Abstract
Ovarian granulosa cell tumors (GCTs) are sex cord stromal tumors that constitute 3–5% of all ovarian cancers. GCTs usually present with an indolent course but there is a high risk of recurrence, which associates with increased mortality, and targeted treatments would be desirable. Anti-Müllerian hormone (AMH), a key factor regulating sexual differentiation of the reproductive organs, has been implicated as a growth inhibitor in ovarian cancer. GCTs and normal granulosa cells produce AMH, but its expression in large GCTs is usually downregulated. Further, as the lack of specific AMH-signaling pathway components leads to GCT development in mice, we hypothesized that AMH inhibits growth of GCTs. Utilizing a large panel of human GCT tissue samples, we found that AMH type I receptors (ALK2, ALK3 and ALK6) and type II receptor (AMHRII), as well as their downstream effectors Smad1/5, are expressed and active in GCTs. AMHRII expression was detected in the vast majority (96%) of GCTs and correlated with AMH mRNA and protein expression. AMH mRNA level was low in large GCTs, confirming previous findings on low-AMH protein expression in large human as well as mouse GCTs. To study the functional role of AMH in this peculiar ovarian cancer, we utilized a human GCT cell line (KGN) and 10 primary GCT cell cultures. We found that the AMH–Smad1/5-signaling pathway was active in these cells, and that exogenous AMH further activated Smad1/5 in KGN cells. Furthermore, AMH treatment reduced the number of KGN cells and primary GCT cells, with increasing amounts of AMH leading to augmented activation of caspase-3 and subsequent apoptosis. All in all, these data support the premise that AMH is a growth inhibitor of GCTs.
Similar content being viewed by others
Main
Granulosa cell tumors (GCTs) are sex cord stromal tumors representing 3–5% of all ovarian cancers, with two distinct subtypes: the rare juvenile and the more common adult subtype (reviewed in Schumer and Cannistra1). Adult GCTs are characterized by a point mutation c.402C → G (codon C134W) in the gene coding for FOXL2,2, 3, 4, 5 a transcription factor crucial for ovarian differentiation and function.6 GCT often presents in an early stage (Ia), and the overall prognosis is favorable. However, recurrences occur in up to 25% of patients,7, 8 presenting even decades after primary diagnosis, and mortality in recurrent disease is high.9 The poor prognosis of recurrent GCTs or those primarily presenting in an advanced stage has warranted the search for new biologically targeted treatment modalities.
Anti-Müllerian hormone (AMH), also referred to as Müllerian inhibiting substance, is a key factor for proper sexual differentiation. In the male fetus, the Sertoli cell-produced AMH induces the regression of the Müllerian duct partially through apoptosis, whereas the lack of AMH in the female fetus allows the development of Müllerian duct derivates (oviduct, uterus, cervix and the upper part of vagina10, 11). Postnatally, AMH produced by the ovarian granulosa cells becomes a regulator of female reproductive function (reviewed in Visser and Themmen12). AMH belongs to the transforming growth factor-β (TGF-β)/bone morphogenic protein (BMP) family of signaling molecules, and exerts its effects by binding to a heterodimeric cell surface receptor complex consisting of type I (ALK2, ALK3 and ALK6) and type II (AMHRII) receptors.13, 14 After binding the ligand, AMHRII acts downstream by phosphorylating Smads 1, 5 and 8.15 The activation leads to altered gene transcription, apoptosis,16 and embyonic regression of the Müllerian duct in the male.14
AMHRII expression has been detected in gynecological cancers, including human GCTs,17, 18 as well as in breast and prostate cancer.19, 20 Ovarian epithelial carcinoma cells, originating from the coelomic epithelium/Müllerian duct, express AMHRII17 and AMHRII positivity is also associated with prolonged overall survival.19 AMH has been indicated as a growth inhibitor of AMHRII-positive ovarian cancer cells in vitro20, 21, 22, 23 and in vivo,24, 25, 26, 27 and this growth-inhibitory effect is characterized by a block in the cell cycle progression and subsequent apoptosis.20, 22 Although AMH has been indicated as a tissue marker for GCTs,28 AMH immunoreactivity in a series of 80 primary GCTs was low or negative in the tumors larger than 10 cm in diameter.29 This suggests that the lack of AMH may give these tumors growth potential, but the role of AMH signaling in human GCTs remains unraveled.
The complex regulation of the TGF-β/BMP signaling relies on the phosphorylation of different Smads by specific ligand–receptor binding (reviewed in Schmierer and Hill30). The TGF-β/BMP signaling can be divided into Smad2/3 activating ligands (TGF-β, activin, and nodal) and Smad1/5/8 activating ligands (BMPs, growth and differentiation factors, and AMH), but a more specific split is downstream of the type I receptors; ALK4, ALK5 and ALK7 activate Smad2/3 whereas ALK1, ALK2, ALK3 and ALK6 activate Smad1/5/8. The balance between these signaling cascade components has been emphasized in GCT pathogenesis. In mice, α-inhibin deficiency leads to overactive activin signaling and development of sex cord stromal tumors of granulosa cell origin,31 but the additional deletion of downstream Smad3 delays tumor formation.32, 33 The loss of the Smad1/5 signaling in mouse granulosa cells leads to overactivity of the TGF-β-type Smad2/3 signaling and formation of aggressive GCTs of the juvenile type.34, 35 Further, deletion of BMP type I receptors ALK3 and ALK6 in mouse granulosa cells leads to GCT development36 putatively through overactivity of the TGF-β pathway, suggesting that the BMP (AMH)-type pathway acts as a tumor suppressor in granulosa cells.
Given these previous data, we now utilized a large tissue sample series,7 a human GCT cell line and primary cell cultures of human GCTs37 to analyze the expression of AMH-signaling components in human GCTs and to test a hypothesis that AMH is a growth inhibitor of human GCTs.
MATERIALS AND METHODS
Human Tissue Samples
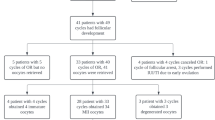
For expression analysis, we utilized the previously characterized29 GCT tissue microarray of quadruple core samples from 80 primary and 12 recurrent GCTs, and freshly frozen samples of 34 GCTs.7, 29, 37, 38 The latter were verified to possess the c.402C → G (p.C134W) mutation in FOXL25 and the mutation frequency of 95% corresponds to other published GCT series.2, 3, 4 All histological diagnoses were carefully reevaluated,29 patient charts were reviewed to obtain clinical data and recurrences were updated as of September 2009.7 For the tumor size, a cutoff of tumor diameter 10 cm was chosen based on earlier GCT studies.39, 40, 41 For controls, we utilized three normal ovarian tissue samples from three pre-menopausal women operated upon for cervical cancer. From July 2008 to December 2010, we obtained 10 fresh tumor samples (7 primary and 3 recurrent GCTs) for primary cell cultures (see below). Informed patient consent was obtained, and the ethical committee of Helsinki University Central Hospital and the National Supervisory Authority for Welfare and Health in Finland approved the study.
mRNA and Protein Isolation and Expression Analyses
RNA and protein were extracted from tissue and cell cultures with Nucleospin RNA/Protein kit (#740 933.250, Macherey-Nagel, Düren, Germany) and the RNA samples were purified with RNA purification kit (Nucleospin RNA Clean up kit, #740 948.50). Semiquantitative PCR was carried out as described.42 Quantitative PCR was performed using SYBR GREEN according to instructions (Applied Biosystems, Foster City, CA, USA) with an ABI PRISM 7700 detector (Applied Biosystems). Primers listed in Table 1 were designed with IDT SciTools software or as previously described.43, 44 Western blotting of the protein samples was performed as described38 with antibodies and dilutions listed in Table 1.
Immunohistochemistry
Immunohistochemical staining of GCT tissue microarray and normal ovarian samples was performed as described29 with primary antibodies in dilutions listed in Table 1; the monoclonal AMHRII-12G4 antibody was kindly provided by Dr Isabelle Navarro-Teulon (INSERM U896, Montpellier, France).18 The stainings for all the antigens were classified into two groups based on the number of positive cells and intensity of staining: high representing >20% of positive cells with intermediary or strong intensity (comparable to the staining of the normal granulosa cells for all the antigens studied), and low representing <20% of positive cells or very low intensity or negative even if detected in 100% of the cells. Two researchers (MA and AF) independently performed the evaluation, and disagreements were resolved by a joint review.
Cell Cultures and Treatments
The KGN cell line (kindly provided by Dr T Yanase, Kyushu University, Fukuoka, Japan) was cultured as previously described in Dulbecco’s modified Eagle’s medium and Ham’s F-12 medium containing 10% fetal bovine serum.45 The primary GCT cell cultures were established as described;37 in brief, the fresh tumor tissue was mechanically minced and treated with 0.5% collagenase (Sigma-Aldrich®, St Louis, MO, USA), filtered through a 140-μm mesh, and the single cells were plated in the KGN culture medium. All the used primary GCT cells harbored the c.402CG mutation in FOXL2. The primary culture and KGN cells were stained with primary antibodies listed in Table 1 as described.37
Recombinant human AMH was purified and tested for bioactivity as described.25 The cells were treated with AMH at different concentrations in 10% female fetal calf serum (FFCS; ie, no AMH in the control medium) for 1–10 days, followed by MTT, bromodeoxyuridine (BrdU), caspase activation, and DAPI staining assays (see below), or protein extraction. The used AMH concentrations (0–25 μg/ml or 0–179 nm) were similar to those used in epithelial ovarian carcinoma cell studies and in AMH bioactivity assays utilizing this particular AMH stock20, 22, 46, 47, 48, 49 that is only partially cleaved (ie, activated) compared with fully cleaved AMH stocks that were recently established.50, 51 The Kd of AMH binding to AMHRII in ovarian carcinoma cell lines (OVCAR5 and OVCAR8) was calculated to be 10.2 nM and 12 nM, respectively,20, 22 and we estimated the Kd to be similar in this study. AMH levels in the culture medium of the control samples with 10% FFCS were analyzed with sensitive enzyme-linked immunosorbent assay (DSL-10–14400), according to instructions (Beckman Coulter, Webster, TX, USA).
Cell Number and Apoptosis Assays
MTT-based cell growth determination kit (#CGD1, Sigma-Aldrich), Cell Proliferation Reagent WST-1 (Cat. No. 05015944001, Roche Applied Science, Indianapolis, IN, USA), and Bromodeoxyuridine (BrdU) Staining Kit (Invitrogen, Carlsbad, CA, USA) were utilized according to instructions. BrdU-labelling solution was added on treated cells 24 h before the staining, and the proportion of BrdU-positive cells was counted in 2000–3000 cells. Caspase-3/7 activation was measured using Caspase-Glo® 3/7 assays (Promega, Madison, WI, USA) following the instructions, and/or western blotting for cleaved caspase-3. DAPI staining was performed as described.37
Data Analysis and Statistics
The immunohistochemical expression data and the clinicopathological data were analyzed with Contingency tabling (2 × 2) and χ2 or Fisher’s exact tests. RNA expression levels and clinicopathological data were analyzed with one-way ANOVA and Student’s t-test when appropriate. The Kaplan–Meier analysis was performed according to the methodology.7 The cell culture data were analyzed with one-way ANOVA. P<0.05 was considered significant. The analyses were carried out with JMP® 7.0.1 (SAS Institute, Cary, NC, USA) software.
RESULTS
AMH, AMHRII, and Their Downstream Effectors are Expressed in Human Granulosa Cell Tumors
The transcript of AMH type II receptor (AMHRII) was detected in 30/30 of primary GCT, and the type I receptors were also readily detected: ALK2 in 29/30, ALK3 in 30/30, and ALK6 in 26/30 GCTs were analyzed (Figure 1a). Quantitative PCR revealed varying expression levels of AMH and AMHRII, and expression of the ligand and the receptor mRNA correlated in the 28 tumors analyzed (Figure 1b). In accordance with our previous results on the AMH protein levels in human GCTs,29 AMH mRNA levels inversely correlated with the tumor size (Figure 1c).
mRNA expression of AMH, AMHRII, ALK2, ALK3, ALK6, Smad1, and Smad5 in GCTs. Thirty GCTs (recurrent GCTs nos 21, 24–26) were analyzed by PCR for the expressions of AMHRII, ALK2, ALK3, ALK6, Smad1, and Smad5 mRNAs (a). AMH and AMHRII mRNA expressions were quantified relative to actin by quantitative PCR in 28 (22 primary and 6 recurrent) GCTs (b, c). AMH mRNA expression correlated positively to AMHRII mRNA expression (b) and negatively to tumor size (c) (P=0.0391).
Tissue microarray analysis revealed that AMHRII expression was high in 45/79 (57%) primary tumor samples (Figure 2 and Table 2) and in 7/12 (58%) recurrent tumor samples (data not shown), compatible with the immunostaining in normal reference tissue; western blotting also revealed AMHRII expression in two normal ovarian lysates and in the 34/34 GCTs analyzed, of which four were recurrent tumors (data not shown). AMHRII expression was detected in all of the 10 GCT primary cell cultures tested and in the corresponding KGN cells (Figure 2). Given that AMHRII immunostaining was totally negative in only three (4%) of the 79 tumors, the results altogether suggest that AMHRII expression is characteristic for GCTs. AMHRII expression correlated with AMH expression at the protein level (Table 2). AMHRII mRNA or protein expression did not correlate with any analyzed clinicopathological parameters of the primary tumors, ie, age and menopause status of the patient at diagnosis, clinical stage, size of the tumor, tumor subtype, nuclear atypia, mitotic index, and risk of recurrence.7, 29 We also employed Kaplan–Meier analysis on the 79 primary GCTs for the correlation of AMHRII expression and recurrence-free survival, and found similar recurrence probability in tumors with high or low expression of AMHRII (data not shown), in contrast to earlier findings in ovarian cancer.19
Immunostaining of AMHRII, Smad1, Smad5, and phospho-Smad1/5 in GCTs and normal reference granulosa cells. Examples of expression in granulosa cell tumor tissue (rows 2–4), and in primary GCT and KGN cell cultures (rows 5–6). Row 3 (b′, g′, l′, q′) shows higher magnification images of the tumor tissue in row 2. Tissue slides or fixed cell specimens were subjected to immunostaining for the antigens, with 3,3-diaminobenzidine being used to visualize the positive staining as brown; nuclei were counterstained with hematoxylin. Normal human ovaries were stained as controls. Asterisks indicate normal granulosa cells in the lining of an antral follicle in row 1. Scalebars=200 μm.
Expression of Phosphorylated Smad1/5 Associates With AMHRII and AMH Expression in GCTs
In mice, lack of Smad1 and Smad5 in granulosa cells leads to the development of GCTs resembling the juvenile subtype of the tumor.34, 35 In our series of adult human GCTs, transcripts for Smad1 and Smad5 were detected in 30/30 samples studied (Figure 1), and protein expression levels of Smad1 and Smad5 correlated positively in the 75 primary tumors (Figure 2 and Table 2). Moreover, immunostaining of phosphorylated-Smad1/5 (phospho-Smad1/5) (Figure 2) strongly correlated with Smad5 expression pattern (Table 2), suggesting that Smad5 is preferably in the active and phosphorylated state in GCTs. Smad1 and Smad5 expression patterns associated with AMH expression pattern and the phospho-Smad1/5 expression pattern associated with AMH and AMHRII expression patterns (Table 2). Similar to AMHRII expression, none of the Smad protein expression patterns, however, correlated with the clinicopathological parameters listed above.
Smad1, Smad5, and phospho-Smad1/5 protein expressions were evident in cultured primary GCT and KGN cells (Figure 2 and Figure 4a). In addition, these GCT cells produced detectable levels of AMH into the culture medium so that average AMH levels in the cell culture medium (with 10% FFCS) were 0.68 ng/ml (range 0.41–1.06 ng/ml) for KGN, 1–3 days after medium change, and 0.77 ng/ml (range 0.43–1.71 ng/ml) for primary tumor cultures (n=5), 1–5 days after medium change. Based on these data, Smad5 signaling can be presumed to be actively functioning in the AMH- and AMHRII-expressing GCTs. Coupled with the cell culture data, this suggests an auto/paracrine regulatory loop of AMH–AMHRII signaling in the GCT microenvironment.
AMH Treatment of Cultured GCT Cells Reduces the Number of Tumor Cells
Given the expression patterns of AMH and its signaling components in GCTs, we tested the effect of AMH on the number of cultured GCT cells by MTT-based assays. We found that AMH (5–25 μg/ml) decreased the number of viable KGN cells relative to control (AMH 0 μg/ml) by 25–38% and by 24–34% after 3 days and 10 days incubation, respectively (Figure 3a). In the untreated wells (AMH 0 μg/ml), the cell number had roughly doubled or tripled from 3 to 10 days incubation. While the cell number decreased relative to control, AMH had, however, no significant effect on the proliferation rate of KGN cells as analyzed by BrdU analysis (Figure 3b). Similar results were obtained in primary GCT cells from two cases; AMH (5–25 μg/ml) reduced the cell number by 36–43% during 2 days incubation (case 1), or by 29–39% during 4 days incubation (case 2) (Figure 3c). With deprivation in 1% FFCS as a control, the reduction was 28% in both cases.
Cell number and proliferation assays on KGN (a, b) and two primary cell cultures (c) after AMH treatments. Cells were treated with indicated doses of AMH for 1–10 days (d) before MTT-based or BrdU incorporation assays. 10% FFCS was used as a control, and 1% FFCS as a control for growth factor deprivation. (a) MTT data on the relative number of viable KGN cells is presented as mean±s.d. of three independent experiments performed in triplicate; the relative cell numbers are shown compared with control. (b) The proportion (%) of proliferative, ie, BrdU-positive, cells is presented as mean±s.d. of three independent experiments; total of 2000–3000 cells was counted for each dose and incubation period. (c) MTT data on the number of viable cells of two primary cell cultures are presented as mean±s.d. of one independent experiment performed in triplicate, treated for 2 days (case 1, white columns) or for 4 days (case 2, black columns). Asterisks indicate significant difference with P<0.05 when compared with control experiment (AMH 0 μg/ml).
AMH Activates Smad1/5 and Also Induces Apoptosis in KGN Cells
AMH treatment increased the phospho-Smad1/5 but not Smad1 or Smad5 levels, and activated caspase-3, a marker of apoptosis induction, during 1 day and 3 days incubation in KGN cells (Figure 4a). During AMH treatments, expression of B-cell lymphoma 2 (Bcl2) and cyclinD2, control proteins related to granulosa cell apoptosis and proliferation regulation (respectively), remained stable (Figure 4a). The level of caspase activation was quantified with caspase-3/7 activation assay (Figure 4b), showing a 2.8–7.7-fold activation during the first day of AMH treatments, whereas after 2 or 3 days a prolonged caspase activation was seen only with the largest AMH dose (25 μg/ml). Compatible with the caspase activation, the number of apoptotic cells increased following 1 day and 3 days of AMH treatments (Figure 4c).
AMH activates Smad1/5, caspase-3, and apoptosis in KGN cells. (a) Representative western blotting results of an experiment performed in triplicate, showing the effect of increasing AMH doses on protein levels of Smad1/5, cleaved (activated) caspase-3, Bcl2, cyclinD2, and β-actin as an internal control. (b) Caspase-3/7 activation assay following increasing doses of AMH for 1–3 days, presenting fold activation relative to control. (c) Number of apoptotic cells analyzed by nuclear morphology following DAPI staining. In b and c the data are presented as mean±s.d. of three independent experiments performed in triplicate. Asterisks in b and c indicate significant difference with P<0.05 when compared with control experiment (AMH 0 μg/ml).
AMH Induces Apoptosis in Primary GCT Cells
Similar to experiments with the KGN cell line, we tested the response of AMH treatment in 10 primary GCT cell cultures, established from fresh tumor tissue (Figure 5). We found caspase-3 activation by western blot or caspase-3/7 assay in 10/10 tumors analyzed, as well as apoptosis activation by DAPI in 5/5 tumors analyzed. Owing to limited number of the recovered primary tumor cells, we were unable to study whether exogenous AMH caused Smad1/5 activation in these primary cell cultures. In cultures from both primary and recurrent primary GCTs, caspase-3 cleavage was increased at 2 days and 5 days (Figure 5a), without a clear effect on Bcl2 and cyclinD2 expression. In addition, apoptosis was detected morphologically by DAPI analysis in both GCT cases (Figures 5b-d and f-h), and prolonged apoptotic activity was seen even after 5 days incubation with the smallest AMH dose (5 μg/ml).
Activation of apoptosis in in vitro GCT cultures by AMH. Two representative cases are presented, data on one recurrent GCT (a–d) and one primary GCT (e–h). Caspase-3 activation was evaluated by western blot (a, e), coupled with DAPI analysis of apoptotic cells for both cases (b–d and f–h); arrows indicate apoptotic cells. Reliable effect on Bcl2 or cyclinD2 levels could not be detected. Single experiments on individual tumors were carried out.
DISCUSSION
The molecular pathogenesis of the GCTs of the ovary has only recently started to get unraveled, along with the discovery of a disease-specific point mutation in a single gene coding for transcription factor FOXL2,2, 3, 4, 5 crucial for normal granulosa cell function.52 Accordingly, several previous studies utilizing human GCT tissue series (reviewed in Fuller and Chu53) have focused on genes and factors involved in the normal granulosa cell function.5, 7, 29, 54 We now describe the expression patterns of the AMH-signaling pathway components in GCT in detail and show evidence for AMH being a growth inhibitor for GCT. Previously, AMHRII positivity and AMH responsiveness have been reported in ovarian cancers originating from the Müllerian duct derivatives.20, 21, 22 In a series of five GCTs, AMHRII expression levels were higher than in other ovarian cancers.17 In in vitro assays of GCTs, we now find that AMH treatment reduces the cell number by activating apoptosis. Previous studies show that while AMH inhibits cell cycle and proliferation, it also induces apoptosis on ovarian carcinoma cell lines.20, 22 In this study, the inhibitory effect on the proliferation rate of GCT cells was undetected, arguing that AMH functions as a GCT growth inhibitor by sensitizing the tumor cells to apoptosis.
We here find that the AMH–Smad1/5 signaling is active and correlates with AMH and AMHRII expression in adult GCTs. The GCT cultures produced AMH into the culture medium, and exogenous, recombinant AMH further activated Smad1/5 in KGN cells. Mice studies show that loss of Smad1/5 in granulosa cells leads to Smad2/3 overactivity and development of aggressive GCTs resembling the human GCT of the juvenile type;34, 35 in adult human GCTs expression of both Smad2 and Smad3 is evident (our unpublished data). The deletion of the BMP/AMH type I receptors ALK3 and ALK6 in mouse granulosa cells leads to the development of more indolent GCTs, with delayed tumor formation and less metastases compared with the Smad1/5 knockout mice.36 In these tumors ALK2 expression is increased, and the alleviation of tumor progression is proposed to be due to ALK2-mediated Smad1/5 activation. Of note, AMH binds most strongly to ALK2;55 in the granulosa cells with ALK3/6 deletion,36 AMH may still be able to suppress GCT formation through ALK2, leading to decelerated tumorigenesis compared with the Smad1/5 knockout mice. In adult human GCTs, we found that the canonical AMH pathway, including all the type I and II receptors and Smad1/5, is present and can be activated by AMH. Further supporting the suppressive role of AMH, we found an inverse correlation of AMH expression level with the tumor size at the mRNA level. More specifically, AMH expression is low in large human and murine GCTs29, 56 both at mRNA and protein level. Taken together, the lowered AMH levels in large human adult GCTs may lead to decreased activation of the suppressive BMP pathway, which may be one of the reasons for malignant growth of human granulosa cells.34, 35, 36
In human GCTs, serum AMH levels have been shown to positively correlate with the tumor size, ie, the bigger the tumor the higher the serum AMH levels.57 While there is a controversy of high serum but low tissue AMH in the large human GCTs, it can be presumed that in a subset of tumors of certain size the AMH level in the microenvironment may be lower than required to sustain the growth inhibition of granulosa cells. Features of this GCT subgroup, thus, closely reflect the highly proliferating granulosa cells of large antral follicles, which exhibit downregulated AMH expression,58 suggesting a positive selection process of these cells with increased growth potential.
Utilizing primary GCT cultures and a large series of human adult GCTs, we here demonstrate that the key components of AMH signaling are expressed in these tumors, and that exogenous AMH is able to inhibit growth of GCT cells through apoptosis. Activation of apoptosis and/or inhibition of cell cycle by AMH in ovarian carcinomas may enhance the effectiveness of chemotherapeutics,27, 59 and lead to less toxicity and increased tolerance to chemotherapy. Further studies utilizing mouse models for human GCT are, however, needed to ultimately address the implications of AMH as a supplementary treatment modality for GCTs. There are several issues to be resolved before clinical use of AMH can be established. Recent results show that endogenous and exogenous AMH needs to be cleaved to attain full activity upon binding to the type II receptor.48, 50, 51, 60 The AMH reagent used in this and earlier studies24, 25, 26, 27, 61 is only partially cleaved. The production of purified, fully cleaved AMH has been achieved only recently,51 and with this AMH one would need only 1:1000 of the dose compared with partially cleaved AMH. Targeting AMHRII with activating antibodies62 or small molecule agonists23, 59 presents another attractive option for supplementary treatment of AMHRII-positive advanced or recurrent GCTs. Nevertheless, the observed activation of apoptosis in GCTs may not necessarily involve AMHRII, given that the doses used in this study are more robust than implicated by the reported Kd for AMH to AMHRII.20, 22 Future studies should clarify how AMH affects the gene expression pattern and function of normal vs malignant granulosa cells of the ovary.
References
Schumer ST, Cannistra SA . Granulosa cell tumor of the ovary. J Clin Oncol 2003;21:1180–1189.
Shah SP, Kobel M, Senz J, et al. Mutation of FOXL2 in granulosa-cell tumors of the ovary. N Engl J Med 2009;360:2719–2729.
Kim MS, Hur SY, Yoo NJ, et al. Mutational analysis of FOXL2 codon 134 in granulosa cell tumour of ovary and other human cancers. J Pathol 2010;221:147–152.
Kim T, Sung CO, Song SY, et al. FOXL2 mutation in granulosa-cell tumours of the ovary. Histopathology 2010;56:408–410.
Jamieson S, Butzow R, Andersson N, et al. The FOXL2 C134W mutation is characteristic of adult granulosa cell tumors of the ovary. Mod Pathol 2010;23:1477–1485.
Uhlenhaut NH, Jakob S, Anlag K, et al. Somatic sex reprogramming of adult ovaries to testes by FOXL2 ablation. Cell 2009;139:1130–1142.
Farkkila A, Anttonen M, Pociuviene J, et al. Vascular endothelial growth factor (VEGF) and its receptor VEGFR-2 are highly expressed in ovarian granulosa cell tumors. Eur J Endocrinol 2011;164:115–122.
Cronje HS, Niemand I, Bam RH, et al. Review of the granulosa-theca cell tumors from the emil Novak ovarian tumor registry. Am J Obstet Gynecol 1999;180:323–327.
Fujimoto T, Sakuragi N, Okuyama K, et al. Histopathological prognostic factors of adult granulosa cell tumors of the ovary. Acta Obstet Gynecol Scand 2001;80:1069–1074.
Munsterberg A, Lovell-Badge R . Expression of the mouse anti-mullerian hormone gene suggests a role in both male and female sexual differentiation. Development 1991;113:613–624.
Xavier F, Allard S . Anti-Mullerian hormone, beta-catenin and Mullerian duct regression. Mol Cell Endocrinol 2003;211:115–121.
Visser JA, Themmen AP . Anti-Mullerian hormone and folliculogenesis. Mol Cell Endocrinol 2005;234:81–86.
Belville C, Jamin SP, Picard JY, et al. Role of type I receptors for anti-Mullerian hormone in the SMAT-1 Sertoli cell line. Oncogene 2005;24:4984–4992.
Visser JA . AMH signaling: from receptor to target gene. Mol Cell Endocrinol 2003;211:65–73.
Tran TT, Segev DL, Gupta V, et al. Mullerian inhibiting substance regulates androgen-induced gene expression and growth in prostate cancer cells through a nuclear factor-kappaB-dependent Smad-independent mechanism. Mol Endocrinol 2006;20:2382–2391.
Catlin EA, Tonnu VC, Ebb RG, et al. Mullerian inhibiting substance inhibits branching morphogenesis and induces apoptosis in fetal rat lung. Endocrinology 1997;138:790–796.
Song JY, Chen KY, Kim SY, et al. The expression of Mullerian inhibiting substance/anti-Mullerian hormone type II receptor protein and mRNA in benign, borderline and malignant ovarian neoplasia. Int J Oncol 2009;34:1583–1591.
Salhi I, Cambon-Roques S, Lamarre I, et al. The anti-Mullerian hormone type II receptor: insights into the binding domains recognized by a monoclonal antibody and the natural ligand. Biochem J 2004;379:785–793.
Bakkum-Gamez JN, Aletti G, Lewis KA, et al. Mullerian inhibiting substance type II receptor (MISIIR): a novel, tissue-specific target expressed by gynecologic cancers. Gynecol Oncol 2008;108:141–148.
Masiakos PT, MacLaughlin DT, Maheswaran S, et al. Human ovarian cancer, cell lines, and primary ascites cells express the human Mullerian inhibiting substance (MIS) type II receptor, bind, and are responsive to MIS. Clin Cancer Res 1999;5:3488–3499.
Chin TW, Parry RL, Donahoe PK . Human mullerian inhibiting substance inhibits tumor growth in vitro and in vivo. Cancer Res 1991;51:2101–2106.
Ha TU, Segev DL, Barbie D, et al. Mullerian inhibiting substance inhibits ovarian cell growth through an Rb-independent mechanism. J Biol Chem 2000;275:37101–37109.
Wei X, Dombkowski D, Meirelles K, et al. Mullerian inhibiting substance preferentially inhibits stem/progenitors in human ovarian cancer cell lines compared with chemotherapeutics. Proc Natl Acad Sci USA 2010;107:18874–18879.
Stephen AE, Masiakos PT, Segev DL, et al. Tissue-engineered cells producing complex recombinant proteins inhibit ovarian cancer in vivo. Proc Natl Acad Sci USA 2001;98:3214–3219.
Stephen AE, Pearsall LA, Christian BP, et al. Highly purified Mullerian inhibiting substance inhibits human ovarian cancer in vivo. Clin Cancer Res 2002;8:2640–2646.
Pieretti-Vanmarcke R, Donahoe PK, Szotek P, et al. Recombinant human Mullerian inhibiting substance inhibits long-term growth of MIS type II receptor-directed transgenic mouse ovarian cancers in vivo. Clin Cancer Res 2006;12:1593–1598.
Pieretti-Vanmarcke R, Donahoe PK, Pearsall LA, et al. Mullerian inhibiting substance enhances subclinical doses of chemotherapeutic agents to inhibit human and mouse ovarian cancer. Proc Natl Acad Sci USA 2006;103:17426–17431.
Rey R, Sabourin JC, Venara M, et al. Anti-Mullerian hormone is a specific marker of sertoli- and granulosa-cell origin in gonadal tumors. Hum Pathol 2000;31:1202–1208.
Anttonen M, Unkila-Kallio L, Leminen A, et al. High GATA-4 expression associates with aggressive behavior, whereas low anti-Mullerian hormone expression associates with growth potential of ovarian granulosa cell tumors. J Clin Endocrinol Metab 2005;90:6529–6535.
Schmierer B, Hill CS . TGFbeta-SMAD signal transduction: molecular specificity and functional flexibility. Nat Rev Mol Cell Biol 2007;8:970–982.
Matzuk MM, Finegold MJ, Su JG, et al. Alpha-inhibin is a tumour-suppressor gene with gonadal specificity in mice. Nature 1992;360:313–319.
Li Q, Graff JM, O’Connor AE, et al. SMAD3 regulates gonadal tumorigenesis. Mol Endocrinol 2007;21:2472–2486.
Li Q, Kumar R, Underwood K, et al. Prevention of cachexia-like syndrome development and reduction of tumor progression in inhibin-deficient mice following administration of a chimeric activin receptor type II-murine Fc protein. Mol Hum Reprod 2007;13:675–683.
Pangas SA, Li X, Umans L, et al. Conditional deletion of Smad1 and Smad5 in somatic cells of male and female gonads leads to metastatic tumor development in mice. Mol Cell Biol 2008;28:248–257.
Middlebrook BS, Eldin K, Li X, et al. Smad1-Smad5 ovarian conditional knockout mice develop a disease profile similar to the juvenile form of human granulosa cell tumors. Endocrinology 2009;150:5208–5217.
Edson MA, Nalam RL, Clementi C, et al. Granulosa cell-expressed BMPR1A and BMPR1B have unique functions in regulating fertility but act redundantly to suppress ovarian tumor development. Mol Endocrinol 2010;24:1251–1266.
Kyronlahti A, Kauppinen M, Lind E, et al. GATA4 protects granulosa cell tumors from TRAIL-induced apoptosis. Endocr Relat Cancer 2010;17:709–717.
Kyronlahti A, Ramo M, Tamminen M, et al. GATA-4 regulates Bcl-2 expression in ovarian granulosa cell tumors. Endocrinology 2008;149:5635–5642.
Chan JK, Zhang M, Kaleb V, et al. Prognostic factors responsible for survival in sex cord stromal tumors of the ovary--a multivariate analysis. Gynecol Oncol 2005;96:204–209.
Nosov V, Silva I, Tavassoli F, et al. Predictors of recurrence of ovarian granulosa cell tumors. Int J Gynecol Cancer 2009;19:628–633.
Ranganath R, Sridevi V, Shirley SS, et al. Clinical and pathologic prognostic factors in adult granulosa cell tumors of the ovary. Int J Gynecol Cancer 2008;18:929–933.
Salonen J, Butzow R, Palvimo JJ, et al. Oestrogen receptors and small nuclear ring finger protein 4 (RNF4) in malignant ovarian germ cell tumours. Mol Cell Endocrinol 2009;307:205–210.
Catteau-Jonard S, Jamin SP, Leclerc A, et al. Anti-Mullerian hormone, its receptor, FSH receptor, and androgen receptor genes are overexpressed by granulosa cells from stimulated follicles in women with polycystic ovary syndrome. J Clin Endocrinol Metab 2008;93:4456–4461.
Reisenauer A, Eickelberg O, Wille A, et al. Increased carcinogenic potential of myeloid tumor cells induced by aberrant TGF-beta1-signaling and upregulation of cathepsin B. Biol Chem 2007;388:639–650.
Nishi Y, Yanase T, Mu Y, et al. Establishment and characterization of a steroidogenic human granulosa-like tumor cell line, KGN, that expresses functional follicle-stimulating hormone receptor. Endocrinology 2001;142:437–445.
Donahoe PK, Ito Y, Hendren III WH . A graded organ culture assay for the detection of Mullerian inhibiting substance. J Surg Res 1977;23:141–148.
MacLaughlin DT, Epstein J, Donahoe PK . Bioassay, purification, cloning, and expression of Mullerian inhibiting substance. Methods Enzymol 1991;198:358–369.
MacLaughlin DT, Hudson PL, Graciano AL, et al. Mullerian duct regression and antiproliferative bioactivities of mullerian inhibiting substance reside in its carboxy-terminal domain. Endocrinology 1992;131:291–296.
Ragin RC, Donahoe PK, Kenneally MK, et al. Human mullerian inhibiting substance: enhanced purification imparts biochemical stability and restores antiproliferative effects. Protein Expr Purif 1992;3:236–245.
di Clemente N, Jamin SP, Lugovskoy A, et al. Processing of anti-Mullerian hormone regulates receptor activation by a mechanism distinct from TGF-{beta}. Mol Endocrinol 2010;24:2193–2206.
Papakostas TD, Pieretti-Vanmarcke R, Nicolaou F, et al. Development of an efficiently cleaved, bioactive, highly pure FLAG-tagged recombinant human Mullerian inhibiting substance. Protein Expr Purif 2010;70:32–38.
Uhlenhaut NH, Treier M . Foxl2 function in ovarian development. Mol Genet Metab 2006;88:225–234.
Fuller PJ, Chu S . Signalling pathways in the molecular pathogenesis of ovarian granulosa cell tumours. Trends Endocrinol Metab 2004;15:122–128.
Schmidt M, Kammerer U, Segerer S, et al. Glucose metabolism and angiogenesis in granulosa cell tumors of the ovary: activation of Akt, expression of M2PK, TKTL1 and VEGF. Eur J Obstet Gynecol Reprod Biol 2008;139:72–78.
Visser JA, Olaso R, Verhoef-Post M, et al. The serine/threonine transmembrane receptor ALK2 mediates Mullerian inhibiting substance signaling. Mol Endocrinol 2001;15:936–945.
Dutertre M, Gouedard L, Xavier F, et al. Ovarian granulosa cell tumors express a functional membrane receptor for anti-Mullerian hormone in transgenic mice. Endocrinology 2001;142:4040–4046.
Chang HL, Pahlavan N, Halpern EF, et al. Serum Mullerian inhibiting substance/anti-Mullerian hormone levels in patients with adult granulosa cell tumors directly correlate with aggregate tumor mass as determined by pathology or radiology. Gynecol Oncol 2009;114:57–60.
Weenen C, Laven JS, Von Bergh AR, et al. Anti-Mullerian hormone expression pattern in the human ovary: potential implications for initial and cyclic follicle recruitment. Mol Hum Reprod 2004;10:77–83.
Renlund N, Pieretti-Vanmarcke R, O’Neill FH, et al. c-Jun N-terminal kinase inhibitor II (SP600125) activates Mullerian inhibiting substance type II receptor-mediated signal transduction. Endocrinology 2008;149:108–115.
Pepinsky RB, Sinclair LK, Chow EP, et al. Proteolytic processing of Mullerian inhibiting substance produces a transforming growth factor-beta-like fragment. J Biol Chem 1988;263:18961–18964.
Donahoe PK, Clarke T, Teixeira J, et al. Enhanced purification and production of Mullerian inhibiting substance for therapeutic applications. Mol Cell Endocrinol 2003;211:37–42.
Yuan QA, Simmons HH, Robinson MK, et al. Development of engineered antibodies specific for the Mullerian inhibiting substance type II receptor: a promising candidate for targeted therapy of ovarian cancer. Mol Cancer Ther 2006;5:2096–2105.
Acknowledgements
We thank all the gynecologists and operation room staff for supporting the patient recruitment and tissue sample collection for the entire GCT project. We also thank Taru Jokinen and Teija Karkkulainen for excellent assistance, and Dr T Yanase and Dr I Navarro-Teulon for kindly providing the KGN cell line and the AMHRII antibody, respectively. This study was supported by grants from the Academy of Finland (to MA and MH), the National Clinical Graduate School (to AF), Helsinki University Central Hospital Research Funds (to MA, LU-K, RB, and MH), the Sigrid Juselius Foundation (to MH), and Finnish Cancer Organizations (to MH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Expression of anti-Müllerian hormone type II receptor is characteristic of human ovarian granulosa cell tumor cells, and its signaling pathway is activated in this cancer. A unique cell model reveals that anti-Müllerian hormone inhibits tumor growth, which raises the possibility of new treatments for patients.
Rights and permissions
About this article
Cite this article
Anttonen, M., Färkkilä, A., Tauriala, H. et al. Anti-Müllerian hormone inhibits growth of AMH type II receptor-positive human ovarian granulosa cell tumor cells by activating apoptosis. Lab Invest 91, 1605–1614 (2011). https://doi.org/10.1038/labinvest.2011.116
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/labinvest.2011.116
Keywords
This article is cited by
-
Evaluation of the p53 pathway in polycystic ovarian syndrome pathogenesis and apoptosis enhancement in human granulosa cells through transcriptome data analysis
Scientific Reports (2023)
-
BPA and BPS affect the expression of anti-Mullerian hormone (AMH) and its receptor during bovine oocyte maturation and early embryo development
Reproductive Biology and Endocrinology (2021)
-
Anti-Müllerian hormone (AMH) autocrine signaling promotes survival and proliferation of ovarian cancer cells
Scientific Reports (2021)
-
The molecular mechanism of ovarian granulosa cell tumors
Journal of Ovarian Research (2018)
-
Effect of Anti-Müllerian hormone (AMH) and bone morphogenetic protein 15 (BMP-15) on steroidogenesis in primary-cultured human luteinizing granulosa cells through Smad5 signalling
Journal of Assisted Reproduction and Genetics (2015)