Abstract
Despite the high prevalence of neurodevelopmental disorders, the influence of maternal diet during pregnancy on child neurodevelopment remains understudied. Here we show that a western dietary pattern during pregnancy is associated with child neurodevelopmental disorders. We analyse self-reported maternal dietary patterns at 24 weeks of pregnancy and clinically evaluated neurodevelopmental disorders at 10 years of age in the COPSAC2010 cohort (n = 508). We find significant associations with attention-deficit hyperactivity disorder (ADHD) and autism diagnoses. We validate the ADHD findings in three large, independent mother–child cohorts (n = 59,725, n = 656 and n = 348) through self-reported dietary modelling, maternal blood metabolomics and foetal blood metabolomics. Metabolome analyses identify 15 mediating metabolites in pregnancy that improve ADHD prediction. Longitudinal blood metabolome analyses, incorporating five time points per cohort in two independent cohorts, reveal that associations between western dietary pattern metabolite scores and neurodevelopmental outcomes are consistently significant in early–mid-pregnancy. These findings highlight the potential for targeted prenatal dietary interventions to prevent neurodevelopmental disorders and emphasise the importance of early intervention.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
For the COPSAC2010 and COPSAC2000 cohort datasets, participant-level personally identifiable data are protected under the Danish Data Protection Act and European Regulation 2016/679 of the European Parliament and of the Council that prohibit distribution even in pseudo-anonymised form. However, participant-level data can be made available under a data-transfer agreement as part of a collaboration effort with COPSAC (ulrik.ralfkiaer@dbac.dk).
For the VDAART cohort dataset, participant-level data are protected under the consent agreements provided by study participants and applicable US data privacy laws. Data access is subject to stringent security and compliance measures to ensure alignment with the participant consent. Use of the data is restricted to approved investigators within the recipient institution, and data cannot be transferred to personal devices or shared with external parties without prior approval. Collaboration and agreement with VDAART investigators are required for any use of the data. Requests for access to VDAART data should include a detailed proposal outlining the intended analyses and collaborative framework with VDAART investigators. For further inquiries, please contact the VDAART leadership team (rejas@channing.harvard.edu).
For the DNBC cohort dataset, participant-level data are subject to controlled access and protected under the Danish Data Protection Act and European Regulation 2016/679 of the European Parliament and of the Council. These regulations prohibit the distribution of personally identifiable data, even in pseudo-anonymised form, outside the permitted framework. Access to DNBC data is granted on a need-to-know basis and requires approval from the DNBC Reference Group, listing of the project on the applicant’s institution’s data processing register and compliance with the conditions for access. Researchers may request access to DNBC data by submitting an application form and protocol to the DNBC Secretariat (dnbc-research@ssi.dk). Source data are provided with this paper.
Code availability
The custom code employed in this research is freely accessible to the public for transparency and reproducibility purposes. Specifically, code used in making the Gaussian graphical models and backward elimination mediation analysis can be found at https://github.com/dlghorn/Code-for-Gaussian-Graphical-Models-and-Backward-Elimination-Mediation-Analysis.
References
Bougeard, C., Picarel-Blanchot, F., Schmid, R., Campbell, R. & Buitelaar, J. Prevalence of autism spectrum disorder and co-morbidities in children and adolescents: a systematic literature review. Front. Psychiatry 12, 744709 (2021).
Dalsgaard, S. et al. Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry 77, 155–164 (2020).
Willcutt, E. G. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 9, 490–499 (2012).
Talantseva, O. I. et al. The global prevalence of autism spectrum disorder: a three-level meta-analysis. Front. Psychiatry 14, 1071181 (2023).
Larsson, H., Anckarsater, H., Råstam, M., Chang, Z. & Lichtenstein, P. Childhood attention-deficit hyperactivity disorder as an extreme of a continuous trait: a quantitative genetic study of 8,500 twin pairs. J. Child Psychol. Psychiatry 53, 73–80 (2012).
Makransky, G. & Bilenberg, N. Psychometric properties of the parent and teacher ADHD Rating Scale (ADHD-RS): measurement invariance across gender, age, and informant. Assessment 21, 694–705 (2014).
Constantino, J. N. et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J. Autism Dev. Disord. 33, 427–433 (2003).
Cortés-Albornoz, M. C., García-Guáqueta, D.P., Velez-van-Meerbeke, A. & Talero-Gutiérrez, C. Maternal nutrition and neurodevelopment: a scoping review. Nutrients https://doi.org/10.3390/nu13103530 (2021).
Fernandes, D. J. et al. Exposure to maternal high-fat diet induces extensive changes in the brain of adult offspring. Transl. Psychiatry 11, 149 (2021).
Giriko, C. Á. et al. Delayed physical and neurobehavioral development and increased aggressive and depression-like behaviors in the rat offspring of dams fed a high-fat diet. Int. J. Dev. Neurosci. 31, 731–739 (2013).
Mitchell, A. J. et al. Maternal western-style diet reduces social engagement and increases idiosyncratic behavior in Japanese macaque offspring. Brain Behav. Immun. https://doi.org/10.1016/j.bbi.2022.07.004 (2022).
Prado, E. L. & Dewey, K.G. Nutrition and brain development in early life. Nutr. Rev. 72, 267–284 (2014).
Cordain, L. et al. Origins and evolution of the western diet: health implications for the 21st century. Am. J. Clin. Nutr. 81, 341–354 (2005).
Devarshi, P. P., Grant, R. W., Ikonte, C. J. & Hazels Mitmesser, S. Maternal omega-3 nutrition, placental transfer and fetal brain development in gestational diabetes and preeclampsia. Nutrients https://doi.org/10.3390/nu11051107 (2019).
Taylor, M. R., Chuang, C., Carrasco, K. D., Nagatomo, S. & Rucklidge, J.J. Dietary and micronutrient treatments for children with neurodevelopment disorders. Curr. Dev. Disord. Rep. https://doi.org/10.1007/s40474-018-0150-5 (2018).
Halliwell, B., Cheah, I. K. & Tang, R. M. Y. Ergothioneine—a diet-derived antioxidant with therapeutic potential. FEBS Lett. 592, 3357–3366 (2018).
Prince, N. et al. Phenotypically driven subgroups of ASD display distinct metabolomic profiles. Brain Behav. Immun. 111, 21–29 (2023).
Poornimai Abirami, G. P. et al. The regulation of reactive neuroblastosis, neuroplasticity, and nutraceuticals for effective management of autism spectrum disorder. Adv. Neurobiol. 24, 207–222 (2020).
Naveed, S., Lakka, T. & Haapala, E.A. An overview on the associations between health behaviors and brain health in children and adolescents with special reference to diet quality. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17030953 (2020).
Basak, S. & Duttaroy, A. K. Maternal PUFAs, placental epigenetics, and their relevance to fetal growth and brain development. Reprod. Sci. https://doi.org/10.1007/s43032-022-00989-w (2022).
Pettersson, E. et al. Genetic influences on eight psychiatric disorders based on family data of 4 408 646 full and half-siblings, and genetic data of 333 748 cases and controls—CORRIGENDUM. Psychol. Med. 49, 351 (2019).
Atladottir, H. O. et al. The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. Eur. Child Adolesc. Psychiatry 24, 173–183 (2015).
Tran, N. Q. V. & Miyake, K. Neurodevelopmental disorders and environmental toxicants: epigenetics as an underlying mechanism. Int. J. Genomics https://doi.org/10.1155/2017/7526592 (2017).
Keers, R. et al. A genome-wide test of the differential susceptibility hypothesis reveals a genetic predictor of differential response to psychological treatments for child anxiety disorders. Psychother. Psychosom. 85, 146–158 (2016).
Faraone, S. V. et al. The World Federation of ADHD International Consensus Statement: 208 evidence-based conclusions about the disorder. Neurosci. Biobehav. Rev. 128, 789–818 (2021).
Borge, T. C. et al. The associations between maternal and child diet quality and child ADHD—findings from a large Norwegian pregnancy cohort study. BMC Psychiatry 21, 139 (2021).
Howard, A. L. et al. ADHD is associated with a “western” dietary pattern in adolescents. J. Atten. Disord. 15, 403–411 (2011).
Vecchione, R. et al. Maternal dietary patterns during pregnancy and child autism-related traits: results from two US cohorts. Nutrients https://doi.org/10.3390/nu14132729 (2022).
Noerman, S. & Landberg, R. Blood metabolite profiles linking dietary patterns with health: toward precision nutrition. J. Intern. Med. 293, 408–432 (2023).
Bjørklund, G. et al. Oxidative stress in autism spectrum disorder. Mol. Neurobiol. 57, 2314–2332 (2020).
Jiang, H., Chen, C. & Gao, J. Extensive summary of the important roles of indole propionic acid, a gut microbial metabolite in host health and disease. Nutrients https://doi.org/10.3390/nu15010151 (2022).
Richardson, A. J. & Ross, M. A. Fatty acid metabolism in neurodevelopmental disorder: a new perspective on associations between attention-deficit/hyperactivity disorder, dyslexia, dyspraxia and the autistic spectrum. Prostaglandins Leukot. Essent. Fatty Acids 63, 1–9 (2000).
Faraone, S. V. & Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol. Psychiatry 24, 562–575 (2019).
Santos, J. X. et al. A role for gene-environment interactions in autism spectrum disorder is supported by variants in genes regulating the effects of exposure to xenobiotics. Front. Neurosci. 16, 862315 (2022).
Ma, S. L. et al. Genetic overlap between attention deficit/hyperactivity disorder and autism spectrum disorder in gene. Front. Neurosci. 15, 649588 (2021).
Bateson, P. & Gluckman, P. Plasticity, Robustness, Development and Evolution (Cambridge University Press, 2011).
Gusev, A. et al. Partitioning heritability of regulatory and cell-type-specific variants across 11 common diseases. Am. J. Hum. Genet. 95, 535–552 (2014).
Newby, P. K. & Tucker, K. L. Empirically derived eating patterns using factor or cluster analysis: a review. Nutr. Rev. 62, 177–203 (2004).
Zhao, J. et al. A review of statistical methods for dietary pattern analysis. Nutr. J. 20, 37 (2021).
Cui, Q. et al. A meta-analysis of the reproducibility of food frequency questionnaires in nutritional epidemiological studies. Int. J. Behav. Nutr. Phys. Act. 18, 12 (2021).
Gürdeniz, G. et al. Neonatal metabolome of caesarean section and risk of childhood asthma. Eur. Respir. J. https://doi.org/10.1183/13993003.02406-2021 (2022).
Brustad, N. et al. Diet-associated vertically transferred metabolites and risk of asthma, allergy, eczema, and infections in early childhood. Pediatr. Allergy Immunol. 34, e13917 (2023).
Savard, C. et al. Trimester-specific dietary intakes in a sample of french-canadian pregnant women in comparison with national nutritional guidelines. Nutrients https://doi.org/10.3390/nu10060768 (2018).
Urbonaite, G., Knyzeliene, A., Bunn, F. S., Smalskys, A. & Neniskyte, U. The impact of maternal high-fat diet on offspring neurodevelopment. Front. Neurosci. https://doi.org/10.3389/fnins.2022.909762 (2022).
Pingault, J. B. et al. Using genetic data to strengthen causal inference in observational research. Nat. Rev. Genet. 19, 566–580 (2018).
Bisgaard, H. et al. Deep phenotyping of the unselected COPSAC 2010 birth cohort study. Clin. Exp. Allergy https://doi.org/10.1111/cea.12213 (2013).
Mohammadzadeh, P. et al. Effects of prenatal nutrient supplementation and early life exposures on neurodevelopment at age 10: a randomised controlled trial—the COPSYCH study protocol. BMJ Open 12, e047706 (2022).
Olsen, J. et al. The Danish National Birth Cohort—its background, structure and aim. Scand. J. Public Health 29, 300–307 (2001).
Olsen, S. F. et al. Data collected on maternal dietary exposures in the Danish National Birth Cohort. Paediatr. Perinat. Epidemiol. 21, 76–86 (2007).
Litonjua, A. A. et al. The vitamin D antenatal asthma reduction trial (VDAART): rationale, design, and methods of a randomized, controlled trial of vitamin D supplementation in pregnancy for the primary prevention of asthma and allergies in children. Contemp. Clin. Trials 38, 37–50 (2014).
Kelly, R. S. et al. Metabolomics and communication skills development in children; evidence from the ages and stages questionnaire. Metabolites https://doi.org/10.3390/metabo9030042 (2019).
Bisgaard, H. The Copenhagen Prospective Study on Asthma in Childhood (COPSAC): design, rationale, and baseline data from a longitudinal birth cohort study. Ann. Allergy Asthma Immunol. 93, 381–389 (2004).
Obel, C. et al. The strengths and difficulties questionnaire in the Nordic countries. Eur. Child Adolesc. Psychiatry 13, II32–II39 (2004).
Sveen, T. H., Berg-Nielsen, T. S., Lydersen, S. & Wichstrøm, L. Detecting psychiatric disorders in preschoolers: screening with the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 52, 728–736 (2013).
Kaufman, J. et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–988 (1997).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR (APA, 2022).
World Health Organization. The International Statistical Classification of Diseases and Health Related Problems ICD-10: Tenth Revision. Vol. 2 (World Health Organization, 2004).
Friis, S., Kruger Kjaer, S., Stripp, C. & Overvad, K. Reproducibility and relative validity of a self-administered semiquantitative food frequency questionnaire applied to younger women. J. Clin. Epidemiol. 50, 303–311 (1997).
Mikkelsen, T. B., Olsen, S. F., Rasmussen, S. E. & Osler, M. Relative validity of fruit and vegetable intake estimated by the food frequency questionnaire used in the Danish National Birth Cohort. Scand. J. Public Health 35, 172–179 (2007).
Mikkelsen, T. B., Osler, M. & Olsen, S. F. Validity of protein, retinol, folic acid and n-3 fatty acid intakes estimated from the food-frequency questionnaire used in the Danish National Birth Cohort. Public Health Nutr. 9, 771–778 (2006).
National Food Institute. Danish Food Composition Databank v.7.01 (Technical University of Denmark, 2013); http://www.foodcomp.dk
Bjerregaard, A. A., Halldorsson, T. I., Kampmann, F. B., Olsen, S. F. & Tetens, I. Relative validity of a web-based food frequency questionnaire for Danish adolescents. Nutr. J. 17, 9 (2018).
Smith, A. D. A. C., Emmett, P. M., Newby, P. K. & Northstone, K. Dietary patterns obtained through principal components analysis: the effect of input variable quantification. Br. J. Nutr. 109, 1881–1891 (2013).
Kachroo, P. et al. Fish oil supplementation during pregnis protective against asthma/wheeze in offspring. J. Allergy Clin. Immunol. Pract. 8, 388–91.e2 (2020).
Schmidt, M. et al. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin. Epidemiol. 7, 449–490 (2015).
Mors, O., Perto, G. P. & Mortensen, P. B. The Danish Psychiatric Central Research Register. Scand. J. Public Health 39, 54–57 (2011).
Pottegård, A. et al. Data resource profile: the Danish National Prescription Registry. Int. J. Epidemiol. 46, 798–798f (2017).
Kessler, R. C. et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol. Med. 35, 245–256 (2005).
Adler, L. A., Faraone, S. V., Sarocco, P., Atkins, N. & Khachatryan, A. Establishing US norms for the Adult ADHD Self-Report Scale (ASRS-v1.1) and characterising symptom burden among adults with self-reported ADHD. Int. J. Clin. Pract. 73, e13260 (2019).
Rago, D. et al. Fish-oil supplementation in pregnancy, child metabolomics and asthma risk. eBioMedicine 46, 399–410 (2019).
Stekhoven, D. J. & Bühlmann, P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28, 112–118 (2012).
Robinson, D., Bryan J. & Elias, J. fuzzyjoin: join tables together on inexact matching v.0.1.6. CRAN https://cran.r-project.org/package=fuzzyjoin (2020).
Piccininni, M., Konigorski, S., Rohmann, J. L. & Kurth, T. Directed acyclic graphs and causal thinking in clinical risk prediction modeling. BMC Med. Res. Methodol. 20, 179 (2020).
Williams, T. C., Bach, C. C., Matthiesen, N. B., Henriksen, T. B. & Gagliardi, L. Directed acyclic graphs: a tool for causal studies in paediatrics. Pediatr. Res. 84, 487–493 (2018).
Demontis, D. et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat. Genet. 51, 63–75 (2019).
Grove, J. et al. Identification of common genetic risk variants for autism spectrum disorder. Nat. Genet. 51, 431–444 (2019).
Ge, T., Chen, C. Y., Ni, Y., Feng, Y. C. A. & Smoller, J. W. Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nat. Commun. 10, 1776 (2019).
Purcell, S. & Chang, C. PLINK 2.0 https://www.cog-genomics.org/plink/2.0/
Williams, D. R. & Rast, P. Back to the basics: rethinking partial correlation network methodology. Br. J. Math Stat. Psychol. 73, 187–212 (2020).
Marsál, K. et al. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 85, 843–848 (1996).
Josse, J. & Husson, F. missMDA: a package for handling missing values in multivariate data analysis. J. Stat. Softw. https://doi.org/10.18637/jss.v070.i01 (2016).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. https://doi.org/10.18637/jss.v067.i01 (2015).
Acknowledgements
We express our deepest gratitude to the children and families of the COPSAC2010, COPSAC2000 and VDAART cohorts for all their support and commitment. We acknowledge and appreciate the unique efforts of the COPSAC research team. We acknowledge all funding received by COPSAC, listed on www.copsac.com. The Lundbeck Foundation (grant numbers R16-A1694 and R269-2017-5); the Ministry of Health (grant number 903516); the Danish Council for Strategic Research (grant number 0603-00280B) and the Capital Region Research Foundation have provided core support to the COPSAC research centre. This project has received funding from the European Research Council under the European Union’s Horizon 2020 research and innovation programme (grant agreement number 946228) (B.C.). MAR is funded by the Novo Nordisk Foundation (grant number NNF21OC0068517). C.P. was supported by an Australian National Health and Medical Research Council L3 Investigator grant (1196508) and by a grant from the Lundbeck Foundation (ID R246-2016-3237). J.L.-S. (R01HL123915, R01HL155742 and R01HL141826) and S.H.C. (K01HL153941) are funded through the National Institute of Heart, Lung and Blood Institute.
The Danish National Birth Cohort was established with a significant grant from the Danish National Research Foundation. Additional support was obtained from the Danish Regional Committees, the Pharmacy Foundation, the Egmont Foundation, the March of Dimes Birth Defects Foundation, the Health Foundation and other minor grants. The DNBC Biobank has been supported by the Novo Nordisk Foundation and the Lundbeck Foundation. Follow-up of mothers and children was supported by the Danish Medical Research Council (SSVF 0646, 271-08-0839/06-066023, O602-01042B, 0602-02738B), the Lundbeck Foundation (195/04, R100-A9193), The Innovation Fund Denmark 0603-00294B (09-067124), the Nordea Foundation (02-2013-2014), Aarhus Ideas (AU R9-A959-13-S804), University of Copenhagen Strategic Grant (IFSV 2012) and the Danish Council for Independent Research (DFF-4183-00594 and DFF-4183-00152).
The funders had no role in study design, data collection and analysis, decision to publish or preparation of the paper.
Author information
Authors and Affiliations
Contributions
D.H., J.R.J.M.J., B.H.E., J.S. and M.A.R. contributed to the conceptualisation of the study and formulated the overarching research goals and aims. Methodology development was carried out by D.H. and M.A.R., while D.H. was responsible for software implementation, including programming and testing of code. D.H. and M.A.R. validated the results and ensured reproducibility. Formal analysis, applying statistical and computational techniques, was conducted by D.H. and overseen by M.A.R. The investigation process, including data collection, was led by J.R.J.M.J. and conducted by R.V., J.B.R., P.M., K.A. and D.H. Resources, including access to study materials and datasets, were provided by B.C., J.S., K.B., B.H.E. and M.A.R. Data curation, including annotation and maintenance of research data, was performed by D.H. and M.A.R. D.H. drafted the original paper, with all co-authors (J.R.J.M.J., B.C., K.A., J.B.R., P.M., A.S., N.F., R.V., B.F., C.P., N.B., C.E.T.P., A.E., S.B., Y.C., N.P., S.H.C., R.S.K., J.L.-S., T.I.H., M.S., K.S.L., S.F.O., B.Y.G., K.B., B.H.E., J.S. and M.A.R.) contributing to critical review, editing and revisions. D.H., J.S. and M.A.R. handled visualisation and data presentation. J.S., B.H.E. and M.A.R. supervised the research activity. J.R.J.M.J., K.B., B.H.E. and B.F. coordinated and managed the project. All authors guarantee that the accuracy and integrity of any part of the work have been appropriately investigated and resolved, and all have approved the final version of the paper. The corresponding authors had full data access, except for the DNBC cohort, where T.I.H. conducted the analysis. The corresponding authors had final responsibility for the decision to submit for publication.
Corresponding authors
Ethics declarations
Ethics statement
The study is conducted in accordance with the Declaration of Helsinki and was approved by the Danish Ethics Committee (H-B-2008-093) and the Danish Data Protection Agency (2015-41-3696). The study is conducted and monitored in accordance with the requirements of GCP as defined in guidelines, EU Clinical Trials Directive (2001/20/EC) and EU GCP Directive (2005/28/EC). All study participants have signed approved informed consent forms before any study-related procedures. The confidentiality of all study participants will be protected in accordance with GCP guidelines.
Competing interests
B.E. is part of the Advisory Board of Eli Lilly Denmark A/S, Janssen-Cilag, Lundbeck Pharma A/S, and Takeda Pharmaceutical Company; and has received lecture fees from Bristol-Myers Squibb, Boehringer Ingelheim, Otsuka Pharma Scandinavia AB, Eli Lilly Company and Lundbeck Pharma A/S. B.Y.G. has been the leader of a Lundbeck Foundation Centre of Excellence for Clinical Intervention and Neuropsychiatric Schizophrenia Research (CINS) (January 2009 to December 2021), which was partially financed by an independent grant from the Lundbeck Foundation based on international review and partially financed by the Mental Health Services in the Capital Region of Denmark, the University of Copenhagen and other foundations. All grants are the property of the Mental Health Services in the Capital Region of Denmark and administered by them. She has no other conflicts to disclose. J.L.-S. is a scientific advisor for Precion and a consultant to Tru Diagnostic. All other authors declare no competing interests. The funding agencies did not have any role in design and conduct of the study; collection, management and interpretation of the data; or preparation, review or approval of the paper. No pharmaceutical company was involved in the study.
Peer review
Peer review information
Nature Metabolism thanks Kristopher Kahle and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Jean Nakhle and Ashley Castellanos-Jankiewicz, in collaboration with the Nature Metabolism team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Biplot of the first two principal components (PCs) from the maternal food frequency questionnaire-derived nutrient constituents.
The left panel displays box-and-whisker plots summarizing the distribution of PC2 scores, and the bottom panel shows PC1 scores, for children stratified by neurodevelopmental diagnosis status (NDD, ADHD, and autism), with boxes representing the interquartile range (IQR; 25th–75th percentile), centre lines indicating the median, and whiskers extending to 1.5 times the IQR. PC2 (Western dietary pattern) is significantly associated with any neurodevelopmental disorder (OR 1.53 (1.17–2.00), p = 0.002), ADHD (OR 1.66 (1.21–2.27), p = 0.002), and autism diagnosis (OR 2.22 (1.33–3.74), p = 0.002). PC1 is not significantly associated with any neurodevelopmental disorders (p > 0.288). Further details of the loadings for each of the 95 nutrient constituents can be viewed in supplementary table 2. Adjustments were not made for multiple comparisons.
Extended Data Fig. 2 Biplot of the first two principal components from the maternal FFQ-derived nutrient constituents.
Biplot of the first two principal components from the maternal FFQ-derived nutrient constituents A) Nutrient constituents are categorized into fatty acids, amino acids, sugars, minerals and vitamins. Fatty acids are a key determinant of PC2 (Western dietary pattern) B) Stratified further by fatty acid type, saturated fatty acids are most associated with PC2 (Western dietary pattern).
Extended Data Fig. 3 Comparison of maternal blood metabolomes at three different pregnancy time points from two mother–child cohorts.
Top panels show a Principal Component Analysis (PCA) scoreplot on all metabolites, as well as the selected metabolite scores for the COPSAC2010 vs VDAART 10-18 weeks (left) and COPSAC2010 vs VDAART 32-38 weeks (right). Bottom panels show the relative variation per metabolite computed by the ratio of sums of squares (SSQtime / SSQresidual) from a one-way anova model with Time/Cohort at predictor and Comparison of per metabolite standard deviation within cohort relative to 24-week gestation pregnancy time point from COPSAC2010 for the COPSAC2010 vs VDAART 10-18 weeks (left) and COPSAC2010 vs VDAART 32-38 weeks (right).
Extended Data Fig. 4 Linear regression associations between pregnancy dietary intake and western dietary pattern metabolite scores in the VDAART cohort.
Linear regression associations between dietary intake from food frequency questionnaires (FFQs) during pregnancy and Western Dietary Pattern Metabolite Scores (WDP-MS) at two distinct time points (10-18 weeks (n = 775) and 32-38 weeks (n = 780)) in the VDAART cohort. The depicted associations, based on the VDAART cohort, were assessed using COPSAC2010 cohort-trained models that shared overlapping metabolites. Positive and negative associations are represented by colour coding, with confidence intervals reflecting the uncertainty of the estimates. Bar plots represent model estimates with error bars indicating 95% confidence limits. Adjustments were not made for multiple comparisons.
Extended Data Fig. 5 Metabolites associated with a western dietary pattern and their mediation of ADHD diagnosis in the VDAART cohort.
Metabolites associated with a Western dietary pattern at VDAART gestational time points (10-18 weeks and 32-38 weeks), based on models from the COPSAC2010 cohort. The selected metabolite scores are depicted by bars, distinguished by their metabolic pathway. Striped bars indicate metabolites that mediate the association with ADHD Diagnosis in COPSAC2010, while solid bars signify non-mediating metabolites. The directionality of the bars represents the positive or negative metabolite score. Metabolite scores from VDAART are colour-coded for each time point: 10-18 weeks (green) and 32-38 weeks (purple).
Extended Data Fig. 6 Comparative analysis of metabolomic data across newborn dried blood spots from the COPSAC2010 and COPSAC2000 cohorts.
Comparative analysis of metabolomic data across newborn dried blood spots from the COPSAC2010 and COPSAC2000 mother–child cohorts. Principal Component Analysis (PCA) plots illustrate the distribution and separation of metabolomic data between cohorts. Panels A–C represent overlapping metabolomes used in our analysis (n = 951, n = 774, n = 626), showcasing subsets of metabolites selected based on varying degrees of correlation and distributional similarity between cohorts. A: displays the PCA for metabolites with correlations greater than 0.4 (n = 951), B: Correlations greater than 0.6 (n = 774), and C: Metabolites with a correlation greater than 0.6 passing the two-sample Kolmogorov-Smirnov test with a threshold of >=0.05 (n = 626).
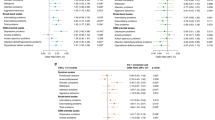
Extended Data Fig. 7 Modulation of the western dietary pattern, stratified by child sex, on neurodevelopmental outcomes.
Odds ratio estimates of ADHD (A) and autism diagnoses (B) based on interactions of the Western dietary pattern, maternal pre-pregnancy BMI (split at median value 23.7), and child’s polygenic risk score (PRS) (median split) for ADHD and autism, stratified by child sex. Linear regression estimates for ADHD (C) and autism symptom loads (D) based on the Western dietary pattern, considering tertiles of maternal pre-pregnancy BMI ( < 22.2, 22.2-25.4, >25.4) and child’s PRS for ADHD and autism, stratified by child sex. Stars represent significance levels: * indicates p < 0.05, ** indicates p < 0.01, and *** indicates p < 0.001, with “NS” denoting non-significant results (p ≥ 0.05). Further details, including the individual associations of these modulating factors, can be found in Supplementary Table S11. Adjustments were not made for multiple comparisons.
Extended Data Fig. 8 Modulation of the western dietary pattern metabolite score on neurodevelopmental outcomes in COPSAC2010 cohort.
Odds ratio estimates for ADHD (A) and autism diagnoses (B) based on interactions of the Western dietary pattern metabolite score, maternal pre-pregnancy BMI (split at median value 23.7), and child’s polygenic risk score (PRS) (median split) for ADHD and autism. Linear regression estimates for ADHD (C) and autism (D) symptom loads are based on the Western dietary pattern metabolite score, considering tertiles of maternal pre-pregnancy BMI and child’s PRS for ADHD and autism. Stars represent significance levels: * indicates p < 0.05, ** indicates p < 0.01, and *** indicates p < 0.001, with “NS” denoting non-significant results (p ≥ 0.05). Further details, including the individual associations of these modulating factors, can be found in Supplementary Table S11. Adjustments were not made for multiple comparisons.
Extended Data Fig. 9 The western dietary patterns metabolite scores association with ADHD and autism symptom loads, considering standard clinical classifications of maternal pre-pregnancy BMI.
Panels A and D represent ADHD and autism symptom loads respectively, stratified by low/high genetic risk (median cut). Panels B and E further contextualize these associations based on maternal pre-pregnancy BMI categories. Panels C and F again contextualize these associations by stratifying by child sex (male sex shown). Panels A–C include n = 522, while Panels D–F include n = 523. Data represent model estimates with error bars indicating 95% confidence limits. Adjustments were not made for multiple comparisons.
Extended Data Fig. 10 Study design and validation of the western dietary pattern–neurodevelopmental association across cohorts.
Study design illustrating the discovery and validation of associations between a western dietary pattern during pregnancy and ADHD outcomes. The primary analysis was conducted in the COPSAC2010 mother-child cohort (n = 508), leveraging dietary data from pregnancy food frequency questionnaires (FFQ) and blood metabolomics profiling to derive a western dietary pattern metabolite score. Validation of findings was performed across three independent cohorts—Danish National Birth Cohort (DNBC, n = 59,625), VDAART (n = 656), and COPSAC2000 (n = 348)—utilizing distinct methodologies: FFQ-based dietary pattern analysis in DNBC, maternal metabolomic validation in VDAART, and neonatal dried blood spot (DBS) metabolomics in COPSAC2000.
Supplementary information
Supplementary Information
Supplementary Tables 1–13
Source data
Source Data Figs. 1–4 and Extended Data Figs. 1–10
Source data for figures and extended data figures.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Horner, D., Jepsen, J.R.M., Chawes, B. et al. A western dietary pattern during pregnancy is associated with neurodevelopmental disorders in childhood and adolescence. Nat Metab 7, 586–601 (2025). https://doi.org/10.1038/s42255-025-01230-z
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s42255-025-01230-z
This article is cited by
-
Air pollution-induced proteomic alterations increase the risk of child respiratory infections
Nature Communications (2025)
-
A Gut Microbial Metabolite Alleviates Stress-Induced Neurobehavioral Dysfunction in an Alzheimer’s Disease Model
Molecular Neurobiology (2025)
-
Maternal monosaccharide diets modulate melanocortin-4 receptor signaling and metabolic state in rat offspring
Pharmacological Reports (2025)