Robotti, F. et al. A micron-scale surface topography design reducing cell adhesion to implanted materials. Sci. Rep. 8, (2018).
Zhao, M. H., Chen, X. P. & Wang, Q. Wetting failure of hydrophilic surfaces promoted by surface roughness. Sci. Rep. 4, (2014).
Zhang, S. et al. Enhanced anti-biofilm and anti-protein adsorption properties of liquid-infused silver-polytetrafluoroethylene coatings. Appl. Surf. Sci. 616, (2023).
Sun, L. et al. Tailoring Materials with Specific Wettability in Biomedical Engineering. Advanced Science vol. 8 Preprint at (2021). https://doi.org/10.1002/advs.202100126
Lord, M. S., Foss, M. & Besenbacher, F. Influence of nanoscale surface topography on protein adsorption and cellular response. Nano Today vol. 5 66–78 Preprint at (2010). https://doi.org/10.1016/j.nantod.2010.01.001
Kim, T., Kwon, S., Lee, J., Lee, J. S. & Kang, S. A metallic anti-biofouling surface with a hierarchical topography containing nanostructures on curved micro-riblets. Microsyst. Nanoeng 8, (2022).
Hsieh, P. C. & Chien, H. W. Biomimetic surfaces: insights on the role of surface topography and wetting properties in bacterial attachment and biofilm formation. Colloids Surf. B Biointerfaces 228, (2023).
Blomströ, M. et al. Jean-Claude Deharo 11. Eur. Heart J. 12, 2012–2032 (2020).
Mittal, S. et al. The World-wide randomized antibiotic envelope infection prevention (WRAP-IT) trial: Long-term follow-up. Heart Rhythm. 17, 1115–1122 (2020).
Mancuso, G., Midiri, A., Gerace, E. & Biondo, C. Bacterial antibiotic resistance: the most critical pathogens. Pathogens vol. 10 Preprint at (2021). https://doi.org/10.3390/pathogens10101310
Hussein, A. A. et al. Microbiol. Cardiac Implantable Electron. Device Infections (2016).
Brogden, K. A. Antimicrobial peptides: Pore formers or metabolic inhibitors in bacteria? Nature Reviews Microbiology vol. 3 238–250 Preprint at (2005). https://doi.org/10.1038/nrmicro1098
Hodges, R. S., Jiang, Z., Whitehurst, J. & Mant, C. T. DEVELOPMENT OF ANTIMICROBIAL PEPTIDES AS THERAPEUTIC AGENTS. (2010). http://www.cdc.gov/drugresistance/community/files/ads/
Cresti, L. et al. Inhalable Polymeric Nanoparticles for Pulmonary Delivery of Antimicrobial Peptide SET-M33: Antibacterial Activity and Toxicity In Vitro and In Vivo. Pharmaceutics 15, (2023).
Falciani, C. et al. Molecular basis of branched peptides resistance to enzyme proteolysis. Chem. Biol. Drug Des. 69, 216–221 (2007).
Thwaite, J. E., Hibbs, S., Titball, R. W. & Atkins, T. P. Proteolytic degradation of human antimicrobial peptide LL-37 by Bacillus anthracis May contribute to virulence. Antimicrob. Agents Chemother. 50, 2316–2322 (2006).
Brunetti, J. et al. Antibacterial and anti-inflammatory activity of an antimicrobial peptide synthesized with D amino acids. Antibiotics 9, 1–17 (2020).
Castiglia, F. et al. NMR study of the secondary structure and biopharmaceutical formulation of an active branched antimicrobial peptide. Molecules 24, (2019).
van der Weide, H. et al. Antimicrobial activity of two novel antimicrobial peptides AA139 and SET-M33 against clinically and genotypically diverse Klebsiella pneumoniae isolates with differing antibiotic resistance profiles. Int. J. Antimicrob. Agents. 54, 159–166 (2019).
Falciani, C. et al. Isomerization of an antimicrobial peptide broadens antimicrobial spectrum to Gram-Positive bacterial pathogens. PLoS One 7, (2012).
van der Weide, H. et al. Investigations into the killing activity of an antimicrobial peptide active against extensively antibiotic-resistant K. pneumon Iae and P. aeruginosa. Biochim. Biophys. Acta Biomembr. 1859, 1796–1804 (2017).
Bazaka, K., Jacob, M. V., Chrzanowski, W. & Ostrikov, K. Anti-bacterial surfaces: Natural agents, mechanisms of action, and plasma surface modification. RSC Adv. 5, 48739–48759 (2015).
Negut, I., Bita, B. & Groza, A. Polymeric Coatings and Antimicrobial Peptides as Efficient Systems for Treating Implantable Medical Devices Associated-Infections. Polymers vol. 14 Preprint at (2022). https://doi.org/10.3390/polym14081611
Robotti, F. et al. Microengineered biosynthesized cellulose as anti-fibrotic in vivo protection for cardiac implantable electronic devices. Biomaterials 229, (2020).
Duan, Y., Kalluri, L., Satpathy, M. & Duan, Y. Effect of electrospinning parameters on the Fiber diameter and morphology of PLGA nanofibers. Dent. Oral Biology Craniofac. Res. https://doi.org/10.31487/j.dobcr.2021.02.04 (2021).
Love, C. J. et al. Preclinical evaluation of a third-generation absorbable antibacterial envelope. Heart Rhythm. 20, 737–743 (2023).
Albano, M., Greenwood-Quaintance, K. E., Karau, M. J., Mandrekar, J. N. & Patel, R. Anti-biofilm activity of antibiotic-loaded Hylomate®. IJC Heart Vasculature 34, (2021).
Huntingdon Life Sciences. Study TR-2013-001, data on file withMedtronic, plc.
Gong, Y., Xu, J. & Buchanan, R. C. Surface roughness: A review of its measurement at micro-/nano-scale. Physical Sciences Reviews vol. 3 Preprint at (2019). https://doi.org/10.1515/psr-2017-0057
Lahiri, D. et al. Bacterial cellulose: Production, characterization and application as antimicrobial agent. International Journal of Molecular Sciences vol. 22 Preprint at (2021). https://doi.org/10.3390/ijms222312984
Chen, Y., Wang, J. & Flanagan, D. R. Fundamental of diffusion and dissolution. in Developing Solid Oral Dosage Forms: Pharmaceutical Theory and Practice: Second Edition 253–270Elsevier Inc., (2017). https://doi.org/10.1016/B978-0-12-802447-8.00009-1
Diffusion in Condensed Matter.
Meogrossi, G. et al. Antibacterial and Anti-Inflammatory activity of branched peptides derived from natural host defense sequences. J. Med. Chem. https://doi.org/10.1021/acs.jmedchem.4c00810 (2024).
Pick, N., Cameron, S., Arad, D. & Av-Gay, Y. Screening of compounds toxicity against human monocytic cell line-THP-1 by flow cytometry. Biol. Proced. Online. 6, 220–225 (2004).
Borov, S. et al. Use of a taurolidine containing antimicrobial wash to reduce cardiac implantable electronic device infection. Europace 25, (2023).
Moore, K. et al. Mapping Bacterial Biofilm on Features of Orthopedic Implants In Vitro. Microorganisms 10, (2022).
Krahn, A. D. et al. Prevention of arrhythmia device infection trial: The PADIT trial. J. Am. Coll. Cardiol. 72, 3098–3109 (2018).
Messori, A. Real-world data on the effectiveness of TYRX and TauroPace for preventing CIED infections. Am. J. Cardiovasc. Dis. 14, 220–229 (2024).
Surface hydrolysis of. poly(glycolic acid) meshes increases the seeding density of vascular smooth muscle cells. Journal of Biomedical Materials Research, 42(3), 417–424
Makadia, H. K. & Siegel, S. J. Poly Lactic-co-Glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polym. (Basel). 3, 1377–1397 (2011).
Yoon, S. K. & Chung, D. J. In vivo degradation studies of PGA-PLA block copolymer and their histochemical analysis for Spinal-Fixing application. Polym. 2022. 14, 3322 (2022).
Widdel, F. Theory and Measurement of Bacterial Growth A. Basic and Practical Aspects. (2007).
Missiakas, D. M. & Schneewind, O. Growth and laboratory maintenance of Staphylococcus aureus. Curr. Protoc. Microbiol. https://doi.org/10.1002/9780471729259.mc09c01s28 (2013).
Editor, R. T. CURRENT TOPICS IN MICROBIOLOGY AND IMMUNOLOGY.
Iyer, D., Laws, E. & LaJeunesse, D. Escherichia coli adhesion and biofilm formation on polymeric nanostructured surfaces. ACS Omega. 8, 47520–47529 (2023).
Acknowledgements
This work was supported by a Horizon Europe MSCA DN-ID grant (grant number 101073263).
Author information
Authors and Affiliations
Contributions
A.M., S.M., A.F., W.U. and C.F. conceptualized the idea, designed the experiments, and wrote the main manuscript.A.M. conducted all the experiments, with S.M. contributing to the experiments in Figs. 5 and 6 and citotoxicity experiments. Together, they analyzed the data and prepared the figures.I.C. synthesized the antimicrobial compounds and its derivatives.F.G.F and L.M. engineered and provided bioluminescent E.coli strain.A.M., A.F, S.M, F.G, L.M.,W.U., C.F., A.P. reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
Biocellulose membrane is covered by a patent owned by Hylomorph. The peptide SET-M33 is covered by a patent owned by the University of Siena and licensed to SetLance srl. Chiara Falciani, and Alessandro Pini are partners of SetLance. The rest of the authors declare that they have no other competing financial interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maranesi, A., Mohammadi, S., Castañon, I. et al. The identity of implant materials governs the antimicrobial efficacy of SET-M33. Sci Rep 15, 16353 (2025). https://doi.org/10.1038/s41598-025-99808-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99808-w