Abstract
Blood clots (BCs) play a crucial biomechanical role in promoting osteogenesis and regulating mesenchymal stem cell (MSC) function and fate. This study shows that BC formation enhances MSC osteogenesis by activating Itgb1/Fak-mediated focal adhesion and subsequent Runx2-mediated bone regeneration. Notably, BC viscoelasticity regulates this effect by modulating Runx2 nuclear translocation. To mimic this property, a viscoelastic peptide bionic hydrogel named BCgel was developed, featuring a nanofiber network, Itgb1 binding affinity, BC-like viscoelasticity, and biosafety. The anticipated efficacy of BCgel is demonstrated by its ability to induce nuclear translocation of Runx2 and promote bone regeneration in both in vitro experiments and in vivo bone defect models with blood clot defect, conducted on rats as well as beagles. This study offers insights into the mechano-transduction mechanisms of MSCs during osteogenesis and presents potential guidelines for the design of viscoelastic hydrogels in bone regenerative medicine.
Similar content being viewed by others
Introduction
The human body houses an impressive assortment of over 200 bones, each possessing its own distinct morphology, size, and function1. These remarkable skeletal structures not only provide essential structural support but also facilitate elegant movement and agile locomotion1. Consequently, bone is known as the most abundant and enduring tissue within the human body, with any diminishment of these vital tissues posing a significant threat to patients’ overall quality of life2. Fortunately, bone possesses remarkable regenerative capabilities that enable healing without compromising its integrity or functionality, and an expanding body of research is now uncovering the biomechanical influence of blood clot formation on bone healing3,4. The primary and pivotal stage after sustaining a bone injury entails the creation of a blood clot (BC), serving both as an essential safeguard against excessive bleeding and as a natural framework for facilitating bone repair and regeneration through the orchestration of subsequent remodeling procedures5,6. Fibrin, an irreplaceable constituent forming an elaborated meshwork comprised of minuscule fibers, fulfills these fundamental roles within the blood clot7. Notably, this intricate structure not only attracts immune cells and mesenchymal stem cells (MSCs), but also demonstrates distinctive viscoelastic characteristics defined by its mechanical reaction to varying rates of loading over different durations8,9. The current focus is increasingly directed towards comprehending the biomechanical role played by bone cells in the process of bone healing, particularly with regards to their ability to reprogram MSCs for osteogenesis7,10, thereby offering a novel mechanically induced strategy for bone repair that can complement other biochemical tissue engineering technologies.
To achieve this goal, two crucial steps must be taken: firstly, uncovering the underlying biomechanical mechanism by which MSCs respond to mechanical stimuli from BC or fibrin; secondly, devising translational bionic strategies for bone repair based on this mechanism. The former refers to the fact that an increasing number of mechanical sensory pathways have been identified in stem cells, such as the Integrin-Fak pathway, RhoX-Rock pathway, and Piezo1 pathway, which are responsible for converting extracellular stress into intracellular kinase activity, cytoskeletal remodeling, and changes in intracellular ion concentration respectively; however, the missing key downstream linker that mediates mechano-sensitivity to convert these mechanochemical coupling signals into osteogenic programming remains unidentified11,12,13,14. As for the latter step, despite numerous successes achieved in creating functional bone substitutes using BC analogues and tissue-engineered biomimetic scaffolds/hydrogels7,15,16,17,18, it still poses a challenge to fully remodel the mechanical environment and induce similar biological behavior of MSCs as observed with BC.
In this work, to address the burgeoning interest in comprehending the intricate biomechanical mechanism underlying bone healing facilitated by fibrin/BC, a model of blood clot defect (BCD) was established through induction of maxillary tooth extraction injury in hypertensive rats with systolic blood pressure (SBP) and diastolic blood pressure (DBP) equal to or surpassing 150/120 mmHg. Comparative analysis of single-cell RNA sequencing (scRNA-seq) data acquired from maxillary bone tissue surrounding the extraction sockets in BCD and Ctrl rats revealed that blood clot formation promotes primary-stage osteogenesis by augmenting Itgb1/Fak-mediated focal adhesion signaling, thereby ensuring a normal and seamless progression of late-stage osteogenesis. Significantly, further research unveiled that Runx2, the transcription factor governing osteogenesis, exhibits viscoelasticity-sensitivity in an Itgb1-dependent manner, thus elucidating the intricate biomechanical mechanism underlying fibrin/BC-mediated bone healing. By employing this approach, a viscoelastic adjustable BC-biomimetic hydrogel named BCgel was fabricated in the present investigation. It possesses an identical nanofiber network microstructure as fibrin, exhibits equivalent binding affinity to Itgb1 as fibrin, and endows a viscoelastic characteristic akin to that of fibrin hydrogel for optimal promotion of bone regeneration. Consequently, this BCgel exhibits remarkable bioactivity by inducing nuclear translocation of Runx2 and promoting bone regeneration both in vitro and in rat as well as beagle bone defect models with blood clot defect. The BCgel derived from peptides exhibits exceptional biocompatibility, particularly with minimal immunotoxicity - a concern commonly associated with fibrin-derived hydrogels. The collective effort presented in this study not only reveals a mechanism of mechanically induced signaling in MSC osteogenic reprogramming (which likely operates alongside other biochemical-mediated osteogenesis signaling), but also introduces an innovative strategy for educating MSCs on osteogenic programming through mechanical stimulation.
Results
The formation of new bone heavily relies on the crucial involvement of blood clots
To investigate the correlation between osteogenesis and blood clots, a comprehensive Meta-analysis was conducted on 312 articles sourced from the web of science using specific keywords related to osteogenesis and blood clots. Out of these articles, only 5 addressed this particular relationship (I2 = 89%, τ2 = 95.4633), encompassing a total of 46 animal research samples. The Meta results depicted in Fig. 1A and Supplementary Table 1 demonstrate a statistically significant (p < 0.01) decrease of 15.78% in newly formed bone volume in cases where physical blood clots were absent, as compared to cases with complete blood clot formation, suggesting the indispensable involvement of blood clots in osteogenesis. By causing maxillary tooth extraction injury in hypertensive rats with systolic and diastolic blood pressures exceeding 150/120 mmHg, blood clot defect (BCD) model was established to provide further evidence (Supplementary Fig. 1A). The rat’s right incisors were extracted by complete removal from the roots to create a meticulously crafted C-shaped wound of tooth extraction (Supplementary Fig. 1B). In the presence of hypertension, elevated bleeding velocity due to high blood pressure tends to result in increased bleeding volume and prolonged bleeding time, leading to partial impairments in blood clot formation19,20. According to this theory, hypertensive rats exhibited a 47% longer blood clotting time and a 137% increase in blood loss compared to the control group of healthy rats (Ctrl) (Fig. 1B), while both groups showed similar static clotting ability (Supplementary Fig. 1C). Furthermore, histological examination of blood clots using fibrin staining consistently demonstrated the formation of complete blood clots within the extraction socket after tooth removal in healthy rats (Fig. 1C). Conversely, in hypertensive rats, the blood clot size was reduced by 41%, 37%, 30%, and 43% at 3 h, 6 h, 24 h, and one week post tooth extraction respectively (Fig. 1C, D). The above data demonstrate the successful establishment of a bone defect models with blood clot defect (BCD) in hypertensive rats through tooth extraction injury.
A Meta analysis using specific keywords related to osteogenesis and blood clots. B Comparison of coagulation time and blood loss after tooth extraction in Ctrl and BCD group (rats). (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). C, D Fibrin staining and quantification D of blood clot at 3 h, 6 h, 24 h, and one week post tooth extraction. (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test, p < 0.0001). E Masson’s trichrome and VG staining of extraction region from Ctrl and BCD group at 1 week post tooth extraction. F Micro-CT analysis of extraction region from Ctrl and BCD group. G The quantification of Micro-CT analysis, including bone mineral density (BMD), bone volume to total volume (BV/TV), trabecular number (Tb.N), trabecular thickness (Tb.Th), and trabecular separation (Tb.Sp). (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). H, I Immunofluorescent staining and quantification (I) of Runx2 and Alp. (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). J, K The immunofluorescent staining of CD73 and CD105 was analyzed using a Confocal Laser Scanning Microscope (CLSM), and the quantification of double positive signals is presented in (K). (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test).
Next, the bone regeneration capacity was comparatively explored between the BCD and Ctrl groups at one week post tooth extraction. Both groups showed new bone formation in the extraction socket according to Masson’s trichrome, VG (Fig. 1E), and H&E staining (Supplementary Fig. 1D). Importantly, quantification of new bone by micro-CT showed that the BCD group exhibited a 29% decrease in bone mineral density (BMD), a 48% decrease in the ratio of bone volume to total volume (BV/TV), a 49% decrease in the number of bone trabeculae (Tb.N), a 51% decrease in trabecular thickness (Tb.Th), and a 71% increase in trabecular separation (Tb.Sp) compared with the Ctrl group (Fig. 1F, G). Further mechanistic research on the immunofluorescent staining of Runx2 and Alp, two key osteogenesis proteins, revealed a statistically significant reduction in the BCD group (Fig. 1H, I, p < 0.0001). Consistent with these findings, there was a statistically significant decrease in the expression of MSC markers CD73 and CD105 within the extraction socket of BCD at 1 week (Fig. 1J, K, p < 0.0001). Additionally, in order to further investigate the recruitment of MSCs after extraction, we also examined the expression of MSC markers CD73 and CD105 in the extraction socket at 1 day and 3 days post-extraction. We observed that there was a higher presence of MSCs in the BCD group at 1 day (Supplementary Fig. 1E, F), but a lower presence at 3 days compared to the control group (Supplementary Fig. 1G, H). This suggests that there is an increased recruitment of MSCs during the initial stages of injury in the BCD group, but their viability and differentiation potential may be compromised. Collectively, these results demonstrate the crucial role played by blood clots in new bone formation.
It is noteworthy that there was minimal difference observed in both leukocyte and granulocyte counts between hypertensive rats and their non-hypertensive counterparts (Supplementary Fig. 1I). Additionally, there was no observed elevation in thrombocytes or erythrocytes in hypertensive rats (Supplementary Fig. 1I), suggesting the absence of heightened infection or inflammation in hypertensive rats with inhibitory osteogenesis. Furthermore, the bone mass in hypertensive rats with systolic and diastolic blood pressures exceeding 150/120 mmHg showed negligible disparity compared to their non-hypertensive counterparts (Supplementary Fig. 1J). These findings suggest that hypertension-induced bone dysplasia is unlikely to be attributed to factors other than hypertension-derived BCD.
The formation of blood clots promotes osteogenesis by enhancing Integrin-mediated focal adhesion signaling in MSCs
Subsequently, scRNA-seq analysis was employed to elucidate the cellular and molecular characteristics of cells within the extraction socket and surrounding bone tissue (marked by a red box in Supplementary Fig. 1A) in both the experimental group (BCD) and the control group at 24 hours after tooth extraction. The reason for selecting this specific time point for scRNA-seq analysis is due to its suitability in capturing the inflammatory response, during which inflammatory factors often recruit a significant number of MSCs, enabling us to investigate the osteoblast differentiation potential of MSCs21,22. In Fig. 2A, B of the single-cell expression atlas (n = 3/group), a remarkable diversity of immune cells, including four distinct types (B lymphocytes, granulocytes, mononuclear phagocytes, and T lymphocytes), along with four populations of histocytes (basal cells, endothelial cells, neurons, and osteogenic cells), were identified within the two contrasting socket regions and their surrounding tissues. Upon analyzing the neuron clusters, it is worth noting that all five genes exhibiting high expression in specific neurons (as indicated in Supplementary Table 2) are associated with sensory neurons. Therefore, these neuron clusters are most likely to represent the maxillofacial sensory nerves. The temporal dynamics of four genes—CD73, CD105, Alpl, and Ocn—during osteogenesis were further analyzed quasi-temporally, resulting in the identification of four distinct yet continuous sub-clusters: MSCs, osteoprogenitor cells, pre-osteoblasts, and osteoblasts (Fig. 2C, D). These four sub-clusters appeared sequentially throughout the process of osteogenesis in theory. The BCD group demonstrated a significant increase in the proportion of MSC and osteoprogenitor cells, as well as a significant decrease in the proportion of pre-osteoblasts and osteoblasts compared to the Ctrl group, indicating an arrest in osteogenic differentiation of poorly differentiated cells. These findings were further supported by the expression levels of four key genes involved in osteogenesis, namely Alpl, Runx2, Ocn, and Col1a1. Notably, there was a potent inhibition of gene expression observed in both pre-osteoblasts and osteoblasts within the BCD groups (Fig. 2E). Furthermore, a comparative single cell Gene Set Enrichment Analysis (sc-GSEA) was conducted on the four sub-clusters to identify the specific signaling pathways between BCD and Ctrl groups. In terms of the signaling pathways associated with osteogenesis in MSCs, we observed four statistically significant (p < 0.05) down-regulations related to Integrin-mediated focal adhesion in BCD compared to Ctrl, including Integrin cell surface interactions, focal adhesion, Integrin binding, and focal adhesion assembly (Fig. 2F). Additionally, signaling and adhesion mediated by Integrin were also down-regulated in osteoprogenitor cells (Fig. 2G). In addition, the two most significantly down-regulated pathways in pre-osteoblasts were the pathway of Runx2 expression and activity, as well as the pathway of transcription regulation by Runx2 (Fig. 2H). Moreover, the two most significantly down-regulated pathways in osteoblasts were found to be related to the organogenesis and development of osteoblasts (Fig. 2I). All these findings suggest that blood clot formation promotes primary-stage osteogenesis by enhancing Integrin-mediated focal adhesion signaling in MSCs, thereby ensuring the normal and seamless progression of late-stage osteogenesis.
A t-Distributed Stochastic Neighbor Embedding (t-SNE) plots of broad cell types within the socket and surrounding tissue in both the Ctrl and BCD groups at 24 h post tooth extraction. (n = 3 independent replicates). B The signature gene expression in each cluster served as the criterion for clustering. C The osteogenic cells were further classified into four sub-clusters based on the dynamic changes of four genes, namely CD73, CD105, Alpl, and Ocn. D The proportion of the sub-cluster within osteogenic cells in quasi-temporal analysis. (n = 3 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test, ***p < 0.001). E The expressions of osteogenic-related genes in the Ctrl group and BCD group. (n = 3 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). F–I A comparative single-cell Gene Set Enrichment Analysis (sc-GSEA) were conducted on the four sub-clusters to identify the specific signaling pathways between Ctrl and BCD groups. The GSEA p-value represents the estimation of significance. We evaluate the significance of an observed Enrichment Score (ES) by comparing it to a distribution of ESNULL scores derived from randomly assigned phenotypes.
Blood clots facilitate osteogenesis by activating mechanical Integrin-mediated focal adhesion signaling and the subsequent force-sensitive transcription factor Runx2
To further demonstrate the promotion of osteogenesis through enhanced Integrin-mediated focal adhesion signaling at the protein level, two crucial proteins - Fak and Itgb1 - in this pathway were semi-quantified within the socket for both BCD and Ctrl groups. Remarkably, a significant reduction of 77% in Fak levels and 83% decrease in Itgb1 levels were observed specifically within the BCD group (Fig. 3A). Additionally, immunofluorescence analysis involving co-staining of CD73 (a marker for MSCs) and Fak revealed a significant 83% reduction in the population of double positive cells within the BCD groups (Supplementary Fig. 2A & B). Furthermore, immunofluorescence analysis involving co-staining of CD73 and Itgb1 demonstrated a remarkable 74% decrease in the population of double positive cells within the BCD groups (Supplementary Fig. 2C & D), indicating a substantial suppression of Integrin-Fak focal adhesion signaling in MSCs. The obtained results have compelled us to propose a hypothesis that fibrin, the crucial component of blood clots, facilitates osteogenesis by activating mechanical Integrin-mediated focal adhesion signaling and subsequently triggering the force-sensitive transcription factor Runx2 in MSCs (Fig. 3B).
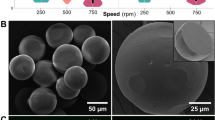
A Immunohistochemical staining and quantification of Fak and Itgb1 were performed on samples obtained from the Ctrl and BCD groups at 1 week post tooth extraction. (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). B Schematic diagram of mechanical Integrin-mediated focal adhesion signaling and its impact on osteogenesis in MSCs. C SEM images of fibrin and MSCs morphology. D–G Immunofluorescent staining of Fak&Itga5 (D) and Fak&Itgb1 (F) in MSCs incubated with or without fibrin for 24 h was analyzed by CLSM. Double positive signals were quantified by Image J with colocalization factor (Pearson’s R value) (E&G). (n = 6 independent replicates, 10 counts per sample, means ± SD, p value calculated by two-tailed Student’s t test). H The quantification of western blotting analysis of Itga5, Itgb1, Fak, active Rhoa (ARhoa), Rock2 and c-Jun in MSCs incubated with or without 0.5% fibrin for 24 h. (n = 3 independent replicates, means ± SD). I Immunofluorescent staining of Runx2 was performed on MSCs incubated with varying concentrations of fibrin for a duration of 24 h. J Quantitative analysis of Runx2 localization in the nucleus and karyoplasm based on fluorescence intensity. (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test, ****p < 0.0001). K Runx2 expression in the nucleus and cytoplasm of MSCs incubated with different concentrations of fibrin were measured by western blotting analysis. (n = 3 independent replicates). L, M MSCs with or without Itgb1 knockdown were incubated with 0.5% fibrin for 24 h. Runx2 expressions were detected through immunofluorescence staining (L) and subsequent quantification (M). (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). N Runx2 expressions were also analyzed by western blotting. (n = 3 independent replicates).
To investigate this hypothesis and explore the underlying mechanisms, fibrin was utilized for the treatment of rat femur-derived bone marrow mesenchymal stem cells (MSCs). It is worth noting that concentrations of 0.1%, 0.2%, 0.5% and 1% fibrin had negligible effects on cell viability (Supplementary Fig. 2E), while at a concentration of 0.5%, fibrin did not induce cell cycle arrest or apoptosis in MSCs (Supplementary Fig. 2F). Of note, the typical concentration of fibrinogen in blood ranges from 0.2% to 0.5%, with the concentrations used in this study varying from 0.1% to 1%, which aligns with established physiological standards23,24. Furthermore, the cavity structure present in 0.5% fibrin (Supplementary Fig. 2G) exhibited biocompatibility with MSCs; allowing them to adhere to its surface and extend tentacles into its holes (Fig. 3C). Importantly, following 24-hour incubation with 0.5% fibrin, there was a significant increase in Fak/Itga5 double positive signaling compared to mock-treated cells (Fig. 3D), accompanied by a 99% increase in Fak-Itga5 focal adhesion (Fig. 3E). Similar results were observed for co-staining of Fak/Itgb1 (Fig. 3F), with a corresponding 485% increase in Fak-Itgb1 focal adhesion upon fibrin incubation (Fig. 3G). Consistent with these findings, exposure to fibrin led to over 40% upregulation of proteins involved in the Integrin-Fak focal adhesion signaling pathway, including Itga5, Itgb1, Fak, active Rhoa (ARhoa), Rock2 and c-Jun (Fig. 3H and Supplementary Fig. 2H). The data presented herein suggest that fibrin possesses the capability to augment mechanical Integrin-Fak focal adhesion signaling. Notably, these findings also indicate that Itgb1 plays a more prominent role in activating this signaling pathway compared to Itga5, as further substantiated by the significantly greater inhibition of this pathway observed with si-Itgb1 than with si-Itga5 (Supplementary Fig. 2I).
Due to the force sensitivity of Integrin-Fak focal adhesion signaling, we hypothesize that fibrin with varying mechanical properties would elicit distinct responses through this pathway. As depicted in Supplementary Fig. 2J, modulating the fibrin concentration from 0.1% to 1% results in a continuous variation of G’ storage modulus from 925 to 5648 pa and G” loss modulus from 54.9 to 569 pa at the low-frequency rotation less than 4 Hz. As anticipated, the utilization of distinct viscoelastic fibrin formulations resulted in varying nuclear transposition ratios of Runx2 as evidence by the CLSM images (Fig. 3I and Supplementary Fig. 2K), with 0.5% fibrin demonstrating the most favorable response to Runx2 nuclear transposition (Fig. 3J). The findings were further supported by the Western blot image and its semi-quantitative analysis of nuclear and cytoplasmic Runx2 (Fig. 3K and Supplementary Fig. 2L). Theoretically, the nuclear translocation of Runx2 enhances its function as a transcription factor, thereby promoting not only the expression of its downstream genes but also its own expression25,26,27,28. The nuclear transposition of Runx2 additionally resulted in an upregulation of transcription (Supplementary Fig. 2M) and subsequent elevation of Runx2 mRNA levels (Supplementary Fig. 2N), indicating the activation of the Runx2 signaling pathway. Furthermore, a series of fibrin clots with varying parameters such as fibrin diameters, fiber densities, porosity levels, and pore sizes were synthesized by adjusting the concentration and thrombin (TB) dosage (Supplementary Fig. 2O and Supplementary Table 3). The viscoelasticity of the fibrin remained consistent, leading to equivalent degrees of Runx2 activation, despite variations in porosity levels, pore sizes, fibrin diameter, and fiber density (Supplementary Fig. 2P, Q and Supplementary Table 3). Conversely, when the porosity remained constant while varying in viscoelasticity, distinct levels of Runx2 activation were observed (Supplementary Fig. 2Q and Supplementary Table 3). These findings suggest that the activation of Runx2 is contingent upon viscoelastic properties rather than porosity-dependent factors.
Furthermore, it was observed that this process of Fibrin-derived Runx2 nuclear transposition was significantly impeded in Itgb1-knock-down (Itgb1KD) MSCs, where the expression of Itgb1 was stably suppressed through Lentivirus-encased shRNA (Fig. 3L–N and Supplementary Fig. 3A). These findings strongly indicate a reliance on Itgb1 for fibrin-mediated Runx2 nuclear translocation. Meanwhile, the knockdown of Itgb1 resulted in the suppression of Runx2 nuclear translocation and concomitantly led to the transactivation of Runx2 (Supplementary Fig. 3B), indicating its dependence on Runx2 translocation. To further confirm the dependence of Runx2 translocation, we knocked down Ipo8, the nuclear transporter for Runx2, which not only restricted its nuclear translocation but also led to a decrease in the transactivation of its downstream protein Alp (Supplementary Fig. 3C, D). Moreover, the nuclear accumulation of Runx2 resulted in the up-regulation Alp (Supplementary Fig. 3E, F), subsequently promoting osteogenic differentiation of MSCs, as evidenced by the elevated activity of ALP (Supplementary Fig. 3G–I) and enhanced ARS staining (Supplementary Fig. 3J, K). The process of osteogenic differentiation was significantly suppressed in Itgb1-knockdown MSCs (Supplementary Fig. 3L), while it was enhanced by the over-expression of Runx2 (Supplementary Fig. 3M). The collective action of fibrin promotes osteogenesis by activating mechanical Integrin-mediated focal adhesion signaling and subsequent force-sensitive nuclear translocation of Runx2 in an Itgb1-dependent manner, indicating the osteogenesis function of blood clots.
The design and fabrication of the blood clot bionic gel (BCgel)
The interaction topological structure between Itgb1 and fibrin was analyzed using αFold 2.0 to further investigate the Itgb1-dependent manner of fibrin’s biofunction. As anticipated, the N-terminal of fibrin contained an RGD motif that could bind with Itgb1 (Fig. 4A). The binding interface covered an area of 431.4 Å2 and exhibited a Gibbs free energy of -2.0 Kcal/mol (Fig. 4B), indicating a strong affinity between the two molecules. A fluorescence polarization (FP) analysis was performed using FITC-labeled fibrin mixed with isodiluted Itgb1 to quantify the binding between Itgb1 and fibrin. The resulting fluorescence polarization was measured and fitted using the standard formula for protein-ligand binding29,30. This analysis revealed a binding affinity of 29.8 nM between Itgb1 and fibrin (Fig. 4C), providing strong evidence that the biofunction of fibrin is achieved through its tight interaction with Itgb1. The discovery has inspired us to develop a bionics hydrogel that can simulate the biochemical and biomechanical microenvironment of fibrin, aiming to address the recurrent bone regeneration disorder caused by mechanical bone clot defects.
A The 3D structure of the interaction between Itgb1 and fibrin, as predicted by Alpha Fold. B The binding interface and Gibbs free energy of the two interactions: Itgb1 and fibrin (upper panel); Itgb1 and BCgel monomer (lower panel). C The binding between Itgb1 and fibrin/BCgel monomer was quantified by performing Fluorescence Polarization (FP) analysis using FITC-labeled fibrin or BCgel monomer mixed with isodiluted Itgb1. (n = 3 independent replicates, means ± SD). D The synthetic BCgel monomer was identified through LC-MS analysis. E The G’ storage modulus and G” loss modulus of BCgel were measured at various concentrations using a rotational rheometer with low-frequency rotation below 4 Hz. F Schematic diagram illustrating a high throughput screening system for determining the optimal proportion of BCgel monomer and Ca2+ ions through measurement of Alp activity. G, H The heat map (G) and curve graph (H) depict the Alp activity results obtained from screening using the (F) method. (n = 3 independent replicates, means ± SD). I Photos of the BCgel with 1.5% or 3% monomer concentration and 0.1 mg/mL Ca2+ ions. J Contact angle measurement of BCgel with 3% monomer concentration and 0.1 mg/mL Ca2+ ions. K The G’ storage modulus and G” loss modulus of BCgel were measured using a rotational rheometer. L SEM and TEM image of BCgel. (M&N) CLSM analysis (M) and field emission scanning electron microscope (FESEM) analysis (N) of BCgel incubation with MSCs. (n = 3 independent replicates).
In this regard, we propose that the gelatinous peptide motif (RADA)4 can mimic the role of the RGD motif in binding with Itgb1 (Fig. 4A). The αFold result regarding the interaction between (RADA)4 and Itgb1, which exhibits an interaction area of 300.4 and a Gibbs free energy of −1.3 Kcal/mol, supports this hypothesis theoretically (Fig. 4B). To further enhance the tunability of viscoelastic properties in this hydrogel derived from (RADA)4, a calcium binding motif was incorporated into its C-terminal region (Supplementary Fig. 4A). Subsequently, we successfully synthesized the BCgel monomer peptide using solid-phase FMOC chemistry with HBTU/HOBT coupling followed by purification through reverse high-pressure liquid chromatography (HPLC). The synthesized BCgel monomer exhibited a molecular weight close to the theoretical value at 2760.15 Da and demonstrated satisfactory purity at 95.6% (Fig. 4D). Furthermore, we measured its binding affinity with Itgb1 using FP analysis and found it to be approximately 90.2 nM, which is comparable to the Kd value of fibrin (Fig. 4C).
To investigate the viscoelastic properties of BCgel, we dissolved it in deionized water at concentrations ranging from 0.5% to 4%, and measured G’ and G” using a rotational rheometer. As shown in Fig. 4E, varying the concentration of BCgel resulted in a continuous change of G’ storage modulus from 62 to 4973 pa and G” loss modulus from 14 to 607 pa at low-frequency rotation less than 4 Hz. Furthermore, the addition of Ca2+ ions expanded the range of viscoelasticity (Supplementary Fig. 4B–D). These results demonstrate that BCgel is a two-dimensional adjustable hydrogel with viscoelastic properties. To identify the optimal viscoelasticity of BCgel for promoting osteogenesis, a high throughput screening system was established to evaluate the 2D parameters related to Ca2+ concentration and BCgel monomer concentration (Fig. 4F). In this system, MSCs were mixed with different viscoelastic BCgel formulations and added into 96-well plates along with cell culture medium containing serum (Fig. 4F). After co-incubation for 24 h, the Alp activity in the culture medium was measured. The resulting heatmap and cumulative curve are shown in Fig. 4G, H respectively, indicating that a combination of 3% BCgel monomer concentration and 0.1 mg/mL Ca2+ concentration exhibited the highest Alp activity (Fig. 4H).
Under these conditions, the BCgel demonstrated injectable hydrogel properties (Fig. 4I, J) and exhibited good viscoelasticity, with a significantly higher G’ modulus compared to the G” loss modulus (Fig. 4K), indicating exceptional elastic behavior and efficient force conduction properties. Notably, the viscoelasticity of this BCgel was comparable to that of 0.5% fibrin. Moreover, at a concentration of 3% and a dosage of 0.1 mg/mL Ca2+, the BCgel displayed a spatial network structure similar to that of 0.5% fibrin (Fig. 4L). The storage modulus (G′) of the 0.5% fibrin ranged from 290 to 3470 Pa, as depicted in Supplementary Fig. 4E, while the loss modulus (G″) ranged from 10.6 to 210 Pa (Supplementary Fig. 4E). Similarly, the BCgel exhibited a storage modulus (G′) varying from 1130 to 2230 Pa, with a corresponding loss modulus (G″) ranging from 63.2 to 162 Pa (Supplementary Fig. 4E). Shear rate sweep measurements unveiled that both fibrin and BCgel displayed comparable viscosity, showcasing remarkable shear-thinning behavior (Supplementary Fig. 4E). Furthermore, step-strain experiments demonstrated the self-healing properties of both fibrin and BCgel; however, it was observed that BCgel exhibited greater resistance against an initial high strain of up to 1000% (Supplementary Fig. 4E). These findings substantiate that a gel-like elastic solid is formed by combining Ca2+ at a concentration of 0.1 mg/mL with BCgel. Furthermore, the bio-degradability of BCgel was assessed in a buffer solution containing chymotrypsin and trypsin (1 mg/mL). Remarkably, Coomassie blue-labeled BCgel exhibited a degradation half-life of 4.96 days (Supplementary Fig. 4F). Importantly, this BCgel not only inherits the biocompatibility of 0.5% fibrin, facilitating MSC adhesion and extension into its pores, but also promotes a more three-dimensional arrangement of stem cells, indicating a preferable environmental fitness (Fig. 4M, N, Supplementary Fig. 4G–I, and Supplementary Movie 1). The collective fabrication of blood clot bionic gel BCgel has yielded a remarkable potential to emulate the biofunction of fibrin.
BCgel facilitates osteogenesis by activating mechanical Itgb1-mediated focal adhesion signaling and the subsequent force-sensitive transcription factor Runx2
To investigate the biofunction of BCgel, we initially examined the Itgb1-mediated focal adhesion by co-staining Itgb1 and Fak, based on the CLSM-captured images. As anticipated, treatment with BCgel significantly increased the Itgb1-mediated focal adhesion by up to 10.7-fold compared to the mock treatment (Fig. 5A, B). Consequently, BCgel treatment markedly enhanced the activity of Itgb1-mediated focal adhesion signaling, as evidenced by the up-regulation of Itgb1, Fak, ARhoa, Rock2, c-Jun in WB blots (Fig. 5C and Supplementary Fig. 5A) and the enrichment analysis of genes involved in focal adhesion assembly measured by RNA-seq (Fig. 5D). Furthermore, GSEA analysis also revealed a significant up-regulation in the BCgel group of the Integrin-mediated signaling pathway, cell adhesion signaling related to integrin function, osteoblast development signaling pathway, and Runx2-mediated bone development signaling pathway (Fig. 5E). This suggests an enhancement of Integrin-mediated focal adhesion signaling and subsequent Runx2-dependent osteogenesis in response to BCgel treatment. To further validate the force-sensitivity of Runx2, a series of BCgels with a fixed Ca2+ concentration of 0.1 mg/mL and tunable BCgel monomer concentrations ranging from 0.1% to 4.0% were fabricated. Subsequently, these BCgels were incubated with MSCs followed by Western blotting analysis of Runx2 expression levels (Fig. 5F). As anticipated, different BCgels exhibited varying degrees of nuclear translocation for Runx2, with the highest level observed in the 3% BCgel (Fig. 5G, H). Additionally, the enhanced nuclear translocation resulted in an increased tansactivation of Runx2 (Supplementary Fig. 5B).
A, B Immunofluorescent staining of Fak&Itgb1 in MSCs incubated with or without BCgel for 24 h was analyzed by CLSM. Double positive signals were quantified by Image J with colocalization factor (Pearson’s R value) (B). (n = 6 independent replicates, 10 counts per sample, means ± SD, p value calculated by two-tailed Student’s t test). C The quantification of western blotting analysis of Itgb1, Fak, active Rhoa (ARhoa), Rock2 and c-Jun in MSCs incubated with or without BCgel for 24 hours. (n = 3 independent replicates, means ± SD). D, E Gene Set Enrichment Analysis (GSEA) was performed to compare the Ctrl and BCgel-treated MSCs in terms of the focal adhesion assembly signaling pathway (D), integrin-mediated signaling pathway, cell adhesion related to integrin signaling pathway, osteoblast development signaling pathway, and Runx2 bone development signaling pathway (E). (n = 3 biological replicates in each group). F Runx2 expression in the nucleus and cytoplasm of MSCs incubated with vary concentrations of BCgel were measured by western blotting analysis. G, H The gray value of the gel is utilized for quantitative analysis of Runx2 in both the nucleus and karyoplasm. (n = 3 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test, **p = 0.0012, ***p < 0.001, ****p < 0.001). I, J MSCs with or without Itgb1 knockdown were incubated with BCgel for 24 hours. Runx2 expressions were subsequently detected by western blotting analysis and quantification (I). The quantification of western blotting analysis of Fak, active Rhoa (ARhoa), Rock2 and c-Jun was shown in (J). (n = 3 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). K–M The osteogenic differentiation of MSCs was assessed on day 7 after osteogenic induction by Alp staining (K), Alp activity analysis (L), and western blotting (M). (n = 6 independent replicates for Alp activity analysis, means ± SD, p value calculated by two-tailed Student’s t test; n = 3 independent replicates for western blotting). N MSCs with or without Itgb1 knockdown were incubated with BCgel, and western blotting analysis was performed on day 7 after osteogenic induction. (n = 3 independent replicates).
These findings not only confirm the force-sensitivity of Runx2 but also reaffirm that utilizing a monomer concentration of 3% for BCgel fabrication along with a Ca2+ concentration of 0.1 mg/mL represents an optimal choice. Furthermore, the BCgel-induced nuclear translocation of Runx2 (Fig. 5I and Supplementary Fig. 5C) as well as the corresponding activation of integrin-mediated focal adhesion signaling (Fig. 5J and Supplementary Fig. 5D) were both repressed in Itgb1-knock-down MSCs, indicating a reliance on Itgb1 for this process. In addition to inhibiting the nuclear translocation of Runx2, knocking down its nuclear transporter Ipo8 also resulted in a reduction of transactivation in downstream protein Alp (Supplementary Fig. 5G, H), indicating the reliance on Runx2 translocation. Additionally, the accumulation of Runx2 in the nucleus also resulted in the stimulation of its downstream protein Alp (Supplementary Fig. 5E, F), subsequently promoting osteogenic differentiation of MSCs (Fig. 5K–M and Supplementary Fig. 5I, J). Moreover, this process of osteogenic differentiation was also hindered in Itgb1-knockdown MSCs (Fig. 5N). Collectively, the effect of BCgel enhances the osteogenic differentiation of MSCs by activating mechanical Itgb1-mediated focal adhesion signaling and subsequent force-sensitive nuclear translocation of Runx2.
The application of BCgel significantly enhances osteogenesis in the rat bone defect models with blood clot defect (BCD)
The remarkable bioactivity of BCgel in vitro prompted us to investigate its efficacy in vivo. To this end, we conducted a comparative study between BCgel and gelform (Ctrl group), a commercially available hemostatic material for tooth extraction, using the BCD model of tooth extraction in hypertensive rats. Interestingly, BCgel also exhibited hemostatic capability and resulted in a significant 55% reduction in coagulation time compared to gelform (Supplementary Fig. 6A). One week after the molding and subsequent treatment, proteome results were obtained by LC-MS using a 4D label-free method. Gene set enrichment analysis (GSEA) of these results revealed the activation of Itgb1/Fak-mediated focal adhesion signaling and subsequent Runx2-mediated bone regeneration signaling pathway (Fig. 6A–C), indicating the effectiveness of BCgel at the protein level. Additionally, micro-CT scans also demonstrated increased new bone formation on the medial wall of the extraction socket in the BCgel group at one-week post-treatment. Quantitative analysis of micro-CT data showed a significant increase in BMD by 73% as well as BV/TV by 84%, and a decrease in Tb.Sp by 47% compared to the Ctrl group, indicating a significantly greater amount of new bone in the BCgel group. In addition, abundant new bone was observed within the extraction socket of the BCgel group in tissue sections obtained at one-month post-treatment, which was notably more than that seen in the Ctrl group (Fig. 6D and Supplementary Movies 2 & 3). Consistent with this result, Micro-CT scans at one-month post-treatment also revealed a higher degree of new bone formation within the extraction socket in the BCgel group (Fig. 6D). After treatment, decalcification and sectioning of the jawbones were performed at one week and one month. Histological staining with H&E, Masson’s trichrome, and VG revealed that new bone formation occurred on the medial wall of the extraction socket in the BCgel group after one week of treatment (Fig. 6E and Supplementary Fig. 6B), and this phenomenon was more pronounced at one month after BCgel treatment. Moreover, the levels of Fak were elevated in the BCgel group compared to the Ctrl group, as evidenced by immunohistochemical staining at one-week and one-month post-treatment (Fig. 6F, G). This further supports the notion that BCgel promotes activation of Itgb1/Fak-mediated focal adhesion signaling. Additionally, in order to further scrutinize the emergence of new bone formation, calcein (green) was intravenously injected into the tail vein one-week post-treatment, succeeded by alizarin red (red) at two weeks and tetracycline (yellow) at four weeks. Subsequently, hard tissue sections were obtained three days after tetracycline injection for sample collection. It is evidently discernible that the width of all three hues within the BCgel group surpasses significantly that observed in the Ctrl group, thereby indicating an accelerated pace of new bone generation induced by BCgel (Fig. 6H). The immunofluorescent co-staining of CD73 and Fak further confirmed this finding, demonstrating a significant 31-fold increase in double positive cells at one-week post-treatment and a 15-fold increase at one-month post-treatment in response to BCgel treatment (Fig. 6I, J). These results suggest that BCgel enhances Itgb1/Fak-mediated focal adhesion signaling in MSCs to a much greater extent. In accordance with these findings, immunofluorescence staining and quantitative analysis demonstrated increased levels of Runx2 and Alp staining in the BCgel group at both one-week and one-month post-treatment compared to the Ctrl group (Supplementary Fig. 6C and Fig. 6K, L), which was accompanied by up-regulation of Itgb1 (Supplementary Fig. 6D). Collectively, these results indicate that BCgel enhances the osteogenesis signaling pathway in this rat model of BCD.
A, B The osteogenic signaling pathway was analyzed for gene set enrichment analysis using proteome data obtained from the socket and surrounding tissue via LC-MS with a 4D label-free method, comparing BCgel vs Ctrl. C The heat map illustrates the key proteins involved in osteogenic signaling in the given dataset in A, B. (n = 3 independent replicates). D Micro-CT analysis and quantitative results of BCD rats treated with gelform (Ctrl) and BCgel for 1 week and 1 month after tooth extraction. (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). E H&E staining of extraction region from Ctrl and BCgel group at 1 week and 1 month post treatment. F, G Immunohistochemical staining and quantification of Fak were performed on samples from Ctrl and BCgel groups at 1 week (F) and 1 month (G) post treatment. (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). H Sequential fluorescent labeling observation showing new bone formation at extraction socket (green: calcein, week 1; red: Alizarin red, week 2; yellow: tetracycline, week 4). I, J Immunofluorescent staining of CD73 and Fak from Ctrl and BCgel groups at 1 week (I) and 1 month (J) post treatment was analyzed by CLSM. Double positive signals were quantified by Image J with colocalization factor (Pearson’s R value). (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). K, L Immunofluorescent staining and quantification (L) of Runx2 and Alp at 1 month post treatment. (n = 6 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test).
Additionally, in order to further challenge BCgel, a larger and more intricate wound was created through molar extraction in rats. To my immense satisfaction, the evaluation conducted one month after administering BCgel or mock treatment revealed a significant 39% increase in bone mineral density (BMD), accompanied by an impressive 75% rise in bone volume fraction (BV/TV) (Supplementary Fig. 6E). Furthermore, there was a remarkable 50% reduction in trabecular separation (Tb.Sp) observed among the BCgel-treated rats compared to the control group (Supplementary Fig. 6E). These findings unequivocally indicate a substantially greater amount of newly formed bone within the BCgel group. Additionally, a mechanically unloaded BCgel with a low concentration of 0.5% was utilized as a non-mechanical control to investigate the bio-functionality of BCgel, as depicted in Supplementary Fig. 6F, G, wherein 0.5% BCgel exhibited negligible osteogenic effects.
It is noteworthy that BCgel treatment exhibited no signs of systemic toxicity in comparison to the control group, as evidenced by the histopathological analysis of heart, liver, spleen, lung, and kidney samples collected at one-week and one-month post-treatment (Supplementary Fig. 7A, B), along with the results from blood routine examinations (Supplementary Fig. 7C). To further assess its biosafety profile, BCgel was subcutaneously implanted in healthy SD rats while a commercial gelform served as the control. As anticipated, BCgel demonstrated a reduced inflammatory response compared to the gelform counterpart, supported by H&E staining (Supplementary Fig. 8A) and immunohistochemical staining for TNF-α (Supplementary Fig. 8B, C) as well as IL-1β (Supplementary Fig. 8D, E) at implantation sites collected at 1 d, 3 d and 7 d post-implantation. Furthermore, this finding was corroborated by serum inflammatory markers including TNF-α, IL-1β, IL-6, IL-8, IFN-γ and IL-17 levels (Supplementary Fig. 8F). Importantly, neither BCgel nor gelform induced any hepatic or renal abnormalities in function (Supplementary Fig. 8G), nor did they have any impact on hematological parameters (Supplementary Fig. 8H). Together, these findings provide compelling evidence that supports the biosafety profile of BCgel and highlights its potential for clinical translation.
BCgel potently enhances osteogenesis in beagle bone defect models with BCD
To further enhance the bioactivity of BCgel in promoting osteogenesis in vivo, an additional bone defect models with blood clot defect was established in beagles, wherein the maxillary incisors were extracted subsequently to heparin injection to disrupt blood clot formation. Next, the extraction sockets were hemostatically treated with BCgel or gelform (Ctrl), resulting in a significant 69% reduction in coagulation time (Fig. 7A). Two months after tooth extraction, the BCgel-treated socket demonstrated significantly enhanced bone regeneration, as evidenced by Micro-CT imaging (Fig. 7B and Supplementary Movies 4 & 5) and corresponding quantitative data of BMD, BV/TV, and Tb.Sp (Fig. 7C). This outcome was further supported by the H&E, Masson’s trichrome, and VG staining of the decalcified tissue section (Fig. 7D). In contrast, the gelform group (Ctrl) showed no statistically significant difference in new bone formation compared to the teeth extraction-only group based on BMD, BV/TV, and Tb.sp measurements (Supplementary Fig. 9A, B). Additionally, the administration of BCgel for a duration of two months did not result in any observed immunotoxicity (Fig. 7E and Supplementary Fig. 9C), hematotoxicity (Fig. 7F and Supplementary Fig. 9D), hepatotoxicity (Fig. 7G, H, and Supplementary Fig. 9E), nephrotoxicity (Fig. 7G, I, and Supplementary Fig. 9E), or cardiotoxicity (Fig. 7G, and Supplementary Fig. 9E, F), suggesting a favorable biosafety profile.
A Photos of beagle tooth extraction and the comparison of coagulation time in gelform (Ctrl) and BCgel treated immediately after tooth extraction. (n = 7, including 4 beagles for 2 months treatment and 3 beagles for 5 months treatment, means ± SD, p value calculated by two-tailed Student’s t test). B, C Micro-CT analysis and quantitative results of Ctrl and BCgel groups after 2 months of treatment. (n = 4 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). D H&E, Masson’s trichrome and VG staining of extraction region from Ctrl and BCgel group at 2 months post treatment. E–I Ctrl and BCgel groups were analyzed for immunotoxicity (E), hematotoxicity (F), hepatotoxicity (H), and nephrotoxicity (I). H&E staining of organs in the BCgel group after 2 months of treatment (G). (n = 4 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). J, K Micro-CT analysis and quantitative results of the Ctrl and BCgel groups were assessed after 5 months of treatment. (n = 3 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test). L H&E, Masson’s trichrome and VG staining of extraction region from Ctrl and BCgel group at 5 months post treatment. M–P)Ctrl and BCgel groups were analyzed for hematotoxicity (M), hepatotoxicity (N), and nephrotoxicity (P). H&E staining of organs in the BCgel group after 5 months of treatment (O). (n = 3 independent replicates, means ± SD, p value calculated by two-tailed Student’s t test).
Five months after tooth extraction, the BCgel-treated socket exhibited complete ossification with regenerated new trabecular bone (Fig. 7J). Furthermore, quantitative analysis of micro-CT results revealed a significant enhancement in BMD by 105%, an increase in BV/TV by 143%, an elevation in Tb.N by 56%, and a reduction in Tb.Sp by 60% compared to the Ctrl group (Fig. 7K). These findings strongly indicate the potent bioactivity of BCgel in promoting osteogenesis. Consistent with these results, histological staining including H&E, Masson’s trichrome, and VG staining of decalcified tissue sections demonstrated nearly complete bone healing within the BCgel-treated socket, contrasting with less than half the level of healing observed within gelform-treated control group (Fig. 7L). Importantly, no signs of physiological toxicity were observed at this time point for BCgel treatment, including hematotoxicity (Fig. 7M), hepatotoxicity (Fig. 7N, O, and Supplementary Fig. 9G), nephrotoxicity (Fig. 7O, P, and Supplementary Fig. 9G), or cardiotoxicity (Fig. 7O, and Supplementary Fig. 9G, H). As a whole, BCgel exerts a potent enhancement of osteogenesis in the blood clot defect (BCD) beagle model, while simultaneously maintaining a favorable biosafety profile.
Discussion
The bone possesses extraordinary regenerative capabilities that facilitate the process of healing without compromising its structural integrity or functionality, and an expanding body of research is currently unveiling the biomechanical impact of blood clot formation on bone regeneration3,4. Notably, the blood clot primarily consists of fibrin, thus forming a type of fibrin hydrogel31,32. The present study reveals a fascinating mechanochemical coupling interaction between MSCs and fibrin, which promotes bone regeneration. Specifically, at sites of bone defects, fibrin hydrogels bind to MSCs’ Itgb1 and utilize its viscoelasticity to facilitate the osteogenic process of MSCs by activating Itgb1/Fak-mediated focal adhesion signaling and subsequent Runx2-mediated bone regeneration signaling. The data presented herein demonstrate that the coagulation of blood through fibrin forms a biophysical matrix, which can seamlessly integrate with the extracellular matrix of MSCs to establish a mechanical milieu conducive to bone regeneration. Furthermore, in line with previous reports emphasizing the profound impact of matrix viscoelasticity on MSC behaviors, including their capacity for osteogenic differentiation33,34, the findings presented in this study not only reaffirm this phenomenon but also reveal its underlying mechanisms of mechanotransduction that promote osteoanagenesis through modulation of the viscoelasticity-sensitive transcription factor Runx2. It is worth noting that while Runx2 is an essential transcription factor for skeletal development and osteoblast differentiation, to our knowledge, this study marks the first identification of its role as a force-sensitive transcription factor with viscoelasticity-sensitive properties.
The discovery opens up exciting possibilities for the development of a hydrogel that mimics the viscoelastic and biochemical properties of fibrin, thereby inducing the nuclear translocation of Runx2 and facilitating bone regeneration. By employing this approach, a viscoelastic adjustable BC-biomimetic hydrogel named BCgel was fabricated in the present investigation, possessing an identical nanofiber network microstructure as fibrin and exhibiting equivalent binding affinity to Itgb1 as fibrin. Moreover, the non-covalent crosslinking among BCgel monomers can be precisely regulated by 2D parameters associated with Ca2+ concentration and BCgel monomer concentration, encompassing underlying hydrogen bonding, hydrophobic interaction, electronic interactions, and ionic interaction. Consequently, this enables the BCgel hydrogel to possess a storage and loss modulus akin to that of fibrin hydrogel for optimal promotion of bone regeneration. As a result, at a concentration of 3% and a dosage of 0.1 mg/mL Ca2+, the BCgel exhibited hydrogel viscoelasticity comparable to that of 0.5% fibrin. Moreover, this BCgel exhibited extraordinary bioactivity by inducing the translocation of Runx2 into the nucleus and promoting bone regeneration both in vitro and in rat as well as beagle models with blood clot defect. The BCgel derived from peptides exhibits exceptional biocompatibility, particularly in terms of minimal immunotoxicity, a concern commonly associated with fibrin-derived hydrogels35,36. Moreover, the BCgel possesses a biomimetic chemical nature characterized by its well-defined molecular structure and precise chemical composition, thereby endowing it with inherent advantages in terms of quality control and mass production compared to biological products like fibrin-derived hydrogels. Thus, BCgel is an immensely promising bone repair hydrogel with significant potential for clinical translation. Besides, BCgel is also a promising treatment option for bone regeneration disorder derived from BCD. In this case, BCgel can bind with the remaining Itgb1 in MSC to activate the Runx2 signaling pathway. This activation not only promotes osteogenesis but also enhances the expression of Itgb137,38, resulting in a positive feedback loop that further activates this osteogenesis pathway. Importantly, this conclusion is supported by the up-regulated levels of Itgb1 and Runx2 observed in both BCgel-treated MSC (Supplementary Fig. 5A & B) and BCgel-treated BCD mice model (Supplementary Fig. 6C & D).
In conclusion, our findings propose that the viscoelastic properties of blood clots (fibrin hydrogels) play a crucial role in orchestrating MSC osteogenic differentiation. The manipulation of fibrin hydrogel’s viscoelasticity regulates the establishment of Itgb1/Fak-mediated focal adhesions and subsequent relocation of Runx2 to the nucleus, thus facilitating bone regeneration. Although BCgel effectively promotes bone regeneration in rat and beagle BCD models, further investigations are warranted to assess its efficacy in diverse models of large complex bone defects or disease-induced bone defects.
Collectively, this study offers valuable insights into stem cell mechano-transduction during osteogenic differentiation and introduces potential guidelines for designing viscoelastic hydrogels in bone regenerative medicine.
Methods
Animals
Normal female Sprague-Dawley (SD) rats, aged 6-8 weeks and weighing between 180–220 g, as well as male beagles aged 12 months and weighing between 8–10 kg, were procured from the Laboratory Animal Center of Xi’an Jiaotong University (license number: SYXK 2020-001). Female spontaneously hypertensive SD rats, also aged 6–8 weeks and weighing between 160–180 g, were obtained from Beijing Vital River Laboratory Animal Technology Co., Ltd.
The animals were provided with standard chow and maintained under a typical light/dark cycle in pathogen-free conditions. All experimental procedures involving these animals adhered to institutional guidelines and received approval from the Laboratory Animal Center of Xi’an Jiaotong University. The animal ethics approval number is No. 20211732.
Tooth extraction models
Rat tooth extraction model
The surgical procedure was performed under general anesthesia utilizing pentobarbital sodium. The maxillary right incisors of the rats were surgically extracted. The rats were randomly assigned to two treatment groups: one group consisting of six rats that received 50 µL of 3% BCgel (w/v) and another group comprising three rats treated with 50 µL of 0.5% BCgel. Control groups were administered a medical gelatin sponge (50 mm³). Blood loss and bleeding time were recorded for each group following the extraction surgery. At the conclusion of the treatment, rats were euthanized through the administration of an overdose of pentobarbital sodium. Blood samples were collected for biochemical analysis, and serum was subsequently separated. The entire maxilla, along with various organs, was harvested for further investigation. Additionally, blood clot experiments were conducted on normal and hypertensive SD rats that had undergone tooth extraction without any treatment (6 per group).
Furthermore, the extraction model for maxillary first molars was incorporated into this study. The rats were randomly assigned to two groups (3 per group): the control group, which received treatment with a 50 mm³ medical gelatin sponge; and the BCgel group, which was administered 50 µL of a designed peptide solution at a concentration of 3% (w/v). Maxillary samples were collected 1 month following the treatment.
Beagle tooth extraction model
To develop a model for blood clot defects, beagles were administered subcutaneously with 1000 U/kg of low-molecular-weight heparin (LMWH) every 12 hours for a total of 6 injections over 3 days prior to tooth extraction. Following this initial treatment phase, the beagles continued to receive 500 U/kg of LMWH once daily throughout the duration of the study to sustain systemic hypocoagulability.
After the extraction of the mandibular lateral incisors, beagles were randomly assigned to three groups: the extraction group, a control group treated with 200 mm³ medical gelatin sponge, and the BCgel group treated with 200 µL of a 3% designed peptide solution. Bleeding times were recorded for each group following the extraction surgery. At 2 months post-extraction (3 per group), at 4 months (4 per group), and at 5 months (3 per group) post-treatment, the dogs were euthanized via intravenous injection of pentobarbital sodium. Blood samples were collected for biochemical analysis. The entire mandible and organs were harvested for further investigation.
Fibrin staining in blood clot
At 3-, 6-, 24-, and 1-week post-tooth extraction, and in the absence of any treatment, the rats were euthanized. Subsequently, the maxilla was harvested, fixed and decalcified using a novel rapid decalcification solution (Servicebio, G1107-500ML, China). This solution, containing 5% formic acid as the effective decalcifying agent, was used in a volume exceeding the tissue block by more than 10 times. The samples underwent gentle agitation on a shaker at a speed of 15–20 rpm for 2–3 days, with regular replacement of the decalcification solution every 2–3 days. Complete decalcification was achieved after a total immersion period of 2 weeks. The samples were then transferred to buffered formalin for approximately 48 h to achieve equilibrium before proceeding with dehydration and embedding.
When sectioning the sample into 4 µm slices, the cutting direction was parallel to the sagittal plane, progressing from the buccal side inward. Following a series of procedures, including fixation, decalcification, dehydration, and embedding, the blood clot within the extraction socket became integrated with the entire socket. The blood clot was embedded in the C-shaped extraction socket sections, and during staining, it is crucial to minimize excessive washing to preserve its relatively intact morphology. The slices were stained using a fibrin stain kit (Solarbio, G2040, China), and scanned by a fully automated scanner (3D HISTECH, Pannoramic DESK, Hungary).
Preparation of BCgel (blood colt gel) peptide
The BCgel monomer peptide sequence is (RADA)4GSVLGYIQIR. Utilizing solid-phase synthesis technology of FMOC peptides, the monomer peptide was synthesized on MBHA resin using an automated peptide synthesizer CS Bio 336X. HBTU served as the condensation agent, while DIEA functioned as the catalyst. After cleavage and deprotection using a reagent mixture comprising 88% TFA, 5% phenol, 5% H2O, and 2% TIPS, the peptides were precipitated with cold ether. The peptides were subsequently characterized by electrospray ionization mass spectrometry (ESI-MS) and high-performance liquid chromatography (HPLC). Purification to homogeneity was achieved via preparative C18 reversed-phase HPLC, utilizing a solvent system of acetonitrile and water with 1/1000 TFA. Peptide solutions at concentrations ranging from 0 to 4% were prepared to satisfy various experimental needs.
Fluorescence polarization assay
Fluorescein isothiocyanate (FITC) was conjugated to the BCgel monomer peptide and fibrin via an N-terminal amino group in DMF. The conjugates were subsequently purified by C4 reversed-phase high-performance liquid chromatography (RP-HPLC) and lyophilized. The binding experiments between the BCgel monomer peptide or fibrin and Itgb1 were conducted in 96-well black plates, and measurements were taken using a SpectraMax® iD5 (Molecular Devices, USA). Serially diluted Itgb1 proteins (Proteintech, Ag24476, Wuhan, China) were prepared in Tris-HCl buffer (10 mM Tris, 150 mM NaCl, 1 mM EDTA, pH 7.0) and incubated with FITC-labeled BCgel and FITC-labeled fibrin in a final volume of 150 μL per well. Following a 2-hour incubation at room temperature, fluorescence polarization (FP) was measured at excitation and emission wavelengths of 470 nm and 530 nm, respectively. Nonlinear regression analysis was performed to determine the Kd values using the following equation:
Where F represents the measured FP, Fc denotes the FP of the BCgel monomer peptide or the Fibrin/Itgb1 complex, F0 indicates the FP of FITC-BCgel and FITC-fibrin, [Pep] signifies the final concentration of the BCgel monomer peptide or fibrin, and [Itgb1] represents the total concentration of the Itgb1 protein.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The raw sequence data reported in this paper have been deposited in the Genome Sequence Archive (Genomics, Proteomics & Bioinformatics 2021) in National Genomics Data Center (Nucleic Acids Res 2022), China National Center for Bioinformation/Beijing Institute of Genomics, Chinese Academy of Sciences (GSA: CRA017883 [ngdc.cncb.ac.cn/gsa/search?searchTerm=CRA017883]) that are publicly accessible at https://ngdc.cncb.ac.cn/gsa. All the other data generated in this study are provided in the Supplementary Information/Source Data file. Source data are provided with this paper.
References
Clarke, B. Normal bone anatomy and physiology. Clin. J. Am. Soc. Nephrol. 3, S131–S139 (2008).
Hadjidakis, D. J. & Androulakis, I. I. Bone Remodeling. Ann. N. Y. Acad. Sci. 1092, 385–396 (2006).
Schell, H. et al. The haematoma and its role in bone healing. J. Exp. Orthop. 4, 5 (2017).
Shiu, H. T., Leung, P. C. & Ko, C. H. The roles of cellular and molecular components of a hematoma at early stage of bone healing. J. Tissue Eng. Regenerative Med. 12, e1911–e1925 (2018).
Shiu, H. T., Goss, B., Lutton, C., Crawford, R. & Xiao, Y. Formation of blood clot on biomaterial implants influences bone healing. Tissue Eng. B: Rev. 20, 697–712 (2014).
Yang, Y. & Xiao, Y. Biomaterials regulating bone hematoma for osteogenesis. Adv. Healthc. Mater. 9, 2000726 (2020).
Noori, A., Ashrafi, S. J., Vaez-Ghaemi, R., Hatamian-Zaremi, A. & Webster, T. J. A review of fibrin and fibrin composites for bone tissue engineering. Int. J. Nanomed. 12, 4937–4961 (2017).
Weisel, J. W. The mechanical properties of fibrin for basic scientists and clinicians. Biophys. Chem. 112, 267–276 (2004).
Weisel, J. W. Structure of fibrin: impact on clot stability. J. Thrombosis Haemost. 5, 116–124 (2007).
Litvinov, R. I. & Weisel, J. W. Blood clot contraction: mechanisms, pathophysiology, and disease. Res. Practice Thrombosis Haemostasis 7 (2023).
Chen, J. C. & Jacobs, C. R. Mechanically induced osteogenic lineage commitment of stem cells. Stem Cell Res. Therapy 4, 107 (2013).
Argentati, C. et al. Insight into mechanobiology: how stem cells feel mechanical forces and orchestrate biological functions. Int. J. Mol. Sci. 20 (2019).
Xia, M. et al. Varying mechanical forces drive sensory epithelium formation. Sci. Adv. 9, eadf2664.
Schrenk-Siemens, K. et al. PIEZO2 is required for mechanotransduction in human stem cell–derived touch receptors. Nat. Neurosci. 18, 10–16 (2015).
Yin, S., Zhang, W., Zhang, Z. & Jiang, X. Recent advances in scaffold design and material for vascularized tissue-engineered bone regeneration. Adv. Healthc. Mater. 8, 1801433 (2019).
Hasanzadeh, R. et al. Biocompatible tissue-engineered scaffold polymers for 3D printing and its application for 4D printing. Chem. Eng. J. 476, 146616 (2023).
Arutyunyan, I., Elchaninov, A., Sukhikh, G. & Fatkhudinov, T. Cryopreservation of tissue-engineered scaffold-based constructs: from concept to reality. Stem Cell Rev. Rep. 18, 1234–1252 (2022).
Niu, X., Li, N., Du, Z. & Li, X. Integrated gradient tissue-engineered osteochondral scaffolds: Challenges, current efforts and future perspectives. Bioact. Mater. 20, 574–597 (2023).
Tutwiler, V. et al. Rupture of blood clots: mechanics and pathophysiology. Sci. Adv. 6, eabc0496.
Previtali, E., Bucciarelli, P., Passamonti, S. M. & Martinelli, I. Risk factors for venous and arterial thrombosis. Blood Transfus. 9, 120 (2011).
Vieira, A. E. et al. Intramembranous bone healing process subsequent to tooth extraction in mice: micro-computed tomography, histomorphometric and molecular characterization. PLoS ONE 10, e0128021 (2015).
de Sousa Gomes, P., Daugela, P., Poskevicius, L., Mariano, L. & Fernandes, M. H. Molecular and cellular aspects of socket healing in the absence and presence of graft materials and autologous platelet concentrates: a focused review. J. Oral Maxillofacial Res. 10 (2019).
Rui, V., Richard, J. F., Alessandro, C. & Marguerite, N.-A. Fibrin(ogen) in human disease: both friend and foe. Haematologica 105, 284–296 (2020).
Kattula, S., Byrnes, J. R. & Wolberg, A. S. Fibrinogen and fibrin in hemostasis and thrombosis. Arterioscler Thromb. Vasc. Biol. 37, e13–e21 (2017).
Abou-Jaoude, A. et al. ShcA promotes chondrocyte hypertrophic commitment and osteoarthritis in mice through RunX2 nuclear translocation and YAP1 inactivation. Osteoarthr. Cartil. 30, 1365–1375 (2022).
Ziros, P. G., Basdra, E. K. & Papavassiliou, A. G. Runx2: of bone and stretch. Int. J. Biochem. Cell Biol. 40, 1659–1663 (2008).
Westendorf, J. J. Transcriptional co-repressors of Runx2. J. Cell. Biochem. 98, 54–64 (2006).
Schroeder, T. M., Jensen, E. D. & Westendorf, J. J. Runx2: A master organizer of gene transcription in developing and maturing osteoblasts. Birth Defects Res. C: Embryo Today.: Rev. 75, 213–225 (2005).
He, W. et al. Turning a Luffa protein into a self-assembled biodegradable nanoplatform for multitargeted cancer therapy. ACS Nano 12, 11664–11677 (2018).
Rossi, A. M. & Taylor, C. W. Analysis of protein-ligand interactions by fluorescence polarization. Nat. Protoc. 6, 365–387 (2011).
Rausch, M. K., Parekh, S. H., Dortdivanlioglu, B. & Rosales, A. M. Synthetic hydrogels as blood clot mimicking wound healing materials. Prog. Biomed. Eng. 3, 042006 (2021).
Guy, R. D., Fogelson, A. L. & Keener, J. P. Fibrin gel formation in a shear flow. Math. Med. Biol. 24, 111–130 (2007).
Lee, H.-P., Stowers, R. & Chaudhuri, O. Volume expansion and TRPV4 activation regulate stem cell fate in three-dimensional microenvironments. Nat. Commun. 10, 529 (2019).
Chaudhuri, O., Cooper-White, J., Janmey, P. A., Mooney, D. J. & Shenoy, V. B. Effects of extracellular matrix viscoelasticity on cellular behaviour. Nature 584, 535–546 (2020).
Ghobril, C. & Grinstaff, M. W. The chemistry and engineering of polymeric hydrogel adhesives for wound closure: a tutorial. Chem. Soc. Rev. 44, 1820–1835 (2015).
Lee, Y. K., Choi, E.-J., Webster, T. J., Kim, S.-H. & Khang, D. Effect of the protein corona on nanoparticles for modulating cytotoxicity and immunotoxicity. Int. J. Nanomed. 10, 97–113 (2015).
Hu, P. et al. Fak silencing impairs osteogenic differentiation of bone mesenchymal stem cells induced by uniaxial mechanical stretch. J. Dent. Sci. 14, 225–233 (2019).
Hamidouche, Z., Fromigué, O., Ringe, J., Häupl, T. & Marie, P. J. Crosstalks between integrin alpha 5 and IGF2/IGFBP2 signalling trigger human bone marrow-derived mesenchymal stromal osteogenic differentiation. BMC Cell Biol. 11, 44 (2010).
Acknowledgements
This work was supported by the National High Level Talents Special Support Plan (W. Liu), Thousand Talents Plan of Shaanxi Province (W. He), The National Natural Science Foundation of China (No. 32271426), The “Young Talent Support Plan” of Xi’an Jiaotong University (W. He and W. Liu). We thank Instrument Analysis Center of Xi’an Jiaotong University for their assistance with SEM, TEM, FP, and Rheology analysis. The assistance of RNA and proteomic analysis provided by BioNovoGene (Suzhou) Co., Ltd. is greatly appreciated.
Author information
Authors and Affiliations
Contributions
W.He. and W.Liu. designed the study and analyzed the data. F.Ding. and L.Zhang. performed the experiments. W.He. wrote the manuscript. W.L. revised the manuscript and supervised the study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Hironori Hojo, Yan Liu, Joaquim Vives, Xin Wang and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
He, W., Ding, F., Zhang, L. et al. In situ osteogenic activation of mesenchymal stem cells by the blood clot biomimetic mechanical microenvironment. Nat Commun 16, 1162 (2025). https://doi.org/10.1038/s41467-025-56513-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-56513-6
This article is cited by
-
Elimination of a neutrophil Pad4 byproduct restores stem cell–mediated bone regeneration in hyperglycemia
Nature Communications (2025)